Abstract
Oseltamivir carboxylate (OC) has been detected in environmental waters at various levels during recent influenza seasons in humans, reflecting levels of usage and stability of this drug. In consideration of the role of waterfowl as hosts for influenza viruses that may contribute to human infections, we evaluated the effect of consumption of low doses of OC on development of oseltamivir-resistant influenza virus mutants in mallard ducks (Anas platyrhynchos) infected with two different low-pathogenic (LP) H5N2 avian influenza viruses (AIV). We detected development of virus variants carrying a known molecular marker of oseltamivir resistance (neuraminidase E119V) in 4 out of 6 mallards infected with A/Mallard/Minnesota/182742/1998 (H5N2) and exposed to 1,000 ng/liter OC. The mutation first appeared as a minor population on days 5 to 6 and was the dominant genotype on days 6 to 8. Oseltamivir-resistant mutations were not detected in virus from ducks not exposed to the drug or in ducks infected with a second strain of virus and similarly exposed to OC. Virus isolates carrying the E119V mutation displayed in vitro replication kinetics similar to those of the wild-type virus, but in vivo, the E119V virus rapidly reverted back to wild type in the absence of OC, and only the wild-type parental strain was transmitted to contact ducks. These results indicate that consumption by wild waterfowl of OC in drinking water may promote selection of the E119V resistance mutation in some strains of H5N2 AIV that could contribute to viruses infecting human populations.
INTRODUCTION
Oseltamivir, a neuraminidase (NA) inhibitor, is one of the most widely prescribed antiviral drugs in the world and is used primarily for treatment of human influenza virus infections. This antiviral is administered orally as oseltamivir phosphate (OP), which is readily absorbed and has high oral bioavailability. In humans, OP is metabolized in the liver to the active metabolite oseltamivir carboxylate (OC), which is not metabolized further and is excreted primarily in urine (58), leading to large quantities of the drug entering wastewater when drug usage in the population is high.
Data from human clinical trials and natural influenza virus infection with or without OP treatment and influenza surveillance in avian species have demonstrated an increase in oseltamivir resistance in seasonal human influenza, low-pathogenic avian influenza virus (LPAIV), and highly pathogenic AIV (HPAIV), such as H5N1 viruses (2–9). The increased detection of seasonal human influenza virus strains showing resistance to oseltamivir is of great concern. The predominant oseltamivir-resistant mutation of H274Y in N1 subtypes, detected from America to Europe to Asia, most likely results from continued transmission of resistant strains among humans, as regional drug use is not suspected to be the problem (7, 10–13).
Experimental studies using ferrets have detected emergence of resistant strains following oseltamivir treatment and H5N1 virus infection (14), highlighting the potential for drug-induced resistance. Another known NA-resistant mutation, E119V, has been shown to retain replicative ability and transmissibility as efficiently as the wild-type virus (15, 16), whereas another mutation, R292K, appears to be compromised both in vitro and in vivo and had limited ability to transmit in the ferret contact model (1, 16). Seasonal human H1N1 viruses with the H274Y mutation have also shown restriction in replicative ability and transmission in ferrets (17), but the virus has the ability to be transmitted if infectious doses are increased (15). Using reverse genetics, an HP H5N1 strain was altered to include the common H274Y and N294S mutations, and the replication efficiency and pathogenicity of the virus was tested in mice; the mutated virus retained its lethality to mice and retained replication efficiency in vitro (18).
Viral fitness has been analyzed utilizing a competitive-mixtures model in ferrets (19). The R292K mutated virus was outcompeted by the R292 wild-type virus and was not transmissible, which is consistent with previous studies on this mutation. The H274Y mutated virus was only marginally outcompeted by the H274 wild-type virus but was equally transmissible among ferrets. Another good model to compare to humans, guinea pigs, has demonstrated the ability to efficiently transmit oseltamivir-resistant strains through direct contact (20). These animal models confirm that the transmission of oseltamivir-resistant viruses is possible and warrant evaluation in the natural reservoir of influenza virus to provide a more complete picture of how this could affect humans.
Currently, stockpiling of the most orally bioavailable drug, oseltamivir, is at a peak. Considering the increased awareness of antivirals by patients, coupled with concern regarding the most recent pandemic of swine H1N1, we can expect that this will ultimately lead to a higher use of the drug. It is imperative that we better understand the possible outcomes of resistance from antiviral treatment, including the case of oseltamivir contamination of the environment.
Importantly, OC is poorly removed or degraded by natural environmental conditions or sewage treatment (21–28), resulting in significant retention in waterways. These same waterways often support large numbers of waterfowl, the primary reservoir of avian influenza A viruses (AIVs), and waterfowl in several parts of the world are likely exposed over lengthy periods to at least low doses of OC in their drinking water. In contrast to mammals, AIVs replicate predominantly in the intestinal tract of ducks and other waterfowl, and there is reason for concern that the presence of OC in the intestinal lumen, acquired through the environment, may promote selection of AIVs that are resistant to oseltamivir.
Recently, concentrations of OC were measured in regional waters of Japan, a country where human use of oseltamivir is high. Prior to the beginning of the 2007-2008 influenza season, OC was not detected in the Yodo River system, but concentrations of 2 to 58 ng/liter were detected during the influenza season (29). During the 2008-2009 influenza season, levels of OC rose to a peak concentration of 293 ng/liter in discharges from sewage treatment plants, and concentrations of OC in river water ranged from 6 to 190 ng/liter (30).
Proposed calculations for the United States and the United Kingdom based on hydrologic modeling, which included catchment sizes, population size, and WHO-recommended dosing of OP, suggest that OC may remain in the environment for up to 18 days at levels of <300 to 32,000 ng/liter during a pandemic (27). The magnitude of a pandemic and the availability of drug dispensed would all play a role in various environmental concentrations.
In order to better understand the risk for emergence of resistance to oseltamivir due to environmental contamination with the drug, we infected mallard ducks with two different LPAIV H5N2 strains of mallard virus, while giving them access to drinking water containing concentrations of OC that fall between recently detected levels and potential pandemic levels. We hypothesized that access to low doses of OC while the mallard was infected would promote the emergence of OC-resistant viruses and that oseltamivir-resistant viruses would be as transmissible as the wild-type progenitor. We also sought to determine the effects on viral replication and emergence of resistance in ducks given a single dose of OP following viral inoculation to evaluate the ramifications of treating birds upon entry at live-bird markets, which has been suggested in Indonesia.
MATERIALS AND METHODS
Ethics statement.
All experiments were approved by the Institutional Animal Care and Use Committee of Colorado State University, Fort Collins, CO, under approval number 09-168A.
Animals.
Mallard ducks were purchased as hatchlings from commercial sources. Ducklings were housed in an ABSL3 facility until 4 to 6 weeks of age at the start of each experiment. Prior to infection, all ducks tested negative by enzyme-linked immunosorbent assay (ELISA) for group-specific antibodies to an influenza type A virus antigen (recombinant nucleoprotein, Flu DETECT BE; Synbiotics Corporation, Kansas City, MO) and strain-specific antibodies to H5N2 by hemagglutination inhibition (HAI) assay, as previously described (31).
Viruses and chemicals.
The viruses used in this study were A/Mallard/Minnesota/346250/2000 (H5N2) and A/Mallard/Minnesota/182742/1998 (H5N2). Both viruses were propagated by passage in 10-day-old specific pathogen-free embryonated chicken eggs (Sunrise Farms, NY). Eggs were incubated at 37°C, and allantoic fluid was harvested 48 to 72 h after inoculation, aliquoted, and stored at −80°C until use. Both viruses were titrated by plaque assay on MDCK cells (ATCC, Manassas, VA) as previously described (31) and stained with either crystal violet or by addition of a second overlay containing neutral red; virus titers were expressed as PFU/ml.
Viruses utilized in the neuraminidase inhibition assay (NAI) were obtained from the Centers for Disease Control and Prevention, Atlanta, GA; grown once in MDCK cells using phenol red-free growth medium; and used as the sensitive and resistant controls. The virus strains used included A/Texas/36/1991 (H1N1) and its H274Y resistant strain and A/Wuhan/395/1995-like (H3N2) and its E119V resistant strain.
Viruses used in the transmission study included the previously mentioned stock of A/Mallard/Minnesota/182742/1998 and its E119V resistant counterpart that was recovered from a duck cloacal swab (duck 2.3, day 6) as a picked plaque, plaque purified, and grown in eggs to obtain the stock virus. The neuraminidase genes of all viruses were sequenced prior to infection of ducks to verify the presence or absence of the E119V mutation.
Oseltamivir phosphate (Ro-64-0796) and oseltamivir carboxylate (Ro-64-0802) were provided by F. Hoffman-La Roche (Roche Diagnostics GmbH, Mannheim, Germany) and were utilized in both the NAI assays and mallard exposure studies.
Replication kinetics.
Single-step and multistep growth curves were determined for both the A/Mallard/Minnesota/182742/1998 and A/Mallard/Minnesota/182742/1998-E119V viruses in MDCK cells. Cells were grown in 6-well tissue culture plates until ∼90 to 95% confluence. Based on cell count, the cells were infected at a multiplicity of infection (MOI) of 2 PFU/cell for the single-step growth curve and an MOI of 0.01 PFU/cell for the multistep growth curve. Following 1 h of incubation at 37°C and 5% CO2, cells were rinsed two times with phosphate-buffered saline (PBS) and overlaid with Dulbecco's modified Eagle's medium (DMEM; Sigma-Aldrich Corp., St. Louis, MO) supplemented with antibiotics, 0.5% bovine serum albumin (BSA) (Sigma-Aldrich), and 1 μg/ml of TPCK trypsin (Sigma-Aldrich). Supernatants were collected at 2, 4, 6, 8, and 10 h postinfection for the single-step growth curve and at 12, 24, 36, 48, 60, and 72 h postinfection for the multistep curve, both in duplicate, and stored at −80°C until titrated by plaque assay.
Neuraminidase inhibition assay.
The inhibition of viral neuraminidase (NA) by oseltamivir was analyzed using the NA-Star influenza neuraminidase inhibitor resistance detection kit (Applied-Biosystems, Foster City, CA) according to the manufacturer's protocol. Initially, duck cloacal swabs were diluted in 10-fold dilutions for the plaque assay to determine the viral titer on each day postinoculation and to pick individual plaques for the NAI assay. Fifty individual plaques were picked and stored in 1 ml of PBS, for all 18 ducks in groups 1 and 2 (900 plaques), from viruses shed at the latest detectable time point. An aliquot from each picked plaque was then inoculated into eggs to obtain stock viruses that were tested for resistance in the NAI assay. Each virus was diluted at least 5-fold to obtain a signal-to-noise ratio of 10:1 to 60:1. Luminescence was measured using the Victor X5 multilabel plate reader (Perkin-Elmer, Waltham, MA) equipped with automatic injectors for the addition of NA-Star accelerator. Fifty-percent inhibitory concentrations (IC50s) were determined using the JASPR version 1.1 (beta) software for curve fitting and analysis, provided by the Virus Surveillance and Diagnosis Branch at the Centers for Disease Control and Prevention, Atlanta, GA. Statistical analysis of IC50s from picked plaques followed the procedure previously described (7), which required an IC50 ± 3 standard deviations (SD) as a cutoff for outliers of resistance as an initial screen to narrow down the number of samples tested by sequencing.
RT-PCR and sequencing analysis.
RNA was extracted from either allantoic fluid or directly from duck cloacal swabs using TRI reagent (Molecular Research Center, Inc., Cincinnati, OH) according to the manufacturer's protocol. Both amplification of PCR product and sequencing of the NA N2 gene utilized primers previously designed (32) and named NA-2.1, NA-2.3, NA-2.5, and NA-2.6 (forward and reverse). We also designed one additional primer, 1413R (5′-ATA GGC ATG AAG TTG ATA TTC GC-3′), to amplify the entire NA gene from the 3′ end. Reverse transcription (RT)-PCR was performed using a one-step RT-PCR kit (Qiagen, Valencia, CA) according to the manufacturer's protocol. Amplification involved an initial RT step of 50°C for 30 min, followed by heating at 95°C for 15 min, 3-step cycling of 35 to 40 cycles with denaturation at 95°C for 1 min, followed with annealing at 53°C for 1 min and extension at 72°C for 1 min, with one final extension of 72°C for 10 min. For hemagglutinin (HA) sequencing, we utilized primers and experimental design as previously described with modifications (33). For sequencing, PCR amplicons were electrophoresed in a 1 to 2% agarose gel, and DNA was extracted using the QIAquick gel extraction kit (Qiagen, Valencia, CA) according to the manufacturer's protocol. PCR fragments were sent to the Proteomics and Metabolomics Facility at Colorado State University. Sequencing was performed in both directions utilizing the same primers as described above. Sequences were aligned and analyzed using the MEGA 5 software (34).
Site-specific RT-PCR.
RNA was extracted as previously described and was subjected to RT-PCR utilizing a specific set of primers designed to detect the specific point mutation of nucleotide 356 A to T, which changes the amino acid at position 119 from glutamic acid (E) to valine (V). The same forward primer (5′-GCAGATTGCCATCCTAGC-3′) was used in both RT-PCR assays, with two different reverse primers to differentiate between wild-type (5′-GGTGTCACATGACACATAAGGTT-3′) and E119V resistant (5′-GGTGTCACATGACACATAAGaTA-3′) viruses. The E119V resistant reverse primer had two specific point mutations, one on the 3′ (A) end to match the resistant virus, and another 3 bp from the terminus on the 3′ end (a). This additional mismatch allowed for destabilization of the primer to help minimize anomalous products from forming (35–37). The RT-PCR cycling parameters are the same as previously described, with an increased annealing temperature of 61°C to differentiate between wild-type and E119V resistant virus using wild-type primers. An annealing temperature of 53°C was used with E119V resistant primers.
Pharmacokinetics of oseltamivir in mallards.
Six juvenile mallard ducks were gavaged using a Foley catheter with 5 mg of OP (Tamiflu, Ro 64-0796) dissolved in 2.5 ml sterile water. Approximately 1 ml of blood was collected into lithium-heparin tubes (Becton, Dickinson and Co., Franklin Lakes, NJ) from each duck at predose and at 0.25, 0.5, 1, 2, 3, 4, 6, 12, 24, and 48 h postdose. Blood samples were centrifuged, and plasma was collected and stored at −80°C until assayed for OP and OC by PRA International (Assen, the Netherlands). Samples were extracted using a C18 solid-phase extraction method, and analysis was performed utilizing liquid chromatography-tandem mass spectrometry (LC-MS/MS). Internal standards included deuterated oseltamivir and oseltamivir carboxylate (Ro 64-0802). Pharmacokinetic data analysis and summary were performed at Roche.
Statistical analysis of pharmacokinetics.
Noncompartmental pharmacokinetic parameters were calculated using WinNonlin Enterprise, version 5.2.1 (Pharsight Corporation, St. Louis, MO). The values of the maximum plasma concentration (Cmax) and time to Cmax (Tmax) for each duck were the observed values. The area under the plasma concentration time curve was determined using the linear trapezoidal method for the time periods of 0 to 12 h postdose (AUC0–12) and from 0 to the last measurable plasma concentration (AUC0–t). The area under the curve from the last measurable concentration (Ct) to infinity was calculated as Ct/λz, where λz is the elimination rate constant, which was calculated using at least 3 time points of the log linear portion of the elimination curve. AUC from 0 to infinity (AUC0–∞) was calculated as AUC0–t + Ct/λz. The elimination half-life was calculated as ln 2/λz. Oral clearance (CL/F) was determined as the dose divided by AUC0–∞, and the oral volume of distribution (Vz/F) was calculated as dose/(AUC0–∞ × λz). CL/F and Vz/F were divided by the weights of ducks to facilitate comparison to human data.
OC treatment of mallards and AIV infection.
Four separate groups of mallard ducks ages 4 to 6 weeks were housed in separate rooms according to the concentration of drug provided in water and were allowed to free range within a 12- by 18-foot area. Briefly, group 1 (ducks 1.1 to 1.10) were inoculated with A/Mallard/MN/346250/00 virus: 8 (2 per dose) were exposed to different concentrations of OC in the drinking water, and 2 control ducks were not exposed to OC. Group 2 consisted of 8 ducks (2.1 to 2.8) inoculated with A/Mallard/MN/182742/98: 6 (2 per dose) exposed to different concentrations of OC in the drinking water and 2 control ducks not exposed to OC. Group 3 (3.1 to 3.8) was a partial replicate of study group 2 in which 4 ducks received 1,000 ng/liter of OC in their drinking water and 4 control ducks received no drug. Group 4 (4.1 to 4.10) was a replicate experiment for group 1 that included 5 ducks that received 1,000 ng/liter of OC in their drinking water and 5 ducks that received no OC in their drinking water.
Beginning 24 to 48 h prior to virus challenge, groups of ducks were provided with drinking water containing between 10 and 10,000 ng/liter OC, while control ducks were supplied water with no OC. Water dishes were refilled daily with the appropriate concentration of OC; determining individual duck water consumption was not possible because of the shared single water source. All ducks were inoculated on day 0 with 106 PFU of either H5N2 virus orally (directly in the mouth) and intranasally (drops in the nares) in the first two groups and through their choanal cleft in groups 3 and 4. The choanal cleft is located on the roof of the mallard's mouth as a slit and connects the nasal cavity with the throat; this inoculation route minimizes the ability of the mallard to “blow out” the inoculum through their nares during intranasal application or by “missing” the nasal cavity entirely when using the oral inoculation route. The change in inoculation route to the choanal cleft was done to facilitate a more natural inoculation route, which led to consistent infection rates and shedding by all inoculated mallards (data not shown).
Cloacal swabs were collected daily in 2 ml BA-1 medium (MEM, 1% BSA, 350 mg/liter sodium bicarbonate, 50 ml/liter 1 M Tris [pH 7.6], 5 mg/liter phenol red) supplemented with antibiotics (50 μg/ml gentamicin, 100 U/ml polymyxin B, 50 U/ml nystatin, 100 U/ml penicillin, and 50 μg/ml streptomycin) from days 0 through 7 or 10. Swab samples were split into duplicate 1-ml volumes and stored at −80°C until tested by plaque assay.
We utilized the NAI and Sanger sequencing as two different strategies to evaluate the development of resistance to oseltamivir in mallard ducks infected with AIV. We initially tested viruses shed from ducks receiving the highest dose of OC that did not completely inhibit virus shedding and analyzed those viruses isolated toward the end of the shedding period, assuming that if resistant viruses evolved, they would be present at the highest frequency at that time due to the selective pressure of continued presence of OC. For those ducks that shed oseltamivir-resistant virus, we tested additional samples earlier during the course of infection to determine the time course of detection of resistance.
For groups 1 and 2, cloacal swabs were tested for viral titer by plaque assay, and individual plaques were picked, grown once in eggs, and tested in the NAI assay for drug resistance. The NA gene of viruses that showed an increased IC50 was sequenced using the Sanger method. For groups 3 and 4, Sanger sequencing was performed on RNA extracted directly from cloacal swabs. The direct sequencing from cloacal swabs was performed to help eliminate the possibility that the growth of picked plaques in eggs contributed to the selection of host-adaptive mutations.
OP treatment of mallards and AIV infection.
This experiment was designed to mimic treatment of ducks with a single dose of OP shortly after exposure to AIV, a practice previously discussed to treat birds in live markets where AIV infection frequently occurs. Nine 5-week-old mallard ducks were inoculated with 106 PFU of A/Mallard/Minnesota/182742/1998 virus via the choanal cleft. Six hours postinoculation, 4 inoculated ducks were gavaged with 5 mg OP diluted in 2.5 ml distilled water, while the other 5 virus-inoculated ducks received 2.5 ml of distilled water. Cloacal swabs were collected on days 0 through 7 and stored at −80°C until tested by plaque assay. Samples from the latest time point of shedding were sequenced for detection of the presence or absence of mutations.
Transmissibility of mutant AIV in mallards.
To evaluate differences in transmissibility of wild-type versus OC-resistant AIV via direct contact or environmental contamination, we infected 5-week-old mallards with each virus, exposed them to noninfected ducks, and monitored the rate of infection in all ducks. Two ducks each were inoculated with 106 PFU of A/Mallard/Minnesota/182742/1998 or A/Mallard/Minnesota/182742/1998-E119V virus, and 2 h later each separate pair of virus-inoculated ducks was introduced to mingle freely with 6 contact ducks. In a second transmissibility experiment, 3 ducks were inoculated with a mixture containing 106 PFU of A/Mallard/Minnesota/182742/1998 virus and 106 PFU of A/Mallard/Minnesota/182742/1998-E119V virus, and 2 h later, each of the 3 inoculated ducks was introduced into a pen containing 3 contact ducks. Blood was collected from all ducks prior to days 0 and on day 14 and tested for anti-AIV antibodies using the competitive ELISA. Cloacal swabs were collected daily from days 0 through 14 from all 28 ducks and assayed for viral titer by plaque assay as described above. RNA was extracted directly from cloacal swabs for sequencing to determine the presence or absence of the E119V mutation.
RESULTS
The goal of this study was to determine whether exposure of ducks to OC in drinking water before and during the course of AIV infection would lead to the emergence of oseltamivir-resistant strains that could subsequently be transmitted to other ducks and eventually humans.
Pharmacokinetics of oseltamivir in mallards.
In order to determine the effects influenza infection may have on mallard ducks, we first sought to see the effects of 5 mg of OP given to ducks and the breakdown of the drug to the active component OC over time. The plasma concentrations of OP and OC in 6 ducks were determined following oral dosing of ducks with 5 mg OP and are listed in Table 1, with the pharmacokinetic parameters listed in Table 2. Plasma concentrations of oseltamivir were detectable at 48 h postdose, while the carboxylate metabolite was detectable only to 24 h (Table 1). The ratio of OC metabolite to parent OP concentrations was maximal at 0.5 h and declined from 0.83 to 0.04 at 24 h. Based on the values of AUC0–∞, the ratio of metabolite to parent was 0.14. In one duck, the concentration of the metabolite was greater than the parent in the first 4 samples for up to 2 h, following a more human-like pattern. The other 5 ducks had consistently higher concentrations of parent than metabolite. The mean Cmaxs for OP and OC were 1,190 and 487 ng/ml, respectively (Table 2). Tmax was approximately 0.5 h for both the parent and metabolite. The mean t1/2 for OP was 10.5 h, which was longer than that for OC, which was 6.48 h. CL/F of oseltamivir was 0.468 liters/h/kg and Vz/F was 6.81 liters/kg. Comparisons of duck pharmacokinetic parameters and human parameters are outlined in Table 3. In humans, systemic exposure to OC is roughly 22 times greater than exposure to OP as determined by AUC 0–∞, reflecting efficient conversion of OP to enzymatically active OC. In contrast, we found this ratio to be only 0.14 in ducks, suggesting either inefficient hepatic conversion or that conversion of OP to OC may occur in the intestinal lumen, which could be significant considering that AIVs replicate in the intestinal tract of ducks. Additionally, OP has a longer half-life in ducks than in humans, but OC has a similar half-life in both species, suggesting that while they appear to have different mechanisms for conversion, they may share the same mechanism for clearance. Further studies are required to determine the complete mechanism of conversion in mallard ducks.
Table 1.
Plasma concentrations of OP and OC in mallard ducks administered a single oral dose (5 mg) of OPa
| Hour | Concn (ng/ml) |
OC/OP ratio | |
|---|---|---|---|
| OP | OC | ||
| 0.25 | 1,170 (585)a | 441 (200) | 0.53 (0.53) |
| 0.5 | 886 (463) | 481 (174) | 0.83 (0.92) |
| 1 | 770 (405) | 320 (134) | 0.68 (0.86) |
| 2 | 637 (347) | 165 (68.4) | 0.39 (0.41) |
| 3 | 552 (273) | 89.4 (39.0) | 0.21 (0.19) |
| 4 | 459 (217) | 64.0 (29.5) | 0.18 (0.14) |
| 6 | 383 (180) | 46.4 (19.3) | 0.16 (0.11) |
| 12 | 292 (99.2) | 24.3 (13.5) | 0.10 (0.06) |
| 24 | 166 (72.3) | 4.83 (7.90) | 0.04 (0.08) |
| 48 | 26.5 (18.9) | 0.00 (0.00) | 0.00 (0.00) |
Values are means (standard deviations) from 6 experiments.
Table 2.
Pharmacokinetic parameters of OP and OC in mallard ducks administered a single oral dose (5 mg) of OP
| Parameter (units) | Valuea |
|
|---|---|---|
| OP | OC | |
| Cmax (ng/ml) | 1,190 (575) | 487 (188) |
| Tmax (h) | 0.54 (0.71) | 0.46 (0.10) |
| AUC0–12 (ng · h/ml) | 5,490 (2,500) | 1,140 (382) |
| AUC0–t (ng · h/ml) | 10,500 (4,030) | 1,240 (528) |
| AUC0–∞ (ng · h/ml) | 11,000 (4,240) | 1,390 (548) |
| AUC0–∞ (ng · h/ml/mg) | 2,200 (847) | 303 (119) |
| t1/2 (h) | 10.5 (3.00) | 6.48 (1.61) |
| CL/F (liters/h) | 0.517 (0.206) | NC |
| CL/F (liters/h/kg) | 0.468 (0.191) | NC |
| Vz/F (liters) | 7.67 (3.60) | NC |
| Vz/F (liters/kg) | 6.81 (2.91) | NC |
Values are means (standard deviations) from 6 experiments. NC, not calculated.
Table 3.
Comparison of pharmacokinetic parameters of OP and OC in mallard ducks and humans following a single oral dose of OP
| Parameter (unit) | Valuea |
|||
|---|---|---|---|---|
| Oseltamivir |
Oseltamivir carboxylate |
|||
| Duck | Human | Duck | Human | |
| Cmax (ng/ml) | 1,190 | 84 | 487 | 215 |
| Tmax (h) | 0.54 | 1.00 | 0.46 | 5.00 |
| AUC0–∞ (ng · h/ml/mg) | 2,200 | 1.87 | 303 | 40.8 |
| t1/2 (h) | 10.5 | 1.70 | 6.48 | 7.7 |
| CL/F (liters/h/kg) | 0.47 | 7.1 | NC | NC |
| Vz/F (liters/kg) | 6.81 | 17.6 | NC | NC |
Pharmacokinetic parameters for ducks following a single oral dose of 5 mg of OP (current study); mean duck weight = 1.11 kg. Pharmacokinetic parameters for humans given a 75-mg oral dose of OP (clinical study WP20727 [57]); mean human weight = 75 kg. NC, not calculated.
OC treatment of mallards and AIV infection.
These studies were designed to simulate exposure of ducks to low levels of OC in drinking water prior to and during infection with AIV. Interestingly, mallards that received 10,000 ng/liter of OC in their drinking water failed to shed detectable virus on any day (ducks 1.1 and 1.2) (Table 4). Virus culture and phenotypic testing with OC was performed with 200 plaque-picked (day 4), egg-grown viruses from the 2 ducks receiving 1,000 ng/liter of OC and the 2 ducks getting no OC. None of these 200 isolates showed an increased IC50 in the NAI assay.
Table 4.
Viral titers from cloacal swab samples in individual ducks infected with AIV while ingesting OC in drinking watera
| Group | Drug concn (ng/ml) | Titer at post-virus inoculation day: |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| 1 | ||||||||||
| 1.1 | 10,000 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | NT | NT |
| 1.2 | 10,000 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | NT | NT |
| 1.3 | 1,000 | 0.00 | 3.30 | 4.43 | 4.30 | 0.00 | 0.00 | 0.00 | NT | NT |
| 1.4 | 1,000 | 0.00 | 2.60 | 4.36 | 2.00 | 0.00 | 0.00 | 0.00 | NT | NT |
| 1.5 | 100 | 0.00 | 0.00 | 4.58 | 2.00 | 0.00 | 0.00 | 0.00 | NT | NT |
| 1.6 | 100 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | NT | NT |
| 1.7 | 10 | 0.00 | 0.00 | 0.00 | 3.78 | 0.00 | 0.00 | 0.00 | NT | NT |
| 1.8 | 10 | 0.00 | 0.00 | 4.78 | 4.40 | 0.00 | 0.00 | 0.00 | NT | NT |
| 1.9 | 0 | 4.00 | 3.95 | 4.48 | 3.30 | 0.00 | 0.00 | 0.00 | NT | NT |
| 1.10 | 0 | 0.00 | 0.00 | 4.88 | 2.85 | 0.00 | 0.00 | 0.00 | NT | NT |
| 2 | ||||||||||
| 2.1 | 10,000 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | NT | NT |
| 2.2 | 10,000 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | NT | NT |
| 2.3 | 1,000 | 0.00 | 3.00 | 7.08 | 4.00 | 3.48 | 3.00 | 1.60 | NT | NT |
| 2.4 | 1,000 | 0.00 | 3.30 | 0.00 | 3.40 | 4.00 | 2.30 | 0.00 | NT | NT |
| 2.5 | 100 | 0.00 | 2.78 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | NT | NT |
| 2.6 | 100 | 0.00 | 2.70 | 1.00 | 2.70 | 3.48 | 0.00 | 0.00 | NT | NT |
| 2.7 | 0 | 0.00 | 3.78 | 3.70 | 0.00 | 0.00 | 0.00 | 0.00 | NT | NT |
| 2.8 | 0 | 0.00 | 3.30 | 0.00 | 0.00 | 0.00 | 1.00 | 0.00 | NT | NT |
| 3 | ||||||||||
| 3.1 | 1,000 | 0.00 | 0.00 | 4.37 | 3.78 | 4.36 | 3.88 | 4.48 | 3.08 | 2.00 |
| 3.2 | 1,000 | 0.00 | 0.00 | 4.90 | 3.11 | 2.70 | 3.18 | 1.78 | 1.85 | 1.48 |
| 3.3 | 1,000 | 0.00 | 0.00 | 4.18 | 3.90 | 4.30 | 4.67 | 2.30 | 2.00 | 2.00 |
| 3.4 | 1,000 | 0.00 | 5.24 | 6.08 | 5.29 | 6.26 | 0.00 | 2.00 | 2.60 | 0.00 |
| 3.5 | 0 | 0.00 | 5.71 | 3.68 | 4.30 | 4.70 | 3.04 | 0.00 | 0.00 | 0.00 |
| 3.6 | 0 | 0.00 | 6.76 | 4.53 | 3.78 | 2.95 | 1.78 | 0.00 | 0.00 | 0.00 |
| 3.7 | 0 | 0.00 | 0.00 | 2.95 | 5.22 | 2.40 | 2.60 | 3.85 | 0.00 | 0.00 |
| 3.8 | 0 | 0.00 | 8.40 | 6.20 | 4.18 | 2.23 | 3.11 | 0.00 | 0.00 | 0.00 |
| 4 | ||||||||||
| 4.1 | 1,000 | 0.00 | 4.48 | 3.48 | 6.00 | 3.60 | 2.60 | 2.48 | 0.00 | 0.00 |
| 4.2 | 1,000 | 1.30 | 3.78 | 3.48 | 4.30 | 3.18 | 2.30 | 2.30 | 2.95 | 2.30 |
| 4.3 | 1,000 | 0.00 | 3.20 | 3.78 | 3.48 | 2.48 | 0.00 | 0.00 | 0.00 | 0.00 |
| 4.4 | 1,000 | 0.00 | 0.00 | 2.78 | 3.79 | 4.03 | 1.95 | 3.00 | 0.00 | 0.00 |
| 4.5 | 1,000 | 0.00 | 3.30 | 2.60 | 5.00 | 4.02 | 2.04 | 0.00 | 1.95 | 0.00 |
| 4.6 | 0 | 4.30 | 5.15 | 4.85 | 3.30 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 4.7 | 0 | 6.90 | 4.30 | 3.70 | 3.30 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 |
| 4.8 | 0 | 4.40 | 3.70 | 4.30 | 2.85 | 2.70 | 0.00 | 0.00 | 0.00 | 0.00 |
| 4.9 | 0 | 0.00 | 5.30 | 4.95 | 3.59 | 4.08 | 2.78 | 0.00 | 0.00 | 0.00 |
| 4.10 | 0 | 0.00 | 3.95 | 4.48 | 2.76 | 0.00 | 3.48 | 0.00 | 0.00 | 0.00 |
Viral titers reported in log10 PFU/ml; values of 0.00 represent titers of <10 PFU/ml. Duck identifiers highlighted in bold (2.3, 3.1, 3.3, 3.4) are those with the detected E119V mutation. NT, not tested.
For group 2, we again observed that ducks exposed to 10,000 ng/liter of OC in drinking water failed to shed detectable virus on any day (Table 4). Virus culture and phenotypic testing with OC was performed with 205 plaque-picked, egg-grown viruses from the 2 ducks receiving 1,000 ng/liter OC and the 2 control ducks. In this group, increased phenotypic IC50was detected in 35 picked plaques, from days 5 and 6, of 1 of 2 ducks (duck 2.3) that received 1,000 ng/liter of OC in drinking water. None of 20 additional plaques picked from the sample collected from duck 2.3 on day 3 had an elevated IC50. Among 50 plaque-picked viruses on days 5 and 6 from duck 2.4, who also received 1,000 ng/liter of OC, none showed an increased IC50. None of the 100 viruses tested from the 2 ducks receiving no OC had an elevated IC50 compared to that of the wild-type 182742 virus.
For group 2 duck 2.3, we compared the IC50s of 55 plaque-picked viruses (35 viruses from days 5 and 6, and 20 viruses from day 3) to the IC50 of the wild-type virus. We determined that the mean IC50 for viruses from group 2 duck 2.3 on days 5 and 6 was 17.43 ± 4.85 nM, which was an 8.8-fold increase over the IC50 for the wild-type strain, which was 1.97 ± 1.16 nM (Table 5). All samples with phenotypic IC50s above a specific cutoff value (mean IC50 + 3 SD) were selected for NA sequencing. All the individual viruses that had a ≥5.45 nM (1.97 + [3 × 1.16])-fold increase were subjected to Sanger sequencing and found to contain an A-to-T nucleotide change at position 356, which causes the amino acid (aa) to change from glutamic acid (E) to valine (V) at position 119 (H3 numbering) in the NA sequence. In ducks with the E119V mutation, we also observed a mutation from A to G at nucleotide 510, but this did not alter the amino acid sequence. The NA gene from five additional plaques from duck 2.3 on day 3 was also sequenced, but no mutations were detected at positions 119 or 510.
Table 5.
IC50 comparisons between control sensitive and resistant strains
| Virus strain | NA subtype | NA mutation | Mean IC50 ± SDa (nM) (fold inc) |
|---|---|---|---|
| A/TX/36/1991 | N1 | 3.20 ± 1.01 | |
| A/TX/36/1991 | N1 | H274Y | 262.3 ± 204.4 (81.96) |
| A/Wuhan/395/1995-like | N2 | 3.215 ± 0.73 | |
| A/Wuhan/395/1995-like | N2 | E119V | 26.25 ± 4.25 (8.16) |
| A/Mallard/182742/1998 | N2 | 1.97 ± 1.16 | |
| A/Mallard/182742/1998 | N2 | E119V | 17.43 ± 4.85 (8.84) |
| A/Mallard/346250/2000 | N2 | 5.14 ± 1.23 |
Means ± SD calculated from data collected from at least 3 independent experiments. fold inc, fold increase in IC50 for oseltamivir compared to that of the matching wild-type strain.
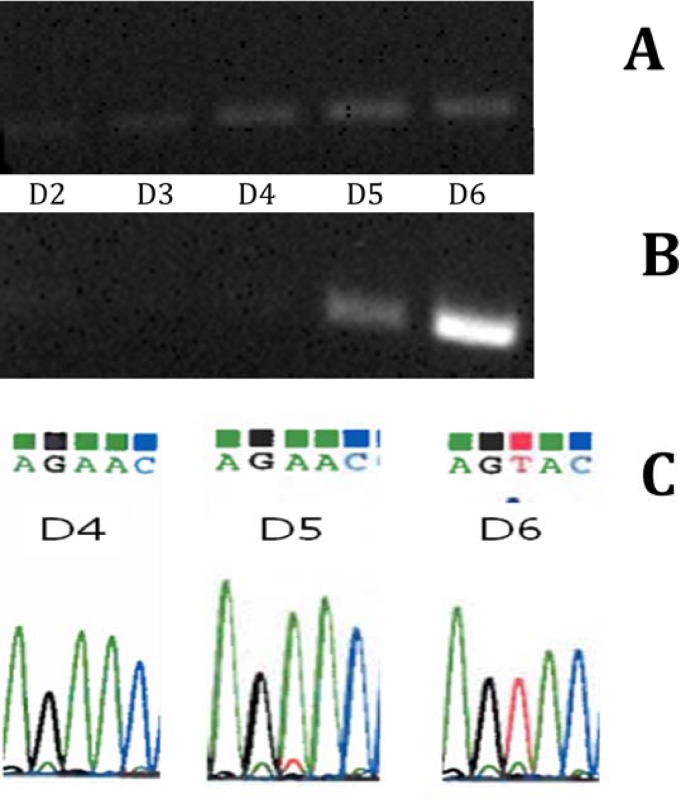
We then evaluated a set of serial NA sequences from group 2 duck 2.3 utilizing RNA extracted from cloacal swabs for days 2, 3, 4, 5, and 6 to determine at which day postinoculation the mutation is first detected. The A-to-T mutation was first detected at day 5 as a mixed A/T population, with the T mutation becoming the dominant nucleotide on day 6 (Fig. 1). This matches the results from the NAI assay that showed no increase in IC50 on day 3 but did detect an increase on day 5. The A/mallard/182742/1998 E119V IC50 8-fold increase results are also consistent with the pair of A/Wuhan/395/95-like (H3N2) sensitive-to-resistant (E119V) control, which showed a similar increase in IC50 values from sensitive-to-resistant strains (Table 5).
Fig 1.
Comparison of site-specific RT-PCR and Sanger sequencing. (A) Site-specific RT-PCR on RNA isolated from cloacal swabs from one duck in group two (2.3) inoculated with A/Mallard/182742/1998 and access to OC at 1,000 ng/liter on days 2 to 6 postinoculation using wild-type primers showing detection of wild-type E119 on all days; (B) site-specific RT-PCR on the same RNA from panel A using E119V resistant primers showing the detection of E119V on days 5 and 6; (C) chromatograms of DNA sequenced from the same duck as that in panels A and B on days 4 to 6 postinoculation showing the visible mutation on day 5 as a small subpopulation, compared with the faint band on day 5 in panel B and as the dominant population on day 6.
For group 3, we did not repeat the 10,000 ng/liter of OC due to lack of viral replication in the previous two experiments. Viral titers were determined by plaque assay on MDCK cells (Table 4), and RNA was extracted directly from original cloacal swabs on the latest time point that virus was detected by plaque assay, followed by RT-PCR and Sanger sequencing of the NA gene. Ducks 3.1, 3.3, and 3.4, who received 1,000 ng/liter of OC in their drinking water, shed virus that had an amino acid change of E119V in the NA gene, along with one other nucleotide change of A to G at position 510 that caused no amino acid change compared to A/Mallard/Minnesota/182742/1998. This is consistent with the results from group 2 from ducks that were inoculated with the same virus.
In group 4, viral titers were determined and RNA was sequenced as outlined for group 3. None of the samples tested from the 10 ducks showed nucleotide or amino acid changes in the NA gene sequence.
Effect of a single dose of oseltamivir phosphate in mallards.
Administration of a single dose of OP shortly after challenge of mallards with the A/Mallard/Minnesota/182742/1998 virus resulted in significant suppression of virus replication in the host. Three of the 4 ducks that received a single dose of OP did not shed any detectable virus on days 0 through 7 (Table 6). One duck shed virus on days 6 and 7 after challenge and drug treatment (Table 6). RNA was extracted from cloacal swabs obtained on days 6 and 7 from this duck, but even though the plaque size of this virus was larger than the parental virus, mutations in the NA gene were not detected by sequencing. Viruses from ducks that did not receive OP were also evaluated by sequencing and no mutations were detected. More work on timing of OP administration, such as administering OP before challenge or administering OP after shedding begins, would help to complete the picture of whether this suggested practice would be beneficial or detrimental.
Table 6.
Viral titers from cloacal swab samples in individual ducks following AIV inoculation and a single dose (5 mg) of OP
| Duck | Drug | Titer at post-virus inoculation daya: |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
| 1 | 5 mg OP | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 2 | 5 mg OP | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 3 | 5 mg OP | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 4 | 5 mg OP | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 2.30 | 3.85 | 0.00 |
| 5 | None | 0.00 | 6.61 | 5.08 | 4.43 | 4.08 | 2.00 | 2.00 | 0.00 |
| 6 | None | 0.00 | 4.08 | 3.95 | 0.00 | 2.18 | 2.30 | 0.00 | 0.00 |
| 7 | None | 0.00 | 6.53 | 0.00 | 0.00 | 5.36 | NT | NT | 0.00 |
| 8 | None | 0.00 | 4.36 | 4.61 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 9 | None | 0.00 | 4.69 | 4.04 | 4.20 | 3.15 | 2.48 | 2.00 | 0.00 |
Viral titers reported in log10 PFU/ml; values of 0.00 represent titers of <10 PFU/ml. Samples highlighted in bold were extracted for RNA, followed by RT-PCR and Sanger sequencing. NT, not tested.
Replication kinetics of wild-type and resistant viruses.
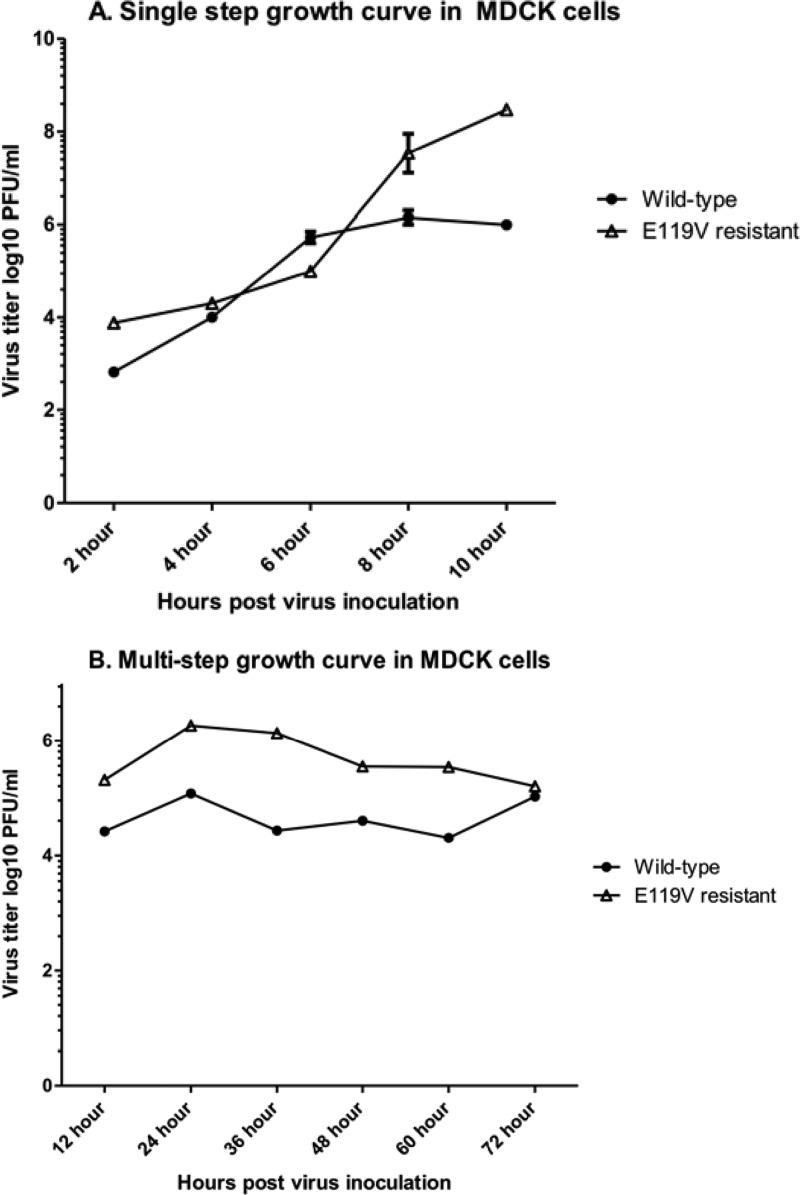
We assayed the replication of both the A/Mallard/Minnesota/182742/1998 virus and its E119V resistant virus, which is the plaque-purified, egg-grown isolate from group 2 duck 2.3, in both single-step and multistep growth curves in MDCK cells. Replication of the MUT-E119V virus was found to be comparable to that of wild-type virus in vitro at each time point, except 8 and 10 h, when the wild type had higher titers than the E119V resistant virus in the single-step growth curve (Fig. 2). For the multistep growth curve, titers of the wild type were higher than the E119V resistant strain until 72 h. A comparison of the slopes of each virus growth curve over time was analyzed using linear regression, and the lack of statistical difference between wild-type and mutant virus slopes over time indicated similar growth rates.
Fig 2.
Growth curves of A/Mallard/Minnesota/182742/1998 and its E119V resistant counterpart. (A) Single-step growth curve of A/Mallard/Minnesota/182742/1998 and E119V resistant virus at an MOI of 2 PFU/cell. Values are plotted as the medians and standard errors from two different replicates for each virus. Replication is similar until 8 h postinoculation, where that of the wild type increases over that of the E119V resistant strain. Statistical evaluation by linear regression determined there were no significant differences in slopes of the two growth curves (P = 0.055). (B) Multistep growth curve of wild-type and E119V resistant viruses at an MOI of 0.01 PFU/cell. Both viruses reach their maximum titer at 24 h postinoculation and vary at all time points except 72 h, with the wild type replicating at a higher titer. The slope comparisons were also not statistically different.
We also observed a change in plaque size between the wild-type and E119V resistant viruses. Plaque size increased from 1 mm in diameter in the wild-type to 3 to 5 mm in diameter for the E119V resistant virus. While the increase in plaque size could reflect a role in the enzymatic activity of NA of the E119V virus, changes in the HA gene or other gene sequences might also cause this change. An occasional large plaque phenotype was detected in the wild-type virus stock, but the sequence analysis of three separate large plaques picked from this stock revealed wild-type NA sequence. Sequencing of the HA genes revealed two amino acid changes between the wild-type and E119V resistant strain at positions 193 (lysine to glutamic acid) and 292 (serine to glycine) in the HA1 portion of the gene.
Transmission of the E119V mutant AIV in mallards.
We evaluated both the replicative ability and transmissibility of the A/Mallard/Minnesota/182742/1998 virus, the E119V resistant virus, and a competitive 1:1 mixture of both viruses in mallard ducks, all in the absence of OC exposure. With the wild-type virus, we demonstrated good replication in the 2 inoculated ducks at day 2 postinoculation and recorded detectable shedding on day 3 from all 6 naïve contact ducks. Viral shedding was detected through day 7 in three ducks, with 1 duck still having detectable virus on day 8, the last day samples were collected (Table 7). Shedding was not detected in the 2 ducks inoculated with the E119V resistant virus until day 3, 1 day later than detectable shedding in ducks inoculated with wild-type virus. The 6 naïve contact control ducks housed with inoculated ducks had detectable virus starting on day 4 and continuing through day 7, showing there was virus transmitted (Table 7). For the 3 ducks inoculated with a 1:1 mixture of wild-type and E119V resistant viruses, there was detectable shedding on day 2 that continued through day 7 in group 1 and through day 8 in groups 2 and 3 (Table 7). These results showed transmission of virus with differing replicative abilities between groups.
Table 7.
Viral titers from cloacal swab samples in individual ducks following transmission experiments
| Virus inoculum | Titer at post-virus inoculation daya: |
|||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| 182742 wild type | ||||||||
| Duck 1 inoculated | 0.00 | 2.00 | 3.70 | 2.30 | 0.00 | 0.00 | 0.00 | 0.00 |
| Duck 2 inoculated | 0.00 | 1.90 | 3.30 | 2.00 | 1.00 | 1.90 | 1.85 | 0.00 |
| Duck 3 contact | 0.00 | 0.00 | 3.75 | 3.30 | 4.04 | 0.00 | 2.60 | 0.00 |
| Duck 4 contact | 0.00 | 0.00 | 3.58 | 1.85 | 3.48 | 2.00 | 1.78 | 0.00 |
| Duck 5 contact | 0.00 | 0.00 | 5.15 | 0.00 | 0.00 | 1.70 | 0.00 | 0.00 |
| Duck 6 contact | 0.00 | 0.00 | 0.00 | 3.30 | 3.30 | 2.00 | 0.00 | 0.00 |
| Duck 7 contact | 0.00 | 0.00 | 4.78 | 2.90 | 3.18 | 0.00 | 0.00 | 2.30 |
| Duck 8 contact | 0.00 | 0.00 | 0.00 | 4.60 | 3.48 | 1.90 | 0.00 | 0.00 |
| E119V resistant | ||||||||
| Duck 9 inoculated | 0.00 | 0.00 | 2.08 | 1.85 | 2.36 | 1.78 | 2.60 | 0.00 |
| Duck 10 inoculated | 0.00 | 0.00 | 1.85 | 2.54 | 3.70 | 1.70 | 1.85 | 0.00 |
| Duck 11 contact | 0.00 | 0.00 | 0.00 | 1.60 | 2.18 | 3.70 | 3.30 | 0.00 |
| Duck 12 contact | 0.00 | 0.00 | 0.00 | 0.00 | 1.70 | 3.48 | 2.60 | 0.00 |
| Duck 13 contact | 0.00 | 0.00 | 0.00 | 1.78 | 2.00 | 3.48 | 2.30 | 0.00 |
| Duck 14 contact | 0.00 | 0.00 | 0.00 | 0.00 | 3.70 | 2.85 | 3.00 | 0.00 |
| Duck 15 contact | 0.00 | 0.00 | 0.00 | 3.30 | 2.04 | 1.78 | 0.00 | 0.00 |
| Duck 16 contact | 0.00 | 0.00 | 0.00 | 0.00 | 3.18 | 4.30 | 0.00 | 0.00 |
| 1:1 mixture | ||||||||
| Duck 17 inoculated | 0.00 | 1.70 | 7.69 | 3.60 | 0.00 | 2.49 | 0.00 | 0.00 |
| Duck 18 contact | 0.00 | 0.00 | 0.00 | 3.18 | 2.23 | 3.30 | 2.60 | 0.00 |
| Duck 19 contact | 0.00 | 0.00 | 4.30 | 3.79 | 4.00 | 3.30 | 1.70 | 0.00 |
| Duck 20 contact | 0.00 | 0.00 | 0.00 | 3.30 | 3.48 | 3.90 | 2.60 | 0.00 |
| Duck 21 inoculated | 0.00 | 3.60 | 4.04 | 2.85 | 3.00 | 2.00 | 0.00 | 1.30 |
| Duck 22 contact | 0.00 | 0.00 | 4.08 | 3.30 | 2.36 | 3.78 | 0.00 | 0.00 |
| Duck 23 contact | 0.00 | 0.00 | 3.95 | 3.85 | 2.00 | 2.60 | 2.18 | 0.00 |
| Duck 24 contact | 0.00 | 0.00 | 3.70 | 3.78 | 3.30 | 0.00 | 0.00 | 0.00 |
| Duck 25 inoculated | 0.00 | 5.60 | 4.00 | 4.48 | 3.58 | 3.30 | 2.78 | 1.85 |
| Duck 26 contact | 0.00 | 0.00 | 0.00 | 4.34 | 3.00 | 2.08 | 2.70 | 0.00 |
| Duck 27 contact | 0.00 | 0.00 | 4.15 | 6.00 | 5.70 | 3.71 | 1.48 | 0.00 |
| Duck 28 contact | 0.00 | 0.00 | 3.49 | 4.20 | 4.34 | 2.78 | 2.60 | 0.00 |
Viral titers reported in log10 PFU/ml; values of 0.00 represent titers of <10 PFU/ml. Samples highlighted in bold were extracted for RNA, followed by RT-PCR and Sanger sequencing.
Virus titers detected from cloacal swabs in both inoculated and naïve contact ducks were analyzed utilizing analysis of variance (ANOVA) by comparing area under the curve (AUC) values for virus shedding. Ducks infected with the wild-type virus by contact had significantly higher AUCs than ducks directly inoculated with the wild-type virus (P = 0.04), ducks directly inoculated with the E119V mutant virus (P = 0.02), ducks directly inoculated with both viruses (P = 0.03), and ducks infected by contact transmission from dually infected ducks (P < 0.0001). Ducks infected with the E119V virus by contact transmission had higher AUCs than ducks housed with dually contact ducks (P = 0.004). Overall, these data revealed higher AUCs from wild-type contact ducks, which was interpreted to indicate that the wild-type virus was more stable and had higher replicative ability in vivo.
Sanger sequencing was performed on RNA from all cloacal swab samples, and all 28 ducks had the E119 wild-type phenotype. Earlier samples from days 2 to 7 from ducks 17, 21, and 25 (Table 7) that were directly inoculated with the E119V resistant virus were also subjected to Sanger sequencing and were determined to not contain the E119V mutation. The lack of detection of E119V in the ducks inoculated with resistant virus, and the lack of transmission of resistant virus, correlates with the higher viral shedding AUC results seen in the wild-type contact ducks and suggests poor replication capacity of the E119V resistant virus in ducks.
Detection of resistant virus in wild-type virus stocks.
We utilized the site-specific RT-PCR to determine whether our original stock of A/Mallard/Minnesota/182742/1998 virus had the E119V mutation at a low level and to discern if the E119V resistant stock had a low level of E119 present in the stock. We did not detect the E119V mutation in the wild-type stock but did detect a faint band suggesting a low level of wild-type E119 in the E119V resistant stock. The low presence of wild-type E119 in the resistant stock virus was not detected by Sanger sequencing, showing the valued addition of this assay. Future experiments could involve reverse genetics making the change E119V to remove the presence of the wild type completely and further assess that this mutation has minimal replicative ability in vivo. It would also be important to analyze transmission of the E119V resistant virus in the presence of OC to determine if the stability of the mutation is dependent on OC or unstable in any scenario.
DISCUSSION
We report here that the E119V NA mutation leading to increased oseltamivir resistance that has been seen in humans has the ability to occur in mallards in the presence of OC, although it appears to be unstable in ducks, with reversion to the oseltamivir-sensitive wild type. In the absence of OC, this mutation did not spontaneously occur in any of the ducks. Since ducks and wading birds are the primary reservoir host of all influenza A virus subtypes, they provide the source of all influenza A viruses that affect mammals, including humans. If oseltamivir-resistant viruses arise in ducks that are stable, they may ultimately contribute to viruses infecting other species, including humans.
Before beginning our AIV studies, we first obtained a baseline understanding of the pharmacokinetics of oseltamivir in ducks. Based on those experiments, it appears that there are some distinct differences in metabolism of this drug in humans versus ducks. Additional research to evaluate concentrations of OC present in the duck digestive tract may better elucidate the actual interaction of drug and virus.
We detected oseltamivir-resistant viruses in 4 out of 6 mallards infected with the A/Mallard/Minnesota/182742/1998 strain of influenza virus exposed to 1,000 ng/liter OC. In these cases, the OC-resistant viruses rapidly came to be the dominant population of virus in treated ducks, likely the result of continued selective pressure. The first day of detection of resistant virus was day 5. The delay in the detection of resistant virus after drug exposure was consistent with previous studies of children treated with oseltamivir during influenza virus infection, in which resistant strains were not detected until day 4 (3) or days 4 and 6 posttreatment (38). Resistant virus was not detected in the 13 control ducks that were not exposed to OC. The 13 ducks that were infected with the A/Mallard/346250/2000 strain, but exposed to OC, also did not produce resistant viruses. Additionally, the 4 ducks exposed to 10,000 ng/liter OC in water failed to shed detectable quantities of virus at any time postinoculation. While both strains of virus used in these experiments were of the subtype H5N2, they were different in their NA sequences and might be expected to behave differently in the presence of oseltamivir, as has been seen within subtypes in human viruses. Analyzing and comparing the other genes may show differences in sequence, leading to a better understanding of the viruses as a whole. In terms of replication capacity of the virus, viral titers displayed in Table 4 show comparable infection and shedding rates between the two viruses. The IC50s of the two mallard wild-type viruses and wild-type controls were comparable (Table 5).
Previous investigations indicate that a considerable amount of OC is not broken down during water treatment processes and is broken down slowly during natural processes, which can lead to the accumulation of OC in the environment (21–28). Therefore, the demonstrated ability of OC in drinking water to select OC-resistant influenza H5N2 virus variants is of concern considering that OC-resistant viruses are already increasing in frequency in human populations (7, 10–12), even in areas of low oseltamivir drug use (8). Differing conditions and more influenza strains should be tested to determine how many virus strains that can replicate in ducks may be subject to possible resistance selection with exposure to OC in drinking water. In this respect, it is interesting to note that a recent study also demonstrated the ability of OC exposure to increase the incidence of the known H275Y resistance mutation in the NA gene of A/Mallard/Sweden/51833/2006 (H1N1) virus in ducks (39).
Analysis of the replication kinetics of both wild-type and E119V resistant viruses indicated that the E119V mutation that arose from the A/Mallard/Minnesota/182742/1998 mallard virus had a selective advantage in the presence of OC that disappeared rapidly in the absence of OC and could not be transmitted to contact ducks, indicating reduced replication fitness in vivo. It was interesting that both wild-type virus and the plaque-purified E119V resistant isolate had similar growth kinetics in MDCK cells, despite rapid conversion to the wild type in vivo. The resistant isolate also showed a large plaque phenotype in vitro. The reason for this in vitro/in vivo difference and for the large plaque phenotype is unknown, although large plaques were also observed occasionally with wild-type virus, and no NA sequence changes were associated with that phenotype. We also evaluated the HA gene of the wild-type and E119V resistant viruses, because interactions between HA and NA could be responsible for the increased plaque size relative to that of the wild type (40–44). HA mutations can also lead to reduced ability of binding of virus to sialic acids that can lead to a reduced dependence of virus on functions provided by NA (45–47). The two amino acid changes in the HA between wild-type and E119V resistant strains do not appear to involve previously noted significant locations, such as sialic acid binding sites or within the HA cleavage site, although the 193-amino-acid change is adjacent to conserved residues for a sialic acid binding site (48).
Within the NA gene there are 8 amino acids identified as catalytic residues (R-118, D-151, R-152, R-224, E-276, R-292, R-371, and Y-406) that are involved in direct contact with the substrate and 11 framework residues (E-119, R-156, W-178, S-179, D-198, I-222, E-227, E-277, N-294, and E-425) which play a role in the stabilization of the active site (49). The E119V mutation has been detected in virus from patients treated with oseltamivir (3, 50–52), and in vitro and in vivo models have shown that viruses with this mutation can replicate and transmit as efficiently as the parent wild-type virus (15, 16).
We observed that mallards inoculated with the E119V resistant virus, alone or as a mixture with the wild-type virus, failed to shed detectable quantities of the E119V resistant virus or to transmit that virus to contact ducks; only the wild-type virus was transmitted in all three groups. This observation suggests that the NA mutation of E119V is not as stable within mallards as it is in cell culture, where it showed similar replication efficiencies. It is possible that the low level of wild-type virus present in the E119V stock used to inoculate the mallards outcompeted the E119V resistant virus within the mallard or that the E119V resistant virus was unstable in the absence of OC and reverted to the wild type following inoculation.
While Sanger sequencing has been shown to be very accurate in detecting mutations, studies have shown that customized pyrosequencing is more sensitive in detecting very low levels of point mutations (53). However, pyrosequencing is expensive and was not pursued as part of these experiments. Other recent research has utilized quantitative real-time or real-time RT-PCR coupled with mathematical models based on differences in Ct values between wild-type and resistant strains for comparison. This can be extremely sensitive for detecting very low levels of a specific mutation (19, 37, 54–56). While we based our site-specific RT-PCR on these models, which correlated with our Sanger sequencing results plus detected one additional sample that Sanger sequencing missed, we recognize that there is a different level of sensitivity between these methods.
We did not detect the E119V resistant strain in the wild-type strain using either Sanger sequencing or site-specific RT-PCR assays but did detect an extremely low level of E119 in the resistant strain by site-specific RT-PCR. We also utilized both methods in the mallard transmission studies and did not detect the E119V mutation in cloacal swabs from any ducks in all 3 groups. However, the delayed appearance of detectable virus (wild type) in the ducks infected with the E119V resistant virus is consistent with de novo reversion of the mutation to wild type, followed by outgrowth of the wild-type virus. While traditional ferret transmission studies look at aerosol or direct contact transmission once the animal is already shedding virus, we choose a different time frame for these mallard studies. Since there is repeated and close interaction of mallards directly in the wild, we allowed this same close contact with the mallard ducks following inoculation of virus to time of interaction with contact naïve ducks. This would be a more likely representation of what happens in nature and would include the possibility of either direct transmission or environmental contamination transmission. Additional avian viruses with neuraminidase mutations should be tested in mallards both in the presence and absence of OC, to better evaluate the potential role such viruses may play in spread of resistant viruses.
As resistant viruses continue to emerge and evolve, we need to evaluate their ability to transmit and persist with or without selective pressure. While ferrets are the acceptable model to evaluate oseltamivir-resistant strains that could affect humans, it is also important to consider the natural reservoir of influenza viruses and the likelihood that these viruses will survive in nature.
ACKNOWLEDGMENTS
This work was supported by cooperative agreement 5 U19 CI000419 from the Centers for Disease Control and Prevention.
The influenza viruses used in these studies were kindly provided by David Stallknecht, Southeastern Cooperative Wildlife Disease Study, University of Georgia. We thank F. Hoffman-La Roche Ltd. for providing us with the OC and OP for our duck studies, as well as John R. Smith for statistical analysis for the pharmacokinetic study and review of the manuscript, and PRA International for testing the mallard plasma concentrations.
We also thank Justin Brown of the University of Georgia for his technical expertise regarding duck inoculations, Jim zumBrunnen at Colorado State University for statistical advice, Jeret Benson, Airn Tolnay, and Angela Bosco-Lauth for their assistance in handling the animals, and Paul Gordy for assistance with animals and sequencing of HA genes.
Footnotes
Published ahead of print 4 March 2013
REFERENCES
- 1. Herlocher ML, Carr J, Ives J, Elias S, Truscon R, Roberts N, Monto AS. 2002. Influenza virus carrying an R292K mutation in the neuraminidase gene is not transmitted in ferrets. Antiviral Res. 54:99–111 [DOI] [PubMed] [Google Scholar]
- 2. Gubareva LV, Kaiser L, Matrosovich MN, Soo-Hoo Y, Hayden FG. 2001. Selection of influenza virus mutants in experimentally infected volunteers treated with oseltamivir. J. Infect. Dis. 183:523–531 [DOI] [PubMed] [Google Scholar]
- 3. Kiso M, Mitamura K, Sakai-Tagawa Y, Shiraishi K, Kawakami C, Kimura K, Hayden FG, Sugaya N, Kawaoka Y. 2004. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet 364:759–765 [DOI] [PubMed] [Google Scholar]
- 4. Le QM, Kiso M, Someya K, Sakai YT, Nguyen TH, Nguyen KH, Pham ND, Ngyen HH, Yamada S, Muramoto Y, Horimoto T, Takada A, Goto H, Suzuki T, Suzuki Y, Kawaoka Y. 2005. Avian flu: isolation of drug-resistant H5N1 virus. Nature 437:1108. [DOI] [PubMed] [Google Scholar]
- 5. de Jong MD, Thanh TT, Khanh TH, Hien VM, Smith GJD, Chau NV, Cam BV, Qui PT, Ha DQ, Guan Y, Peiris JSM, Hien TT, Farrar J. 2005. Brief report—oseltamivir resistance during treatment of influenza A (H5N1) infection. N. Engl. J. Med. 353:2667–2672 [DOI] [PubMed] [Google Scholar]
- 6. McKimm-Breschkin JL, Selleck PW, Usman TB, Johnson MA. 2007. Reduced sensitivity of influenza A (H5N1) to oseltamivir. Emerg. Infect. Dis. 13:1354–1357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sheu TG, Deyde VM, Okomo-Adhiambo M, Garten RJ, Xu X, Bright RA, Butler EN, Wallis TR, Klimov AI, Gubareva LV. 2008. Surveillance for neuraminidase inhibitor resistance among human influenza A and B viruses circulating worldwide from 2004 to 2008. Antimicrob. Agents Chemother. 52:3284–3292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hauge SH, Dudman S, Borgen K, Lackenby A, Hungnes O. 2009. Oseltamivir-resistant influenza viruses A (H1N1), Norway, 2007-08. Emerg. Infect. Dis. 15:155–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Boltz DA, Douangngeun B, Phommachanh P, Sinthasak S, Mondry R, Obert C, Seiler P, Keating R, Suzuki Y, Hiramatsu H, Govorkova EA, Webster RG. 2010. Emergence of H5N1 avian influenza viruses with reduced sensitivity to neuraminidase inhibitors and novel reassortants in Lao People's Democratic Republic. J. Gen. Virol. 91:949–959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dharan NJ, Gubareva LV, Meyer JJ, Okomo-Adhiambo M, McClinton RC, Marshall SA, George KS, Epperson S, Brammer L, Klimov AI, Bresee JS, Fry AM, Oseltamivir-Resistance Working Group 2009. Infections with oseltamivir-resistant influenza A (H1N1) virus in the United States. JAMA 301:1034–1041 [DOI] [PubMed] [Google Scholar]
- 11. Meijer A, Lackenby A, Hungnes O, Lina B, van der Werf S, Schweiger B, Opp M, Paget J, van de Kassteele J, Hay A, Zambon M, European Influenza Surveillance Scheme 2009. Oseltamivir-resistant influenza virus A (H1N1), Europe, 2007–08 season. Emerg. Infect. Dis. 15:552–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hurt AC, Ernest J, Deng YM, Iannello P, Besselaar TG, Birch C, Buchy P, Chittaganpitch M, Chiu SC, Dwyer D, Guigon A, Harrower B, Kei IP, Kok T, Lin C, McPhie K, Mohd A, Olveda R, Panayotou T, Rawlinson W, Scott L, Smith D, D'Souza H, Komadina N, Shaw R, Kelso A, Barr IG. 2009. Emergence and spread of oseltamivir-resistant A(H1N1) influenza viruses in Oceania, South East Asia and South Africa. Antiviral Res. 83:90–93 [DOI] [PubMed] [Google Scholar]
- 13. Hauge SH, Blix HS, Borgen K, Hungnes O, Dudman SG, Aavitsland P. 2009. Sales of oseltamivir in Norway prior to the emergence of oseltamivir resistant influenza A(H1N1) viruses in 2007–08. Virol. J. 6:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Govorkova EA, Ilyushina NA, Boltz DA, Douglas A, Yilmaz N, Webster RG. 2007. Efficacy of oseltamivir therapy in ferrets inoculated with different clades of H5N1 influenza virus. Antimicrob. Agents Chemother. 51:1414–1424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Herlocher ML, Truscon R, Elias S, Yen HL, Roberts NA, Ohmit SE, Monto AS. 2004. Influenza viruses resistant to the antiviral drug oseltamivir: transmission studies in ferrets. J. Infect. Dis. 190:1627–1630 [DOI] [PubMed] [Google Scholar]
- 16. Yen HL, Herlocher LM, Hoffmann E, Matrosovich MN, Monto AS, Webster RG, Govorkova EA. 2005. Neuraminidase inhibitor-resistant influenza viruses may differ substantially in fitness and transmissibility. Antimicrob. Agents Chemother. 49:4075–4084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ives JAL, Carr JA, Mendel DB, Tai CY, Lambkin R, Kelly L, Oxford JS, Hayden FG, Roberts NA. 2002. The H274Y mutation in the influenza A/H1N1 neuraminidase active site following oseltamivir phosphate treatment leaves virus severely compromised both in vitro and in vivo. Antiviral Res. 55:307–317 [DOI] [PubMed] [Google Scholar]
- 18. Yen HL, Ilyushina NA, Salomon R, Hoffmann E, Webster RG, Govorkova EA. 2007. Neuraminidase inhibitor-resistant recombinant A/Vietnam/1203/04 (H5N1) influenza viruses retain their replication efficiency and pathogenicity in vitro and in vivo. J. Virol. 81:12418–12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hurt AC, Nor'e SS, McCaw JM, Fryer HR, Mosse J, McLean AR, Barr IG. 2010. Assessing the viral fitness of oseltamivir-resistant influenza viruses in ferrets using a competitive-mixtures model. J. Virol. 84:9427–9438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bouvier NM, Lowen AC, Palese P. 2008. Oseltamivir-resistant influenza A viruses are transmitted efficiently among guinea pigs by direct contact but not by aerosol. J. Virol. 82:10052–10058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Accinelli C, Sacca ML, Fick J, Mencarelli M, Lindberg R, Olsen B. 2010. Dissipation and removal of oseltamivir (Tamiflu) in different aquatic environments. Chemosphere 79:891–897 [DOI] [PubMed] [Google Scholar]
- 22. Accinelli C, Barra Caracciolo A, Grenni P. 2007. Degradation of the antiviral drug oseltamivir carboxylate in surface water samples. Int. J. Environ. Anal. Chem. 87:579–587 [Google Scholar]
- 23. Bartels P, von Tumpling W. 2008. The environmental fate of the antiviral drug oseltamivir carboxylate in different waters. Sci. Total Environ. 405:215–225 [DOI] [PubMed] [Google Scholar]
- 24. Fick J, Lindberg RH, Tysklind M, Haemig PD, Waldenstrom J, Wallensten A, Olsen B. 2007. Antiviral oseltamivir is not removed or degraded in normal sewage water treatment: implications for development of resistance by influenza A virus. PLoS One 2:e986 doi:10.1371/journal.pone.0000986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hutchinson TH, Beesley A, Frickers PE, Readman JW, Shaw JP, Straub JO. 2009. Extending the environmental risk assessment for oseltamivir (Tamiflu) under pandemic use conditions to the coastal marine compartment. Environ. Int. 35:931–936 [DOI] [PubMed] [Google Scholar]
- 26. Sacca ML, Accinelli C, Fick J, Lindberg R, Olsen B. 2009. Environmental fate of the antiviral drug Tamiflu in two aquatic ecosystems. Chemosphere 75:28–33 [DOI] [PubMed] [Google Scholar]
- 27. Singer AC, Nunn MA, Gould EA, Johnson AC. 2007. Potential risks associated with the proposed widespread use of Tamiflu. Environ. Health Persp. 115:102–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Straub JO. 2009. An environmental risk assessment for oseltamivir (Tamiflu) for sewage works and surface waters under seasonal-influenza- and pandemic-use conditions. Ecotox. Environ. Safe. 72:1625–1634 [DOI] [PubMed] [Google Scholar]
- 29. Soderstrom H, Jarhult JD, Olsen B, Lindberg RH, Tanaka H, Fick J. 2009. Detection of the antiviral drug oseltamivir in aquatic environments. PLoS One 4:e6064 doi:10.1371/journal.pone.0006064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ghosh GC, Nakada N, Yamashita N, Tanaka H. 2010. Oseltamivir carboxylate, the active metabolite of oseltamivir phosphate (Tamiflu), detected in sewage discharge and river water in Japan. Environ. Health Persp. 118:103–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Achenbach JE, Bowen RA. 2011. Transmission of avian influenza A viruses among species in an artificial barnyard. PLoS One 6:e17643 doi:10.1371/journal.pone.0017643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chander Y, Jindal N, Stallknecht DE, Sreevatsan S, Goyal SM. 2010. Full-length sequencing of all nine subtypes of the neuraminidase gene of influenza A viruses using subtype specific primer sets. J. Virol. Met. 165:116–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275–2289 [DOI] [PubMed] [Google Scholar]
- 34. Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. 2011. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol. Biol. Evol. 28:2731–2739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Latorra D, Campbell K, Wolter A, Hurley JM. 2003. Enhanced allele-specific PCR discrimination in SNP genotyping using 3′ locked nucleic acid (LNA) primers. Hum. Mutat. 22:79–85 [DOI] [PubMed] [Google Scholar]
- 36. Newton CR, Graham A, Heptinstall LE, Powell SJ, Summers C, Kalsheker N, Smith JC, Markham AF. 1989. Analysis of any point mutation in DNA—the amplification refractory mutation system (ARMS). Nucleic Acids Res. 17:2503–2516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Renaud C, Kuypers J, Corey L. 2010. Diagnostic accuracy of an allele-specific reverse transcriptase-PCR assay targeting the H275Y oseltamivir resistant mutation in 2009 pandemic influenza A/H1N1 virus. J. Clin. Virol. 49:21–25 [DOI] [PubMed] [Google Scholar]
- 38. Whitley RJ. 2001. Oral oseltamivir treatment of influenza in children. Pediatr. Infect. Dis. J. 20:127–133 [DOI] [PubMed] [Google Scholar]
- 39. Jarhult JD, Muradrasoli S, Wahlgren J, Soderstrom H, Orozovic G, Gunnarsson G, Brojer C, Latorre-Margalef N, Fick J, Grabic R, Lennerstrand J, Waldenstrom J, Lundkvist A, Olsen B. 2011. Environmental levels of the antiviral oseltamivir induce development of resistance mutation H274Y in influenza A/H1N1 virus in mallards. PLoS One 6:24742 doi:10.1371/journal.pone.0024742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gerloff NA, Kremer JR, Mossong J, Opp M, Muller CP. 2009. Genomic diversity of oseltamivir-resistant influenza virus A (H1N1), Luxembourg, 2007–08. Emerg. Infect. Dis. 15:1523–1524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kaverin NV, Gambaryan AS, Bovin NV, Rudneva IA, Shilov AA, Khodova OM, Varich NL, Sinitsin BV, Makarova NV, Kropotkina EA. 1998. Postreassortment changes in influenza A virus hemagglutinin restoring HA-NA functional match. Virology 244:315–321 [DOI] [PubMed] [Google Scholar]
- 42. Mitnaul LJ, Matrosovich MN, Castrucci MR, Tuzikov AB, Bovin NV, Kobasa D, Kawaoka Y. 2000. Balanced hemagglutinin and neuraminidase activities are critical for efficient replication of influenza A virus. J. Virol. 74:6015–6020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rameix-Welti MA, Enouf V, Cuvelier F, Jeannin P, van der Werf S. 2008. Enzymatic properties of the neuraminidase of seasonal H1N1 influenza viruses provide insights for the emergence of natural resistance to oseltamivir. PLoS Pathog. 4:e1000103 doi:10.1371/journal.ppat.1000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wagner R, Matrosovich M, Klenk HD. 2002. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev. Med. Virol. 12:159–166 [DOI] [PubMed] [Google Scholar]
- 45. Gubareva LV, Bethell R, Hart GJ, Murti KG, Penn CR, Webster RG. 1996. Characterization of mutants of influenza A virus selected with the neuraminidase inhibitor 4-guanidino-Neu5Ac2en. J. Virol. 70:1818–1827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. McKimm-Breschkin JL, Blick TJ, Sahasrabudhe A, Tiong T, Marshall D, Hart GJ, Bethell RC, Penn CR. 1996. Generation and characterization of variants of NWS/G70C influenza virus after in vitro passage in 4-amino-Neu5Ac2en and 4-guanidino-Neu5Ac2en. Antimicrob. Agents Chemother. 40:40–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Staschke KA, Colacino JM, Baxter AJ, Air GM, Bansal A, Hornback WJ, Munroe JE, Laver WG. 1995. Molecular basis for the resistance of influenza viruses to 4-guanidino-Neu5Ac2en. Virology 214:642–646 [DOI] [PubMed] [Google Scholar]
- 48. McCullough C, Wang M, Rong L, Caffrey M. 2012. Characterization of influenza hemagglutinin interactions with receptor by NMR. PLoS One 7:e33958 doi:10.1371/journal.pone.0033958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Colman PM, Varghese JN, Laver WG. 1983. Structure of the catalytic and antigenic sites in influenza virus neuraminidase. Nature 303:41–44 [DOI] [PubMed] [Google Scholar]
- 50. Baz M, Abed Y, McDonald J, Boivin G. 2006. Characterization of multidrug-resistant influenza A/H3N2 viruses shed during 1 year by an immunocompromised child. Clin. Infect. Dis. 43:1555–1561 [DOI] [PubMed] [Google Scholar]
- 51. Ison MG, Gubareva LV, Atmar RL, Treanor J, Hayden FG. 2006. Recovery of drug-resistant influenza virus from immunocompromised patients: a case series. J. Infect. Dis. 193:760–764 [DOI] [PubMed] [Google Scholar]
- 52. Okomo-Adhiambo M, Demmler-Harrison GJ, Deyde VM, Sheu TG, Xu XY, Klimov AI, Gubareva LV. 2010. Detection of E119V and E119I mutations in influenza A (H3N2) viruses isolated from an immunocompromised patient: challenges in diagnosis of oseltamivir resistance. Antimicrob. Agents Chemother. 54:1834–1841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Levine M, Sheu TG, Gubareva LV, Mishin VP. 2011. Detection of hemagglutinin variants of the pandemic influenza A (H1N1) 2009 virus by pyrosequencing. J. Clin. Microbiol. 49:1307–1312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Chidlow GR, Harnett GB, Williams SH, Tempone SS, Speers DJ, Hurt AC, Deng YM, Smith DW. 2010. The detection of oseltamivir-resistant pandemic influenza A/H1N1 2009 viruses using a real-time RT-PCR assay. J. Virol. Methods 169:47–51 [DOI] [PubMed] [Google Scholar]
- 55. Liu CM, Driebe EM, Schupp J, Kelley E, Nguyen JT, McSharry JJ, Weng QM, Engelthaler DM, Keim PS. 2010. Rapid quantification of single-nucleotide mutations in mixed influenza A viral populations using allele-specific mixture analysis. J. Virol. Methods 163:109–115 [DOI] [PubMed] [Google Scholar]
- 56. van der Vries E, Jonges M, Herfst S, Maaskant J, Van der Linden A, Guldemeester J, Aron GI, Bestebroer TM, Koopmans M, Meijer A, Fouchier RAM, Osterhaus ADME, Boucher CA, Schutten M. 2010. Evaluation of a rapid molecular algorithm for detection of pandemic influenza A (H1N1) 2009 virus and screening for a key oseltamivir resistance (H275Y) substitution in neuraminidase. J. Clin. Virol. 47:34–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Brennan BJ, Davies B, Cirrincione-Dall G, Morcos PN, Beryozkina A, Chappey C, Baldo PA, Lennon-Chrimes S, Rayner CR. 2012. Safety, tolerability, and pharmacokinetics of intravenous oseltamivir: single- and multiple-dose phase I studies with healthy volunteers. Antimicrob. Agents Chemother. 56:4729–4737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. He G, Massarella J. 1999. Clinical pharmacokinetics of the prodrug oseltamivir and its active metabolite Ro 64-0802. Clin. Pharmacokinet. 37:471–484 [DOI] [PubMed] [Google Scholar]