Abstract
Background
To date, research on mental health in HIV-affected children (children who have an HIV-positive caregiver or live with the virus themselves) has focused on risk factors associated with the disease. However, simultaneous identification of factors that contribute to resilience in the face of risks is also needed. A greater understanding of modifiable protective processes that contribute to resilience in the mental health of children affected by HIV can inform the design of interventions that bolster naturally-occurring supports and contribute to early prevention or better management of risks.
Methods
We reviewed the recent literature on mental health and resilience in children and adolescents affected by HIV/AIDS. Literature searches of PsycInfo and PubMed were conducted during July-December 2011 consistent with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards. Qualitative and quantitative studies were included for review if primary research questions pertained to mental health and coping or protective processes in children and families affected by HIV/AIDS. All studies subject to full review were evaluated for quality using a modified Systematic Assessment of Quality in Observational Research (SAQOR) rating system.
Results
171 unique studies were returned from online searches of the literature and bibliography mining. Of these, 29 were evaluated as pertaining directly to mental health and resilience in families and children living with HIV/AIDS. Eight studies presented qualitative analyses. Ten quantitative studies examined individual resources contributing to child resilience and four quantitative studies looked at family-level resources. Ten studies also investigated community-level interactions. Four presented findings from resilience-focused interventions.
Conclusions
There is a clear need for rigorous research on mental health and resilience in HIV-affected children and adolescents. The evidence base would greatly benefit from more standardized and robust approaches to thinking about resilience from an ecological perspective inclusive of resources at multiple levels and their interactions.
Keywords: HIV/AIDS, Children, Families, Resilience, Mental Health
Background
Impact of HIV/AIDS on mental health in the family and community
HIV/AIDS poses direct threats to child and adolescent mental health as well as family functioning and well-being. At present, UNAIDS estimates that nearly 17 million children have been orphaned by HIV/AIDS, 90% of whom live in sub-Saharan Africa (Joint United Nations Programme on HIV/AIDS, 2010). However, orphans are only one part of the problem. An even greater number of children live with HIV-positive family members. For these young people, risks are numerous, including the pressure to drop out of school to care for sick relatives and the psychological burden associated with witnessing caregiver illness and coping with death.
Globally, approximately 2.1 million children under the age of 15 are living with HIV, and more than 280,000 died of AIDS in 2008 (Joint United Nations Programme on HIV/AIDS, 2010). In some of the most affected countries, such as Botswana and Zimbabwe, AIDS is now the leading cause of death in children under the age of 5 (Mason, 2006; Mathers, Boerma, & Ma Fat, 2009). In many parts of the globe, young people, particularly young women, are at great risk of contracting the virus through sexual activity as well as sexual exploitation and abuse. Recent estimates indicate that 40% of all new HIV infections—approximately 6,200 every day—are among young people between the ages of 15 to 24 (UNAIDS, 2008).
HIV and mental health are often described as having bi-directional relationships, meaning that the effects of living with HIV/AIDS or having an affected family member can increase risk for mental illnesses such as depression and anxiety, while poor mental health can inspire behaviors which place individuals at risk for HIV (Briere & Jordan, 2004; Cluver, Gardner, & Operario, 2007; Cluver, Orkin, Gardner, & Boyes, 2011). In families, psychological sequelae related to HIV/AIDS have been shown to predict parental depression, hopelessness, and risk behaviors such as drug abuse (Rochat et al., 2006), which may in turn lead to increased mental health problems among children (Smith Fawzi et al., 2010). Overly aggressive discipline, poor interpersonal functioning, and violence between parents may also be associated with HIV in the family (Forehand, Biggar, & Kotchick, 1998; Garcia-Moreno & Watts, 2000; Gielen et al., 2007). Disease progression and parental impairment can result in task-shifting within the family, with children taking on adult responsibilities such as caring for younger siblings or, in many low resource settings, dropping out of school to earn money (Cluver & Operario, 2008). These issues are particularly salient for children orphaned by AIDS (Pelton & Forehand, 2005). Young people may also have anxieties about their own health status, as well as misconceptions about how HIV is transmitted and the risk of contracting it from an HIV-positive caregiver.
HIV/AIDS also amplifies vulnerability to risk factors at the community level. Stigma related to the illness often erodes social supports that have traditionally supported families and children in challenging circumstances (Cluver & Orkin, 2009). Work opportunities, inclusion in religious organizations, and perceived social equity may all be compromised by lack of community understanding or sensitization to HIV (Anderson et al., 2008; Rutta et al., 2008; Salisbury, 2000). Evaporation of resources due to medical bills combined with loss of employment or difficulty finding and sustaining work can compound other risk factors and drive families into poverty (Silver, Bauman, Camacho, & Hudis, 2003). While access to anti-retroviral treatment (ART) and other forms of HIV-related health care is improving (Perez et al., 2004; Betancourt, Abrams, McBain, & Fawzi, 2010), systems of social protection and social welfare to better support the socio-emotional needs of children orphaned or made vulnerable due to HIV/AIDS remain weak or nonexistent (UNAIDS, UNICEF, & USAID, 2004; UNICEF, 2006).
Resilience despite HIV/AIDS
In order to contribute to early prevention or better management of ongoing risks, resources for promoting resilience in HIV-affected families and communities must be better understood. In particular, research that applies a developmental and ecological lens to the study of resilience has high potential to illuminate how mental health and well-being are shaped by the interplay between individual, family, community, and societal factors (Masten, 2001; Sapienza & Masten, 2011). In his original writings on the social ecology, Bronfenbrenner stressed how “settings” of development interact with one another to support positive child development, creating a nurturing physical and emotional environment that includes, and extends beyond, the immediate family to peer, school and community settings, and cultural and political belief systems (Bronfenbrenner, 1979). For children, HIV represents a fundamental alteration of the social ecology which undergirds healthy child development, disrupting variables at the individual, family and peer/community levels (Benard, 1995) that ordinarily mitigate risks and promote resilience (Cowan, Cowan, & Schulz, 1996; Werner, 1989). Stabilizing a compromised social ecology is therefore fundamental to improving and safeguarding the mental health of HIV-affected children as their setting of development changes to respond to HIV in the family.
Investigations that leverage social ecological theories in the context of HIV/AIDS can help broaden what is known about factors contributing to children’s long-term well-being, and can contribute to the growing evidence base on protective processes that help children achieve good functioning despite exposure to a range of difficult life circumstances (Betancourt, McBain, Newnham, & Brennan, In press; Evans, 2005; Luthar & Goldstein, 2004). To date, however, there is little coordination across research on resilience in HIV/AIDS-affected children and families, and resultant gaps in the evidence base limit our understanding of an integrated social ecological model of resilience in the mental health of HIV/AIDS-affected children and adolescents.
This paper examines the concept of resilience in children affected by HIV/AIDS with particular attention to potentially modifiable protective processes which may be the targets of intervention. Though various definitions of resilience are used in the literature (Luthar, 1993, 2004; Luthar, Cicchetti, & Becker, 2000; Luthar & Cushing, 1999; Masten, 1994; Rutter, 1985, 1987), we define resilience as the attainment of desirable social and emotional adjustment, despite risks due to HIV (Luthar, 1993; Rutter, 1985). With this definition, we acknowledge the well-documented risks facing children affected by HIV/AIDS, and seek to highlight the physical, social and individual outcomes relevant to their healthy development and “resistance to environmental risk experiences, or the overcoming of stress or adversity” (Rutter, 2006). Because the protective processes and factors mitigating the impact of risks have not been well explored in this population, it is important to understand the full range of processes with potential to increase resilience in HIV/AIDS-affected children, and to use this knowledge to develop interventions that may be implemented at different levels.
In the present review, we aim to organize existing resilience research using a social-ecological model; the goal is to achieve an integrative review of what is known about resilience in HIV/AIDS-affected families and children, and to provide recommendations for future research. Questions of interest include:
To date, what strengths and resources at the individual, family, and community levels have been identified as contributing to resilience in HIV/AIDS-affected families and children?
What clinical or intervention strategies exist to bolster resilient mental health outcomes in HIV/AIDS-affected families and children? What processes contributing to resilience are targeted by these interventions?
What innovations are recommended in future research on resilience in HIV/AIDS-affected children and families?
Methods
Literature search
To identify studies evaluating mental health and resilience in families and children living with HIV/AIDS, we conducted a systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards (Moher, Liberati, Tetzlaff, Altman, & The PRISMA Group, 2009). Inclusion criteria included being: (a) a peer-reviewed, original research article that (b) studied resilience and (c) mental health in (d) children under age 18 OR in families with children under age 18. Subjects included children and adults of both sexes from across the globe. Studies were excluded if they did not explicitly examine resilience constructs or mental health. Opinion pieces, reviews, and articles focusing only on adults in families were also excluded.
To conduct the review, we searched PubMed and PsycINFO from 1990 to December 2011 for all peer-reviewed, English language publications which contained key words within a matrix of relevant terminology (Table 1).
Table 1.
Matrix of search terminology
| Search terms for subjects | [AND] | Search terms for HIV | [AND] | Search terms for resilience | [AND] | Search terms for mental health |
|---|---|---|---|---|---|---|
| Child* [or] | HIV [or] | Resilien* [or] | Mental health [or] | |||
| Adolesc* [or] | AIDS | Protective factors [or] | Psycholog* [or] | |||
| Family [or] | Protective processes [or] | Psychiatr* [or] | ||||
| Families | Coping [or] | Internalizing [or] | ||||
| Adaptive coping | Anxiety [or] | |||||
| Depression [or] | ||||||
| MDD [or] | ||||||
| Trauma [or] | ||||||
| Externalizing [or] | ||||||
| Conduct |
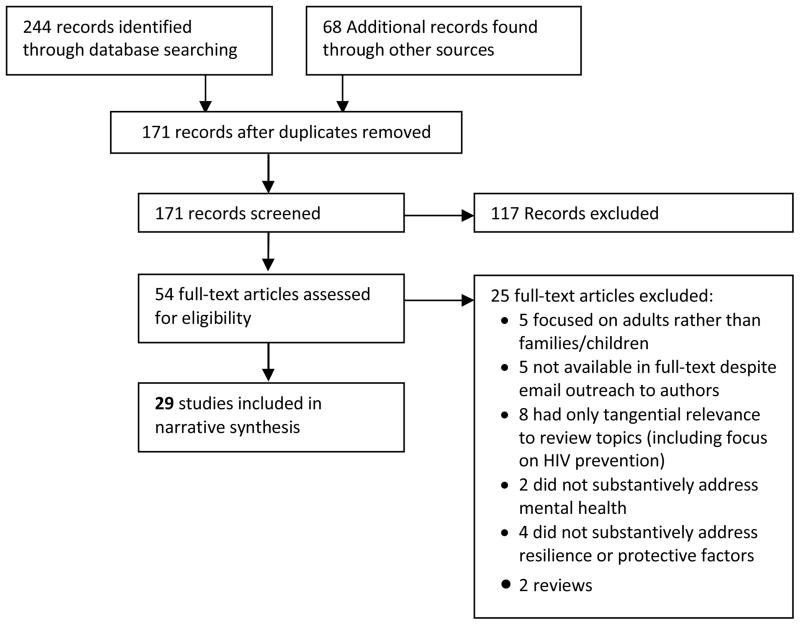
Figure 1 presents the systematic review process. A total of 244 records were returned from database queries; when duplicates were eliminated, 103 remained. An additional 68 records were identified through bibliography mining and direct outreach to experts in the field. Of the 171 unique studies, 54 met the screening criteria listed above. These articles were read in full and coded for quality and for focus on mental health, resilience, and protective processes (see Analysis). Suitability for inclusion in full review was assessed and 25 studies were eliminated. The remaining 29 articles were included in the final analysis and narrative synthesis. Because the evidence base on the topics of interest is limited, both quantitative and qualitative studies contributed to the final selection.
Figure 1.
Systematic review following PRISMA standards
Analysis
In accordance with emerging best practices for conducting systematic reviews, we first evaluated included studies for author, year of publication, journal, objectives, population, design, and methodology. To assess the quality of evidence, we used a rating system developed by Ross et al. (2011). The Systematic Assessment of Quality in Observational Research (SAQOR) was ideal for the present review since it can be flexibly applied to both quantitative and qualitative studies. Using SAQOR, the rater can adjust for factors that are “non-applicable” to qualitative studies (e.g., use of controls, randomized samples), and thereby harmonize scores across different types of studies (Downs & Black, 1998; Guyatt et al., 2008). During evaluation, the rater assesses a range of criteria by answering yes or no questions about the study’s design (see Appendix 1). Each criterion is then grouped within a sub-category, which is graded “Adequate”, “Inadequate”, “Unclear,” or “Not Applicable” depending on the number of positive (or not-applicable) responses. A grade of overall quality—High, Moderate, Low, Very Low—is then determined based on performance in each of the six sub-categories.
Appendix 1.
SAQOR Criteria
| Sampling | Control/Comp. | Quality of measures | Follow-up | Distorting influences | Reporting of data | |
|---|---|---|---|---|---|---|
| Sample is representative of the population | Control group is included (required for quant. studies) | Adequate assessment of exposure to HIV/AIDS | Number of participants lost to follow-up stated | Confounders stated | Missing data is stated and addressed | |
| Source of sample is clear | Control group is easily identifiable | Adequate measure of outcomes | Explanation for loss to follow-up stated | Potential confounders considered, assessed, and accounted for in analysis | Data are clearly and accurately presented | |
| Sampling method is described | Source of controls is clear | All data numbers add up | ||||
| Sample size is adequate to identify statistical differences between groups for primary outcomes | Controls are matched or randomized | There is no confusion in regards to any data presented | ||||
| Inclusion/Exclusion criteria are clear and justified | Statistical differences between cases and controls have been controlled for | |||||
| Adequate | Meets 3–5 criteria | Meets 3–5 criteria | Meets both criteria | Meets 1–2 criteria | Meets both criteria | Meets 3–4 criteria (2–3 when missing data is N/A) |
| Inadequate | Meets 0–2 criteria | Meets 0–2 criteria | Meets 0–1 criteria | Meets 0 criteria | Meets 0–1 criteria | Meets 0–2 criteria (0–1 when missing data is N/A) |
| Unclear | 3–5 criteria “Unclear” | 3–5 criteria “Unclear” | 1–2 criteria “Unclear” | 1–2 criteria “Unclear” | Both criteria “Unclear” | Must be either Adequate or Inadequate |
| N/A | Sampling criteria applicable to all studies | Qualitative and observational studies | Qualitative and observational studies | Qualitative and observational studies | Qualitative and observational studies | Reporting of data criteria applicable to all studies |
| FINAL RATINGS | ||
|---|---|---|
| Qualitative | Quantitative | |
| HIGH | 5–6 Adequate | |
| MODERATE | 2 Adequate AND strong, consistent evidence | 4 Adequate |
| LOW | 1–2 Adequate | 3 Adequate |
| VERY LOW | 2 Inadequate | 4–6 Inadequate |
| Down 1 grade if: | Serious limitations; Important inconsistency | Cross-sectional only; Serious limitations; Important inconsistency |
| Up 1 grade if: | Strong, consistent, and direct evidence | RCT design; Strong, consistent, and direct evidence |
Normally, SAQOR gives preference to randomized controlled trials (RCT) by upgrading studies if they meet RCT standards and downgrading them if a design is cross-sectional. In this review, we modified SAQOR to award similar upgrades to observational and qualitative studies that demonstrated strong quality indicators in required fields as well as strong, consistent, and direct evidence. This adaptation acknowledges that the research questions for qualitative studies are different than those in survey research, and allows for more sensitivity to the level of evidence produced by qualitative research. Following these adapted SAQOR guidelines, studies were considered to have “High” quality if five or more domains were adequate; “Moderate” quality if evidence was strong AND 2 (for qualitative) or 4 (for quantitative) required domains were adequate; “Low” quality if 1 (for qualitative) or 3 (for quantitative) required domains were inadequate; “Very Low” if 2 (for qualitative) or 4 (for quantitative) required domains were inadequate.
In our study, two graders worked independently to evaluate each study using the SAQOR system. Graders achieved 90% agreement; discrepancies between grades were discussed by the authors, and studies were re-evaluated as needed to address points of disagreement. Final SAQOR grades were determined by consensus and are available in Appendix 2.
Appendix 2.
Level of evidence of reviewed studies
| SAQOR Rating | ||||||||
|---|---|---|---|---|---|---|---|---|
| References | Sampling | Control/Comp. | Quality of measures | Follow-up | Distorting influences | Reporting of data | Quality | Notes |
| Ayres et al., 2006 | Adequate | N/A | N/A | N/A | N/A | Adequate | LOW | Does not focus on resilience; mental health outcomes not reported |
| Betancourt, Rubin-Smith et al., 2011; Betancourt, Meyers-Ohki et al., 2011 | Adequate | N/A | N/A | N/A | N/A | Adequate | MOD | Plus 1: Strong, no plausible confounders, consistent and direct evidence |
| Brook et al., 2002 | Adequate | N/A | N/A | N/A | N/A | Adequate | MOD | Plus 1: Strong, no plausible confounders, consistent and direct evidence |
| Cluver et al., 2007 | Adequate | Inadequate matching; source unclear | Adequate | N/A | Steps to account for confounding unclear | Adequate | LOW |
Minus 1: Cross-sectional only Comparison to a sample of community adolescents is not adequately described; study focuses mainly on coping specifically, without mention of resilience; Fathers who were HIV+ OR “at risk” of contracting HIV comprised the same sample; Causal pathways may be bi-directional, or may be influenced by mothers |
| Cluver et al., 2009 | Adequate | N/A | N/A | N/A | N/A | Adequate | MOD | Plus 1: Strong, no plausible confounders, consistent and direct evidence |
| Daniel et al., 2007 | Adequate | Adequate | Adequate | N/A | Inadequate | Adequate | MOD | This study did not examine mental health problems that could confound PTSD symptoms and perceptions of social support |
| Doku et al., 2010 | Adequate | N/A | N/A | N/A | N/A | Adequate | MOD |
Plus 1: Strong, no plausible confounders, consistent and direct evidence The focus of this study is clearly defined, and uses qualitative data effectively to illustrate arguments for disclosure of HIV status as resilience-enhancing |
| Dutra et al., 2010 | Adequate | Adequate | Inadequate | N/A | Adequate | Adequate | MOD | This study was limited by its minimal exploration of resilience (focused mainly on mental health outcomes) |
| Fang et al., 2009 | Adequate | Inadequate1 | Adequate | N/A | Adequate | Adequate | MOD |
Minus 1: Cross-sectional only Plus 1: Strong, no plausible confounders, consistent and direct evidence High relevance to topic of interest; Some imprecision should be noted (study tools not validated for this demographic – steps taken to correct) |
| Funck-Brentano et al., 2005 | Adequate | Adequate | Adequate | Adequate | Steps to account for confounding unclear | Adequate | MOD | Minus 1: Serious limitations This intervention study was limited by its small sample size and narrow exploration of resilience factors. Methods to create the study control groups are well-explained, but may have limited validity. |
| Garvie et al., 2011 | Adequate | Adequate | Adequate | N/A | Adequate | Adequate | HIGH | Sample not representative of general population (sample largely drawn from one ethnic background); Some psychological scales demonstrated low reliability; HIV status of enrolled children not known |
| Harms et al., 2009 | Inadequate | Inadequate1 | Inadequate | Inadequate | Steps to account for confounding unclear | Inadequate2 | VERY LOW | Study seriously limited by small sample size; inadequate information on recruitment, inclusion/exclusion criteria, missingness; study was largely limited to measures of coping and did not assess other factors of resilience |
| Kumakech et al., 2009 | Adequate | Adequate | Inadequate | Adequate | Adequate | Inadequate2 | LOW |
Minus 1: Serious limitations This study was limited in its relevance to child resilience. Only one subscale of ‘self-concept’ was used to assess positive attributes/constructs. Results are further limited by the differences in baseline characteristics of the two groups, and by clustering effects. |
| Leonard et al., 2008 | Adequate (Small) | N/A | N/A | N/A | N/A | Adequate | MOD | Plus 1: Strong, no plausible confounders, consistent and direct evidence |
| Lyon et al., 2011 | Adequate | Adequate | Adequate | N/A | Steps to account for confounding unclear | Adequate | MOD |
Minus 1: Uncertainty of conclusions This report on baseline characteristics of a sample for an RCT is somewhat unclear. Authors do not clearly describe how complex parental social histories may confound results. Conclusions related to resilience are somewhat superficial/speculative |
| Moss et al., 1998 | Adequate | Adequate | Inadequate | Adequate | Adequate | Adequate | MOD |
Minus 1: Uncertainty of conclusions related to mental health and resilience Limited scope of resilience and mental health measures; study focuses on associations between spirituality and adherence |
| Murphy et al., 2000 | Adequate (Small) | Inadequate1 | Adequate | Adequate description | Confounding recognized but not accounted for | Adequate | MOD |
Minus 1: Cross-sectional only Study was limited by a small sample size and lack of a comparison group; while confounding due to social context was recognized, authors were unable to address this in analysis |
| Murphy et al., 2008 | Adequate | Inadequate1 | Adequate | Adequate | Steps to account for confounding unclear | Adequate | MOD |
Minus 1: Cross-sectional only Moderate attrition; hierarchical cluster analysis leaves room for some bias |
| Nichols et al., 2000 | Adequate | Inadequate1 | Adequate | N/A | Adequate | Inadequate2 | LOW | Minus 1: Cross-sectional only |
| Orban et al., 2010 | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate | HIGH | This well-designed study was limited by use of caregiver report only (i.e., no child self-report) |
| Petersen et al., 2010 | Adequate | Adequate | Adequate | N/A | Adequate | Inadequate2 | MOD | This baseline study is somewhat limited by lack of HIV-negative control group, and by use of child self-report measures only |
| Pivnick et al., 2000 | Adequate | N/A | N/A | N/A | N/A | Adequate | MOD | Plus 1: Strong, no plausible confounders, consistent and direct evidence |
| Rosenblum et al., 2005 | Adequate (Small) | Inadequate1 | Adequate | Inadequate | Inadequate | Inadequate2 | LOW | This article does a good job contextualizing the population’s experience, but quantitative links/pathways to resilience are weak and there is inadequate discussion of loss to follow-up, confounding, and missingness; Resilience is not quantitatively measured, and connections between resilience and mental health are not explicit |
| Rotheram-Borus et al., 2006 | Adequate | Inadequate1 | Adequate | N/A | Adequate | Inadequate2 | MOD |
Minus 1: Cross-sectional only Plus 1: Strong, consistent and direct evidence This article has high relevance to the topic at hand. Robust analyses strengthen this study, as does the consideration given to family, peer, and community factors. |
| Skovdal et al., 2009 | Adequate | N/A | N/A | N/A | N/A | Adequate | MOD | Plus 1: Strong, no plausible confounders, consistent and direct evidence |
| Sopena et al., 2010 | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate | HIGH | This RCT of a family-based intervention to improve adolescent adjustment assessed a number of resilience factors and protective processes; makes an important contribution to the literature. |
| Stein et al., 2007 | Adequate (Small) | Inadequate1 | Adequate | N/A | Adequate | Adequate | MOD | Minus 1: Cross-sectional only |
| Wood et al., 2006 | Adequate | Inadequate1 | Adequate | Adequate | Adequate | Adequate | HIGH |
Related to Rotheram-Borus et al. study (above) Minus 1: Cross-sectional only |
| Zhao et al., 2011 | Adequate | Adequate | Adequate | Unclear | Inadequate | Adequate | MOD | Related to Fang et al. study (above). Minus 1: Represents second wave of assessment, but information on follow-up is not provided, and analyses are not longitudinal |
No control group
Inadequate discussion of missingness
Following the SAQOR rating process, we further analyzed articles using NVivo, a qualitative data analysis software package (QSR International, 2010). This step examined each study’s major areas of investigation, findings, and conclusions in more detail. To organize these points by theme, analysts assigned a “code” or label to each major point raised in the methods, discussion, and conclusion. Codes identified a broad range of risk and protective factors positioned by studies in relation to mental health and resilience. This analysis was useful in helping to organize each study’s area of inquiry, and helped to examine and integrate evidence to make cross-study comparisons of findings on different aspects of resilience. A synthesis of findings is presented below.
Results
A summary of the reviewed studies may be found in Table 2. In general, the quality of evidence—as graded using adapted SAQOR criteria—was moderate (see Appendix 2). Ten of the quantitative studies lacked adequate control/comparison groups, and two longitudinal studies lacked adequate description of loss to follow-up. Most studies were found to have adequate quality of mental health measurement, but low or limited quality of resilience measurement. Only one study was found to have an inadequate or unclear sampling strategy. Among the quantitative studies, presentation and explanation of missing data and analyses to account for confounding were generally weak. Overall, only four studies received a “High” Score. Recommendations for improving the evidence base in future research are provided later on.
Table 2.
Summary of Studies
| Study site | Sample (N)* | Age (years) | Determination of child and caregiver serostatus | Domain(s) assessed | Mental Health Measurements | Resilience Measurements | |
|---|---|---|---|---|---|---|---|
| Ayres et al., 2006 | Brazil | 35 adolescents | 13–20 |
|
Social, programmatic | Qualitative inquiry | Qualitative inquiry |
| Betancourt et al., 2011 | Rwanda | 53 children 71 caregivers 10 professionals |
10–17 |
|
Individual, family, social | Qualitative inquiry | Qualitative inquiry |
| Brook et al., 2002 | USA | 101 adolescents 101 fathers |
mean 16† |
|
Individual and parent | Composite measure of rebelliousness, impulsivity, depression, substance use (see original publication for details) | Coping scale by Pearlin et al., 1981; Father-adolescent relationship (authors’ own measure of availability; measure of satisfaction from Brook et al., 1990; measure of rules from Brook et al., 1980; measures of support and child centeredness from Schaefer, 1965) |
| Cluver et al., 2007 | South Africa | 60 children 42 caregivers 20 professionals |
8–19 |
|
Individual, family, social | Qualitative inquiry | Qualitative inquiry |
| Cluver et al., 2009 | South Africa | 425 children and adolescents | 10–19 |
|
Individual and social | Child PTSD Checklist | Social Support Scale |
| Daniel et al., 2007 | Uganda | 20 children 14 caregivers |
11–18 |
|
Cultural, family | Qualitative inquiry | Qualitative inquiry |
| Doku et al., 2010 | Ghana | 200 children | 10–18 |
|
Individual | SDQ | None |
| Dutra et al., 2010 | USA | 82 children 82 mothers |
6–11 |
|
Individual, family | Children: CBCL, CDI Parents: BSI | Parent’s Rating Scale of Child’s Actual Competence, Parenting Convergence Scale, Interaction Behavior Questionnaire, Monitoring and Control Questionnaire, Family Routines Inventory |
| Fang et al., 2009 | Rural China | 1,329 children | 6–18 |
|
Individual | CES-DC, Children’s Loneliness Scale | Self-Esteem Scale, Children Future Expectation Scale, 4-item hopefulness scale, 7-item perceived control over the future scale |
| Funck-Brentano et al., 2005 | France | 30 adolescents | 12–18 |
|
Individual | Perceived Illness Experience Scale, Perceived Treatment Inventory | Self-Esteem Inventory |
| Garvie et al., 2011 | USA | 20 youth | 16–24** |
|
Individual | BDI, BHS, Adult Self-Report, Beliefs About Medicine Scale | Coping Responses Inventory |
| Harms et al., 2009 | Uganda | 13 youth | 12–18 |
|
Individual, family, social, programmatic | Qualitative inquiry | Qualitative inquiry |
| Kumakech et al., 2009 | Uganda | 326 children | 10–15 |
|
Individual | BYI | BYI Self-Concept Subscale (self-confidence, positive self-worth) |
| Leonard et al., 2008 | USA | 105 adolescents | 11–18 |
|
Individual | YSR, CTQ, National Alcohol Survey | None |
| Lyon et al., 2011 | USA | 40 youth 40 caregivers |
14–21 |
|
Spirituality | None | Functional Assessment of Chronic Illness Therapy—Spiritual Well-Being Scale (v.4) |
| Moss et al., 1998 | USA | 24 children | 8–15** |
|
Individual | CDI, State/Trait Anxiety Inventory, Conners’ Parent Rating Scale, CBCL | Perceived Competence Scale for Children, Q-Sort Rating Procedure (Resilience Scale) |
| Murphy et al., 2000 | USA | 230 adolescents | 13–19 |
|
Individual, social | CES-DC, Revised Children’s Manifest Anxiety Scale | Authors’ own scales of social support and coping |
| Murphy et al., 2008 | USA | 222 children 162 caregivers |
6–11** |
|
Individual | CDI, CBCL, Revised Children’s Manifest Anxiety Scale | Children’s Coping Strategies Checklist, Children’s Self-Concept Scale, Social Skills Rating System |
| Nichols et al., 2000 | USA | 403 children | 6–19** |
|
Individual | Pediatric Behavior Scale | Vineland Adaptive Behavior Scales |
| Orban et al., 2010 | USA | 166 youth | 13–21 |
|
Individual | YSR, BDI | Kidcope |
| Petersen et al., 2010 | South Africa | 25 adolescents 15 caregivers |
14–16 |
|
Individual, family, social | Qualitative inquiry | Qualitative inquiry |
| Pivnick et al., 2000 | USA | 25 children | 10–18 |
|
Individual, family, social, programmatic | BDI, clinical interview | Qualitative inquiry |
| Rosenblum et al., 2005 | USA | 77 adolescents | 11–15 |
|
CTQ, YSR, Scales from the Social Development Research Group (Peer Deviance) | Scales from the Social Development Research Group (Opportunities, Social Rewards, Family Functioning), Perceived Competence Scale, Authors’ own scale of prosocial skills, Scale of moral disengagement by Bandura et al. | |
| Rotheram-Borus et al., 2006 | USA | 288 adolescents | mean 15†** |
|
Individual, family | BSI, Authors’ own scale of substance abuse | Authors’ own scale of positive future expectations, Parker Bonding Instrument |
| Skovdal et al., 2009 | Kenya | 48 children 10 adults |
11–17 |
|
Individual, family | Qualitative inquiry | Qualitative inquiry |
| Sopena et al., 2010 | UK | 30 adolescents | 11–17 |
|
Individual | SDQ | Adolescent Coping Orientation for Problem Experiences |
| Stein et al., 2007 | USA | 213 adolescents** | 11–19 |
|
Individual, family | BSI, Authors’ own scale of substance abuse | Adult-Adolescent Parenting Inventory, adapted Dealing with Illness Questionnaire |
| Wood et al., 2006 | Zimbabwe | 56 children and young people 41 caregivers | 7–22 |
|
Individual, family, social | Qualitative inquiry | Qualitative inquiry |
| Zhao et al., 2011 | Rural China | 1,299 children | mean 12 |
|
Individual | CES-DC, Children’s Loneliness Scale, Authors’ own measure of conduct problems | Multiple Functions and Multiple Resources Perceived Social Support Scale, Authors’ own measure of educational resilience |
Sample as defined by study authors
Age range at baseline
Rounded to nearest whole number
BDI – Beck Depression
Inventory
BHS – Beck Hopelessness Scale
BSI – Brief Symptom Inventory
BYI – Beck Youth Inventory
CBCL – Child Behavior Checklist
CDI – Child Depression Inventory
CES-DC – Center for Epidemiological Studies Depression Scale for Children
CTQ – Childhood Trauma Questionnaire
SDQ – Strengths and Difficulties Questionnaire
YSR – Youth Self Report
Although this review focuses on resilience and positive outcomes, it is notable that most studies highlighted a high level of overall mental health problems among sampled HIV/AIDS-affected children. We therefore provide an overview of these results first in order to establish adequate context for appreciating resilience in the context of mental health. Findings on resilient capacities of the individual child or adolescent, family resources, community resources, and interventions for promoting resilience in HIV/AIDS-affected children form the majority of the results section.
Prevalence of Mental Health Problems
Children and adolescents living with HIV infection
Five quantitative studies focused on children and adolescents who were living with HIV infection (as opposed to being affected by HIV or AIDS in the family). However, none of these studies used the same measure(s) of psychological adjustment, which limits our ability to make direct comparisons between studies.
Within their sample of 166 American HIV-positive adolescents age 13–21, Orban and colleagues found that 21% of adolescents reported borderline or clinical thresholds in internalizing emotional and behavioral problems, and 30% reported externalizing problems, as measured by the Achenbach Youth Self Report (Orban et al., 2010). In Murphy et al.’s baseline intervention study, also conducted in the United States, 18% of 230 HIV-infected adolescents demonstrated elevated anxiety on the Children’s Manifest Anxiety Scale and 17% demonstrated elevated depression on the Child Depression Inventory, relative to the cohort mean (Murphy, Moscicki, Vermund, & Muenz, 2000). In this sample, negative life events at different levels of the social ecology were associated with increased depression and anxiety; for instance, the authors demonstrated increased risk for mental health problems among adolescents who experienced family financial problems, parental alcohol abuse, parental conflict including arguing and fighting, changing schools, serious accidents, and death in the family (Murphy, et al., 2000).
Only three studies on HIV-infected children assessed the prevalence of psychological distress with respect to a comparison sample. In two (Moss, Bose, Wolters, & Brouwers, 1998; Sopena, Evangeli, Dodge, & Melvin, 2010), levels of mental health problems and resilience among HIV-infected children were compared to published national norms in the U.S. and U.K. (respectively); no significant differences were found in either case. The third study (conducted in the U.S.) used a control/comparison design to assess adaptive outcomes and levels of emotional and behavioral problems among 403 children and adolescents (age 6–19 at study initiation) at varying stages of disease progression (four groups based on CD4 counts were created from the sample to account for disease progression, including a non-affected control group) (Nichols et al., 2000). In this study, participants with low CD4 cell counts showed greater declines in communication skills, socialization skills, and composite adaptive behavior among group members. However, all groups also increased scores on daily living and decreased behavior problems over time, indicating improvements in resilience across groups.
Children and adolescents affected by HIV
In the studies reviewed, children and adolescents affected by HIV were generally found to demonstrate elevated rates of psychological distress as compared to non-HIV-affected controls. For example, in a study performed in Ghana, Doku (2010) examined psychosocial adjustment and resilience among 200 children in four comparison groups: children orphaned by AIDS, children orphaned for other reasons, HIV-affected children, and non-HIV-affected non-orphaned controls. In this sample, non-HIV-affected non-orphaned controls showed significantly less emotional problems than the three other groups. In a similarly-designed large comparison study with 1,625 children from rural China, Fang and colleagues found that children orphaned by AIDS and HIV-affected children scored significantly higher on depression and loneliness as compared to a non-HIV-affected sample, with children orphaned by AIDS scoring highest on depression and HIV-affected children scoring highest on loneliness (Fang et al., 2009). A follow-up study of this cohort performed by Zhao et al. (2011) confirmed these trends.
In their New York City study of 82 adolescents with drug-abusing fathers (37% of fathers were HIV-positive), Brook et al. (2002) found that children with HIV-positive drug abusing fathers demonstrated higher levels of interpersonal difficulty, delinquency, and substance use, as compared to a random sample of adolescents from the region. By contrast, a similar New York City study of 105 low-income adolescents with substance-abusing mothers did not find significantly more alcohol or drug use among HIV-affected participants as compared to non-HIV-affected participants; in fact, rates of substance use and sexual behavior among both the HIV-affected and non-HIV-affected participants in this study were similar to national samples of same-aged peers (Leonard, Gwadz, Cleland, Vekaria, & Ferns, 2008). A third study of HIV-affected adolescents from New York City reported high rates of substance use (40%) among their sample of 77 11–15 year-olds, but did not provide information on how these rates compared to national or regional rates (Rosenblum et al., 2005).
In a longitudinal study with HIV-affected children, Murphy and Marelich (2008) found that depression and worry decreased over time across their sample of 111 HIV-affected children from the U.S., with resilient children demonstrating steeper declines in depression over time as well as significantly lower feelings of ineffectiveness and negative self-esteem (“resilience” was measured along a continuum by combining five measures of psychosocial adjustment). In a particularly at-risk sample of 25 low-income adolescents studied by Pivnick and Villeagas (2000) in the U.S. (many study participants had spent time with foster families, had been exposed to parental negligence, parental drug use, physical abuse, and sexual abuse), all adolescents expressed high degrees of somatization, many were diagnosed with sleep disorder, and many reported not doing well in school. Over time, depression and anxiety in study participants decreased. Unfortunately, however, aside from participation in a supportive program at a Women’s Center, the study did not explicitly explore the resilience factors that may have contributed to these outcomes, and the study’s lack of a control group and small sample size limited the generalizability of findings.
Individual Factors of Resilience
Among studies that investigated factors of resilience at the individual level, the majority examined aspects of coping with HIV-related stressors among children and adolescents. Three studies also investigated perseverance, self-esteem, and positive future expectations as components of resilience among HIV-affected children and adolescents.
Coping
Research indicates strong associations between coping strategies, mental health, and resilience in HIV-positive and HIV-affected children and adolescents. In their study in the U.S., Orban et al. (2010) found that passive coping (e.g., blaming, wishful thinking, withdrawal, self-criticism) was significantly associated with greater depression, and was more frequently used by adolescents reporting medication-related stressors. In Murphy and Marelich’s longitudinal investigation of HIV-affected children from the U.S., coping self-efficacy was significantly correlated with child resilience (defined as better than expected mental health outcomes), and resilient children demonstrated steeper declines in depression over time (Murphy & Marelich, 2008). These trends resonated with findings from a qualitative study of 25 HIV-positive adolescents and 15 caregivers in South Africa, in which a number of adolescents reported that goal-setting helped them to cope with their diagnosis (Petersen et al., 2010).
In their study of 82 HIV-affected adolescents from New York City, Brook et al. found associations between adolescent rebelliousness, interpersonal difficulties, substance use, depression, and maladaptive coping (Brook, et al., 2002). By contrast, Murphy et al. did not find that adaptive coping significantly moderated the relationship between stressful life events and outcomes of anxiety or depression in their U.S. baseline intervention study (Murphy, et al., 2000). In Sopeña et al.’s U.K. study, investigators observed correlations between psychological adjustment and two coping strategies (ventilating feelings and being humorous); however, these associations were no longer significant after controlling for age (Sopena, et al., 2010).
Self-esteem and hope for the future
In this review, we considered self-esteem as a protective factor in itself, rather than as a measure of mental ill health. This interpretation was reinforced by two qualitative studies—the first with 68 children and adults in Rwanda (Betancourt, Meyers-Ohki, Stulac, et al., 2011), the second with 13 youth age 12–18 in Uganda (Harms, Kizza, Sebunnya, & Jack, 2009)—which both independently categorized perseverance and self-esteem as defining characteristics of resilience in their study samples. In the one quantitative study to examine self-esteem and hope for the future, Fang et al. found that non-HIV-affected children scored significantly higher on self-esteem, positive future expectations, hopefulness about the future, and perceived control over the future, as compared with children orphaned by AIDS and HIV-affected children (Fang, et al., 2009). In Fang et al.’s study, children orphaned by AIDS reported higher self-esteem than HIV-affected children.
Family Factors of Resilience
Seven studies focused on factors of resilience at the family level. Four identified associations between resilience and parental monitoring, parental attachment, and positive family functioning. In addition, three studies explored how children and adolescents may achieve strong resilient outcomes in the face of parental impairment and early parentification.
Parental monitoring and attachment
In research with 82 HIV-affected inner-city African-American families, Dutra et al. found that high levels of parental monitoring combined with positive parent-child relationship were associated with higher resilience in children (resilience rated using a continuous measure of five combined scales to assess child-reported internalizing and externalizing as well as parent-reported externalizing, cognitive competence, and social competence) (Dutra et al., 2000). Brook et al. (2002) found that father presence in the home was associated with adaptive coping in HIV-affected and non-HIV-affected adolescents, regardless of parental HIV status. Further, Brook et al. also found that aspects of the father-child relationship (including parental availability and support, child-centeredness, and satisfaction with the child) and paternal coping strategies increased the likelihood that adolescents themselves would engage in adaptive coping (Brook, et al., 2002).
Family functioning
In their New York City study, Rosenblum et al. (2005) observed correlations between positive family functioning, resilience, and lower likelihood of deviant peer affiliation, and substance abuse. By contrast, child abuse, children’s deviant peer affiliation, and fewer indicators of resilience were also correlated in this study (Rosenblum, et al., 2005). In Betancourt et al.’s qualitative study of HIV-affected children in Rwanda, family unity (kwizerana) emerged as an important local resilience construct, comprising indicators such as “living together in harmony,” cooperation, mutual respect, and strong communication (Betancourt, Meyers-Ohki, Stulac, et al., 2011).
Coping in response to parental impairment
Evidence of links between parental impairment and poor mental health in children has been well-documented (Donald & Clacherty, 2005; Thurman et al., 2008), and is supported by some of the research reviewed here. For instance, in Murphy and Marelich’s study in the U.S. (2008), decreases in child resilience were associated with maternal viral load and disease progression. This finding was reinforced by qualitative findings linking parental impairment and child well-being in a study in Zimbabwe (Wood, Chase, & Aggleton, 2006).
However, examinations of child resilience in the face of parental impairment or death are more rare. In our review, we found two studies that investigated these issues. In work by Skovdal and colleagues (Skovdal, Ogutu, Aoro, & Campbell, 2009), researchers used qualitative methods including interviews, group discussions, written narratives, and child-created photographic documentation, to examine themes and strategies of child resilience in Western Kenya. Among the 48 HIV-affected child participants, most depicted their role as caregiver in a positive light characterized by independence, problem-solving, and work ethic. Although significant hardships were identified, the study emphasized how social resources can facilitate children’s adaptive coping and resilience. Interestingly, quantitative results from a 6-year longitudinal study in the U.S. seem to support findings from the Skovdal study: in their sample of 213 adolescents, Stein et al. (2007) found that while early parentification due to HIV/AIDS was associated with more emotional distress, substance use, and conduct problems in adolescents during the 6 months following death, parentified adolescents actually demonstrated more adaptive coping skills (including positive action and engaging social support) and less alcohol and tobacco use over time as compared to non-parentified HIV-affected adolescents.
Community and Cultural Factors of Resilience
Thirteen studies focused on factors of resilience at the community or cultural level. Three of these studies highlighted the protective roles of education and information sharing. Nine studies highlighted protective social supports at the community, family, and peer levels. One study found that the type of housing available for children orphaned by AIDS can also impact resilience in this population.
Access to educational resources
In their qualitative study with adolescents and caregivers from Brazil, Ayres and colleagues investigated the health care needs of 35 adolescents age 13–20 living with HIV/AIDS, as well as the services and programming available to them (Ayres et al., 2006). The authors found that stigma and lack of social inclusion were major themes which influenced adolescents’ willingness/ability to disclose HIV-status, and interfered with their access to community resources such as education. Limited access to HIV/AIDS information may in turn place adolescents at higher risk for contracting the virus themselves, as was highlighted by Daniel et al.’s qualitative (2007) study from Uganda: in their research with local HIV/AIDS-affected orphans and caregivers, Daniel and colleagues found that disclosure and openness was related to resilience and self-efficacy, while silence, secrecy, and stigma contributed to feelings of self-hate, anxiety, hopelessness, and confusion among HIV/AIDS-affected children (Daniel, et al., 2007). Similar themes were highlighted in Pivnick and Villeagas’s (2000) mixed-methods study of 25 adolescents from the Bronx. The research was based out of a women’s center which provided community supports and information on safer sex and HIV. The authors of this study hypothesized that the center’s stigma-free social context and encouragement of family communication about HIV/AIDS contributed to promoting adolescent resilience.
Social support
The protective role of social support, including perceived financial, physical, and emotional help from family, friends, and the larger community, was examined by several studies. In Cluver et al.’s (2009) study with 703 children and adolescents (425 AIDS-orphaned and 278 non-orphaned) in South Africa, perceived social support was associated with lower symptoms of PTSD at all levels of trauma, suggesting that support from peers, carers, family mentors, and other people from the community may reduce the deleterious effects of a range of traumatic experiences. In the study by Orban et al. performed in the United States, adolescents rated social support and problem solving among the “most helpful” coping strategies; however, results showed that these strategies were not widely used, perhaps, the authors speculated, because fear of discrimination discourages youth from reaching out to others (Orban, et al., 2010). In rural China, Zhao et al. also found that tangible support from family predicted less depression and loneliness and more positive social interactions, while emotional support was associated with reduced delinquent behavior (Zhao, et al., 2011). However, other unexpected associations were also observed in this study, including a correlation between support from teachers/friends/significant others and increased risk of delinquent behaviors (Zhao, et al., 2011).
Peer support
Peer affiliations and community interactions were examined by Rosenblum and colleagues (2005) in their New York City study of HIV-affected adolescents. In this study, positive community experience was correlated with less deviant peer affiliation. Peer deviance was associated with older age, community risk factors, and less resilience. These findings appear to be consistent with several of the intervention and qualitative studies reviewed (Betancourt, Meyers-Ohki, Stulac, et al., 2011; Funck-Brentano et al., 2005; Harms, et al., 2009; Kumakech, Cantor-Graae, Maling, & Bajunirwe, 2009; Petersen, et al., 2010; Wood, et al., 2006), which suggest that positive interactions with peers at school are emotionally-beneficial, as is having access to elders in the community and to psychosocial programs. In Cluver and Gardner’s (2007) qualitative study of 60 South African children orphaned by AIDS, caregiving, contact with extended family, school/peer support, and positive activities emerged as key protective factors in the lives of children orphaned by AIDS. By contrast, negative peer interactions such as bullying and gossip were identified as risks (Cluver & Gardner, 2007). The Cluver and Gardner study was one of the only studies included in this review to examine physical safety and neighborhood crime as related to risk and resilience in HIV affected young people. The research indicated that violent crimes in the community (e.g., muggings, assault, violence toward friends and family) are particularly distressing to children, and that caregivers view the lack of safe play areas as associated with increased behavioral problems in orphans (Cluver & Gardner, 2007).
Group homes and orphanages
In the only study in this review to examine the context of group living, Fang et al. found that the 30 orphans from their sample living in group homes (small family-style residences of 4 to 6 orphans managed by local residents that are common in China) demonstrated significantly less depression and more perceived control over the future, but higher loneliness and lower self-esteem, as compared to orphans living in orphanages or kinship (extended family) care (Fang, et al., 2009). Based on study findings, the authors suggested that group homes may be a more adaptive environment than orphanages and kinship households, although further investigation is needed to understand the contextual factors and mechanisms of the outcomes associated with these different care arrangements.
Interventions
Mental health interventions to improve resilience in HIV-affected children are rare (King, De Silva, Stein, & Patel, 2009). In this review, we identified four intervention studies (Funck-Brentano, et al., 2005; Kumakech, et al., 2009; Lyon et al., 2011; Rotheram-Borus, Stein, & Lester, 2006) aimed at facilitating child and family adjustment to HIV. Of these, only the longitudinal, randomized controlled trial conducted by Rotheram-Borus, Stein, and Lester in the U.S. rated high on the SAQOR evaluation given its rigorous follow-up procedures, holistic consideration of potential risk and protective factors, and robust analytic plan. Findings from this study of 288 parents living with HIV and their adolescent children showed that adolescents randomized to the intervention reported less substance abuse in later years (Rotheram-Borus, et al., 2006). Positive parental bonds at baseline were associated with more resilient outcomes after three and six years, including less risky behavior and emotional distress, and more positive future expectations. Overall, study findings indicate that family-based interventions have high potential for facilitating more resilient mental health and developmental trajectories among HIV-affected children.
The second intervention study (Lyon, et al., 2011)—a randomized trial with an active control group also implemented in the U.S.—investigated the effects of a family-centered advance care planning and medication adherence intervention on the spirituality and religious beliefs of the 40 participating HIV-affected adolescents. While qualitative studies have indicated that faith in god or religious belief can contribute to resilience in HIV-affected children (Betancourt, Meyers-Ohki, Stulac, et al., 2011), the Lyon et al. study was the only quantitative study in this review to assess spirituality as a resilience factor. In this research, trends suggesting an association between low adherence to medication (treated as a proxy for coping) and the belief that HIV is a punishment from God held true across time points and groups. Additionally, the authors observed that both intervention and control adolescents exhibited increases in “sense of meaning” and “purpose” between baseline and 3 months follow-up, but that changes were only significant for control adolescents. The authors also noted declines in faith (defined as “comfort and strength in one’s beliefs”) among intervention participants, versus significant increases in faith among controls. Study investigators speculated that increased feelings of control over medical care or feelings of anger with God may explain some of these findings. Unfortunately, mechanisms linking the intervention content, spirituality, and additional dimensions of resilience were not assessed.
The last two studies focused on yet another potential mechanism for improving resilience: peer-group support. In Uganda, Kumakech and colleagues (2009) performed a cluster randomized trial of 326 children orphaned by AIDS comparing a combined school-based peer support/somatic health care treatment to a control condition. Intervention activities—including sharing of fears and worries, trust-building exercises, problem-solving activities, and action-planning exercise—were administered by trained teachers and were intended to use social support to improve coping; however, a discreet measure of coping was not used (resilient characteristics were measured only using the self-concept subscale of the Beck Youth Inventory), and no significant intervention effects on self-concept were observed. This study was limited by significant between-group differences at baseline: children in the intervention groups demonstrated significantly lower self-concept and higher depression as compared to children in the control group. Additionally, knowledge of AIDS as the cause of parental death was not an enrollment criterion for this study, and some children learned of their association with AIDS through their involvement in the intervention. The confounding effects of this limitation were not explored. Though the study investigators did observe significant improvements in depression, anxiety, and anger in the intervention group, the lack of improvement in self-concept and significant weaknesses in the study design limit the generalizeability of this research. In the one other intervention study on peer support groups for HIV-positive adolescents, Funck-Brentano and colleagues observed improvements in preoccupations about illness and fears about medication, as well as reduced viral load (Funck-Brentano, et al., 2005). However, this small pilot study of 30 HIV-infected adolescents (intervention group of n=10), was insufficiently powered to provide substantive data on intervention effectiveness, and improvements in self-esteem or other resilient constructs were not reported. Additional research on peer group support interventions is clearly needed.
In addition to the four formal intervention trials, a fifth study was identified as relating to interventions for family strengthening and empowerment in the context of HIV/AIDS, but was excluded from the formal review process because it lacked sufficient methods for assessing mental health and resilience. This descriptive study by Kmita et al. (2002) explored different strategies and contexts of psychosocial intervention to decrease social isolation of families and improve coping, self-esteem, and community integration in Poland. Through qualitative analysis of clinical observations from both medical (hospital setting) and non-medical psychosocial intervention settings, the authors identified group activities, interventions that involved both children and caregivers, and strong collaboration between service providers as critical components of interventions with this population. While this study’s assessments of improvements in psychosocial functioning were limited to observations by interventionists, findings suggest that both medical and non-medical interventions contributed to improving emotional functioning of parents and children, increasing the number of people in the family’s social network, improving flexible coping in study participants, and reducing family silence about those who died. Further, findings underscored that a range of interventions undertaken in both clinical and non-clinical settings may help improve resilience in HIV-affected families.
Associations with Age and Gender
Few studies reported comparisons by age or gender. Across their four comparison groups from China (296 orphans who lost both parents to AIDS, 459 orphans with one parental death due to AIDS, 466 HIV-affected children, and 404 non-HIV/AIDS-affected children), Fang et al. observed lower loneliness, higher self-esteem, positive future expectation, higher hopefulness, and better perceived control over the future in older children (Fang, et al., 2009). In their study of HIV-affected adolescents from New York City, Rosenblum et al. (2005) found associations between older age, peer deviance, and lower family functioning. No other studies found significant differences in outcomes of interest by age.
Few gender differences were reported. Exceptions include: among Chinese orphans whose parents both died from AIDS, male gender was associated with higher self-esteem and lower perceived control over the future (Fang, et al., 2009); and in Ghana, males reported significantly higher rates of peer problems as compared to females, with a large effect size (Doku, 2010).
DISCUSSION
The mental health and wellbeing of children and families affected by HIV/AIDS must be viewed as a dynamic process involving a number of ecological levels from the biological to the family to the larger community and culture, with each level presenting risks (Betancourt & Khan, 2008; Lazarus & Folkman, 1984; Masten & Obradovic, 2008) as well as sources of potential protection and resilience (Bronfenbrenner, 1979; Ungar, 2011). Of the 29 studies included in this review, only a handful of qualitative investigations tapped into the full range of resilience factors implied in holistic models of resilience. While information is available on physical, cultural, and community constructs that contribute to the environments in which HIV-affected children grow and develop, there remains a much greater focus on risk than resilience in the available literature, and strong quantitative studies in diverse cultural settings are lacking. In this review, none of the five quantitative studies on children living with HIV (Moss, et al., 1998; Murphy, et al., 2000; Nichols, et al., 2000; Orban, et al., 2010; Sopena, et al., 2010) examined resilience at different levels of the social ecology, and social support factors were only minimally explored. By contrast, the studies on resilience and mental health in HIV/AIDS-affected children assessed a broader range of individual resilience characteristics, perhaps because they were less concerned with how children cope with illness and more focused on how children react to dramatic shifts in family configuration and the sequelae of parental impairment. We note that limitations in the existing literature, such as the lack of adequate comparison conditions and variation in measurement across studies, limits our ability to make comparisons across studies and between important categories such as HIV status, age of children, and cultural context. These limitations are discussed later on.
Despite some design limitations, the studies reviewed point to a number of important trends. Parenting and family support, in particular, were associated with resilient outcomes in children. Specifically, family attitudes towards parenting and the availability of supportive caregivers to provide nurturance and guidance appear to be critical to the mental health and psychosocial adjustment of HIV/AIDS-affected children and adolescents. As such, it is logical to conclude that interventions which aim to normalize the experience of living with a chronic illness such as HIV personally or in one’s family are extremely valuable, as demonstrated by Rotheram-Borus et al.’s longitudinal RCT study (Rotheram-Borus, et al., 2006). In research that focuses on family dynamics more broadly (without a specific focus on HIV/AIDS), parenting has been shown to predict children’s own poor functioning and ineffective problem solving as they grow older (Ehrensaft et al., 2003; Fergusson & Horwood, 1998). Studies have also shown that negative family dynamics, including intimate partner violence and aggressive parenting, compromise children’s ability to establish positive peer or romantic interactions (Capaldi & Clark, 1998; Dodge & Price, 1994; Gilliom, Shaw, Beck, Schonberg, & Lukon, 2002). Given this evidence from the broader literature and findings from the present review, we can conclude that interventions which target support to families made vulnerable by HIV hold great promise (Betancourt, Meyers-Ohki, Stevenson, et al., 2011; Richter, Foster, & Sherr, 2005; Smith Fawzi, et al., 2010).
As noted in several of the studies reviewed here, and consistent with a social ecological model of resilience, perceived social equity in the community is highly relevant to promoting individual strengths in children. Two of the reviewed studies identified community stigma and social exclusion of children and adolescents living with or affected by HIV as risk factors that contribute to vulnerability and poorer outcomes (Ayres, et al., 2006; Daniel, et al., 2007), and nearly all of the studies identified various aspects of social support as protective. For example, in China, government-supported group homes that are managed by the local community and create a proxy of a family environment appear to provide better mental health outcomes and life satisfaction among children orphaned by AIDS (Fang, et al., 2009). Similarly, in Zimbabwe, Rwanda, Uganda, and Kenya, social support from peers, community programs and leaders, and family appear to contribute to resilience in children and adolescents affected by HIV. Finally, supportive psychosocial programs were found to be protective in the settings where these were available.
For many HIV/AIDS-affected children and families, navigating community stigma remains a very challenging issue, particularly in lower-resource settings where misinformation about the virus prevails. In many settings, social support and social stigma may co-occur for HIV-affected children. For instance, in Wood et al.’s household case studies of 56 AIDS-affected children from Zimbabwe (also including interviews with 41 adults), some children cited family and community support as a positive resource, while others reported experiencing maltreatment from adoptive family members (Wood, et al., 2006). Child participants from this and other studies (Betancourt, Meyers-Ohki, Stulac, et al., 2011; Cluver & Gardner, 2006) reported taking on adult and caring responsibilities, felt “grown up”, and had dropped out of school. In general, many children expressed a desire to share thoughts and worries, but this went against the general opinion that perseverance and “not breaking down” are the most positive ways to cope.
Community sensitization campaigns and peer-to-peer education have high potential for raising community awareness and combating stigma at a community level (de Souza, 2009; Sayson & Meya, 2001; Selikow, Ahmed, Flisher, Mathews, & Mukoma, 2009; Sweifach & LaPorte, 2007). Further, family-based interventions can also contribute to dispelling internalized stigma within the family through open discussion about HIV and related adversities (Betancourt, Meyers-Ohki, Stevenson, et al., 2011; Betancourt, McBain, et al., in press). In this review, studies across settings indicated that interventions are needed to teach children how to talk to trusted friends and seek support from leadership in the community. Since stigma from peers can be particularly detrimental to children living with and affected by HIV, peer-to-peer support programs and school based awareness raising programs (Kennedy et al., 2004) have the potential to combat stigma at the level of the school or larger community ecology. Rosenblum et al. suggested that interventions which address peer-affiliation among HIV-affected children and adolescents may help delay substance use, and that interventions to improve family functioning and parenting can improve resiliency (Rosenblum, et al., 2005). In particular, increasing multiple social support structures for AIDS-orphaned children and adolescents may help counteract the negative consequences of AIDS-related losses (Cluver, et al., 2009). Developing such supports is a key area to be targeted by future interventions.
Limitations
Our findings should be viewed within the limitations that exist in this review. We note that the quality of a review is limited by the quality of the literature being synthesized. As such, studies screened for inclusion in this review were subject to rigorous inclusion criteria to ensure adequate quality, specificity and focus. While the narrow number and range of included studies may be considered a limitation, it is also representative of the scant evidence base focused on resilience in HIV/AIDS-affected children and adolescents. The small number of available studies engendered additional limitations related to the breadth and depth of findings on such topics as HIV positivity in children and its effects on resilience profiles, differences in resilience due to age and gender, and comparisons between HIV-positive children and HIV-affected children. As research in these topics increases, future reviews will benefit from a richer evidence base.
Our evaluation of the quality of evidence also faced limitations. In general, rating systems like SAQOR are inherently limited by the range of criteria that can be feasibly and reliably assessed. While we selected SAQOR for its more sensitive approach to rating a range of study designs (qualitative, quantitative, intervention), an alternative or more heavily adapted rating system may have resulted in different findings. However, given the limitations identified in applying the SAQOR criteria, we feel that a “moderate” rating for the overall rating of the quality of research on resilience among children and adolescents infected and affected by HIV is an accurate representation of the current literature.
In grading the literature reviewed here, the following limitations were noted: (1) The overall number and quality of studies in the existing literature is limited. (2) Many of the quantitative studies lacked adequate control or comparison groups. (3) There was almost universal low or limited quality of resilience measurement. (4) There remains a need for validated, sensitive measures of protective factors. In fact the lack of adequate comparison conditions, and consistent definitions or measures for resilience and other study constructs severely restricted our ability to anchor findings to relevant community or national norms, or to compare findings across studies, gender, age, HIV status, or culture/country/region. (5) The majority of research focused on adolescents, with little attention paid to younger age groups. Only two studies examined associations between older age and resilience constructs (Fang, et al., 2009; Rosenblum, et al., 2005). (6) Within many studies of children affected by HIV (rather than infected with HIV), the HIV status of children and adolescents was not specified, making it was unclear whether children living with HIV were included in the sample, potentially confounding findings. (7) The majority of studies reviewed here were qualitative, descriptive, cross-sectional, and/or quasi-experimental designs which did not account for confounding or alternative hypotheses, thus limiting our ability to make causal inferences from existing data. (8) Longitudinal studies did not provide adequate description of loss to follow-up. (9) Analyses rarely controlled for environmental stressors that may confound both parenting and child outcomes. This includes variables such as duration of exposure or age of HIV disclosure. (10) There was a lack of strong studies investigating how protective processes in families operate in other countries and cultural contexts. Given the burden of HIV in many low-resource countries, the lack of literature examining resilience related to HIV and mental health in a global health context was concerning. Finally, (11) the intervention studies reviewed were well-designed but still very limited in scope.
Recommendations
Future research should address the limitations noted above by developing consensus on definitions and measures that can be used across multiple contexts to facilitate comparisons across studies. Additionally, stronger study designs (e.g., longitudinal, experimental) that utilize appropriate comparison or control conditions or eliminate or control for confounding variables, are needed. In particular, studies that compare outcomes across age groups are needed to inform age-appropriate programming for children and adolescents.
There are also many areas where additional research on protective processes is critically needed, particularly in the global South where the disease burden is high but research attention is limited. Interestingly, all qualitative studies included in this review investigated samples of HIV-affected children and adolescents from low-resource settings, with seven out of eight focusing on Africa. Such work provides a good foundation for embarking on critical quantitative and intervention focused research.
At the individual level, there is much more to be learned about the function of different individual level processes (e.g., communication skills, assertiveness, self-esteem, optimism, self-efficacy, etc) in addition to strengths and vulnerabilities due to immutable factors such as sex or age. At the family level, research on the role of attachment, parental monitoring, warmth, guidance and other features of caregiver-child relationships in the mental health of children living with and affected by HIV would provide a stronger evidence base for indentifying intervention targets. Similarly, at the larger community and cultural level, research on the role of acceptance and efforts to reduce community stigma, and the provision of community programs, education, and social support could contribute greatly to efforts to promote mental health and well-being in children and families affected by HIV.
Additionally, while children and adolescents affected by HIV are likely to experience numerous problems, such as internalizing and externalizing behaviors, depression, and poor self-esteem, it appears these problems can be attenuated through supportive programs and as well as maturation and improved skills development (Funck-Brentano, et al., 2005; Kmita, et al., 2002; Kumakech, et al., 2009; Lyon, et al., 2011; Rotheram-Borus, et al., 2006). Thus, there is a particular need for intervention research that promotes resilience and positive outcomes across all ecological levels. For example, at the child level, interventions are needed that increase service utilization, coping skills, self-efficacy, self-esteem, and stigma resistance. At the family level, interventions are needed that increase family support and functioning, parenting skills, communication, and communal problem-solving. At the community level, interventions are needed to reduce community stigma, develop effective prevention efforts, and increase safe and health-promoting environments.
Finally, most studies reviewed here focused on at-risk populations who are vulnerable to multiple adversities beyond HIV/AIDS, including poverty and parental drug use. For these populations encountering risks at multiple levels of the social ecology, consideration of a range of protective processes is even more critical. This may help to explain some of the differences between results in mental health outcomes in the reviewed studies of HIV-infected children (which mostly sampled children from middle-class U.S. or U.K. populations) as compared to other studies examining children affected by HIV more broadly (many sampled from high-risk and resource-constrained settings). As such, more attention to the generalizability of U.S.-developed interventions is warranted, as is more research to develop and adapt locally-relevant programs for diverse settings and populations.
In conclusion, we found that applying an ecological framework to understanding risk and protective processes in the lives of children and families affected by HIV/AIDS helps to identify key leverage points for both prevention and intervention in a manner that is holistic, systematic and responsive to the complex nature of risks and resilience. In fact, a great strength of the research reviewed here is the predominant focus on modifiable factors of resilience which can be targeted and successfully intervened upon. The few studies of interventions have provided evidence that targeting the family or caregiving system and providing better integration of community support structures can result in increased resilience and reduced substance use, risk behavior, and emotional distress. By addressing remaining gaps in the evidence base, future research can strengthen our understanding of appropriate targets for promoting resilience in children and families affected by HIV/AIDS.
Key Points.
The literature on mental health and resilience in HIV/AIDS-affected children is extremely limited, despite a large evidence base on risks associated with HIV in the family.
This review proposes that a social-ecological model of resilience is relevant to the experience and developmental context of children affected by HIV/AIDS. The existing literature is organized according to study findings on protective processes at the individual, family, and community levels.
To date, no quantitative studies have comprehensively examined factors contributing to resilience at various social ecological levels. A more comprehensive understanding of the mechanisms connecting mental health, resilience, and experience of HIV/AIDS can help to develop more targeted, strengths-based interventions for vulnerable children, adolescents, and families.
Future research guided by the ecological framework may help to identify key leverage points for both prevention and intervention in a manner that is holistic, systematic and responsive to the complex nature of risks and resilience.
Acknowledgments
We would like to thank the Harvard School of Public Health and the François-Xavier Bagnoud Center for Health and Human Rights. This study was supported by Grant K01MH077246-05, Grant R34MH084679-02, and Grant R34MH087223-02 from the National Institute of Mental Health and Grant P60 MD002261 from the National Center for Minority Health and Disparities.
This review article was invited by the journal, for which the principal author has been offered a small honorarium payment towards personal expenses.
Abbreviations
- AIDS
Acquired immune deficiency syndrome
- ART
Anti-retroviral therapy
- CD4
Cluster of differentiation 4
- HIV
Human immunodeficiency virus
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analyses
- SAQOR
Systematic Assessment of Quality in Observational Research
- UNAIDS
Joint United Nations Programme on HIV/AIDS
Footnotes
No conflicts of interest for any authors are declared.
References
- Anderson M, Elam G, Gerver S, Solarin I, Fenton K, Easterbrook P. HIV/AIDS-related stigma and discrimination: Accounts of HIV-positive Caribbean people in the United Kingdom. Social Science & Medicine. 2008;67(5):790–798. doi: 10.1016/j.socscimed.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Ayres JR, Paiva V, Franca I, Jr, Gravato N, Lacerda R, Della Negra M, Silva MH. Vulnerability, human rights, and comprehensive health care needs of young people living with HIV/AIDS. Am J Public Health. 2006;96(6):1001–1006. doi: 10.2105/AJPH.2004.060905. AJPH.2004.060905 [pii] 10.2105/AJPH.2004.060905 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benard B. ERIC/EECE Digest, EDO-PS-95-9. 1995. Fostering Resilience in Children. [Google Scholar]
- Betancourt TS, Khan KT. The mental health of children affected by armed conflict: Protective processes and pathways to resilience. International Review of Psychiatry. 2008;20(3):317–328. doi: 10.1080/09540260802090363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, McBain R, Newnham EA, Brennan RT. Trajectories of internalizing problems in war-affected Sierra Leonean youth: Roles of conflict and post-conflict factors. Child Development. doi: 10.1111/j.1467-8624.2012.01861.x. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Meyers-Ohki S, Stulac SN, Elizabeth Barrera A, Mushashi C, Beardslee WR. Nothing can defeat combined hands (Abashize hamwe ntakibananira): Protective processes and resilience in Rwandan children and families affected by HIV/AIDS. Social Science & Medicine. 2011;73(5):693–701. doi: 10.1016/j.socscimed.2011.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Meyers-Ohki SE, Stevenson A, Ingabire C, Kanyanganzi F, Munyana M, Beardslee WR. Using Mixed-Methods Research to Adapt and Evaluate a Family Strengthening Intervention in Rwanda. African Journal of Traumatic Stress. 2011;2(1):32–45. [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Meyers-Ohki SE, Stulac S, Barrera AE, Mushashi C, Beardslee WR. Global Mental Health Programs for Children and Families Facing Adversity: Development of a Family Strengthening Intervention in Rwanda. In: Corbin JN, editor. Children and Families Affected by Armed Conflicts in Africa: Implications and Strategies for Helping Professionals in the United States. Washington, DC: National Association of Social Workers Press; 2012. pp. 113–142. [Google Scholar]
- Betancourt TS, Abrams E, McBain R, Fawzi M. Family-centred approaches to the prevention of mother to child transmission of HIV. Journal of the International AIDS Society. 2010;13(Suppl 2):S2. doi: 10.1186/1758-2652-13-S2-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Rubin-Smith J, Beardslee WR, Stulac SN, Fayida I, Safren SA. Understanding locally, culturally, and contextually relevant mental health problems among Rwandan children and adolescents affected by HIV/AIDS. AIDS Care. 2011;iFirst:1–12. doi: 10.1080/09540121.2010.516333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J, Jordan CE. Violence against women: outcome complexity and implications for assessment and treatment. J Interpers Violence. 2004;19(11):1252–1276. doi: 10.1177/0886260504269682. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: The Harvard University Press; 1979. [Google Scholar]
- Brook DW, Brook JS, Whiteman M, Arencibia-Mireles O, Pressman MA, Rubenstone E. Coping in adolescent children of HIV-positive and HIV-negative substance-abusing fathers. J Genet Psychol. 2002;163(1):5–23. doi: 10.1080/00221320209597965[doi]. [DOI] [PubMed] [Google Scholar]
- Brook JS, Lukoff IF, Whiteman M. Initiation into adolescent marijuana use. Journal of Genetic Psychology. 1980;137:133–142. doi: 10.1080/00221325.1980.10532808. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Clark S. Prospective family predictors of aggression toward female partners for at-risk young men. Developmental Psychology. 1998;34(6):1175–1188. doi: 10.1037/0012-1649.34.6.1175. [DOI] [PubMed] [Google Scholar]
- Cluver L, Fincham DS, Seedat S. Posttraumatic stress in AIDS-orphaned children exposed to high levels of trauma: The protective role of perceived social support. J Trauma Stress. 2009;22(2):106–112. doi: 10.1002/jts.20396. [DOI] [PubMed] [Google Scholar]
- Cluver L, Gardner F. The psychological well-being of children orphaned by AIDS in Cape Town, South Africa. Ann Gen Psychiatry. 2006;5:8. doi: 10.1186/1744-859X-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cluver L, Gardner F. Risk and protective factors for psychological well-being of children orphaned by AIDS in Cape Town: a qualitative study of children and caregivers’ perspectives. AIDS Care. 2007;19(3):318–325. doi: 10.1080/09540120600986578. [DOI] [PubMed] [Google Scholar]
- Cluver L, Gardner F, Operario D. Psychological distress amongst AIDS-orphaned children in urban South Africa. Journal of Child Psychology and Psychiatry. 2007;48(8):755–763. doi: 10.1111/j.1469-7610.2007.01757.x. [DOI] [PubMed] [Google Scholar]
- Cluver L, Operario D. Inter-generational Linkages of AIDS: Vulnerability of Orphaned Children for HIV Infection. IDS Bulletin. 2008;39(5):27–35. doi: 10.1111/j.1759-5436.2008.tb00492.x. [DOI] [Google Scholar]
- Cluver L, Orkin M. Cumulative risk and AIDS-orphanhood: Interactions of stigma, bullying and poverty on child mental health in South Africa. Social Science & Medicine. 2009;69(8):1186–1193. doi: 10.1016/j.socscimed.2009.07.033. [DOI] [PubMed] [Google Scholar]
- Cluver LD, Orkin M, Gardner F, Boyes ME. Persisting mental health problems among AIDS-orphaned children in South Africa. Journal of Child Psychology and Psychiatry. 2012;53(4):363–370. doi: 10.1111/j.1469-7610.2011.02459.x. [DOI] [PubMed] [Google Scholar]
- Cowan PA, Cowan CP, Schulz MS. Thinking about risk and resilience in families. In: Hetherington EM, Blechman EA, editors. Stress, coping, and resiliency in children and families. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. pp. 1–34. [Google Scholar]
- Daniel M, Apila HM, Bjargo R, Lie GT. Breaching cultural silence: Enhancing resilience among Ugandan orphans. African Journal of AIDS Research. 2007;6(2):109–120. doi: 10.2989/16085900709490405. [DOI] [PubMed] [Google Scholar]
- de Souza R. Creating “communicative spaces”: A case of ngo community organizing for HIV/AIDS prevention. Health Communication. 2009;24(8):692–702. doi: 10.1080/10410230903264006. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Price JM. On the Relation between Social Information Processing and Socially Competent Behavior in Early School-Aged Children. Child Dev. 1994;65(5):1385–1397. doi: 10.1111/j.1467-8624.1994.tb00823.x. [DOI] [PubMed] [Google Scholar]
- Doku PN. Psychosocial adjustment of children affected by HIV/AIDS in Ghana. Journal of Child and Adolescent Mental Health. 2010;22(1):25–34. doi: 10.2989/17280583.2010.493662. [DOI] [PubMed] [Google Scholar]
- Donald D, Clacherty G. Developmental vulnerabilities and strengths of children living in child-headed households: a comparison with children in adult-headed households in equivalent impoverished communities. African Journal of AIDS Research. 2005;4(1):21–28. doi: 10.2989/16085900509490338. [DOI] [PubMed] [Google Scholar]
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra R, Forehand R. Child resiliency in inner-city families affected by HIV: the role of family variables. Behaviour Research & Therapy. 2000;38(5):471–486. doi: 10.1016/s0005-7967(99)00070-4. [DOI] [PubMed] [Google Scholar]
- Ehrensaft MK, Cohen P, Brown J, Smailes E, Chen H, Johnson JG. Intergenerational transmission of partner violence: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2003;71(4):741–753. doi: 10.1037/0022-006x.71.4.741. [DOI] [PubMed] [Google Scholar]
- Evans RMC. Social Networks, Migration, and Care in Tanzania: Caregivers’ and children’s resilience to coping with HIV/AIDS. Journal of Children and Poverty. 2005;11(2):111–129. doi: 10.1080/10796120500195527. [DOI] [Google Scholar]
- Fang X, Li X, Stanton B, Hong Y, Zhang L, Zhao G, Lin D. Parental HIV/AIDS and psychosocial adjustment among rural Chinese children. J Pediatr Psychol. 2009;34(10):1053–1062. doi: 10.1093/jpepsy/jsp006. jsp006 [pii] 10.1093/jpepsy/jsp006 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ. Exposure to Interparental Violence in Childhood and Psychosocial Adjustment in Young Adulthood. Child Abuse & Neglect. 1998;22(5):339–357. doi: 10.1016/s0145-2134(98)00004-0. [DOI] [PubMed] [Google Scholar]
- Forehand R, Biggar H, Kotchick BA. Cumulative risk across family stressors: short- and long-term effects for adolescents. J Abnorm Child Psychol. 1998;26(2):119–128. doi: 10.1023/a:1022669805492. [DOI] [PubMed] [Google Scholar]
- Funck-Brentano I, Dalban C, Veber F, Quartier P, Hefez S, Costagliola D, Blanche S. Evaluation of a peer support group therapy for HIV-infected adolescents. AIDS. 2005;19(14):1501–1508. doi: 10.1097/01.aids.0000183124.86335.0a. [DOI] [PubMed] [Google Scholar]
- Garcia-Moreno C, Watts C. Violence against women: its importance for HIV/AIDS. AIDS (London, England) 2000;14(Suppl 3):S253–265. [PubMed] [Google Scholar]
- Garvie PA, Flynn PM, Belzer M, Britto P, Hu C, Graham B, Gaur AH. Psychological Factors, Beliefs About Medication, and Adherence of Youth With Human Immunodeficiency Virus in a Multisite Directly Observed Therapy Pilot Study. Journal of Adolescent Health. 2011;48(6):637–640. doi: 10.1016/j.jadohealth.2010.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O’Campo P. HIV/AIDS and Intimate Partner Violence. Trauma, Violence, & Abuse. 2007;8(2):178–198. doi: 10.1177/1524838007301476. [DOI] [PubMed] [Google Scholar]
- Gilliom M, Shaw DS, Beck JE, Schonberg MA, Lukon JL. Anger regulation in disadvantaged preschool boys: Strategies, antecedents, and the development of self-control. Developmental Psychology. 2002;38(2):222–235. doi: 10.1037//0012-1649.38.2.222. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harms S, Kizza R, Sebunnya J, Jack S. Conceptions of mental health among Ugandan youth orphaned by AIDS. African Journal of AIDS Research. 2009;8(1):7–16. doi: 10.2989/ajar.2009.8.1.2.715. [DOI] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. UNAIDS Report on Global AIDS Epidemic. 2010. [Google Scholar]
- Kennedy SB, Johnson K, Harris AO, Lincoln A, Neace W, Collins D. Evaluation of HIV/AIDS prevention resources in Liberia: strategy and implications. AIDS Patient Care & STDs. 2004;18(3):169–180. doi: 10.1089/108729104322994856. [DOI] [PubMed] [Google Scholar]
- King E, De Silva M, Stein A, Patel V. Interventions for improving the psychosocial well-being of children affected by HIV and AIDS. Cochrane Database of Systematic Reviews. 2009 doi: 10.1002/14651858.CD006733.pub2. Issue 2. Art. No.: CD006733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kmita G, Baranska M, Niemiec T. Psychosocial intervention in the process of empowering families with children living with HIV/AIDS -- a descriptive study. AIDS Care. 2002;14(2):279–284. doi: 10.1080/09540120120076959. [DOI] [PubMed] [Google Scholar]
- Kumakech E, Cantor-Graae E, Maling S, Bajunirwe F. Peer-group support intervention improves the psychosocial well-being of AIDS orphans: Cluster randomized trial. Social Science & Medicine. 2009;68(6):1038–1043. doi: 10.1016/j.socscimed.2008.10.033. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Psychological stress and the coping process. New York, NY: Springer; 1984. [Google Scholar]
- Leonard NR, Gwadz MV, Cleland CM, Vekaria PC, Ferns B. Maternal substance use and HIV status: Adolescent risk and resilience. Journal of Adolescence. 2008;31(3):389–405. doi: 10.1016/j.adolescence.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar S. Annotation: Methodological and conceptual issues in research on childhood resilience. Journal of Child Psychology and Psychiatry. 1993;34(4):441–453. doi: 10.1111/j.1469-7610.1993.tb01030.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar S. Resilience and Vulnerability: Adaptation in the Context of Childhood Adversities. New York, NY: Cambridge University Press; 2004. [Google Scholar]
- Luthar S, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71(3):543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar S, Cushing G. Measurement issues in the empirical study of resilience: An overview. In: Glantz MD, Johnson JL, editors. Resilience and development: Positive life adaptations. New York: Plenum; 1999. pp. 129–160. [Google Scholar]
- Luthar S, Goldstein A. Children’s exposure to community violence: Implications for understanding risk and resilience. Journal of Clinical Child & Adolescent Psychology. 2004;33(3):499–505. doi: 10.1207/s15374424jccp3303_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon ME, Garvie PA, Kao E, Briggs L, He J, Malow R, McCarter R. Spirituality in HIV-infected Adolescents and Their Families: FAmily CEntered (FACE) Advance Care Planning and Medication Adherence. Journal of Adolescent Health. 2011;48(6):633–636. doi: 10.1016/j.jadohealth.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason E. Positioning paediatric HIV in the child survival agenda. Paper presented at the Presentation to UNICEF WHO consultation; New York, New York. 2006. [Google Scholar]
- Masten AS. Resilience in individual development: Successful adaptation despite risk and adversity. In: Wang MC, Gordon EW, editors. Educational resilience in innercity America: Challenges and prospects. Hillsdale, NJ: Erlbaum; 1994. pp. 3–25. [Google Scholar]
- Masten AS. Ordinary magic: Resilience processes in development. American Psychologist. 2001;56(3):227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- Masten AS, Obradovic J. Disaster preparation and recovery: Lessons from research on resilience in human development. Ecology and Society. 2008;13(1):1–16. [Google Scholar]
- Mathers CD, Boerma T, Ma Fat D. Global and regional causes of death. British Medical Bulletin. 2009;92(1):7–32. doi: 10.1093/bmb/ldp028. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses. PLoS Medicine. 2009;6(6):e10000097. [PMC free article] [PubMed] [Google Scholar]
- Moss H, Bose S, Wolters P, Brouwers P. A preliminary study of factors associated with psychological adjustment and disease course in school-age children infected with the human immunodeficiency virus. Journal of Developmental and Behavioral Pediatrics. 1998;19(1):18–25. doi: 10.1097/00004703-199802000-00003. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD. Resiliency in young children whose mothers are living with HIV/AIDS. AIDS Care. 2008;20(3):284–291. doi: 10.1080/09540120701660312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Moscicki AB, Vermund SH, Muenz LR. Psychological distress among HIV(+) adolescents in the REACH study: effects of life stress, social support, and coping. The Adolescent Medicine HIV/AIDS Research Network. J Adolesc Health. 2000;27(6):391–398. doi: 10.1016/s1054-139x(00)00158-0. S1054139X00001580 [pii] [DOI] [PubMed] [Google Scholar]
- Nichols S, Mahoney EM, Sirois PA, Bordeaux JD, Stehbens JA, Loveland KA, Amodei N. HIV-associated changes in adaptive, emotional, and behavioral functioning in children and adolescents with hemophilia: results from the Hemophilia Growth and Development Study. J Pediatr Psychol. 2000;25(8):545–556. doi: 10.1093/jpepsy/25.8.545. [DOI] [PubMed] [Google Scholar]
- Orban LA, Stein R, Koenig LJ, Conner LC, Rexhouse EL, Lewis JV, LaGrange R. Coping strategies of adolescents living with HIV: disease-specific stressors and responses. AIDS Care. 2010;22(4):420–430. doi: 10.1080/09540120903193724. 919128925 [pii] 10.1080/09540120903193724 [doi] [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Pelton J, Forehand R. Orphans of the AIDS epidemic: an examination of clinical level problems of children. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(6):585–591. doi: 10.1097/01.chi.0000157551.71831.57. [DOI] [PubMed] [Google Scholar]
- Perez F, Orne-Gliemann J, Mukotekwa T, Miller A, Glenshaw M, Mahomva A, Dabis F. Prevention of mother to child transmission of HIV: evaluation of a pilot programme in a district hospital in rural Zimbabwe. BMJ. 2004;329(7475):1147–1150. doi: 10.1136/bmj.329.7475.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen I, Bhana A, Myeza N, Alicea S, John S, Holst H, Mellins C. Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: A qualitative investigation. AIDS Care. 2010;22(8):970–978. doi: 10.1080/09540121003623693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pivnick A, Villegas N. Resilience and risk: Childhood and uncertainty in the AIDS epidemic. Culture, Medicine and Psychiatry. 2000;24(1):101–136. doi: 10.1023/a:1005574212572. [DOI] [PubMed] [Google Scholar]
- QSR International. NVivo. Vol. 9. Cambridge, MA: 2010. [Google Scholar]
- Richter L, Foster G, Sherr L. Where the heart is: Meeting the psychosocial needs of young children in the context of HIV/AIDS. The Hague Bernard van Leer Foundation; 2005. pp. 1–54. [Google Scholar]
- Rochat TJ, Richter LM, Doll HA, Buthelezi NP, Tomkins A, Stein A. Depression Among Pregnant Rural South African Women Undergoing HIV Testing. JAMA: The Journal of the American Medical Association. 2006;295(12):1376–1378. doi: 10.1001/jama.295.12.1376. [DOI] [PubMed] [Google Scholar]
- Rosenblum A, Magura S, Fong C, Cleland C, Norwood C, Casella D, Curry P. Substance Use Among Young Adolescents in HIV-Affected Families: Resiliency, Peer Deviance, and Family Functioning. Substance Use & Misuse. 2005;40(5):581–603. doi: 10.1081/ja-200030816. [DOI] [PubMed] [Google Scholar]
- Ross LE, Grigoriadis S, Mamisashvili L, Koren G, Steiner M, Dennis CL, Mousmanis P. Quality assessment of observational studies in psychiatry: an example from perinatal psychiatric research. International Journal of Methods in Psychiatric Research. 2011;20(4):224–234. doi: 10.1002/mpr.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Stein JA, Lester P. Adolescent Adjustment over Six Years in HIV-Affected Families. Journal of Adolescent Health. 2006;39(2):174–182. doi: 10.1016/j.jadohealth.2006.02.014. [DOI] [PubMed] [Google Scholar]
- Rutta E, Gongo R, Mwansasu A, Mutasingwa D, Rwegasira V, Kishumbu S, Ramadhani H. Prevention of mother-to-child transmission of HIV in a refugee camp setting in Tanzania. Glob Public Health. 2008;3(1):62–76. doi: 10.1080/17441690601111924. 789682835 [pii] 10.1080/17441690601111924 [doi] [DOI] [PubMed] [Google Scholar]
- Rutter M. Resilience in the face of adversity. Protective factors and resistance to psychiatric disorder. British Journal of Psychiatry. 1985;147(6):598–611. doi: 10.1192/bjp.147.6.598. [DOI] [PubMed] [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Rutter M. Implications of Resilience Concepts for Scientific Understanding. In: Lester B, Masten A, McEwen B, editors. Resilence in Children: Annals of the New York Academy of Sciences. Vol. 1094. Blackwell; 2006. [DOI] [PubMed] [Google Scholar]
- Salisbury KM. National and state policies influencing the care of children affected by AIDS. Child Adolesc Psychiatr Clin N Am. 2000;9(2):425–449. [PubMed] [Google Scholar]
- Sapienza JK, Masten AS. Understanding and promoting resilience in children and youth. Current Opinion in Psychiatry. 2011;24(4):267–273. doi: 10.1097/YCO.0b013e32834776a8. 210.1097/YCO.1090b1013e32834776a32834778. [DOI] [PubMed] [Google Scholar]
- Sayson R, Meya AF. Strengthening the roles of existing structures by breaking down barriers and building up bridges: Intensifying HIV/AIDS awareness, outreach, and intervention in Uganda. Child Welfare: Journal of Policy, Practice, and Program. 2001;80(5):541–550. [PubMed] [Google Scholar]
- Schaefer ES. Children’s Reports of Parental Behavior: An Inventory. Child Dev. 1965;36(2):413–424. [PubMed] [Google Scholar]
- Selikow T-A, Ahmed N, Flisher AJ, Mathews C, Mukoma W. I am not ‘umqwayito’: A qualitative study of peer pressure and sexual risk behaviour among young adolescents in Cape Town, South Africa. Scandinavian Journal of Public Health. 2009;37(2, Suppl):107–112. doi: 10.1177/1403494809103903. [DOI] [PubMed] [Google Scholar]
- Silver EJ, Bauman LJ, Camacho S, Hudis J. Factors associated with psychological distress in urban mothers with late-stage HIV/AIDS. AIDS Behav. 2003;7(4):421–431. doi: 10.1023/b:aibe.0000004734.21864.25. [DOI] [PubMed] [Google Scholar]
- Skovdal M, Ogutu VO, Aoro C, Campbell C. Young carers as social actors: Coping strategies of children caring for ailing or ageing guardians in Western Kenya. Social Science & Medicine. 2009;69(4):587–595. doi: 10.1016/j.socscimed.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Smith Fawzi MC, Eustache E, Oswald C, Surkan P, Louis E, Scanlan F, Mukherjee J. Psychosocial functioning among HIV-affected youth and their caregivers in Haiti: implications for family-focused service provision in high HIV burden settings. AIDS patient care and STDs. 2010;24(3):147–158. doi: 10.1089/apc.2009.0201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sopena S, Evangeli M, Dodge J, Melvin D. Coping and psychological adjustment in adolescents with vertically acquired HIV. AIDS Care. 2010;22(10):1252–1258. doi: 10.1080/09540121003668110. 924492141 [pii] 10.1080/09540121003668110. [DOI] [PubMed] [Google Scholar]
- Stein JA, Rotheram-Borus MJ, Lester P. Impact of parentification on long-term outcomes among children of parents with HIV/AIDS. Family Process. 2007;46(3):317–333. doi: 10.1111/j.1545-5300.2007.00214.x. [DOI] [PubMed] [Google Scholar]
- Sweifach J, LaPorte HH. Perceptions of peer to peer HIV/AIDS education: A social work perspective. Journal of HIV/AIDS Prevention in Children & Youth. 2007;7(2):119–134. doi: 10.1300/J499v07n02_08. [DOI] [Google Scholar]
- Thurman TR, Snider LA, Boris NW, Kalisa E, Nyirazinyoye L, Brown L. Barriers to the community support of orphans and vulnerable youth in Rwanda. Social Science & Medicine. 2008;66(7):1557–1567. doi: 10.1016/j.socscimed.2007.12.001. [DOI] [PubMed] [Google Scholar]
- UNAIDS. 2008 Report on the global AIDS epidemic. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- UNAIDS, UNICEF, & USAID. Children on the brink 2004: A joint report of new orphan estimates and a framework for action. New York: United Nations; 2004. [Google Scholar]
- Ungar M. The Social Ecology of Resilience: Addressing Contextual and Cultural Ambiguity of a Nascent Construct. American Journal of Orthopsychiatry. 2011;81(1):1–17. doi: 10.1111/j.1939-0025.2010.01067.x. [DOI] [PubMed] [Google Scholar]
- UNICEF. Africa’s orphaned and vulnerable generations: Children affected by AIDS. Vol. 2008. New York: UNICEF, UNAIDS, & PEPFAR; 2006. [Google Scholar]
- Werner EE. High-risk children in young adulthood: A longitudinal study from birth to 32 Years. American Journal of Orthopsychiatry. 1989;59(1):72–81. doi: 10.1111/j.1939-0025.1989.tb01636.x. [DOI] [PubMed] [Google Scholar]
- Wood K, Chase E, Aggleton P. ‘Telling the truth is the best thing’: Teenage orphans’ experiences of parental AIDS-related illness and bereavement in Zimbabwe. Social Science & Medicine. 2006;63(7):1923–1933. doi: 10.1016/j.socscimed.2006.04.027. [DOI] [PubMed] [Google Scholar]
- Zhao G, Li X, Fang X, Zhao J, Hong Y, Lin X, Stanton B. Functions and sources of perceived social support among children affected by HIV/AIDS in China. AIDS Care. 2011;23(6):671–679. doi: 10.1080/09540121.2010.525619. [DOI] [PMC free article] [PubMed] [Google Scholar]