Abstract
Meta-analysis of the heterogeneous symptoms of obsessive-compulsive disorder (OCD) has found a four-factor structure of symptom dimensions consisting of cleaning, forbidden thoughts, symmetry, and hoarding. Research into age of onset of symptom dimensions has yielded inconsistent results, and it is unknown whether symptoms along these dimensions differ in their clinical course. We assessed age of onset and clinical course of different OCD symptom dimensions in a large cohort of adult patients. Nine-hundred fifty-five subjects were assessed using the Dimensional Yale-Brown Obsessive-Compulsive Scale. For age of onset analysis, we tested across three methods of classification: (1) primary (more severe) symptom dimension (2) clinically significant symptoms within a dimension or (3) any symptoms within a dimension. Age of onset was defined as the earliest age of onset reported for any individual item within a symptom dimension. For analysis of different types of clinical course, we used chi-square tests to assess for differences between primary symptom dimensions. OCD symptoms in the symmetry dimension had an earlier age of onset than other OCD symptom dimensions. These findings remained significant across all three methods of classification and controlling for gender and comorbid tics. No significant differences were found between the other dimensions. Subjects with primary OCD symptoms in the forbidden thoughts dimension were more likely to report a waxing-and-waning course, whereas symmetry symptoms were less likely to be associated with a waxing-and-waning course.
Keywords: Obsessive-Compulsive Disorder, Symptom Dimensions, Age of Onset, Clinical Course
Obsessive-compulsive disorder (OCD) is a highly heterogeneous condition (Miguel, Leckman et al. 2005). While current nosology (DSM-IV and ICD-10) considers OCD to be a unitary entity, there is great variability in symptomatic presentation (Lochner and Stein 2003). Indeed, symptoms can present in such dramatically different ways that several individuals with equally severe OCD may have no specific symptoms in common (Ferrao, Shavitt et al. 2006; Bloch, Landeros-Weisenberger et al. 2008).
OCD symptom dimensions are a tool for capturing this heterogeneity. Factor analytic studies have yielded a fairly consistent four-factor structure of OCD symptom dimensions across the lifespan, consisting of cleaning, forbidden (aggressive/sexual/religious) thoughts, symmetry (ordering/counting/repeating) and hoarding (Bloch, Landeros-Weisenberger et al. 2008). Recent studies suggest that these symptom dimensions differ in genetic association (Hasler, Pinto et al. 2007; Samuels, Shugart et al. 2007), neurocircuitry (Rauch, Dougherty et al. 1998; Mataix-Cols, Wooderson et al. 2004), and response to pharmacological (Mataix-Cols, Rauch et al. 1999; Landeros-Weisenberger, Bloch et al. 2010) and behavioral (Mataix-Cols, Marks et al. 2002) treatments.
It remains unclear whether symptoms along the different dimensions have a different natural history. Several studies have yielded conflicting results, with some indicating differences in age of onset {Honjo, 1989 #23;Mataix-Cols, 1999 #9;Minichiello, 1990 #62} and others not finding any age-related patterns (Rettew, Swedo et al. 1992). Interpretation of these conflicting results is further burdened by the limited sample sizes differing methodology; particularly problematic is their different methods of assessing and classifying symptom dimensions. For instance, several common OCD symptoms are often evaluated in a manner that leaves it unclear which dimension certain symptoms belong within (e.g. was “checking” due to harm-related obsessions, or due to obsessions that something was not done correctly). Additionally, participants generally only indicated whether or not particular classes of symptoms were present (and in some cases whether they were a major problem), meaning there was no distinction made between symptoms at varying levels of severity. This distinction is important, as without it, nascent and minor symptoms within a dimension might have been coded in the same manner as well-established and problematic symptoms. Distinct patterns of onset and natural history may be found at different severity thresholds – that is, if one considers all symptoms, or only clinically significant symptoms, or only primary symptoms. Further, identifying whether different symptoms are associated with distinct clinical course can potentially help clinicians to provide more accurate prognostic information and identify symptoms that demand treatment priority.
In an effort to enhance understanding of OCD symptom dimensions, we examined age of onset and clinical course of OCD symptomatology according to symptom dimension in a large cohort of OCD patients. We hypothesized that differences in age of onset would exist between dimensions, with the symmetry dimension having the earliest onset. Given that converging evidence (i.e. genetics, neuroimaging, clinical evaluation) suggests that OCD symptom dimensions may have distinct neurobiological underpinnings and differential response to treatment, we additionally hypothesized that OCD symptom dimensions would display differences in their clinical course.
Methods
Participants
A sample of 1001 OCD patients were recruited from 7 sites located across Brazil as part of the Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders from 2005–2010. A full description of the recruitment and assessment procedure of this sample has been published elsewhere (Miguel, Ferrao et al. 2008). Due to the possibility of the clinical course not having fully emerged in adolescents, it was decided prior to data analysis that those under age 18 would be excluded; fifty-six subjects were excluded as a result. Nine-hundred fifty-five adults age 18–65 were ultimately included in our analyses.
Procedure
Each site’s ethics review boards reviewed and approved all methods. Experts in OCD trained to reliably use protocol instruments interviewed participants. Participants with primary OCD (per DSM-IV criteria) were included. An OCD diagnosis was established by administration of the Structured Clinical Interview for DSM-IV (First, Spitzer et al. 1995). OCD was considered the primary psychiatric condition when this was the disorder for which the patient sought treatment and the diagnosis was verified by an experienced clinician. This diagnostic evaluation was conducted at the same session or in close temporal proximity to when symptom ratings were conducted. Exclusions included comorbid schizophrenia or any condition that interfered with participants’ ability to effectively take part in the protocol. Demographic and clinical data was obtained through use of a questionnaire produced by the Consortium.
OCD symptom severity within each symptom dimension was assessed with the Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS) (Rosario-Campos, Miguel et al. 2006). The time spent on symptoms, level of anxiety, and level of interference are each rated on a 0 (least severe) to 5 (most severe) scale, for a total score of 0–15, for each dimension at the current and worst-ever time period. For the age of onset analysis, OCD symptom dimensions of subjects were classified in three ways: (1) primary symptom dimension (2) clinically significant symptoms within a dimension or (3) any symptoms within a dimension. The DY-BOCS ratings of symptom dimensions were restructured into the four symptom dimensions identified by a large meta-analysis of previous studies in the area (Bloch, Landeros-Weisenberger et al. 2008). Severity in the forbidden thoughts dimension was defined for a subject as the higher of the severity scores in either the sexual/religious or aggressive DY-BOCS dimensions. As a sensitivity analysis we also report results for sexual/religious and aggressive OCD symptoms separately. For analysis involving primary symptom dimension, subjects that scored highest on their worst-ever ratings in the miscellaneous dimension or had a tie between two or more symptom dimensions were excluded. Clinically significant symptoms within a dimension was defined by having a worst-ever DY-BOCS score in a dimension equal to or greater than 6, which roughly corresponds to a score on the more widely used Yale-Brown Obsessive Compulsive Scale (Y-BOCS) of 16, a standard threshold to identify clinically significant symptoms. Any symptom within a dimension was defined as having a worst-ever score greater than 0 in that dimension. Thus, a participant could (and often did) qualify for more than one dimension when symptom dimensions were defined by clinical significance or presence of symptoms but could only qualify for one primary dimension.
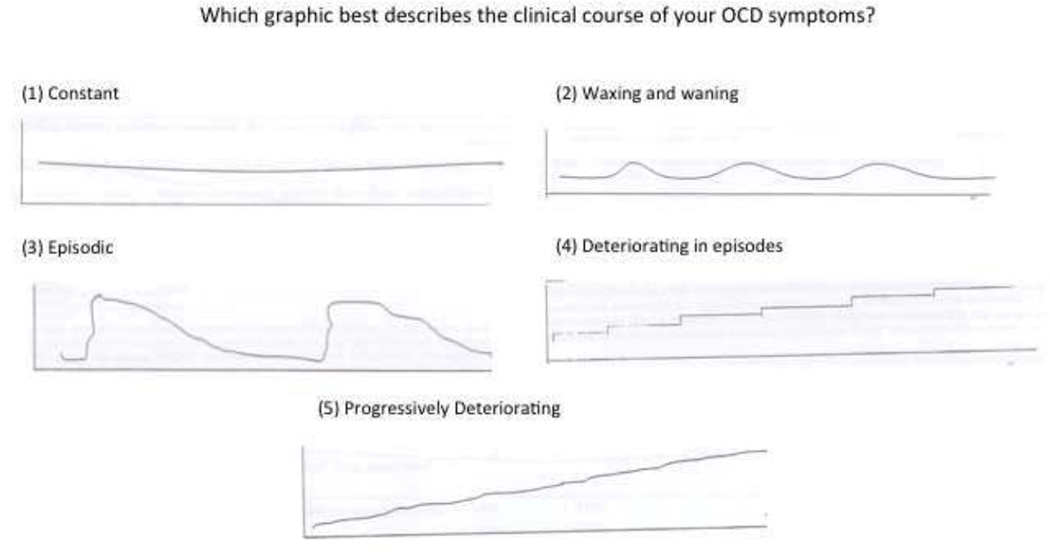
Age of onset for each symptom dimension was determined by the earliest age of onset reported for any individual item within a symptom dimension on the DY-BOCS checklist. This information was reported at the same time to when a clinical diagnosis was established. Clinical course of OCD was determined using a graphical-based question in which individuals were given six possible graphical options to describe their OCD course. These options are depicted in figure 1 and include (1) constant, (2) episodic, (3) waxing-and-waning, (4) deteriorating then constant, (5) progressively deteriorating and (6) other. Subjects who chose “other” were excluded from this analysis.
Figure 1.
Graphical Question that probed clinical course of OCD symptoms.
Analyses were conducted in SPSS 19.0. One-way omnibus analysis of variance (ANOVA) was used to test for overall significance in age of onset of DY-BOCS symptom dimensions. Analyses were conducted testing primary symptoms, clinically significant symptoms, and any symptoms. Post-hoc pairwise comparisons were then conducted to identify significant differences between OCD symptom dimensions when the overall test was significant. For analysis of the association between primary symptom dimension and type of clinical course, chi-square tests were utilized. When the overall chi-square test was significant, individual post-hoc tests were performed to determine which clinical course options were reported at significantly increased or decreased rates for each dimension.
For results related to the primary symptom dimension, we conducted additional analyses to determine the possible confounding effects of gender and comorbid tic disorders on our findings, as male gender and comorbid tic disorders have been associated with both an earlier age of onset (de Mathis, Diniz et al. 2009) and increased likelihood of symptoms in particular OCD dimensions (Rosario-Campos, Miguel et al. 2006; Labad, Menchon et al. 2008).( For the age of onset data, we added gender and tic disorder as additional covariates in a one-way ANOVA in SPSS.
The evidence concerning a relationship between gender, the presence of tic disorders, and longitudinal course of symptoms is considerably sparser, but there exists some evidence, at least in pediatric OCD, that gender and presence of a comorbid tic disorder is associated with adulthood outcome (Bloch, Peterson et al. 2006; Bloch, Craiglow et al. 2009). Therefore, we decided to examine possible confounders in this analysis as well. The Mantel-Haenszel chi-square test was used to assess confounding across gender and tic disorder strata.
Results
Participants
Demographics characteristics of subjects are depicted in Table 1.
Table 1.
Demographics
| Demographic Characteristics | Mean ± SD N (%) |
|---|---|
| Age | 35.82 ± 12.49 |
| Male Gender (%) | 400 (42%) |
| YBOCS total score | 25.6 ± 7.46 |
| YBOCS obsessions subscale | 12.73 ± 3.91 |
| YBOCS compulsions subscale | 12.87 ± 4.11 |
| Lifetime Comorbid Conditions | |
| Generalized anxiety disorder | 321 (33.6%) |
| Social anxiety disorder | 312 (32.7%) |
| Post-traumatic stress disorder | 97 (10.2%) |
| Panic disorder | 44 (4.6%) |
| Specific phobia | 296 (31%) |
| Major depression | 549 (57.5%) |
| Bipolar Disorder | 51 (5.3%) |
| Body dysmorphic disorder | 105 (11%) |
| Trichotillomania | 45 (4.7%) |
| Tic Disorder | 264 (27.6%) |
| Primary OCD Dimension | |
| Forbidden Thoughts | 202 (22%) |
| Symmetry | 148 (16.1%) |
| Cleaning | 146 (15.9%) |
| Hoarding | 27 (2.8%) |
| Previous Treatments | |
| Psychotherapy | 614 (61.3%) |
| Serotonin Reuptake Inhibitors | 679 (71%) |
| Antipsychotic Augmentation | 194 (20.3%) |
YBOCS = Yale-Brown Obsessive-Compulsive Scale
Age of onset
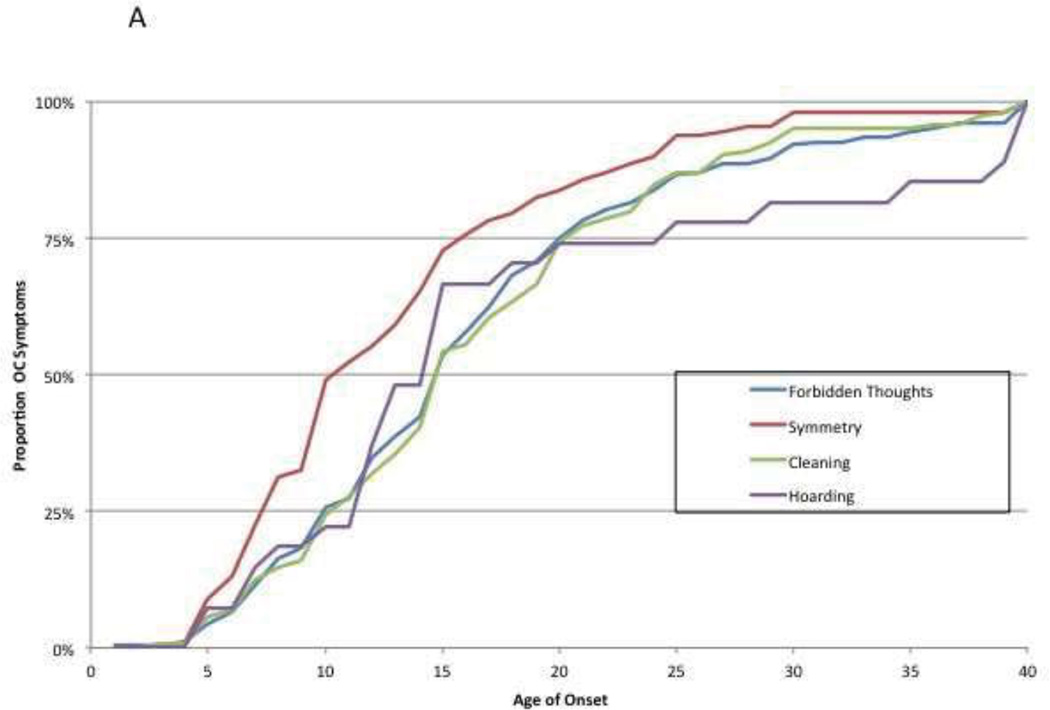
We found a significant association between age of onset and primary dimension of OCD symptoms F(3, 519)= 5.43, p < 0.001. Symptoms in the symmetry dimension (age of onset = 13.6±8.6) were associated with an earlier age of onset than symptoms in the hoarding (age of onset = 18.3±11.3, p < .05), cleaning (age of onset = 16.9±8.3, p < .01), and forbidden thoughts dimensions (age of onset = 16.9±8.9, p < .001). No other significant differences in age of onset of symptoms were found between the OCD symptom dimensions. Figure 2A depicts a cumulative histogram of the age of onset of symptoms in each subject’s primary OCD dimension when defined by the primary dimension of symptomatology in each subject.
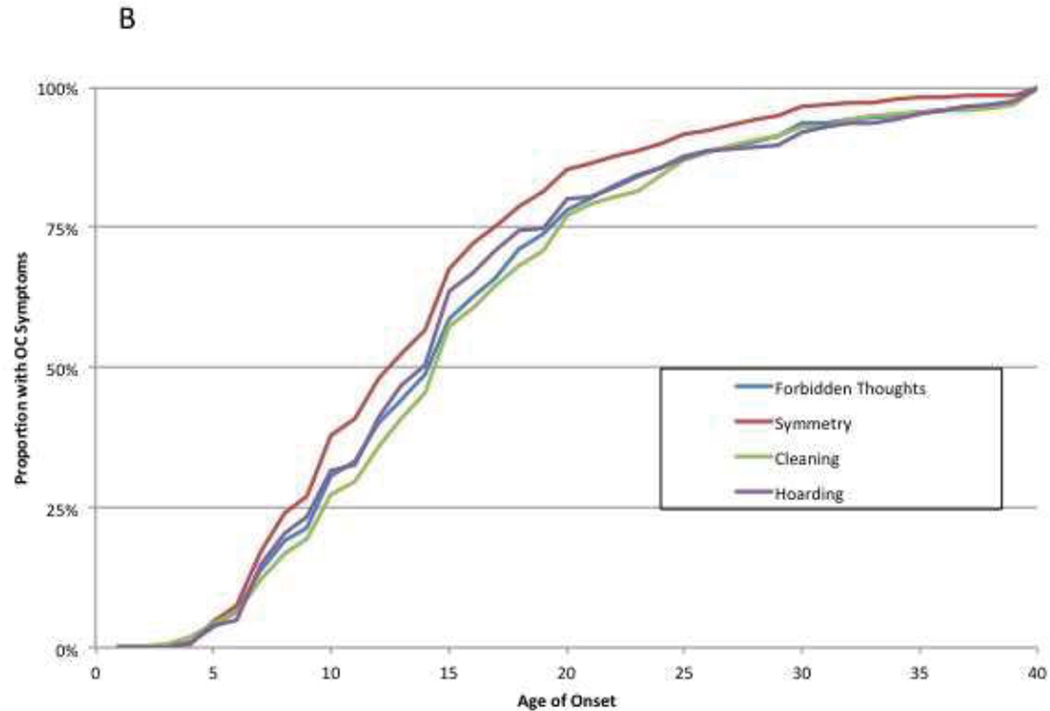
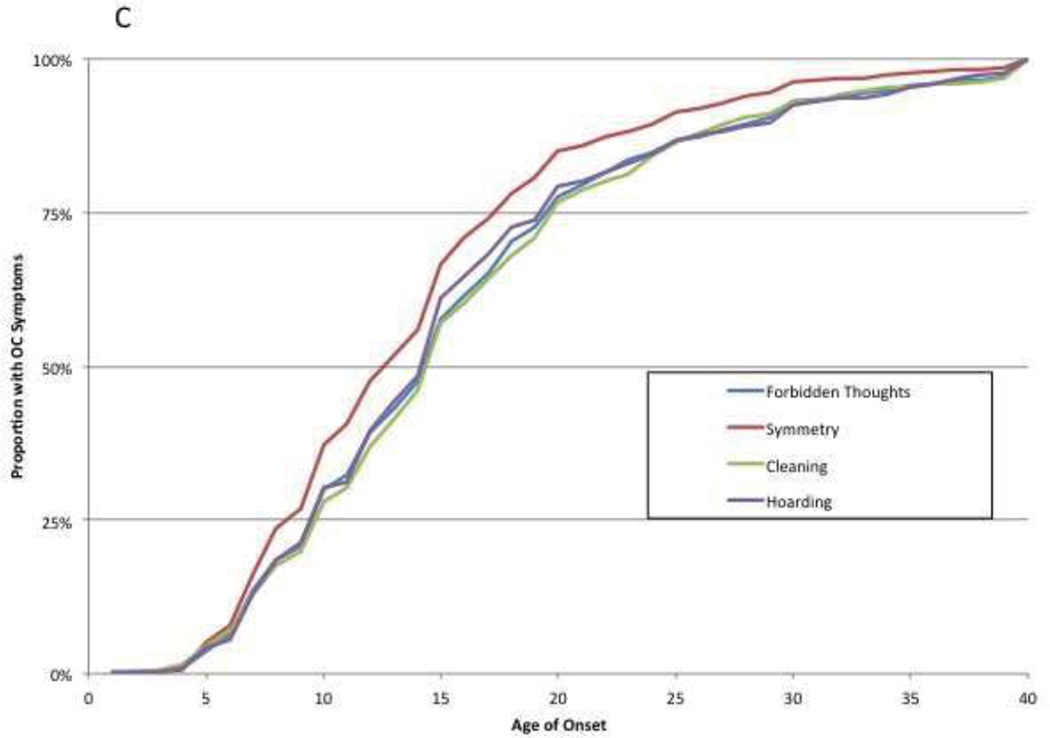
Figure 2.
A–C: Cumulative Histograms of Age of Onset by OCD Symptom Dimension. Cumulative histograms depict the proportion of subjects experiencing onset of symptoms within each OCD symptom dimension by a given age. Figures define presence of symptoms within OCD dimensions differently – Figure 2A primary symptom dimension, Figure 2B by presence of clinically significant symptoms and Figure 2C by presence of any symptoms.
We additionally conducted a sensitivity analysis where symptoms in the forbidden thoughts dimensions were separated into either sexual/religious or aggressive symptoms. Both sexual/religious (age of onset = 16.6±7.3, p < .001) and aggressive (age of onset = 19.3±10.5, p < .001) OCD symptoms were associated with a significantly later age of onset than symptoms in the symmetry dimension. The age of onset of sexual/religious and aggressive OCD symptoms did not significantly differ from other OCD symptom dimensions or from each other.
A significant association between OCD symptom dimension and age of onset was also demonstrated when symptom dimension was defined by clinically significant symptoms (F(3, 2366)= 8.53, p < .0001). As previously, OCD symptoms in the symmetry dimension (age of onset = 14.4±7.7) had an earlier age of onset than hoarding (age of onset = 15.8±8.8, p < .01), cleaning (age of onset = 16.5±8.8, p value<0.001) and forbidden thoughts (age of onset = 16.1±8.7, p < .001). No other significant differences in age of onset of symptoms were found between the OCD symptom dimensions. Figure 2B depicts a cumulative histogram of the age of onset of symptoms in each OCD dimension when defined by the presence of lifetime clinically significant symptoms. When a sensitivity analysis was conducted separating the forbidden thoughts dimension into two dimensions, both sexual/religious (age of onset = 16.5±8.1, p < .001) and aggressive (age of onset = 17.5±9.3, p < .001) OCD symptoms were associated with a significantly later age of onset than symptoms in the symmetry dimension. The age of onset of sexual/religious and aggressive OCD symptoms did not significantly differ from other OCD symptom dimensions or from each other.
A significant association between OCD symptom dimension and age of onset was demonstrated when symptom dimension was defined by the presence of any lifetime symptoms (F(3, 2738) = 8.67, p < .0001). Pairwise comparisons found that symptoms in the symmetry dimension (age of onset = 14.5±7.8) had an earlier onset than symptoms in the hoarding dimension (age of onset = 16.1±8.8, p < .001), the cleaning dimension (age of onset = 16.5±8.8, p < .001), and the forbidden thoughts dimension (age of onset = 16.3±8.8, p < .001). No other significant differences in age of onset of symptoms were found between the OCD symptom dimensions. Figure 2C depicts a cumulative histogram of the age of onset of symptoms in each OCD dimension when defined by the presence of any lifetime symptoms. When a sensitivity analysis was conducted separating the forbidden thoughts dimension into two dimensions, both sexual/religious (age of onset = 16.7±8.6, p < .001) and aggressive (age of onset = 17.5±9.3, p < .001) OCD symptoms were associated with a significantly later age of onset than symptoms in the symmetry dimension. The age of onset of sexual/religious and aggressive OCD symptoms did not significantly differ from other OCD symptom dimensions or from each other.
Effects of gender and comorbid tics on age of onset
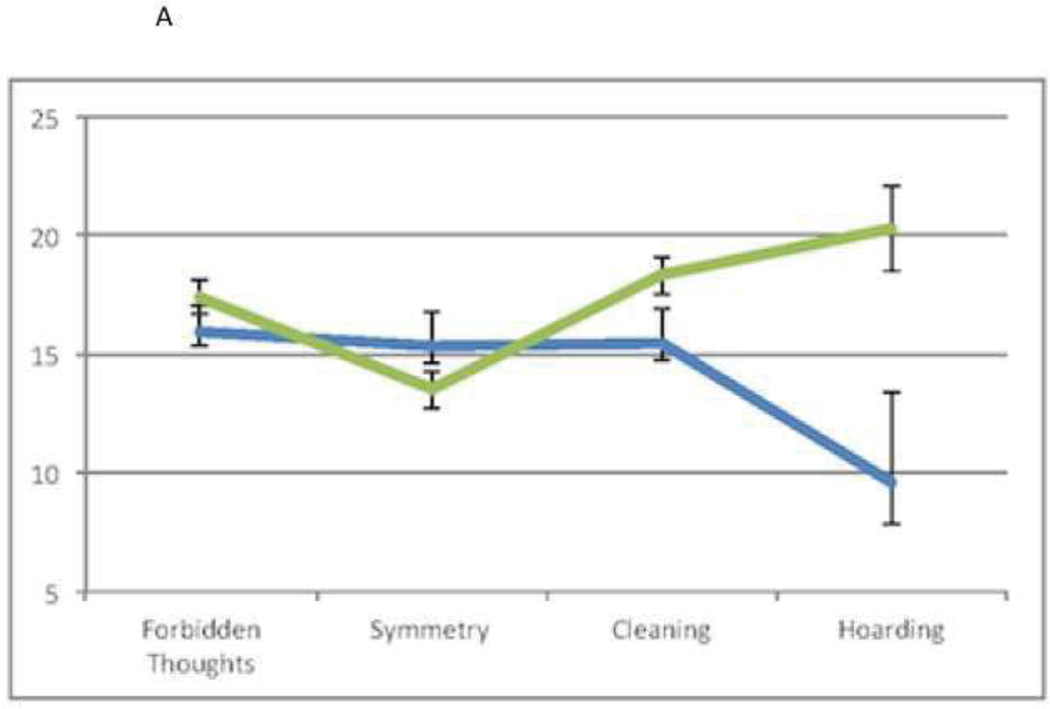
The association between symptom dimension and age of onset remained significant when we adjusted for gender and tic comorbidity. In a model adjusting for the presence of comorbid tics, a significant main effect was found for primary symptom dimension (F(3, 511) = 2.84, p = .038) and for comorbid tics (F(1, 511) = 9.69, p = .002); OCD patients with comorbid tics had an earlier age of onset. There was also a significant interaction between primary symptom dimension and comorbid tics F(3, 511) = 2.83, p = .038. Figure 3A depicts age of onset of OCD symptom dimensions stratified by presence of comorbid tics. OCD patients without comorbid tics reported an earlier age of onset for symptoms in the symmetry dimension whereas OCD patients with comorbid tics did not. OCD patients with comorbid tics had earlier age of onset of cleaning and hoarding symptoms compared to OCD patients without comorbid tics.
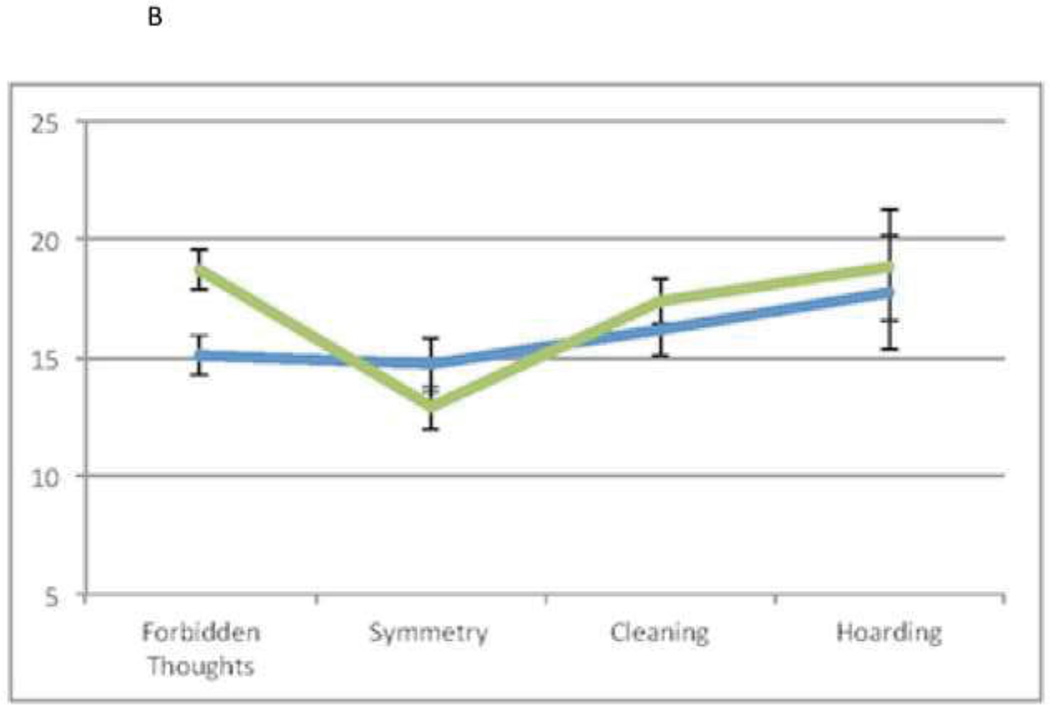
Figure 3.
A–B: Age of Onset in Symptom Dimensions Stratified by Potential Confounders. Figure 3A is stratified by the presence (blue) or absence (green) of a comorbid tic disorder. Figure 3B is stratified by gender (males-blue and females-green).
In a model adjusting for gender, one-way ANOVA found a significant main effect for primary symptom dimension (F(3, 511) = 4.6, p = .003) but not gender (F(1,511) = .92, p = .338). There was an interaction of primary dimension and gender trending towards but not reaching significance (F(3, 511) = 2.6, p = .051). A greater difference in age of onset by symptom dimension tended to be reported by females compared to males (Figure 3B).
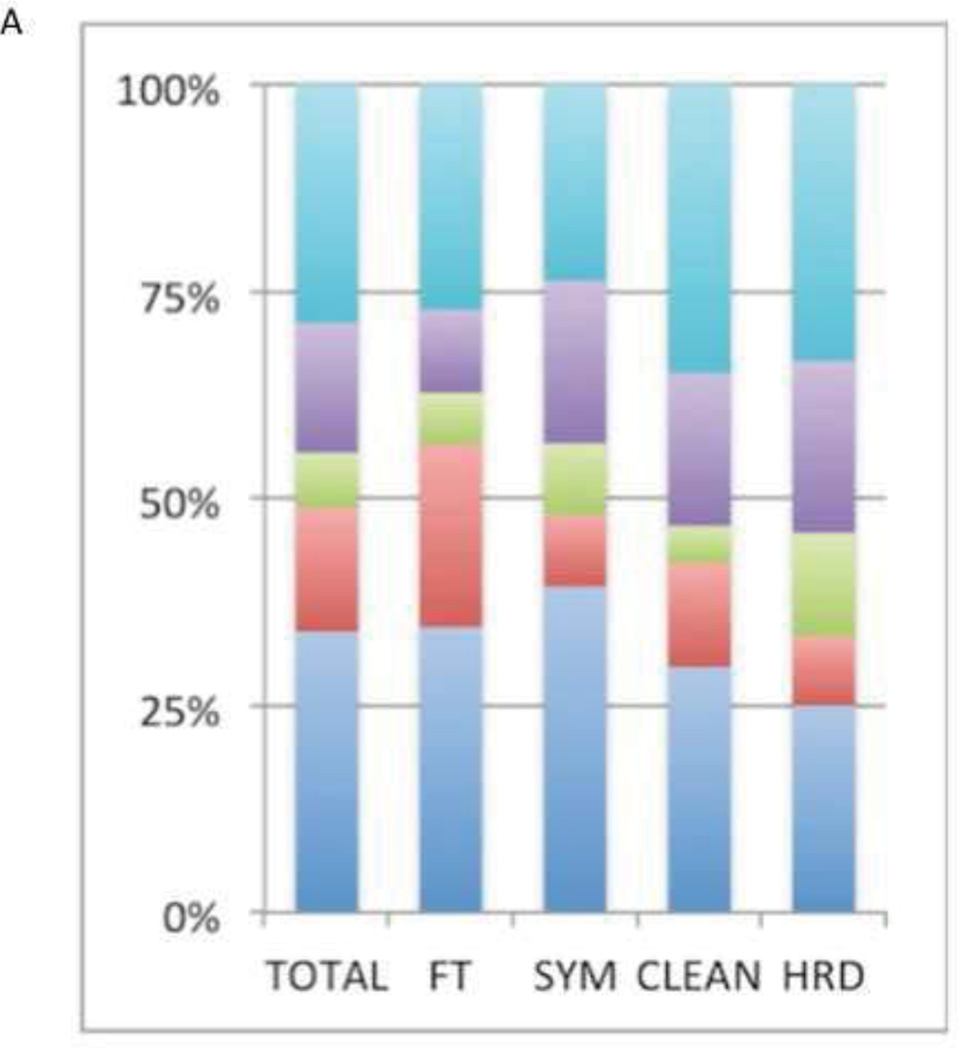
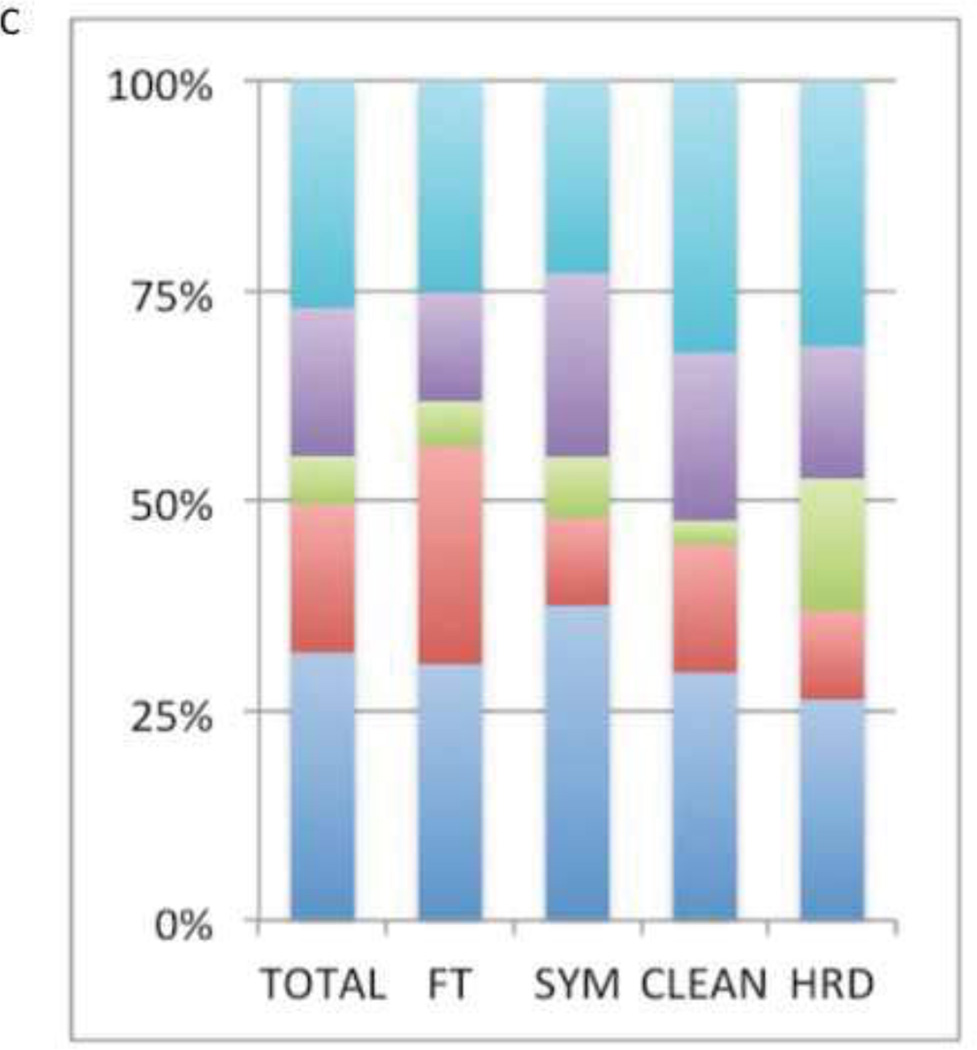
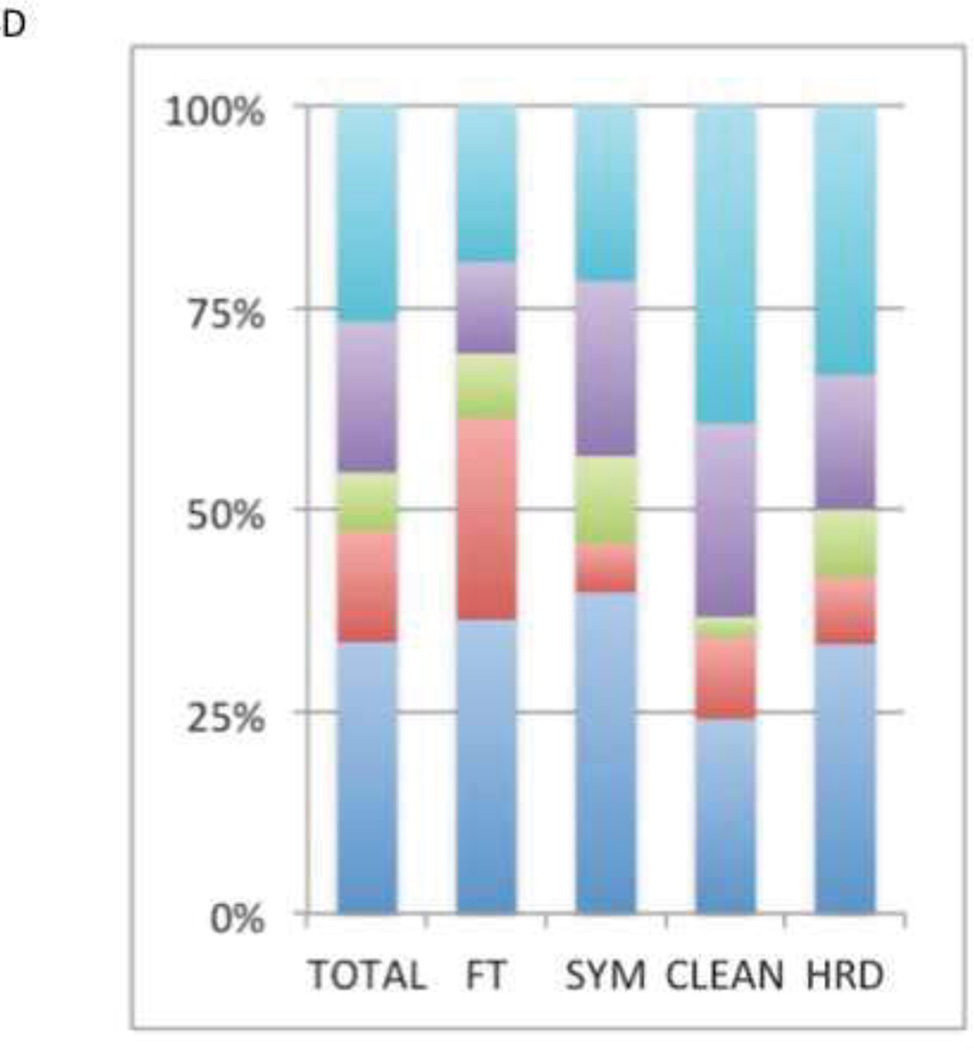
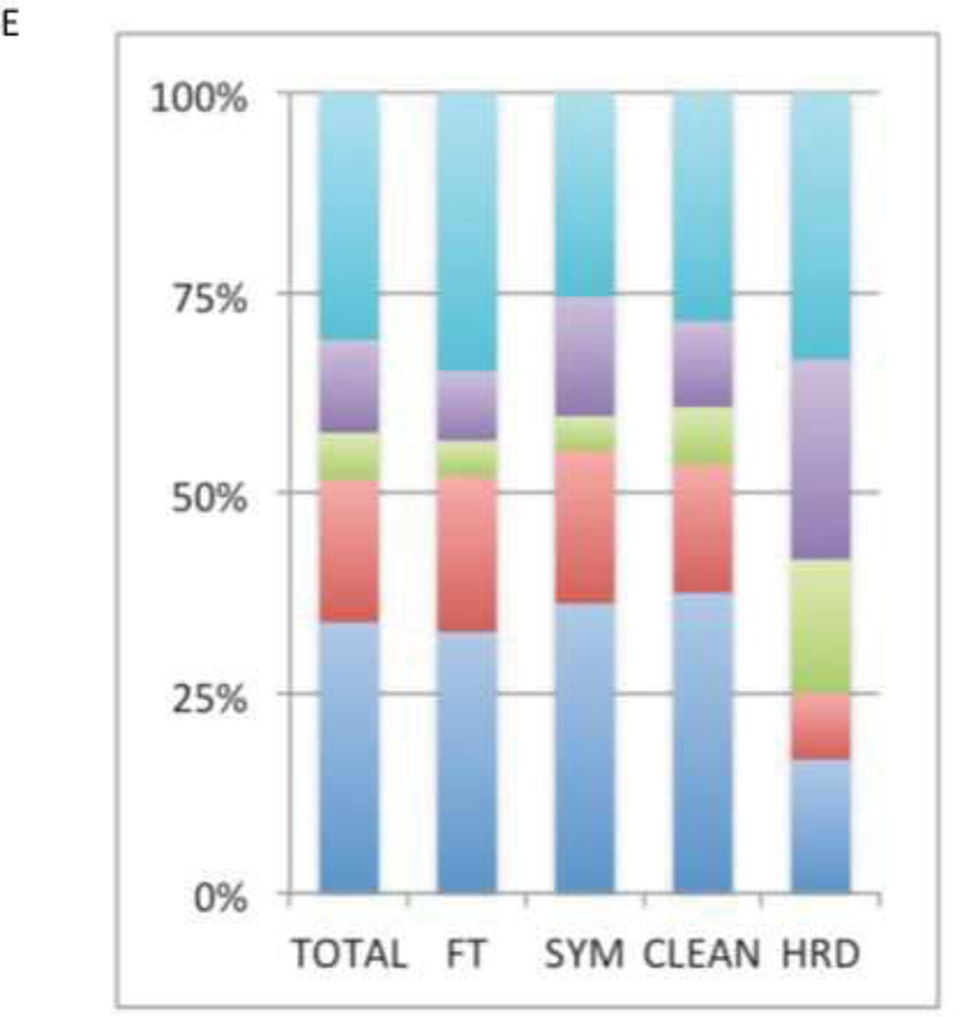
Clinical course
There was a significant association between primary OCD symptom dimension and reported clinical course of OCD symptoms (χ2(df=12, n = 466) = 25.7, p = .012). Participants with primary OCD symptoms in the forbidden thoughts dimension were more likely to endorse a fluctuating course (χ2(df=1, n = 466) = 11.9, p = .0006) and less likely to endorse a deteriorating then constant course (χ2(df=1, n = 466) = 7.1, p = .008). Participants with primary symptoms in the symmetry dimension were less likely to report their clinical course as waxing-and-waning (χ2(df=1, n = 466) = 5.8, p = .02). Participants with primary symptoms in the cleaning dimension more often reported a deteriorating course at trend levels (χ2(df=1, n = 466) = 3.4, p = .07). Figure 4A depicts the proportion of patients reporting each type of clinical course by primary OCD symptom dimension.
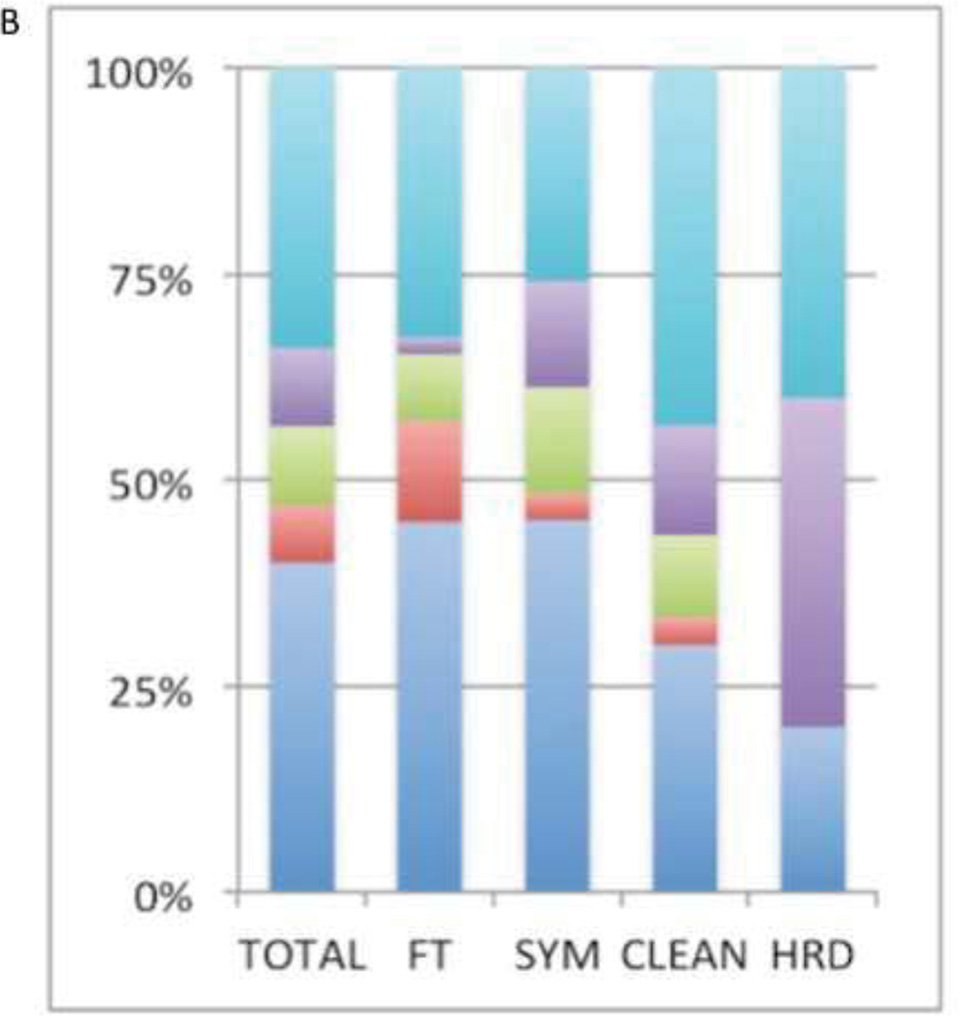
Figure 4.
A–E: Clinical course of OCD Symptom Dimensions. Figure 4A includes the entire sample, Figures 4B and 4C depict OCD patients with and without comorbid tic disorders respectively. Figures 4D and 4E depict women and men with OCD respectively. Turquoise denotes a deteriorating course; purple denotes a worsening with plateau course; green denotes a constant course; red denotes an episodic course; blue denotes a waxing and waning course.
Effects of gender and comorbid tics on clinical course
We examined the potential confounding effects of comorbid tics on the associations we found between OCD symptom dimensions and clinical course (figure 4A,B and C). The pattern of association was similar in subjects with and without tic disorders, although the significance of the effect of primary symptom dimension on clinical course was only at trend level in the patients with tics (χ2(df=12, n = 115) = 16.2, p = 0.18) and without comorbid tics (χ2(df=12, n = 351) = 20.6, p=0 .06), perhaps due to the lower number of subjects in these subgroups and therefore to reduced statistical power.
In OCD patients without tics, subjects with primary symptoms in the forbidden thoughts dimension more often reported a waxing-and-waning course (χ2(df=1, n = 351) = 9.9, p = .002) and less often reported a deteriorating then constant course at trend levels (χ2(df=1, n = 351) = 3.2, p = .07). Subjects with primary symmetry symptoms less often reported a waxing-and-waning course (χ2(df=1, n = 351) = 4.8, p = .03). In OCD patients with comorbid tics, subjects with primary symptoms in the forbidden thoughts dimension were also more likely to report a waxing-and-waning course (χ2(df=1, n = 115) = 3.8, p = .05) and less likely to report a deteriorating then constant course (χ2(df=1, n = 115) = 5.6, p = .02).
We also examined the potential confounding effects of gender on the association between OCD symptom dimension and clinical course (Figure 4A, D AND E). There was a strong, statistically significant association between OCD symptom dimension and clinical course in females (χ2(df=12, n = 262) = 31.6, p=0.002) but not males (χ2(df=12, n = 207) = 9.8, p =0.63).
Females with primary symptoms in the forbidden thoughts dimension more often reported a waxing-and-waning course (χ2(df=1, n = 262) = 14.2, p = .0002) and less often reported a deteriorating then constant course (χ2(df=1, n = 262) = 4.7, p = .03). Females with primary symmetry symptoms were less likely to report a waxing-and-waning course (χ2(df=1, n = 262) = 6.1, p = .01). Additionally, females with primary cleaning symptoms were more likely to report a deteriorating course (χ2(df=1, n = 262) = 10.2, p = .001) and less likely to report an episodic course (χ2(df=1, n = 262) = 10.2, p = .001).
Males did not demonstrate any significant association between OCD symptom dimensions and clinical course. The significant associations present in the overall sample all occurred in the same direction among males only but did not approach statistical significance (forbidden thoughts/waxing-and-waning course: χ2(df=1, n = 204) = 1.0, p = .31; forbidden thoughts/deteriorating then constant course: χ2(df=1, n = 204) = 1.5, p = .22; symmetry/waxing-and-waning course: χ2(df=1, n = 204) = 0, p = .96).
Discussion
The heterogeneity of OCD symptoms can be described along several orthogonal dimensions (1). We report that symptoms along these distinct dimensions are associated with different natural histories. Specifically, symmetry symptoms have an earlier onset than symptoms in other dimensions. Longitudinally, patients with primary symptoms in the forbidden thoughts dimension were more likely to report a waxing-and-waning course whereas patients with primary symptoms in the symmetry dimension were less likely to report a waxing-and-waning course. Females with primary OCD symptoms in the cleaning dimension were more likely to report a progressively deteriorating course.
This association between age of onset and symptom dimension is in line with previous research on this topic (Honjo, Hirano et al. 1989; Minichiello, Baer et al. 1990). Direct comparisons are difficult, as previous studies used very different methods of assessment and classification. Nevertheless, the association between symmetry symptoms and earlier age of onset has been reported previously (Mataix-Cols, Rauch et al. 1999; Denys, de Geus et al. 2004; Matsunaga, Hayashida et al. 2010). We show this association to be robust to method of analysis, as our results did not vary on how symptom dimension was defined (Figure 2B–D).
In contrast to an earlier study, we did not find an association between an earlier onset and symptoms of the forbidden thoughts (FT) dimension (Mataix-Cols, Rauch et al. 1999). Differences in methodology may explain the different results between the two studies. Specifically, the earlier study assessed global age of onset of OCD, while we assessed dimension-specific age of onset (Mataix-Cols, Rauch et al. 1999). It may be that patients with primary FT symptoms in adulthood had earlier onset of symptoms in another dimension. This would obscure the age of onset of the FT dimension itself. Our methodology avoids this confound.
The association of symmetry dimension symptoms with an earlier age of onset may be understood in a developmental context. A need for symmetry, ordering and arranging compulsions, and “just right” feelings are very common in young children (<4 years of age) (Evans, Gray et al. 1999). In some cases these symptoms can persist into adulthood. The greater prevalence of symmetry-related issues in children (as compared to other OCD-type issues) could explain our observed difference in age of onset.
The association we found between the forbidden thoughts dimension and a more fluctuating course may be due to active coping attempts by affected individuals. These symptoms are often triggered by the presence of other people or objects (e.g. obsessions about accidentally harming others), and a primary coping strategy for individuals with such symptoms is the avoidance of external symptom triggers. However, since complete avoidance is rarely possible, chance encounters with symptomatic triggers may result in symptom spikes, which may at least partially account for our finding.
We found no association between hoarding symptoms and age of onset, relative to other OCD symptoms. This result is somewhat surprising given the accumulating evidence suggesting that hoarding symptoms are distinct from the rest of OCD (Saxena 2007. The relatively few number of subjects with primary hoarding symptoms, compared to other symptom dimensions, and a consequent lack of statistical power may partially explain this lack of association. However, this was a large sample, and included over 300 patients that reported some hoarding symptoms (which were included in the analyses presented in Figure 2B and 2C even if they were not the primary OCD symptom). This lack of distinct age of onset for hoarding symptoms should not be viewed as evidence against the growing consensus that these symptoms are distinct from the rest of OCD; many other diagnostically discrete conditions such as depression, schizophrenia, and substance abuse also have similar ages of onset as OCD (Torres, Fontenelle et al. 2012).
Our study represents a significant advance over previous investigations of the relationship between symptom subtypes and the natural history of OCD. We analyzed a large, clinically referred sample of 955 adults with OCD, which provided increased power relative to previous research with much smaller samples. Our use of the standard DY-BOCS provided a continuous measure of symptom severity, whereas previous research only provided categorical data. Additionally, we were able to assess the age of onset of each OCD symptom dimension, as opposed to previous research that relied on global age of onset. Nevertheless, there remain several limitations to our study. As our data was derived from retrospective patient reports, its accuracy may be affected by factors such as level of insight, comorbid conditions, or the distortions in memory that can always complicate retrospective data. Our main question probing retrospective clinical course has never been validated. In addition, treatment factors were not controlled for, and thus it is possible that the treatment history of our subjects affected the results, particularly as related to clinical course.
In conclusion, we find that different dimensions of OCD symptoms are associated with different patterns of natural history. Specifically, symmetry symptoms tend to have the earliest onset and a less fluctuating longitudinal course; forbidden thoughts symptoms more often had a waxing-and-waning course; and cleaning symptoms were more likely to have a progressively deteriorating course, among females only. Future studies prospectively evaluating the age of onset and course of symptom dimensions would be beneficial. Age of onset can be evaluated in several ways (initial subclinical symptoms vs. initial clinical symptoms; global symptoms vs. specific subtypes of symptoms). Heterogeneity in the definition of symptom onset may explain the heterogeneity in research on these matters (although we found similar results when onset was described in different ways; Figure 2A–C).
Acknowledgements
This study was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, grant 2005/ 55628-8 to Dr. Miguel) and from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ, grant 573974/2008-0 to ECM). We thank Aristides V. Cordioli, MD, PhD; Katia Petribu, MD, PhD; Christina H. Gonzalez, MD, PhD; Maria Alice de Mathis, MsC, and all colleagues from the Brazilian Research Consortium of Obsessive-Compulsive Spectrum Disorders (C-TOC) for their help with data collection.
The authors acknowledge the National Institute of Mental Health support of the Yale Child Study Center Research Training Program (MHB), National Institutes of Health grants K23MH091240 (MHB) and K08MH081190 (CP), the APIRE/Eli Lilly Psychiatric Research Fellowship (MHB), the AACAP/ Eli Lilly Junior Investigator Award (MHB), the Trichotillomania Learning Center (MHB), NARSAD (MHB), the Doris Duke Charitable Foundation (CP), and UL1 RR024139 from the National Center for Research Resources, a component of the National Institutes of Health, and NIH roadmap for Medical Research (MHB, CP).
Footnotes
Disclosures: The authors have no conflicts of interest to disclose
References
- Bloch MH, Craiglow BG, et al. Predictors of early adult outcomes in pediatric-onset obsessive-compulsive disorder. Pediatrics. 2009;124(4):1085–1093. doi: 10.1542/peds.2009-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloch MH, Landeros-Weisenberger A, et al. Meta-analysis of the symptom structure of obsessive-compulsive disorder. The American journal of psychiatry. 2008;165(12):1532–1542. doi: 10.1176/appi.ajp.2008.08020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloch MH, Peterson BS, et al. Adulthood outcome of tic and obsessivecompulsive symptom severity in children with Tourette syndrome. Archives of pediatrics & adolescent medicine. 2006;160(1):65–69. doi: 10.1001/archpedi.160.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Mathis MA, Diniz JB, et al. Early onset obsessive-compulsive disorder with and without tics. CNS spectrums. 2009;14(7):362–370. doi: 10.1017/s1092852900023014. [DOI] [PubMed] [Google Scholar]
- Denys D, de Geus F, et al. Use of factor analysis to detect potential phenotypes in obsessive-compulsive disorder. Psychiatry research. 2004;128(3):273–280. doi: 10.1016/j.psychres.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Evans DW, Gray FL, et al. The rituals, fears and phobias of young children: insights from development, psychopathology and neurobiology. Child psychiatry and human development. 1999;29(4):261–276. doi: 10.1023/a:1021392931450. [DOI] [PubMed] [Google Scholar]
- Ferrao YA, Shavitt RG, et al. Clinical features associated to refractory obsessive-compulsive disorder. Journal of affective disorders. 2006;94(1-3):199–209. doi: 10.1016/j.jad.2006.04.019. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, et al. Scructured clinical interview for DSM-IV axis I disorders-Patient edition. New York: Biometrics Reseach Department, New York Psychiatric Institute; 1995. [Google Scholar]
- Hasler G, Pinto A, et al. Familiality of factor analysis-derived YBOCS dimensions in OCD-affected sibling pairs from the OCD Collaborative Genetics Study. Biological psychiatry. 2007;61(5):617–625. doi: 10.1016/j.biopsych.2006.05.040. [DOI] [PubMed] [Google Scholar]
- Honjo S, Hirano C, et al. Obsessive-compulsive symptoms in childhood and adolescence. Acta psychiatrica Scandinavica. 1989;80(1):83–91. doi: 10.1111/j.1600-0447.1989.tb01304.x. [DOI] [PubMed] [Google Scholar]
- Labad J, Menchon JM, et al. Gender differences in obsessive-compulsive symptom dimensions. Depression and anxiety. 2008;25(10):832–838. doi: 10.1002/da.20332. [DOI] [PubMed] [Google Scholar]
- Landeros-Weisenberger A, Bloch MH, et al. Dimensional predictors of response to SRI pharmacotherapy in obsessive-compulsive disorder. Journal of affective disorders. 2010;121(1-2):175–179. doi: 10.1016/j.jad.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lochner C, Stein DJ. Heterogeneity of obsessive-compulsive disorder: a literature review. Harvard review of psychiatry. 2003;11(3):113–132. doi: 10.1080/10673220303949. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Marks IM, et al. Obsessive-compulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: results from a controlled trial. Psychotherapy and psychosomatics. 2002;71(5):255–262. doi: 10.1159/000064812. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Rauch SL, et al. Use of factor-analyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive-compulsive disorder. The American journal of psychiatry. 1999;156(9):1409–1416. doi: 10.1176/ajp.156.9.1409. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Wooderson S, et al. Distinct neural correlates of washing, checking, and hoarding symptom dimensions in obsessive-compulsive disorder. Archives of general psychiatry. 2004;61(6):564–576. doi: 10.1001/archpsyc.61.6.564. [DOI] [PubMed] [Google Scholar]
- Matsunaga H, Hayashida K, et al. The clinical utility of symptom dimensions in obsessive-compulsive disorder. Psychiatry research. 2010;180(1):25–29. doi: 10.1016/j.psychres.2009.09.005. [DOI] [PubMed] [Google Scholar]
- Miguel EC, Ferrao YA, et al. The Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders: recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Revista brasileira de psiquiatria. 2008;30(3):185–196. doi: 10.1590/s1516-44462008000300003. [DOI] [PubMed] [Google Scholar]
- Miguel EC, Leckman JF, et al. Obsessive-compulsive disorder phenotypes: implications for genetic studies. Molecular psychiatry. 2005;10(3):258–275. doi: 10.1038/sj.mp.4001617. [DOI] [PubMed] [Google Scholar]
- Minichiello WE, Baer L, et al. Age of onset of major subtypes of obsessivecompulsive disorder. Journal of anxiety disorders. 1990;4:147–150. [Google Scholar]
- Rauch SL, Dougherty DD, et al. Neural correlates of factor-analyzed OCD symptom dimensions. CNS spectrums. 1998;3:37–43. [Google Scholar]
- Rettew DC, Swedo SE, et al. Obsessions and compulsions across time in 79 children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31(6):1050–1056. doi: 10.1097/00004583-199211000-00009. [DOI] [PubMed] [Google Scholar]
- Rosario-Campos MC, Miguel EC, et al. The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Molecular psychiatry. 2006;11(5):495–504. doi: 10.1038/sj.mp.4001798. [DOI] [PubMed] [Google Scholar]
- Samuels J, Shugart YY, et al. Significant linkage to compulsive hoarding on chromosome 14 in families with obsessive-compulsive disorder: results from the OCD Collaborative Genetics Study. The American journal of psychiatry. 2007;164(3):493–499. doi: 10.1176/ajp.2007.164.3.493. [DOI] [PubMed] [Google Scholar]
- Saxena S. Is compulsive hoarding a genetically and neurobiologically discrete syndrome? Implications for diagnostic classification. The American journal of psychiatry. 2007;164(3):380–384. doi: 10.1176/ajp.2007.164.3.380. [DOI] [PubMed] [Google Scholar]
- Torres AR, Fontenelle LF, et al. Clinical features of obsessive-compulsive disorder with hoarding symptoms: a multicenter study. Journal of psychiatric research. 2012;46(6):724–732. doi: 10.1016/j.jpsychires.2012.03.005. [DOI] [PubMed] [Google Scholar]