Abstract
Understanding the impact of place on health is a key element of epidemiologic investigation, and numerous tools are being employed for analysis of spatial health-related data. This review documents the huge growth in spatial epidemiology, summarizes the tools that have been employed, and provides in-depth discussion of several methods. Relevant research articles for 2000–2010 from seven epidemiology journals were included if the study utilized a spatial analysis method in primary analysis (n = 207). Results summarized frequency of spatial methods and substantive focus; graphs explored trends over time. The most common spatial methods were distance calculations, spatial aggregation, clustering, spatial smoothing and interpolation, and spatial regression. Proximity measures were predominant and were applied primarily to air quality and climate science and resource access studies. The review concludes by noting emerging areas that are likely to be important to future spatial analysis in public health.
Keywords: geographic information systems, epidemiologic methods, spatial distribution, geography, space-time clustering
INTRODUCTION
Place has long been recognized as an essential component in epidemiological science (118). Over the past 20 years, interest in place has experienced resurgence, facilitated by improved accessibility of computer-based geographic information systems (GIS). Personal computing, improvements in processing speed, and user-friendly applications have placed spatial analysis within reach of a large number of researchers (38, 86). In the late 1990s and early 2000s, at least three books (26, 35, 134) and a number of reviews (23, 36, 45, 87, 103, 105) were published on spatial methods in health research. These publications have advanced the application of spatial methods to public health data and likely contributed to the growth of the field.
This article reviews the past ten years of literature on spatial analysis methods from major epidemiology journals and assesses trends in the research; it discusses the methods applied and research areas that are emerging. Previous reviews covered the history of GIS and functional capabilities for health research (23), spatial analysis approaches, and tools, along with examples from public health research (23, 36, 45, 87, 103, 105). Most reviews discussed visualization or mapping and emphasized the importance of choice of spatial scale, the mismatch between the most relevant areas for disease risk and the data actually available, the modifiable area unit problem, ecologic fallacies, and incomplete data and measurement error. Given the breadth of previous reviews, the primary focus of this review is spatial analysis.
When examining place-based effects as determinants of risks and rates of diseases, epidemiologists have relied primarily on pre-existing discrete georeferenced data to specify exposures or outcomes; for example, census data are frequently utilized for area-level exposure. Although these studies are useful in their own right, their methods remain essentially aspatial. Many studies have examined characteristics that are spatially defined, and many incorporate multilevel data structures; yet most do not consider local relationships between spatially contiguous entities or incorporate spatial autocorrelation into statistical modeling. The interest of this review is not just in discrete spatial geographic units per se, but in the utilization of methods employing spatial aggregation, proximity, clustering, or spatial regression.
METHODS
Journal Selection
This article reviews literature from the seven English-language journals listed in Table 1. We selected journals targeted to epidemiologists, along with one leading public health journal frequently read and cited by epidemiologists (American Journal of Public Health). Because this review aims to inform trends in the general field of epidemiology, journals with a primary focus on spatial analysis/health geographics were not included. For example, Health & Place, International Journal of Health Geographics, Environmental Health Perspectives, and Environmental Research all emphasize geography but do not target epidemiology as their primary discipline and so were excluded. Journals that were not published for the full 2000–2011 period of the review were also excluded (Epidemiologic Perspectives and Innovation and Spatial and Spatio-Temporal Epidemiology), as were journals emphasizing reviews and commentaries (Annual Review of Public Health and Epidemiologic Reviews).
Table 1.
Articles published January 1, 2000 through February 28, 2011, in seven target journals and number (and percent) of articles that utilized a spatial analysis method (see search criteria in text)
| Journal name | Stage 1 All citations |
Stage 2 After applying broad search terms |
Stage 3 Selected for inclusion |
||
|---|---|---|---|---|---|
| N | N | % | N | % | |
| American Journal of Epidemiology | 3,239 | 1,225 | 38% | 52 | 2% |
| American Journal of Public Health | 3,442 | 1,293 | 38% | 30 | 1% |
| Annals of Epidemiology | 1,228 | 415 | 34% | 21 | 2% |
| Epidemiology | 1,177 | 419 | 36% | 44 | 4% |
| European Journal of Epidemiology | 1,290 | 570 | 44% | 11 | 1% |
| International Journal of Epidemiology | 1,466 | 712 | 49% | 15 | 1% |
|
Journal of Epidemiology and Community Health |
1,921 | 1,007 | 52% | 34 | 2% |
| Total | 13,763 | 5,641 | 41% | 207 | 1% |
Search Method
The literature review consisted of three stages (Table 1). In stage 1, all abstracts appearing between 1/1/2000–2/28/2011 were extracted from PubMed into a citation database. In stage 2, citations were limited to those that began with “spa,” “geo,” “neigh,” “area,” “dist,” “proxim,” “map,” “census,” or “place” anywhere in the citation. Approximately 40% of stage 1 citations met stage 2 criteria. Relevant articles lacked key word uniformity, necessitating manual review. In stage 3, articles utilizing a spatial analysis method were identified. Articles were excluded if spatial analysis (a) was a small subcomponent of the study [e.g., see Silhol et al. (116)]; or (b) was not described in the body of the full article [e.g., see Stark Casagrande et al. (120)]; or (c) if geographic data came from predefined discrete spatial data that were not spatially altered by the researchers and no explicitly spatial methods were used in the analysis of the article’s primary findings [for example of an article excluded, see Turrell et al. (130)]. Area-level studies using census data were not included unless the investigators employed a spatial analytic tool (for example, block group smoothing or calculation of distance statistics) or accounted for spatial autocorrelation in regression.
Abstraction Method
Stage 3 abstracts were reviewed and coded using a term list derived from the frequency of words in the abstracts (summative content analysis of words in the abstracts) and phrases based on expert knowledge of spatial methodology (directed content analysis) (55) (see Supplemental Table 1 for the list of topics. Follow the Supplemental Material link from the Annual Reviews home page at http://www.annualreviews.org). Each abstract received multiple spatial analysis codes and substantive codes. The results summarized the frequency of spatial methods classifications, and the graphs explore trends in classes over time.
SUBSTANTIVE TOPICS
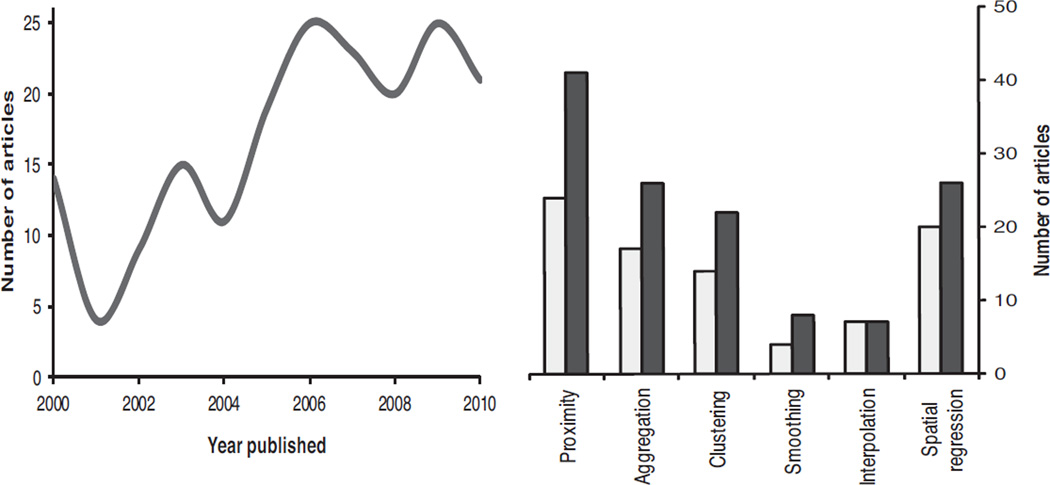
Table 1 shows the distribution of articles published by each journal and the proportion selected for the review. Approximately 14,000 articles were published in the 7 selected journals. Among these, 5,641 were reviewed manually for inclusion. One percent (n = 207) of articles utilized a spatial analysis method, and the proportion rose to 4% for articles published in Epidemiology. Selected for inclusion were 193 spatial methods citations (shown in Figures 1 and 2) plus 14 articles that address georeferencing issues (see Supplemental Table 2 for complete list of articles). Figure 1 illustrates the steep increase in the number of articles using spatial methods over the past 10 years. The most common spatial methods or spatial tools employed were calculations of distances (proximity calculation), estimation of summary measures across prespecified geographic areas (aggregation methods), tools used to assess various forms of clustering, spatial smoothing and interpolation methods, and spatial regression. The largest increase during the period examined was in proximity and cluster analyses methods.
Figure 1.
Number of articies using spatial methods, total by year and total for first part of decade and second part of decade (2000–2011).
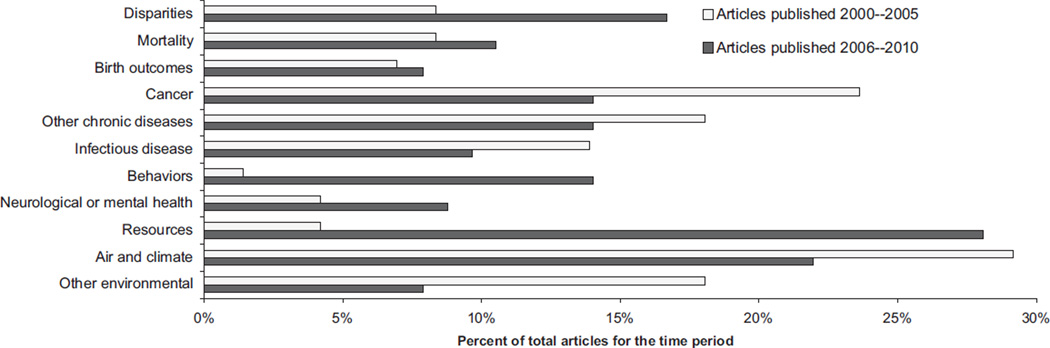
Figure 2.
Percent of total articles using spatial methods by substantive topic and publication during the first (2000–2005) and second parts of decade (2006–2010) “Resources” category includes health care, food and physical activity environments, facility location analyses etc.; “Other environmental” includes toxic waste, pesticides, electromagnetic fields, etc.
During the decade under review, some shifts occurred in substantive areas utilizing spatial methods. Cancer and air pollution epidemiology have long applied sophisticated spatial methods, and these fields continue to dominate the spatial literature (16, 49, 53, 58, 132). The declines evident in Figure 2 may have resulted from investigators who submitted their work to alternate journals. By contrast, from the first to second half of the decade, studies in resource availability rose fourfold (8% to 32%; Figure 2), spatial methods applied to disparities research more than doubled (6% to 17%), and studies of health-related behaviors increased the use of spatial methods. The spatial patterning of resources by race and/or socioeconomic status was a popular area of study; most studies focused on differential access to health care, to food or alcohol stores, and to health-promoting features of the built environments (8, 12, 60, 79, 88, 98, 117, 139). Spatial methods facilitate this work; however, estimating the contribution of local resources to health disparities requires cross-classification of resources within sociodemographic groups. Because of residential segregation, there is usually very little cross-classification; thus when adjusted for confounders, this work has found generally weak or nondetectable spatial effects for disparities in health conditions/outcomes (48, 76, 92).
Georeferencing
A number of articles focused on georeferencing (the procedure for assigning spatial coordinates by matching addresses to a reference map or “geocoding”). Of 14 georeferencing articles, most were concerned with positional accuracy and repeatability of geocoding procedures. Geocoding accuracy was generally insensitive to urbanized areas at a census tract resolution or larger. However, if accuracy of street address was critical, then geocoding method discrepancies became much larger (75, 112, 135). Several articles discussed novel ways to improve accuracy of geocodes by using telephone exchanges in combination with other address data (111, 133). The articles cautioned that spatial alignment of overlays (94) and the quality of the reference map (41, 140) have received insufficient attention. The articles caution that the ease of using GIS software masks complexities in geocoding and, thus, novice users need to be careful that they are applying best practices.
Spatial Methods
The most common spatial methods or spatial tools employed in the papers reviewed were calculations of distances (proximity calculation), estimation of summary measures across prespecified geographic areas (aggregation methods), assessment of various forms of clustering, spatial smoothing and interpolation methods, and spatial regression.
Spatial Proximity
Measuring distance between an index location (often a residence or workplace) and resources or adverse exposures is relatively simple, and the measurement is frequently used to estimate environmental exposure. In the reviewed articles, air pollution and climate researchers often calculate distance to the nearest major roadway [for example, Allen et al. (2, 54) and Houston et al. (2, 54)], and behavioral researchers assess proximity to resources such as fast-food restaurants and grocery stores (28, 139) (see Supplemental Table 1). The majority of studies incorporating proximity use simple straight line/Euclidean distances (n = 51, or 80% of proximity articles). Straight-line distance can be a poor proxy for estimating access if there are no direct roads or other means of traveling to a particular destination. For this reason, four articles use network street distance or another network path such as path distance to a park (84) or a pharmacy (137). When travel time is a strong impediment, proximity measures have adjusted distance for travel mode [e.g., walking or taking public transportation (125) or road speed limits, type of road surface, or topography (97)].
Aggregation Methods
Aggregating spatial features within a given area is another method frequently used to characterize exposure. Often, a simple summary total or a simple average is computed within a predefined buffer size or an administratively defined unit such as a census tract. Examples are simple summaries of vehicle counts to determine traffic exposure (10, 42, 134) and number of street intersections or other features of the built environment to assess environmental suitability for walking (18, 74, 76). Aggregation can be combined with proximity analysis via distance-weighted averaging such as kernel densities [used in nine of the reviewed studies (see examples in 29, 79, 89, 126)]. Kernel densities assign greater weight to nearby features and thus are often used in resource access studies (10, 134).
A challenge in using aggregation is accounting for variability in the underlying population distribution. For example, when studying resource availability, it may be important to account for population density if the presence of a larger population implies more competition for resources; two approaches can address this. First, the buffer size can vary depending on population density [referred to as adaptive buffers, which are utilized in several studies (12, 21)]. Second, researchers can use a fixed buffer size, with densities weighted by population. For an example of the latter, one article uses kernel densities for physical activity resources weighted by population density (29) because facilities are a fixed quantity (e.g., a gym with 10 treadmills); thus, when demand is high and the resource is in use it is no longer available.
Although buffer size aggregation is a relatively simple tool, complexities can arise. For example, correction factors need to be applied when deriving buffers for partially measured regions (29). In addition, there is often little prior knowledge regarding the relevant buffer size thus necessitating extensive sensitivity analysis for alternate buffer sizes (29, 37).
Cluster Detection Techniques
Used in 36 studies, spatial cluster methods are the most common tool for assessing nonrandom spatial patterns. Many statistical methods have been developed to determine if disease clusters are of sufficient geographic size and concentration to have not occurred by chance (65, 69). Global clustering tests evaluate without pinpointing the specific locations of clusters, whereas local clustering tests specific small-scale clusters and focused clustering assesses clustering around a prefixed point source such as a nuclear installation. These tests have different substantive interpretations and detection methods; the presence of one does not imply the presence of the other (57). Overall, in this literature a total of 35 studies use spatial cluster detection methods. Such methods have had to overcome limitations to statistical power, including the availability of few cases, high variability in the background population density, multiple testing, and size and shape of cluster windows.
Twelve studies tested for global clustering to determine the existence of clustering in a study area without pinpointing specific locations. Tests most frequently used in the selected literature are Diggle and Chetwynd’s bivariate K-function (9, 13, 31), Mantel-Bailar’s test (27), and the Potthoff-Whittinghill method (PW) (1, 63, 85, 100, 109). Global tests used less frequently in this literature are Moran’s I statistic (91), and Cuzick and Edwards’s nearest neighbors and Tango’s maximized excess events tests (MEET) (68, 124). Tango’s MEET generally has the best statistical power, adjusts for multiple testing, and has the added value of being able to evaluate spatial autocorrelation and spatial heterogeneity (119).
Local cluster detection, also called hot spot analysis, can be assessed using Anselin’s local indicator of spatial association (LISA) (4, 47) and the Besag-Newell test (14, 96). Kulldorff’s spatial scan statistic tends to be the preferred local cluster detection method because it can adjust for multiple testing and heterogeneous background population densities, along with other confounding variables, is applicable to both point and aggregated data, and has been adapted to detect noncircular clusters (67, 70, 71). Implemented in SaTScan, the spatial scan statistic is the most common cluster detection method used in the studies identified in this review (at least 11 studies), including a recent extension for cluster detection of survival data (48, 58). Finally, Diggle’s test (30) and Stone’s conditional test (122) evaluate focal clustering and determine whether risk declines from prespecified point sources (85, 96).
Although most investigations of disease clusters are purely spatial in nature, a number of studies explore space-time clustering of cancer and infectious diseases. Seven studies apply a global space-time Knox technique (49, 53, 64, 80–82, 101, 128) and two studies apply Diggle’s global space-time K-function (32, 53, 82). The K-function is a preferred method because it corrects for edge effects and allows for a range of spatial and temporal scales. Kuldorff’s spatial scan was extended for local space-time clustering and was employed to investigate space-time of clustering of childhood mortality in rural Burkina Faso (108) and for sentinel cluster detection of influenza outbreaks in urban areas in southern Japan (95). Other space-time cluster detection tests include the dynamic continuous-area space-time (DYCAST) system, which was used to identify and prospectively monitor high-risk areas for West Nile virus (128); generalized Bayesian maximum entropy (GBME), which is useful when there is considerable data uncertainty (138); and spatial velocity techniques, used to explore the speed of epidemic waves in long-term temporal data such as influenza (24).
Spatial Interpolation and Smoothing Methods
Interpolation and smoothing methods are utilized by epidemiologists in many contexts to improve estimation. Applied to spatial epidemiology, these tools can be used to derive a spatial surface from sampled data points (filling in where data are unobserved) or to smooth across polygons (aggregate data) to create more robust estimates (87). Both approaches use nearby observations or spatially contiguous entities to fill in or otherwise improve spatial estimation.
Spatial interpolation methods include fitting spatial coordinates as penalized splines (8, 131) and as weighted averages for local populations (115). Both methods have low computational requirements and are advantageous when the large-scale trend is strong. Penalized thin-plate splines have the added advantage of being distribution-free and are thereby useful when spatial continuity is complex and prone to mis-specification. Local interpolation methods are preferred in the presence of a sufficient number of observations and small-scale spatial variability. Kriging is one such local interpolation procedure that uses a weighted linear combination of nearby observations to obtain an exact best linear unbiased predictor (46, 59). Four articles used model-based geostatistical kriging to predict disease rates at unmeasured locations and/or produce smoothed rates (43, 44, 99, 107).
Smoothing methods are used frequently to improve the accuracy of death or disease rates for small areas with few observations. However, most smoothing has been aspatial even when applied to geographic data. For example, empirical Bayes estimation has been used to weight small area estimates that have high random variation toward an observed global average derived from all areas. Most public health researchers have weighted toward the global average, which is potentially problematic because it can oversmooth the data and remove informative local variability. Spatial empirical Bayes estimation incorporates information from local, spatially contiguous areas; it goes beyond simply utilizing the overall global mean. Five studies included in this review derive estimates using spatial empirical Bayes; examples include smoothing estimates of deaths due to stomach cancer and stroke across 54 counties in England and Wales (77) and cryptosporidiosis incidence across 163 statistical local areas in Brisbane, Australia, during an 8-year period (56).
Multivariable Spatial Regression
Standard statistical regression models, which assume independence of the observations, are not appropriate for analyzing spatially dependent data (10). Spatial modeling requires iterative assessment of the strength of spatial autocorrelation in raw and adjusted data. If data are spatially autocorrelated and covariate information does not fully account for that pattern, then incorporating spatial dependencies into the modeling is likely a necessity. Although differences between spatial and aspatial models can be sizable (20, 21), there may be low sensitivity to the choice of spatial model. For example, among the reviewed articles, a number of studies evaluate sensitivity to various spatial regression approaches and find negligible differences (8, 15, 102). Nevertheless, notable differences among spatial regression models include their computational complexity, their ability to capture spatial heterogeneity, and their ability to quantify the uncertainty associated with parameter estimates.
Spatial regression, both frequentist and Bayesian, was used in 45 studies to address spatial autocorrelation and/or spatial heterogeneity. This review does not provide details on these complex methods, and the reader is advised to consult standard references for the field (3, 35, 72, 134).
Spatial autoregressive models
Simultaneous autoregressive (SAR) models are frequentist approaches designed to address spatial autocorrelation. They incorporate spatial autocorrelation using neighborhood matrices that specify relationships between neighboring data points. The form of the SAR model depends on whether the spatial autocorrelation processes are thought to derive from omitted variables (motivating a spatially lagged error term) or from the dependent variable (motivating a spatially lagged term for the dependent variable); a mixed SAR model assumes both processes (3). SAR models are commonly used in spatial econometrics, and only three reviewed articles use SAR models (8, 37, 50). A more recently developed SAR local regression technique, geographically weighted regression (GWR) (17, 40), explicitly allows for heterogeneity in the relation between predictor and response variables over space; thus, it can be used to diagnose spatial heterogeneity. Using this tool, one study identified considerable heterogenity in local effect estimates predicting childhood obesity. The study identifies microarea factors that are likely to be most important for preventing childhood obesity, thus this tool can be used to design appropriate microarea interventions (34).
Bayesian regression models
Bayesian regression models provide an alternative to SAR models. One of these models, the Besag York and Molliè (BYM) model, can be used to estimate the effects of potential risk factors related to a disease by including fixed covariates along with the random effects. At least 11 reviewed articles employ the BYM model to estimate local regression coefficients of covariates at the aggregated level (15, 33, 52, 61, 62, 66, 102, 106, 114, 123, 129). Although most of the reviewed articles model a single disease, at least four articles use the BYM model with shared component models or multivariate CAR models for joint spatial modeling of bivariate and multivariate diseases with common risk factors (39, 51, 78, 127). Shared component models were employed to investigate the similarities of the spatial patterns of childhood acute lymphoblastic leukemia and diabetes mellitus type 1 in the United Kingdom (39), incidence of ischemic stroke and acute myocardial infarction in Finland (51), and spatial-temporal similarities of childhood leukemia and diabetes in the United Kingdom (78). In addition, two reviewed articles extend the spatial BYM model for spatial-temporal analysis (63, 113). At least six articles also apply Bayesian geostatistical models for spatial regression of point-referenced data where the spatial correlation random effects are modeled using a multivariate normal distribution, with the covariance matrix defined as a function of the distance between locations (19–21, 43, 110). For example, Chaix and colleagues use Bayesian geostatistical logistics to study neighborhood effects on health care utilization (20) in France and mental disorders in Malmo, Sweden (21).
Spatial regression has been adapted to many complex data structures and methodologies, including Bayesian maximum entropy methods for spatiotemporal analysis (138) and spatial classification and regression tree models (56). However, there are simple methods to incorporate spatial parameters that may be suitable for many research questions and data types. Sometimes referred to as trend surface modeling, coordinates can be entered as polynomials (22) or flexibly modeled using smoothed terms [e.g., LOESS (136)], or a deterministic distribution-free approach can be implemented using thin-plate splines (8, 121). Spatially implicit modeling is another approach that can be applied on its own or in tandem with spatial covariance modeling. At its most basic, a spatially implicit model includes spatially distributed predictors and assumes their sufficiency to account for the spatial autocorrelation in model residuals. At least 11 reviewed studies rely on this technique for some stage of their analyses (see examples in 16, 93, 104). Spatially colocated covariate data, required for this approach, can be critical to any modeling effort. Covariate data can stabilize nonstationarity in the mean, and importantly, examining spatial variation before and after adjustment for covariates can identify which factors determine—at least in part—the observed spatial patterns (6, 8). Whereas detection of spatial patterns can lead us to closer investigation of the underlying phenomenon, covariate data are needed for real insight into which factors are driving observable patterns.
SUMMARY
The past ten years saw a steep growth in the use of spatial methods in the scientific literature, and much of the growth was in spatial applications to resource availability and disparities research. Overall, proximity measures were the predominant spatial method. Other frequently utilized methods were tools to aggregate spatial data, with spatial smoothing and interpolation methods employed less frequently. Use of cluster detection tools continues to expand, and local clustering methods and public health studies that incorporate space-time clustering and spatial regression have been growing increasingly sophisticated.
Despite recent growth, viewed as a percent of all articles published in major epidemiology journals, use of any spatial method was small (1%, as defined by this review). This may be explained by several factors: (a) Research questions that involve spatial relationships have remained a minority in the discipline; (b) expertise in spatial methods tends to lie in the disciplines of geography and statistics, thus necessitating interdisciplinary collaboration; and (c) spatial epidemiologists can publish their work in many excellent journals not including the seven journals selected for this review. The seven selected journals are well read and well cited by epidemiologists and are able to illustrate trends in the discipline. A review of all public health journals was beyond the scope of this article. Researchers applying spatial methods are advised to consult comprehensive texts (5, 10, 25, 35, 69, 83, 134) because this review was also not intended as a definitive review of best practices, although clearly many best practices have been employed. Rather, the review was intended to summarize the most prevalent methods and substantive applications and to set the stage for discussing where the field may be headed.
FUTURE DIRECTIONS
Employing Spatial Methods to Understand Better How Place-Based Features Affect Health
This review excluded numerous studies that did not execute a spatial analysis—defined as calculating a spatial metric, examining local relationships between spatially contiguous entities, or utilizing a spatial statistic—even though the study investigated spatial exposures or outcomes. Despite an exponential growth of interest in place, most research in public health, with few exceptions, remains aspatial (20). Even among articles included in the review, spatial interpolation or smoothing methods to estimate geographically varying exposures (8) and the use of spatial regression alone or in combination with multilevel models (21, 123) have been underutilized. These techniques should be applied more widely because they are likely to improve specificity of exposure and disease relationships, reduce measurement error, and deepen our understanding of the relationships between place and health.
Integration of Spatial Methods, Digital Media, and Social Networks to Enable Space-Time Research
Reviews have noted the need for more space-time health-related research, as well as a lack of data to support these investigations (83). A significant boost to availability of data has come from the ubiquity of GPS receivers, including wearable GPS devices and cellular phones. These devices facilitate active and passive data gathering to support space-time research. In addition, location-stamped social network Web communications (from Web sites such as Foursquare and Facebook Places) continue to grow in popularity, and these data sources have not yet been utilized in spatial epidemiology. In general, the integration of spatial epidemiology with social network analyses has been underexplored. Only two papers reviewed here examined the joint effects of social and geographic networks on disease or utilized GPS devices in the research (11, 90). Integration of spatially referenced data and social network methods into spatial epidemiology presents methodological challenges (73), and results can be difficult to interpret (11). However, assuming that progress is made to address those challenges, this area will likely be of growing interest to public health researchers.
Spatial Simulation
Interest is increasing in the use of simulation models to better understand and capture the bidirectional relationships between people and places over time (7). Simulation models can be used to create synthetic populations in space and can include individuals who interact with each other in spatially constrained ways that are in turn affected by spatially patterned environments. Computer modeling can be used to program space-time interactions in response to spatial dimensions and environmental features. One of the reviewed articles illustrates this potential: Investigators derived a synthetic population with microarea data and then used geographically weighted regression to suggest how antiobesity policies could be tailored to the specific needs of each microarea (34). A number of challenges and limitations exist for merging spatial methods and simulation frameworks (7). Nevertheless, we anticipate that, increasingly, these two broad methodologies will work in tandem to yield additional insights into the spatial determinants of health and the interventions that may be most useful.
CONCLUSION
To our knowledge, this article is the first review to derive an inventory of spatial epidemiology during the past decade, to document huge growth in this field systematically, and to summarize the tools that have been employed. Space and place have been key dimensions of epidemiology and public health for decades, yet advanced spatial methods have been relatively slow to trickle into epidemiology, likely owing to disciplinary focus and training. Today there are many rich tools to employ for a more sophisticated treatment of space and to understand better the interacting contributions to health of individual characteristics and spatially varying place-based factors. Such factors are potentially amenable to policy and thus have particular importance to public health. Increased use of spatial methods is likely to continue, in tandem with interest in the relationship between place and health, as spatial software tools become more accessible and geographically referenced data become more available.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the National Heart, Lung, and Blood Institute R01HL071759 and National Institute on Minority Health and Health Disparities P60MD002249. The authors thank Dan Figueras for his assistance in compiling the literature and Charlotte Gerzak for her editing work.
Footnotes
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- 1.Abdullah NA, Pearce MS, Parker L, Wilkinson JR, McNally RJ. Evidence of an environmental contribution to the aetiology of cryptorchidism and hypospadias? Eur. J. Epidemiol. 2007;22:615–620. doi: 10.1007/s10654-007-9160-z. [DOI] [PubMed] [Google Scholar]
- 2.Allen RW, Criqui MH, Diez Roux AV, Allison M, Shea S, et al. Fine particulate matter air pollution, proximity to traffic, and aortic atherosclerosis. Epidemiology. 2009;20:254–264. doi: 10.1097/EDE.0b013e31819644cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anselin L. Spatial Econometrics: Methods and Models. Dordrecht: Kluwer Acad; 1988. [Google Scholar]
- 4.Anselin L. Local Indicators of Spatial Association—LISA. Geogr. Anal. 1995;27:93–115. [Google Scholar]
- 5.Anselin L. Under the hood—issues in the specification and interpretation of spatial regression models. Agric. Econ. 2002;27:247–267. [Google Scholar]
- 6.Anselin L. Spatial externalities, spatial multipliers, and spatial econometrics. Int. Reg. Sci. Rev. 2003;26:153–166. [Google Scholar]
- 7.Auchincloss AH, Diez Roux AV. A new tool for epidemiology: the usefulness of dynamic-agent models in understanding place effects on health. Am. J. Epidemiol. 2008;168:1–8. doi: 10.1093/aje/kwn118. [DOI] [PubMed] [Google Scholar]
- 8.Auchincloss AH, Diez Roux AV, Brown DG, Raghunathan TE, Erdmann CA. Filling the gaps: spatial interpolation of residential survey data in the estimation of neighborhood characteristics. Epidemiology. 2007;18:469–478. doi: 10.1097/EDE.0b013e3180646320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Austin SB, Melly SJ, Sanchez BN, Patel A, Buka S, Gortmaker SL. Clustering of fast-food restaurants around schools: a novel application of spatial statistics to the study of food environments. Am. J. Public Health. 2005;95:1575–1581. doi: 10.2105/AJPH.2004.056341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bailey TC, Gatrell AC. Interactive Spatial Data Analysis. Hoboken, NJ: Wiley; 1995. [DOI] [PubMed] [Google Scholar]
- 11.Bates SJ, Trostle J, Cevallos WT, Hubbard A, Eisenberg JN. Relating diarrheal disease to social networks and the geographic configuration of communities in rural Ecuador. Am. J. Epidemiol. 2007;166:1088–1095. doi: 10.1093/aje/kwm184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berke EM, Tanski SE, Demidenko E, Alford-Teaster J, Shi X, Sargent JD. Alcohol retail density and demographic predictors of health disparities: a geographic analysis. Am. J. Public Health. 2010;100:1967–1971. doi: 10.2105/AJPH.2009.170464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bernstein KT, Curriero FC, Jennings JM, Olthoff G, Erbelding EJ, Zenilman J. Defining core gonorrhea transmission utilizing spatial data. Am. J. Epidemiol. 2004;160:51–58. doi: 10.1093/aje/kwh178. [DOI] [PubMed] [Google Scholar]
- 14.Besag J, Newell J. The detection of clusters in rare diseases. J. R. Stat. Soc. Ser. Stat. Soc. 1991;154:143–155. [Google Scholar]
- 15.Boyd HA, Flanders WD, Addiss DG, Waller LA. Residual spatial correlation between geographically referenced observations: a Bayesian hierarchical modeling approach. Epidemiology. 2005;16:532–541. doi: 10.1097/01.ede.0000164558.73773.9c. [DOI] [PubMed] [Google Scholar]
- 16.Brauer M, Hoek G, van Vliet P, Meliefste K, Fischer P, et al. Estimating long-term average particulate air pollution concentrations: application of traffic indicators and geographic information systems. Epidemiology. 2003;14:228–239. doi: 10.1097/01.EDE.0000041910.49046.9B. [DOI] [PubMed] [Google Scholar]
- 17.Brunsdon C, Fotheringham AS, Charlton ME. Geographically weighted regression: a method for exploring spatial nonstationarity. Geogr. Anal. 1996;28:281–298. [Google Scholar]
- 18.Cervero R, Duncan M. Walking, bicycling, and urban landscapes: evidence from the San Francisco Bay Area. Am. J. Public Health. 2003;93:1478–1483. doi: 10.2105/ajph.93.9.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaix B, Leyland AH, Sabel CE, Chauvin P, Rastam L, et al. Spatial clustering of mental disorders and associated characteristics of the neighbourhood context in Malmo, Sweden, in 2001. J. Epidemiol. Community Health. 2006;60:427–435. doi: 10.1136/jech.2005.040360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaix B, Merlo J, Chauvin P. Comparison of a spatial approach with the multilevel approach for investigating place effects on health: the example of healthcare utilisation in France. J. Epidemiol. Community Health. 2005;59:517–526. doi: 10.1136/jech.2004.025478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chaix B, Merlo J, Subramanian SV, Lynch J, Chauvin P. Comparison of a spatial perspective with the multilevel analytical approach in neighborhood studies: the case of mental and behavioral disorders due to psychoactive substance use in Malmo, Sweden, 2001. Am. J. Epidemiol. 2005;162:171–182. doi: 10.1093/aje/kwi175. [DOI] [PubMed] [Google Scholar]
- 22.Che D, Decludt B, Campese C, Desenclos JC. Sporadic cases of community acquired legionnaires’ disease: an ecological study to identify new sources of contamination. J. Epidemiol. Community Health. 2003;57:466–469. doi: 10.1136/jech.57.6.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clarke KC, McLafferty SL, Tempalski BJ. On epidemiology and geographic information systems: a review and discussion of future directions. Emerg. Infect. Dis. 1996;2:85–92. doi: 10.3201/eid0202.960202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cliff AD, Haggett P, Smallman-Raynor M. An exploratory method for estimating the changing speed of epidemic waves from historical data. Int. J. Epidemiol. 2008;37:106–112. doi: 10.1093/ije/dym240. [DOI] [PubMed] [Google Scholar]
- 25.Cressie NAC. Statistics for Spatial Data. xx. New York: Wiley; 1993. p. 900. [Google Scholar]
- 26.Cromley EK, McLafferty SL. GIS and Public Health. New York: Guilford; 2002. [Google Scholar]
- 27.D’Aignaux JH, Cousens SN, Delasnerie-Laupretre N, Brandel JP, Salomon D, et al. Analysis of the geographical distribution of sporadic Creutzfeldt-Jakob disease in France between 1992 and 1998. Int. J. Epidemiol. 2002;31:490–495. [PubMed] [Google Scholar]
- 28.Davis B, Carpenter C. Proximity of fast-food restaurants to schools and adolescent obesity. Am. J. Public Health. 2009;99:505–510. doi: 10.2105/AJPH.2008.137638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diez Roux AV, Evenson KR, McGinn AP, Brown DG, Moore L, et al. Availability of recreational resources and physical activity in adults. Am. J. Public Health. 2007;97:493–499. doi: 10.2105/AJPH.2006.087734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diggle PJ. A point process modeling approach to raised incidence of a rare phenomenon in the vicinity of a prespecified point. J. R. Stat. Soc. Ser. Stat. Soc. 1990;153:349–362. [Google Scholar]
- 31.Diggle PJ, Chetwynd AG. Second-order analysis of spatial clustering for inhomogeneous populations. Biometrics. 1991;47:1155–1163. [PubMed] [Google Scholar]
- 32.Diggle PJ, Chetwynd AG, Haggkvist R, Morris SE. Second-order analysis of space-time clustering. Stat. Methods Med. Res. 1995;4:124–136. doi: 10.1177/096228029500400203. [DOI] [PubMed] [Google Scholar]
- 33.Dominguez-Berjon MF, Gandarillas A, Segura del Pozo J, Zorrilla B, Soto MJ, et al. Census tract socioeconomic and physical environment and cardiovascular mortality in the region of Madrid (Spain) J. Epidemiol. Community Health. 2010;64:1086–1093. doi: 10.1136/jech.2008.085621. [DOI] [PubMed] [Google Scholar]
- 34.Edwards KL, Clarke GP, Ransley JK, Cade J. The neighbourhood matters: studying exposures relevant to childhood obesity and the policy implications in Leeds, UK. J. Epidemiol. Community Health. 2010;64:194–201. doi: 10.1136/jech.2009.088906. [DOI] [PubMed] [Google Scholar]
- 35.Elliott P, Wakefield JC, Best NG, Briggs DJ, editors. Spatial Epidemiology: Methods and Applications. Oxford: Oxford Univ. Press; 2000. [Google Scholar]
- 36.Elliott P, Wartenberg D. Spatial epidemiology: current approaches and future challenges. Environ. Health Perspect. 2004;112:998–1006. doi: 10.1289/ehp.6735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Emch M, Ali M, Park JK, Yunus M, Sack DA, Clemens JD. Relationship between neighbourhood-level killed oral cholera vaccine coverage and protective efficacy: evidence for herd immunity. Int. J. Epidemiol. 2006;35:1044–1050. doi: 10.1093/ije/dyl100. [DOI] [PubMed] [Google Scholar]
- 38.Environ. Syst. Res. Inst. (ESRI) ArcGIS Desktop: Release 8. Redlands, CA: ESRI; 2000. [Google Scholar]
- 39.Feltbower RG, Manda SO, Gilthorpe MS, Greaves MF, Parslow RC, et al. Detecting small-area similarities in the epidemiology of childhood acute lymphoblastic leukemia and diabetes mellitus, type 1: a Bayesian approach. Am. J. Epidemiol. 2005;161:1168–1180. doi: 10.1093/aje/kwi146. [DOI] [PubMed] [Google Scholar]
- 40.Fotheringham AS, Charlton ME, Brunsdon C. Geographically weighted regression: a natural evolution of the expansion method for spatial data analysis. Environ. Plann. A. 1998;30:1905–1927. [Google Scholar]
- 41.Frizzelle BG, Evenson KR, Rodriguez DA, Laraia BA. The importance of accurate road data for spatial applications in public health: customizing a road network. Int. J. Health Geogr. 2009;8:24. doi: 10.1186/1476-072X-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gauderman WJ, Avol E, Lurmann F, Kuenzli N, Gilliland F, et al. Childhood asthma and exposure to traffic and nitrogen dioxide. Epidemiology. 2005;16:737–743. doi: 10.1097/01.ede.0000181308.51440.75. [DOI] [PubMed] [Google Scholar]
- 43.Gemperli A, Vounatsou P, Kleinschmidt I, Bagayoko M, Lengeler C, Smith T. Spatial patterns of infant mortality in Mali: the effect of malaria endemicity. Am. J. Epidemiol. 2004;159:64–72. doi: 10.1093/aje/kwh001. [DOI] [PubMed] [Google Scholar]
- 44.Gesink Law DC, Bernstein KT, Serre ML, Schumacher CM, Leone PA, et al. Modeling a syphilis outbreak through space and time using the Bayesian maximum entropy approach. Ann. Epidemiol. 2006;16:797–804. doi: 10.1016/j.annepidem.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 45.Glass GE. Update: spatial aspects of epidemiology: the interface with medical geography. Epidemiol. Rev. 2000;22:136–139. doi: 10.1093/oxfordjournals.epirev.a018010. [DOI] [PubMed] [Google Scholar]
- 46.Goovaerts P. Geostatistics for Natural Resources Evaluation. Oxford: Oxford Univ. Press; 1997. [Google Scholar]
- 47.Greene SK, Ionides EL, Wilson ML. Patterns of influenza-associated mortality among US elderly by geographic region and virus subtype, 1968–1998. Am. J. Epidemiol. 2006;163:316–326. doi: 10.1093/aje/kwj040. [DOI] [PubMed] [Google Scholar]
- 48.Gregorio DI, Huang L, DeChello LM, Samociuk H, Kulldorff M. Place of residence effect on likelihood of surviving prostate cancer. Ann. Epidemiol. 2007;17:520–524. doi: 10.1016/j.annepidem.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 49.Gustafsson B, Carstensen J. Space-time clustering of childhood lymphatic leukaemias and non-Hodgkin’s lymphomas in Sweden. Eur. J. Epidemiol. 2000;16:1111–1116. doi: 10.1023/a:1010953713048. [DOI] [PubMed] [Google Scholar]
- 50.Havard S, Deguen S, Zmirou-Navier D, Schillinger C, Bard D. Traffic-related air pollution and socioeconomic status: a spatial autocorrelation study to assess environmental equity on a small-area scale. Epidemiology. 2009;20:223–230. doi: 10.1097/EDE.0b013e31819464e1. [DOI] [PubMed] [Google Scholar]
- 51.Havulinna AS, Paakkonen R, Karvonen M, Salomaa V. Geographic patterns of incidence of ischemic stroke and acute myocardial infarction in Finland during 1991–2003. Ann. Epidemiol. 2008;18:206–213. doi: 10.1016/j.annepidem.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 52.Hickson DA, Waller LA, Gebreab SY, Wyatt SB, Kelly J, et al. Geographic representation of the Jackson Heart Study cohort to the African-American population in Jackson, Mississippi. Am. J. Epidemiol. 2011;173:110–117. doi: 10.1093/aje/kwq317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Houben MP, Coebergh JW, Birch JM, Tijssen CC, van Duijn CM, McNally RJ. Space-time clustering of glioma cannot be attributed to specific histological subgroups. Eur. J. Epidemiol. 2006;21:197–201. doi: 10.1007/s10654-006-0003-0. [DOI] [PubMed] [Google Scholar]
- 54.Houston D, Ong P, Wu J, Winer A. Proximity of licensed child care facilities to near-roadway vehicle pollution. Am. J. Public Health. 2006;96:1611–1617. doi: 10.2105/AJPH.2005.077727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual. Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 56.Hu W, Mengersen K, Tong S. Spatial analysis of notified cryptosporidiosis infections in Brisbane, Australia. Ann. Epidemiol. 2009;19:900–907. doi: 10.1016/j.annepidem.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 57.Huang L, Pickle LW, Das B. Evaluating spatial methods for investigating global clustering and cluster detection of cancer cases. Stat. Med. 2008;27:5111–5142. doi: 10.1002/sim.3342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang L, Pickle LW, Stinchcomb D, Feuer EJ. Detection of spatial clusters: application to cancer survival as a continuous outcome. Epidemiology. 2007;18:73–87. doi: 10.1097/01.ede.0000249994.30736.24. [DOI] [PubMed] [Google Scholar]
- 59.Isaaks EH, Srivastava RM. An Introduction to Applied Geostatistics. New York: Oxford Univ. Press; 1989. [Google Scholar]
- 60.Kamphuis CB, Giskes K, Kavanagh AM, Thornton LE, Thomas LR, et al. Area variation in recreational cycling in Melbourne: a compositional or contextual effect? J. Epidemiol. Community Health. 2008;62:890–898. doi: 10.1136/jech.2007.067116. [DOI] [PubMed] [Google Scholar]
- 61.Kazembe LN, Namangale JJ. A Bayesian multinomial model to analyse spatial patterns of childhood co-morbidity in Malawi. Eur. J. Epidemiol. 2007;22:545–556. doi: 10.1007/s10654-007-9145-y. [DOI] [PubMed] [Google Scholar]
- 62.Kleinschmidt I, Sharp B, Mueller I, Vounatsou P. Rise in malaria incidence rates in South Africa: a small-area spatial analysis of variation in time trends. Am. J. Epidemiol. 2002;155:257–264. doi: 10.1093/aje/155.3.257. [DOI] [PubMed] [Google Scholar]
- 63.Kleinschmidt I, Sharp BL, Clarke GP, Curtis B, Fraser C. Use of generalized linear mixed models in the spatial analysis of small-area malaria incidence rates in Kwazulu Natal, South Africa. Am. J. Epidemiol. 2001;153:1213–1221. doi: 10.1093/aje/153.12.1213. [DOI] [PubMed] [Google Scholar]
- 64.Knox EG, Bartlett MS. The detection of space-time interactions. J. R. Stat. Soc. Ser. C (Appl. Stat.) 1964;13:25–30. [Google Scholar]
- 65.Knox G. Detection of clusters. In: Elliott P, editor. Methodology of Enquires Into Disease Clustering. London: Small Area Health Stat. Unit; 1989. pp. 17–22. [Google Scholar]
- 66.Kousa A, Moltchanova E, Viik-Kajander M, Rytkonen M, Tuomilehto J, et al. Geochemistry of ground water and the incidence of acute myocardial infarction in Finland. J. Epidemiol. Community Health. 2004;58:136–139. doi: 10.1136/jech.58.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kulldorff M. A spatial scan statistic. Commun. Stat. Part A Theory Methods. 1997;26:1481–1496. [Google Scholar]
- 68.Kulldorff M. Prospective time periodic geographical disease surveillance using a scan statistic. J. R. Stat. Soc. Ser. Stat. Soc. 2001;164:61–72. [Google Scholar]
- 69.Kulldorff M. Tests of spatial randomness adjusted for an inhomogeneity: a general framework. J. Am. Stat. Assoc. 2006;101:1289–1305. [Google Scholar]
- 70.Kulldorff M, Huang L, Pickle L, Duczmal L. An elliptic spatial scan statistic. Stat. Med. 2006;25:3929–3943. doi: 10.1002/sim.2490. [DOI] [PubMed] [Google Scholar]
- 71.Kulldorff M, Song C, Gregorio D, Samociuk H, DeChello L. Review—Cancer map patterns: Are they random or not? Am. J. Prev. Med. 2006;30:S37–S49. doi: 10.1016/j.amepre.2005.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lawson AB, Biggeri A, Boehning D, Lesaffre E, Viel J-F, Bertollini R. Disease Mapping and Risk Assessment for Public Health. New York: Wiley; 1999. [Google Scholar]
- 73.Lerman K. Harvesting geospatial knowledge from online social networks; Presented at Spatio-Temporal Constraints on Social Networks Workshop, Cent. Spat. Stud., Univ. Calif.; Santa Barbara. 2010. http://www.ncgia.ucsb.edu/projects/spatio-temporal/docs/Lerman-position.pdf. [Google Scholar]
- 74.Li F, Fisher KJ, Brownson RC, Bosworth M. Multilevel modelling of built environment characteristics related to neighbourhood walking activity in older adults. J. Epidemiol. Community Health. 2005;59:558–564. doi: 10.1136/jech.2004.028399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liese AD, Colabianchi N, Lamichhane AP, Barnes TL, Hibbert JD, et al. Validation of 3 food outlet databases: completeness and geospatial accuracy in rural and urban food environments. Am. J. Epidemiol. 2010;172:1324–1333. doi: 10.1093/aje/kwq292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lovasi GS, Neckerman KM, Quinn JW, Weiss CC, Rundle A. Effect of individual or neighborhood disadvantage on the association between neighborhood walkability and body mass index. Am. J. Public Health. 2009;99:279–284. doi: 10.2105/AJPH.2008.138230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Maheswaran R, Strachan DP, Dodgeon B, Best NG. A population-based case-control study for examining early life influences on geographical variation in adult mortality in England and Wales using stomach cancer and stroke as examples. Int. J. Epidemiol. 2002;31:375–382. [PubMed] [Google Scholar]
- 78.Manda SO, Feltbower RG, Gilthorpe MS. Investigating spatio-temporal similarities in the epidemiology of childhood leukaemia and diabetes. Eur. J. Epidemiol. 2009;24:743–752. doi: 10.1007/s10654-009-9391-2. [DOI] [PubMed] [Google Scholar]
- 79.McLafferty S, Grady S. Immigration and geographic access to prenatal clinics in Brooklyn, NY: a geographic information systems analysis. Am. J. Public Health. 2005;95:638–640. doi: 10.2105/AJPH.2003.033985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McNally RJ, Colver AF. Space-time clustering analyses of occurrence of cerebral palsy in Northern England for births 1991 to 2003. Ann. Epidemiol. 2008;18:108–112. doi: 10.1016/j.annepidem.2007.07.104. [DOI] [PubMed] [Google Scholar]
- 81.McNally RJ, Pearce MS, Parker L. Space-time clustering analyses of testicular cancer amongst 15–24-year-olds in Northern England. Eur. J. Epidemiol. 2006;21:139–144. doi: 10.1007/s10654-005-5698-9. [DOI] [PubMed] [Google Scholar]
- 82.McNally RJ, Rankin J, Shirley MD, Rushton SP, Pless-Mulloli T. Space-time analysis of Down syndrome: results consistent with transient pre-disposing contagious agent. Int. J. Epidemiol. 2008;37:1169–1179. doi: 10.1093/ije/dyn083. [DOI] [PubMed] [Google Scholar]
- 83.Meliker JR, Sloan CD. Spatio-temporal epidemiology: principles and opportunities. Spat. Spatio Temporal Epidemiol. 2011;2:1–9. doi: 10.1016/j.sste.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 84.Michael YL, Perdue LA, Orwoll ES, Stefanick ML, Marshall LM. Physical activity resources and changes in walking in a cohort of older men. Am. J. Public Health. 2010;100:654–660. doi: 10.2105/AJPH.2009.172031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Michelozzi P, Capon A, Kirchmayer U, Forastiere F, Biggeri A, et al. Adult and childhood leukemia near a high-power radio station in Rome, Italy. Am. J. Epidemiol. 2002;155:1096–1103. doi: 10.1093/aje/155.12.1096. [DOI] [PubMed] [Google Scholar]
- 86.Miranda ML, Silva JM, Overstreet Galeano MA, Brown JP, Campbell DS, et al. Building geographic information system capacity in local health departments: lessons from a North Carolina project. Am. J. Public Health. 2005;95:2180–2185. doi: 10.2105/AJPH.2004.048785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Moore DA, Carpenter TE. Spatial analytical methods and geographic information systems: use in health research and epidemiology. Epidemiol. Rev. 1999;21:143–161. doi: 10.1093/oxfordjournals.epirev.a017993. [DOI] [PubMed] [Google Scholar]
- 88.Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am. J. Public Health. 2006;96:325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR., Jr Associations of the local food environment with diet quality—a comparison of assessments based on surveys and geographic information systems: the multi-ethnic study of atherosclerosis. Am. J. Epidemiol. 2008;167:917–924. doi: 10.1093/aje/kwm394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Morabia A, Mirer FE, Amstislavski TM, Eisl HM, Werbe-Fuentes J, et al. Potential health impact of switching from car to public transportation when commuting to work. Am. J. Public Health. 2010;100:2388–2391. doi: 10.2105/AJPH.2009.190132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Moran PA. Notes on continuous stochastic phenomena. Biometrika. 1950;37:17–23. [PubMed] [Google Scholar]
- 92.Morris SE, Sale RC, Wakefield JC, Falconer S, Elliott P, Boucher BJ. Hospital admissions for asthma and chronic obstructive airways disease in east London hospitals and proximity of residence to main roads. J. Epidemiol. Community Health. 2000;54:75–76. doi: 10.1136/jech.54.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nordling E, Berglind N, Melen E, Emenius G, Hallberg J, et al. Traffic-related air pollution and childhood respiratory symptoms, function and allergies. Epidemiology. 2008;19:401–408. doi: 10.1097/EDE.0b013e31816a1ce3. [DOI] [PubMed] [Google Scholar]
- 94.Ong P, Graham M, Houston D. Policy and programmatic importance of spatial alignment of data sources. Am. J. Public Health. 2006;96:499–504. doi: 10.2105/AJPH.2005.071373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Onozuka D, Hagihara A. Spatial and temporal dynamics of influenza outbreaks. Epidemiology. 2008;19:824–828. doi: 10.1097/EDE.0b013e3181880eda. [DOI] [PubMed] [Google Scholar]
- 96.Oyana TJ, Rogerson P, Lwebuga-Mukasa JS. Geographic clustering of adult asthma hospitalization and residential exposure to pollution at a United States-Canada border crossing. Am. J. Public Health. 2004;94:1250–1257. doi: 10.2105/ajph.94.7.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pearce J, Hiscock R, Blakely T, Witten K. The contextual effects of neighbourhood access to supermarkets and convenience stores on individual fruit and vegetable consumption. J. Epidemiol. Community Health. 2008;62:198–201. doi: 10.1136/jech.2006.059196. [DOI] [PubMed] [Google Scholar]
- 98.Pearce J, Witten K, Bartie P. Neighbourhoods and health: a GIS approach to measuring community resource accessibility. J. Epidemiol. Community Health. 2006;60:389–395. doi: 10.1136/jech.2005.043281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pikhart H, Bobak M, Kriz B, Danova J, Celko MA, et al. Outdoor air concentrations of nitrogen dioxide and sulfur dioxide and prevalence of wheezing in school children. Epidemiology. 2000;11:153–160. doi: 10.1097/00001648-200003000-00012. [DOI] [PubMed] [Google Scholar]
- 100.Potthoff RF, Whittinghill M. Testing for homogeneity. II. The Poisson distribution. Biometrika. 1966;53:183–190. [PubMed] [Google Scholar]
- 101.Pugliatti M, Riise T, Sotgiu MA, Satta WM, Sotgiu S, et al. Evidence of early childhood as the susceptibility period in multiple sclerosis: space-time cluster analysis in a Sardinian population. Am. J. Epidemiol. 2006;164:326–333. doi: 10.1093/aje/kwj190. [DOI] [PubMed] [Google Scholar]
- 102.Ramis Prieto R, Garcia-Perez J, Pollan M, Aragones N, Perez-Gomez B, Lopez-Abente G. Modelling of municipal mortality due to haematological neoplasias in Spain. J. Epidemiol. Community Health. 2007;61:165–171. doi: 10.1136/jech.2005.041491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rezaeian M, Dunn G, St Leger S, Appleby L. Geographical epidemiology, spatial analysis and geographical information systems: a multidisciplinary glossary. J. Epidemiol. Community Health. 2007;61:98–102. doi: 10.1136/jech.2005.043117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rogers JF, Thompson SJ, Addy CL, McKeown RE, Cowen DJ, Decoufle P. Association of very low birth weight with exposures to environmental sulfur dioxide and total suspended particulates. Am. J. Epidemiol. 2000;151:602–613. doi: 10.1093/oxfordjournals.aje.a010248. [DOI] [PubMed] [Google Scholar]
- 105.Rushton G. Public health, GIS, and spatial analytic tools. Annu. Rev. Public Health. 2003;24:43–56. doi: 10.1146/annurev.publhealth.24.012902.140843. [DOI] [PubMed] [Google Scholar]
- 106.Salah AB, Kamarianakis Y, Chlif S, Alaya NB, Prastacos P. Zoonotic cutaneous leishmaniasis in central Tunisia: spatio temporal dynamics. Int. J. Epidemiol. 2007;36:991–1000. doi: 10.1093/ije/dym125. [DOI] [PubMed] [Google Scholar]
- 107.Samuelsson U, Lofman O. Geographical mapping of type 1 diabetes in children and adolescents in south east Sweden. J. Epidemiol. Community Health. 2004;58:388–392. doi: 10.1136/jech.2002.004135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Sankoh OA, Ye Y, Sauerborn R, Muller O, Becher H. Clustering of childhood mortality in rural Burkina Faso. Int. J. Epidemiol. 2001;30:485–492. doi: 10.1093/ije/30.3.485. [DOI] [PubMed] [Google Scholar]
- 109.Schmiedel S, Blettner M, Kaatsch P, Schuz J. Spatial clustering and space-time clusters of leukemia among children in Germany, 1987–2007. Eur. J. Epidemiol. 2010;25:627–633. doi: 10.1007/s10654-010-9488-7. [DOI] [PubMed] [Google Scholar]
- 110.Schootman M, Jeff DB, Gillanders WE, Yan Y, Jenkins B, Aft R. Geographic clustering of adequate diagnostic follow-up after abnormal screening results for breast cancer among low-income women in Missouri. Ann. Epidemiol. 2007;17:704–712. doi: 10.1016/j.annepidem.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 111.Schootman M, Jeffe D, Kinman E, Higgs G, Jackson-Thompson J. Evaluating the utility and accuracy of a reverse telephone directory to identify the location of survey respondents. Ann. Epidemiol. 2005;15:160–166. doi: 10.1016/j.annepidem.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 112.Schootman M, Sterling DA, Struthers J, Yan Y, Laboube T, et al. Positional accuracy and geographic bias of four methods of geocoding in epidemiologic research. Ann. Epidemiol. 2007;17:464–470. doi: 10.1016/j.annepidem.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 113.Schootman M, Sun D. Small-area incidence trends in breast cancer. Epidemiology. 2004;15:300–307. doi: 10.1097/01.ede.0000121605.41388.7c. [DOI] [PubMed] [Google Scholar]
- 114.Sebert Kuhlmann AK, Brett J, Thomas D, Sain SR. Environmental characteristics associated with pedestrian-motor vehicle collisions in Denver, Colorado. Am. J. Public Health. 2009;99:1632–1637. doi: 10.2105/AJPH.2007.131961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Shi X, Duell E, Demidenko E, Onega T, Wilson B, Hoftiezer D. A polygon-based locally-weighted-average method for smoothing disease rates of small units. Epidemiology. 2007;18:523–528. doi: 10.1097/EDE.0b013e3181271ac8. [DOI] [PubMed] [Google Scholar]
- 116.Silhol R, Zins M, Chauvin P, Chaix B. Investigating the spatial variability in incidence of coronary heart disease in the Gazel cohort: the impact of area socioeconomic position and mediating role of risk factors. J. Epidemiol. Community Health. 2011;65:137–143. doi: 10.1136/jech.2009.087379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Smith DM, Cummins S, Taylor M, Dawson J, Marshall D, et al. Neighbourhood food environment and area deprivation: spatial accessibility to grocery stores selling fresh fruit and vegetables in urban and rural settings. Int. J. Epidemiol. 2010;39:277–284. doi: 10.1093/ije/dyp221. [DOI] [PubMed] [Google Scholar]
- 118.Snow J. On the Mode of Communication by Cholera. London: J. and A. Churchill; 1855. [Google Scholar]
- 119.Song C, Kulldorff M. Power evaluation of disease clustering tests. Int. J. Health Geogr. 2003;2:9. doi: 10.1186/1476-072X-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Stark Casagrande S, Gittelsohn J, Zonderman AB, Evans MK, Gary-Webb TL. Association of walkability with obesity in Baltimore City, Maryland. Am. J. Public Health. 2010:e1–e7. doi: 10.2105/AJPH.2009.187492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Steenland K, Deddens JA. A practical guide to dose-response analyses and risk assessment in occupational epidemiology. Epidemiology. 2004;15:63–70. doi: 10.1097/01.ede.0000100287.45004.e7. [DOI] [PubMed] [Google Scholar]
- 122.Stone RA. Investigations of excess environmental risks around putative sources—statistical problems and a proposed test. Stat. Med. 1988;7:649–660. doi: 10.1002/sim.4780070604. [DOI] [PubMed] [Google Scholar]
- 123.Sullivan AB, Gesink DC, Brown P, Zhou L, Kaufman JS, et al. Are neighborhood sociocultural factors influencing the spatial pattern of gonorrhea in North Carolina? Ann. Epidemiol. 2011;21:245–252. doi: 10.1016/j.annepidem.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tango T. A test for spatial disease clustering adjusted for multiple testing. Stat. Med. 2000;19:191–204. doi: 10.1002/(sici)1097-0258(20000130)19:2<191::aid-sim281>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 125.Tanser F. Methodology for optimising location of new primary health care facilities in rural communities: a case study in KwaZulu-Natal, South Africa. J. Epidemiol. Community Health. 2006;60:846–850. doi: 10.1136/jech.2005.043265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tanser F, Barnighausen T, Cooke GS, Newell ML. Localized spatial clustering of HIV infections in a widely disseminated rural South African epidemic. Int. J. Epidemiol. 2009;38:1008–1016. doi: 10.1093/ije/dyp148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Tassone EC, Waller LA, Casper ML. Small-area racial disparity in stroke mortality: an application of Bayesian spatial hierarchical modeling. Epidemiology. 2009;20:234–241. doi: 10.1097/EDE.0b013e3181935aee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Theophilides CN, Ahearn SC, Grady S, Merlino M. Identifying West Nile virus risk areas: the Dynamic Continuous-Area Space-Time system. Am. J. Epidemiol. 2003;157:843–854. doi: 10.1093/aje/kwg046. [DOI] [PubMed] [Google Scholar]
- 129.Thomas W, Birgit R, Edith S. Changing geographical distribution of diabetes mellitus type 1 incidence in Austrian children 1989–2005. Eur. J. Epidemiol. 2008;23:213–218. doi: 10.1007/s10654-008-9223-9. [DOI] [PubMed] [Google Scholar]
- 130.Turrell G, Kavanagh A, Draper G, Subramanian SV. Do places affect the probability of death in Australia? A multilevel study of area-level disadvantage, individual-level socioeconomic position and all-cause mortality, 1998–2000. J. Epidemiol. Community Health. 2007;61:13–19. doi: 10.1136/jech.2006.046094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ugarte MD, Goicoa T, Etxeberria J, Militino AF, Pollan M. Age-specific spatio-temporal patterns of female breast cancer mortality in Spain (1975–2005) Ann. Epidemiol. 2010;20:906–916. doi: 10.1016/j.annepidem.2010.07.102. [DOI] [PubMed] [Google Scholar]
- 132.Viel JF, Arveux P, Baverel J, Cahn JY. Soft-tissue sarcoma and non-Hodgkin’s lymphoma clusters around a municipal solid waste incinerator with high dioxin emission levels. Am. J. Epidemiol. 2000;152:13–19. doi: 10.1093/aje/152.1.13. [DOI] [PubMed] [Google Scholar]
- 133.Voigt LF, Davis S, Koepsell TD. Do cases and controls matched on the first eight digits of their telephone number share geographic proximity and socioeconomic characteristics? Ann. Epidemiol. 2006;16:299–304. doi: 10.1016/j.annepidem.2005.06.050. [DOI] [PubMed] [Google Scholar]
- 134.Waller LA, Gotway CA. Applied Spatial Statistics for Public Health Data. Hoboken, NJ: Wiley; 2004. [Google Scholar]
- 135.Ward MH, Nuckols JR, Giglierano J, Bonner MR, Wolter C, et al. Positional accuracy of two methods of geocoding. Epidemiology. 2005;16:542–547. doi: 10.1097/01.ede.0000165364.54925.f3. [DOI] [PubMed] [Google Scholar]
- 136.Werneck GL, Costa CH, Walker AM, David JR, Wand M, Maguire JH. The urban spread of visceral leishmaniasis: clues from spatial analysis. Epidemiology. 2002;13:364–367. doi: 10.1097/00001648-200205000-00020. [DOI] [PubMed] [Google Scholar]
- 137.Williams CT, Metzger DS. Race and distance effects on regular syringe exchange program use and injection risks: a geobehavioral analysis. Am. J. Public Health. 2010;100:1068–1074. doi: 10.2105/AJPH.2008.158337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yu HL, Chiang CT, Lin SD, Chang TK. Spatiotemporal analysis and mapping of oral cancer risk in Changhua county (Taiwan): an application of generalized Bayesian maximum entropy method. Ann. Epidemiol. 2010;20:99–107. doi: 10.1016/j.annepidem.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 139.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am. J. Public Health. 2005;95:660–667. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Zhan FB, Brender JD, De Lima I, Suarez L, Langlois PH. Match rate and positional accuracy of two geocoding methods for epidemiologic research. Ann. Epidemiol. 2006;16:842–849. doi: 10.1016/j.annepidem.2006.08.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.