Abstract
Many Proteobacteria use acyl-homoserine lactone-mediated quorum-sensing (QS) to activate specific sets of genes as a function of cell density. QS often controls the virulence of pathogenic species, and in fact a previous study indicated that QS was important for Burkholderia mallei mouse lung infections. To gain in-depth information on the role of QS in B. mallei virulence, we constructed and characterized a mutant of B. mallei strain GB8 that was unable to make acyl-homoserine lactones. The QS mutant showed virulence equal to that of its wild-type parent in an aerosol mouse infection model, and growth in macrophages was indistinguishable from that of the parent strain. Furthermore, we assessed the role of QS in B. mallei ATCC 23344 by constructing and characterizing a mutant strain producing AiiA, a lactonase enzyme that degrades acyl-homoserine lactones. Although acyl-homoserine lactone levels in cultures of this strain are very low, it showed full virulence. Contrary to the previous report, we conclude that QS is not required for acute B. mallei infections of mice. QS may be involved in some stage of chronic infections in the natural host of horses, or the QS genes may be remnants of the QS network in B. pseudomallei from which this host-adapted pathogen evolved.
INTRODUCTION
Burkholderia mallei, the causative agent of the equine disease glanders, is a member of the class Betaproteobacteria. It infrequently infects humans and other mammals in areas where equine disease is endemic (including regions in the Middle East and Asia) (1–3). B. mallei is classified as a category B priority pathogen by the Centers for Disease Control and Prevention because human disease is severe, the species is highly infectious by aerosol delivery, and options for disease prevention and treatment are limited (http://www.bt.cdc.gov/agent/agentlist-category.asp). Furthermore, B. mallei was deployed as a bioweapon during World Wars I and II, was weaponized by multiple countries until 1972 (4, 5), and remains a potential agent of bioterrorism (4). Despite the documented virulence of B. mallei, little is known about the mechanisms of bacterial colonization and pathogenesis that lead to disease progression. B. mallei is a host-restricted pathogen that is closely related to the nonpathogenic saprophyte Burkholderia thailandensis and the opportunistic human pathogen Burkholderia pseudomallei, which causes the emerging infectious disease of melioidosis (6). B. thailandensis and B. pseudomallei have been isolated from soils and waters in regions of endemicity in Southeast Asia and Northern Australia (7–10). B. mallei, however, has only been isolated from infected animals. These three species represent a unique situation where closely related bacteria occupy diverse and divergent niches.
Our particular focus is on the role of acyl-homoserine lactone (AHL) quorum sensing (QS) in Proteobacteria during microbial adaptations to changing environments. AHL QS allows cells of a bacterial species to assess population density and execute group activities when diffusible AHL signals reach a critical concentration (11). AHL QS was first described as a system for transcriptional activation of luminescence genes in the marine bacterium Vibrio fischeri. This luminescent bacterium possesses luxI, which codes for an enzyme that synthesizes 3-oxo-C6-homoserine lactone (3OC6-HSL), as well as luxR, which codes for a 3OC6-HSL-dependent activator of luminescence gene transcription (12). V. fischeri has a dual lifestyle; it lives freely in seawater at low densities and can also colonize light organs of certain marine animals at high population densities. QS allows V. fischeri to discriminate between its low-population-density seawater habitat and the high-population-density, light-organ habitat. AHL quorum sensing is most commonly viewed as a means to allow bacteria to discern a low-density, free-living lifestyle from a higher-density, host-associated lifestyle (12, 13).
We are particularly interested in B. mallei because it is a rare example of a host-restricted pathogen with a functional AHL QS system (1, 14, 15). There is no apparent free-living lifestyle. The genome of B. mallei contains two sets of linked luxI-luxR homologs, bmaI1-bmaR1 and bmaI3-bmaR3, and two additional luxR-like genes called bmaR4 and bmaR5 (15). The bmaI1 gene product is an octanoyl-homoserine lactone (C8-HSL) synthase, and bmaI3 codes for a 3-hydroxy-octanoyl-HSL (3OHC8-HSL) synthase (14–16). Previously, it was reported that a number of B. mallei AHL QS mutants showed a strong virulence attenuation phenotype in mouse and hamster models of acute infection (15). This publication encouraged us to think it might be possible to develop anti-QS therapeutic approaches for B. mallei infections and to better understand the role of QS in an acute infection. Here, we present several lines of evidence that QS is not required for acute B. mallei disease in mice, and we discuss possible explanations for maintenance of a functional quorum-sensing circuit in light of these findings.
MATERIALS AND METHODS
Bacterial strains, plasmids, and growth conditions.
Bacteria and plasmids used in this study are listed in Table 1. Escherichia coli was grown in low-salt Luria-Bertani (LB) broth (10 g of tryptone, 5 g of yeast extract, 5 g of NaCl per liter), and B. mallei was grown in low-salt LB broth supplemented with 4% glycerol and 50 mM morpholinepropanesulfonic acid (MOPS), pH 7.0. Antibiotics were used where appropriate at the following concentrations for E. coli: gentamicin (Gm), 20 μg/ml; kanamycin (Km), 35 μg/ml; zeocin (Zeo) 25 μg/ml. For B. mallei, we used Km (5 μg/ml) and Zeo (25 μg/ml). Diaminopimelic acid (DAP; Sigma) was added (400 μg/ml) when needed. All experiments with live B. mallei bacteria were performed in a class II biological safety cabinet housed in a biological safety level 3 (BSL-3)-enhanced laboratory.
Table 1.
Bacterial strains and plasmids and PCR primers
| Strain, plasmid, or primer | Relevant characteristics or sequencea | Source or reference |
|---|---|---|
| E. coli strains | ||
| DH10B | Invitrogen | |
| RH03 | SM10(λpir) Δasd::FRT ΔaphA::FRT | 17 |
| B. mallei strains | ||
| GB8 | Derived by passage of ATCC 23344 in horse | D. Woods |
| ATCC 23344 | Human isolate | 6 |
| CM8 | GB8 ΔbmaI1 | This study |
| CM9 | GB8 ΔbmaI3 | This study |
| CM38 | GB8 ΔbmaI1 ΔbmaI3 | This study |
| CM3 | GB8 with MCS-luxCDABE fusion-ble; Zeor | This study |
| CM4 | GB8 with PbmaI1-luxCDABE fusion-ble; Zeor | This study |
| CM11 | GB8 with PbmaI3 -luxCDABE fusion-ble; Zeor | This study |
| CM31 | ATCC 23344 with S12 ribosomal protein promoter-aiiA fusion construct; Zeor | This study |
| Plasmids | ||
| pBADSce | Zeor | 17 |
| pEXKm5 | sacB plasmid; Kmr | 17 |
| pTNS2 | R6K replicon TnsABC+D expression vector | 18 |
| pUC18-mini-Tn7T-Gm-lux | Gmr on mini-Tn7T; luxCDABE transcriptional fusion vector; Apr, Gmr | 18 |
| pCM53 | pUC18-mini-Tn7T-luxCDABE-ble; luxCDABE transcriptional fusion vector; Zeor, Apr | This study |
| pBD4 | pJN105 derivative with bmaR1; Gmr | 14 |
| pBD5 | pQF50 with bmaI1 promoter; Apr | 14 |
| pBD7 | pQF50 with bmaI3 promoter; Apr | B. Duerkop |
| pCM56 | pUC18-mini-Tn7T-pbmaI1-luxCDABE-ble; Zeor | This study |
| pCM66 | pUC18-mini-Tn7T-pbmaI3-luxCDABE-ble; Zeor | This study |
| pUC18T-mini-Tn7T-Zeo-FRT | Zeor on mini-Tn7T; Zeor, Apr | 19 |
| pCM112 | pUC18T-mini-Tn7T-ble-pS12; Zeor, Apr | This study |
| pAD123::aiiA | pAD123 containing aiiA from B. cereus ATCC 14579 | S. B. Peterson |
| pCM117 | pUC18T-mini-Tn7T-ble-pS12-aiiA; Zeor, Apr | This study |
| pCM02 | bmaI1 deletion plasmid for making unmarked bmaI1 deletions; Kmr | This study |
| pCM03 | bmaI3 deletion plasmid for making unmarked bmaI3 deletions; Kmr | This study |
| pJNR2 | pJN105 with btaR2; Gmr | 20 |
| pI2P50 | pQF50 containing the btaI2 promoter; Apr | 20 |
| Primers | ||
| bmaI1-A | ATCACCCGGGCGATCATGTTCGAGCTGAGCGC | This study |
| bmaI1-B | CAGCAGCGGGTCGAGATCGAGGAAAGTTCGCATGTCGTCCTCGTG | This study |
| bmaI1-C | AGGACGACATGCGAACTTTCCTCGATCTCGACCCGCTGCTGTGC | This study |
| bmaI1-D | TGATGCGGCCGCAGGAGAACGAGCGCTATATCCGCA | This study |
| bmaI3-A | ATCACCCGGGCTCAACGCGAATATCGAACAG | This study |
| bmaI3-B | AAACGACAAGACGCGTGTCTGCTTGGTTCTCCGATG | This study |
| bmaI3-C | ATCCATCGGAGAACCAAGCAGACACGCGTCTTGTCG | This study |
| bmaI3-D | AATCTAGAATTCATCACGTCGAGCGATTCTTC | This study |
| S12 prom-A | GATCGAGCTGTTGACTCGCTTGGGATTTTCGGAATATCATGCCGGGTGTGCA | This study |
| S12 prom-B | CACCCGGCATGATATTCCGAAAATCCCAAGCGAGTCAACAGCTC | This study |
Endonuclease restriction sites are underlined.
Construction of B. mallei mutants.
We used standard molecular biology procedures with E. coli DH10B as a cloning vehicle. The bmaI1 (BMAA1347) and bmaI3 (BMAA1577) deletions were constructed by using a strategy based on the dual-plasmid method of Lopez et al. for B. pseudomallei (17). To create the gene deletion vectors, we used overlap extension PCR to generate approximately 1,000 bp of DNA flanking each gene with genomic DNA (gDNA) from B. mallei ATCC 23344 as the template. The flanking sequences were annealed together and PCR amplified to generate each deletion construct. Primers used in cloning are listed in Table 1 and include two sets of four primers for the bmaI1 and bmaI3 deletion constructs, bmaI1-A-D and bmaI3-A-D, respectively. Primer-encoded restriction sites were introduced into the ends of the PCR products during amplification. The bmaI1 deletion construct and pEXKm5 were digested with NotI and SmaI to yield pCM02 following ligation. The bmaI3 deletion construct and pEXKm5 were digested with SmaI and EcoRI and ligated to yield pCM03 following ligation.
The bmaI1 or bmaI3 deletion vector pCM02 or pCM03 was used to transform E. coli RHO3, which was used for mating with B. mallei to create the unmarked B. mallei bmaI1 and bmaI3 mutants. For matings, we mixed equal volumes of overnight cultures of B. mallei GB8 and E. coli RHO3 with either pCM02 or pCM03 and plated the mixtures on low-salt LB agar with DAP. After 10 to 16 h at 37°C, cells were scraped from plates and suspended in 1 ml of low-salt LB broth. The suspended cells were pelleted by centrifugation, washed in 1 ml of low-salt LB broth, and suspended in 300 μl of low-salt LB broth. Cells from the 300-μl suspension were serially diluted and plated on low-salt LB agar containing Km. After 24 h at 37°C, single colonies were picked as candidate merodiploids. Candidate merodiploids were grown in low-salt LB broth for 10 to 16 h at 37°C and then transformed with pBADSce as follows. Nine milliliters of culture was pelleted by centrifugation, washed with 9 ml of 300 mM sucrose, pelleted, washed with an additional 6 ml of 300 mM sucrose, and centrifuged, and the pellet was suspended in 100 μl of 300 mM sucrose. The sucrose-suspended cells were then electrotransformed with 0.5 to 1 μg of pBADSce. The transformation mixture was suspended in 1 ml of low-salt LB broth, grown for 1 to 3 h at 30°C, and then plated on low-salt LB agar plus Zeo. Plates were incubated for 5 days at 30°C, after which colonies were picked and patched on low-salt LB agar and low-salt LB agar plus Km. We screened for Km-sensitive B. mallei isolates and confirmed unmarked gene deletions by DNA sequencing. We cured the mutants of pBADSce by growth at 37°C. As a confirmation of plasmid curing, we showed that the mutants were Zeo sensitive. The double bmaI1 bmaI3 mutant was generated by introducing the bmaI1 mutation into a confirmed bmaI3 mutant B. mallei strain, as described above.
The chromosomal bmaI1 promoter-lux and bmaI3 promoter-lux fusions were generated by exploiting a mini-Tn7 tool previously used with B. mallei (21). To generate fusion plasmids, the Gm resistance gene was removed from pUC18-mini-Tn7T-Gm-lux by digestion with EagI and SpeI. The vector was then Klenow treated to create blunt ends and self-ligated. The resulting plasmid was digested with KpnI, blunt ended with the Klenow fragment, and ligated with the ble gene (Zeor) fragment from pBADSce that had been treated with PmII, Klenow, and NotI. The resulting plasmid, pCM53, is essentially pUC18 with a mini-Tn7T-MCS-luxCDABE-ble insert (where MCS is multiple-cloning site). We found this gene organization necessary to achieve low-background luminescence. For construction of the bmaI1 promoter-luxCDABE fusion vector (pCM56), we isolated a bmaI1 promoter from pBD5 following treatment with EcoRI, Klenow, and then BglII. The vector, pCM53, was cut with PstI, Klenow treated, and then digested with BamHI. The bmaI1 promoter and the cut vector were ligated to yield pCM56. The plasmids were used to transform E. coli DH10B for maintenance and purification. To create the bmaI3 promoter fusion construct, the bmaI3 promoter from pBD7 was isolated following treatment with HindIII, Klenow, and then BglII. The vector, pCM53, was prepared as described above. The bmaI3 promoter fragment and cut vector were then ligated together to generate pCM66. For each fusion, DNA sequencing confirmed that the promoter was driving luxCDABE expression.
The bmaI1 promoter-lux and bmaI3 promoter-lux fusions on pCM56 and pCM66 were inserted in the B. mallei GB8 chromosomal Tn7 attachment site (attTn7) site downstream of glmS1 by electroporation together with pTNS2 essentially as described above to yield B. mallei strains CM4 and CM11, respectively. Transformants were selected as Zeor colonies. The resulting colonies were screened for insertion in either glmS1 or glmS2 by PCR. Isolates with a single insertion downstream of glmS1 were used for our subsequent studies. The promoterless fusion construct on pCM53 was also introduced into the chromosome in this way to yield B. mallei strain CM3.
The AHL-lactonase producing B. mallei ATCC 23344 derivative CM31 was constructed by introducing the S12 ribosomal protein promoter-driven B. cereus aiiA gene into the attTn7 site by coelectrotransformation with pCM117 and pTNS2, as described above. To construct pCM117, the S12 ribosomal protein promoter was introduced into pUC18T-mini-Tn7T-Zeo-FRT (where FRT is Flp recognition target). The S12 ribosomal protein promoter was prepared by using previously described methods (22). Briefly, the oligonucleotide S12 prom-A was annealed with a complementary oligonucleotide, S12 prom-B. The annealed oligonucleotides comprise a short double-stranded fragment encoding the S12 ribosomal protein promoter flanked by BamHI and PstI sticky ends. This promoter fragment was then treated with T4 polynucleotide kinase and was ligated to BamHI- and PstI-cut pUC18T-mini-Tn7T-Zeo-FRT to create pCM112. Then, the Bacillus cereus ATCC 14579 AHL lactonase gene was inserted immediately downstream of the S12 ribosomal protein promoter to generate pCM117. Briefly, a lactonase gene (aiiA) fragment was purified from aiiA::pAD123 following digestion with XbaI and EcoRI. The aiiA fragment was then treated with Klenow for blunt-end ligation with pCM112, which had been cut with EcoRI and also Klenow treated. DNA sequencing confirmed the orientation of the aiiA gene and the S12 promoter. The ligation product was pCM117.
In vitro luminescence measurements.
B. mallei colonies from a low-salt LB agar plate were used to inoculate a 3-ml culture of low-salt LB medium. This culture and four additional 3-ml cultures with successive 100-fold dilutions of the initial inoculum were incubated overnight with shaking at 37°C. The next day, flasks were selected that contained cultures with an optical density at 600 nm (OD600) below 0.5 and were used to inoculate a fresh low-salt LB culture at the desired optical density at OD600, maintaining a flask-to-volume ratio of 1:10. The OD600 and luminescence were measured throughout growth with aeration.
To assess activity of promoters fused to the Photorhabdus luminescens luxCDABE in B. mallei, we diluted cultures into fresh low-salt LB broth in wells of a 96-well plate, aerated the cells, and measured luminescence by using a SpectraMax M3 reader. We normalized the luminescence values as relative light units (RLU) per 100 μl of culture.
Measurements of C8-HSL and 3OHC8-HSL in B. mallei cultures.
To measure AHLs in stationary B. mallei cultures, we twice extracted 20 ml of an overnight culture with acidified ethyl acetate and dried the extract under a stream of N2 gas. The extract was dissolved in 1 ml of acidified ethyl acetate. We used a previously described bioassay to measure C8-HSL in the ethyl acetate concentrate. The reporter in this assay was E. coli(pBD4, pBD5) (14). We generated a standard curve by using synthetic C8-l-HSL (Sigma Chemical Co.). We measured 3OHC8-HSL as follows. We dried 500 μl of the ethyl acetate concentrates and dissolved the dried material in 50 μl 50% methanol. The methanol solution was separated by C18 reverse-phase high-performance liquid chromatography (HPLC), and fractions in which 3OHC8-HSL eluted were collected and pooled. We measured 3OHC8-HSL in the pooled fractions by a previously described bioassay that makes use of E. coli(pJNR, pI2P50) (20). We determined the 3OHC8-HSL HPLC elution profile and prepared standard curves for the bioassay by using 3OHC8-l-HSL synthesized as described below.
Synthesis of 3OHC8-HSL.
We prepared 3OHC8-l-HSL by coupling (R/S)-3-hydroxyoctanoic acid with l-homoserine lactone hydrobromide according to published protocols (23). (R/S)-3-hydroxyoctanoic acid was prepared by alkaline hydrolysis of the product from the Reformatsky coupling of methyl bromoacetate and hexanal (24).
Cell culture and mouse infection assays.
Murine macrophage-like RAW 264.7 cells were grown in Dulbecco's modified Eagle's medium (DMEM; HyClone) containing 4.5 mg/ml glucose, 0.1 mg/ml sodium pyruvate, 4 mM l-glutamine, and 10% fetal bovine serum (FBS; Sigma) and incubated at 37°C with 5% CO2. For infection studies, cells were seeded at 2.5 × 105 cells/cm2 in 24-well tissue culture plates 12 to 24 h prior to infection. The monolayers were infected at a multiplicity of infection (MOI) of 0.1. Immediately after bacteria were added, the plates were centrifuged for 5 min at 500 × g, and this was followed by incubation for 1 h at 37°C. The RAW 264.7 cells were then washed with Dulbecco's phosphate-buffered saline (DPBS; HyClone) to remove extracellular bacteria. To measure invasion, the monolayer cells were lysed by treatment with 0.2% Triton X-100 in DPBS for 5 min. Bacterial cell counts in the lysis solution were determined by plating and are reported as numbers of CFU. To measure bacterial replication, RAW 264.7 cells were infected as described above except that we added DMEM containing Km (250 μg/ml) to the monolayers following the DPBS wash. The infected cell layers were incubated for 20 h prior to lysis and bacterial cell counting. As a control to confirm the absence of extracellular bacterial cells, we plated 50 to 100 μl of DMEM over the cell layers at 20 h of incubation and found no CFU.
The B. mallei inocula for RAW 264.7 cell infections were prepared as follows. Starter cultures were inoculated from growth on a fresh agar plate into low-salt LB broth containing 4% glycerol and 50 mM MOPS, pH 7.0. After 6 to 8 h at 37°C, starter cultures were used to inoculate low-salt LB broth containing 4% glycerol and 50 mM MOPS, pH 7.0, so that the optical density at 600 nm at the time of inoculation was 0.01. Cultures were grown for 10 to 16 h, diluted in DPBS, and used to infect RAW 264.7 cells as described above.
Animal infection experiments were with 6- to 8-week-old female BALB/c mice (Charles River Laboratories, Wilmington, MA). Mice were housed under specific-pathogen-free conditions. All mouse experiments were approved by the Institutional Animal Care and Use Committee of the University of Washington. The AeroMP (Biaera Technologies, Fredericksburg, MD) aerosol management platform was used to deliver B. mallei to mice. All components of the AeroMP, except air pump, vacuum, desiccator, electronics interface box, and computer, were housed inside a class II biological safety cabinet. Mice were exposed to aerosols generated from 10-ml 10 mM phosphate-buffered (pH 7.0) B. mallei suspensions by using a Hi-Flo MiniHeart nebulizer (WestMed, Inc., Tucson, AZ) running at 15 liters/min (generator, 5.4 liters/min; dilution, 9.6 liters/min) and delivered to mice in a whole-body exposure chamber at ambient temperature and pressure. To measure deposition, one mouse per infection group was sacrificed, and the lungs were removed and homogenized in 2 ml of 10 mM phosphate buffer (pH 7.0) in gentle MACS C tubes (Mitenyi Biotech, Inc.). The homogenate was serially diluted, and CFU numbers were determined by plate counting. Following exposure, mice were observed for the development of symptoms of lethal glanders disease including weight loss, hypothermia, piloerection, forced ventilation, ocular discharge, impaired mobility, and altered physical behaviors. Mice that manifested symptoms of imminent death were euthanized with pentobarbital (intraperitoneal injection, 200 mg/kg).
Bacterial suspensions for mouse infections were prepared as follows. Bacteria from a fresh agar plate were used to inoculate 25 ml of low-salt LB broth containing 4% glycerol and 50 mM MOPS, pH 7.0, in a 125-ml baffled flask. After growth for 12 to 16 h at 37°C with shaking at 225 rpm, cells were pelleted by centrifugation, suspended in 3 ml of low-salt LB broth containing 15% glycerol, and frozen in 0.75-ml aliquots at −80°C. On the day of an animal infection, an aliquot was thawed and used to prepare aerosol suspensions.
In vivo luminescent images were acquired following mouse infection with luminescent bacteria, essentially as described above. Following exposure to bacteria, mice were imaged by an IVIS Spectrum in vivo imaging system and analyzed with the Living Image software program (PerkinElmer, CA) once every other day. For luminescent imaging, the system acquires a photograph and a luminescence image simultaneously and automatically generates an overlay image with a scale bar. Before in vivo imaging, mice were anesthetized with 3% isoflurane in an oxygen-filled chamber. Once anesthetized, mice were transferred to a sealable optically clear visualization chamber (PerkinElmer, CA); the chamber was then connected to a continuous supply of isoflurane, and the mice were imaged.
RESULTS
Characterization of B. mallei GB8 quorum-sensing signal synthesis mutants.
We are interested in understanding the role of QS in the biology of the host-adapted pathogen B. mallei. The mutants used in the previous study of QS and virulence of B. mallei (15) no longer exist. Several years after the initial description of these mutants (15), the antibiotic marker used to disrupt the QS genes was disallowed for use. U.S. government authorities asked the authors of the previous publication to destroy their constructs, and they complied. We constructed QS mutant strains containing unmarked deletions of the AHL synthase genes bmaI1, bmaI3, or both bmaI1 and bmaI3 by adapting a method recently developed by Lopez et al. (17) for generating mutations in the closely related B. pseudomallei, as described in Materials and Methods. We used B. mallei GB8, which was isolated from a horse infected with the sequenced strain ATCC 23344 (Don Woods, personal communication).
We measured AHLs in stationary-phase cultures of the parent and the three QS mutants (Table 2). The wild-type B. mallei GB8 produced much more of the BmaI1 signal (C8-HSL) than the BmaI3 signal (3OHC8-HSL). The bmaI1 mutant (CM8) did not produce detectable levels of either AHL. The bmaI3 mutant (CM9) produced wild-type levels of C8-HSL, but it did not produce detectable levels of 3OHC8-HSL. These data are consistent with the idea that BmaI1 is required for C8-HSL and that C8-HSL is required for activation of bmaI3. BmaI3 is required for 3OHC8-HSL production, but this does not influence C8-HSL production. Finally, as expected, the double bmaI1 bmaI3 mutant (CM38) did not produce detectable levels of either AHL.
Table 2.
AHL levels in stationary phase B. mallei cultures
| Strain | Mean concn (nM [range])a |
|
|---|---|---|
| C8-HSL | 3OH C8-HSL | |
| GB8 (wild type) | 158 (±89) | 5.2 (±0.4) |
| CM8 (BmaI1−) | ≤1 | ≤1 |
| CM9 (BmaI3−) | 207 (±25) | ≤1 |
| CM38 (BmaI1− BmaI3−) | ≤1 | ≤1 |
| ATCC 23344 (wild type) | 294 (±170) | 3.5 (±0.4) |
| CM31 (ATCC 23344 aiiA) | 6 (±4) | ≤1 |
Values are the means from at least two independent biological replicates.
Expression of bmaI1 and bmaI3 during B. mallei growth.
We sought to better understand the relationship between culture density, bmaI1 and bmaI3 expression, and AHL accumulation. To do this, we employed strains CM4 and CM11 (Table 1), which contain a lux operon fusion to either the bmaI1 or bmaI3 promoter at a neutral site in the B. mallei chromosome. Growth, promoter activity, and AHL accumulation of each strain were monitored (Fig. 1). Both bmaI1 promoter activity and the product of BmaI1 (C8-HSL) showed a rapid rise starting in late logarithmic phase. We could not detect bmaI3 promoter activity, and we were able to detect the product of BmaI3 (3OHC8-HSL) only when the culture was in late stationary phase following overnight growth (Fig. 1 and data not shown). At least under the conditions of our experiments, both the BmaI1 and BmaI3 proteins are functional, but bmaI1 is expressed at much higher levels than bmaI3. Furthermore, the BmaI3-BmaR3 system appears to depend on the BmaI1-BmaR1 system (Table 2).
Fig 1.
B. mallei bmaI1 and bmaI3 promoter activity and AHL production. (A) Luminescence (RLU, relative light units) was monitored during growth of B. mallei cells containing a bmaI1 promoter-lux fusion in a neutral site on the chromosome (strain CM4; squares) or a bmaI3 promoter-lux fusion at a neutral site (strain CM11; triangles). A strain containing a promoterless lux cassette at the same neutral site (CM3; circles) was used as a control. (B) C8-HSL concentrations during growth of strain CM4. Cell density was measured as optical density at 600 nm (OD600). We did not detect 3OHC8-HSL in strain CM11 during exponential and early-stationary-phase growth (data not shown). The data for each strain are from three separate cultures, which were started at different densities (OD600 of 0.01, 0.05, or 0.1). The BSL-3 requirement necessitated this approach to capture entire growth curves (stationary phase commences at a density of >2) within 10 h.
B. mallei GB8 QS mutants are virulent.
It was previously reported that virulence of B. mallei QS mutants is severely attenuated in an aerosol mouse infection (15). We asked whether virulence was attenuated in our unmarked QS deletion mutants. B. mallei is a facultative intracellular pathogen (25). As is the case for several intracellular pathogens, the ability to replicate inside host cells has been linked to virulence. For this reason, tissue culture infection in macrophages can serve as a proxy to identify virulence factors. Thus, we began by following the growth of B. mallei GB8 and its unmarked QS deletion mutants in macrophage-like RAW 264.7 cells (Fig. 2). To our surprise, intracellular replication levels of wild-type B. mallei GB8 and the QS mutants were indistinguishable.
Fig 2.
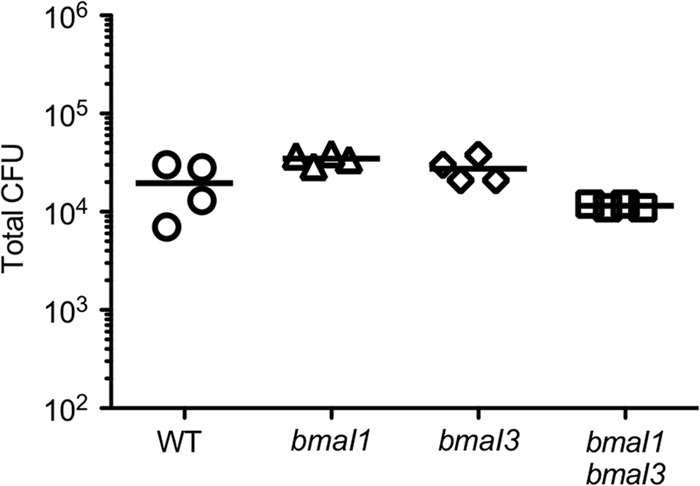
Replication of wild-type B. mallei and B. mallei AHL synthesis mutants in RAW 264.7 macrophage-like cells. Monolayers were infected with the wild-type (WT) GB8, the bmaI1 mutant (CM8), the bmaI3 mutant (CM9), or the double bmaI1 bmaI3 mutant (CM38) at an MOI of 0.1. The AHL synthesis mutations did not influence initial attachment (data not shown). The amount of intracellular bacteria harvested from RAW 264.7 cells after 20 h is shown as total CFU count.
It could be that the connection between QS and virulence reported previously involved a step that was independent of macrophage growth or that we were unable to uncover the QS mutant phenotype during this in vitro infection assay for other reasons. Therefore, we also used a mouse aerosol infection model similar to that described in the previous publication on QS and virulence in B. mallei (15). With this whole-body aerosol infection model, we estimated the 50% lethal dose (LD50) of wild-type GB8 to be between 5,000 to 10,000 CFU (Fig. 3B). The LD50 of wild-type GB8 is modestly higher than the reported LD50 of wild-type ATCC 23344 (1,000 CFU) by aerosol delivery (26). When we tested wild-type GB8 or its QS null strain (CM38) at a dose slightly above the determined LD50 (20,000 CFU), all mice succumbed to infection within 1 week (Fig. 3A). Similarly, we observed comparable survival kinetics of wild-type GB8 and the single bmaI1 or bmaI3 mutant (CM8 or CM9) at doses near the LD50 (Fig. 3B). In some instances, mice infected with either the single bmaI1 or bmaI3 mutant showed decreased survival relative to mice infected with the isogenic wild-type strain (Fig. 3B). These results suggest that the QS mutants might be slightly more virulent than the wild type. Alternatively, the small differences may represent inherent variability that occurs at doses around the LD50. It is clear from these experiments that all QS mutants of strain GB8 are virulent, indicating that in our horse-passaged derivative of B. mallei ATCC 23344, quorum sensing is not critical for virulence during acute disease in mouse aerosol infections.
Fig 3.
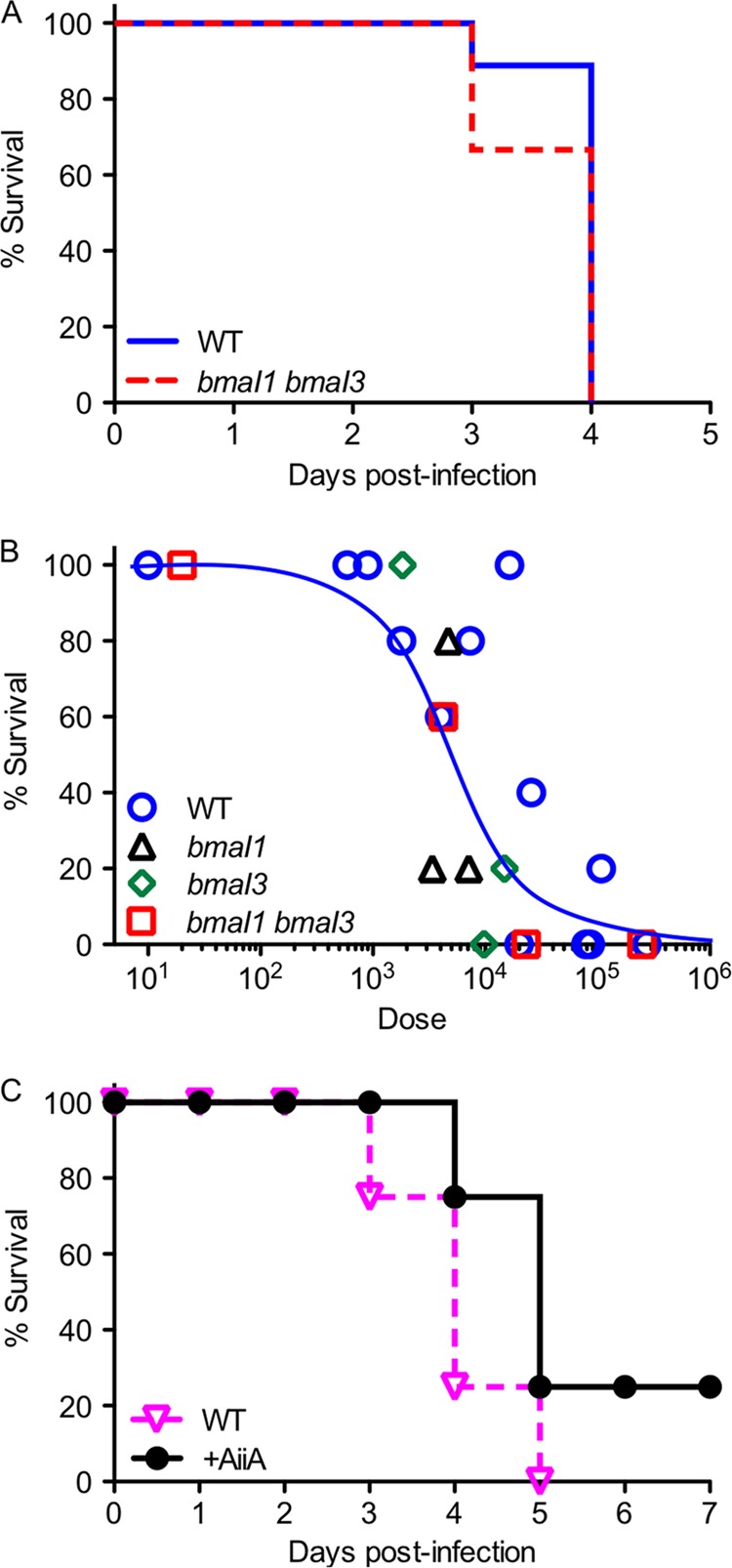
Mouse survival after B. mallei infection. (A) Mice were infected by aerosol delivery of wild-type (WT) GB8 or the double bmaI1 bmaI3 mutant CM38. Results are from two independent experiments. The data were plotted using GraphPad Prism software, which generated survival fraction calculations (Kaplan-Meier limit method) and analyzed the data (log rank Mantel-Cox test). By this analysis the wild-type and mutant results are not statistically different. The initial doses for each replicate of WT GB8 were 20,000 CFU and 79,000 CFU, and the doses of CM38 were 24,800 CFU and 20,000 CFU. (B) Mouse survival was monitored for 1 week following aerosol infection with increasing doses of wild-type GB8 B. mallei (WT), the bmaI1 mutant CM8, the bmaI3 mutant CM9, or the double bmaI1 bmaI3 mutant CM38. Each data point represents one exposure group from independent experiments consisting of at least four mice. (C) Mice were infected with wild-type B. mallei ATCC 23344 (WT) or ATCC 23344 producing the AHL lactonase AiiA CM31 (+AiiA). Initial doses were 2,184 CFU and 1,416 CFU for ATCC 23344 and CM31, respectively. The results shown are from one experiment. In a second similar experiment, all infected mice experienced comparable signs of acute disease through day 4 postinfection, after which the mice were euthanized. For most experiments each infection group consisted of five mice. Some of the groups in Fig. 3B consisted of four mice. Initial doses were measured as deposition (see Materials and Methods).
Perhaps the discrepancy between our experiments and the prior finding that quorum sensing is required for virulence of B. mallei ATCC 23344 reflects bacterial strain differences. Although the original study used strain ATCC 23344, we utilized a derivative of that strain, which was passed through a horse (GB8). The B. mallei genome is unstable and plastic, and it has been shown that passage of B. mallei through animals can result in genetic changes (27). Therefore, we sought to study strain ATCC 23344 itself. For unknown reasons, we found it difficult to construct QS mutants of strain ATCC 23344. Thus, we developed a different strategy to create an AHL-negative ATTC 23344 strain. We constructed a B. mallei ATCC 23344 derivative, which carries the B. cereus AHL lactonase gene aiiA driven by a strong promoter (CM31). We measured AHLs in stationary-phase cultures of strain CM31 and found that C8-HSL was about 2% of the level seen in the wild-type ATCC 23344. We could not detect any 3OHC8-HSL (Table 2). We found that virulence of the AHL lactonase-expressing strain CM31 was comparable to its parent ATCC 23344 in the murine infection model (Fig. 3C).
Is QS active during infection?
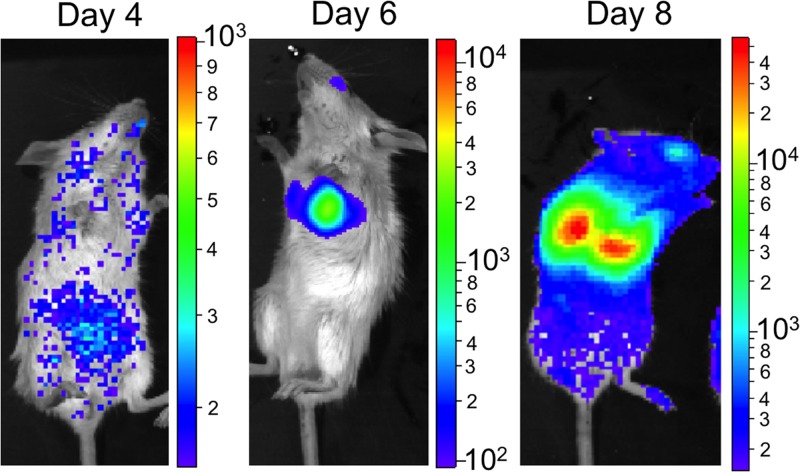
Apparently, quorum sensing is not required for acute B. mallei murine aerosol infections. Our evidence indicates that during in vitro growth of B. mallei, bmaI1 is expressed in late logarithmic phase, and bmaI3 is expressed in stationary phase and then only poorly. These genes may or may not be expressed during an acute infection. We sought to evaluate if the strongly QS-activated bmaI1 promoter was induced in the mouse during infection. To assess bmaI1 expression, we infected mice with the luminescent bmaI1 promoter fusion strain CM4. We followed bmaI1 expression by monitoring luminescence in whole animals (Fig. 4). Strong luminescence appeared in the lungs of mice infected with strain CM4 at the time that an individual showed marked signs of acute disease (most notably respiratory distress, reduced mobility, ocular discharge, and decreased body temperature). Thus, though bmaI1 is not required for B. mallei disease in this animal model, the BmaI1-BmaR1 system is active at least after the disease has progressed.
Fig 4.
In vivo imaging of bmaI1 activity during acute murine glanders. Mice were infected with 3,900 CFU of B. mallei strain CM4 with a bmaI1 promoter-lux fusion. Infected mice were imaged using an in vivo imaging system (see Materials and Methods). Luminescence is shown from a single CM4-infected mouse on days 4, 6, and 8 following infection. On day 8, the mouse was moribund and was euthanized following imaging. Note that the luminescence scale bar for each image is different.
DISCUSSION
To probe the role of QS in B. mallei pathogenesis, we constructed mutants of the horse-passaged strain GB8 with clean, unmarked deletions in the two AHL QS signal synthase genes. As expected, a double bmaI1 bmaI3 mutant does not produce AHLs. The bmaI3 mutant does not produce the BmaI3 signal (3OHC8-HSL), but it does produce the BmaI1 signal (C8-HSL). The bmaI mutant does not produce detectable levels of either AHL: it behaves like the double mutant. We interpret this result to mean that the BmaI1-BmaR1 quorum-sensing circuit is required for activation of bmaI3 expression. This sort of hierarchical quorum-sensing circuitry has been well established in the case of Pseudomonas aeruginosa, where the LasR-LasI QS circuit is required to activate a battery of genes including a second QS circuit, RhlR-RhlI (28, 29).
Substantial amounts of the BmaI1 signal C8-HSL are produced by both of the wild-type B. mallei strains we examined, GB8 and ATCC 23344. Much lower levels of the BmaI3 product 3OHC8-HSL are produced by the wild-type strains, and 3OHC8-HSL is not detected until cultures reach late stationary phase (Fig. 1 and Table 2). We note that measured levels of 3OHC8-HSL are low, in the range of 5 nM compared to levels of 150 to 300 nM of C8-HSL. Two recently discovered QS systems are fully functional at signal levels even lower than those we measured for 3OHC8-HSL. In certain species of Bradyrhizobium, signal concentrations in cultures reach about 5 to 10 nM, and these concentrations are in considerable excess with responses saturating at signal concentrations on the order of 10 pM (30, 31).
We assessed the impact of all three of our B. mallei quorum-sensing mutants on growth in macrophage-like cells and on virulence in an acute murine infection (Fig. 2 and 3). QS did not appear to have any significant influence on B. mallei pathogenesis in either of these infection models. This result was surprising for three reasons. First and foremost, a previous report provided evidence that both the BmaI1-BmaR1 and BmaI3-BmaR3 systems were key virulence determinants (15). We used infection parameters nearly identical to those previously employed, including a similar infectious dose and aerosol delivery method. Second, QS has been previously linked to virulence in the related opportunistic pathogen B. pseudomallei; three independent studies examined the role of C8-HSL QS in a total of five infection models using three different parent and mutant strains (32–34). In each case, the mutants were attenuated. In one of these studies, mutants defective in the 3OHC8-HSL QS system were also attenuated (34). Thus, it seems that QS in the opportunistic pathogen B. pseudomallei is relevant in acute disease. We were surprised when the same did not appear to be true for B. mallei. Third, evidence indicates that B. mallei evolved from a clone of B. pseudomallei and that it has undergone expansive genetic loss and pseudogene acquisition, with a reduction of about 20% of its ancestral genome (approximately 1.4 Mb of DNA). Genome erosion is one factor that defines B. mallei as a host-restricted pathogen equipped for life and persistence in an animal reservoir. It is believed that genes likely important for saprophytic survival and unwanted immunogenicity were inactivated or have been eliminated from the B. mallei genome (5, 35). In fact B. pseudomallei has three AHL quorum-sensing gene pairs, bpsI1-bpsR1, bpsI2-bpsR2, and bpsI3-bpsR3. A large bpsI2-bpsR2-containing B. pseudomallei chromosomal region has been eliminated from the B. mallei genome. Implicit in the fact that bmaI1-bmaR1 and bmaI3-bmaR3 have been conserved in B. mallei is the idea that they are important for the success of this pathogen in an animal host.
What are possible explanations for the discrepancy between our finding and the previous finding that QS is a key virulence determinant in B. mallei? Unfortunately, the mutants used in the prior study no longer exist, and we cannot do comparative analysis. As discussed above, the genome of B. mallei is plastic (6). Laboratory passage of this species can result in the accumulation of spontaneous mutations or insertions/deletions (indels), which can attenuate virulence (27, 36). Ulrich et al. (15) had more limited genetic tools available to study B. mallei, and the mutants they examined had antibiotic resistance markers on plasmids inserted in the quorum-sensing genes. It is possible that their mutant construction selected for attenuation. It is also possible that the differences reflect the fact that we used a horse-passaged derivative of the B. mallei strain studied previously. To address this possibility, we constructed an AHL lactonase-producing derivative of the strain used in the original study. During in vitro growth, this strain made barely detectable levels of AHLs. Yet it remained virulent in mice (Table 2 and Fig. 3). Thus, we do not believe that the explanation for the discordant results resides in differences in parental strains (with the caveat that we did not measure AHLs in infected mice). Regardless of the explanation, our results showing that QS is not required for acute B. mallei disease following aerosol infection of mice reduces enthusiasm for development of anti-quorum-sensing therapeutics for B. mallei infections.
Several key factors for acute B. mallei infections in mice have been identified. These factors include capsular polysaccharide (36), a type III secretion system, and a type VI secretion system (37, 38). We infer that QS must not be required for activation of genes coding for these known virulence factors.
We do not know why the bmaI1-bmaR1 and bmaI3-bmaR3 genes have been retained in the B. mallei genome. We do know, however, that the AHL synthase genes produce functional, active proteins. Perhaps the genes are simply silent in the host, and the cost of their maintenance is low enough that there has been little or no selection against them. However, we showed that the bmaI1 promoter is active during a mouse infection by using luminescence imaging of mice infected with B. mallei carrying a bmaI1 promoter-driven lux gene cassette (Fig. 4). Glanders is a complicated disease in that it appears B. mallei has specifically evolved for persistence in the horse host. For example, glanders in horses most commonly presents in chronic and subacute forms (2, 3, 39). However, in other mammals, including humans, glanders is more commonly a life-threatening acute disease (2, 40, 41). It may be that QS is important during acute infection in the horse. However, we believe it more likely that QS is involved in establishment or maintenance of a chronic phase of infection. Whether or not this is the case will require further experimentation to reveal the genes controlled by QS in B. mallei, and it will require studies of chronic infections. It is interesting that bmaI1 promoter activity in mouse lungs coincided with the onset of overt disease symptoms. Perhaps QS could serve in the development of a chronic state in horses, whereas mice do not limit the acute infection to the same extent.
ACKNOWLEDGMENTS
This research was supported by Northwest Regional Center of Excellence for Biodefense and Emerging Infectious Diseases grant U54AI057141 to E.P.G.
We thank S. Brook Peterson for use of pBAD123::aiiA.
Footnotes
Published ahead of print 19 February 2013
REFERENCES
- 1. Khan I, Wieler LH, Melzer F, Elschner MC, Muhammad G, Ali S, Sprague LD, Neubauer H, Saqib M. 27 May 2012, posting date Glanders in animals: a review on epidemiology, clinical presentation, diagnosis and countermeasures. Transbound. Emerg. Dis. doi:10.1111/j.1865-1682.2012.01342 [DOI] [PubMed] [Google Scholar]
- 2. Whitlock GC, Estes DM, Torres AG. 2007. Glanders: off to the races with Burkholderia mallei. FEMS Microbiol. Lett. 277:115–122 [DOI] [PubMed] [Google Scholar]
- 3. Malik P, Singha H, Khurana SK, Kumar R, Kumar S, Raut AA, Riyesh T, Vaid RK, Virmani N, Singh BK, Pathak SV, Parkale DD, Singh B, Pandey SB, Sharma TR, Chauhan BC, Awasthi V, Jain S, Singh RK. 2012. Emergence and re-emergence of glanders in India: a description of outbreaks from 2006 to 2011. Vet. Ital. 48:167–178 [PubMed] [Google Scholar]
- 4. Rotz LD, Khan AS, Lillibridge SR, Ostroff SM, Hughes JM. 2002. Public health assessment of potential biological terrorism agents. Emerg. Infect. Dis. Dis. 8:225–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gregory BC, Waag DM. 2008. Glanders, p 121–146 In Dembek ZF, Lenhart M, Lounsbury D, Martin J. (ed), Medical aspects of biological warfare. Office of the Surgeon General, Washington, DC: [Google Scholar]
- 6. Nierman WC, Deshazer D, Kim HS, Tettelin H, Nelson KE, Feldblyum T, Ulrich RL, Ronning CM, Brinkac LM, Daugherty SC, Davidsen TD, Deboy RT, Dimitrov G, Dodson RJ, Durkin AS, Gwinn ML, Haft DH, Khouri H, Kolonay JF, Madupu R, Mohammoud Y, Nelson WC, Radune D, Romero CM, Sarria S, Selengut J, Shamblin C, Sullivan SA, White O, Yu Y, Zafar N, Zhou L, Fraser CM. 2004. Structural flexibility in the Burkholderia mallei genome. Proc. Natl. Acad. Sci. U. S. A. 101:14246–14251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smith MD, Wuthiekanun V, Walsh AL, White NJ. 1995. Quantitative recovery of Burkholderia pseudomallei from soil in Thailand. Trans. R. Soc. Trop. Med. Hyg. 89:488–490 [DOI] [PubMed] [Google Scholar]
- 8. Brett PJ, DeShazer D, Woods DE. 1998. Burkholderia thailandensis sp. nov., a Burkholderia pseudomallei-like species. Int. J. Syst. Bacteriol. 48:317–320 [DOI] [PubMed] [Google Scholar]
- 9. Limmathurotsakul D, Wuthiekanun V, Chantratita N, Wongsuvan G, Amornchai P, Day NPJ, Peacock SJ. 2010. Burkholderia pseudomallei is spatially distributed in soil in northeast Thailand. PLoS Negl. Trop. Dis. 4:e694 doi:10.1371/journal.pntd.0000694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cheng AC, Currie BJ. 2005. Melioidosis: epidemiology, pathophysiology, and management. Clin. Microbiol. Rev. 18:383–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fuqua WC, Winans SC, Greenberg EP. 1994. Quorum sensing in bacteria: the LuxR-LuxI family of cell density-responsive transcriptional regulators. J. Bacteriol. 176:269–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fuqua C, Winans SC, Greenberg EP. 1996. Census and consensus in bacterial ecosystems: the LuxR-LuxI family of quorum-sensing transcriptional regulators. Annu. Rev. Microbiol. 50:727–751 [DOI] [PubMed] [Google Scholar]
- 13. Visick KL, McFall-Ngai MJ. 2000. An exclusive contract: specificity in the Vibrio fischeri-Euprymna scolopes partnership. J. Bacteriol. 182:1779–1787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Duerkop BA, Ulrich RL, Greenberg EP. 2007. Octanoyl-homoserine lactone is the cognate signal for Burkholderia mallei BmaR1-BmaI1 quorum sensing. J. Bacteriol. 189:5034–5040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ulrich RL, Deshazer D, Hines HB, Jeddeloh JA. 2004. Quorum sensing: a transcriptional regulatory system involved in the pathogenicity of Burkholderia mallei. Infect. Immun. 72:6589–6596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Duerkop BA, Herman JP, Ulrich RL, Churchill MEA, Greenberg EP. 2008. The Burkholderia mallei BmaR3-BmaI3 quorum-sensing system produces and responds to N-3-hydroxy-octanoyl homoserine lactone. J. Bacteriol. 190:5137–5141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. López CM, Rholl DA, Trunck LA, Schweizer HP. 2009. Versatile dual-technology system for markerless allele replacement in Burkholderia pseudomallei. Appl. Environ. Microbiol. 75:6496–6503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Choi K-H, Gaynor JB, White KG, Lopez C, Bosio CM, Karkhoff-Schweizer RR, Schweizer HP. 2005. A Tn7-based broad-range bacterial cloning and expression system. Nat. Methods 2:443–448 [DOI] [PubMed] [Google Scholar]
- 19. Choi K-H, Schweizer HP. 2006. mini-Tn7 insertion in bacteria with single attTn7 sites: example Pseudomonas aeruginosa. Nat. Protoc. 1:153–161 [DOI] [PubMed] [Google Scholar]
- 20. Duerkop BA, Varga J, Chandler JR, Peterson SB, Herman JP, Churchill MEA, Parsek MR, Nierman WC, Greenberg EP. 2009. Quorum-sensing control of antibiotic synthesis in Burkholderia thailandensis. J. Bacteriol. 191:3909–3918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Choi K-H, Deshazer D, Schweizer HP. 2006. mini-Tn7 insertion in bacteria with multiple glmS-linked attTn7 sites: example Burkholderia mallei ATCC 23344. Nat. Protoc. 1:162–169 [DOI] [PubMed] [Google Scholar]
- 22. Choi K-H, Mima T, Casart Y, Rholl D, Kumar A, Beacham IR, Schweizer HP. 2008. Genetic tools for select-agent-compliant manipulation of Burkholderia pseudomallei. Appl. Environ. Microbiol. 74:1064–1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cao JG, Wei ZY, Meighen EA. 1995. The lux autoinducer-receptor interaction in Vibrio harveyi: binding parameters and structural requirements for the autoinducer. Biochem. J. 312:439–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Picotin G, Miginiac P. 1987. Activation of zinc by trimethylchlorosilane. An improved procedure for the preparation of β-hydroxy esters from ethyl bromoacetate and aldehydes or ketones (Reformatsky reaction). J. Org. Chem. 52:4796–4798 [Google Scholar]
- 25. Galyov EE, Brett PJ, Deshazer D. 2010. Molecular insights into Burkholderia pseudomallei and Burkholderia mallei pathogenesis. Annu. Rev. Microbiol. 64:495–517 [DOI] [PubMed] [Google Scholar]
- 26. Jeddeloh JA, Fritz DL, Waag DM, Hartings JM, Andrews GP. 2003. Biodefense-driven murine model of pneumonic melioidosis. Infect. Immun. 71:584–587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Romero CM, Deshazer D, Feldblyum T, Ravel J, Woods D, Kim HS, Yu Y, Ronning CM, Nierman WC. 2006. Genome sequence alterations detected upon passage of Burkholderia mallei ATCC 23344 in culture and in mammalian hosts. BMC Genomics 7:228 doi:10.1186/1471-2164-7-228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Latifi A, Foglino M, Tanaka K, Williams P, Lazdunski A. 1996. A hierarchical quorum-sensing cascade in Pseudomonas aeruginosa links the transcriptional activators LasR and RhIR (VsmR) to expression of the stationary-phase sigma factor RpoS. Mol. Microbiol. 21:1137–1146 [DOI] [PubMed] [Google Scholar]
- 29. Pearson JP, Pesci EC, Iglewski BH. 1997. Roles of Pseudomonas aeruginosa las and rhl quorum-sensing systems in control of elastase and rhamnolipid biosynthesis genes. J. Bacteriol. 179:5756–5767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ahlgren NA, Harwood CS, Schaefer AL, Giraud E, Greenberg EP. 2011. Aryl-homoserine lactone quorum sensing in stem-nodulating photosynthetic bradyrhizobia. Proc. Natl. Acad. Sci. U. S. A. 108:7183–7188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lindemann A, Pessi G, Schaefer AL, Mattmann ME, Christensen QH, Kessler A, Hennecke H, Blackwell HE, Greenberg EP, Harwood CS. 2011. Isovaleryl-homoserine lactone, an unusual branched-chain quorum-sensing signal from the soybean symbiont Bradyrhizobium japonicum. Proc. Natl. Acad. Sci. U. S. A. 108:16765–16770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Valade E, Thibault FM, Gauthier YP, Palencia M, Popoff MY, Vidal DR. 2004. The PmlI-PmlR quorum-sensing system in Burkholderia pseudomallei plays a key role in virulence and modulates production of the MprA protease. J. Bacteriol. 186:2288–2294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Song Y, Xie C, Ong YM, Gan YH, Chua KL. 2005. The BpsIR quorum-sensing system of Burkholderia pseudomallei. J. Bacteriol. 187:785–790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ulrich RL, Deshazer D, Brueggemann EE, Hines HB, Oyston PC, Jeddeloh JA. 2004. Role of quorum sensing in the pathogenicity of Burkholderia pseudomallei. J. Med. Microbiol. 53:1053–1064 [DOI] [PubMed] [Google Scholar]
- 35. Schwarz SS, West TE, Boyer F, Chiang WC, Carl MA, Hood RD, Rohmer L, Tolker-Nielsen TT, Skerrett JS, Mougous JD. 2010. Burkholderia type VI secretion systems have distinct roles in eukaryotic and bacterial cell interactions. PLoS Pathog. 6:e1001068 doi:10.1371/journal.ppat.1001068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. DeShazer D, Waag DM, Fritz DL, Woods DE. 2001. Identification of a Burkholderia mallei polysaccharide gene cluster by subtractive hybridization and demonstration that the encoded capsule is an essential virulence determinant. Microb. Pathog. 30:253–269 [DOI] [PubMed] [Google Scholar]
- 37. Ulrich RL, Deshazer D. 2004. Type III secretion: a virulence factor delivery system essential for the pathogenicity of Burkholderia mallei. Infect. Immun. 72:1150–1154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schell MA, Ulrich RL, Ribot WJ, Brueggemann EE, Hines HB, Chen D, Lipscomb L, Kim HS, Mrázek J, Nierman WC, Deshazer D. 2007. Type VI secretion is a major virulence determinant in Burkholderia mallei. Mol. Microbiol. 64:1466–1485 [DOI] [PubMed] [Google Scholar]
- 39. Arun S, Neubauer H, Gürel A, Ayyildiz G, Kusçu B, Yesildere T, Meyer H, Hermanns W. 1999. Equine glanders in Turkey. Vet. Rec. 144:255–258 [DOI] [PubMed] [Google Scholar]
- 40. Khaki P, Mosavari N, Khajeh NS, Emam M, Ahouran M, Hashemi S, Taheri MM, Jahanpeyma D, Nikkhah S. 2012. Glanders outbreak at Tehran Zoo, Iran. Iran J. Microbiol. 4:3–7 [PMC free article] [PubMed] [Google Scholar]
- 41. Coleman W, Ewing J. 1903. A case of septicemic glanders in the human subject. J. Med. Res. 9:223–240.3 [PMC free article] [PubMed] [Google Scholar]