Abstract
BACKGROUND
Little is known about the long-term outcomes in elderly survivors of in-hospital cardiac arrest. We determined rates of long-term survival and readmission among survivors of in-hospital cardiac arrest and examined whether these outcomes differed according to demographic characteristics and neurologic status at discharge.
METHODS
We linked data from a national registry of inpatient cardiac arrests with Medicare files and identified 6972 adults, 65 years of age or older, who were discharged from the hospital after surviving an in-hospital cardiac arrest between 2000 and 2008. Predictors of 1-year survival and of readmission to the hospital were examined.
RESULTS
One year after hospital discharge, 58.5% of the patients were alive, and 34.4% had not been readmitted to the hospital. The risk-adjusted rate of 1-year survival was lower among older patients than among younger patients (63.7%, 58.6%, and 49.7% among patients 65 to 74, 75 to 84, and ≥85 years of age, respectively; P<0.001), among men than among women (58.6% vs. 60.9%, P = 0.03), and among black patients than among white patients (52.5% vs. 60.4%, P = 0.001). The risk-adjusted rate of 1-year survival was 72.8% among patients with mild or no neurologic disability at discharge, as compared with 61.1% among patients with moderate neurologic disability, 42.2% among those with severe neurologic disability, and 10.2% among those in a coma or vegetative state (P<0.001 for all comparisons). Moreover, 1-year readmission rates were higher among patients who were black, those who were women, and those who had substantial neurologic disability (P<0.05 for all comparisons). These differences in survival and readmission rates persisted at 2 years. At 3 years, the rate of survival among survivors of in-hospital cardiac arrest was similar to that of patients who had been hospitalized with heart failure and were discharged alive (43.5% and 44.9%, respectively; risk ratio, 0.98; 95% confidence interval, 0.95 to 1.02; P = 0.35).
CONCLUSIONS
Among elderly survivors of in-hospital cardiac arrest, nearly 60% were alive at 1 year, and the rate of 3-year survival was similar to that among patients with heart failure. Survival and readmission rates differed according to the demographic characteristics of the patients and neurologic status at discharge. (Funded by the American Heart Association and the National Heart, Lung, and Blood Institute.)
Little is known about the long-term outcomes in survivors of in-hospital cardiac arrest. Previous studies have focused on rates of in-hospital survival,1-3 and the few studies that have examined longer-term rates of survival4-8 have had modest samples and limited generalizability. Although the rates of long-term survival may be expected to be low, quantifying these rates is important, given the substantial efforts and hospital resources that are involved in acute resuscitation and postresuscitation care. If the overwhelming majority of survivors die within 1 year after discharge, a reassessment of contemporary practices and goals during resuscitation treatment in hospitals may be warranted.
In addition to quantifying the rates of overall survival, characterizing the prognostic value of key clinical factors, such as race and sex, would provide insights into possible differences among population subgroups in the long-term outcomes after in-hospital cardiac arrest. Moreover, the association between neurologic status at hospital discharge and long-term survival is important to understand, because previous studies have classified patients with moderate neurologic disability together with those with mild or no disability as having a “favorable neurologic outcome.” Finally, previous studies of in-hospital cardiac arrest have not examined freedom from readmission, a topic of growing interest with respect to other conditions, including myocardial infarction, heart failure, and pneumonia.9,10
To address these gaps in knowledge, we linked data from a large, national registry of in-hospital cardiac arrests with Medicare claims files. We examined the rates of survival and freedom from readmission among patients who survived to discharge after an in-hospital cardiac arrest, as well as the rates of these outcomes in subgroups defined according to various demographic characteristics, initial cardiac-arrest rhythm, and neurologic status at hospital discharge.
METHODS
Data Sources and Linkage
The Get with the Guidelines–Resuscitation registry, formerly the National Registry of Cardiopulmonary Resuscitation, is a large, prospective, quality-improvement registry of in-hospital cardiac arrests. The design of the registry has been described in detail previously.1 In brief, hospital personnel trained in quality-improvement measures enroll all patients who have had a cardiac arrest (defined as the absence of a palpable central pulse, apnea, and unresponsiveness) and who do not have do-not-resuscitate orders. Cases are identified with the use of multiple methods, including centralized collection of cardiac-arrest flow sheets, reviews of hospital paging-system logs, and routine checks of code carts (carts stocked with emergency medications and equipment), pharmacy tracer drug records, and hospital billing charges for resuscitation medications.1 The registry uses standardized definitions for patient variables and outcomes to facilitate uniform reporting across hospitals, adhering to recommended Utstein-style templates for cardiac-arrest data.11,12 The accuracy of the data is further ensured by rigorous certification of hospital staff and the use of standardized software with data checks for completeness and accuracy.13
We linked patient-level data from the Get with the Guidelines–Resuscitation registry from January 1, 2000, through December 31, 2008, with Medicare inpatient files using six identifiers: the dates of hospital admission and discharge, the patient’s age and sex, the admitting hospital (deidentified), and the diagnosis and procedure codes in the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM).14 We selected Medicare records for the linkage if they included a diagnosis code for cardiac arrest (427.5), ventricular fibrillation (427.41), or ventricular flutter (427.42) or a procedure code for cardiopulmonary resuscitation (99.60), defibrillation (99.62), or closed chest massage (99.63). To allow for an even closer match, we also selected records that included a diagnosis code for acute respiratory failure (518.81) or shock (785.5x, where x indicates that more than one number is applicable to that diagnosis) to identify patients who did not have a diagnosis of cardiac arrest in the Medicare claims data but otherwise were uniquely matched on all other identifiers, including hospital. For each linked patient, we obtained Medicare denominator files and inpatient files from 2000 through 2010.
Study Population
The study cohort included 523 acute care hospitals that submitted data to the Get with the Guidelines–Resuscitation registry between January 1, 2000, and December 31, 2008. A total of 19,373 patients, 18 years of age or older, had a pulseless in-hospital cardiac arrest and survived to discharge (see Fig. S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). We excluded 9057 patients who were younger than 65 years of age, leaving 10,316 Medicare age-eligible patients. Using the method described above, we linked 7080 patients (68.6%) to Medicare claims data; 3236 patients could not be linked. The demographic and clinical characteristics of patients who were linked to Medicare files and those who were not linked were similar (Table S1 in the Supplementary Appendix). Finally, for patients who had a cardiac arrest during multiple hospitalizations, we used the first hospitalization as the index hospitalization (108 cardiac arrests were excluded). The final study cohort included 6972 patients at 401 hospitals.
Study Outcomes
The outcomes of interest were survival and freedom from readmission 1 year after discharge from the index hospitalization. Outcomes at 2 years were examined as secondary analyses. We determined vital status from the Medicare denominator files and readmission from the Medicare inpatient files.
Statistical Analysis
The baseline characteristics of the study cohort were described with the use of proportions for categorical variables and means with standard deviations for continuous variables. We constructed survival curves using Kaplan–Meier estimates to determine unadjusted rates of survival and freedom from readmission.
Multivariable logistic-regression models with generalized estimating equations were used to examine predictors of 1-year survival. In addition to age (65 to 74 years, 75 to 84 years, or ≥85 years), sex, race (white, black, or other), and initial cardiac-arrest rhythm, all models were adjusted for baseline neurologic deficit, as well as for the following coexisting conditions and events occurring within 24 hours before the cardiac arrest: heart failure, myocardial infarction, diabetes mellitus, renal insufficiency, hepatic insufficiency, respiratory insufficiency, acute stroke, pneumonia, hypotension, sepsis, major trauma, metabolic or electrolyte abnormality, metastatic or hematologic cancer, requirement for mechanical ventilation, and need for hemodialysis. The models were also adjusted for the time of day (work hours [7 a.m. to 10:59 p.m.] vs. after hours [11 p.m. to 6:59 a.m.]) and day of the week (weekday vs. weekend) of the cardiac arrest,13 the use or nonuse of a hospital-wide cardiopulmonary arrest alert, and the neurologic status of the patient at discharge. The last variable was assessed with the use of the cerebral-performance category (CPC) scale, which categorizes the neurologic status of a patient on a 5-point scale, with 1 indicating mild or no neurologic disability, 2 indicating moderate disability, 3 indicating severe disability, 4 indicating coma or vegetative state, and 5 indicating brain death.15 Finally, we adjusted for the primary reason for the initial hospitalization, which we determined from ICD-9-CM codes for the principal discharge diagnosis in the Medicare inpatient files.
Modified Poisson regression with robust variance estimates was used at all steps to directly estimate rate ratios, because the outcome was not rare (e.g., occurred in >10% of patients).16,17 From the rate ratios, we derived risk-adjusted rates of 1-year survival in prespecified subgroups defined according to the following variables: age, sex, race, initial cardiac-arrest rhythm, and neurologic status at discharge.
We also examined temporal trends in long-term survival using hierarchical logistic-regression models, which accounted for differences among hospitals in the initial year of participation in the Get with the Guidelines–Resuscitation registry. These models evaluated calendar year as a continuous variable, with adjustment for the same covariates as in the models above, and examined survival trends separately for patients who had a cardiac arrest due to asystole or pulseless electrical activity and those who had a cardiac arrest due to ventricular fibrillation or ventricular tachycardia, because the prognosis of these types of cardiac arrests differs.
To place our findings on survival in the proper context, we compared the survival rate of our cohort with the survival rate of hospitalized patients with heart failure (ICD-9-CM diagnosis codes 428.×, 402.×1, 404.×1, or 404.×3) who survived to discharge, with the two cohorts matched according to age, sex, admitting hospital, and date of hospitalization (±1 year). To determine patient characteristics associated with readmission to the hospital within 1 year after discharge, we constructed multivariable Cox regression models and adjusted for the aforementioned patient covariates. As secondary analyses, we repeated all models for an analysis of the rates of survival at 2 years and readmission within 2 years after discharge.
Overall, the rates of missing data were low. Data on race were missing for 396 patients (5.7%), and data on neurologic status at discharge were missing for 858 patients (12.3%). For the multivariable models, we performed multiple imputation with IVEware software (University of Michigan, Ann Arbor).18 Results with and without imputation were not meaningfully different, so we present the former.
For each analysis, we evaluated the null hypothesis at a two-sided significance level of 0.05 and calculated 95% confidence intervals using robust standard errors. All analyses were performed with the use of SAS software, version 9.2 (SAS Institute), and R software, version 2.10.0 (R Foundation for Statistical Computing).19
RESULTS
Patients
Of the 6972 survivors of in-hospital cardiac arrest in our cohort, 55.5% were men and 11.8% were black; the mean (±SD) age was 75.8±7.0 years (Table 1). Ventricular fibrillation and pulseless electrical activity were the most common cardiac-arrest rhythms. Approximately one quarter of the patients had a diagnosis of heart failure, myocardial infarction, or renal insufficiency. At hospital discharge, 48.1% of the patients had mild or no neurologic disability, and the rest of the patients had moderate-to-severe disability or were in a coma or vegetative state. More than half the patients (55.3%) were discharged to an inpatient skilled nursing or rehabilitation facility, 40.0% were discharged home, and 4.8% went to hospice, with the discharge destination differing according to the demographic characteristics of the patients and other variables (Table S2 in the Supplementary Appendix).
Table 1. Characteristics of the Study Cohort.*.
| Characteristic | Patients (N = 6972) |
|---|---|
|
| |
| Age — yr | 75.8±7.0 |
| Male sex — no. (%) | 3872 (55.5) |
| Race — no./total no. (%)† | |
| White | 5634/6576 (85.7) |
| Black | 778/6576 (11.8) |
| Other | 164/6576 (2.5) |
| Initial cardiac-arrest rhythm – no. (%) | |
| Asystole | 1707 (24.5) |
| Pulseless electrical activity | 2031 (29.1) |
| Pulseless ventricular tachycardia | 1109 (15.9) |
| Ventricular fibrillation | 2125 (30.5) |
| CPC score at discharge — no./total no. (%)‡ | |
| 1 | 2943/6114 (48.1) |
| 2 | 2097/6114 (34.3) |
| 3 | 879/6114 (14.4) |
| 4 | 195/6114 (3.2) |
| Preexisting conditions – no. (%) | |
| Heart failure at admission | 1625 (23.3) |
| History of heart failure | 1848 (26.5) |
| Myocardial infarction at admission | 1897 (27.2) |
| History of myocardial infarction | 1805 (25.9) |
| Hypotension | 1313 (18.8) |
| Renal insufficiency | 1836 (26.3) |
| Respiratory insufficiency | 2368 (34.0) |
The plus–minus value is a mean ±SD.
Race was self-reported. Data on race were missing for 396 patients.
The cerebral-performance category (CPC) scores are used to assess neurologic status after a cardiac arrest. Scores range from 1 to 5, with 1 indicating mild or no neurologic disability, 2 mild neurologic disability, 3 severe neurologic disability, 4 coma or vegetative state, and 5 brain death. The CPC score was missing for 858 patients.
Outcomes
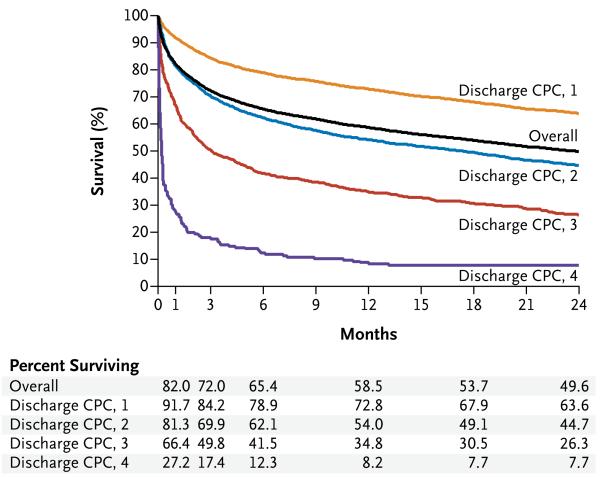
The overall rate of survival after hospital discharge was 82.0% at 30 days, 72.0% at 3 months, 58.5% at 1 year, and 49.6% at 2 years (Fig. 1). Table 2 shows the risk-adjusted rates of 1-year survival according to prespecified subgroups. The risk-adjusted rate of 1-year survival was 63.7% among patients who were 65 to 74 years of age, as compared with 58.6% among patients 75 to 84 years of age and 49.7% among patients 85 years of age or older (P<0.001 for both comparisons). The risk-adjusted rate of 1-year survival was lower among black patients than among white patients (52.5% vs. 60.4%, P = 0.001) and among men than among women (58.6% vs. 60.9%, P = 0.03). The risk-adjusted rate of 1-year survival was 72.8% among patients with mild or no neurologic disability at discharge, as compared with 61.1% among patients with moderate neurologic disability, 42.2% among patients with severe disability, and 10.2% among patients in a coma or vegetative state (P<0.001 for all comparisons). The risk-adjusted rates of 1-year survival were similar among patients with asystole, those with pulseless electrical activity, and those with pulseless ventricular tachycardia as the cardiac-arrest rhythm, whereas patients with ventricular fibrillation had a higher rate of survival (Table 2). The results in all the subgroups that were analyzed are shown in Table S3 in the Supplementary Appendix.
Figure 1. Kaplan–Meier Estimates of Rates of Survival over Time among Patients Who Have Survived an In-Hospital Cardiac Arrest.
Shown below the graph are the estimated rates of survival at specific follow-up time points. The cerebral-performance category (CPC) scores are used to assess neurologic status at discharge after a cardiac arrest. Scores range from 1 to 5, with 1 indicating mild or no neurologic disability, 2 indicating mild neurologic disability, 3 indicating severe neurologic disability, 4 indicating coma or vegetative state, and 5 indicating brain death.
Table 2. Risk-Adjusted Rates of 1-Year Survival in Prespecified Subgroups.*.
| Subgroup | Unadjusted Rate of Survival |
Risk-Adjusted Rate of Survival |
Adjusted Rate Ratio (95% CI) |
P Value |
|---|---|---|---|---|
|
| ||||
| percent | ||||
| Age | ||||
| 65–74 yr | 63.7 | 63.7 | 1.00 | — |
| 75–84 yr | 56.7 | 58.6 | 0.92 (0.88–0.96) | <0.001 |
| ≥85 yr | 45.1 | 49.7 | 0.78 (0.73–0.84) | <0.001 |
| Sex | ||||
| Male | 58.6 | 58.6 | 1.00 | — |
| Female | 58.5 | 60.9 | 1.04 (1.00–1.08) | 0.03 |
| Race | ||||
| White | 60.4 | 60.4 | 1.00 | — |
| Black | 43.3 | 52.5 | 0.87 (0.81–0.95) | 0.001 |
| Other | 54.9 | 62.8 | 1.04 (0.90–1.20) | 0.63 |
| Initial cardiac-arrest rhythm | ||||
| Pulseless electrical activity | 50.1 | 50.1 | 1.00 | — |
| Asystole | 53.3 | 51.1 | 1.02 (0.96–1.09) | 0.44 |
| Pulseless ventricular tachycardia | 60.7 | 51.1 | 1.02 (0.95–1.09) | 0.60 |
| Ventricular fibrillation | 69.7 | 54.6 | 1.09 (1.04–1.15) | 0.001 |
| CPC score at discharge | ||||
| 1 | 72.8 | 72.8 | 1.00 | — |
| 2 | 54.0 | 61.1 | 0.84 (0.80–0.88) | <0.001 |
| 3 | 34.8 | 42.2 | 0.58 (0.52–0.65) | <0.001 |
| 4 | 8.2 | 10.2 | 0.14 (0.09–0.23) | <0.001 |
The model was adjusted for the variables listed in Table S1 in the Supplementary Appendix. P values are for the comparison of the risk-adjusted survival rates in each subgroup with the designated reference for each categorical variable. CI denotes confidence interval.
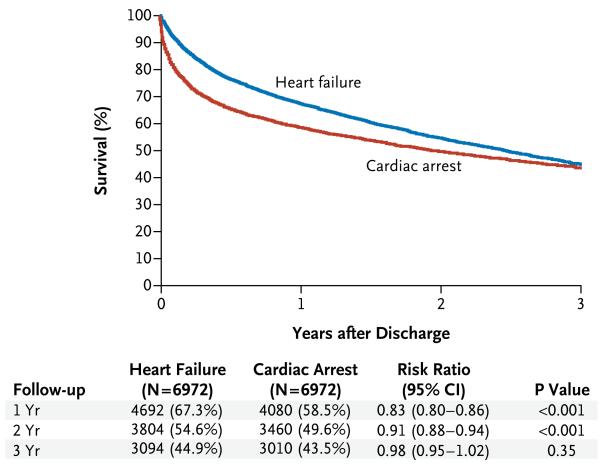
Over the course of the study, there were no significant temporal trends in the rates of 1-year survival after cardiac arrests due to asystole or pulseless electrical activity (P = 0.32, adjusted for trend) or after cardiac arrests due to ventricular fibrillation or ventricular tachycardia (P = 0.49, adjusted for trend) (Fig. S2 and Table S4 in the Supplementary Appendix). As compared with patients who had been hospitalized with heart failure and discharged alive, survivors of in-hospital cardiac arrest were 9% less likely to survive to 2 years (risk ratio, 0.91; 95% confidence interval [CI], 0.88 to 0.94; P<0.001), but this difference dissipated by 3 years (risk ratio, 0.98; 95% CI, 0.95 to 1.02; P = 0.35) (Fig. 2).
Figure 2. Long-Term Survival after In-Hospital Cardiac Arrest and after Hospitalization for Heart Failure.
By the 3-year follow-up, the rate of survival among patients who had had an in-hospital cardiac arrest and were discharged alive was nearly identical to that of patients who had been hospitalized for heart failure and were discharged alive. The 3-year rates are Kaplan–Meier survival estimates, since patients enrolled during 2008 did not have 3 complete years of follow-up.
At 1 year and 2 years after discharge from the hospital, 34.4% and 23.8% of the patients, respectively, had not been readmitted (Fig. S3 in the Supplementary Appendix). After multivariable adjustment, the rates of readmission within 1 year after discharge were similar in subgroups defined according to age and cardiac-arrest rhythm; however, black patients, women, and patients with substantial neurologic disability at discharge were more likely to have been readmitted (Table 3). Similar findings were obtained in models assessing survival at 2 years and readmission within 2 years after discharge (Tables S5 and S6 in the Supplementary Appendix).
Table 3. Associations between Selected Patient Characteristics and Readmission at 1 Year.*.
| Variable | Adjusted Hazard Ratio (95% CI) |
P Value |
|---|---|---|
|
| ||
| Age | ||
| 65–74yr | 1.00 | — |
| 75–84yr | 1.05 (0.98–1.13) | 0.19 |
| ≥85 yr | 1.06 (0.94–1.19) | 0.34 |
| Sex | ||
| Male | 1.00 | — |
| Female | 1.09 (1.01–1.17) | 0.02 |
| Race | ||
| White | 1.00 | — |
| Black | 1.22 (1.08–1.37) | 0.002 |
| Other | 0.99 (0.77–1.28) | 0.96 |
| Initial cardiac-arrest rhythm | ||
| Pulseless electrical activity | 1.00 | — |
| Asystole | 0.95 (0.87–1.05) | 0.33 |
| Pulseless ventricular tachycardia | 1.02 (0.91–1.14) | 0.76 |
| Ventricular fibrillation | 0.94 (0.85–1.04) | 0.20 |
| CPC score at discharge | ||
| 1 | 1.00 | — |
| 2 | 1.23 (1.13–1.35) | <0.001 |
| 3 | 1.29 (1.14–1.46) | <0.001 |
| 4 | 0.86 (0.58–1.28) | 0.45 |
The model was adjusted for the variables listed in Table S1 in the Supplementary Appendix.
DISCUSSION
Among patients 65 years of age or older who survived an in-hospital cardiac arrest, 59% survived for at least 1 year and 50% survived for at least 2 years. The most vulnerable period after discharge was the first 3 months, during which 56% of the total number of deaths during the first 2 years occurred. The rates of 1-year survival were significantly lower among older patients than among younger patients, among men than among women, among blacks than among whites, and among patients with moderate or more severe neurologic disability at discharge than among those with mild or no neurologic disability. In addition, more than one third of the patients were not readmitted to the hospital within 1 year after discharge, and many of the patient characteristics associated with lower rates of 1-year survival were also associated with higher rates of readmission.
Until recently, there has been limited information on long-term outcomes in survivors of in-hospital cardiac arrest.4-8 The lack of data on long-term outcomes has prevented patients and clinicians from understanding what they may expect after recovery and has potentially contributed to nihilistic attitudes toward resuscitation efforts, especially for older patients. Our findings that almost 60% of patients were alive at 1 year and more than one third had not been readmitted to the hospital provide new insights into this population and challenge earlier assumptions. We found that survivors of in-hospital cardiac arrest had only modestly lower 2-year survival rates than did patients hospitalized for heart failure, with their survival curves converging at 3 years. Our findings suggest that survivors of in-hospital cardiac arrest do not have markedly worse survival trajectories than do patients with other serious medical conditions, such as heart failure.
We observed several predictors of 1-year survival. The finding that older age was associated with lower survival was not surprising, yet half the patients 85 years of age or older who were discharged from the hospital were alive at 1 year. Although in-hospital resuscitation efforts in patients of advanced age may be perceived as futile, the relatively high survival rate among these patients suggests that discussions about advance directives should be individualized and informed by patients’ preferences and health status. We also found that men were less likely than women to survive to 1 year, mirroring the pattern of lower rates of in-hospital survival among men after cardiac arrest.20 The physiological basis for the differences in these outcomes between men and women remains a focus of ongoing investigation.
The association of black race with lower rates of long-term survival is not intuitive and raises the possibility of disparities in care after discharge. We found racial differences in the rate of survival even after adjusting for factors, such as renal disease, that are more prevalent among black patients and are associated with a worse prognosis. To better understand the reasons for racial differences in the rates of survival after discharge, further investigations are needed to determine whether there are racial differences in discharge destination (e.g., hospice), rates of cardiac catheterization and implantation of a cardioverter–defibrillator during the index hospitalization, access to follow-up outpatient care, or other practice patterns. Finally, we found that patients with moderate neurologic disability at discharge had a significantly lower rate of 1-year survival than did patients with mild or no neurologic disability. This finding suggests that renewed efforts are needed to minimize neurologic injury during resuscitation care.
Our study has some limitations. First, Get with the Guidelines–Resuscitation is a quality-improvement registry. Although data are collected from a diverse group of hospitals, long-term outcomes in nonparticipating hospitals may differ. Second, we restricted the analysis to Medicare beneficiaries; outcomes in patients younger than 65 years of age may differ. Third, we excluded patients for whom a Get with the Guidelines–Resuscitation record could not be linked to a Medicare hospitalization. This scenario occurred when a patient was admitted to a non-Medicare hospital (e.g., a Veterans Affairs hospital), had insurance other than fee-for-service Medicare, was admitted to a hospital with few patients included in the registry (thus precluding a unique match), or did not have a qualifying ICD-9-CM diagnosis or procedure code for cardiac arrest in the Medicare files. Nonetheless, the characteristics of patients who were excluded from the study were similar to those of patients in the study cohort; therefore, the exclusion of those patients was unlikely to significantly bias the results. Finally, we did not have access to serial assessments of neurologic status or quality of life after discharge to allow for a more refined understanding of the trajectory of health status among those with long-term survival,21 nor did we have information about cause of death.
In conclusion, we found that 59% of elderly survivors of an in-hospital cardiac arrest were alive at 1 year, and one third were not readmitted to the hospital during that time. Survival and readmission rates differed according to the patients’ age, sex, race, and neurologic status at discharge.
Supplementary Material
Acknowledgments
Supported by the American Heart Association and by a Career Development Grant Award (K23HL102224, to Dr. Chan) from the National Heart, Lung, and Blood Institute. Dr. Krumholz was supported, in part, by a grant (1U01HL105270-02) from the National Heart, Lung, and Blood Institute to the Center for Cardiovascular Outcomes Research at Yale University.
We thank Damon M. Seils, M.A., Duke University, for providing editorial assistance on an earlier version of this manuscript. (Mr. Seils did not receive compensation for his assistance apart from his employment at the institution where the study was conducted.)
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
REFERENCES
- 1.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 2.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 3.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–7. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 4.Kalbag A, Kotyra Z, Richards M, Spearpoint K, Brett SJ. Long-term survival and residual hazard after in-hospital cardiac arrest. Resuscitation. 2006;68:79–83. doi: 10.1016/j.resuscitation.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Kutsogiannis DJ, Bagshaw SM, Laing B, Brindley PG. Predictors of survival after cardiac or respiratory arrest in critical care units. CMAJ. 2011;183:1589–95. doi: 10.1503/cmaj.100034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bloom HL, Shukrullah I, Cuellar JR, Lloyd MS, Dudley SC, Jr, Zafari AM. Long-term survival after successful inhospital cardiac arrest resuscitation. Am Heart J. 2007;153:831–6. doi: 10.1016/j.ahj.2007.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herlitz J, Andréasson AC, Bång A, Aune S, Lindqvist J. Long-term prognosis among survivors after in-hospital cardiac arrest. Resuscitation. 2000;45:167–71. doi: 10.1016/s0300-9572(00)00187-8. [DOI] [PubMed] [Google Scholar]
- 8.Zoch TW, Desbiens NA, DeStefano F, Stueland DT, Layde PM. Short- and long-term survival after cardiopulmonary resuscitation. Arch Intern Med. 2000;160:1969–73. doi: 10.1001/archinte.160.13.1969. [DOI] [PubMed] [Google Scholar]
- 9.Keenan PS, Normand SL, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 10.Krumholz HM, Lin Z, Drye EE, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4:243–52. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style.’. Circulation. 1997;95:2213–39. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–97. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 13.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299:785–92. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 14.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to Medicare claims data using indirect identifiers. Am Heart J. 2009;157:995–1000. doi: 10.1016/j.ahj.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 16.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–5. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 17.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 18.Raghunathan TESP, Van Hoeyk J. IVEware: Imputation and Variance Estimation software: user guide. University of Michigan Survey Research Center, Institute for Social Research; Ann Arbor: 2002. [Google Scholar]
- 19.R Development Core Team . R: a language and environment for statistical computing. R Foundation for Statistical Computing V; Vienna: 2008. http://www.R-project.org. [Google Scholar]
- 20.Topjian AA, Localio AR, Berg RA, et al. Women of child-bearing age have better inhospital cardiac arrest survival outcomes than do equal-aged men. Crit Care Med. 2010;38:1254–60. doi: 10.1097/CCM.0b013e3181d8ca43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Becker LB, Aufderheide TP, Geocadin RG, et al. Primary outcomes for resuscitation science studies: a consensus statement from the American Heart Association. Circulation. 2011;124:2158–77. doi: 10.1161/CIR.0b013e3182340239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.