Abstract
Introduction
We report a case of isolated intra-spinal tuberculosis in a 45 year-old woman. The uncommon findings in MRI were more suggestive of tumor lesion.
Materials and methods
After 3 month history of low back pain and 2 weeks radiated pain of right lower extremity, an operation was performed and the total intra-spinal mass was resected. Histological examination revealed a granulomatous necrosis with caseum. Symptoms were greatly improved postoperatively and then the patient was treated with four anti-tuberculosis drugs.
Conclusion
This case indicated the complexity of differentiating atypical spinal tuberculosis from disease which could cause spinal cord and cauda equina compression.
Keywords: Spinal tuberculosis, Spinal tumors, Atypical spondylitis, Spinal abscess
Introduction
Tuberculosis (TB) is a common infectious disease worldwide, which usually attacks the lungs. With the discovery of antibiotics, the prevalence of TB has markedly decreased in Europe, but the incidence still remains very high in developing countries. Besides lung, bone joint is the most common site of TB involvement, which accounts for 5 % of all case of TB. Among them, spinal region is easily affected and accounts for almost 50 % of skeletal TB [1]. The classical spinal TB affected anterior aspect of the vertebral body as well as the disc leading to destruction of adjacent vertebral bodies, intervertebral disc and even soft tissues. However, a small number of cases do not have the character of tuberculous spondylitis. These kinds of atypical spinal TB are rarely reported and often make diagnostic delays and even errors [2, 3]. Here we reported an atypical spinal TB mistaken for neoplasia in a female patient.
Case
A 45-year-old female visited the hospital with a history of intermittent back pain for 3 months. Two weeks ago, the soreness worsened with radiating pain to the right lower extremity. She complained of numbness in the right foot especially after movements. There was no history of exposure to TB, no recent weight loss, low-grade fever, decreased appetite and night sweats. The patient had regular bowel movement and urination. Physical examination revealed that the sensation was decreased in the lateral side of her right leg. The straight leg raise test was positive in the right side. Manual muscle testing revealed that the muscle strength of extensor hallucis longus was Grade 4/5 in the right side. Laboratory studies showed normal hemoglobin and white blood cell count. Erythrocyte sedimentation rate (ESR, 10 mm/h) and C-reactive protein (CRP, 8 mg/L) did not increase significantly. Both HIV and PPD tests were negative.
Further image analysis showed normal chest X-ray and abdominal ultrasound evidenced normal findings. A lumbosacral spine radiograph and CT reconstruction indicated no destruction of vertebral body and vertebral arch (Figs. 1, 2, 3). Based on the above results, the patient underwent an MRI examination. A dorsal mass in the extradural compartment of the spinal canal was observed in T2 weighted MRI images of the lumbosacral spine. The superior border of the mass reached the level of the intervertebral disk between L4 and L5. The inferior border reached the L5–S1 level and the theca was compressed. The signal of L4–5 and L5–S1 disc was observed to be normal and no bone structure was involved (Figs. 4, 5).
Fig. 1.

A-P lumbar spine radiograph
Fig. 2.

Lateral lumbar spine radiograph
Fig. 3.

CT reconstruction observed normal and no bone structure involved
Fig. 4.

MRI revealed a dorsal mass in extradural compartment of the spinal canal
Fig. 5.
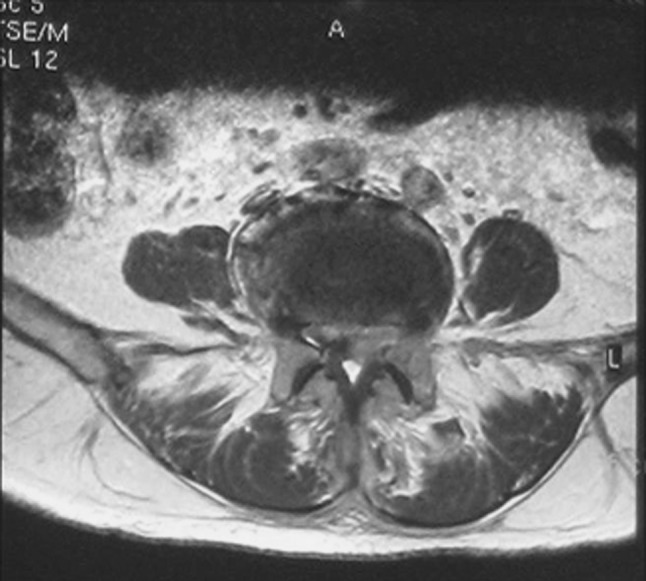
Axial MRI image of the epidural compression
Based on the symptoms and all these examinations of this patient, neoplasia in spinal canal was suspected. But it is not clear whether it is a primary or metastatic one. Instead of CT-guided needle biopsy, open biopsy was chosen to confirm the diagnosis. We observed that the edge of the mass was clear and it is feasible to resect it and decompress the spinal cord at the same time. A posterior laminectomy was performed at L5 level. Intraoperatively, greyish granulomas were seen out of the dura mater. The dura mater expanded well after removing the mass.
Histological analysis of fast frozen section demonstrated a chronic granulomatous inflammation with caseation, a character of tuberculosis, so we ceased the operation without further resection of the structure nearby. The final diagnosis of TB was confirmed later by pathologic examination with a positive culture of acid-fast bacilli (Fig. 6). The patient’s symptoms had greatly improved after operation. Meanwhile, combination therapy of antituberculous (rifampicin, isoniazid, pyrazinamide and ethambutol) was given to the patient on the next day of the operation for 12 months. Till the time of publication, the patient had recovered well and lived a normal life.
Fig. 6.
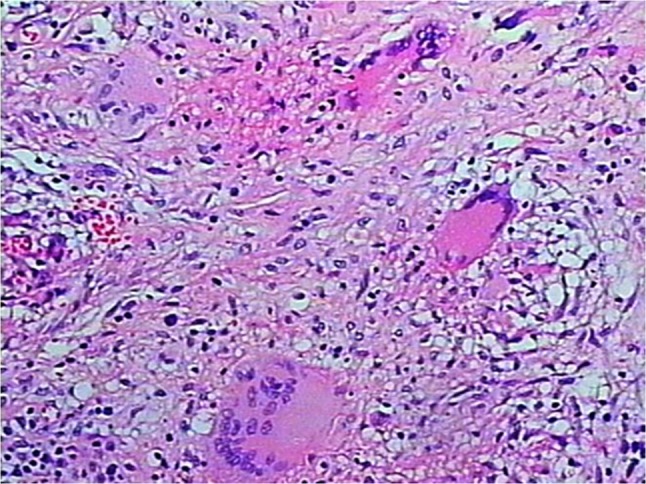
Frozen section revealed as chronic granulomatous inflammation with caseation
Discussion
Spinal TB in early stage has no specific features on radiological image, so plain radiography is of little help unless the collapse of disc margin or vertebra body appears. CT scan is valuable in revealing bony destruction and paraspinal abscesses formation. But MRI is more sensitive in diagnosing tuberculous spondylitis. It can detect abnormal bone marrow with a low signal on T1-weighted images as well as a high signal on T2-weighted images which can not be detected by radiographs and CT scans [4, 5]. In addition, special MRI sequences such as T1+ Gadolinium injection and/or diffusion MRI may be useful for diagnosis.
Generally, the features of atypical spinal TB include the following aspects: (1) involvement of the posterior elements of the spinal column with complete sparing of the anterior elements (vertebral bodies and discs), (2) skip lesions separated far enough from each other, (3) extradural spinal cord compression without radiographic evidence of bony involvement. Naim Ur et al. [6] summarized these characters and reported a case which included the features mentioned above and another destructive lesion of the sacrum with palpable pelvic mass. Thus, it is important to know more of atypical spinal TB and to identify it from other spinal disorders.
Concerning the present case we reported, the systemic condition of our patient was good without any symptoms of TB such as febris and night sweats. Laboratory examinations such as ESR and CRP are within the normal range. The only complaint of the patient was numbness of the right foot and decreased sensation in the lateral aspect of the right leg. These evidences suggested symptoms of disk herniation. Wellons et al. [7] retrospected the literature about spinal TB and disk herniation. His study showed that some patients with primary diagnosis as disk interval and on whom surgery was performed, were finally confirmed to have TB. He analyzed the possible mechanism that local TB lesion leads to the interruption of blood supply and nutrition to the disc, resulting in the similar symptom as reherniation. However, in our case, MRI examination indicated a dorsal mass in the spinal canal while intervertebral discs were dispensed with destruction, which is usually seen in spinal tumor [8]. Therefore, it prompted us to make the diagnosis as neoplasia.
For the first time, we reported here a very rare case of Pott’s disease which only has a single extradural tuberculous spondylitis in the spinal canal with a surprisingly negative PPD test. Usually, less response to Mycobacterium tuberculosis could occur in certain patients such as those with extremes of age, malnutrition, HIV positive or immune suppression. The inflammatory markers of these patients may be within the normal range and without any bony destruction. Granulomas could be found in the canal and sometimes accompanying dorsal soft tissue abscess in operation [9]. However, our patient was a healthy 45-year-old female. She has no sign of systemic involvement and the HIV test was negative. It definitely demonstrated the diagnostic difficulties of the atypical forms of spinal TB.
According to the criteria of Naim Ur R, the present case can be grouped to the third atypical spinal TB with extradural spinal cord compression. Compressing to the cauda equina could also cause rapid progressive paraparesis and paraplegia. Generally, most compressions on spinal cord result from epidural abscess. Tuberculous spinal epidural abscess usually occurred secondary to tuberculous spondylitis [10, 11]. Meanwhile, lesions are more commonly found in the lower thoracic region but less in lumbar and cervical spine. Laminectomies and catheter draining could be adopted for treating local or extensive epidural abscess [12, 13]. The case we reported was not an epidural abscess, but an isolated lesion and we did not find the primary foci of TB. Local granulomas finding in the canal of lower lumber spine were also reported for the first time.
Ringshausen et al. [14] have even described a fatal case of a patient with spinal TB, who was mistakenly irradiated for suspected metastatic lung cancer of the spine. They claimed that the most common cause in delaying the diagnosis of Pott’s disease is failure to consider this disease. So it is very important to consider skeletal TB in patients with focal bony or soft tissue abnormalities of the spine.
Conflict of interest
None.
Contributor Information
Yang Yu, Email: doctoryoung2008@hotmail.com.
Xinwei Wang, Email: orth.wang@263.net.
References
- 1.Huang B, Li CQ, Liu T, Zhou Y. Primary non-Hodgkin’s lymphoma of the lumbar vertebrae mimicking tuberculous spondylitis: a case report. Arch Orthop Trauma Surg. 2009;129:1621–1625. doi: 10.1007/s00402-009-0835-7. [DOI] [PubMed] [Google Scholar]
- 2.Sankaran-Kutty M. Atypical tuberculous spondylitis. Int Orthop. 1992;16:69–74. doi: 10.1007/BF00182990. [DOI] [PubMed] [Google Scholar]
- 3.Papagelopoulos PJ, Papadopoulos E, Mavrogenis AF, Themistocleous GS, Korres DS, Soucacos PN. Tuberculous sacroiliitis: a case report and review of the literature. Eur Spine J. 2005;14:683–688. doi: 10.1007/s00586-004-0831-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsai C-Y, Tsai T-H, Lin C-H, Cheng Y-H, Lieu A-S. Unusual exophytic neurocytoma of thoracic spine mimicking meningioma: a case report and review of the literature. Eur Spine J. 2011;20:239–242. doi: 10.1007/s00586-010-1625-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Polley P, Dunn R. Noncontiguous spinal tuberculosis: incidence and management. Eur Spine J. 2009;18:1096–1101. doi: 10.1007/s00586-009-0966-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naim Ur R, El-Bakry A, Jamjoom A, Jamjoom ZA, Kolawole TM. Atypical forms of spinal tuberculosis: case report and review of the literature. Surg Neurol. 1999;51:602–607. doi: 10.1016/S0090-3019(98)00101-3. [DOI] [PubMed] [Google Scholar]
- 7.Wellons JC, Zomorodi AR, Villaviciencio AT, Woods CW, Lawson WT, Eastwood JD. Sacral tuberculosis: a case report and review of the literature. Surg Neurol. 2004;61:136–139. doi: 10.1016/S0090-3019(03)00265-9. [DOI] [PubMed] [Google Scholar]
- 8.Murphey MD, Andrews CL, Flemming DJ, Temple HT, Smith WS, Smirniotopoulos JG. From the archives of the AFIP. Primary tumors of the spine: radiologic pathologic correlation. Radiographics. 1996;16:1131–1158. doi: 10.1148/radiographics.16.5.8888395. [DOI] [PubMed] [Google Scholar]
- 9.Polley P, Dunn R. Noncontiguous spinal tuberculosis: incidence and management. Eur Spine J. 2009;18:1096–1101. doi: 10.1007/s00586-009-0966-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joseffer SS, Cooper PR. Modern imaging of spinal tuberculosis. J Neurosurg Spine. 2005;2:145–150. doi: 10.3171/spi.2005.2.2.0145. [DOI] [PubMed] [Google Scholar]
- 11.Kumar A, Singh AK, Badole CM, Patond KR. Tubercular epidural abscess in children: report of two cases. Indian J Tuberc. 2009;56:217–219. [PubMed] [Google Scholar]
- 12.Alg VS, Demetriades AK, Naik S, Gunasekera L. Isolated subacute tuberculous spinal epidural abscess of the cervical spine: a brief report of a special case. Acta Neurochir (Wien) 2009;151:695–696. doi: 10.1007/s00701-009-0233-5. [DOI] [PubMed] [Google Scholar]
- 13.Mathew J, Tripathy P, Grewal S. Epidural tuberculosis involving the entire spine. Neurol Neurochir Pol. 2009;43:470–474. [PubMed] [Google Scholar]
- 14.Ringshausen FC, Tannapfel A, Nicolas V, Weber A, Duchna HW, Schultze-Werninghaus G, Rohde G. A fatal case of spinal tuberculosis mistaken for metastatic lung cancer: recalling ancient Pott’s disease. Ann Clin Microbiol Antimicrob. 2009;8:32. doi: 10.1186/1476-0711-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]


