Abstract
OBJECTIVE
We sought to estimate the number of women who will undergo inpatient and outpatient surgery for stress urinary incontinence (SUI) or pelvic organ prolapse (POP) in the United States from 2010 through 2050.
STUDY DESIGN
Using the 2007 Nationwide Inpatient Sample and the 2006 National Survey of Ambulatory Surgery, we calculated the rates for inpatient and outpatient SUI and POP surgery. We applied the surgery rates to the US Census Bureau population projections from 2010 through 2050.
RESULTS
The total number of women who will undergo SUI surgery will increase 47.2% from 210,700 in 2010 to 310,050 in 2050. Similarly, the total number of women who will have surgery for prolapse will increase from 166,000 in 2010 to 245,970 in 2050.
CONCLUSION
If the surgery rates for pelvic floor disorders remain unchanged, the number of surgeries for urinary incontinence and POP will increase substantially over the next 40 years.
Keywords: future predictions, pelvic floor disorders, pelvic organ prolapse, surgery, urinary incontinence
Pelvic floor disorders (PFD), including urinary incontinence (UI) and pelvic organ prolapse (POP), represent a major public health burden given their high prevalence,1 significant impairment of quality of life,2,3 and substantial economic costs.4,5 Surgical management of PFD is common with almost 1 of every 10 women undergoing surgery for UI or prolapse in their lifetime.6 Unfortunately, the risk for reoperation is as high as 30%.
Given the aging population in the United States7 and the fact that PFD are more common in the elderly,1 these conditions will represent an even greater public health burden in the coming years. Over the next 4 decades, the US population is estimated to increase 42% from 310.2 million in 2010 to 439.0 million in 2050,8 with the fastest growing segment of the population being women aged >65 years.9 Using the US Census Bureau population projections, we estimated that the prevalence of symptomatic PFD will increase by 56% from 28.1 million to 43.8 million over the next 40 years.10 Because a substantial portion of women with symptomatic PFD will be managed surgically, the next critical question is how many women will undergo surgery for stress UI (SUI) and POP in the future.
Data regarding the future demand for PFD surgery will be critical to surgeons, including gynecologists, urogynecologists, and urologists, as well as to residency and fellowship training programs. Furthermore, these estimates will inform public health officials and policymakers regarding the potential future disease burden and economic impact of these surgical procedures. Lastly, the potential magnitude of future SUI and POP surgeries may underscore the importance of identifying effective preventive measures and nonsurgical management options. Thus, the objective of this study was to estimate the number of women who currently undergo both inpatient and outpatient surgeries for SUI and POP in the United States and to predict these estimates into the future to 2050.
Materials and Methods
Data sources
To estimate the number of women who will undergo surgery for SUI and POP in the future, we utilized 2 critical components of data: (1) inpatient and outpatient surgery rates for SUI and POP; and (2) US population growth estimates. To be as comprehensive as possible, we evaluated both inpatient as well as outpatient procedures. Inpatient data were based on the 2007 Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality.11 The 2007 NIS represents the largest publicly available database of hospital discharges in the United States and provides weights to account for its complex sampling design to calculate national estimates.
Outpatient data were based on the 2006 National Survey of Ambulatory Surgery (NSAS), National Center for Health Statistics, Centers for Disease Control and Prevention.12,13 The NSAS was conducted annually from 1994 through 1996 and then again in 2006 and includes surgical procedures performed on an outpatient basis in a hospital-based or freestanding ambulatory surgery center but does not include physician office-based procedures.
The second critical component was the US population projections, which is provided by Census Bureau Population Projections Program.14 The 2008 projections were based on the 2000 census and were produced using a cohort-component method.15 These projections are based on key assumptions for future births, deaths, and net international migration, and they estimate population growth from 2010 through 2050 by age, sex, race, and ethnicity. Because the primary set of population projections are based on middle estimates for all 3 parameters (fertility rate, life expectancy, and net immigration), these data are also referred to as the middle series.16 The middle series predicts that the total population will grow from 310.2 million in 2010 to 439.0 million in 2050.
This study was exempt from institutional review board review because only publicly available data were analyzed.
Analysis
The first step in the analysis was to determine the annual number of women who underwent both inpatient and outpatient procedures for SUI and POP. For inpatient SUI procedures, cases were identified by searching the NIS for any discharge associated with both a diagnosis for UI and a SUI procedure using a question diagram.17 For SUI, diagnoses and procedures were based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. UI ICD-9-CM diagnoses codes included 625.6, 599.82, and 788.30–788.39 and procedure codes included 59.3–59.79. For prolapse, the ICD-9-CM diagnoses codes were 618.0–618.8, and the procedures codes ranged from 68.3–68.9, 69.2–69.29, and 70.4–70.92 and included all routes of surgery (vaginal, abdominal, and minimally invasive). Similarly for outpatient procedures, ICD-9-CM codes were used to identify women who underwent SUI or POP surgery in the NSAS.
We accounted for the complex sampling design and used the sampling weights, strata, and cluster information provided by the 2007 NIS to determine national estimates for SUI and POP surgery using STATA 10.0 (Stata-Corp, College Station, TX). For outpatient data, we used sampling weights provided by the 2006 NSAS to obtain national estimates of SUI and POP procedures using SAS 9.1.3 (SAS Institute Inc, Cary, NC) and STATA 10.0.
Next, we calculated the age-specific rates for SUI and POP surgery. Rates were calculated by dividing the number of women who had surgery in a specific age group in that year by the total number of women in that same age group in the same year. We calculated the rates of surgery for women in 20-year age cohorts (20–39, 40–59, 60–79, ≥80) to determine the age-specific rates for each type of surgery. We also estimated the 95% confidence intervals (CIs) for inpatient and outpatient SUI and POP surgery by 20-year age cohort; however, for several of the age groups in outpatient surgeries, we were unable to calculate the 95% CI due to the relatively low frequency of the procedures. Since we did not have consistent 95% CI data for all age cohorts for both SUI and POP surgery, we did not use the 95% CI in our sensitivity analysis.
We then applied the rates for both inpatient and outpatient SUI and POP surgery to the population projections. We multiplied the age-specific surgery rates by the number of women in each age cohort, for each decade from 2010 through 2050. Given that we cannot accurately predict changes in PFD surgery rates in the future, we assumed that the rates for both inpatient and outpatient SUI and POP surgery remain unchanged from 2010 through 2050.
For our primary analysis, we used the 2008 national population projections middle series. In addition to the middle series, the US Census Bureau also estimates the lowest and highest population projections. Because the lowest and highest series combine the extreme values of all 3 major components that favor the lowest and highest population growth, respectively, these extreme projections do not represent likely scenarios. However, they represent the extremes between which the most likely outcomes should occur.15 Projections based on the lowest series estimate a total population of 291.4 million in 2010 to 313.5 million in 2050.18 In contrast, the highest series predicts the population to grow from 310.9 million in 2010 to 552.8 million in 2050. Given that the lowest and highest series represent the most extreme scenarios for population growth, these estimates were ideal for sensitivity analyses. We applied the inpatient and outpatient surgery rates for SUI and POP procedures to the lowest and highest series to present the widest range for future predictions.
Results
The projections for women who will undergo surgery for SUI and POP were based on the age-specific rates for both inpatient and outpatient surgery (Table 1). Overall, these estimates reflect that women aged 20–39 years had the lowest rates for both inpatient and outpatient surgery for SUI and POP and that these rates increased with each successive 20-year interval until decreasing for women aged >80 years.
TABLE 1.
Inpatient and outpatient surgery rates for stress urinary incontinence and pelvic organ prolapse
| Stress urinary incontinence (rates per 1000 women per year) |
Pelvic organ prolapse (rates per 1000 women per year) |
|||
|---|---|---|---|---|
| Age, y | Inpatient (95% CI) | Outpatient (95% CI) | Inpatient (95% CI) | Outpatient (95% CI) |
| 20–39 | 0.260 (0.229–0.292) | 0.213 | 0.343 (0.296–0.391) | 0.157 |
| 40–59 | 1.126 (1.004–1.248) | 1.264 | 1.159 (1.037–1.282) | 0.486 |
| 60–79 | 1.443 (1.286–1.601) | 1.651 | 1.986 (1.783–2.189) | 0.733 |
| ≥80 | 0.583 (0.501–0.664) | 1.101 | 0.840 (0.736–0.944) | 0.229 |
| Total | 0.843 (0.754–0.931) | 0.948 (0.709–1.187) | 1.009 (0.908–1.110) | 0.398 (0.267–0.529) |
CI, confidence interval.
Wu. Incontinence and prolapse surgeries, 2010 to 2050. Am J Obstet Gynecol 2011.
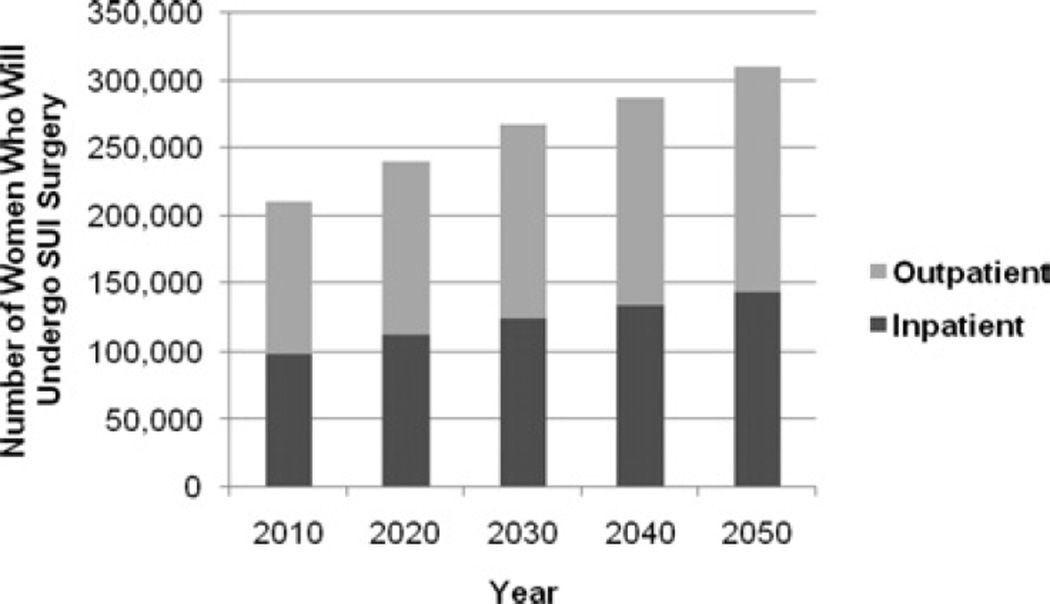
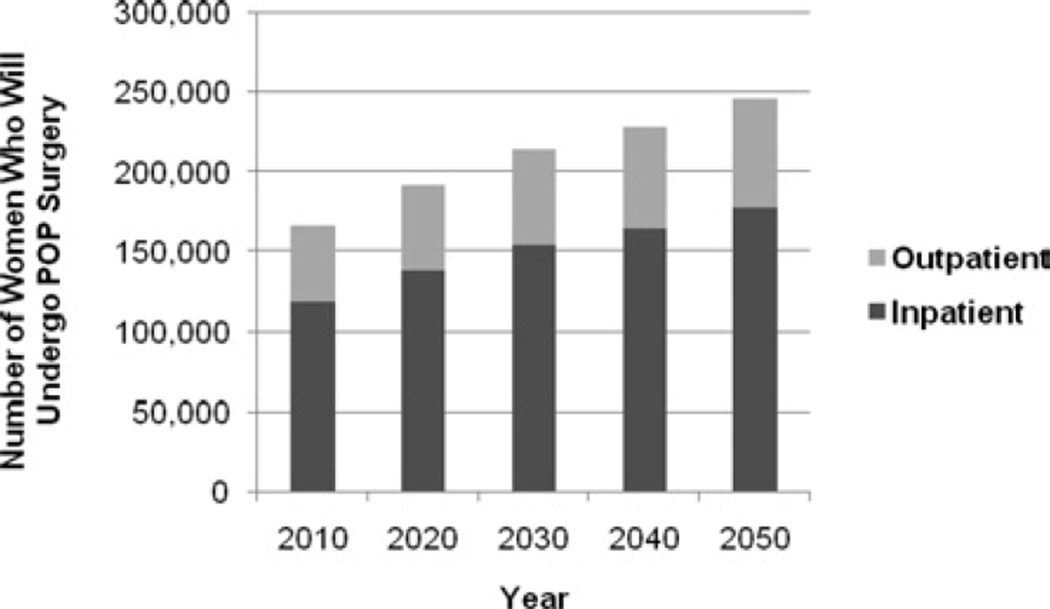
The number of women who will undergo surgery for SUI or POP in the United States will increase substantially from 2010 through 2050 (Table 2; Figures 1 and 2). The number of women who will undergo a SUI procedure will increase 47.2% from 210,700–310,050 (Table 2 and Figure 1), and the number of women who will undergo surgery for prolapse will increase 47.2% from 166,000–245,970 annually (Table 2 and Figure 2). Because we abstracted the data for inpatient and outpatient SUI and POP separately, it is important to remember that these estimates reflect the number of women who will undergo surgery for either SUI or POP.
TABLE 2.
Number of women who will undergo inpatient and outpatient surgery, 2010 through 2050
| Disorder | 2010 | 2020 | 2030 | 2040 | 2050 |
|---|---|---|---|---|---|
| Stress urinary incontinence | |||||
| Total (inpatient + outpatient) | 210,700 | 240,030 | 267,560 | 287,760 | 310,050 |
| Range | 203,810–211,860 | 224,860–245,780 | 237,770–281,360 | 242,100–314,710 | 243,610–354,250 |
| Inpatient | 98,930 | 112,610 | 124,890 | 133,500 | 143,540 |
| Range | 95,610–99,460 | 104,900–115,270 | 110,780–131,330 | 111,960–146,120 | 112,310–164,260 |
| Outpatient | 111,770 | 127,420 | 142,680 | 154,260 | 166,510 |
| Range | 108,200–112,340 | 119,960–130,510 | 126,990–150,040 | 130,140–168,590 | 131,300–189,980 |
| Pelvic organ prolapse | |||||
| Total (inpatient + outpatient) | 166,000 | 192,100 | 214,350 | 228,650 | 245,970 |
| Range | 160,310–166,870 | 179,640–196,720 | 190,720–225,330 | 191,840–249,920 | 192,560–281,070 |
| Inpatient | 118,920 | 137,980 | 154,300 | 164,790 | 177,370 |
| Range | 114,880–119,550 | 128,840–141,300 | 137,430–162,180 | 138,420–180,000 | 139,070–202,480 |
| Outpatient | 47,080 | 54,120 | 60,050 | 63,860 | 68,600 |
| Range | 45,430–47,320 | 50,800–55,410 | 53,290–63,150 | 53,420–69,920 | 53,490–78,590 |
Wu. Incontinence and prolapse surgeries, 2010 to 2050. Am J Obstet Gynecol 2011.
FIGURE 1.
Number of women who will undergo surgery for SUI in the United States from 2010 through 2050
SUI, stress urinary incontinence.
Wu. Incontinence and prolapse surgeries, 2010 to 2050. Am J Obstet Gynecol 2011.
FIGURE 2.
Number of women who will undergo surgery for POP in the United States from 2010 through 2050
POP, pelvic organ prolapse.
Wu. Incontinence and prolapse surgeries, 2010 to 2050. Am J Obstet Gynecol 2011.
These calculations are based on the assumption that the surgery rates for SUI and POP surgery will remain unchanged. Because we cannot predict how these rates may vary in the future, we conducted sensitivity analyses using the US Census Bureau lowest and highest population projections to present the range of possibilities for these procedures in the future (Table 2). The ranges for the 2010 estimates are the narrowest, and these ranges widen over the coming decades as there is greater uncertainty in the assumptions used to determine the lowest and highest population projections. The lowest number of women who will undergo SUI or POP surgeries in 2050 will be 243,610 and 192,560, respectively, whereas the highest 2050 projections indicate that these estimates will be 354,250 and 281,070 for stress incontinence and prolapse, respectively.
Comment
With the aging population in the United States and the higher prevalence of PFD in the elderly, the number of women who will undergo surgery for SUI and POP will increase dramatically over the next 4 decades. If the rates for these surgeries remain unchanged, 310,050 and 245,970 women will have surgery for SUI or POP, respectively, in 2050 compared to 210,700 and 166,000 in 2010, representing an overall increase of approximately 47% over that time period.
This increasing trend for SUI surgeries has been described in previous decades. The number of women who underwent inpatient SUI procedures increased from 48,345 in 1979 to 103,467 in 2004.19 There was also a concomitant increase in outpatient SUI surgeries from 34,968 in 1996 to 105,656 in 2006.20 It is likely that this dramatic increase was secondary to the introduction of the minimally invasive tension-free vaginal tape; however, there are no specific ICD-9-CM codes for midurethral slings making it difficult to make definitive conclusions. For prolapse, the total number of women undergoing inpatient surgery may be decreasing as the number of inpatient cases was highest in 1979 at approximately 230,000 and decreased to 187,000 in 2006.21,22 Outpatient prolapse surgery has remained fairly stable over the last decade at 43,000 in 1996 and 44,000 in 2006.20
A major strength of this study is that we used high-quality, rigorously derived, national data regarding the size of the US population as well as evaluated both inpatient and outpatient surgeries in the same analysis. The US Census Bureau predicts the growth of the US population using an intricate methodology, and we utilized both the middle series of projections for our primary estimates and the lowest and highest series for our sensitivity analyses.15,16 We also evaluated both inpatient and outpatient SUI and POP procedures using national data from the NIS11 and NSAS.12 Furthermore, these data sets can be used to estimate national data using the sampling weights; thus, the NIS and NSAS provide the best estimates for national surgery rates.
One of the limitations of this study is that we assumed that the rates for SUI and POP surgery remain unchanged, as no one can accurately predict how these rates may vary in the future. Based on previous data, it appears that SUI rates may be increasing19,20 while POP rates may be decreasing.20,21 However, numerous factors can impact these surgical rates, such as improved prevention strategies, advances in technology and surgical techniques, and changes in risk factors that impact the prevalence of SUI and POP. These factors may either increase or decrease future rates. Given these uncertainties, we thought that the best estimates to use in our analyses were the current surgical rates. More complex models, which incorporate changes in risk factors, thresholds for surgery, and variation in long-term surgical effectiveness, might give different projections but it is likely that these would fall within the wide ranges created by uncertainty in the population estimates. Another limitation is that we were unable to account for differences by race or ethnicity given that limited data exist regarding differences in surgical rates for SUI and POP by race. Lastly, because the NIS and NSAS databases are based on surveys, errors due to nonsampling or measurement error could occur. These errors include hospital nonresponse, incomplete information, inaccurately recorded data, and processing errors. However, these databases are rigorously maintained by the Agency for Healthcare Research and Quality (NIS) and the National Center for Health Statistics at the Centers for Disease Control and Prevention (NSAS).
Our future projections for SUI and POP surgery have profound implications for women, surgeons, trainees, policymakers, and public health advocates. The consequences of performing surgery on an older patient population need to be considered. Although older patients may be less likely to choose surgery for treatment of SUI or POP, those who opt for surgery have a significantly increased risk of morbidity and mortality.23,24 Our data suggest that surgeons will be faced with a higher demand for these procedures, and as a result, residency and fellowship training programs need to ensure that their graduates are able to diagnose, manage, and treat these disorders. The fields of gynecology, urogynecology, and urology will need to assess whether a sufficient number of trained surgeons will be available and accessible to address the increased demand especially given limitations in work hours over the last several years.
Currently, female PFD represent a substantial financial burden on both the individual and the health care system, and given these surgical projections, the future economic impact of SUI and POP surgery is substantial. Thom et al25 estimated the annual inpatient costs for UI to be $110.1 million in 1999. Subak et al5 estimated the direct costs for POP surgery based on 1997 Medicare reimbursement to be $1.0 billion, including $494 million for vaginal hysterectomy, $279 million for cystocele and rectocele repair, and $135 million for abdominal hysterectomy. With the increase in projected surgical volume for SUI and POP, we predict that the treatment costs will increase accordingly unless significant changes occur in our health care system.
In summary, these data illustrate an expectation that there will be an increase in the number of surgical procedures performed for both SUI and POP over the coming decades. While it is unclear how factors such as procedural efficacy, preventive strategies, and nonsurgical management will change during that time period, the progressive aging of the US population seems to ensure an increasing health care burden of surgeries to manage PFD. Studies, such as this, underscore the critical importance of future research on effective prevention and treatment options for UI and prolapse. Furthermore, we need to evaluate whether we are adequately training sufficient health care providers to manage the potential future demand for the surgical management of SUI and POP.
Acknowledgments
Supported by Grant nos. K12HD043446 (Dr Wu) and K23HD060665-02 (Dr Sung) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Footnotes
Presented at the 31st Annual Scientific Meeting of the American Urogynecologic Society, Long Beach, CA, Sept. 29-Oct. 2, 2010.
REFERENCES
- 1.Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300:1311–1316. doi: 10.1001/jama.300.11.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coyne KS, Zhou Z, Thompson C, Versi E. The impact on health-related quality of life of stress, urge and mixed urinary incontinence. BJU Int. 2003;92:731–735. doi: 10.1046/j.1464-410x.2003.04463.x. [DOI] [PubMed] [Google Scholar]
- 3.Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. 2006;194:1455–1461. doi: 10.1016/j.ajog.2006.01.060. [DOI] [PubMed] [Google Scholar]
- 4.Wilson L, Brown JS, Shin GP, Luc KO, Subak LL. Annual direct cost of urinary incontinence. Obstet Gynecol. 2001;98:398–406. doi: 10.1016/s0029-7844(01)01464-8. [DOI] [PubMed] [Google Scholar]
- 5.Subak LL, Waetjen LE, van den Eeden S, Thom DH, Vittinghoff E, Brown JS. Cost of pelvic organ prolapse surgery in the United States. Obstet Gynecol. 2001;98:646–651. doi: 10.1016/s0029-7844(01)01472-7. [DOI] [PubMed] [Google Scholar]
- 6.Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–506. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 7.Vincent GK, Velkoff VA. The next four decades, the older population in the United States: 2010 to 2050 current population reports. Washington, DC: US Census Bureau; 2010. [Google Scholar]
- 8.Ortman JM, Guarneri CE. US population projections: 2000 to 2050; US Census Bureau 2010. [Accessed March 1, 2010]; Available at: http://www.census.gov/population/www/projections/2009projections.html.
- 9.He W, Sengupta M, Velkoff VA, Debarros KA. US Census Bureau, current population reports, P23-209, 65+ in the United States: 2005. Washington, DC: US Government Printing Office; 2005. [Google Scholar]
- 10.Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in US. Women: 2010 to 2050. Obstet Gynecol. 2009;114:1278–1283. doi: 10.1097/AOG.0b013e3181c2ce96. [DOI] [PubMed] [Google Scholar]
- 11.HCUP Nationwide Inpatient Sample (NIS) Healthcare cost and utilization project (HCUP) Rockville, MD: Agency for Healthcare Research and Quality; 2007. [Google Scholar]
- 12.National Center for Health Statistics. Ambulatory surgery in the United States, 2006. [Accessed Oct. 22, 2009];2009 09/04/2009. Available at: www.cdc.gov/nchs/data/nhsr/nhsr011.pdf.
- 13.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Rep. 2009:1–25. [PubMed] [Google Scholar]
- 14.US Census Bureau. US population projections. [Accessed July 18, 2010]; Available at: http://www.census.gov/population/www/projections/index.html.
- 15.Hollmann FW, Mulder TJ, Kallan JE. Methodology and assumptions for the population projections of the United States: 1999 to 2100. US Census Bureau, 2000. [Accessed March 1, 2010]; Available at: http://www.census.gov/population/www/documentation/twps0038/twps0038.html.
- 16.Day JC. US Bureau of the Census, current population reports, P25-1130. Washington, DC: US Government Printing Office; 1996. Population projections of the United States by age, sex, race and Hispanic origin: 1995 to 2050. [Google Scholar]
- 17.Pietrobon R, Guller U, Martins H, Menezes AP, Higgins LD, Jacobs DO. A suite of web applications to streamline the interdisciplinary collaboration in secondary data analyses. BMC Med Res Methodol. 2004;4:29. doi: 10.1186/1471-2288-4-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Census Bureau. Annual projections of the resident population by age, sex, race, and Hispanic origin: lowest, middle, highest series and zero international migration series, 1999 to 2100 (NP-D1-A) [Accessed March 1, 2010]; Available at: http://www.census.gov/population/www/projections/natdet-D1A.html.
- 19.Oliphant SS, Wang L, Bunker CH, Lowder JL. Trends in stress urinary incontinence inpatient procedures in the United States, 1979–2004. Am J Obstet Gynecol. 2009;200:521.e1–521.e6. doi: 10.1016/j.ajog.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erekson EA, Lopes VV, Raker CA, Sung VW. Ambulatory procedures for female pelvic floor disorders in the United States. Am J Obstet Gynecol. 2010;203:497.e1–497.e5. doi: 10.1016/j.ajog.2010.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones KA, Shepherd JP, Oliphant SS, Wang L, Bunker CH, Lowder JL. Trends in inpatient prolapse procedures in the United States, 1979–2006. Am J Obstet Gynecol. 2010;202:501.e1–501.e7. doi: 10.1016/j.ajog.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boyles SH, Weber AM, Meyn L. Procedures for pelvic organ prolapse in the United States, 1979–1997. Am J Obstet Gynecol. 2003;188:108–115. doi: 10.1067/mob.2003.101. [DOI] [PubMed] [Google Scholar]
- 23.Heit M, Rosenquist C, Culligan P, Graham C, Murphy M, Shott S. Predicting treatment choice for patients with pelvic organ prolapse. Obstet Gynecol. 2003;101:1279–1284. doi: 10.1016/s0029-7844(03)00359-4. [DOI] [PubMed] [Google Scholar]
- 24.Sung VW, Weitzen S, Sokol ER, Rardin CR, Myers DL. Effect of patient age on increasing morbidity and mortality following urogynecologic surgery. Am J Obstet Gynecol. 2006;194:1411–1417. doi: 10.1016/j.ajog.2006.01.050. [DOI] [PubMed] [Google Scholar]
- 25.Thom DH, Nygaard IE, Calhoun EA. Urologic diseases in America project: urinary incontinence in women-national trends in hospitalizations, office visits, treatment and economic impact. J Urol. 2005;173:1295–1301. doi: 10.1097/01.ju.0000155679.77895.cb. [DOI] [PubMed] [Google Scholar]