Abstract
Objective(s)
To characterize the epidemiology and identify risk factors for complications necessitating removal of peripherally inserted central venous catheters (PICCs) in children.
Design
Cohort study
Setting
The Johns Hopkins Children’s Center, Baltimore, Maryland.
Participants
Hospitalized children who had a PICC inserted outside of the neonatal ICU between January 1, 2003 and December 1, 2009.
Main Exposures
Age, PICC dwell time, PICC insertion site, PICC tip location, pediatric ICU exposure, indication for PICC insertion
Outcome Measures
Complications necessitating PICC removal as recorded by the PICC Team.
Results
During the study period, 2574 PICCs were placed in 1807 children. Complications necessitating catheter removal occurred in 20.8% of PICCs during 46,021 catheter days (11.6 complications per 1,000 catheter days). These included accidental dislodgement (4.6%), infection (4.3%), occlusion (3.6%), local infiltration (3.0%), leakage (1.5%), breaks (1.4%), phlebitis (1.2%) and thrombosis (0.5%). From 2003 to 2009 complications decreased by 15% per year (IRR 0.85; 95%CI 0.81-0.89). In adjusted analysis, all non-central PICC tip locations - midline (IRR 4.59, 95% CI 3.69-5.69), mid-clavicular (IRR 2.15, 95% CI 1.54-2.98), and other (IRR 3.26 95% CI 1.72-6.15) - compared to central tip location were associated with an increased risk of complications. Pediatric ICU exposure and age less than one year old were independently associated with complications necessitating PICC removal.
Conclusion(s)
Non-central PICC tip locations, younger age, and pediatric ICU exposure were independent risk factors for complications necessitating PICC removal. Despite reductions in PICC complications, further efforts are needed to prevent PICC-associated complications in children.
Keywords: Catheter-Related infection, Pediatrics, Catheters, Epidemiology
BACKGROUND
Central venous catheters (CVCs) provide secure vascular access to facilitate delivery of medications and nutrition to hospitalized children.1 Peripherally inserted central venous catheters (PICCs) can be conveniently inserted at the bedside without the need for surgical intervention and are commonly used in pediatrics. Despite these advantages, PICCs are prone to infectious, thrombotic and mechanical complications. These complications are associated with morbidity, so data are needed to inform quality improvement efforts.
Previous studies have identified risk factors for complications of PICCs in children including young age, severity of illness, catheter dwell time, catheter tip location, and catheter insertion site.1-3 Identifying modifiable risk factors of complications is especially important as clinicians work to prevent catheter complications. Previous studies evaluating modifiable risk factors such as catheter dwell time, catheter insertion site, and catheter tip location have had inconsistent results.2-15 Our objective was to determine the association between patient and catheter characteristics and the risk of complications necessitating PICC removal in children.
MATERIALS AND METHODS
PATIENTS AND SETTING
A cohort was compiled of 1819 children who were admitted to the 175-bed Johns Hopkins Children’s Center and had a PICC inserted between January 2003 and December 2009. Children admitted to the 30-bed Pediatric Intensive Care Unit (ICU) and the medical/surgical wards were included, but patients in the neonatal ICU were excluded. The pediatric PICC team placed all PICCs, and as previously described2 maintained a database of all children with PICCs. The database contains indications for PICC insertion. Members of the PICC team, who were not blinded to patient characteristics, prospectively documented complications necessitating PICC removal, including infectious complications and non infectious complications (see eTable 1) and reviewed hospital records and contacted home care companies or healthcare providers to determine PICC disposition and complications following discharge.
DATA COLLECTION
The PICC team prospectively collected age, sex, race, ethnicity, indication for catheter insertion, and other catheter characteristics. Medical records were queried to validate the PICC database. An administrative claims database was queried to extract information regarding ICU admissions, ICD-9 codes, and length of hospital stay. PICCs were defined as peripherally inserted central venous catheters that were inserted with the intention of terminating at or close to the heart or in one of the great vessels. Exposures were determined prospectively by the PICC team. PICCs were defined as central at time of placement if they resided in the superior vena cava (SVC), right atrial junction (RAJ), or high inferior vena cava (IVC) or above the level of the diaphragm for lower extremity catheters, and as non-central if located elsewhere.16 For PICCs placed in the arm, non-central tip locations were further categorized as ‘midline’ if catheter tip extended no further than axilla, as ‘midclavicular’ if the catheter tip extended to the middle of the clavicle on x-ray, and as ‘other tip location’ if the tip extended beyond the middle of the clavicle on x-ray but not into the SVC, or were scalp catheters with tips above the level of the clavicle or lower extremity PICCs with tips below the IVC.
Catheters were removed after completion of therapy or due to a complication. The primary outcome, complications necessitating PICC removal, was defined as outlined in eTable 1 and was divided into secondary outcomes of infectious and non-infectious complications necessitating PICC removal recognizing that risk factors may vary for different complications. The time at risk for complication was the PICC dwell time, calculated as the number of days between PICC insertion and PICC removal.
After exploratory data analysis, variables were categorized for analysis. Age was not evenly distributed and was categorized into quartiles. ICD9 codes were collected for each patient’s hospitalization and categorized into underlying complex chronic medical conditions.2, 17 To account for severity of illness, patients were categorized as those requiring intensive care in the pediatric ICU (PICU) (referred to as having “PICU exposure”) and those not requiring intensive care or having “no PICU exposure”. PICC insertion sites were categorized into upper extremity, lower extremity, and head and neck.
STATISTICAL ANALYSIS
Descriptive analyses were performed to characterize the patients and catheter characteristics. We report median values along with the 25th and 75th percentiles for age, PICC duration and length of stay. Patients whose PICCs were removed in the hospital, but who did not have a documented reason for PICC removal in the PICC database or the medical record (n=12, <1%) were not included in the analysis. Patients transferred to another facility for which outcome data were not available were censored at time of hospital discharge.
Independent predictors of any complication necessitating PICC removal were assessed in bivariate and multivariable analyses using Poisson regression models to estimate incidence rate ratios (IRR). Covariates determined a priori to be independent predictors of complications and those with P <0.10 in bivariate analysis were included. Variables were retained in the final model if they were deemed clinically relevant or if they were observed to have a confounding effect on the association between another predictor and risk of complication. A confounding effect was defined as a change in a model coefficient by >10% after removal of a single variable from the model. After exploring the initial data, cubic spline terms were introduced for modeling PICC dwell time to account for a non-linear association of complications over time.18, 19 Similar multivariable models were used to identify risk factors for infectious complications and non-infectious complications as outcomes. An interaction between catheter dwell time and tip location was explored by (1) including interaction terms explicitly in the full model and by (2) evaluating a graph of the model-estimated complication rates across catheter dwell time for a given catheter tip location, age group, PICU and antibiotic exposure status, site of PICC insertion, and year. The interaction term was not included in the final model as it did not improve model fit based on Bayesian Information Criterion (BIC) (results not shown).20 Bootstrapping techniques with 1000 replications were used to assess the internal validity of the final model.21, 22 Model fit was confirmed by using Pearson’s goodness-of-fit test.
This study was approved by Johns Hopkins University School of Medicine Institutional Review Board with waiver of informed consent. Data were maintained in Microsoft Access and were analyzed using Stata version 11.0 and R version 2.12.23
RESULTS
During the study period, 2574 PICCs were placed in 1807 children. Over half of the children were male (55.6%). Fifty six percent of children were Caucasian, 32% were African American, and the median age was 5 years old (see Table 1). Median PICC dwell time was 13 days, and median length of hospitalization was 12 days. PICCs were inserted for indications such as administration of antibiotics (1352, 52.5%), total parenteral nutrition (200, 7.8%), chemotherapy (252, 9.8%) or for intravenous access (770, 29.9%). The majority of PICCs (1961, 76.4%) were inserted in the upper extremity. In this cohort, 2152 (83.9%) catheters had a central tip location, while 414 (16.1%) had a non-central tip location. Children with non-central PICCs were younger than those with central PICCs (median age 2 years vs. 7 years, p<0.001).
Table 1. Characteristics of Hospitalized Children with Peripherally Inserted Central Venous Catheters (PICCs).
| Age in years, Median (IQR) | 5 (0.83-13) |
| Sex, n (%) | |
| Male | 1005 (55.6) |
| Female | 802 (44.4) |
| Race and Ethnicity, n (%) | |
| Caucasian | 1017 (56.3) |
| African American | 575 (31.8) |
| Asian | 161 (8.9) |
| Hispanic | 43 (2.4) |
| Other | 11 (0.6) |
| PICC Duration in days, Median (IQR) | 13 (7-21) |
| Length of hospital stay, Median (IQR) | 12 (6-27) |
| Indication for PICC insertion, n (%) | |
| Antibiotics | 1352 (52.5) |
| Total Parenteral Nutrition | 200 (7.8) |
| Chemotherapy | 252 (9.8) |
| Intravenous access | 770 (29.9) |
| Complex chronic conditions, n (%) * | |
| Neuromuscular | 270 (14.9) |
| Cardiovascular | 767 (42.4) |
| Respiratory | 263 (14.5) |
| Renal | 107 (5.9) |
| Gastrointestinal | 121 (6.7) |
| Hematologic and Immunodeficiencies | 57 (3.2) |
| Metabolic | 71 (3.9) |
| Congenital & Genetic | 101 (5.6) |
| Malignancy | 198 (11) |
| None | 455(25.2) |
| Site of PICC Insertion, n (%) | |
| Upper Extremity (Basilic, Cephalic, Brachial) | 1961 (76.4) |
| Lower extremity (Saphenous) | 132 (5.6) |
| Head and Neck (Facial, Post Auricular, Ext Jugular) | 464 (18.1) |
| Catheter Tip Location | |
| Central | 2152(83.9) |
| Midline | 262 (10.2) |
| Mid-Clavicular | 121 (4.7) |
| Other | 31(1.2) |
| Total Number of children hospitalized over study period, n | 1807 |
All conditions do not add up to a 100% as many chronic conditions overlap.
3.32% patients were transferred outside the hospital, and their lines were removed elsewhere
Most PICCs (1901, 73.8%) were removed electively on completion of therapy, and 139 (5.4%) remained in place at time of patient transfer to an outside facility (see Table 2). Five hundred and thirty four PICCs (20.8%) were removed due to a complication during 46,021 catheter days (incidence rate 11.6 per 1000 catheter days), including 422 PICCs removed secondary to non-infectious complications and 112 PICCs removed for infectious complications. Of those removed for infectious complications, 66 (55.4%) met the National Healthcare Safety Network’s criteria as a central line-associated bloodstream infections (CLABSI).24
Table 2. Disposition of Peripherally Inserted Central Venous Catheters (PICCs).
| Catheter Disposition | Total number (%) |
|---|---|
| Removed - no longer needed | 1901(73.8) |
| Removed - infectious complications | 112 (4. 3) |
| Infection involving PICC | 103 (4.0) |
| Suspected infection involving PICC | 9 (0.3) |
| Removed -non infectious complications | 422 (16.4) |
| Phlebitis | 32 (1.2) |
| Local Infiltration | 77 (3.0) |
| Thrombosis | 14 (0.5) |
| Leakage | 38 (1.5) |
| Occlusion | 94 (3.6) |
| Dislodgement | 119 (4.6) |
| Breakage | 36 (1.4) |
| Other | 12 (0.5) |
| Transferred * | 139 (5.4) |
Transferred to another health-care facility with PICC, no further information is available on these patient
The incidence of complications declined from 17.2 per 1000 catheter days in the year 2003 to 5.5 per 1000 catheter days in 2009 (see Table 3). In parallel, the use of non-central PICCs declined from 14% in 2003 to 2.8% in 2009. Non-central PICCs were more likely to have complications necessitating removal than central catheters (46% vs. 17.6%; P< .001).
Table 3. Incidence Rate of complications by Year.
| Year | Incidence Rate of complications (per 1000 catheters days) |
Incidence Rate of Infectious complications (per 1000 catheters days) |
Incidence Rate of Non-infectious complications (per 1000 catheters days) |
Number of PICCs placed |
Number of Non- central PICCs placed |
|---|---|---|---|---|---|
| 2003 | 17.2 | 2.7 | 14.5 | 323 | 45 (14%) |
| 2004 | 17.9 | 4.1 | 13.9 | 380 | 42 (11%) |
| 2005 | 17.9 | 2.6 | 15.4 | 356 | 34 (9.6%) |
| 2006 | 10.4 | 1.6 | 8.9 | 326 | 35 (10.7%) |
| 2007 | 9.2 | 2.2 | 7.0 | 380 | 38 (10%) |
| 2008 | 7.2 | 2.1 | 5.2 | 441 | 29 (6.6%) |
| 2009 | 5.5 | 1.9 | 3.7 | 352 | 10 (2.8%) |
Bivariable analyses of potential risk factors for complications necessitating PICC removal are shown in Table 4. All non-central PICC tip locations - midline (IRR 5.57, 95% CI 4.54-6.83), mid-clavicular (IRR 3.62, 95% CI 2.65-4.95) and other (IRR: 4.12, 95% CI 2.20-7.72) compared to central tip location were associated with an increased risk of complications. Compared to children less than one year old, children in older age categories had lower risks of developing complications, with the most significant reduction in risk in those >13 years (IRR 0.35, 95% CI 0.27-0.44). PICU exposure was also associated with a significantly increased risk for complications leading to PICC removal (IRR 1.71, 95% CI 1.44-2.03).
Table 4. Adjusted and Unadjusted Risk Factors for Peripherally Inserted Central Venous Catheter (PICC) Complications.
| Variable | No Complication Number (%) |
Complication Number (%) |
IRR (95% CI) | p value | Adjusted IRR* (95% CI) |
p value |
|---|---|---|---|---|---|---|
| Age | ||||||
| <1 year | 585 (28.7) | 255 (47.8) | 1 | 1 | ||
| ≥1 to 7 years | 401 (19.7) | 103 (19.3) | 0.58 (0.47-0.71) | <0.001 | 0.75 (0.60-0.94) | 0.01 |
| >7 to 13 years | 560 (27.5) | 77 (14.4) | 0.28 (0.21-0.37) | <0.001 | 0.44 (0.33-0.60) | <0.001 |
| >13 years | 494 (24.2) | 99 (18.5) | 0.35 (0.27-0.44) | <0.001 | 0.45 (0.35-0.59) | <0.001 |
| Sex | ||||||
| Male | 1073 (52.6) | 301 (56.4) | 1 | 1 | ||
| Female | 967 (47.4) | 233 (43.63) | 0.85(0.72-1.01) | 0.07 | 0.99 (0.83-1.18) | 0.94 |
| Site of PICC Insertion ** | ||||||
| Upper Extremity | 1592 (78.2) | 369 (69.3) | 1 | 1 | ||
| Lower extremity | 91 (4.5) | 52 (9.8) | 2.34 (1.75-3.13) | <0.001 | 1.08 (0.79-1.48) | 0.64 |
| Head and neck | 353 (17.3) | 111 (20.9) | 1.34(1.09-1.67) | 0.006 | 1.11 (0.89-1.39) | 0.37 |
|
Clinical Indication for PICC insertion |
||||||
| Intravenous Access | 547 (26.8) | 223 (41.7) | 1 | 1 | ||
| Antibiotics | 158 (7.8) | 42 (7.9) | 0.62 (0.51-0.76) | <0.001 | 0.86 (0.69-1.06) | 0.15 |
| Total Parenteral Nutrition | 183 (9.0) | 69 (13.0) | 0.89 (0.64-1.24) | 0.50 | 1.21 (0.86-1.69) | 0.27 |
| Chemotherapy | 1152 (56.4) | 200 (37.4) | 1.08 (0.82-1.42) | 0.58 | 0.95 (0.71-1.28) | 0.74 |
| Catheter Tip Location | ||||||
| Central | 1803 (88.6) | 349 (65.8) | 1 | 1 | ||
| Non-Central | ||||||
| Midline | 136 (6.7) | 126 (23.8) | 5.57 (4.54-6.83) | <0.001 | 4.59 (3.69-5.69) | <0.001 |
| Mid-Clavicular | 76 (3.7) | 23 (8.5) | 3.62 (2.65-4.95) | <0.001 | 2.15 (1.54-2.98) | <0.001 |
| Other | 21 (1.0) | 10 (1.9) | 4.12 (2.20-7.72) | <0.001 | 3.26 (1.72-6.15) | <0.001 |
| PICU Exposure | ||||||
| No | 1236 (60.6) | 221 (41.4) | 1 | 1 | ||
| Yes | 804 (39.4) | 313 (58.6) | 1.71 (1.44-2.03) | <0.001 | 1.24 (1.03-1.52) | 0.03 |
| Line Year | - | - | 0.81 (0.78-0.85) | <0.001 | 0.85 (0.81-0.89) | <0.001 |
Abbreviations: CI, confidence interval; IRR, incidence rate ratio; PICU, pediatric intensive care unit.
Adjusted for catheter dwell time using cubic spline terms
Insertion sites for PICCs were classified as upper extremity, lower extremity and head and neck based on where the PICC was inserted
After adjusting for other variables including catheter dwell time, age, insertion site, PICU exposure, indication for PICC insertion, and year of PICC insertion, non-central tip locations were associated with an increased risk of complications compared to central locations (all non-central tip locations - IRR 3.58; 95% CI 2.94-4.34; midline tip location - IRR 4.59, 95% CI 3.69-5.69; mid-clavicular tip location - IRR 2.15, 95% CI 1.54-2.98, and other tip locations - IRR 3.26 95% CI 1.72-6.15) (Table 4). Compared to age group less than 1 year, all age groups remained important risk factors for complications. After adjusting for other variables, children who had PICU exposure during their hospitalization were at 24% increased risk for developing a complication that necessitated PICC removal (IRR: 1.24, 95% CI 1.03-1.52). However, site of PICC insertion and clinical indication for PICC insertion were no longer associated with complications in adjusted analyses.
Recognizing that there may be different risk factors for infectious and non-infectious complications necessitating catheter removal, we performed a sub-analysis to look at variables associated with each outcome (Table 5). After adjusting for catheter dwell time, age, insertion site, tip location, indication for PICC insertion, and year of PICC insertion, ICU exposure was a risk factor for infectious complications, but not non-infectious complications. A non-central tip location was strongly associated with non-infectious complications but not with infectious complications (IRR 4.56 95% CI 3.67-5.61 and IRR 0.75 95% CI 0.34-1.50, respectively).
Table 5. Adjusted Risk Factors for Infectious Complications and Non-Infectious Complications.
| Infectious Complications | Non-Infectious Complications | |||
|---|---|---|---|---|
| Variable | Adjusted IRR* (95% CI) |
p value | Adjusted IRR* (95% CI) |
p value |
| Age categories | ||||
| <1 year | 1 | 1 | ||
| ≥1 to 7 years | 0.89(0.54-1.48) | 0.66 | 0.75(059-0.97) | 0.03 |
| >7 to 13 years | 0.56(0.30-1.56) | 0.07 | 0.43(0.30-0.59) | <0.001 |
| >13 years | 0.56(0.32-0.98) | 0.04 | 0.47(0.35-0.63) | <0.001 |
| Site of PICC Insertion ** | ||||
| Upper Extremity | 1 | 1 | ||
| Lower extremity | 0.71(0.32-1.56) | 0.41 | 1.21(0.85-1.70) | 0.29 |
| Head and neck | 0.45(0.24-0.83) | 0.01 | 1.26(0.99-1.61) | 0.06 |
| Tip Location | ||||
| Central | 1 | 1 | ||
| Non-Central*** | 0.75(0.34-1.50) | 0.38 | 4.56(3.67-5.61) | <0.001 |
| PICU Exposure | ||||
| No | 1 | 1 | ||
| Yes | 2.23(1.43-3.48) | <0.001 | 1.11(0.89-1.38) | 0.35 |
| Line Year | 0.86(0.78-0.95) | 0.003 | 0.86(0.82-0.91) | <0.001 |
Abbreviations: CI, confidence interval; IRR, incidence rate ratio; PICU, pediatric intensive care unit.
Adjusted for catheter dwell time using cubic spline terms, sex, and indication for catheter insertion
Insertion sites for PICCs were classified as upper extremity, lower extremity and head and neck based on where the PICC was placed
Catheter tip locations were categorized as non-central if they did not reside in the superior vena cava, right atrium, or high inferior vena cava or above the level of the diaphragm for lower extremity catheters.
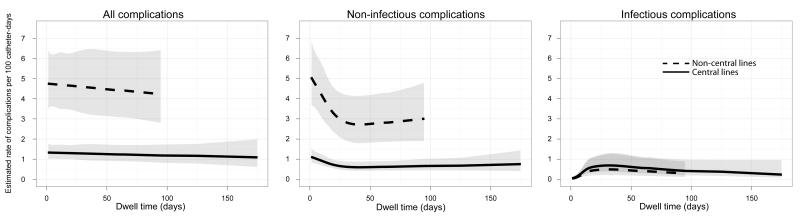
Figure 1 illustrates the complex and non-linear interaction of catheter dwell time and risk of complication in PICCs with central and non-central locations. PICCs with non-central locations have a consistently higher risk of non-infectious complication regardless of catheter duration, but this association is not seen for infectious complications.
Figure 1.
Predicted complication rates over catheter dwell time for a given catheter tip location, age group, PICU and antibiotic exposure status, site, and year. Rates for all complications, non-infectious complications, and infectious complications are stratified for PICCs with a central tip location (solid line) and a non-central tip location (dashed line) with 95% confidence intervals (shading).
DISCUSSION
We report results from a large cohort of hospitalized children with PICCs that will help clinicians provide anticipatory guidance to families when discussing PICC complications, and that identifies a target for future quality improvement efforts. Although PICCs with a non-central catheter tip location represented a small percentage (16.1%) of inserted PICCs, these catheters were more than three times as likely to be removed secondary to a complication compared with PICCs with a central tip location. Younger children and those with pediatric ICU exposure during the current hospitalization were at increased risk of complications. At our institution, PICC complication rates in children decreased from 17.2 per 1000 catheter days in 2003 to 5.5 per 1000 catheter days in 2009, but further efforts are needed to prevent infectious and non-infectious complications of PICCs in children.
Our data represent the largest study of children with PICCs to report complications necessitating PICC removal. Our study reports similar complication rates to prior studies that have reported rates ranging from 17% to 50%.2, 3, 12, 15, 25-28 This large variation in complication rates may be in part explained by differences in types of complications reported (infectious, non-infectious, or both combined), and different populations studied (e.g. oncology or ICU). Additionally, ascertainment of complications can vary by study, for example, our study was unique in that our PICC team followed children to determine PICC disposition after hospital discharge. This approach identified that 25% of complications necessitating removal occurred after hospital discharge.
The association of catheter-tip location and PICC complications remains unclear from conflicting studies in children. Some pediatric studies have found that PICCS placed in non-central veins provided safe and reliable intravenous access13, 15, while others suggested that PICCs terminating in non-central venous locations have higher complication risks.10, 14 These studies are difficult to compare in part because of inconsistent definitions of central veins. For example, many authors and clinicians define a PICC to terminate in a central vein if the tip is located in the IVC, SVC, or RAJ.9, 14 Other authors, clinicians, and the Centers for Disease Control and Prevention include the subclavian veins as central veins.15, 24, 29 Given the size of our cohort, these are the first pediatric data to compare PICCs with distal tip locations in the IVC, SVC and RAJ with PICCs in the subclavian veins and other non-central sites. After adjusting for other important predictors of PICC complications including age, catheter dwell time, PICC insertion site, PICU exposure, and indication for PICC insertion, our data confirmed previous findings that non-central catheter tip location are associated with increased complication rates.10, 14 Additionally, we found that PICCs terminating in any site outside the IVC, SVC, or RAJ, including subclavian veins, had an increased risk of complications necessitating removal. A previous study that found no difference in complication rates between central and non-central PICCs classified 46% of PICCs terminating in the subclavian vein as central which may explain our differing results.15
Increased complication rates, especially mechanical complications in non-central PICCs may result from a combination of factors including turbulence, vessel size, blood flow rate and endothelial injury.14 Our data suggest that non-central catheters were an independent risk factor for non-infectious complications. When a central venous catheter is positioned in the SVC, the tip lies parallel to the vessel wall, so infused solutions dilute rapidly. PICCs cannot always be advanced to the SVC due to venospasm, venous valves, and vessel tortuosity.10 When the catheter tip lies in a non-central location, the tip may contact the vessel, irritate and disrupt the endothelial cell layer, expose the basement membrane, and trigger coagulation.30 We observed a parallel in the reduction in PICC complication rates and the declining use of non-central PICCs from 2003 to 2009. Therefore, non-centrally located PICCs should be used with caution due to their increased risk of complication necessitating catheter removal.
Catheter dwell time has also been suggested as a risk factor for PICC complications with some studies finding longer dwell times associated with complications2, 18, 19, 31 and others finding shorter dwell times associated with complications.3 We illustrated the complex interaction of catheter dwell time and risk of complication in PICCs. For example the risk of infectious complications seemed to increase over the first few weeks then plateau, where the risk of non-infectious complications seemed to decrease over the first few weeks then plateau. We also showed that PICCs with non-central locations were prone to a consistently higher risk of non-infectious complication regardless of catheter duration, but were not prone to higher risk of non-infectious complications. These results may explain differences in associations between catheter dwell time and risk of complications in previous studies. Given that non-infectious complications were three times more common than infectious complications, ensuring a central tip location at the RAJ, IVC, or SVC is an appropriate step to prevent PICC complications. However, given the complex association of catheter dwell time with complications, these data do not support the hypothesis that prolonged catheter dwell times are associated with increased PICC complications.
Our data found that younger children were at increased risk of complications requiring PICC removal. Children older than 13 years were at lowest risk for complications, while those less than 1 year were at highest risk, consistent with previous findings that older age may protect against CVC-associated complications.32 Older children have structurally larger and more stable vessels that may tolerate catheters better. Therefore, age may confound the association between tip location and PICC complication, because advancing PICCs in younger children may be more challenging and this may lead to more unintended non-central PICCs in this age group. However, after adjusting for age, we still found an increased risk of complication in those PICCs with a non-central tip location.
Previous studies have identified insertion site as a risk factor for catheter-associated infection2, 5, 7; however these findings have not been supported by other studies.4, 6, 33 In unadjusted analysis of our cohort, PICCs placed in the head and neck and lower extremities were associated with an increased risk for complications necessitation removal, however, after adjusting for other important variables including age, catheter dwell time, ICU exposure, indication for PICC insertion, and tip location, insertion site was no longer a significant risk factor for complications. Younger children were more likely to have complications and were more likely to have PICCs placed in the head and neck and lower extremities (data not shown), which may confound this perceived association.
Several limitations should be considered when interpreting our findings. First, a small percentage of patients (5%) were lost to follow up, mostly due to transfer to other healthcare facilities. However, for most catheters, prospective follow up by our PICC team reduced missing data and captured entire PICC dwell time including time after discharge. Secondly, we could only document complications that necessitated line removal; hence we likely underestimated the risk of complications, such as occlusion requiring tissue plasminogen activator (TPA) administration. Additionally, some catheter infections may have been treated with antibiotics while the PICC remained in place, a complication that was not captured. Finally, despite this large cohort, because this is a single-institution study, our findings may not be generalizable to other institutions.
CONCLUSION
Our large cohort and robust adjusted analyses identified non-central catheter tip location as a modifiable risk factor for complications necessitating PICC removal. Clinicians should be cautious in weighing the risks and benefits of maintaining a non-central PICC. Quality improvement initiatives should reinforce the importance of inserting PICCs to terminate in the RAJ, IVC, or SVC to reduce risk of complications. National efforts have dramatically reduced the risk of bloodstream insertions complicating central-venous catheters34, but further efforts are needed to prevent all complications that lead to additional procedures, patient morbidity, and increased healthcare costs.
Supplementary Material
ACKNOWLEDGEMENTS
We thank members of The JHH Pediatric PICC Team for their support of this study.
Financial Support: This work was supported by National Institute of Allergy and Infectious Disease, National Institutes of Health (1 K23 AI081752-03 to AM) and the National Institute for Nursing Research, National Institutes of Health (1R03NR012558-02 to AM).
Role of the Sponsors: The study sponsors had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
Abbreviations
- CVCs
Central venous catheters
- PICCs
Peripherally inserted central venous catheters
- CLABSI
Central Line–Associated Bloodstream Infection
- RAJ
right atrial junction
- SVC
superior vena cavas
- IVC
inferior vena cava
- PICU
Pediatric Intensive Care Unit
- BIC
Bayesian Information Criterion
- IRR
Incidence Rate ratio
- TPA
tissue plasminogen activator
Footnotes
Potential conflicts of interest: A.M. receives grant support from Sage Products. All other authors (KJ, SA, LG, NR) report no disclosures.
The data from this study were presented in part at the 49th Annual Scientific Meeting of the Infectious Diseases Society of America, Boston, October 2011.
Disclaimer: The contents of this article are solely the responsibility of the authors and do not necessarily represent the official view of the National Center for Research Resources or NIH.
Author Contributions: Dr. Milstone had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Milstone, Gosey, Jumani, Advani. Acquisition of data: Milstone, Advani, Jumani, Gosey. Analysis and interpretation of data: Milstone, Advani, Jumani, Gosey, Reich. Drafting of the manuscript: Jumani, Advani. Critical revision of the manuscript for important intellectual content: Milstone, Advani, Jumani, Gosey, Reich. Statistical analysis: Milstone, Advani, Jumani, Reich. Obtained funding: Milstone. Administrative, technical, and material support: Milstone, Advani, Jumani, Gosey, Reich. Study supervision: Milstone.
References
- 1.Bourgeois FC, Lamagna P, Chiang VW. Peripherally inserted central catheters. Pediatr Emerg Care. 2011;27(6):556–61. doi: 10.1097/PEC.0b013e31821dc9b6. quiz 62-3. [DOI] [PubMed] [Google Scholar]
- 2.Advani S, Reich NG, Sengupta A, Gosey L, Milstone AM. Central line-associated bloodstream infection in hospitalized children with peripherally inserted central venous catheters: extending risk analyses outside the intensive care unit. Clin Infect Dis. 2011;52(9):1108–15. doi: 10.1093/cid/cir145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrier A, Williams DJ, Connelly M, Creech CB. Frequency of peripherally inserted central catheter complications in children. Pediatr Infect Dis J. 2011;31(5):519–21. doi: 10.1097/INF.0b013e31824571b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bonventre EV, Lally KP, Chwals WJ, Hardin WD, Jr., Atkinson JB. Percutaneous insertion of subclavian venous catheters in infants and children. Surg Gynecol Obstet. 1989;169(3):203–5. [PubMed] [Google Scholar]
- 5.Goetz AM, Wagener MM, Miller JM, Muder RR. Risk of infection due to central venous catheters: effect of site of placement and catheter type. Infect Control Hosp Epidemiol. 1998;19(11):842–5. doi: 10.1086/647742. [DOI] [PubMed] [Google Scholar]
- 6.Lally KP, Brennan LP, Sherman NJ, Grushkin C, Lieberman E, Atkinson JB. Use of a subclavian venous catheter for short- and long-term hemodialysis in children. J Pediatr Surg. 1987;22(7):603–5. doi: 10.1016/s0022-3468(87)80108-2. [DOI] [PubMed] [Google Scholar]
- 7.Merrer J, De Jonghe B, Golliot F, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001;286(6):700–7. doi: 10.1001/jama.286.6.700. [DOI] [PubMed] [Google Scholar]
- 8.Cadman A, Lawrance JA, Fitzsimmons L, Spencer-Shaw A, Swindell R. To clot or not to clot? That is the question in central venous catheters. Clin Radiol. 2004;59(4):349–55. doi: 10.1016/j.crad.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 9.Chait PG, Ingram J, Phillips-Gordon C, Farrell H, Kuhn C. Peripherally inserted central catheters in children. Radiology. 1995;197(3):775–8. doi: 10.1148/radiology.197.3.7480755. [DOI] [PubMed] [Google Scholar]
- 10.Colacchio K, Deng Y, Northrup V, Bizzarro MJ. Complications associated with central and non-central venous catheters in a neonatal intensive care unit. J Perinatol. 2012 doi: 10.1038/jp.2012.7. [DOI] [PubMed] [Google Scholar]
- 11.Frey AM. Pediatric peripherally inserted central catheter program report: a summary of 4,536 catheter days. J Intraven Nurs. 1995;18(6):280–91. [PubMed] [Google Scholar]
- 12.Graham DR, Keldermans MM, Klemm LW, Semenza NJ, Shafer ML. Infectious complications among patients receiving home intravenous therapy with peripheral, central, or peripherally placed central venous catheters. Am J Med. 1991;91(3B):95S–100S. doi: 10.1016/0002-9343(91)90351-w. [DOI] [PubMed] [Google Scholar]
- 13.Harwood IR, Greene LM, Kozakowski-Koch JA, Rasor JS. New peripherally inserted midline catheter: a better alternative for intravenous antibiotic therapy in patients with cystic fibrosis. Pediatr Pulmonol. 1992;12(4):233–9. doi: 10.1002/ppul.1950120407. [DOI] [PubMed] [Google Scholar]
- 14.Racadio JM, Doellman DA, Johnson ND, Bean JA, Jacobs BR. Pediatric peripherally inserted central catheters: complication rates related to catheter tip location. Pediatrics. 2001;107(2):E28. doi: 10.1542/peds.107.2.e28. [DOI] [PubMed] [Google Scholar]
- 15.Thiagarajan RR, Bratton SL, Gettmann T, Ramamoorthy C. Efficacy of peripherally inserted central venous catheters placed in noncentral veins. Arch Pediatr Adolesc Med. 1998;152(5):436–9. doi: 10.1001/archpedi.152.5.436. [DOI] [PubMed] [Google Scholar]
- 16.Fricke BL, Racadio JM, Duckworth T, Donnelly LF, Tamer RM, Johnson ND. Placement of peripherally inserted central catheters without fluoroscopy in children: initial catheter tip position. Radiology. 2005;234(3):887–92. doi: 10.1148/radiol.2343031823. [DOI] [PubMed] [Google Scholar]
- 17.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980-1997. Pediatrics. 2000;106(1 Pt 2):205–9. [PubMed] [Google Scholar]
- 18.Milstone AM, Sengupta A. Do prolonged peripherally inserted central venous catheter dwell times increase the risk of bloodstream infection? Infect Control Hosp Epidemiol. 2010;31(11):1184–7. doi: 10.1086/656589. [DOI] [PubMed] [Google Scholar]
- 19.Sengupta A, Lehmann C, Diener-West M, Perl TM, Milstone AM. Catheter duration and risk of CLA-BSI in neonates with PICCs. Pediatrics. 2010;125(4):648–53. doi: 10.1542/peds.2009-2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwarz G. Estimating the dimension of a model. Annals of Statistics. 1978;6(2):461–4. [Google Scholar]
- 21.Efron BTR. An introduction to the bootstrap. Chapman & Hall/CRC; Boca Raton, FL: 1993. [Google Scholar]
- 22.Harrell FE, Jr., Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–87. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 23.Ihaka R GRR. R: A Language for Data Analysis and Graphics. Journal of Computational and Graphical Statistics. 1996;5(3):299–314. [Google Scholar]
- 24.Central Line-Associated Bloodstream Infection (CLABSI) Event [Accessed August 22, 2012];2012 at http://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf.
- 25.Matsuzaki A, Suminoe A, Koga Y, Hatano M, Hattori S, Hara T. Long-term use of peripherally inserted central venous catheters for cancer chemotherapy in children. Support Care Cancer. 2006;14(2):153–60. doi: 10.1007/s00520-005-0848-x. [DOI] [PubMed] [Google Scholar]
- 26.Abedin S, Kapoor G. Peripherally inserted central venous catheters are a good option for prolonged venous access in children with cancer. Pediatr Blood Cancer. 2008;51(2):251–5. doi: 10.1002/pbc.21344. [DOI] [PubMed] [Google Scholar]
- 27.Ng PK, Ault MJ, Ellrodt AG, Maldonado L. Peripherally inserted central catheters in general medicine. Mayo Clin Proc. 1997;72(3):225–33. doi: 10.4065/72.3.225. [DOI] [PubMed] [Google Scholar]
- 28.Levy I, Bendet M, Samra Z, Shalit I, Katz J. Infectious complications of peripherally inserted central venous catheters in children. Pediatr Infect Dis J. 2010;29(5):426–9. doi: 10.1097/INF.0b013e3181c94d9e. [DOI] [PubMed] [Google Scholar]
- 29.O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162–93. doi: 10.1093/cid/cir257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Di Costanzo J, Sastre B, Choux R, et al. Experimental approach to prevention of catheter-related central venous thrombosis. JPEN J Parenter Enteral Nutr. 1984;8(3):293–7. doi: 10.1177/0148607184008003293. [DOI] [PubMed] [Google Scholar]
- 31.Chathas MK, Paton JB, Fisher DE. Percutaneous central venous catheterization. Three years’ experience in a neonatal intensive care unit. Am J Dis Child (1960) 1990;144(11):1246–50. doi: 10.1001/archpedi.1990.02150350078030. [DOI] [PubMed] [Google Scholar]
- 32.Ruebner R, Keren R, Coffin S, Chu J, Horn D, Zaoutis TE. Complications of central venous catheters used for the treatment of acute hematogenous osteomyelitis. Pediatrics. 2006;117(4):1210–5. doi: 10.1542/peds.2005-1465. [DOI] [PubMed] [Google Scholar]
- 33.Chwals WJ. Vascular access for home intravenous therapy in children. JPEN J Parenter Enteral Nutr. 2006;30(1 Suppl):S65–9. doi: 10.1177/01486071060300S1S65. [DOI] [PubMed] [Google Scholar]
- 34.Miller MR, Griswold M, Harris JM, 2nd, et al. Decreasing PICU catheter-associated bloodstream infections: NACHRI’s quality transformation efforts. Pediatrics. 2010;125(2):206–13. doi: 10.1542/peds.2009-1382. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.