Abstract
Human experimental pain models are essential in understanding the pain mechanisms and appear to be ideally suited to test analgesic compounds. The challenge that confronts both the clinician and the scientist is to match specific treatments to different pain-generating mechanisms and hence reach a pain treatment tailored to each individual patient. Experimental pain models offer the possibility to explore the pain system under controlled settings. Standardized stimuli of different modalities (i.e., mechanical, thermal, electrical, or chemical) can be applied to the skin, muscles, and viscera for a differentiated and comprehensive assessment of various pain pathways and mechanisms. Using a multimodel-multistructure testing, the nociception arising from different body structures can be explored and modulation of specific biomarkers by new and existing analgesic drugs can be profiled. The value of human experimental pain models is to link animal and clinical pain studies, providing new possibilities for designing successful clinical trials. Spontaneous pain, the main compliant of the neuropathic patients, but currently there is no human model available that would mimic chronic pain. Therefore, current human pain models cannot replace patient studies for studying efficacy of analgesic compounds, although being helpful for proof-of-concept studies and dose finding.
Keywords: Analgesics, multimodel-multitissue, pain models, proof-of-concept, spontaneous pain
INTRODUCTION
Pain is the most prevalent health care problem, and characterization of pain is of major importance in the diagnosis and choice of treatment.[1] In clinical practice, the different symptoms of the underlying disease or complaints relating to psychological, cognitive and social aspects of the illness, as well as systemic reactions such as fever and general malaise confound the characterization of pain.[2] This may bias the clinical evaluation in assessing the efficacy of analgesics; also, repeated exposures to drug make patients familiar with its side effects and increase the chance of "active placebo" effects.[3] Because of these limitations, human experimental pain models are often helpful in preclinical studies of new analgesics. Also, in human models, the investigator can control the experimentally induced pain, including the nature, localization, intensity, frequency and duration of the stimulus and provide quantitative measures of the psychological, behavioral or neurophysiological responses.[4]
Most of the animal models of pain rely on detecting a change in the threshold or response to an applied stimulus and the absence of verbal communication in animals is undoubtedly an obstacle to the evaluation of pain. Also, the neurobiology of nociceptive systems differ between species and this limits the extrapolation of findings from animal studies to man.[5] However, the animal models can be used as tools to help to find-out the relative contribution of different pain mechanisms in changing an animal's behavior in a given situation.[6]
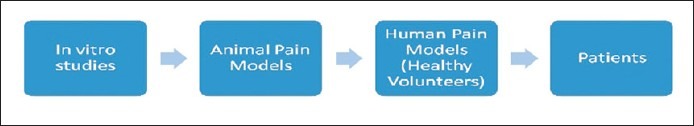
Human experimental pain models can act as a translational bridge between animal and clinical research and many of the mechanisms tested in animals can also be translated [Figure 1] and evaluated in healthy volunteers and used to predict the efficacy of a given drug in specific patient populations[4] [Figure 2]. Finally, reproducibility of the method is an important factor; if reproducibility is good, the model can be useful in drug screening[7] and randomized controlled trials are the ideal to explore the effectiveness of the clinical intervention.[8]
Figure 1.
Human experimental pain models: Focus on translation
Figure 2.

Examples for the scope of pain indications
Assessment of the output from these pain models can be based on psychophysical or neurophysiological methods.[9] Psychophysical methods are the simplest way to assess the pain response[10] and are based on subjective experience of pain, measured on standard scales or as pain thresholds and neurophysiological methods include measurement of evoked brain potentials or nociceptive withdrawal reflexes.
DEFINITIONS
Allodynia
Pain due to a stimulus which does not normally provoke pain [Figure 3].
Figure 3.

Illustrates hyperalgesia; manifested locally (primary hyperalgesia) and by central sensitization (secondary hyperalgesia), for example, after freeze injury or 30 minutes after application of capsaicin
Hyperalgesia
An increased response to a noxious stimulus, caused by sensitization of peripheral nociceptors (primary hyperalgesia: The area of tissue injury) and/or by sensitization of central neurons (secondary hyperalgesia: outside the area of the original tissue injury) [Figure 3].
Temporal Summation/Windup Like Pain
It is a phenomenon that occurs when a repetition of a stimulus increases pain perception.
Spatial summation
It is a phenomenon that occurs when a non-painful stimulus is perceived as painful when applied to a wider area.
Referred pain
Pain that is felt in a part of the body at a distance from the area of stimulation.
PAIN-INDUCTION METHODS
Pain models can be classified according to their presumed mechanism (inflammatory vs neuropathic), the involved tissue (skin vs muscle vs viscera) and their time course (phasic - shorter, lasting for milliseconds to seconds vs tonic - longer, lasting for minutes). However, mechanistically the most important categories are peripheral or central sensitization. Conceptually, the two forms of sensitization are strictly separated; but, most of the pain models are characterized by a combination of peripheral and central sensitization. For example, cutaneous freeze injury lead to both allodynia and hyperalgesia.[11] The present review gives a brief overview of the pain models according to the tissue type, with an intention for the development of the sensitive pain model methods based on the knowledge of earlier methods described in the present review.
MECHANICAL STIMULATION
Mechanical stimulation of the skin
Mechanical stimulation of the skin can be grouped into Touch, Pin Prick, and Pinching. This method has been used to evaluate the effect of clonidine, oxycodone, morphine, mepivacain, bupivacain, gabapentin, carbamazepine, and amitriptyline.
Touch
Sensitivity to touch can be assessed by applying a light pressure with a finger[12] or using a von Frey hair.[13] A-beta fiber mediate touch sensation.[14]
Major shortcomings
The von Frey hair activates both low threshold mechanoreceptors and nociceptors and is not specific.[6] Also, touch is used mainly to explore allodynia evoked by other pain stimuli.[15]
Pin-prick
Stimulation of the skin gently with a needle[16] or a safety pin[17] or thick von Frey filament and pain is reported as pricking or "first pain".[15] Pin-prick stimulation predominantly activates A-delta fibres.[14]
Major shortcomings
The rapidity of pain onset and termination is not easily controlled.[6,18]
Pressure
A skin flap can be squeezed between two pressure sensors[19] or a finger, toe[20] or an ear lobe[16] can be pinched between the algometer probe and a pinch handle.
Major shortcomings
The rapidity of pain onset and termination is not easily controlled.[6,18] Pain during pinching is a combination of mechanical stimulation and local ischemia.[21]
Mechanical stimulation of the muscle
This is typical exogenous experimental pain model and has been used for drug assessment of morphine, oxycodone, rofecoxib, tramadol, codeine, imipramine, and ketamine.
Pressure algometry is the most frequently applied technique for quantification of pain, where the probe is applied to a hard body structures, such as periosteum[16] or soft tissue such as muscles.[19] Both A-delta and C-fibers mediate pain induced by pressure stimulation.[22]
Major shortcomings
The technique is nonspecific since receptors in the skin, and probably deeper tissues will be activated.
Mechanical stimulation of the viscera
Mechanical stimulation of viscera has been used to evaluate the effect of serotonin (5-HT) 4receptor agonist tegaserod, as well as oxycodone, morphine, Octreotide (a somatostatin analog), nifedipine, NMDA receptor antagonist ketamine, tricyclic antidepressants like imipramine, amitriptyline.
Mechanical stimulation in viscera using balloon distension has been widely used to study pain perception thresholds, referred pain and cerebral activation patterns[23] as well as, to screen new analgesics in healthy subjects and those with gut disorders.[24,25] The introduction of the electronic barostat, has helped to ensure proper location of the balloon, regardless of the inflation paradigm that was used. The newer methods based on impedance planimetry, allows recording of the luminal cross-sectional area directly and estimation of the radius in the distended segment of the esophagus or intestine.[26]
Major shortcomings
Unlike the rectum and the stomach, the esophagus doesn′t serve as a storage organ, but rather as a conduct. Consequently intraesophageal distensions do not mimic a normal, physiologic stimulus and thus perceptual responses to such a stimulus may have no scientific merit. In addition, difficulties in tolerating balloon distension, commonly results in poor recruitment rates as well as the potential for esophageal perforation, have made esophageal balloon distensions by a barostat a less attractive research tool.
THERMAL STIMULATION
Thermal stimulation of the skin
A cold stimulation/cold pressor pain. Application of ice,[27] a cold gel bag,[28] a wet alcohol sponge[12] menthol[29,30] ether, or a Peltier thermode to the skin evokes cold sensation. The method has been intensively used for drug screening such as imipramine, paroxetine, morphine, codeine, tramadol, and oxycodone.
Nociceptors of cutaneous veins appear to mediate cold pain in humans[31] via activation of A-delta and C-fibres.[32] However, a lack of standardization in the cold pressor model is revealed, with substantial variation in both equipment and methodology used.[33]
Major shortcomings
Vascular reactions strongly affect the response and cold pressor pain has shown contradictionary results in the testing of analgesics.[7] Also, pain onset and offset are gradual, and the experiment is not repeatable within a 1--2 hour session.[18]
Freeze lesion
Application of cold temperatures (-20°C) at a standardised pressure provides stable testing conditions for 1 day.[34]
Major shortcomings
A central component of the analgesia can be explored, even if the method is thought to evoke mainly peripheral mechanisms.[35]
Contact heat
The most commonly used heat/cold contact stimulators are based on the Peltier principle (one direction of the current causes cooling and the other way heating).[36] Warm sensation is mediated by C-fibers.[37,38] At threshold determinations, rapid skin heating activates first A-delta fibres, corresponds to the "first pain" followed by a C-fibre mediated second pain, being described as ′throbbing, burning or swelling′.[39] Slow heating gives a preferential activation of C-fibers (thought to be most important for peripheral opioid receptors) and the best evaluation of second pain.[7] In order to prevent injuries to the skin, the high temperature limit is recommended to be 50 °C and the low limit 5 °C.[40]
Major shortcomings
Contact of the thermode with the skin activates concomitant low-threshold non-nociceptors. The rate of thermal transfer depends on the thermode-skin contact and thus on the pressure of application of the thermode. Therefore it is important that the thermode is applied to skin at a standardized fashion.
Radiant heat
Laser pulses evoke a distinct pricking pain in skin.[40,41] Intensities higher than those evoking pricking pain are avoided, as they may cause superficial burns.[42] Depending on the stimulus intensity, laser-induced thermal stimulation produces a double pain sensation: an initial prick sensation attributable to A-delta fiber activity[41] and a second diffuse burning sensation due to C-fiber activity.[43] Different laser emission sources have been developed in pain research e.g. argon, copper vapor[44,45] thulium-YAG and laser diodes, but CO 2-laser[46] is most commonly used.[40] The argon[44] and copper vapor lasers[45] operate, a different principle than CO2-laser, where in CO2-laser, radiation is absorbed within the epidermis, independent of skin pigmentation and application angle. Whereas, in the Argon-laser much of the radiant heat is reflected, causing variation depending on the skin pigmentation and the application angle.[47] In all laser studies, the spot of stimulation has to be shifted slightly between consecutive stimuli in order not to cause receptor sensitization/fatigue. Irradiation using ultraviolet B (UVB), produces stable areas of primary hyperalgesia over several hours.[48,49]
Major shortcomings
Variability in responses between the individuals was observed.[6,47]
Burn injury
The burn injury model illustrates hyperalgesia. Contact heat and radiant heat can induce burn injury by, e.g., application of a constant temperature of 47 °C for 5 min (leads to long lasting sensitization). The brief thermal sensitization model (BTS; 45 °C for 3 min) provides short lasting sensitization and can be induced 2-3 times at hourly intervals without skin injury. Among the endogenous inflammatory mediators, prostaglandin E2 may be responsible for early heat hyperalgesia.[50] Whereas in longer lasting mechanical hyperalgesia nerve growth factor may be involved.[51,52] Both A-delta and C-fibres mediate pain after a burn injury.[15]
Major shortcomings
The threshold for activation of mainly A delta-fibres may transform into thresholds for activation of C-fibres. As these respond to other stimulus modalities it may confuse the testing of an analgesic.[6]
Thermal stimulation of the muscle
Warm and cold pain has been evoked from muscle tissue when saline at different temperatures is injected intramuscularly.[53]
Major shortcomings
No drug studies have been performed.
Thermal stimulation of viscera
Phasic thermal stimuli of the human gastrointestinal tract are believed to activate unmyelinated afferents in the mucosa selectively. This is opposed to mechanical and electrical stimuli, which activate afferents in both superficial and deep layers.[54] Thermosensitive mucosal afferents have been demonstrated in the human esophagus, stomach and rectum.[26,54] Human gastrointestinal tract shows a uniform perception of thermal stimuli with different reflex responses from the stomach to the jejunum.[55] The temperature of recirculating water, when continuously measured inside a balloon positioned in the esophagus, showed a linear stimulus-response relationship, demonstrating the validity of the activation.[26]
Major shortcomings: Only a few pharmacological studies have been performed using thermal visceral stimulation (e.g., oxycodone and morphine).
ELECTRICAL STIMULATION
Electrical stimulation of the skin
Various electrical stimulator devices connected to electrodes applied either to the skin surface[28] or the intracutaneous tissue[56] evoke electrical stimulation. Stimulator devices can deliver different stimulation pattern, for example, different waveforms, frequencies and duration of stimuli. This activates with some selectivity different afferents and nervous structures, and hence evokes different kinds of pain.[6,7] Electrical stimulation excites nerve fiber populations and the relative proportion of activation of individual fiber types depends on the stimulus intensity.[7] C-fibers have a higher activation threshold than A-delta fibers. Drug studies on drug classes like opioids, tricyclic antidepressants and NSAIDs have been performed using electrical stimulus of different intensities.
Major shortcomings
Electrical stimulation bypasses the receptors and activates the nerve fibers directly, and the method is not a specific activation of the nociceptors. The electrical threshold is related to the fiber diameter and one cannot usually excite small-diameter nerves without additionally exciting others.
Electrical stimulation of the muscle
Electrical stimulation of the muscle can be performed via small needle electrodes with un-insulated tips.[57] Repeated electrical stimulation can induce temporal summation and cause increase in referred pain areas, thus reflecting central changes.[58,59] The technique has been used to evaluate drugs such as remifentanil, morphine, alfentanil, oxycodone, and ketamine.
Major shortcomings
Electrical stimulation is not nociceptive specific as it bypasses the receptors. Furthermore, concurrent activated muscle twitches may confound the sensation evoked by intramuscular electrical stimulation.[60]
Electrical stimulation of the viscera
Electrical stimulation of the gut has been widely used to study basic pain mechanisms, pain characteristics, referred pain and evoked brain potentials. The use of electrical stimulation has demonstrated safety in all parts of the gastrointestinal system. Furthermore, the well-defined onset and offset of the stimulation eliminates the latency as observed with other methods, making this particularly suitable for neurophysiological assessments.-[2,61] The technique has been used successfully in drug studies of valdecoxib, parecoxib, morphine, oxycodone, and ketamine.
Major shortcomings
Electrical gut stimulation, bypasses the receptors and activates the nerve fibers directly. The major drawback with earlier methods was the varying electrode contact with the mucosa, giving inconsistent results.
CHEMICAL STIMULATION
Chemical stimulation of the skin
Capsaicin
Intradermal injection or topical application of capsaicin directly evokes pain, and hyperalgesia.[62] Capsaicin induced pain has been suggested as a surrogate model of changes observed in neuropathic pain. Mostly C-fibres are thought to mediate pain.[63] Capsaicin application activates t ransient receptor potential vanilloid 1 (TRPV1) receptors. This model is widely used for drug evaluations, such as the effect of neurotoxins (e.g., Botox) on TRPV1 sensitive nociceptive endings, as well as ketamine, magnesium, lidocaine, alfentanil, diclofenac, orphenadrine, gabapentin, cannabis, lamotrigine, H1 antagonists, hydromorphone, and the lidocaine patch.
Major shortcomings
Variable response was obtained with the model, e.g., pharmacological testing of lamotrigine and desipramine which are used in the treatment of neuropathic pain failed to show any effects in the model.[63,64] On the other hand gabapentin, which is also used to treat neuropathic pain, suppresses hyperalgesia following heat-capsaicin sensitization.[65]
Mustard oil
Topical application of mustard oil induces pain and hyperalgesia. C-fibres are thought to mediate the burning pain, while A-beta fibers are believed to mediate allodynia to light mechanical stimuli.[15]
Major shortcomings
The method has not been used much in the testing of analgesics. The use of these models is basically limited to target engagement studies.
Chemical stimulation of muscle
Intramuscular infusion of hypertonic saline[59,66] glutamate[67] and capsaicin[68] induces pain and referred pain areas. Hypertonic saline mimics musculoskeletal pain in both subjectively perceived quality as well as its effects on motor performance.[69] The dominant sensation following hypertonic saline injections in the muscle is a deep and diffuse pain, via activation of C-fibres. Earlier manual bolus infusions of hypertonic saline were used. Standardization of a small bolus volume is easy to accomplish by a computer-controlled infusion pump. This provides more reproducible method[60] and have been used to evaluate the effects of the NMDA receptor blocker, ketamine, as well as morphine and alfentanil. Intramuscular injections of algesic substances such as bradykinin[70] , serotonin[70] , substance P[70] , potassium chloride, L-ascorbic acid, and acid phosphate buffer are other chemical stimulation methods to evoke muscular pain.
Major shortcomings
Hypertonic saline injections may excite both non-nociceptive and nociceptive nerve fibers. The chemical stimulation methods all have a problematic reproducibility with large interindividual differences.[71]
Chemical stimulation of the viscera
Chemical stimulation is believed to be the ideal experimental visceral pain stimulus, closely resembles clinical inflammation. Acid stimulation of the esophagus is the most common method to sensitize the gut.[72] Application of glycerol to the large intestine evoked pain in patients with the irritable bowel syndrome.[73] In the colon mucosa, injections of 2%--6% hypertonic saline resulted in deep as well as referred nonpainful and painful perceptions.[2] Most chemical stimuli are believed to activate predominantly unmyelinated C-fibers.[74] Application of capsaicin in the ileum resulted in a dose-dependent pain response and referred pain.[2] Chemical stimulation of gut using algogenic substances like alcohol, bradykinin has also been performed in humans.[2]
Major shortcomings
The major disadvantage of chemical stimulation is a relatively long latency time to the onset of effects and often responses are not reproducible when repeated.
ENDOGENOUS METHODS OF MUSCLE STIMULATION
Ischemic stimulation
The tourniquet model is a classical experimental pain model that induces ischemic muscle pain. Earlier methods of producing experimental pain by occluding the blood flow of exercising muscles failed to demonstrate satisfactory response. The modified method developed by smith et al.[75] more closely resembles pain of pathologic origin. It has been used in human analgesic assays such as morphine, tramadol, caffeine, rofecoxib, aspirin, ibuprofen. This model is applicable in experimental studies requiring a general tonic pain stimulus.[60]
Major shortcomings
It is a very efficient model to induce pain in the muscles but is non-specific, since skin, periosteum, and other tissues will contribute to the overall pain perception. When activating nociceptors, concomitantly low-threshold non-nociceptive nerves can be activated by the contact of the tourniquet with the skin. This activation can exert an inhibitory influence on pain mechanisms.
Pain evoked by exercise
Delayed onset muscle soreness (DOMS) is a sensation of muscular pain during active contractions or passive stretch of a muscle after unaccustomed or eccentric exercise, which peaks 24-48 hours after exercise.[76] DOMS is thought to be caused by structural damage to muscle that leads to the release in the muscle of algogenic substances such as prostaglandins.[77–79] These algogenic substances sensitize A-delta and C nociceptive fibres.[79] Large mechanoreceptor afferents from muscle, muscle spindle and tendons are activated in DOMS, and may also contribute to the pain syndromes.[80–84] This model was used for drug evaluations, such as morphine, tramadol, codeine, ketoprofen, diclofenac, ibuprofen, rofecoxib and naproxen.
Major shortcomings
Neural mechanisms that leads to DOMS were incompletely understood. Variable results were obtained.[85,86,87] Animal studies show that a stress-induced analgesia can occur with eccentric exercise.[88] These also bias the results in analgesic testing.
SCOPE OF TRANSLATIONAL PAIN RESEARCH
Traditionally, translational research is regarded as a process of bridging bench findings to clinical application and the process requires coordinated bidirectional approaches between bedside and bench because of the subjective nature of the pain. This is an advantage in proof-of-concept studies, where the efficacy of a given compound on specific mechanisms can be assessed and the dose-response relationship can be determined.
The link between sensitization in inflammatory models such as UVB burn and clinical inflammatory conditions is considerably good. Also, a new model of peripheral and central sensitization without inflammation: intracutaneous injection of nerve growth factor[89] which appears to generate a combination of symptoms similarly found in patients. However, even these models only reflect part of the disease. Still we lack information about the role of trophic factors for the long-term modulation of nociceptor structure and sensitivity. Therefore, current theories or concepts of pain mechanisms need to be critically reviewed and analyzed to provide a new roadmap of contemporary pain research.
Spontaneous pain is a salient feature of clinical pain, which is the main complaint of neuropathic patients, reported to have more severe depression and physical disability[90] is not mimicked in most of the human pain models.[10] This essential gap is based on ethical limitations of human models according to which no healthy volunteers can be turned into a chronic pain patient. Irrespective of this limitation, the mechanism leading to spontaneous pain is unknown and even the site of origin is debated.
Finally, the pain arising from the skin, muscles and viscera differ from one another, and hence compounds may show very different effects on pain from these structures. Therefore, the concept of multimodel, multitissue pain assessment has been developed, where advanced drug screening in healthy volunteers and patients is possible. Therefore, a meaningful translation process through clinical studies should begin with careful choices of appropriate clinical pain conditions that are consistent with the conditions examined in preclinical models.
ACKNOWLEDGMENTS
We thank the Director, Nizam's Institute of Medical Sciences for providing necessary infrastructure.
Footnotes
Source of Support: ICMR, Government of India
Conflict of Interest: None declared.
REFERENCES
- 1.Konig HH, Bernert S, Angermeyer MC. Health Status of the German Population: Results of a Representative Survey Using the euroqol questionnaire. Gesundheitswesen. 2005;67:173–82. doi: 10.1055/s-2005-857991. [DOI] [PubMed] [Google Scholar]
- 2.Drewes AM, Gregersen H, Arendt-Nielsen L. Experimental pain in gastroenterology: A reappraisal of human studies. Scand J Gastroenterol. 2003;38:1115–30. doi: 10.1080/00365520310004399. [DOI] [PubMed] [Google Scholar]
- 3.Leber PD, Davis CS. Threats to the validity of clinical trials employing enrichment strategies for sample selection. Control Clin Trials. 1998;19:178–87. doi: 10.1016/s0197-2456(97)00118-9. [DOI] [PubMed] [Google Scholar]
- 4.Arendt-Nielsen L, Curatolo M, Drewes A. Human experimental pain models in drug development: Translational pain research. Curr Opin InvestigDrugs. 2007;8:41–53. [PubMed] [Google Scholar]
- 5.Le Bars D, Gozariu M, Cadden SW. Animal Models of Nociception. Pharmacol Rev. 2001;53:597–652. [PubMed] [Google Scholar]
- 6.Woolf CJ, Max MB. Mechanism-based Pain Diagnosis: Issues for Analgesic Drug Development. Anesthesiology. 2001;95:241–9. doi: 10.1097/00000542-200107000-00034. [DOI] [PubMed] [Google Scholar]
- 7.Handwerker HO, Kobal G. Psychophysiology of experimentally induced pain. Physiol Rev. 1993;73:639–71. doi: 10.1152/physrev.1993.73.3.639. [DOI] [PubMed] [Google Scholar]
- 8.Dolatian M, Hasanpour A, Montazeri Sh, Heshmat R, Alavi Majd H. The Effect of Reflexology on Pain Intensity and Duration of Labor on Primiparas. Iran Red Crescent Med J. 2011;13:475–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Gracely RH. Pain measurement. Acta Anaesthesiol Scand. 1999;43:897–908. doi: 10.1034/j.1399-6576.1999.430907.x. [DOI] [PubMed] [Google Scholar]
- 10.Schmelz M. Translating nociceptive processing into human pain models. Exp Brain Res. 2009;196:173–8. doi: 10.1007/s00221-009-1809-2. [DOI] [PubMed] [Google Scholar]
- 11.Chassaing C, Schmidt J, Eschalier A, Cardot JM, Dubray C. Hyperalgesia induced by cutaneous freeze injury for testing analgesics in healthy volunteers. Br J Clin Pharmacol. 2006;61:389–97. doi: 10.1111/j.1365-2125.2006.02582.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rocco AG, Raymond SA, Murray E, Dhingra U, Freiberger D. Differential spread of blockade of touch, cold and pin prick during spinal anesthesia. Anesth Analg. 1985;64:917–23. [PubMed] [Google Scholar]
- 13.Liu SS, Ware PD. Differential sensory block after spinal bupivacaine in volunteers. Anesth Analg. 1997;84:115–9. doi: 10.1097/00000539-199701000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Burke D, Mackenzie RA, Skuse NF, Lethlean AK. Cutaneous afferent activity in median and radial nerve fascicles: A microelectrode study. J Neurol Neurosurg Psychiatry. 1975;38:855–64. doi: 10.1136/jnnp.38.9.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curatolo M, Petersen-Felix S, Arendt-Nielsen L. Sensory assessment of regional anaesthesia in humans.A review of methods and applications. Anesthesiology. 2000;93:1517–30. doi: 10.1097/00000542-200012000-00025. [DOI] [PubMed] [Google Scholar]
- 16.Curatolo M, Petersen-Felix S, Arendt-Nielsen L, Zbinden AM. Epidural epinephrine and clonidine: Segmental analgesia and effects on different pain modalities. Anesthesiology. 1997;87:785–94. doi: 10.1097/00000542-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Butterworth J, Ririe DG, Thompson RB, Walker FO, Jackson D, James RL. Differential onset of median nerve block: Randomized, double-blind comparision of mepivacaine and bupivacaine in healthy volunteers. Br J Anaesth. 1998;81:515–21. doi: 10.1093/bja/81.4.515. [DOI] [PubMed] [Google Scholar]
- 18.FW Quimby. Pain in animals and humans. ILAR J. 1991;1:1–33. (Formerly ILAR News) [Google Scholar]
- 19.Staahl C, Christrup LL, Andersen SD, Arendt-Nielsen L, Drewes AM. A comparative study of oxycodone and morphine in a multi-model, tissue-differentiated experimental pain model. Pain. 2006;123:28–36. doi: 10.1016/j.pain.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 20.Brennum J, Kjeldsen M, Jensen K, Jensen TS. Measurements of human pressure-pain thresholds on fingers and toes. Pain. 1989;38:211–7. doi: 10.1016/0304-3959(89)90240-6. [DOI] [PubMed] [Google Scholar]
- 21.Schmelz M, Schmidt R, Bickel A, Handwerker HO, Torebjörk HE. Differential sensitivity of mechanosensitive and insensitive C-fibers in human skin to tonic pressure and capsaicin. Soc Neurosci Abstr. 1997;23:1004. [Google Scholar]
- 22.Adriaensen H, Gybels J, Handwerker HO, Van Hees J. Nociceptor discharges and sensations due to prolonged noxious mechanical stimulation. A paradox. Hum Neurobiol. 1984;3:53–8. [PubMed] [Google Scholar]
- 23.Silverman DH, Munakata JA, Ennes H, Mandelkern MA, Hoh CK, Mayer EA. Regional cerebral activity in normal and pathological perception of visceral pain. Gastroenterology. 1997;112:64–72. doi: 10.1016/s0016-5085(97)70220-8. [DOI] [PubMed] [Google Scholar]
- 24.Van der Schaar PJ, Lamers CB, Masclee AA. The role of the barostat in human research and clinical practice. Scand J Gastroenterol Suppl. 1999;230:52–63. doi: 10.1080/003655299750025552. [DOI] [PubMed] [Google Scholar]
- 25.Delvaux M, Louvel D, Lagier E, Scherrer B, Abitbol JL, Frexinos J. The k agonist fedotozine relieves hypersensitivity to colonic distension in patients with irritable bowel syndrome. Gastroenterology. 1999;116:38–45. doi: 10.1016/s0016-5085(99)70226-x. [DOI] [PubMed] [Google Scholar]
- 26.Drewes AM, Schipper KP, Dimcevski G, Petersen P, Andersen OK, Gregersen H, et al. Multimodal assessment of pain in the esophagus: A new experimental model. Am J Physiol Gastrointest Liver Physiol. 2002;283:G95–103. doi: 10.1152/ajpgi.00496.2001. [DOI] [PubMed] [Google Scholar]
- 27.Liu S, Kopacz DJ, Carpenter RL. Quantitative assessment of differential sensory nerve block after lidocaine spinal anaesthesia. Anesthesiology. 1995;82:60–3. doi: 10.1097/00000542-199501000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Curatolo M, Petersen-Felix S, Arendt-Nielsen L, Lauber R, Hogstrom H, Scaramozzino P, et al. Adding sodium bicarbonate to lidocaine enhances the depth of epidural blockade. Anesth Analg. 1998;86:341–7. doi: 10.1097/00000539-199802000-00024. [DOI] [PubMed] [Google Scholar]
- 29.Wasner G, Schattschneider J, Binder A, Baron R. Topical menthola human model for cold pain by activation and sensitization of C nociceptors. Brain. 2004;127:1159–71. doi: 10.1093/brain/awh134. [DOI] [PubMed] [Google Scholar]
- 30.Peier AM, Moqrich A, Hergarden AC, Reeve AJ, Andersson DA, Story GM, et al. A TRP channel that senses cold stimuli and menthol. Cell. 2002;108:705–15. doi: 10.1016/s0092-8674(02)00652-9. [DOI] [PubMed] [Google Scholar]
- 31.Klement W, Arrndt JO. The role of nociceptors of cutaneous veins in the mediation of cold pain in man. J Physiol. 1992;449:73–83. doi: 10.1113/jphysiol.1992.sp019075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davis KD. Cold-induced pain and prickle in the glabrous and hairy skin. Pain. 1998;75:47–57. doi: 10.1016/S0304-3959(97)00203-0. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell LA, MacDonald RAR, Brodie EE. Temperature and the Cold Pressor Test. J Pain. 2004;5:233–7. doi: 10.1016/j.jpain.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 34.Lötsch J, Angst M. The mopioid agonist remifentanil attenuates hyperalgesia evoked by blunt and punctuated stimuli with different potency: A pharmacological evaluation of the freeze lesion in humans. Pain. 2003;102:151–61. doi: 10.1016/s0304-3959(02)00349-4. [DOI] [PubMed] [Google Scholar]
- 35.Burian M, Irmgaard T, Seegel M, Geisslinger G. Peripheral and central antihyperalgesic effects of diclofenac in a model of human inflammatory pain. Clin Pharmacol Ther. 2003;74:113–20. doi: 10.1016/S0009-9236(03)00165-6. [DOI] [PubMed] [Google Scholar]
- 36.Kenshalo DR, Bergen DC. A device to measure cutaneous temperature sensitivity in humans and subhuman species. J Appl Physiol. 1975;39:1038–40. doi: 10.1152/jappl.1975.39.6.1038. [DOI] [PubMed] [Google Scholar]
- 37.Fowler , CJ , Sitzoglou K, Ali Z, Halonen P. The conduction velocities of peripheral nerve fibres conveying sensations of warming and cooling. J Neurol Psychiatry. 1988;51:1164–70. doi: 10.1136/jnnp.51.9.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yarnitsky D, Ochoa JL. Warm and cold specific somatosensory systems.Psychophysical thresholds, reaction times and peripheral conduction velocities. Brain. 1991;114:1819–26. doi: 10.1093/brain/114.4.1819. [DOI] [PubMed] [Google Scholar]
- 39.Hughes AM, Rhodes J, Fisher G, Sellers M, Growcott JW. Assessment of the effect of dextromorphan and ketamine on the acute nociceptive threshold and wind-up of the second pain response in healthy male volunteers. Br J Clin Pharmacol. 2002;53:604–12. doi: 10.1046/j.1365-2125.2002.01602.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arendt-Nielsen L, Chen AC. Lasers and other thermal stimulators for activation of skin nociceptors in humans. Neurophysiol Clin. 2003;33:259–68. doi: 10.1016/j.neucli.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 41.Arendt-Nielsen L. First pain event related potentials to argon laser stimuli: Recording and quantification. J Neurol Neurosurg Psychiatry. 1990;53:398–404. doi: 10.1136/jnnp.53.5.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arendt-Nielsen L, Oberg B, Bjerring P. Quantitative assessment of extradural bupivacaine analgesia. Br J Anaesth. 1990;65:633–8. doi: 10.1093/bja/65.5.633. [DOI] [PubMed] [Google Scholar]
- 43.Arendt-Nielsen L. Second pain event related potentials to argon laser stimuli: Recording and quantification. J Neurol Neurosurg Psychiatry. 1990;53:405–10. doi: 10.1136/jnnp.53.5.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Arendt-Nielsen L, Bjerring P. Sensory and pain threshold characteristics to laser stimuli. J Neurol Neurosurg Psychiatry. 1988;51:35–42. doi: 10.1136/jnnp.51.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Svensson P, Bjerring P, Arendt-Nielsen L, Nielsen JC, Kaaber S. Comparison of four laser types for experimental pain stimulation on oral mucosa and hairy skin. Lasers Surg Med. 1991;11:313–24. doi: 10.1002/lsm.1900110402. [DOI] [PubMed] [Google Scholar]
- 46.Mor J, Carmon A. Laser emitted radiant heat for pain research. Pain. 1975;1:233–7. doi: 10.1016/0304-3959(75)90040-8. [DOI] [PubMed] [Google Scholar]
- 47.Bromm R, Treede RD. Laser-evoked cerebral potentials in the assessment of cutaneous pain sensitivity in normal subjects and patients. Revue Neurol(Paris) 1991;147:625–43. [PubMed] [Google Scholar]
- 48.Gustor VB, Anzenhofer S, Sycha T, Lehr S, Kress HG. The sunburn pain model: The stability of primary and secondary hyperalgesia over 10 hours in a crossover setting. Anesth Analg. 2004;98:173–7. doi: 10.1213/01.ANE.0000093224.77281.A5. [DOI] [PubMed] [Google Scholar]
- 49.Koppert W, Brueckl V, Weidner C, Schmelz M. Mechanically induced axon reflex and hyperalgesia in human UV-B burn are reduced by systemic lidocaine. Eur J Pain. 2004;8:237–44. doi: 10.1016/j.ejpain.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 50.Miller CC, Hale P, Pentland AP. Ultraviolet B injury increases prostaglandin synthesis through a tyrosine kinase-dependent pathway, Evidence for UVB-induced epidermal growth factor receptor activation. J Biol Chem. 1994;269:3529–33. [PubMed] [Google Scholar]
- 51.Bishop T, Hewson DW, Yip PK, Fahey MS, Dawbarn D, Young AR, et al. Characterisation of ultraviolet-B-induced inflammation as a model of hyperalgesia in the rat. Pain. 2007;131:70–82. doi: 10.1016/j.pain.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 52.Bishop T, Ballard A, Holmes H, Young AR, McMahon SB. Ultraviolet-B induced inflammation of human skin: Characterization and comparison with traditional models of hyperlagesia. Eur J Pain. 2009;13:524–32. doi: 10.1016/j.ejpain.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 53.Graven-Nielsen T, Arendt-Nielsen L, Mense S. Thremosensitivity of muscle: High-intensity thermal stimulation of muscle tissue induces muscle pain in humans. J Physiol. 2002;540:647–56. doi: 10.1113/jphysiol.2001.013336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sengupta JN, Gebhart GF. Physiology of the gastrointestinal tract. In: Johnson L, editor. Gastrointestinal afferent fibers and sensation. New York: Raven Press; 1994. pp. 484–519. [Google Scholar]
- 55.Villanova N, Azpiroz F, Malagelada JR. Perception and gut reflexes induced by stimulation of gastrointestinal thermoreceptors in humans. J Physiol. 1997;502:215–22. doi: 10.1111/j.1469-7793.1997.215bl.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brennum J, Arendt-Nielsen L, Secher NH, Jensen TS, Bjerring P. Quantitative sensory examination in human epidural anaesthesia and analgesia: Effects of lidocaine. Pain. 1992;51:27–34. doi: 10.1016/0304-3959(92)90005-V. [DOI] [PubMed] [Google Scholar]
- 57.Laursen RJ, Graven-Nielsen T, Jensen TS, Arendt-Nielsen L. Referred pain is dependent on sensory input from the periphery: A psychophysical study. Eur J Pain. 1997;1:261–9. doi: 10.1016/s1090-3801(97)90035-5. [DOI] [PubMed] [Google Scholar]
- 58.Laursen RJ, Graven-Nielsen T, Jensen TS, Arendt-Nielsen L. Quantification of local and referred pain in humans induced by intramuscular electrical stimulation. Eur J Pain. 1997;1:105–13. doi: 10.1016/s1090-3801(97)90068-9. [DOI] [PubMed] [Google Scholar]
- 59.Schulte H, Graven-Nielsen T, Sollevi A, Jansson Y, Arendt-Nielsen L, Segerdahl M. Pharmacological modulation of experimental phasic and tonic muscle pain by morphine, alfentanil and ketamine in healthy volunteers. Acta Anaesthesiol Scand. 2003;47:1020–30. doi: 10.1034/j.1399-6576.2003.00204.x. [DOI] [PubMed] [Google Scholar]
- 60.Graven-Nielsen T, Segerdahl M, Svensson P, Arendt-Nielsen L. Methods for induction and assessment of pain in humans with clinical and pharmacological examples. In: Kruger L, editor. Methods in pain research. Boca Raton FL: CRC Press; 2001. pp. 264–304. [Google Scholar]
- 61.Frobert O, Arendt-Nielsen L, Bak P, Andersen OK, Funch-Jensen P, Bagger JP. Electric stimulation of the esophageal mucosa.Perception and brain-evoked potentials. Scand J Gastroenterol. 1994;29:776–81. doi: 10.3109/00365529409092509. [DOI] [PubMed] [Google Scholar]
- 62.Andersen OK, Felsby S, Nicolaisen L, Bjerring P, Jensen TS, Arendt-Neilsen L. The effect of ketamine on stimulation of primary and secondary hyperalgesic areas induced by capsaicin - a double-blind, placebo-contolled, human experimental study. Pain. 1996;66:51–62. doi: 10.1016/0304-3959(96)02995-8. [DOI] [PubMed] [Google Scholar]
- 63.Wallace MS, Barger D, Schulteis G. The effect of chronic oral desipramine on capsaicin-induced allodynia and hyperalgesia: A double-blinden, placebo-controlled, crossover study. Anaesth Analg. 2002;95:973–8. doi: 10.1097/00000539-200210000-00034. [DOI] [PubMed] [Google Scholar]
- 64.Petersen KL, Maloney A, Hoke F, Dahl BJ, Rowbotham MC. A randomised study of the effect of oral lamitrigine and hydromorphone on pain and hyperalgesia following heat/capsaicin sensitization. J Pain. 2003;4:400–6. doi: 10.1016/s1526-5900(03)00718-1. [DOI] [PubMed] [Google Scholar]
- 65.Dirks J, Petersen KL, Rowbotham MC, Dahl JB. Gabapentin supresses cutaneous hyperalgesia following heat-capsaicin sensitization. Anesthesiology. 2002;97:102–7. doi: 10.1097/00000542-200207000-00015. [DOI] [PubMed] [Google Scholar]
- 66.Graven-Nielsen T, Arendt-Nielsen L, Svensson P, Jensen TS. Quantification of local and referred muscle pain in humans after sequential i.m. injections of hypertonic saline. Pain. 1997;69:111–7. doi: 10.1016/s0304-3959(96)03243-5. [DOI] [PubMed] [Google Scholar]
- 67.Cairns BE, Svensson P, Wang K, Castrillon E, Hupfeld S, Sessle BJ, et al. Ketamine attenuates glutamate-induced mechanical sensitization of the masseter muscle in human males. Exp Brain Res. 2006;169:467–72. doi: 10.1007/s00221-005-0158-z. [DOI] [PubMed] [Google Scholar]
- 68.Witting N, Svensson P, Gottrup H, Arendt-Nielsen L, Jensen TS. Intramuscular and Intradermal injection of capsaicin: A comparison of local and referred pain. Pain. 2000;84:407–12. doi: 10.1016/s0304-3959(99)00231-6. [DOI] [PubMed] [Google Scholar]
- 69.Korotkov A, Ljubisavljevic M, Thunberg J, Kataeva G, Roudas M, Pakhomov S, et al. Changes in human regional cerebral blood flow following hypertonic saline induced experimental muscle pain: A positron emission tomography study. Neurosci Lett. 2002;335:119–23. doi: 10.1016/s0304-3940(02)01181-3. [DOI] [PubMed] [Google Scholar]
- 70.Babenko V, Graven-Nielsen T, Svensson P, Drewes A, Jensen TS, Arendt-Nielsen L. Experimental human muscle pain induced by intramuscular injections of bradykinin, serotonin and substance P. Eur J Pain. 1999;3:93–102. doi: 10.1053/eujp.1998.0103. [DOI] [PubMed] [Google Scholar]
- 71.Mørk H, Ashina M, Bendtsen L, Olesen J, Jensen R. Experimental pain and tenderness following infusion of endogenous substances in humans. Eur J Pain. 2003;7:145–53. doi: 10.1016/S1090-3801(02)00096-4. [DOI] [PubMed] [Google Scholar]
- 72.Drewes AM, Schipper KP, Dimcevski G, Petersen P, Andersen OK, Gregersen H, et al. Multi-model induction and assessment of allodynia and hyperalgesia in the human oesophagus. Eur J Pain. 2003;7:539–49. doi: 10.1016/s1090-3801(03)00053-3. [DOI] [PubMed] [Google Scholar]
- 73.Louvel D, Delvaux M, Staumont G, Camman F, Fioramonti J, Bueno L. Intracolonic injection of glycerol: A model for abdominal pain in irritable bowel syndrome? Gastroenterology. 1996;110:351–61. doi: 10.1053/gast.1996.v110.pm8566580. [DOI] [PubMed] [Google Scholar]
- 74.Longhurst JC. Chemosensitive abdominal visceral afferent. In: Gebhart GF, editor. Visceral pain. Seattle WA: IASP Press; 1995. pp. 99–132. [Google Scholar]
- 75.Smith GM, Egbert LD, Markowitz RA, Mosteller F, Beecher HK. An experimental pain method sensitive to morphine in man: The submaximum effort tourniquet technique. J Pharmacol Exp Ther. 1966;154:324–32. [PubMed] [Google Scholar]
- 76.Armstrong R. Mechanisms of exercise-induced delayed onset muscle soreness: A brief review. Med Sci Sports Exerc. 1984;16:529–38. [PubMed] [Google Scholar]
- 77.Tegeder L, Zimmermann J, Meller ST, Geisslinger G. Release of algesic substances in human experimental muscle pain. Inflamm Res. 2002;51:393–402. doi: 10.1007/pl00000320. [DOI] [PubMed] [Google Scholar]
- 78.Cheung K, Hume P, Maxwell L. Delayed onset muscle soreness.Treatment strategies and performance factors. Sports Med. 2003;33:145–64. doi: 10.2165/00007256-200333020-00005. [DOI] [PubMed] [Google Scholar]
- 79.Mense S. The pathogenesis of muscle pain. Curr Pain Headache Rep. 2003;7:419–25. doi: 10.1007/s11916-003-0057-6. [DOI] [PubMed] [Google Scholar]
- 80.Barlas P, Walsh DM, Baxter GD, Allen JM. Delayed onset muscle soreness: Effect of an ischaemic block upon mechanical allodynia in humans. Pain. 2000;87:221–5. doi: 10.1016/S0304-3959(00)00287-6. [DOI] [PubMed] [Google Scholar]
- 81.Weerakkody NS, Whitehead NP, Canny BJ, Gregory JE, Proske U. Large-fiber mechanoreceptors contribute to muscle soreness after eccentric exercise. J Pain. 2001;2:209–19. doi: 10.1054/jpai.2001.22496. [DOI] [PubMed] [Google Scholar]
- 82.Weerakkody NS, Percival P, Hickey MW, Morgan DL, Gregory JE, Canny BJ, et al. Effects of local pressure and vibration on muscle pain from eccentric exercise and hypertonic saline. Pain. 2003;105:425–35. doi: 10.1016/S0304-3959(03)00257-4. [DOI] [PubMed] [Google Scholar]
- 83.Graven-Nielsen T, Arendt-Nielsen L. Induction and assessment of muscle pain, referred pain, and muscular hyperalgesia. Curr Pain Headache Rep. 2003;7:443–51. doi: 10.1007/s11916-003-0060-y. [DOI] [PubMed] [Google Scholar]
- 84.Taguchi T, Matsuda T, Tamura R, Sato J, Mizumura K. Muscular mechanical hyperalgesia revealed by behavioural pain test and c-Fos expression in the spinal dorsal horn after eccentric contraction in rats. J Physiol. 2005;564:259–68. doi: 10.1113/jphysiol.2004.079483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Trappe TA, White F, Lambet CP, Cesar D, Hellerstein M, Evans WJ. Effect of ibuprofen and acetaminophen on post-exercise muscle protein synthesis. Am J Physiol Endocrinol Metab. 2002;282:E551–6. doi: 10.1152/ajpendo.00352.2001. [DOI] [PubMed] [Google Scholar]
- 86.Trappe TA, Fluckey JD, White F, Lambert CP, Evans WJ. Skeletal muscle PGF(2)(alpha) and PGE(2) in response to eccentric resistance exercise: Influence of ibuprofen acetaminophen. J Clin Endocrinol Metab. 2001;86:5067–70. doi: 10.1210/jcem.86.10.7928. [DOI] [PubMed] [Google Scholar]
- 87.Tokmakidis SP, Kokkinidis EA, Smilios I, Douda H. The effects of ibuprofen on delayed muscle soreness and muscular performance after eccentric exercise. J Strength Cond Res. 2003;17:53–9. doi: 10.1519/1533-4287(2003)017<0053:teoiod>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 88.Kehl LJ, Fairbanks CA. Experimental animal models of muscle pain and analgesia. Exerc Sport Sci Rev. 2003;31:188–94. doi: 10.1097/00003677-200310000-00006. [DOI] [PubMed] [Google Scholar]
- 89.Rukwied R, Meyer A, Schley M, Kluschina O, Schmelz M. Nerve growth factor causes sustained nociceptor sensitization in human skin. Soc Neurosci Abstr. 2008;38:267–14. [Google Scholar]
- 90.Asghari A, Julaeiha S, Godarsi M. Disability and depression in patients with chronic pain: Pain or pain-related beliefs? Arch Iran Med. 2008;11:263–9. [PubMed] [Google Scholar]


