Abstract
Objectives:
Life evolved in an environment filled with a wide variety of ionizing and non-ionizing radiation. It was previously reported that medical exposures to pregnant women increases the risk of low birth weight. This study intends to investigate the relationship between exposure to ionizing and non-ionizing radiation and the risk of low birth weight.
Materials and Methods:
One thousand two hundred mothers with their first-term labor (vaginal or cesarean) whose newborns’ history had been registered in neonates’ screening program in Shiraz were interviewed and surveyed. Data collection was performed by the assessment of mother's history of radiography before and during pregnancy, physical examination of the mother for height and weight and weighing and examining the newborn for any diagnosis of disease and anomalies.
Results:
There were no statistical significant differences between the mean weight of newborns whose mothers had been exposed to some common sources of ionizing and non-ionizing radiations such as dental or non dental radiographies, mobile phone, cordless phone and cathode ray tube (CRT) and those of non-exposed mothers.
Conclusions:
The findings of this study cast doubt on previous reports, which indicated that exposure to ionizing radiation during pregnancy increased the risk of low birth weight.
Keywords: Ionizing radiation, low birth weight, non-ionizing radiation, pregnancy, term labor
INTRODUCTION
Life was evolved in an environment filled with different radiations of natural origin. It is believed that irradiation of non-reproductive organs with low dose in pregnant mothers is without risk.[1] However, in a study, it was argued that dental radiography during pregnancy increased the risk of low birth weight owing to its effect on hypothalamus-pituitary-thyroid (HPT) axis (not direct irradiation of reproductive organs or fetus).[1]
As the study referred to suffering from some structural drawbacks such as ignoring the interfering variables and lack of data on dental radiation, we have made an attempt in the present study to investigate the issue more accurately by making some changes in methodology. Although, the effects of diagnostic radiation on women during pregnancy or non-pregnancy have been emphasized, the findings of some studies, particularly studies on the mothers receiving radiation from radioactive iodine (I-131) shows that radiation does not have any relationship with newborns birth weight.[2,3]
Pre-term labor is a serious problem occurring in 8% of pregnancies. The neonates born before 37th week are pre-mature or preterm. About 2/3 of newborns with low birth weight (LBW) are preterm. Using the World Health Organization (WHO) classification,[4] LBW refers to the weight lower than 2500 g., very LBW, the weight lower than 1500 g. and extremely LBW, the weight lower than 1000 g. Two-thirds of pre-mature deaths in the newborns are due to pre-term labor. The pre-term neonate might be larger than, smaller than or the right size in proportion to the gestational age. Smaller neonates due to intrauterine growth retardation (IUGR) who are below 10% of weight to gestational age are called term low birth weight (TLBW). In such cases, labor is after 37 weeks. It is suspected that 3 to 4% of newborns suffer from IUGR. It is also maintained that size and weight of the fetus is determined in the first and second trimester of pregnancy. Unfavorable growth in the first trimester of pregnancy is with growth limitation and pre-term labor occurs within 24 to 32 weeks.[5,6] The weight of fetus grows significantly during the third trimester. In a study on pregnancy outcomes of offspring of women previously exposed to therapeutic doses of radioiodine (I-131), it is reported that the incidences of stillbirths, preterm births, low birth weight, congenital malformations, and death during the first year of life were not significantly different before and after 131I therapy.[7] In contrast with the previous report, it has been argued that for each cGy radiation, there is 37.6 g weight reduction in the newborn.[8] One study revealed that the women, who had flank abdominal radiotherapy, were susceptible to premature labor and low birth weight infants.[9] It was found in another study that the girls who had received high doses of radiation for their childhood cancer were liable to LBW newborns.[10,11] It has also been reported that ionizing radiation affects ovarian and uterine function and causes pregnancy complications such as low birth weight.[12]
Furthermore, it has been shown that the adults who undergo diagnostic radiography for idiopathic scoliosis are susceptible to having LBW newborns.[8] Likewise, it has been reported that the rate of radiation exposure in mothers with LBW newborns was more than those with normal weight newborns.[13]
In 2005, some researchers studied the effects of thyroid irradiation and subsequently malfunction of thyroid because of the effect of radiation on IUGR and found that thyroid diagnostic radiography correlates with low birth weight to a small extent. It is claimed that diagnostic radiologic procedures in pregnancy does not usually increase the natural risk of congenital anomalies but they cause maternal anxiety.[14] Studies with 60Co have shown that the irradiation of the whole body of the mother during pregnancy correlates with the growth of the newborn after birth.[13] In a study in 2004, it has been argued that radiation with a determined dose in dental radiography increases the risk of LBW.[1] It is interesting that the cause has been reported to be the effect of radiation on hypothalamus-pituitary-thyroid (HPT) axis. The percentage of dental radiography in American pregnant women was around 10%. According to this study, such irradiation increases the risk of LBW and particularly TLBW.
On the other hand, there are reports indicating an increased risk of delivering low birth weight infants (<2500 g) in patients treated with abdominal or pelvic radiation.[11,15–18] Moreover, it has been shown that radiation due to the presence of radioactive 137Cs in the environment (due to Chernobyl accident) did not have any relationship with birth weight.[19] Another study indicated no effect due to radiation after Chernobyl accident on pregnancy outcome, particularly LBW.[20] Most studies have found that radiations emitted from radiographies of non-reproductive organs in low doses does not affect the fetus.[21] Reviewing the studies in this connection, we find different and sometimes contradictory results. Over the past years our laboratory has focused on studying the health effects of exposure of humans to some common sources of electromagnetic fields such as mobile phones[22–24] and MRI.[25] Consequently, the present study intends to investigate the effect of exposure to some common sources of ionizing and non-ionizing radiations as dental or non dental radiographies, mobile phone, cordless phone and cathode ray tube (CRT) on low birth weight.
MATERIALS AND METHODS
All mothers with their first-term labor (vaginal or cesarean) whose newborns’ history had been registered in the neonates’ screening program in Shiraz were interviewed and surveyed. That is, based on the mothers’ history and their history of exposure to ionizing and non-ionizing radiation, 1,200 newborns were divided into exposed and non-exposed groups. These groups were matched regarding the age of pregnancy, sex of the newborn and the mother body mass index (BMI). Mothers with at least one of the following factors were excluded from the study (exclusion criteria): 1) Mother's illness (chronic blood pressure, blood pressure resulting from pregnancy, apparent diabetes or diabetes during pregnancy, heart diseases, chronic anemia, renal diseases, chronic pulmonary diseases, rheumatologic diseases, and hyperthyroidism). 2) Smoking and/or drinking alcohol. 3) Mother's addiction. 4) Multiples. 5) Congenital anomalies. 6) Placenta abnormalities. 7) Multipars. 8) Mother's age less than 20 and more than 40. 9) Mother's weight less than 45 kg and more than 70 kg.
The following were used to collect the related data: 1) Mother's history of radiography during pregnancy. 2) Physical examination of the mother for height and weight. 3) Weighing and examining the newborn for any diagnosis of disease and anomalies.
In this study, labor in the week 37 or later was considered on term and birth weight less than 2500 g as LBW. As it is argued that what happens to hypothalamus-pituitary-thyroid axis due to radiation from dental radiography leads to low birth weight, we made attempts to collect more accurate data by investigating non-dental (head and neck) radiography, in addition to those obtained from dental radiography. As there was no intervention, ethical considerations did not provide any considerable limitation for the study. However, written informed consent was obtained from all participants.
The data obtained were analyzed, using SPSS, statistical t-tests and ANOVA. In all cases, a difference with P < 0.05 was considered significant.
RESULTS
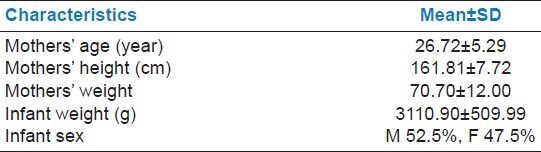
Of 1200 mothers whose newborns were studied, their age, height and weight means were 26.72 ± 5.29 years, 161.81 ± 7.72 cm and 70.70 ± 12.00 kg, respectively. Demographic characteristics of the mothers and their neonates are indicated in Table 1. Regarding the sex of the newborns, 52.5% were male and 47.5% female. On the whole, only 1.1% of the newborns were twins, 0.1% multiples and the rest (98.8%) were singleton. Based on the inclusion criteria, only the singleton newborns were investigated here.
Table 1.
Demographic characteristics of mothers and their neonates
In this study, only 19 mothers (1.58%) had been exposed to radiations from dental radiography. Based on the information on the potential dose of radiation in dental radiography in Iran, the amount of radiation exposure to mothers and fetuses were estimated. The mean birth weight of newborns to these mothers was 2988.95 ± 424.80 g. and that of newborns to mothers not exposed to dental radiation was 3113.00 ± 511.24g [Table 2]. The difference between these means was not statistically significant. Only 22 mothers (1.8%) had been exposed to non-dental radiography. The mean birth weight of newborns to such mothers was 3017.50 ± 497.21 g and that of newborns to mothers not exposed to non-dental radiography was 3112.59 ± 510.28g. The difference between these means was not statistically significant, either. Only 50 mothers (4.16%) had been exposed to radiations from dental and non-dental radiographies before their pregnancy. The mean birth weight of newborns to mothers with a radiography history was 3015.08 ± 469.90 g. and that of newborns to mothers without radiography history was 3116.22 ± 511.80 g. The difference between these two means was not statistically significant either.
Table 2.
Effects of pregnant mother's exposure to some ionizing and non-ionizing radiation on birth weight
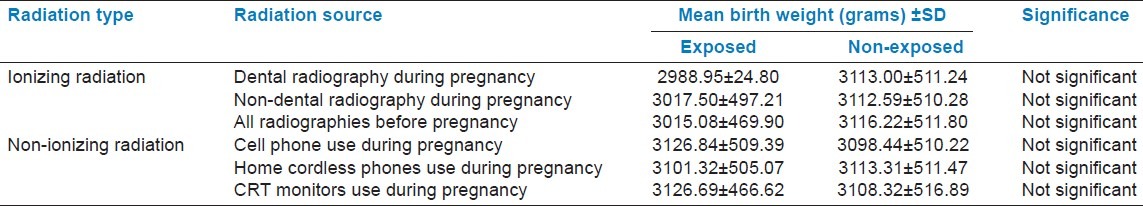
Regarding the non-ionizing radiation, we found that there was not statistically any significant difference between the birth weight of newborns to mothers exposed to electromagnetic fields (cell phones, cordless telephone, cathode-ray tube and so on) during their pregnancy and that of newborns to mothers not exposed to such radiations. Among these mothers in our study, 52.75% had made use of cell phones during their pregnancy. The mean birth weight of newborns to mothers making use of cell phones was 3126.84 ± 509.39 g and that of newborns to mothers not using cell phones was 3098.44 ± 51.22 g. Again, the difference was not statistically significant.
Also among these mothers in our study, 78.5% had never made use of home cordless phones during their pregnancy. The mean birth weight of newborns to these mothers was 3113.31 ± 511.47 g and the mean birth weight of newborns to mothers who had used such phones during their pregnancy was 3101.32 ± 505.07 g. Again the difference between the means was not statistically significant.
Finally, among these mothers in this study, 84.5% had never used monitors with the cathode ray tube (CRT) technology during their pregnancy. The mean birth weight of newborns to such mothers was 3108.32 ± 516.89 g and newborns to mothers using such devices was 3126.69 ± 466.69 g. Again no statistically significant difference was found between these two groups. The effects of exposure to ionizing and non-ionizing radiation during pregnancy on birth weight are displayed in Table 1.
DISCUSSION
Altogether, our study could not show any statistical significant difference between the mean weight of newborns whose mothers had been exposed to some common sources of ionizing and non-ionizing radiations such as dental or non dental radiographies, mobile phone, cordless phone and cathode ray tube (CRT) and those of the non-exposed mothers. In contrast with what is claimed in a previously published article that pregnant women's exposure to dental radiography increases the risk of low birth weight.[1] our study showed that there was no statistically significant difference between the birth weight of newborns to mothers exposed to dental radiography during their pregnancy and that of newborns to mothers not exposed.
As was mentioned above, in our study only 19 mothers (1.58%) had undergone dental radiography, but the percentage of dental radiography in pregnant women in America is not clearly reported. However, it is claimed that only 22 to 34% of women in the United States consult a dentist during pregnancy.[26] The low percentage of Iranian mothers who have radiography during pregnancy can be mainly due to their fear of the radiography risk (so-called radiophobia) on one hand, and expensive dental services in the country and lack of insurance coverage by insurance companies, on the other hand.
Although, the percentage of dental radiography by pregnant women is much more in America than that in our study, previous studies by Mortazavi, et al. shows that unlike intraoral radiography, the exposure dose in OPG in Iran is more than that in other countries. Lack of any dose reference level in the country had intensified such problems.[27,28]
Furthermore, the difference between the mean birth weight of newborns to mothers exposed and mothers not exposed to radiations from dental and non-dental radiographies was not statistically significant. Our findings are in contrast with some reports with a low sample size, which have suggested a correlation between mean birth weight and radiographies in women during pregnancy. In this regard, it was shown in a study that radiography by pregnant women is associated with the increasing risk of LBW. Also, it is indicated that girls exposed to a large dose of therapeutic radiation before puberty were susceptible of having newborns with LBW.[10,11] Meanwhile, Hujoel, et al. in their longitudinal study (from 1993 to 2000) concluded that both low and high doses of radiography increased the risk of LBW, particularly TLBW because of the effects of radiography on HPT axis.[1] A group of investigators in their study came to the conclusion that for each cGy radiation, there will be a weight loss of 37.6 g in the newborn.[8]
It is widely believed that women exposed to therapeutic radiation for a long time are susceptible to premature labor, if they get pregnant.[6] In their studies, Goldberg et al. found that adolescents who undergo diagnostic radiography for idiopathic scoliosis are susceptible to having newborns with LBW.[8] The findings of two surveys; i.e. National Natality Survey (NNS) and National Fetal Mortality Survey (NFMS) showed that radiation exposure rates were higher for mothers who had low birth weight infants (<2,500 g) than for those who had normal weight infants.[13]
In a study performed by Benson and Shulman in the United States in 2005, an increase in low birth weight was reported in areas with high levels of natural (background) radiation.[29] Although, our results are not in line with those reported by Benson and Shulman, they are in line with the findings of another study that indicated those diagnostic radiographies during pregnancy, which are not involving direct abdominal/pelvic exposure to high doses of ionizing radiation, are not associated with any significant adverse events.[30]
The different findings can be explained by the fact that it has been turned out that radiation doses causing growth anomalies in newborns are much higher than those in dental radiographies.[21] As a result, it seems that within low dose domains, the probability of the effect of radiation on birth weight is very low.
Furthermore, the mean birth weight of newborns to mothers who have been exposed to electromagnetic fields (cell phones, cordless telephone, cathode ray tube, and so on) was not statistically different from that of newborns to mothers not exposed to such devices.
CONCLUSION
The present findings on the extent of the effects of radiation with low doses in pregnant women on newborns birth weight are different and somehow contradictory. This study did not find any clear relationship between mothers’ exposure to some common sources of ionizing and non-ionizing radiation during pregnancy and their newborns’ weight. Our findings, particularly, cast serious doubts on findings published in JAMA that dental radiography by pregnant women increases the risk of low birth weight in newborns.
ACKNOWLEDGMENT
This study was supported by the Center for Research on Radiation Sciences (CRRS), Shiraz University of Medical Sciences. This project was financially supported by Shiraz University of Medical Sciences (grant No. 4124).
Footnotes
Source of Support: Shiraz University of Medical Sciences (grant No. 4124).
Conflict of Interest: None declared
REFERENCES
- 1.Hujoel PP, Bollen AM, Noonan CJ, del Aguila MA. Antepartum dental radiography and infant low birth weight. JAMA. 2004;291:1987–93. doi: 10.1001/jama.291.16.1987. [DOI] [PubMed] [Google Scholar]
- 2.Schlumberger M, De Vathaire F, Ceccarelli C, Delisle MJ, Francese C, Couette JE, et al. Exposure to radioactive iodine-131 for scintigraphy or therapy does not preclude pregnancy in thyroid cancer patients. J Nucl Med. 1996;37:606–12. [PubMed] [Google Scholar]
- 3.Casara D, Rubello D, Saladini G, Piotto A, Pelizzo MR, Girelli ME, et al. Pregnancy after high therapeutic doses of iodine-131 in differentiated thyroid cancer: Potential risks and recommendations. Eur J Nucl Med. 1993;20:192–4. doi: 10.1007/BF00169997. [DOI] [PubMed] [Google Scholar]
- 4.International statistical classification of diseases and related health problems. Genava: World Health Organization; 2004. WHO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Gilstrap LM, Wenstrom KD. Williams obstetrics. 21st ed. New York: McGraw-Hill; 2001. [Google Scholar]
- 6.Smith GC. First trimester origins of fetal growth impairment. Semin Perinatol. 2004;28:41–50. doi: 10.1053/j.semperi.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Garsi JP, Schlumberger M, Rubino C, Ricard M, Labbe M, Ceccarelli C, et al. Therapeutic administration of 131I for differentiated thyroid cancer: Radiation dose to ovaries and outcome of pregnancies. J Nucl Med. 2008;49:845–52. doi: 10.2967/jnumed.107.046599. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg MS, Mayo NE, Levy AR, Scott SC, Poitras B. Adverse reproductive outcomes among women exposed to low levels of ionizing radiation from diagnostic radiography for adolescent idiopathic scoliosis. Epidemiol. 1998;9:271–8. [PubMed] [Google Scholar]
- 9.Critchley HO, Bath LE, Wallace WH. Radiation damage to the uterus-review of the effects of treatment of childhood cancer. Hum Fertil (Camb) 2002;5:61–6. doi: 10.1080/1464727022000198942. [DOI] [PubMed] [Google Scholar]
- 10.Edgar AB, Wallace WH. Pregnancy in women who had cancer in childhood. Eur J Cancer. 2007;43:1890–4. doi: 10.1016/j.ejca.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Reulen RC, Zeegers MP, Wallace WH, Frobisher C, Taylor AJ, Lancashire ER, et al. Pregnancy outcomes among adult survivors of childhood cancer in the British Childhood Cancer Survivor Study. Cancer Epidemiol Biomarkers Prev. 2009;18:2239–47. doi: 10.1158/1055-9965.EPI-09-0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hudson MM. Reproductive outcomes for survivors of childhood cancer. Obstet Gynecol. 2010;116:1171–83. doi: 10.1097/AOG.0b013e3181f87c4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hamilton PM, Roney PL, Keppel KG, Placek PJ. Radiation procedures performed on U.S. women during pregnancy: Findings from two 1980 surveys. Public Health Rep. 1984;99:146–51. [PMC free article] [PubMed] [Google Scholar]
- 14.De Santis M, Di Gianantonio E, Straface G, Cavaliere AF, Caruso A, Schiavon F, et al. Ionizing radiations in pregnancy and teratogenesis: A review of literature. Reprod Toxicol. 2005;20:323–9. doi: 10.1016/j.reprotox.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 15.Green DM, Whitton JA, Stovall M, Mertens AC, Donaldson SS, Ruymann FB, et al. Pregnancy outcome of female survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Am J Obstet Gynecol. 2002;187:1070–80. doi: 10.1067/mob.2002.126643. [DOI] [PubMed] [Google Scholar]
- 16.Green DM, Sklar CA, Boice JD, Jr, Mulvihill JJ, Whitton JA, Stovall M, et al. Ovarian failure and reproductive outcomes after childhood cancer treatment: Results from the Childhood Cancer Survivor Study. J Clin Oncol. 2009;27:2374–81. doi: 10.1200/JCO.2008.21.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Signorello LB, Cohen SS, Bosetti C, Stovall M, Kasper CE, Weathers RE, et al. Female survivors of childhood cancer: Preterm birth and low birth weight among their children. J Natl Cancer Inst. 2006;98:1453–61. doi: 10.1093/jnci/djj394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green DM, Lange JM, Peabody EM, Grigorieva NN, Peterson SM, Kalapurakal JA, et al. Pregnancy outcome after treatment for Wilms tumor: A report from the national Wilms tumor long-term follow-up study. J Clin Oncol. 2010;28:2824–30. doi: 10.1200/JCO.2009.27.2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Irgens LM, Lie RT, Ulstein M, Skeie Jensen T, Skjaerven R, Sivertsen F, et al. Pregnancy outcome in Norway after Chernobyl. Biomed Pharmacother. 1991;45:233–41. doi: 10.1016/0753-3322(91)90023-m. [DOI] [PubMed] [Google Scholar]
- 20.Matteson SR, Joseph LP, Bottomley W, Finger HW, Frommer HH, Koch RW, et al. The report of the panel to develop radiographic selection criteria for dental patients. Gen Dent. 1991;39:264–70. [PubMed] [Google Scholar]
- 21.White SC, Pharoah MJ. Oral Radiology: Principles and. Interpretation. 5th ed. United States: Mosby; 2004. [Google Scholar]
- 22.Mortazavi SM, Ahmadi J, Shariati M. Prevalence of subjective poor health symptoms associated with exposure to electromagnetic fields among University students. Bioelectromagnetics. 2007;28:326–30. doi: 10.1002/bem.20305. [DOI] [PubMed] [Google Scholar]
- 23.Mortazavi SM, Mahbudi A, Atefi M, Bagheri S, Bahaedini N, Besharati A. An old issue and a new look: Electromagnetic hypersensitivity caused by radiations emitted by GSM mobile phones. Technol Health Care. 2011;19:435–43. doi: 10.3233/THC-2011-0641. [DOI] [PubMed] [Google Scholar]
- 24.Mortazavi SM, Rouintan MS, Taeb S, Dehghan N, Ghaffarpanah AA, Sadeghi Z, et al. Human short-term exposure to electromagnetic fields emitted by mobile phones decreases computer-assisted visual reaction time. Acta Neurol Belg. 2012;112:171–5. doi: 10.1007/s13760-012-0044-y. [DOI] [PubMed] [Google Scholar]
- 25.Mortazavi SM, Daiee E, Yazdi A, Khiabani K, Kavousi A, Vazirinejad R, et al. Mercury release from dental amalgam restorations after magnetic resonance imaging and following mobile phone use. Pak J Biol Sci. 2008;11:1142–6. doi: 10.3923/pjbs.2008.1142.1146. [DOI] [PubMed] [Google Scholar]
- 26.Silk H, Douglass AB, Douglass JM, Silk L. Oral health during pregnancy. Am Fam Physician. 2008;77:1139–44. [PubMed] [Google Scholar]
- 27.Mortazavi SM, Shareghi A, Ghiassi-Nejad M, Kavousi A, Jafari-Zadeh M, Nazeri F, et al. The need for national diagnostic reference levels: Entrance surface dose measurement in intraoral radiography. Iran J Radiat Res. 2004;2:127–33. [Google Scholar]
- 28.Mortazavi SM, Ghiassi-Nejad M, Bakhshi M, Jafari-Zadeh M, Kavousi A, Ahmadi J, et al. Entrance surface dose measurement on the thyroid gland in orthopantomography: The need for optimization. Iran J Radiat Res. 2004;2:21–6. [Google Scholar]
- 29.Benson BW, Shulman JD. Effect of antepartum natural background radiation on infant low birth weight: A pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:E22. [Google Scholar]
- 30.Lowe SA. Diagnostic radiography in pregnancy: Risks and reality. Aust N Z J Obstet Gynaecol. 2004;44:191–6. doi: 10.1111/j.1479-828X.2004.00212.x. [DOI] [PubMed] [Google Scholar]


