Abstract
Characterization and biological roles of the peroxisome proliferator-activated receptor (PPAR) isotypes are well known in monogastrics, but not in ruminants. However, a wealth of information has accumulated in little more than a decade on ruminant PPARs including isotype tissue distribution, response to synthetic and natural agonists, gene targets, and factors affecting their expression. Functional characterization demonstrated that, as in monogastrics, the PPAR isotypes control expression of genes involved in lipid metabolism, anti-inflammatory response, development, and growth. Contrary to mouse, however, the PPARγ gene network appears to controls milk fat synthesis in lactating ruminants. As in monogastrics, PPAR isotypes in ruminants are activated by long-chain fatty acids, therefore, making them ideal candidates for fine-tuning metabolism in this species via nutrients. In this regard, using information accumulated in ruminants and monogastrics, we propose a model of PPAR isotype-driven biological functions encompassing key tissues during the peripartal period in dairy cattle.
1. Introduction
In humans, mouse, and rat, nuclear receptors (NR), including PPARs, form a transcription factor family of 47–49 members [1]. Activity of NR allows for long-term (hours to days) control of metabolism because they can affect mRNA expression of target genes, including metabolic enzymes [2]. Thus, NR represent an important regulatory system in cells, tissues, and organs playing a central role in metabolic coordination of the entire organism.
Peroxisome proliferator-activated receptors (PPARs) were originally identified in Xenopus frogs [3] as novel members of the NR that induced the proliferation of peroxisomes in cells, a process that was accompanied by activation of the promoter of the acyl-CoA oxidase gene (ACOX1) encoding the key enzyme of peroxisomal long-chain fatty acid (LCFA) β-oxidation. The PPARα was the first member or isotype of the PPARs to be discovered in mammals during the search of a molecular target for liver peroxisome proliferators [4]. Those compounds include hypolipidemic drugs, that is, fibrates (e.g., clofibrate, fenofibrate, or Wy-14643), whose main effect is to lower blood triacylglycerol (TAG) and regulate cholesterol concentrations [5].
Initial characterization of PPARα (gene symbol PPARA in human and ruminants) in the adult mouse revealed that it was highly expressed in liver, kidney, and heart [4]. Shortly after PPARα was discovered, the isotypes PPARγ (gene symbol PPARG) and PPARβ/δ (gene symbol PPARD) were cloned [3, 6]. In monogastrics, PPARA is highly abundant in liver, intestine, heart, and kidney; PPARG is abundant in adipose and immune cells, while PPARD is ubiquitously expressed [7, 8]. In the mouse, both PPARγ isoforms γ1 and γ2 act in white and brown adipose tissue to promote adipocyte differentiation and lipid storage. While PPARγ2 is mainly expressed in adipocytes, PPARγ1 is expressed at modest levels also in other cells/tissues [9]. Expression of PPARβ/δ in murine resembled closely that of PPARα and was the sole isotype expressed in brain [6]. More recent studies in rats have established that PPARβ/δ is expressed ubiquitously throughout the body but is substantially more abundant in skeletal muscle than PPARα or PPARγ [7].
The PPARs form and function as heterodimers with retinoid-X-receptor (RXR). Once the ligand binds (e.g., LCFA, fibrates, thiazolidinedione (TZD)) to the ligand-binding domain (LBD), it produces a covalent modification of the PPAR structure [10] activating the NR. The activated PPAR/RXR binds to a specific DNA sequence (PPAR response element, PPRE) in the promoter region of specific target genes inducing or repressing their expression. The PPRE is a direct repeat of a hexanucleotide (AGGTCA) separated by a single nucleotide (i.e., DR-1). The DR-1 varies for each of the PPAR isotypes, thus conferring greater or lower strength to the PPAR/RXR complex for binding to PPRE and the strength of activation [11]. All PPAR isotypes are activated by ligand concentrations in the μM range or below, at least in nonruminants [12–14].
2. Role of PPAR in Monogastrics
The PPAR isotypes play multiple roles in mammals. There are a vast number of excellent reviews discussing those aspects in detail (e.g., [2, 5, 15–19]). Among others, the PPAR isotypes play important roles in regulating lipid and glucose metabolism, controlling inflammatory response, regulating tissue repair and differentiation, and cancer progression. Although with contrasting roles, PPAR isotypes affect blood vessel formation [20]. The PPARγ is pivotal in controlling the switch between adipogenesis and osteogenesis [17, 21] and insulin sensitivity [22], and it has an important neuroprotective role [23]. Similarly, it is well established that PPARα plays a crucial role in hepatic fatty acid catabolism in mitochondria, peroxisome, and microsomes [18]. The PPARβ/δ controls fatty acid catabolism in skeletal muscle and heart [2]. The PPAR isotypes are known to play important roles in all the reproductive tissues studied to date (reviewed in [24]). Due to the important functions played by the PPAR isotypes, PPARα and PPARγ have long been considered promising drug targets for human metabolic disorders as they regulate lipid and/or glucose homeostasis by controlling uptake, synthesis, storage, and clearance [25].
3. PPAR Isotype Expression in Ruminant Tissues
Judging from the published literature, the interest on PPAR isotypes in ruminants, particularly their role in lipid metabolism, has been modest compared to the vast literature in nonruminants, including human. Therefore, information about protein and gene expression abundance in ruminants is relatively scant. In order to help close this gap of knowledge we have performed Real-Time RT-PCR (qPCR) analysis to provide an evaluation of the relative distribution of PPAR isotypes in bovine tissues of adult Holstein dairy cows (i.e., three adipose depots, jejunum, liver, kidney, hoof corium, lung, placenta, and mammary), Holstein calves (semitendinosus muscle and rumen epithelium), longissimus muscle from Angus beef steers, and two cell lines obtained from adult bovines (Figure 1(a)). The data revealed that overall the relative distribution of PPAR isotypes in bovine tissues/cells is similar to other species.
Figure 1.
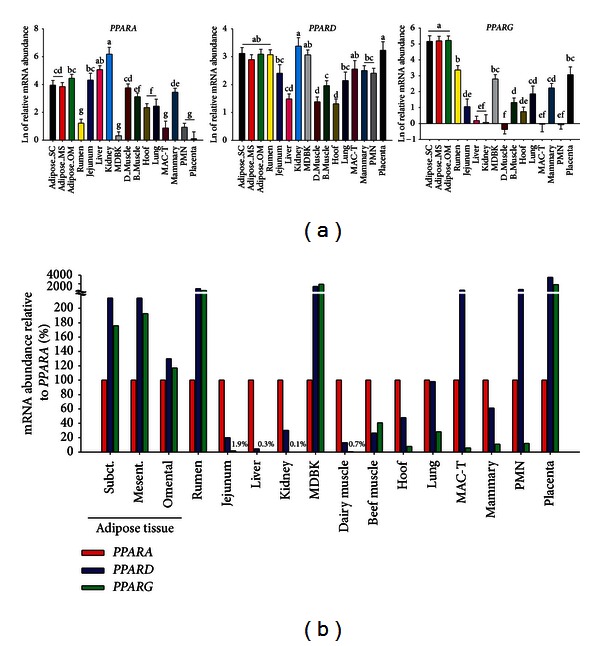
(a) Relative transcript abundance of each PPAR isotype in several bovine tissues and cells. We measured gene expression of PPAR isotypes in 14 different tissues including tissues from adult dairy cattle: adipose tissue (subcutaneous, mesenteric, and omental), small intestine (jejunum), liver, hoof corium, lung, kidney, mammary gland, blood polymorphonuclear leukocytes (PMN), and placenta; from dairy calves: rumen papillae and semitendinosus muscle (D-muscle); skeletal muscle of beef cattle (Longissimus lombarum); and two cell lines: Madin-Darby Bovine Kidney (MDBK) and bovine mammary alveolar cells (MAC-T). The total RNA was extracted and qPCR performed as previously described [26]. The qPCR data were normalized by the geometrical mean of 5 internal control genes (PPP1R11, RPS15A, ACTB1, MRPL39, and UXT). For the difference of each PPAR isotype abundance between tissues, the qPCR data were transformed using a 6-point standard curve prior statistical analysis using PROC GLM of SAS (version 9.3) with tissue as main effect. Dissimilar letters denote significant differences (P < 0.05). (b) Tissue-specific relative mRNA abundance between PPAR isotypes. The % relative abundance of the three PPAR isotypes in each tissue was calculated using the delta Ct method as previously described [27]. The final data for PPARG and PPARD were obtained as % relative to PPARA. N.B.: the y-axis values in (a) are least square means of the Ct values transformed using the standard curve and then log2-transformed. The values in (b) are calculated without use of a standard curve. Therefore, the values in (a) are radically different compared to the values in (b) and the two cannot be compared.
3.1. PPARγ
This PPAR isotype has been the most-studied in ruminants. Our results from qPCR analysis (Figure 1(a)) indicated that PPARG expression is very high in all adipose tissues, followed by rumen, Madin-Darby Bovine Kidney cell line (MDBK), and placenta with moderate-to-low mRNA expression in small intestine, beef cattle longissimus muscle, hoof corium, lung, and mammary gland. In contrast, the lowest expression of PPARG was detected in liver, kidney, dairy calf semitendinosus muscle, bovine mammary alveolar cell line (MAC-T), and blood polymorphonuclear leukocytes (PMN) (Figure 1(a)). In an early study bovine PPARγ mRNA expression (via northern blot) was characterized in several tissues [29]. Similar to our data (Figure 1(a)), a greater expression of PPARG was detected in adipose tissue followed by spleen, lung, and ovary. Although lower, expression was also detected in mammary gland and small intestine. Expression was absent in pancreas and almost undetectable in liver. In other tissues the expression was very low or nondetectable. The PPARG is highly expressed in adipose tissue of mice [6], human [9], and chicken [30], all of which agree with the relative high expression in bovine adipose tissues (Figure 1(a)). Similar to mouse [6], human [9], pig [31], chicken [30], and beef bulls [32], the expression of PPARG in bovine liver, or other tissues such as kidney and intestine, was very low (Figure 1(a)).
We and others have previously detected expression of PPARG in bovine mammary tissue and the MAC-T cell line using qPCR [26, 33, 34]. In a recent study in our laboratory comparing gene expression between mammary gland and MAC-T cells, the former had greater expression of PPARG both during pregnancy and lactation [35]. The relatively high expression of PPARG in MDBK cells detected (Figure 1) confirmed previous observations [36]. Expression of PPARG was detected also in goat mammary, although at a significant lower level compared to bovine [37].
The PPARG is expressed at all stages during bovine embryo development (both in the inner mass and in the trophectoderm [38]) and in the placenta (cotyledons and caruncles) of bovine [39] and sheep [40], with an evident expression in the trophoblast [41]. Lutein cells [42] and uterus [43] express PPARG, but not bovine endometrial cells [44], while endometrial cells of pregnant ewes express this NR [41]. The expression of PPARG in ovary was confirmed in sheep [45] and the same study reported expression in pituitary gland but not hypothalamus. In previous studies it has been shown that this PPAR isotype is expressed in bovine aortic endothelial cells [46], beef cattle skeletal muscle (including intramuscular fat) [47], ovine intramuscular fat [48], bovine perimuscular preadipocytes [49], and bovine retinal pericytes [50]. In several beef cattle breeds, PPARG had a similar degree of expression in perirenal and omental adipose depots, followed by intramuscular fat and, in a minor quantity, in the longissimus muscle [47, 51].
The expression of various PPARγ isotypes in buffalo was recently evaluated [52] and found to be expressed in all tissues tested: ovary (follicles and corpus luteum), mammary gland, adipose tissue, liver, spleen, and lung. The isoforms PPARγ1a and 1b were highly expressed in ovarian tissue followed by spleen and mammary gland, respectively, while PPARγ2 was highly abundant in adipose tissue.
3.2. PPARα
This isotype has been less studied compared with PPARγ. The bovine PPARα gene is located in chromosome 5 in cattle [53]. The qPCR analysis of the relative mRNA abundance of PPARA highlighted, as in mice [6], human [54], and pig [31], that PPARA is very abundant in kidney (Figure 1(a)). Contrary to this general feature, even though the PPARA in liver of chicken is expressed at lower level than kidney, its expression in liver is similar to other tissues [30]. In contrast to what is observed in human [54], our data revealed that the relative abundance of PPARA was not statistically different between jejunum and adipose tissues of bovine (Figure 1(a)). In general the data in Figure 1(a) reveals a more widespread expression of this PPAR isotype among the tissues and cells evaluated compared to PPARG. The highest expression was observed in kidney and liver followed by adipose tissues, small intestine, and dairy cattle semitendinosus muscle. Beef cattle longissimus muscle and mammary gland had relatively modest expression of PPARA followed by the least expression in hoof corium, lung, rumen, MDBK, MAC-T, PMN, and placenta (Figure 1(a)). We and others have consistently detected expression of PPARA in liver [55–60] and in MDBK cells in which also its activity was confirmed [28, 36, 61]. Partly corroborating our data (Figure 1), this PPAR isotype has been detected in bovine endothelial cells [62], skeletal muscle [63], rumen [64], uterus [43, 65], and neutrophils [66]. Similar to our data, it was observed very recently in young Limousin bulls that PPARA is expressed in liver, adipose, and muscle, with the greatest expression observed in liver, followed by semitendinosus muscle, and, then, intermuscular adipose tissue [32]. In ewes, its expression was detected in superficial endometrium and trophoblast during early pregnancy [41]. Lastly, expression of PPARA was demonstrated in sheep heart [67].
3.3. PPARβ/δ
As for nonruminants, the PPARβ/δ is the least-studied PPAR isotype also in ruminants, with few published information available. The results of our qPCR analysis indicate relatively similar PPARD mRNA expression in all the 14 tissues and cells assessed (Figure 1(a)); however, the greatest expression was observed in kidney and placenta followed by adipose tissues, rumen, and MDBK cells with the lowest expression observed in hoof corium, liver, and skeletal muscle (Figure 1(a)). The relative distribution of PPARD expression among cattle tissues/cells, even though similar to that in mouse [6], is rather curious particularly considering its low expression in skeletal muscle and the marked expression in blood neutrophils, placenta, and rumen tissue, that is, tissues that probably do not rely on LCFA oxidation as source of energy. Previous studies have observed expression of PPARD in bovine liver [56], aortic endothelial cells [68], mammary cells [69, 70], rumen [64], and uterus [43]. The PPARD was also shown to be expressed in longissimusmuscle of beef steers [47] and in both superficial endometrium and trophoblast of early pregnant ewes [41].
3.4. Relative Abundance between PPAR Isotypes in Cattle Tissues
To date, there is almost a complete lack of data available in the literature of a direct comparison of PPAR isotypes expression in ruminant tissues. Among the few available studies, it was observed that liver of dairy cows expresses a similar amount of PPARA and PPARD but does not express PPARG [44]. In a recent study where the expression of the three PPAR isotypes was evaluated in liver and muscle of beef bulls, the greatest expression was observed for PPARA, followed by PPARG, with the lowest expression for PPARD in liver, while, the largest expression in muscle was observed for PPARG [71]. This relative distribution among tissues is somewhat comparable to our data (Figure 1(b)). More numerous are the studies comparing mRNA abundance between PPAR isotypes in bovine cell culture. Those have revealed that bovine endometrial cells express PPARA and PPARD at a similar level, but not PPARG [44]. In addition, bovine aortic endothelial cells express both PPARA and PPARG [46] and mammary cells express both PPARG and PPARD [69].
When the relative mRNA abundance between the three PPAR isotypes was evaluated in several tissues from bovine (Figure 1(b)), we observed that the three adipose tissues along with rumen, MDBK cells, and placenta have a marked abundance of PPARD and PPARG compared with PPARA, whereas MAC-T cells and PMN were characterized by marked abundance of PPARD but very low abundance of the other two PPAR isotypes. Despite the relatively low abundance, at least in vitro, PPARγ appears to be functional in bovine neutrophils [72] and MAC-T cells [26]. Paradoxically, given its well-established function in monogastrics, with few exceptions (i.e., MDBK and beef cattle longissimus muscle), PPARD is more abundant than PPARG, even in the three adipose depots (Figure 1(b)). The PPARA instead was the more abundant PPAR isotype in small intestine, liver, kidney, skeletal muscle, hoof corium, lung, and mammary gland (Figure 1(b)).
Overall, the data in Figure 1 depict a distribution of PPAR isotypes that, similar to other species, seems to underscore the putative biological role of each PPAR isotype. For instance, the expression of PPARA is more abundant in tissues where LCFA oxidation is generally higher (e.g., liver and kidney) and PPARG is more abundant in lipogenic tissues (e.g., the three adipose tissues).
4. Sequence Homology, 3D Structure, and Activation of PPARα among Bovine, Mouse, and Human
We recently carried out an in silico analysis to compare the amino acid sequence homology of PPARα between bovine, mouse, and human [28]. The analysis revealed more than 90% conservation of this PPAR isotype between the three species, with bovine having greater overall homology to human (94.9%) than mouse (91.2%). When the four domains of the PPARα protein were compared, we observed lower conservation in the N-terminal A/B domain containing the ligand-independent activation function (AF-1), which was 86% conserved between bovine and human and 81% between bovine and mouse [17], and the largest conservation (i.e., 100%) in the DNA-binding domain. The latter suggests that the capacity of the domain for the recognition of the PPRE is highly conserved between species. This has been confirmed by the high responsiveness of rat PPRE when transfected in bovine endothelial cells [73].
The LBD is also highly conserved with greater homology of bovine with human (98%) than with mouse (92%). The lower conservation of the LBD and AF-1, which is common between species, could indicate a difference in interspecies sensitivity of PPARα activation [17] and a greater similarity between bovine and human than bovine and mouse. Surprisingly, when the transcription response of 30 putative PPARα target genes to the potent and specific PPARα agonist Wy-14643 were compared between mouse liver, human liver, and MDBK, we observed a greater number of genes with a common response between bovine and mouse (73%) than bovine and human (60%) [28]. Despite the limitation of comparing liver with kidney cells, those data indicate a good degree of conservation of PPARα response between species. There are no published studies comparing PPARγ or PPARβ/δ response between ruminant and nonruminant species considering the same (or similar) tissue/cells. An attempt to compare the activation of PPARγ in mammary gland between dairy cattle and mouse is reported (see Section 9.2.1).
In order to further investigate the potential differences in PPARα between mouse and bovine we performed an in silico 3-dimensional (3D) structure analysis of the publicly available PPARα protein sequence [28]. The alignment analysis identified an overall high degree of conservation of PPARα amino acid sequence between the two species; however, when the overlap of the 3D structure of the PPARα of the two species was performed, we observed important differences in spatial structure of the LBD. In particular, the residues Leu462 and Tyr466 of the LBD in bovine result in a completely different spatial position compared with mouse (Figure 2). When the electrostatic potential of the surface was visualized, it was apparent that the bovine PPARα has an overall more neutral charge, particularly in the ligand pocket, compared with the highly negatively charged mouse PPARα. This allowed inferring that longer and more saturated LCFA (i.e., more neutrally charged and with a more straight configuration) might be more easily accommodated (Figure 2), hence, likely be better inducers in bovine.
Figure 2.
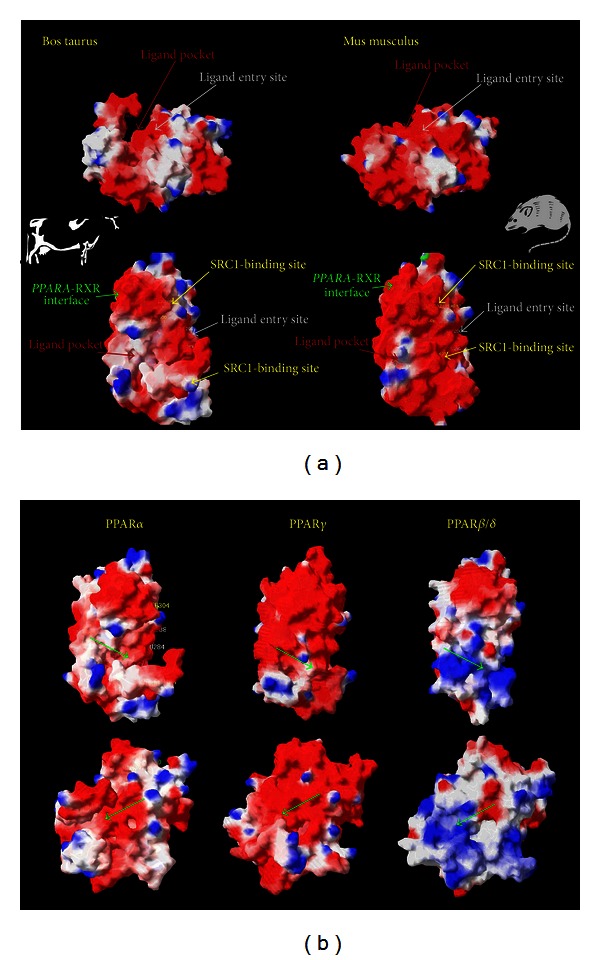
Inter-species and inter-isotypes three-dimensional PPAR protein structure comparisons. (a) Three-dimensional surface structure of bovine (residue 202–470; UniProtKB/TrEMBL Q5EA13) and mouse (residue 202–468; UniProtKB/TrEMBL P23204) PPARα ligand binding domain (LBD). The upper and lower panels include two views of the 3D structure of the PPARα protein in bovine and mouse species. The 3D structure is in full alignment between species. From the comparison, the difference in the ligand pocket of the PPARα between the two species is evident, with a larger and more pronounced pocket in bovine compared with mouse. In addition, the bovine PPARα appears to be more neutrally charged compared with the same protein in mouse. (b) Three-dimensional surface structure comparisons between PPARα (residue 202–470; Q5EA13), PPARγ (residue 234–505; O18971), and PPARβ/δ (residue 171–441; A4IFL4) LBD of bovine. Shown is the ligand pocket domain (green arrow) in two diverse views for each of the PPAR isotypes. The comparison highlights the larger and more neutrally charged ligand pocket in PPARα compared with the more negatively charged PPARγ ligand pocket and positively charged and small PPARβ/δ ligand pocket. The images were modified from [28]. Legend: red = negative charge; white = neutral charge; blue = positive charge. The 3D analyses were performed using Swiss-Pdb Viewer software (freely available at http://spdbv.vital-it.ch/).
It has been demonstrated, however, that the activation of PPAR isotypes is highly dependent on the A/B domain rather than the LBD [74]. This last observation could explain the interspecies differences observed, considering also that the A/B domain is the least-conserved between species and also between PPAR isotypes (see below). However, this does not fully explain the results from the comparison in PPARα response between bovine, mouse, and human [28] because the conservation of the A/B domain is lower between mouse and bovine than between human and bovine, despite the greater similarity in response between bovine and mouse compared to bovine and human [28].
5. Structural Similarity between PPAR Isotypes in Bovine
Approximately 80% of the 34 amino acid residues in the binding cavity of the three PPAR isotypes (α, β/δ, and γ) are conserved in humans and rodents [75]. The main features dictating the ligand specificity across the PPAR isotypes appear to be the topology of the ligand binding cavity; for example, the PPARβ/δ cavity is much narrower than PPARα and PPARγ and, thus, cannot accommodate bulky polar heads found in thiazolidinedione (TZD) [75, 76]. In contrast, TZD is a potent ligand of PPARγ. Once inside the cavity, the side chains of the ligand (e.g., hydrogen, carboxyl groups) interact with the amino acid residues to achieve a stable configuration.
In bovine, the three PPAR isotype proteins have low conservation overall, with PPARα being more similar to PPARβ/δ (59%) than PPARγ (52%) [28]. The three proteins have a large degree of conservation in the DNA binding domain (>80%), but a low degree of conservation in the A/B domain (<21%) [28]. The PPARα has a greater degree of conservation in the LBD with PPARβ/δ (71%) than PPARγ (64%) [28]. This last observation suggests that among the three isotypes, the expected response to agonists should be more similar between PPARα and PPARβ/δ as it is the case in nonruminants [2]. This would imply that activation of PPARα and PPARβ/δ could result in similar outcomes, for example, fatty acid catabolism.
The 3D depiction of the bovine PPAR isotypes surface reveals a difference in the ligand pocket (Figure 2) [28]. The PPARα appears to have a larger pocket compared with the other two PPAR isotypes. In addition, analysis of the electrostatic potential of the surface indicates a greater negative charge in PPARγ than PPARα and PPARβ/δ, with the latter being mostly positively charged. Those observations suggest a greater capacity of PPARα for binding neutrally charged and/or more structurally rigid compounds. Clearly, this inference is only speculative.
6. Ruminant PPAR Response to Synthetic and Natural Agonists
The effect of PPAR agonists in nonruminants has been tested in different models using in vitro systems with specific assays such as the Coactivator-Dependent Receptor Ligand Assay (CARLA) [18] or the transfection of PPRE with firefly luciferase (e.g., [96]). An additional assay available today is the direct measurement of activation of PPAR isotypes after nuclear isolation by the presence of PPRE immobilized onto the bottom of cell culture wells; however, such assays have not been developed for ruminants [61]. The use of these techniques with greater sensitivity, precision, and reliance in ruminants has been scant [61]. Most of the studies performed in ruminants are based on measurements of changes in expression of genes or proteins after treatment with PPAR isotype-specific agonists.
6.1. Ruminant PPAR Response to Synthetic Agonists
Several synthetic PPAR agonists are available today for nonruminants [18]. Among the most commonly used are Wy-14643 and fenofibrate as PPARα agonists and TZD and rosiglitazone as PPARγ agonists. Very few synthetic agonists of PPARβ/δ are known (e.g., GW501516). Besides agonists, a few antagonists have been developed, for example, the PPARγ specific antagonists GW9662 [97] and BADGE [98], the PPARα antagonists T0070907 [99] and GW6471 [100], and the PPARβ/δ antagonists GSK0660 [101] and GSK3787 [102]. The use of the specific agonists in combination with antagonists could be a valid, though indirect, approach to uncover both the existence of an active PPAR isotype in cells or tissues and PPAR target genes.
Supplementary Table 1 (see Supplementary Material available online at http://dx.doi.org/10.1155/2013/684159) contains a summary of studies performed to date using specific PPAR agonists in ruminants. From the data, it is evident that most of the studies dealt with bovine with few ones in sheep and goat. A large amount of the bovine studies were performed with bovine endothelial cells. Those cells have been widely used as a model to study endothelial physiology and pathology, particularly for the inflammatory status related to arteriosclerosis, that is, with a clear biomedical purpose and not to understand ruminant biology. Overall those studies established important roles of PPAR in endothelial cells [46, 92, 103, 104]. In particular the activation of PPARγ and PPARα appears to have a protective role for endothelium (Supplementary Table 1).
The first study performed using a PPAR agonist with a clear aim to understand the biology of ruminants was performed in 1998 by a German group [42] where it was observed that PPARγ controls progesterone synthesis in lutein cells isolated from dairy cows. Subsequent studies in granulosa cells of sheep confirmed the role of PPARγ in controlling progesterone synthesis [45].
In 1998, a Japanese group demonstrated that activation of PPARγ is central for adipogenic differentiation of vascular stromal cells from bovine adipose tissue [105] and intramuscular fibroblast-like cells [106]. In 2001, another Japanese group demonstrated that in vivo injection of the PPARγ agonist 2,4-TZD partially reversed the insulin resistance induced by TNFα in dairy steers. The phenomenon was explained by the activation of PPARγ in adipose tissue [107]. A year later a group of researchers from a pharmaceutical company fed the PPARα agonist Wy-14643 to lactating goats [108]. The authors reported an overall increase in hepatic β-oxidation and aromatase activity by Wy-14643 and decreased cholesterol in blood (with numerical decrease of TAG as well). No effects were observed on liver size, milk composition, or content of hepatic cytochrome P450. The low magnitude of changes and the unexpected lack of effect of the treatment on P450 led the authors to conclude that the goat is a weak responder to PPARα agonists.
The two studies in vivo mentioned above were critical for animal bioscientists interested in PPAR because they demonstrated that PPARα in liver and PPARγ in adipose tissue of ruminants are active and likely play similar roles as in monogastrics: regulation of β-oxidation for PPARα and regulation of adipogenesis and insulin sensitivity for PPARγ. Since then, few additional in vivo studies using PPAR agonists with agricultural aims have been performed (Supplementary Table 1). Recently, we tested the effects of oral administration for 14 days of the PPARα agonist clofibrate on liver of weaned dairy calves [78] (see also Supplementary Table 1). The treatment had several expected effects such as the increase in expression of several PPARα target genes (see Section 7 for details about PPAR targets in ruminants), but the magnitude of response was lower than usually observed in rodents; thus, we concluded, as for the work performed on goats, that the bovine hepatic PPARα is a weaker responder compared to rodents.
The above observations from in vivo studies of a weak response in ruminants might be explained by the inherent differences in digestive physiology. Contrary to monogastrics, in ruminants, the digestion of any feed is markedly affected by the process of fermentation in the rumen via microorganisms. None of the above studies have assessed the effect of the rumen on PPAR agonists. In this regard, it could have been interesting to measure the blood concentration of the agonists. Interestingly, the human PPAR isotypes also appear to have a lower response compared with rodents [19]. It can also be the case that Wy-14643, a recognized potent PPARα agonist in rodents, is not as potent in ruminants. In accord with this, we have observed in bovine cells a greater increase in expression of PPARα target genes by saturated LCFA compared to Wy-14643 [28]. Those responses indicate a species-specific response to PPAR induction and a different effect of agonists between species.
The results obtained during the in vivo study of the Japanese group mentioned above led to a series of in vivo experiments in pregnant and lactating dairy cows [82, 84, 109, 110]. The purpose of those studies was to evaluate the effects of PPARγ activation on preventing metabolic problems typical of the peripartal period. The specific PPARγ agonist 2,4-TZD was used (via injection) for that purpose (Supplementary Table 1). The treatment with 4 mg/kg BW daily of 2,4-TZD during the last two or three weeks prepartum until parturition decreased substantially the NEFA post-partum. Such effect was ascribed to enhanced insulin sensitivity and PPARG expression in adipose. In addition, the treatment improved the overall metabolic health postpartum, as reflected in greater feed intake, lower hepatic lipid accumulation, and greater glycogen content in the liver. Overall, the data also suggested an improved fertility (i.e., lower open days) in cows treated with 2,4-TZD.
This series of in vivo experiments reported above (see also Supplementary Table 1) was the first demonstration that PPAR isoforms can play a pivotal role in the physiology and metabolism of dairy cattle. It also underscores the concrete possibility of fine-tuning the PPAR isotype activity through appropriate treatments in order to improve overall performance and health of dairy cattle.
An elegant in vivo study performed recently in pregnant sheep involved the injection of rosiglitazone into the fetuses for >10 days beginning at ca. 25 days before term [81]. The experiment demonstrated that activation of PPARγ had a similar effect on fetuses as overnutrition of the pregnant mother, which is known to induce obesity in later life in offsprings. For instance, rosiglitazone treatment increased expression of lipoprotein lipase and adiponectin in adipose tissue and PPARA and PPARγ coactivator 1 alpha (PPARGC1A) in liver of fetuses (Supplementary Table 1).
Several in vitro studies using synthetic agonists have demonstrated that activation of PPAR isotypes (except gamma) affects fertility by increasing the expression and/or production of prostaglandins, for example, prostaglandin (PG) F2α, and PGE2 in bovine endometrial cells [44, 77]. Other in vitro studies were carried out in order to test the response to PPAR isotypes in two bovine cell lines (MDBK and MAC-T) with the purpose of determining PPARα and PPARγ target genes [26, 28, 36, 61]. Besides target genes, those studies also uncovered several biological functions of PPAR isotypes in ruminants. For instance, the activation of PPARγ in MAC-T cells with rosiglitazone provided a demonstration that PPARγ controls expression of several genes known to be involved in milk fat synthesis [26] while activation of PPARα controls lipid metabolism at the cellular and organismal level (i.e., by controlling expression of several signaling molecules) [28].
All the above studies clearly demonstrated an active role of PPAR isotypes in ruminants. The studies also established that PPAR isotypes can be manipulated by using synthetic agonists; however, from a practical stand-point the suggestion of using synthetic agonists is not feasible, namely, because of the high costs that would be incurred. Clearly that could be circumvented if natural ligands are identified.
6.2. Ruminant PPAR Response to Natural Agonists
6.2.1. LCFA
The great interest in PPARs in the area of nutrition stems from the ability to bind and be activated (or inhibited) by LCFA or chemically related derivatives [18, 111, 112].
Monogastrics. In monogastrics all PPAR isotypes are sensitive to fatty acids, particularly LCFA. Although the potency varies with each PPAR isotype, the most-potent PPAR endogenous ligands in nonruminants are linoleic acid, linolenic acid, arachidonic acid, and also derivatives of arachidonic acid such as leukotriene B4 (LTB4) or PG [12]. In general it is safe to conclude that PPAR isotypes in most monogastrics species studied to date have a greater sensitivity towards unsaturated than saturated [17, 18]. However, in nonruminants both saturated and unsaturated LCFA enhance PPAR transactivation in vitro (e.g., [12, 113, 114]).
In vivo data have been more variable and in some instances high dietary fat activated PPAR target genes regardless of whether the dietary lipid was mostly polyunsaturated (PUFA), monounsaturated, or saturated (e.g., [115]). At the cellular level studies with endogenous ligands such as free LCFA or LCFA-CoA (i.e., activated 16:0, 18:2n-6, 18:3n-3, and 20:4n-6) have demonstrated (at least for PPARα) that both forms of the FA exhibit high affinity (i.e., low nanomolar dissociation values) for the ligand-binding domain of PPAR [114]. This point is important because intranuclear concentrations of free LCFA and LCFA-CoA range between 120–500 nM and 8 nM, respectively [116].
From a mechanistic standpoint it is important to point out that FA binding proteins (FABP, particularly FABP1 and FABP4) are important in channeling intracellular nonactivated (i.e., without addition of the CoA group) LCFA not only to the various organelles but also to the nucleus where the LCFA can activate PPAR. The essential role of FABP in transporting LCFA into the nucleus for the activation of PPAR isotypes was first reported in rodent liver where the amount of FABP1 protein significantly correlated with transactivation of PPAR in response to LCFA (linoleic acid, linolenic acid, and arachidonic acid) as well as other chemical ligands [117].
Ruminants. To our knowledge there are only two published studies where PPRE luciferase was used to test activation of PPAR isotypes in bovine cells [62, 68]. In one study, however, only activation of PPARβ/δ was assessed and no LCFA were tested. In another study the activation of PPARα by free LCFA or oleic acid was demonstrated in bovine aortic endothelial cells [62]. So far the effect of LCFA on ruminant PPAR activity has been evaluated primarily in an indirect way through measuring changes in expression of target genes after addition of specific LCFA. This model has limitations, one being the capacity of LCFA to bind and activate additional transcription factors (TF). Besides PPARs, also Hepatic Nuclear Factor 4 (HNF4α), Liver X Receptor (LXR), and RXR can bind LCFA, as shown in human, mouse, and rat [118]; however, in those species the LXRβ and the RXRα appear to be weakly activated by natural LCFA while PPARα, PPARβ/δ, and PPARγ are strongly activated [119]. The greater sensitivity of PPAR compared with other TF provides some support for the use of target gene expression as a proxy for evaluating activation of PPARs by LCFA. Another limitation of the indirect approach is the inability to distinguish the activation between PPAR isotypes. Using the above indirect approach it was demonstrated that ruminant PPAR are activated by several physiologically relevant LCFA (Table 1).
Table 1.
Activation of PPAR isotypes in ruminants by main long-chain fatty acids or glucose.
| LCFA/glucose | Effect on PPAR isotype@ | Method# | References | ||
|---|---|---|---|---|---|
| PPARα | PPARγ | PPARβ/δ | |||
| 16:0 | +++ | +++ | n/a | Indirect | [26, 28, 61] |
| 18:0 | +++ | +++ | n/a | Indirect | [26, 28] |
| c9-18:1 | ++ | + | n/a | Indirect/Luciferase | [26, 28, 62] |
| t10-18:1 | n/a& | + | n/a | Indirect | [26] |
| 18:2 | + | n/a | n/a | Indirect | [26, 28] |
| c9,t11-18:2 | + | n/a | n/a | Indirect | [26, 28] |
| t10,c12-18:2 | + | ± | n/a | Indirect | [26, 28] |
| CLAmix$ | + | n/a | n/a | Indirect | [36, 77] |
| 20:0 | ++ | n/a | n/a | Indirect | [26, 28] |
| 20:4n-6 | ++ | n/a | ++* | Indirect/Luciferase | [68, 77] |
| 20:5n-3 | ++ | ++ | n/a | Indirect | [26, 28] |
| 22:6n-3 | + | n/a | n/a | Indirect | [26, 28] |
| Glucose | No | n/a | ++ | Luciferase | [68] |
@+++: strong agonist; ++: agonist; +: weak agonist; ±: mixture between agonist and antagonist.
*The 12-HETE, a metabolite of the 20:4n-6 is the actual agonist.
#Indirect: the effect on PPAR isotype target genes was uncovered by the use of specific PPAR synthetic agonists; luciferase: the use of the PPRE-luciferase construct to test activation of PPAR by agonists.
$A mixture (ca. 50% each) of the t10,c12- and c9,t11-conjugated 18:2
&Not available.
The LCFA experiments in ruminants were mainly performed with MAC-T and MDBK cells and focused on PPARα and PPARγ [26, 28, 36, 61]. In both cell types the LCFA clearly induced expression of genes previously shown using specific agonists (Wy-14643 and rosiglitazone) to be PPARα and PPARγ target genes (see Table 2 and Section 7 for details). The potency of saturated was greater than unsaturated LCFA. In particular, in MDBK cells we observed weaker induction of target genes as the degree of unsaturation increased [28]. Above all it was observed that palmitate and stearate induced a very strong activation of transcription of PPARα and PPARγ target genes [26, 28]. Those data were suggestive of an evolutionary adaptation of the PPAR in ruminants to respond to saturated LCFA, which are the most abundant LCFA in the circulation of ruminants [120, 121] compared to monogastrics [122, 123] due to extensive ruminal hydrogenation of unsaturated LCFA. However, our studies suggested that the LCFA activated gene expression not only through PPAR isotypes but also other TF, probably the ones mentioned above, or even other unknown TF [28]. This point, as well as the role of coactivators and their relative abundance [76], deserves further investigation in order to select with greater confidence the most suitable mixture of LCFA for modulating metabolism in ruminants.
Table 2.
PPAR isotype target genes in ruminants grouped by main biological function.
| Gene | HUGO gene name | Tissue/cells1 | PPAR2 | Reference |
|---|---|---|---|---|
| Fatty acid import and activation | ||||
|
| ||||
| ACSL1 | Acyl-CoA synthetase long-chain family member 1 | MDBK | ⇑ PPARα | [28, 61] |
| Liver | ⇑ PPARα | [78] | ||
| ACSL3 | Acyl-CoA synthetase long-chain family member 3 | MDBK | ⇑ PPARα | [28] |
| CD36 | Thrombospondin receptor | MDBK | ⇑ PPARα | [28] |
| BAEC | ⇑ PPARγ | [79] | ||
| MAC-T | ⇔ PPARγ | [26] | ||
| FABP4 | Fatty acid binding protein 4 | Muscle | ⇑ PPARγ | [80]# |
| MDBK | ⇑ PPARα | [28] | ||
| MAC-T | ⇔ PPARγ | [26] | ||
| LPL | Lipoprotein lipase | sP. adipose | ⇑ PPARγ | [81] |
| MAC-T | ⇔ PPARγ | [26] | ||
| bS. adipose | ⇔ PPARγ | [82] | ||
|
| ||||
| Fatty acid synthesis | ||||
|
| ||||
| ACACA | Acetyl-CoA carboxylase alpha | MAC-T | ⇑ PPARγ | [26] |
| FASN | Fatty acid synthase | MAC-T | ⇑ PPARγ | [26, 83] |
| bS. adipose | ⇔ PPARγ | [82] | ||
| bS. adipose | ⇓ PPARγ | [84] | ||
| INSIG1 | Insulin induced gene 1 | MAC-T | ⇑ PPARγ | [26] |
| SCD | Stearoyl-CoA desaturase (delta-9-desaturase) | MDBK | ⇑ PPARα | [28] |
| SREBF1 | Sterol regulatory element binding factor 1 | MAC-T | ⇑ PPARγ | [26] |
| MDBK | ⇑ PPARα | [28] | ||
|
| ||||
| Fatty acid oxidation | ||||
|
| ||||
| ACADVL | Acyl-CoA dehydrogenase, very long chain | MDBK | ⇑ PPARα | [61] |
| Liver | ⇑ PPARα | [78] | ||
| ACOX1 | Acyl-coenzyme A oxidase 1 | MDBK | ⇔ PPARα | [61] |
| Liver** | ⇑ PPARα | [78] | ||
| CPT1A | Carnitine palmitoyltransferase 1A (liver) | MDBK | ⇑ PPARα | [28, 36, 61] |
| Liver** | ⇑ PPARα | [78] | ||
| CPT2 | Carnitine palmitoyltransferase 2 | PAEC | ⇑ PPARγ | [85] |
| CRAT | Carnitine O-acetyltransferase | PAEC | ⇑ PPARγ | [85] |
| CYP4A11 | Cytochrome P450, family 4, subfam. A, polypeptide 11 | Liver | ⇑ PPARα | [78] |
|
| ||||
| Triacylglycerol synthesis | ||||
|
| ||||
| AGPAT6 | 1-acylglycerol-3-phosphate O-acyltransferase 6 | MAC-T | ⇑ PPARγ | [26] |
| DGAT1 | Diacylglycerol O-acyltransferase 1 | MAC-T | ⇑ PPARγ | [26] |
| LPIN1 | Lipin 1 | MAC-T | ⇑ PPARγ | [26] |
| MDBK | ⇑ PPARα | [28, 61] | ||
| LPIN3 | Lipin 3 | MDBK | ⇑ PPARα | [28, 78] |
|
| ||||
| Cholesterol synthesis | ||||
|
| ||||
| HMGCR | 3-Hydroxy-3-methylglutaryl-CoA reductase | MDBK | ⇑ PPARα | [28] |
| SREBF2 | Sterol regulatory element binding transcription factor 2 | MAC-T | ⇑ PPARγ | [26] |
|
| ||||
| Signaling molecules | ||||
|
| ||||
| ANGPTL4 | Angiopoietin-like 4 | Liver | ⇑ PPARα | [56, 86]++ |
| MDBK | ⇑ PPARα | [28] | ||
| FGF21 | Fibroblast growth factor 21 | Liver | ⇑ PPARα | [86]++ |
| EDN1 | Endothelin 1 | BAEC | ⇓ PPARα | [87] |
| ⇓ PPARγ | ||||
| LEP | Leptin | bS. adipose | ⇑ PPARγ | [84] |
| NOS3 | Nitric oxide synthase 3 (endothelial cell) | BAEC | ⇑ PPARα | [88] |
| PTGS2 | Prostaglandin-endoperoxide synthase 2 | BEND | ⇑ PPARα | [44] |
| ⇑ PPARγ | [44] | |||
| pBESC | ⇑ PPARα | [77] | ||
| MAC-T | ⇔ PPARγ | [26] | ||
| SPP1 | Osteopontin | MDBK | ⇑ PPARα | [28] |
| VEGF | Vascular endothelial growth factor | BAEC | ⇑ PPARγ | [89] |
|
| ||||
| Other functions | ||||
|
| ||||
| CDKN2A | Cyclin-dependent kinase inhibitor 2A | BAEC | ⇓ PPARγ | [90] |
| GAPDH $ | Glyceraldehyde-3-phosphate-dehydrogenase | s. ASC | ⇑ PPARγ | [91] |
| ⇑ PPARβ/δ | ||||
| OLR1 | Oxidized low density lipoprotein receptor 1 | BAEC | ⇑ PPARα | [92] |
| ⇓ PPARγ | [46] | |||
| PC | Pyruvate carboxylase | Hepatoma* | ⇑ PPARα | [93] |
| MDBK | ⇔ PPARα | [28] | ||
| SLC2A1 | Solute carrier family 2, member 1 | BAEC | ⇓ PPARβ/δ | [68] |
| TERF2 | Telomeric repeat binding factor 2 | BAEC | ⇑ PPARγ | [90] |
|
| ||||
| PPAR activation-related functions | ||||
|
| ||||
| PPARA | Peroxisome-proliferator-activated receptor alpha | BAEC | ⇑ PPARα | [62] |
| MDBK | ⇔ PPARα | [28, 61] | ||
| Liver | ⇑ PPARγ | [81] | ||
| Muscle** | ⇑ PPARγ | [81] | ||
| PPARG | Peroxisome-proliferator-activated receptor gamma | bEPC | ⇑ PPARγ | [94] |
| MAC-T | ⇔ PPARγ | [26] | ||
| PPARGC1A | PPARγ, coactivator 1 alpha | s. Muscle | ⇑ PPARγ | [81] |
1Acronyms: BAEC: Bovine Aortic Endothelial Cells; BEND: Bovine Endometrial Cells; bEPC: bovine renal Epithelial cells; BRCP: Bovine Retinal Capillary Pericytes; bS. Adipose: bovine subcutaneous adipose; pBESC: primary (16-day cycle) bovine endometrial stromal cells; MDBK: Madin-Darby Kidney Cell Line; PAEC: ovine pulmonary arterial endothelial cells; sP.adipose: sheep perirenal adipose; 1s. ASC: sheep adipose stem cells; s. Muscle: sheep muscle.
2The PPAR activated by the treatment with a different effect on expression of the target gene (⇑ induction; ⇓ inhibition; ⇔ no change).
*Rat hepatoma was transfected with bovine PC promoter region.
**The increase in expression was with P < 0.10 but P > 0.05.
$The activity and not the mRNA expression of GAPDH was measured.
#Inferred based on the high correlation of expression between PPARG and FABP4.
Because intracellular LCFA pools are a mixture of saturated and unsaturated LCFA, it is interesting that PPARγ (and maybe other PPAR isotypes) is capable of binding two LCFA simultaneously, at the least in monogastrics [124]. This suggests that there could exist a mechanism whereby the composition of LCFA in the cytosol dictates the “strength” of the response, that is, the ability to bind two LCFA simultaneously could allow PPARγ to give a graded response to the varying composition of the intracellular LCFA pool [124].
6.2.2. Glucose
Besides LCFA, it has been also reported that glucose binds and activates PPARα in mouse connecting glucose with lipid metabolism [125]. This has not been confirmed in ruminants; however, it has been shown that ruminant PPARβ/δ binds and is activated by glucose [68]. Specifically, it was demonstrated in bovine endothelial cells that when PPARβ/δ is activated by glucose, it downregulates glucose transport in order to prevent hyperglycemia.
6.2.3. Other Natural Agonists/Antagonists
As with nonruminants, PPARγ in bovine vascular endothelial and mammary cells is activated by PGJ2 [46, 69]. The PPARγ is inhibited and its expression decreased by the oxidative stress intermediate H2O2 in bovine endothelial cells [94, 126]. Nitric oxide appears to be an inhibitor because it decreased the expression of the PPARGC1A, a known PPARγ target gene [94]. This compound decreased the expression of PPARGC1A during the first 12 h after treatment but increased the expression of the same gene in the longer term (>24 h) [127]. The increase in expression of PPARGC1A was demonstrated to be crucial for the mechanism of protection from oxidative stress [127]. In bovine articular chondrocytes, the presence of oxidized LDL increased expression of vascular endothelial growth factor (VEGF) through PPARγ [128].
7. PPAR Isotype Target Genes in Ruminants
In several of our studies, the overall response of PPARα and PPARγ in bovine cells was strong and consistent [26, 28, 61, 129]. Those studies allowed uncovering several bovine-specific PPARα target genes (Table 2), and several were already established as PPARα targets in other species. Among bovine-specific PPARα target genes, the osteopontin (SPP1) gene had a large increase in expression after Wy-14643 treatment in bovine kidney cells [28] contrary to what has been observed in human and mouse [130, 131]. Between bovine, human, and mouse, only 67% of the putative PPARα target genes tested responded in a similar fashion, suggesting a species-specific response of PPAR [28].
The activation of PPARα by Wy-14643 resulted in a general increase in lipid metabolism-related genes including several involved in lipid synthesis, such as lipin 1 (LPIN1) and sterol regulatory element binding transcription factor 1 (SREBF1) [28]. Interestingly, expression of both genes was not induced in a previous study using the same model [61]. The only difference between the two studies was the addition of insulin in the latter [28]. In support of a potentially important role of insulin for PPAR activation, in a recent study with MDBK, we observed a faster response in expression of PPARα target genes after addition of insulin [61]. Therefore, insulin in bovine seems essential for PPAR activation but may be more crucial for some genes (e.g., LPIN1 and SREBF1 versus carnitine palmitoyltransferase 1A (CPT1A)) [28, 61].
The increased expression of SREBF1 with Wy-14643 in the MDBK study might also be due to the activation of PPARγ because we observed that activation of PPARγ with rosiglitazone increased expression of SREBF1 in MAC-T cells [26]. The activation of PPARγ in MAC-T cells appeared to be robust [26]; however, the use of 10 μM TZD for 12 h in MDBK cells did not affect expression of any gene tested using microarray technology, suggesting that activity of PPARγ in MDBK is extremely low or inexistent (Bionaz et al. unpublished data). This observation is intriguing considering that overall expression of PPARG in MDBK is relatively high compared with other tissues/cells (Figure 1(a)), and higher than PPARA (Figure 1(b)). Furthermore, the response to PPARα agonists is consistently high in those cells [28]. Therefore, it cannot be excluded that the increase in expression of SREBF1 after addition of Wy-14643 was due exclusively to PPARα activation.
Compiled data from our and other groups in Table 2 suggest that there are some inconsistencies in the response of target genes between tissues or cells, or even between the same tissue/cell. This is not surprising considering that several conditions can change the activity of PPAR isotypes, for example, the addition of insulin mentioned above. However, another important factor that might explain the different response between cell types or experiments is the abundance and activity of coregulators [132].
Some unexpected findings can be seen from data reported in Table 2. For instance, the well-established PPARγ target in nonruminants FABP4 [133] does not appear to be affected by activation of PPARγ in ruminants, at least in MAC-T cells [26] but was induced by activation of PPARα in MDBK cells [28]. In a study performed in intramuscular fat of growing beef steers, it was observed a very high correlation between the expression of FABP4 and PPARG suggesting a dependence of FABP4 expression from PPARγ [80]. Contrary to such observation, in a recent study in pregnant overfed versus normal fed energy dairy cows, no change in expression of FABP4 was observed but a greater expression of PPARG in subcutaneous adipose [134]. As for others, this unexpected finding in ruminant cells needs to be further confirmed; however, it underscores the limitation of using nonruminant data in the context of bovine.
Another cause of discrepancy might be due to methodological differences between studies, such as the methods used to perform qPCR. Most of the target genes reported in Table 2 were uncovered using qPCR. This technique relies on the identification and use of proper internal control genes [135], which is seldom conducted. As a result, some of the data generated by qPCR may lack accuracy prompting for a more routine application of all quality controls. In order to overcome several of the critical limitations often found in work reporting qPCR data, the minimum information for Publication of quantitative Real-Time PCR experiments (MIQE) [136] was created. Adherence to those guidelines will help standardize protocols, thus, enhancing data reliability. The use of such guidelines should be required by a greater number of scientific journals.
8. Effect of NEFA, Energy in the Diet and Fetal Reprogramming, on PPAR Isotypes
8.1. NEFA
The provision of LCFA to mammalian cells is from NEFA originating from adipose tissue lipolysis or from lipolysis of chylomicron or very low density lipoproteins (VLDL). The activation of bovine PPARα by NEFA was demonstrated recently in bovine aortic endothelial cells, where it was observed that PPARα activity was increased by release of free FA from VLDL via the action of lipoprotein lipase (LPL) [62]. In the same experiment it was demonstrated that ~10 μM of released NEFA in the media activated PPARα by ca. 80% compared to 10 μM of the specific PPARα agonist Wy-14643. A similar concentration of oleic acid alone activated bovine PPARα up to ca. 60% compared to Wy-14643. The activation of PPARα was due to free FA uptaken by the cells as demonstrated by the strong linear relationship between activation of PPARα and uptake of LCFA [62]. In addition, the activation of PPARα was proportionally inhibited by amount of albumin in the medium [62]. The results from the same study also indicated that the free FA released by the LPL, and not the circulating plasma FA (i.e., albumin-bounded NEFA), are the ones able to activate PPARα. The authors explained this by proposing that the high concentration of LCFA needed for PPARα activation can be achieved only by local release by lipase of LCFA from lipoproteins. Those results need to be further confirmed because of their important implications in the fine-tune activation of PPARs by dietary approaches.
The activation of PPAR by FA entering the cells via the unsaturable process is supported by the fact that endogenous activation of PPARα in vivo seems to occur mainly with high levels of LCFA that occur under fasting conditions in nonruminants [137]. In addition, we have shown in bovine cells that the expression of PPARα target genes is faster and more pronounced if cells are treated with free palmitate instead of palmitate bound to albumin [61].
The above-mentioned findings are relevant to dairy cattle soon after parturition when the hypoinsulinemia due to negative energy balance (NEB) reduces insulin sensitivity, and uncoupling of the growth hormone-insulin-like growth factor-1 axis results in substantial increase in NEFA, a mixture of LCFA whose composition can be partly altered through dietary approaches.
Evidence of increased activation and/or expression of PPARs due to the surge in NEFA has been reported in cattle. In particular, it has been observed that during the transition from pregnancy to lactation, characterized by a large surge of plasma NEFA, there is upregulation in expression of several PPAR target genes (e.g., CPT1A, ACOX1, see Table 2) in liver of dairy cattle, with a concomitant increase in expression of PPARA [57, 138, 139]; however, not all the studies found this to be a consistent response [140].
8.2. Nutrient Restriction
Nutrient restriction in dairy cows, causing a concomitant increase in blood NEFA, enhanced expression of PPARA and PPARD in liver [56] and protein expression of PPARγ in the hypothalamus [141]. Similarly, a 60-day period of body weight loss in beef cows was associated with greater expression of all three PPAR isotypes in biceps femoris muscle and several PPAR target genes, compared with cows that maintained body weight [142]. Overall, the data indicated that the NEB, with a consequent increase in NEFA, appears to induce expression and activation of all PPAR isotypes, but particularly of PPARA and PPARD.
8.3. High Dietary Energy
High dietary energy during pregnancy in dairy cows was associated with lower expression of liver PPARA early post-partum [143]. High dietary energy in weaned Angus steers, but not Angus × Simmental steers, was associated with lower expression of PPARD in Longissimus lumborum muscle [47].
8.4. Dietary Energy and Fetal Reprogramming
In ovine, nutrient restriction in ewes during early pregnancy (between 28 to 80 days gestation) increased expression of PPARA in the adipose tissue of the near-term fetus [144]. However, this was true only if the ewes were fed to requirements after this period of pregnancy; the adipose tissue of fetuses from ewes fed ad libitum from 80 days of pregnancy to term had lower PPARA expression [144]. The above data clearly indicate that level of energy in the diet of the mother has a strong effect on the fetal transcriptome, that is, fetal reprogramming.
The fetal reprogramming of PPAR due to dietary energy level also has been observed when animals were overfed energy during pregnancy, such that fetuses of those dams had greater expression of PPARG and other lipogenic genes [145]. In contrast, either control or a high-energy diet in the periconception period or during pregnancy did not affect expression of PPARG in perirenal, omental, or subcutaneous adipose tissue of 4-month-old lambs [146]. Interestingly, intrafetal administration of a PPARγ agonist, rosiglitazone, increased expression of LPL, a putative PPARγ target gene, in perirenal adipose tissue of sheep fetuses [81]. No effect was observed for PPARG itself. In contrast, in the same study rosiglitazone increased expression of PPARA in liver.
9. Biological Effects of PPAR Activation in Ruminants
Most of the biological roles of PPAR uncovered in monogastrics can likely be extrapolated to ruminants; however, before those roles can be considered established also in ruminants, experiments need to be performed. Due to the modest amount of research performed to date, the biological significance of PPAR isotypes in ruminants is not well established, but the studies so far conducted have confirmed the existence of conserved roles between monogastrics and ruminants. In this section we provide an overview of the biological roles suggested by most of the experiments on PPAR carried out in ruminants besides those mentioned above on bovine endothelial cells.
9.1. Control of Adipogenesis and Lipid Metabolism
9.1.1. PPARγ
As for nonruminants [21], PPARγ plays a pivotal role in adipogenesis in ovine and bovine [91, 147], and in dairy cows its expression is high in adipose tissue (Figure 1) and appears to control lipogenesis by acutely responding to energy level in the diet [82, 134, 148, 149]. The importance of PPARγ in adipogenesis has been highlighted also by the identification of this as one of the candidate genes related to bovine marbling [150]. Besides lipogenesis, PPARγ might also play a role in LCFA oxidation as recently observed in lamb pulmonary arterial endothelial cells [85]. In that study it was demonstrated that PPARγ controls the expression of carnitine palmitoyltransferase 2 (CPT2) and carnitine O-acetyltransferase (CRAT), both genes involved in the entry of LCFA into the mitochondria, while it controls the translation of CPT1A but not its expression [85].
9.1.2. PPARα
The activation of goat PPARα in vivo increased fatty acid oxidation in liver [108]. The oral administration of Wy-14643 increased palmitate oxidation in liver of dairy calves with a concomitant increase in expression of several genes known to be PPARα targets (see Table 2) involved in FA oxidation in nonruminants [78]. Therefore, it is apparent that the activation of PPARα in ruminants controls catabolism of fatty acids. Other pieces of evidence supporting that conclusion include the fact that FA catabolism in mitochondria and peroxisome increases during the transition from pregnancy into lactation [151]. This appears to be consequence of the large surge of NEFA and the concomitant increase in expression of few key genes rather than an increase of overall pathway flux [152]. However, the expression of PPARA in liver of dairy cattle increases from pregnancy to early post-partum [57, 138]. In the same time, several PPARα target genes involved in lipid metabolism have a similar increase in expression as PPARA in liver during the transition from pregnancy to lactation; those include ACOX1 and acyl-coenzyme A dehydrogenase, medium chain (ACADM) [57, 138]. Finally, the use of Wy-14643 in MDBK cells increased expression of several genes involved in lipid catabolism [28, 61] (Supplementary Table 1). One of those key genes is the well-known PPARα target CPT1A [57, 138].
9.1.3. PPARβ/δ
Compared with PPARα and PPARγ, the role on lipid metabolism of PPARβ/δ activation in ruminants is less clear. The PPARβ/δ was shown to have a role in adipogenesis in sheep because its activation increased activity of GAPDH [91]. An involvement of PPARβ/δ in adipogenesis also was reported by several experiments performed in monogastrics [2]. However, a contrasting role of PPARγ and PPARβ/δ was observed in primary bovine mammary cells, where several PPARγ ligands reduced the expression of PPARβ/δ [69]. PPARα unarguably has a primary role in controlling fatty acid oxidation in rodents; however, PPARβ/δ also controls fatty acid oxidation in skeletal muscle, heart, and brown and white adipose tissue [2]. Several data indirectly suggest a similar role in ruminants. It was observed that during nutrient restriction [56] and during body weight loss in muscle of beef cows [142], both situations that enhance LCFA oxidation, there was a concomitant increase in expression of PPARA and PPARD.
In summary, the pivotal role of PPARγ in controlling adipogenesis and lipogenesis in adipose tissue, which was clearly established in nonruminants, can also be considered established in ruminants. The control of fatty acid oxidation by PPARα in ruminants appears supported by the data published to date. The few data available also suggest a role for PPARβ/δ in lipid catabolism in ruminants.
9.2. Control of Milk Fat Synthesis by PPARγ in Dairy Cattle
Milk fat synthesis in dairy cows appears to be controlled at least in part by PPARγ. This was originally suggested by the increase in expression of PPARG in mammary gland of dairy cows between pregnancy and lactation [33]. In the same study, a large increase in expression of a network of genes potentially involved in milk fat synthesis and for the most part putative PPARγ target genes was observed. Based, on those data we then tested, and demonstrated, the hypothesis that PPARγ controls expression of key genes involved in milk fat synthesis, including SREBF1 [26].
A pivotal role of milk fat synthesis regulation by SREBP1 has been originally proposed based on the consistent reduction of SREBF1 expression by t10,c12-CLA, a minor unsaturated FA produced during ruminal biohydrogenation of long-chain polyunsaturated FA [153]. The activity of SREBP1 is largely due to its abundance, which is controlled by the transcription and posttranscriptional regulation, and abundance and activation of the cofactors SREBP cleavage-activating protein (SCAP) and insulin induced gene 1 and 2 (INSIG1 and INSIG2) [2, 33]. The INSIGs protein blocks SREBP1 activity when the level of oxysterol is high (see references in [33]). The reduced activity of SREBP1 by t10,c12-CLA is also controlled at the posttranslational level [2], but in this regard it is interesting that t10,c12-CLA consistently decreases the expression of SREBF1. Considering the unidirectional response of SREBP1 to t10,c12-CLA (i.e., inhibition of milk fat synthesis), and the inability of this TF to bind and be activated by other LCFA, it appears obvious that other TF must be involved in the positive response of milk fat synthesis to LCFA. Hence, it is remarkable that the activation of PPARγ by rosiglitazone in MAC-T cells was accompanied by a significant increase in expression of SREBF1, demonstrating that SREBF1 is a PPARγ target gene in ruminants [26]. Our overall data [26, 33] suggest a concerted action of SREBP1 and PPARγ in controlling milk fat synthesis but underscore a more fundamental role of PPARγ, the only one among the two that is able to be activated by LCFA.
The evidence supporting a role of PPARγ in controlling milk fat synthesis has recently been dismissed [153] using three different arguments; here we briefly outline those arguments and present the counterarguments.
The ca. 2-fold increase in expression of PPARG in bovine mammary gland from pregnancy to lactation [33] was interpreted as “related to differentiation and the initiation of milk synthesis rather than the regulation of milk fat synthesis during established lactation” [153]. The PPARγ is known to be involved in differentiation, but almost exclusively of the adipose tissue where it plays an essential role [21, 154]. For the rest, it is known that PPARγ has a negligible role in the differentiation of epidermis, one among several epithelial tissues [155]; however, a role for this PPAR isotype in differentiation of sebaceous gland after skin injury has been reported [15]. Although a role for PPARγ in the differentiation of mammary gland cells cannot be fully discarded, it has not yet been reported.
The authors based their conclusions on the fact that CLA are activators of PPARγ in monogastrics, de facto disregarding the findings showing that ruminant PPARγ does not seem to be activated by CLA, especially in mammary epithelial cells [26] (see Table 1).
The most critical misinterpretation dealt with the observed increase in expression of genes related to milk fat synthesis in MAC-T cells after treatment with the PPARγ agonist rosiglitazone [26]. The data clearly pointed to an active role of PPARγ in controlling milk fat synthesis. The authors, using the above argument about activation of PPARγ by CLA, interpreted those data exclusively from a milk fat depression angle; that is, activation of PPARγ by CLA should be responsible for depressing milk fat synthesis. That was neither what the data suggested nor our conclusions [26].
In an in vivo experiment the activation of PPARγ prepartum by TZD affected adipose tissue post-partum but, apparently in contrast to the above data, decreased milk fat production [109]. This result is not completely surprising considering that the TZD treatment was provided pre-partum when there is a large abundance of PPARγ in adipose tissue and a low abundance in mammary gland [33], whereas, when PPARγ is expected to increase in mammary gland due to the onset of lactation [33], the TZD was no longer supplemented and the amount of NEFA, which could have played a role in activating PPARγ, was decreased in cows treated with TZD [109]. In addition, the adipose tissue competes with mammary gland for lipogenic substrates, especially if the insulin sensitivity is high, as demonstrated by the reduced milk fat by injection of insulin in cows [156]. From this point of view it would be interesting to test the effect of TZD injection post-partum on milk fat synthesis in dairy cows.
Besides PPARγ and SREBP1, data from another laboratory suggested that LXR also plays a role in controlling de novo FA synthesis [157]. It is recognized that in order to demonstrate the central role of PPARγ, SREBP1, LXR, or their combination in controlling milk fat synthesis in dairy cows, there is need for more fundamental studies, for instance, via gene-specific knock-outs. Recently, two studies from the same laboratories [158, 159] used siRNA specific for SREBF1 in order to define the role on controlling milk fat synthesis of this transcription factor. From the studies it was shown that basal transcription of genes involved in de novo FA synthesis in bovine mammary epithelium is partly under control of SREBP1. Some of the same genes were induced when LXR was activated using a specific agonist. Studies using siRNA specific for PPARG in bovine mammary cells are lacking. In the context of milk fat synthesis regulation, we deem more relevant the unbiased discovery of the role of LCFA in affecting the transcriptome by binding specific TF than demonstrating a more crucial role of one or another TF.
9.2.1. Is PPARγ Crucial for Milk Fat Synthesis Also in Mouse?
Contrary to dairy cows [33], in mouse the mammary PPARG expression decreased between pregnancy to lactation [160], also after accounting for the large disappearance of adipose tissue [161]. In porcine mammary gland, the PPARG was not affected by lactation [162]. The expression of PPARG in mouse and pig mammary gland suggests that PPARγ likely does not control milk fat synthesis in monogastrics. In order to further study the role of PPARγ on milk fat synthesis in monogastrics, we have performed an in vitro experiment in mouse mammary epithelial cells (HC11; Figure 3). The experiment also was performed with the purpose of comparing the data previously generated with bovine mammary cells [26]. For this reason, the experiment was performed in HC11 with the same experimental design as the one previously performed in MAC-T cells [26]. Most of the treatments in HC11 were the same as in MAC-T cells with the exception of the PPARγ inhibitor GW9662.
Figure 3.
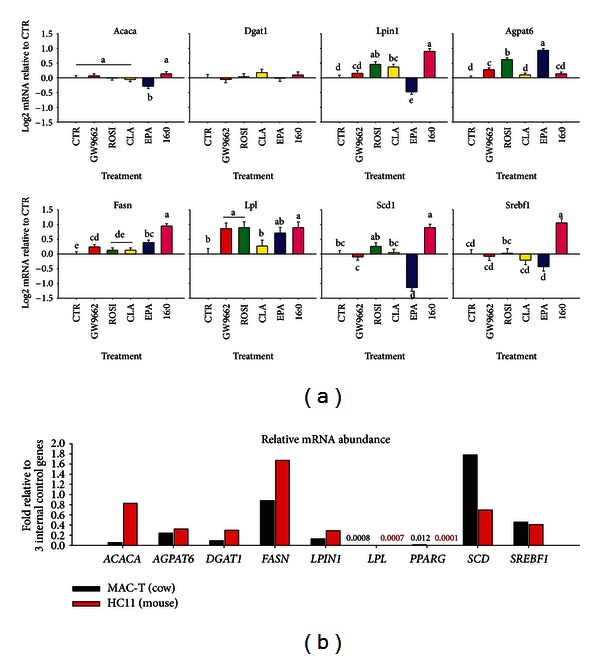
Effect of PPARγ activation on genes coding for proteins involved in milk fat synthesis in mouse mammary epithelial cells HC11. The experiment was performed with the purpose to test the effects of 50 μM of the PPARγ activator rosiglitazone, the PPARγ inhibitor GW9662, or 100 μM of several long-chain fatty acids (trans-10,cis 12-conjugated linoleic acid (CLA), eicosapentaenoic acid (EPA), or palmitate (16:0)) for 12 hours in HC11 cells and compare the data with results using the same experimental design (except the GW9662 treatment) in MAC-T cells [26]. All the procedures with few modifications were as previously described [26]. The RNA was extracted and qPCR performed for several genes known to be involved in milk fat synthesis and significantly upregulated by rosiglitazone in MAC-T cells and the same 3 internal control genes used [26]. In (a), the effect of treatments on HC11 cell is reported. For that experiment, the qPCR data were calculated as fold change relative to control and log2 transformed prior statistical analysis using Proc GLM of SAS with treatment as main effect and replicate as random. Dissimilar letters denote significant differences between treatments (P < 0.05). In (b), a comparison in mRNA abundance between measured genes in the control group of HC11 and MAC-T cells is presented. The relative mRNA abundance was calculated as previously described [26] but as fold difference relative to the geometric mean of the median Ct values of the 3 internal control genes instead as % relative abundance. The same analysis was performed for the MAC-T cells using data previously published [26]. The PPARG was detectable only for few samples in HC11 cells and LPL was barely detectable in both HC11 and MAC-T cells.
As observed in MAC-T cells, the saturated LCFA palmitate increased expression of several lipogenic genes in HC11 but, differently than in MAC-T cells [26], the effect appeared to be PPARγ-independent due to the extremely low expression and activity of PPARγ (Figure 3(a)). Those findings are intriguing because, together with the greater abundance of PPARA compared with PPARG in MAC-T cells (Figure 1(b)), suggests that the observed increase in mammary lipogenic genes due to palmitate are via PPARα or other TF rather than PPARγ in immortalized mammary cells from cattle and mouse.
Contrary to what was observed in MAC-T cells [26] and in vivo in mouse mammary gland [163], the t10,c12-CLA failed to inhibit the expression of lipogenic genes in HC11 (Figure 3(a)). This observation is surprising considering that the Srebp1 expression is relatively high and with similar level in HC11 compared with MAC-T cells (Figure 3(b)). Only EPA decreased expression of few lipogenic genes in HC11; among those the SCD was downregulated by EPA also in MAC-T cells [26]. The relative abundance of genes measured in HC11 compared to MAC-T cells (Figure 3(b)) revealed that lipogenic gene expression is overall greater in HC11 than MAC-T, with exception of SCD that is more abundant in MAC-T cells. The PPARG had low expression in both cell lines but was virtually absent in HC11, while clearly detectable in MAC-T cells. This observation likely accounted for the fact that the PPARγ agonist rosiglitazone and the inhibitor GW9662 had little effect on the expression of most genes in HC11 (Figure 3(a)). On the contrary, rosiglitazone increased the expression of all those genes in MAC-T cells [26].
The virtual absence of Pparg expression in HC11 (Figure 3(b)) together with the lack of decrease in expression of milk fat-related genes by CLA despite the large expression of SREBF1 seems to indicate a role of PPARγ, and more likely PPARγ-SREBP1 crosstalk, in translating the lipogenic inhibition, and particularly milk fat depression effect, of CLA (and likely EPA) usually observed in vivo. However, the data also point to a more complex nutrigenomics response to LCFA, likely involving additional TF besides SREBP1 and PPARγ.
Overall, the comparison between the mouse and the bovine mammary epithelial cell lines, with all the limitations of in vitro experiments, highlights a crucial difference between rodents and bovine in the genomic control of milk fat synthesis. The data clearly uncovered no roles for PPARγ in controlling milk fat synthesis in mouse. Those observations suggest caution when inferring physiological responses using data from a different species.
9.3. Control of Inflammatory Response
The activation of PPARγ, PPARα, and PPARβ/δ has anti-inflammatory effects in nonruminants [19, 164] and some data are available in ruminants suggesting a similar effect. The first demonstration that PPARγ might play an anti-inflammatory role in ruminants was carried out by a Japanese group by injecting for 9 days human recombinant TNFα plus TZD in dairy steers. They observed that the TZD treatment partially reversed the insulin resistance caused by TNFα [107]. The TZD effect was probably due to enhanced insulin signaling through PPARγ activation by also counteracting the effect of TNFα [165]. The anti-inflammatory effect of PPARγ in ruminants is elicited not only by counteracting the effect of TNFα, but also by reducing the production of this cytokine. This was demonstrated recently when treatment of bovine peripheral blood mononuclear cells with 100 μM of t10,c12-CLA or 10 μM of rosiglitazone attenuated the production of TNFα in vitro, with a stronger effect observed in cells treated with rosiglitazone [166].
In bovine primary mammary epithelial cells (bMEC), the activation of PPARγ by several agonists caused downregulation of several proinflammatory cytokines and increased expression of the chemokine CCL2 and TNFα [69]. In contrast, PGJ2 enhanced markedly the expression of both interleukin 8 (IL8) and chemokine (C-X-C motif) ligand 6 (CXCL6) and had no effect on other cytokines [69]. The same study also demonstrated that the generation of proinflammatory mediators in bMEC treated with lipopolysaccharide (LPS) can be modulated by synthetic PPARγ agonists. These findings support a role of PPARγ in mastitis resistance in dairy cows.
Some additional evidences support an anti-inflammatory role of PPAR in ruminants. The activation of PPARα has shown to limit leukocyte adhesion to the bovine endothelium [167]. The expression of PPARG is reduced by intramammary infection with Escherichia coli [168] and PPAR signaling was evidently inhibited by intramammary infection with Streptococcus uberis [169]. The PPARG and PPARA were also markedly downregulated in PMN soon after an inflammatory challenge; however, the expression of PPARD increased markedly and was substantially more abundant than the other isotypes (Moyes et al. unpublished data). In contrast, the expression of PPARA and PPARG in liver was not affected after intramammary treatment with Escherichia coli that induced a strong hepatic acute-phase reaction [170]; however, the most-impacted biological effect of the treatment was the reduction of lipid metabolism in the liver, particularly steroid synthesis and PPAR signaling [171]. The involvement of PPARβ/δ in the process of inflammation was recently underscored when an intramammary infusion of LPS led to marked upregulation of PPARD and several proinflammatory genes in liver of dairy cows (e.g., TNF, NFKB1) [172].
The potential role of PPAR isotypes on inflammation can also be inferred by the fact that the expression of the PPARα agonist ANGPTL4 (Table 2) increases markedly in response to inflammation not only in mouse liver [173] but also in bovine liver [172], and it has been proposed to serve as a positive acute phase protein (+APP) [173]. In that context, it is interesting that the expression of ANGPTL4 in adipose tissue increases markedly after parturition [134, 174], when the animals experience inflammatory-like conditions [175, 176]. Whether the upregulation of ANGPTL4 in adipose tissue after parturition denotes a response of the tissue to an inflammatory state remains to be determined; however, there is evidence of activation of immune-related pathways in adipose tissue soon after parturition [177].
9.4. Control of Intertissue Metabolic Adaptations during Changes in Nutritional Status and Physiological State
In monogastrics, the PPARα targets angiopoietin-like 4 (ANGPTL4) [178] and fibroblast growth factor 21 (FGF21) [179, 180] have been identified as extra-hepatic signals (hepatokines) that play an important role in the coordination of tissue adaptations to fasting, undernutrition, and the transition into lactation in bovine [56, 95, 174]. Although direct proof of bovine PPARα activation as the trigger for the marked upregulation of liver FGF21 after parturition [86, 95] is not available, the fact that the upregulation of FGF21 was observed in animals with greater NEFA [86] is suggestive of FGF21 as a PPARα target in bovine. The link between PPARα activation and ANGPTL4 was previously discussed with data from cows suffering from undernutrition-driven ketosis [56] and was partly confirmed in vitro [28]. However, it was recently observed that hepatic ANGPTL4 and PPARD (not PPARA) expression was upregulated during acute inflammation suggesting that in bovine this PPAR isotype also may regulate expression of the hepatokine [172]. Specific molecular work would need to be carried out to clarify the validity of the observed relationship in terms of a functional link.
9.5. Other Roles
The use of PPARγ agonists decreases protein synthesis, but as demonstrated in bovine aortic endothelial cells, the mechanism appears to be independent of PPARγ [181]. As with nonruminants, the activation of PPARγ improves insulin sensitivity in dairy cows [82]. The activation of PPARα in the liver might also increase gluconeogenesis. This was inferred by the impaired gluconeogenesis in PPARα-null mice [182]; however, none of the main enzymes involved in gluconeogenesis are known to be PPARα targets in nonruminants [182]. One of the three known promoter regions of bovine pyruvate carboxylase (PC), a key enzyme in gluconeogenesis, was activated by Wy-14643 when transfected as a construct with firefly luciferase into rat hepatoma cells, indicating a potential control of expression of this enzyme by PPARα in ruminants [93]. However, the PC expression was not induced in MDBK cells treated with Wy-14643 or single LCFA [28]. The expression of PC was instead induced by cocktails of LCFA and particularly the concentration mimicking NEFA composition in dairy cows around parturition [183]. Therefore, an increase in gluconeogenesis via the activation of PPARα in ruminants still needs to be fully proven.
It has been demonstrated that the high-glucose-induced downregulation of the glucose transport system in bovine endothelial cells is mediated by PPARβ/δ [68]. It was shown that activation of PPARβ/δ inhibits the expression of the solute carrier family 2 member 1 (or facilitated glucose transporter GLUT1) coupled with an increase in expression of calreticulin, a protein that increases degradation of GLUT1 mRNA. The condition tested in the study (i.e., high glucose) has probably little implication for ruminants, considering the low level of circulating glucose compared with nonruminants (<4 mM in dairy cows [176] versus ca. 5 mM in human and >6 mM in mouse [184]). However, the control of glucose transport by PPARβ/δ could have implications in milk synthesis, considering that GLUT1 is one of the most important glucose transporter and its expression increases drastically during lactation in mammary tissue of dairy cows [185]. Thus, this PPAR isotype could play a pivotal role in provision of glucose for lactose synthesis. Interestingly, in mammary gland during lactation, PPARD is significantly downregulated [186] concomitant with an increase in expression of several glucose transporters, including GLUT1 [70, 185]. If the suggested link is real, this offers the opportunity of using PPARβ/δ antagonists in order to improve milk production.
More recently, it was demonstrated that PPARD transcript in rumen epithelium of neonatal dairy calves is substantially more abundant than PPARA (see also Figure 1(b)), and its expression increased markedly from the milk-fed stage to the roughage-fed (i.e., high-structural fiber) stage at ~10 weeks of age [64]. The increase correlated with greater mass of the rumen, which suggested a potential link between PPARβ/δ and mechanisms driving ruminal epithelial cell development and proliferation [64].
10. What Controls Abundance of PPAR in Tissues?
The sensitivity of various tissues to PPAR isotype-specific agonists is closely related with the abundance of the specific isotype and other essential factors such as the abundance of coactivators or corepressors, LCFA, and hormones [76, 187–189]. As for nonruminants, the abundance of various isotypes in tissues appears to be directly related with the specific function they perform; for example, PPARγ abundance is relatively high in lipogenic tissues while PPARα is relatively high in tissues with elevated FA catabolic capacity (see Figure 1(a)). Besides tissue-specific distribution, other factors can control the abundance of PPAR isotypes in tissues.
Among factors controlling PPAR isotypes expression in ruminants (Supplementary Table 2), it is evident that several lipid molecules, some nutritionally relevant such as LCFA and retinoids, and propionate (likely indirectly via glucose and insulin) can affect expression of PPAR isotypes, with a different sensitivity based on tissue type. The expression of ruminant PPAR isotypes is also affected by physiological status, level of energy in the diet, mechanical cues (e.g., laminar flow, mechanical load), oxygen and peroxide levels, hormones, and other growth factors (Supplementary Table 2). In addition, data from several groups also suggest that the activation of PPARγ increases expression of its own gene and, in the case of sheep, also the expression of PPARA (Supplementary Table 2). Interestingly, in bovine mammary epithelial cells several PPARγ agonists decreased the expression of PPARD, with one case (ciglitazone) in which PPARG also was downregulated [69].
Overall the data presented in Supplementary Table 2 suggest that it is possible to increase or decrease the abundance, hence the sensitivity, of PPAR isotypes in ruminant tissues. Among the factors affecting the PPAR isotype expression, the more interesting from a nutrigenomics point of view are the LCFA and the level of dietary energy because they can be easily manipulated.
11. PPAR Isotype Activation during the Peripartal Period in Dairy Cattle: A Hypothesis
11.1. The Peripartal Condition
The transition from pregnancy into lactation (also called simply “transition period”) is one of the most stressful stages of the life of dairy cattle [190]. Physiologically, the transition period is a complex phenomenon intertwining various metabolic activities (e.g., lipid, glucose, protein) and functions (e.g., inflammatory response) of several organs and tissues (e.g., adipose tissue, mammary, liver, uterus, and immune system) [152, 190]. A key feature of the transition period from a metabolic and health standpoint is the increase in plasma of NEFA and ketone bodies (KB), both of which can be toxic above certain thresholds, and by a general decrease in both insulin sensitivity (except for the mammary gland) and blood insulin concentration [191]. The transition period is also characterized by inflammatory-like conditions as consequence of the release of proinflammatory cytokines, which along with NEFA affects directly liver functionality leading to poor performance [192].
The metabolic load placed on the liver of periparturient cows is exacerbated by this inflammatory-like conditions and also by the decrease in feed intake and the ensuing NEB, which often occurs as early as 10 days prior to parturition (reviewed in [193]). All of the above increase the risk of dairy cattle for developing metabolic disorders such as fatty liver [194] and ketosis [195, 196], but more importantly these disorders are tightly connected with other typical peripartal diseases [197]. Therefore, a smooth transition period is an important target in order to optimize performance and overall welfare of dairy cows. Interestingly, most of the above-described conditions (e.g., high NEFA, insulin insensitivity, fatty liver, inflammatory-like conditions) with the exception of the NEB are common to the metabolic syndrome that afflicts human [198].
11.2. PPAR Isotype Activation to Help Transition Dairy Cattle
It has been proposed previously that the PPAR isotypes are ideal targets for the prevention and cure of the metabolic syndrome in humans [199]. The use of PPARγ agonists is a clinical approach currently in practice to treat insulin resistance, one of the main problems related with the metabolic syndrome [22, 200]. Similarly, it was proposed earlier that PPAR isotypes play a pivotal role in the physiological adaptation of dairy cattle to the transition period [36, 201]. It was proposed that fine-tuning the activity of PPARα and PPARγ, in particular, by nutritional approaches at specific time/s during the transition period might be a way to prevent and/or help the cows overcome metabolic disorders. Among nutritional approaches in order to affect PPARs, the saturated LCFA appear to be the most promising based on in vitro data (see above and [28]). The effects of saturated LCFA on PPARs activation and the consequent improvement of lipid metabolism appear to be supported by recent in vivo data [202]. In that study it was observed that the adaptations in lipid metabolism in dairy cows fed high-saturated fat compared with a low-fat control diet or a high-linseed diet (high in unsaturated LCFA) for up to 5 weeks pre-partum was better.
In Figure 4 a qualitative hypothetical model describing the potential role of PPAR isotypes in transition dairy cows is depicted. That model rests on the well-established fact that the liver, adipose, rumen, skeletal muscle, immune system, and mammary gland play a crucial role in the adaptations leading to the onset of lactation. Other organs such as uterus, kidney, and pancreas also are crucial in this context but less is known about their molecular adaptations to lactation. In particular, data partly reviewed above strongly support a pivotal role of PPAR isotypes in the regulation of fertility and pregnancy; however, the overall effect of PPAR isotypes activation on fertility is not fully clear. In addition, the PPAR isotypes likely play a more important role before pregnancy compared with early lactation, when the cows are not yet cycling. Once the role of PPAR isotypes is better defined for the reproductive organs, it can become an important component of the overall model proposed.
Figure 4.
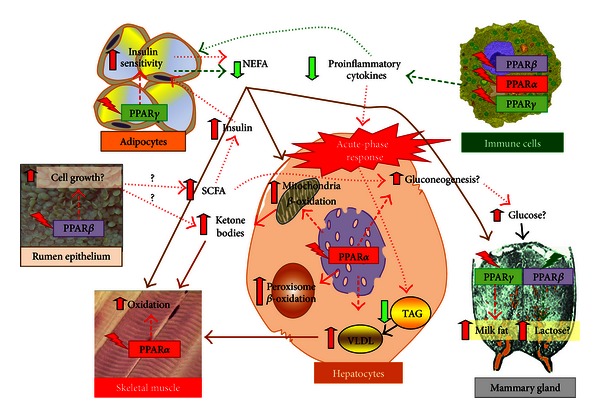
Improving transition from pregnancy into lactation in high producing dairy cows by nutrigenomics approach through PPAR isotypes: a hypothesis. The liver buffer cells from the excessive concentration of circulating nonesterified fatty acids (NEFA) by both catabolizing long-chain fatty acids (LCFA) with production of ketone bodies (KB) and esterifying them as triacylglycerol (TAG). The TAG are then accumulated in lipid droplets and packed into VLDL for release into the bloodstream. The liver is also induced by proinflammatory cytokines to produce positive acute phase proteins (+APP) taking away hepatic resources for normal liver functions. Despite the decrease in peripheral insulin concentration postpartum, the activation of PPARγ prior to parturition can decrease NEFA postpartum through greater insulin sensitivity primarily on the adipose tissue. The activation of PPARβ/δ (PPARβ in the figure) via LCFA can increase rumen epithelium growth with consequent larger production of short-chain fatty acids (SCFA) including propionate, which stimulate insulin production, and butyrate, augmenting the KB in blood. The increased activation of PPARα just before parturition and during the first 14 days postpartum in the liver and muscle can increase NEFA oxidation with greater proportion of KB produced per amount of NEFA uptake. The activation of PPARα in the liver has the potential to increase gluconeogenesis and VLDL synthesis. The KB can serve as fuels by skeletal muscle instead of NEFA and glucose; both molecules are substrates for mammary gland. In this tissue, the activation of PPARγ postpartum should increase or maintain milk fat. In addition, the inhibition of PPARβ/δ postpartum can potentially increase glucose import with a consequent increase in lactose synthesis, and hence, milk yield. The activation of PPAR isotypes just prior to parturition and during the first two weeks post-partum should diminish the inflammatory-like conditions preventing, on one hand, the stimulation of NEFA release and, on the other hand, hepatic acute-phase reaction, both determined by proinflammatory cytokines. This coordinated set of reactions should provide an ideal metabolic situation leading to a smoother transition from pregnancy into lactation, that is, allow the liver to allocate its resources for “normal” functions. As a consequence of this, the incidence of diseases typical of the peripartal period would be reduced, and hence, cows with higher performance and more healthy. Regular dashed arrows represent “effect on” due to PPAR isotype activation/inhibition, and round dot arrows denote secondary (or indirect) effects of PPAR isotype activation. In both cases red = activation or increase and green = inhibition or decrease.
Dairy cattle during the transition from pregnancy into lactation experience a multitiered set of adaptations aimed at allowing the mammary gland to begin and maintain lactogenesis. From a physiological perspective, the inherently low capacity of animals to consume enough dietary energy and the detrimental inflammatory-like conditions due to release of proinflammatory cytokines lead to the marked release of LCFA into the bloodstream from the adipose tissue. Those LCFA are mostly metabolized by the liver. A greater level of dietary energy in the form of nonstructural carbohydrate provided to the animal early postpartum can partly alleviate the negative shortfall in energy status; such approach would enhance production of short-chain fatty acids (SCFA), of which propionate metabolism via gluconeogenesis could serve as a trigger for greater insulin secretion [193]. The latter has been shown to promote rumen epithelial cell proliferation and might work in concert with PPARs to coordinate metabolism and development of these cells [64]. During the peripartal period, proinflammatory cytokines are released and induce the liver to produce +APP [176], taking away hepatic resources for normal liver functions (e.g., glucose synthesis, lipid metabolism, and ureagenesis) [175, 176, 197]. This condition effectively exacerbates the tissue's capacity to coordinate appropriately metabolism of lipid and to provide the required glucose to mammary gland for milk synthesis. The marked NEFA concentration is only partly oxidized by liver with the rest accumulating as TAG. The TAG are then packed into VLDL for release into the bloodstream, but at a lower rate relative to monogastrics [203]. An excessive accumulation of TAG can have detrimental effects on liver function [194].
We propose that the increased abundance pre-partum of PPAR isotypes and the timely and isotype-specific activation pre- or post-partum might be beneficial in preparing and allowing the animal to face the above-described conditions favoring a smooth transition into lactation. In particular the following:
the greater abundance and activation of PPARγ prepartum in adipose tissue can prevent the large NEFA surge due partly to an increase in insulin sensitivity, leading to reduced lipid overload on the liver with a consequent reduction of fatty liver, ketone body production, and any potential satiety effects (as consequence of high FA oxidation) [204]. The activation of PPARγ postpartum in mammary gland can allow to increase or to maintain the amount of milk fat in the early stages of lactation when NEFA provide exogenous LCFA for the mammary gland. Several pieces of evidence support such expected effects in adipose tissue [82, 109] and mammary tissue [26, 33, 186];
the greater abundance and activation of PPARα in liver and skeletal muscle in postpartum relative to prepartum can increase oxidation of NEFA leading to a lower accumulation of lipid in the liver. The greater oxidation capacity of liver (i.e., increase ketone body synthesis per unit of NEFA oxidized) would help prevent any substantial alteration in the production of ketone bodies due to the systemic decrease of NEFA as a consequence of PPARγ activation. The activation of PPARα in liver might also increase gluconeogenesis rate, an essential process in ruminants particularly for milk synthesis. Another expected response would be increased VLDL synthesis and secretion by preventing the negative effect of the acute-phase reaction as a consequence of inflammatory-like conditions on apolipoproteins and other molecules involved in VLDL synthesis and TAG export. This suggestion is based on several pieces of evidence such as the observed negative association between apolipoprotein B100 or other VLDL components with inflammatory-like conditions in ruminants [170, 175, 176, 194, 205, 206];
the activation of PPARα, PPARγ, and particularly PPARβ/δ in immune (e.g., neutrophils, macrophages) and endothelial cells might contribute to a reduction of the NEFA surge induced by proinflammatory cytokines [207] and also increase insulin sensitivity and prevent the negative effect of acute phase reaction on liver functionality [166, 176].
The hypothetical model for fine-tuning PPAR isotypes for prevention of metabolic disorders in transition dairy cows we propose (Figure 4) is indirectly supported by several in vivo and in vitro studies, but a number of major details remain to be understood. One of the most important pertains to the effects of LCFA on PPAR isotype activation and, particularly, on how they could be used to target activation of a particular PPAR isotype at a particular stage of the transition period. More detailed and mechanistic studies with LCFA, for example, effective dose/s of individual LCFA or mixtures, are essential in order for these nutrients to have practical application as proposed in our model (Figure 4).
12. Conclusions and Perspectives
The understanding of physiological roles of PPAR isotypes in ruminants has advanced incrementally over the last decade. There is enough direct and indirect evidence compiled to conclude that these NR are biologically relevant in this species. The data suggest that the harmonized activity of PPAR isotypes across tissues is one facet of the multitiered set of control points that evolved to coordinate metabolism and physiological responses to endogenous and exogenous ligands. The transition from pregnancy to lactation provides the clearest example of the need for control points to ensure the nourishment of the neonate offspring, while ensuring the fitness of the dam. At a fundamental level, the functional activity of PPARs during this physiological state provides an elegant example of the multitiered concept because it links biological molecules with cellular responses that encompass several tissues. The model proposed based on the most-current knowledge is quite complex and its full evaluation obviously requires an integrative systems approach, that is, several tissues at various levels (e.g., cells and the underlying molecular networks) need to be studied simultaneously considering their dynamic adaptation.
If the model/hypotheses proposed hold, it would become the first “true” nutrigenomics application in dairy cattle biosciences. Benefits would go beyond simply establishing the physiological role of PPAR isotypes in ruminants. Improving the transition from pregnancy into lactation means to provide benefits for farmers, dairy cattle, and the society as a whole. We envisage farmers modulating the LCFA in the diets of dairy cattle to fine-tune metabolism through PPAR isotypes. Today, the continuous development of high-throughput technologies and bioinformatics tools permits the study of complex phenomena as is the case of the transition from pregnancy to lactation in dairy cattle [152]. This is an exciting era for expanding scientific knowledge and, apparently, the proper one for nutrigenomics.
Supplementary Material
Supplementary Table 1: Summary of the studies where activation of PPAR isotypes was performed in ruminants using synthetic agonists or other known natural ligands (e.g., 15-deoxy-Δ12,14-prostaglandin J2 for PPARγ). The studies are sorted by year of publication.
Supplementary Table 2: Factors affecting the expression of PPAR isotype genes in various ruminant tissues/cells.
Acknowledgments
The mouse mammary epithelial cell line HC11 and protocols for cultivation and differentiation (i.e., induction into lactation [208, 209]) were gently provided by Dr. Daniel G. Peterson (Animal Science Department, California Polytechnic State University). The comments from Dr. Afshin Hosseini were also helpful in completing the final version of the paper. The authors thank the three anonymous reviewers for their suggestions that greatly helped to improve the paper.
Abbreviations
- +APP:
Positive acute phase proteins
- ACOX1:
Acyl-coenzyme A oxidase 1, palmitoyl
- AF-1:
Activation Function 1 or ligand-independent activation function
- ANGPTL4:
Angiopoietin-like 4
- bMEC:
Bovine primary mammary epithelial cells
- CARLA:
Coactivator-dependent receptor ligand assay
- CCL2:
Chemokine (C-C motif) ligand 2
- CLA:
Conjugated linoleic acid
- CPT1A:
Carnitine palmitoyltransferase 1A (liver)
- CPT2:
Carnitine palmitoyltransferase 2
- CRAT:
Carnitine O-acetyltransferase
- CXCL6:
Chemokine (C-X-C motif) ligand 6
- EPA:
Eicosapentaenoic acid
- FA:
Fatty acid(s)
- FABP:
Fatty acid binding protein
- FGF21:
Fibroblast growth factor 21
- GAPDH:
Glyceraldehyde-3-phosphate dehydrogenase
- GLUT1:
Glucose transporter 1
- IL-8:
Interleukin 8
- INSIG1:
Insulin induced genes 1
- INSIG2:
Insulin induced genes 2
- KB:
Ketone bodies
- LBD:
Ligand binding domain
- LCFA:
Long-chain fatty acid(s)
- LCFA-CoA:
LCFA-coenzyme A (i.e., activated LCFA)
- LDL:
Low density lipoprotein(s)
- LPIN1:
LiPIN 1 (coding for a phosphatidate phosphatase)
- LPL:
Lipoprotein lipase
- LPS:
Lipopolysaccharide
- LXR:
Liver X receptor
- MAC-T:
Bovine mammary alveolar cells transfected with simian virus-40 (SV-40) large T-antigen
- MDBK:
Madin-Darby bovine kidney cells
- MIQE:
Minimum Information for Publication of Quantitative Real-Time PCR Experiments
- NEB:
Negative energy balance
- NEFA:
Nonesterified fatty acid(s)
- NFKB1:
Nuclear factor of kappa light polypeptide gene enhancer in B-cells 1
- NR:
Nuclear receptor(s)
- PC:
Pyruvate carboxylase
- PG:
Prostaglandin(s)
- PGJ2:
15-Deoxy-delta-12,14-prostaglandin J2
- PMN:
Polymorphonuclear cells
- PPAR:
Peroxisome proliferator-activated receptor
- PPRE:
PPAR response element
- PUFA:
Polyunsaturated fatty acid(s)
- qPCR:
Quantitative Real-Time reverse transcription polymerase chain reaction
- RXR:
Retinol X receptor
- SCAP:
SREBP cleavage-activating protein
- SCD:
Stearoyl-CoA desaturase
- SCFA:
Short-chain fatty acid(s)
- siRNA:
Short interference RNA
- SREBF1:
Sterol regulatory element-binding transcription factor 1
- TAG:
Triacylglycerol(s)
- TF:
Transcription factor(s)
- TNF:
Tumor necrosis factor(s)
- TZD:
Thiazolidinedione
- VEGF:
Vascular endothelial growth factor
- VLDL:
Very low density lipoprotein(s)
- Wy-14643:
Pirinixic acid.
References
- 1.Zhang Z, Burch PE, Cooney AJ, et al. Genomic analysis of the nuclear receptor family: new insights into structure, regulation, and evolution from the rat genome. Genome Research. 2004;14(4):580–590. doi: 10.1101/gr.2160004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Desvergne B, Michalik L, Wahli W. Transcriptional regulation of metabolism. Physiological Reviews. 2006;86(2):465–514. doi: 10.1152/physrev.00025.2005. [DOI] [PubMed] [Google Scholar]
- 3.Dreyer C, Krey G, Keller H, Givel F, Helftenbein G, Wahli W. Control of the peroxisomal β-oxidation pathway by a novel family of nuclear hormone receptors. Cell. 1992;68(5):879–887. doi: 10.1016/0092-8674(92)90031-7. [DOI] [PubMed] [Google Scholar]
- 4.Issemann I, Green S. Activation of a member of the steroid hormone receptor superfamily by peroxisome proliferators. Nature. 1990;347(6294):645–650. doi: 10.1038/347645a0. [DOI] [PubMed] [Google Scholar]
- 5.Feige JN, Gelman L, Michalik L, Desvergne B, Wahli W. From molecular action to physiological outputs: peroxisome proliferator-activated receptors are nuclear receptors at the crossroads of key cellular functions. Progress in Lipid Research. 2006;45(2):120–159. doi: 10.1016/j.plipres.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Kliewer SA, Forman BM, Blumberg B, et al. Differential expression and activation of a family of murine peroxisome proliferator-activated receptors. Proceedings of the National Academy of Sciences of the United States of America. 1994;91(15):7355–7359. doi: 10.1073/pnas.91.15.7355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braissant O, Foufelle F, Scotto C, Dauça M, Wahli W. Differential expression of peroxisome proliferator-activated receptors (PPARs): tissue distribution of PPAR-α, -β, and -γ in the adult rat. Endocrinology. 1996;137(1):354–366. doi: 10.1210/endo.137.1.8536636. [DOI] [PubMed] [Google Scholar]
- 8.Jones PS, Savory R, Barratt P, et al. Chromosomal localisation, inducibility, tissue-specific expression and strain differences in three murine peroxisome-proliferator-activated-receptor genes. European Journal of Biochemistry. 1995;233(1):219–226. doi: 10.1111/j.1432-1033.1995.219_1.x. [DOI] [PubMed] [Google Scholar]
- 9.Vidal-Puig A, Jimenez-Liñan M, Lowell BB, et al. Regulation of PPAR γ gene expression by nutrition and obesity in rodents. The Journal of Clinical Investigation. 1996;97(11):2553–2561. doi: 10.1172/JCI118703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waku T, Shiraki T, Oyama T, et al. Structural insight into PPARγ activation through covalent modification with endogenous fatty acids. Journal of Molecular Biology. 2009;385(1):188–199. doi: 10.1016/j.jmb.2008.10.039. [DOI] [PubMed] [Google Scholar]
- 11.Heinäniemi M, Uski JO, Degenhardt T, Carlberg C. Meta-analysis of primary target genes of peroxisome proliferator-activated receptors. Genome Biology. 2007;8(7, article R147) doi: 10.1186/gb-2007-8-7-r147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forman BM, Chen J, Evans RM. The peroxisome proliferator-activated receptors: ligands and activators. Annals of the New York Academy of Sciences. 1996;804:266–275. doi: 10.1111/j.1749-6632.1996.tb18621.x. [DOI] [PubMed] [Google Scholar]
- 13.Krey G, Braissant O, L’Horset F, et al. Fatty acids, eicosanoids, and hypolipidemic agents identified as ligands of peroxisome proliferator-activated receptors by coactivator-dependent receptor ligand assay. Molecular Endocrinology. 1997;11(6):779–791. doi: 10.1210/mend.11.6.0007. [DOI] [PubMed] [Google Scholar]
- 14.Xu HE, Lambert MH, Montana VG, et al. Molecular recognition of fatty acids by peroxisome proliferator- activated receptors. Molecular Cell. 1999;3(3):397–403. doi: 10.1016/s1097-2765(00)80467-0. [DOI] [PubMed] [Google Scholar]
- 15.Yessoufou A, Wahli W. Multifaceted roles of peroxisome proliferator-activated receptors (PPARs) at the cellular and whole organism levels. Swiss Medical Weekly. 2010;140(article w13071) doi: 10.4414/smw.2010.13071. [DOI] [PubMed] [Google Scholar]
- 16.Michalik L, Wahli W. Peroxisome proliferator-activated receptors (PPARs) in skin health, repair and disease. Biochimica et Biophysica Acta. 2007;1771(8):991–998. doi: 10.1016/j.bbalip.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 17.Escher P, Wahli W. Peroxisome proliferator-activated receptors: insight into multiple cellular functions. Mutation Research. 2000;448(2):121–138. doi: 10.1016/s0027-5107(99)00231-6. [DOI] [PubMed] [Google Scholar]
- 18.Desvergne B, Wahli W. Peroxisome proliferator-activated receptors: nuclear control of metabolism. Endocrine Reviews. 1999;20(5):649–688. doi: 10.1210/edrv.20.5.0380. [DOI] [PubMed] [Google Scholar]
- 19.Varga T, Czimmerer Z, Nagy L. PPARs are a unique set of fatty acid regulated transcription factors controlling both lipid metabolism and inflammation. Biochimica et Biophysica Acta. 2011;1812(8):1007–1022. doi: 10.1016/j.bbadis.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bishop-Bailey D. PPARs and angiogenesis. Biochemical Society Transactions. 2011;39:1601–1605. doi: 10.1042/BST20110643. [DOI] [PubMed] [Google Scholar]
- 21.Takada I, Kouzmenko AP, Kato S. Wnt and PPARgamma signaling in osteoblastogenesis and adipogenesis. Nature Reviews. Rheumatology. 2009;5(8):442–447. doi: 10.1038/nrrheum.2009.137. [DOI] [PubMed] [Google Scholar]
- 22.Olefsky JM, Saltiel AR. PPARγ and the treatment of insulin resistance. Trends in Endocrinology and Metabolism. 2000;11(9):362–368. doi: 10.1016/s1043-2760(00)00306-4. [DOI] [PubMed] [Google Scholar]
- 23.Gillespie W, Tyagi N, Tyagi SC. Role of PPARγ, a nuclear hormone receptor in neuroprotection. Indian Journal of Biochemistry and Biophysics. 2011;48(2):73–81. [PubMed] [Google Scholar]
- 24.Froment P, Gizard F, Defever D, Staels B, Dupont J, Monget P. Peroxisome proliferator-activated receptors in reproductive tissues: from gametogenesis to parturition. Journal of Endocrinology. 2006;189(2):199–209. doi: 10.1677/joe.1.06667. [DOI] [PubMed] [Google Scholar]
- 25.Sonoda J, Pei L, Evans RM. Nuclear receptors: decoding metabolic disease. FEBS Letters. 2008;582(1):2–9. doi: 10.1016/j.febslet.2007.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kadegowda AKG, Bionaz M, Piperova LS, Erdman RA, Loor JJ. Peroxisome proliferator-activated receptor-γ activation and long-chain fatty acids alter lipogenic gene networks in bovine mammary epithelial cells to various extents. Journal of Dairy Science. 2009;92(9):4276–4289. doi: 10.3168/jds.2008-1932. [DOI] [PubMed] [Google Scholar]
- 27.Bionaz M, Loor JJ. ACSL1, AGPAT6, FABP3, LPIN1, and SLC27A6 are the most abundant isoforms in bovine mammary tissue and their expression is affected by stage of lactation. The Journal of Nutrition. 2008;138(6):1019–1024. doi: 10.1093/jn/138.6.1019. [DOI] [PubMed] [Google Scholar]
- 28.Bionaz M, Thering BJ, Loor JJ. Fine metabolic regulation in ruminants via nutrient-gene interactions: saturated long-chain fatty acids increase expression of genes involved in lipid metabolism and immune response partly through PPAR-alpha activation. The British Journal of Nutrition. 2012;107:179–191. doi: 10.1017/S0007114511002777. [DOI] [PubMed] [Google Scholar]
- 29.Sundvold H, Brzozowska A, Lien S. Characterisation of bovine peroxisome proliferator-activated receptors γ1 and γ2: genetic mapping and differential expression of the two isoforms. Biochemical and Biophysical Research Communications. 1997;239(3):857–861. doi: 10.1006/bbrc.1997.7564. [DOI] [PubMed] [Google Scholar]
- 30.Meng H, Li H, Zhao JG, Gu ZL. Differential expression of peroxisome proliferator-activated receptors alpha and gamma gene in various chicken tissues. Domestic Animal Endocrinology. 2005;28(1):105–110. doi: 10.1016/j.domaniend.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 31.Sundvold H, Grindflek E, Lien S. Tissue distribution of porcine peroxisome proliferator-activated receptor α: detection of an alternatively spliced mRNA. Gene. 2001;273(1):105–113. doi: 10.1016/s0378-1119(01)00562-5. [DOI] [PubMed] [Google Scholar]
- 32.Cherfaoui M, Durand D, Bonnet M, et al. Expression of enzymes and transcription factors involved in n-3 long chain PUFA biosynthesis in limousin bull tissues. Lipids. 2012;47:391–401. doi: 10.1007/s11745-011-3644-z. [DOI] [PubMed] [Google Scholar]
- 33.Bionaz M, Loor JJ. Gene networks driving bovine milk fat synthesis during the lactation cycle. BMC Genomics. 2008;9, article 366 doi: 10.1186/1471-2164-9-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mani O, Sorensen MT, Sejrsen K, Bruckmaier RM, Albrecht C. Differential expression and localization of lipid transporters in the bovine mammary gland during the pregnancy-lactation cycle. Journal of Dairy Science. 2009;92(8):3744–3756. doi: 10.3168/jds.2009-2063. [DOI] [PubMed] [Google Scholar]
- 35.Sharma R, Bionaz M, Kadegowda AKG, et al. Transcriptomics comparison of MacT cells and mammary tissue during pregnancy and lactation. Journal of Dairy Science. 2009;92(article M145) [Google Scholar]
- 36.Bionaz M, Baumrucker CR, Shirk E, Vanden Heuvel JP, Block E, Varga GA. Short communication: characterization of Madin-Darby bovine kidney cell line for peroxisome proliferator-activated receptors: temporal response and sensitivity to fatty acids. Journal of Dairy Science. 2008;91(7):2808–2813. doi: 10.3168/jds.2007-0789. [DOI] [PubMed] [Google Scholar]
- 37.Bernard L, Torbati MB, Graulet B, Leroux C, Chilliard Y. Long-chain fatty acids differentially alter lipogenesis in bovine and caprine mammary slices. Journal of Dairy Research. 2013;80(1):89–95. doi: 10.1017/S0022029912000726. [DOI] [PubMed] [Google Scholar]
- 38.Mohan M, Malayer JR, Geisert RD, Morgan GL. Expression patterns of retinoid X receptors, retinaldehyde dehydrogenase, and peroxisome proliferator activated receptor gamma in bovine preattachment embryos. Biology of Reproduction. 2002;66(3):692–700. doi: 10.1095/biolreprod66.3.692. [DOI] [PubMed] [Google Scholar]
- 39.Miles JR, Farin CE, Rodriguez KF, Alexander JE, Farin PW. Angiogenesis and morphometry of bovine placentas in late gestation from embryos produced in vivo or in vitro. Biology of Reproduction. 2004;71(6):1919–1926. doi: 10.1095/biolreprod.104.031427. [DOI] [PubMed] [Google Scholar]
- 40.Yiallourides M, Sebert SP, Wilson V, et al. The differential effects of the timing of maternal nutrient restriction in the ovine placenta on glucocorticoid sensitivity, uncoupling protein 2, peroxisome proliferator-activated receptor-γ and cell proliferation. Reproduction. 2009;138(3):601–608. doi: 10.1530/REP-09-0043. [DOI] [PubMed] [Google Scholar]
- 41.Cammas L, Reinaud P, Bordas N, Dubois O, Germain G, Charpigny G. Developmental regulation of prostacyclin synthase and prostacyclin receptors in the ovine uterus and conceptus during the peri-implantation period. Reproduction. 2006;131(5):917–927. doi: 10.1530/rep.1.00799. [DOI] [PubMed] [Google Scholar]
- 42.Löhrke B, Viergutz T, Shahi SK, et al. Detection and functional characterisation of the transcription factor peroxisome proliferator-activated receptor γ in lutein cells. Journal of Endocrinology. 1998;159(3):429–439. doi: 10.1677/joe.0.1590429. [DOI] [PubMed] [Google Scholar]
- 43.Coyne GS, Kenny DA, Childs S, Sreenan JM, Waters SM. Dietary n-3 polyunsaturated fatty acids alter the expression of genes involved in prostaglandin biosynthesis in the bovine uterus. Theriogenology. 2008;70(5):772–782. doi: 10.1016/j.theriogenology.2008.05.048. [DOI] [PubMed] [Google Scholar]
- 44.MacLaren LA, Guzeloglu A, Michel F, Thatcher WW. Peroxisome proliferator-activated receptor (PPAR) expression in cultured bovine endometrial cells and response to omega-3 fatty acid, growth hormone and agonist stimulation in relation to series 2 prostaglandin production. Domestic Animal Endocrinology. 2006;30(3):155–169. doi: 10.1016/j.domaniend.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 45.Froment P, Fabre S, Dupont J, et al. Expression and functional role of peroxisome proliferator-activated receptor-γ in ovarian folliculogenesis in the sheep. Biology of Reproduction. 2003;69(5):1665–1674. doi: 10.1095/biolreprod.103.017244. [DOI] [PubMed] [Google Scholar]
- 46.Chiba Y, Ogita T, Ando K, Fujita T. PPARγ ligands inhibit TNF-α-induced LOX-1 expression in cultured endothelial cells. Biochemical and Biophysical Research Communications. 2001;286(3):541–546. doi: 10.1006/bbrc.2001.5361. [DOI] [PubMed] [Google Scholar]
- 47.Graugnard DE, Piantoni P, Bionaz M, Berger LL, Faulkner DB, Loor JJ. Adipogenic and energy metabolism gene networks in Longissimus lumborum during rapid post-weaning growth in Angus and Angus × Simmental cattle fed high-starch or low-starch diets. BMC Genomics. 2009;10, article 142 doi: 10.1186/1471-2164-10-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang ZG, Xiong L, Liu ZS, et al. The developmental changes and effect on IMF content of H-FABP and PPARγ mRNA expression in sheep muscle. Yi Chuan Xue Bao. 2006;33(6):507–514. doi: 10.1016/S0379-4172(06)60079-6. [DOI] [PubMed] [Google Scholar]
- 49.Taniguchi M, Guan LL, Zhang B, Dodson MV, Okine E, Moore SS. Adipogenesis of bovine perimuscular preadipocytes. Biochemical and Biophysical Research Communications. 2008;366(1):54–59. doi: 10.1016/j.bbrc.2007.11.110. [DOI] [PubMed] [Google Scholar]
- 50.Kim J, Oh YS, Shinn SH. Troglitazone reverses the inhibition of nitric oxide production by high glucose in cultured bovine retinal pericytes. Experimental Eye Research. 2005;81(1):65–70. doi: 10.1016/j.exer.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 51.Huff PW, Ren MQ, Lozeman FJ, Weselake RJ, Wegner J. Expression of peroxisome proliterator-activated receptor (PPARγ) mRNA in adipose and muscle tissue of Holstein and Charolais cattle. Canadian Journal of Animal Science. 2004;84(1):49–55. [Google Scholar]
- 52.Sharma I, Monga R, Singh N, Datta TK, Singh D. Ovary-specific novel peroxisome proliferator activated receptors-gamma transcripts in buffalo. Gene. 2012;504:245–252. doi: 10.1016/j.gene.2012.04.090. [DOI] [PubMed] [Google Scholar]
- 53.Sundvold H, Olsaker I, Gomez-Raya L, Lien S. The gene encoding the peroxisome proliferator-activated receptor (PPARA) maps to chromosome 5 in cattle. Animal Genetics. 1997;28(5):p. 374. doi: 10.1111/j.1365-2052.1997.tb03275.x. [DOI] [PubMed] [Google Scholar]
- 54.Kersten S, Rakhshandehroo M, Knoch B, Müller M. Peroxisome proliferator-activated receptor alpha target genes. PPAR Research. 2010;2010 doi: 10.1155/2010/612089.612089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bionaz M, Drackley JK, Rodriguez-Zas SL, et al. Uncovering adaptive hepatic gene networks due to prepartum plane of dietary energy and physiological state in periparturient Holstein cows. Journal of Dairy Science. 2007;90:678–678. [Google Scholar]
- 56.Loor JJ, Everts RE, Bionaz M, et al. Nutrition-induced ketosis alters metabolic and signaling gene networks in liver of periparturient dairy cows. Physiological Genomics. 2007;32(1):105–116. doi: 10.1152/physiolgenomics.00188.2007. [DOI] [PubMed] [Google Scholar]
- 57.Loor JJ, Dann HM, Everts RE, et al. Temporal gene expression profiling of liver from periparturient dairy cows reveals complex adaptive mechanisms in hepatic function. Physiological Genomics. 2005;23(2):217–226. doi: 10.1152/physiolgenomics.00132.2005. [DOI] [PubMed] [Google Scholar]
- 58.Loor JJ, Dann HM, Janovick Guretzky NA, et al. Plane of nutrition prepartum alters hepatic gene expression and function in dairy cows as assessed by longitudinal transcript and metabolic profiling. Physiological Genomics. 2006;27(1):29–41. doi: 10.1152/physiolgenomics.00036.2006. [DOI] [PubMed] [Google Scholar]
- 59.Bionaz M, Samadi F, D'Occhio MJ, Loor JJ. Altered liver gene expression and reproductive function in postpartum suckled beef cows on different planes of nutrition. Journal of Dairy Science. 2007;90:649–649. [Google Scholar]
- 60.Selberg KT, Staples CR, Luchini ND, Badinga L. Dietary trans octadecenoic acids upregulate the liver gene encoding Peroxisome Proliterator-Activated Receptor-α in transition dairy cows. Journal of Dairy Research. 2005;72(1):107–114. doi: 10.1017/s0022029904000573. [DOI] [PubMed] [Google Scholar]
- 61.Thering BJ, Bionaz M, Loor JJ. Long-chain fatty acid effects on peroxisome proliferator-activated receptor-α-regulated genes in Madin-Darby bovine kidney cells: optimization of culture conditions using palmitate. Journal of Dairy Science. 2009;92(5):2027–2037. doi: 10.3168/jds.2008-1749. [DOI] [PubMed] [Google Scholar]
- 62.Ruby MA, Goldenson B, Orasanu G, Johnston TP, Plutzky J, Krauss RM. VLDL hydrolysis by LPL activates PPAR-α through generation of unbound fatty acids. Journal of Lipid Research. 2010;51(8):2275–2281. doi: 10.1194/jlr.M005561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Waters SM, Kelly JP, O’Boyle P, Moloney AP, Kenny DA. Effect of level and duration of dietary n-3 polyunsaturated fatty acid supplementation on the transcriptional regulation of {Delta}9-desaturase in muscle of beef cattle. Journal of Animal Science. 2009;87(1):244–252. doi: 10.2527/jas.2008-1005. [DOI] [PubMed] [Google Scholar]
- 64.Naeem A, Drackley JK, Stamey J, Loor JJ. Role of metabolic and cellular proliferation genes in ruminal development in response to enhanced plane of nutrition in neonatal Holstein calves. Journal of Dairy Science. 2012;95:1807–1820. doi: 10.3168/jds.2011-4709. [DOI] [PubMed] [Google Scholar]
- 65.Balaguer SA, Pershing RA, Rodriguez-Sallaberry C, Thatcher WW, Badinga L. Effects of bovine somatotropin on uterine genes related to the prostaglandin cascade in lactating dairy cows. Journal of Dairy Science. 2005;88(2):543–552. doi: 10.3168/jds.S0022-0302(05)72716-8. [DOI] [PubMed] [Google Scholar]
- 66.Graugnard DE. Immune Function, Gene Expression, Blood Indices and Performance in Transition Dairy Cows Affected by Diet and Inflammation. Urbana, Ill, USA: University of Illinois; 2011. [Google Scholar]
- 67.Buroker NE, Ning XH, Portman M. Cardiac PPARα protein expression is constant as alternate nuclear receptors and PGC-1 coordinately increase during the postnatal metabolic transition. PPAR Research. 2008;2008 doi: 10.1155/2008/279531.279531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Riahi Y, Sin-Malia Y, Cohen G, et al. The natural protective mechanism against hyperglycemia in vascular endothelial cells: roles of the lipid peroxidation product 4-hydroxydodecadienal and peroxisome proliferator-activated receptor δ . Diabetes. 2010;59(4):808–818. doi: 10.2337/db09-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lutzow YS, Gray C, Tellam R. 15-deoxy-Δ12,14-prostaglandin J2 induces chemokine expression, oxidative stress and microfilament reorganization in bovine mammary epithelial cells. Journal of Dairy Research. 2008;75(1):55–63. doi: 10.1017/S0022029907003056. [DOI] [PubMed] [Google Scholar]
- 70.Bionaz M, Periasamy K, Rodriguez-Zas SL, Hurley WL, Loor JJ. A novel dynamic impact approach (DIA) for functional analysis of time-course omics studies: validation using the bovine mammary transcriptome. PloS One. 2012;7(article e32455) doi: 10.1371/journal.pone.0032455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Arevalo-Turrubiarte M, Gonzalez-Davalos L, Yabuta A, et al. Effect of 2,4-thiazolidinedione on limousin cattle growth and on muscle and adipose tissue metabolism. PPAR Research. 2012;2012:8 pages. doi: 10.1155/2012/891841.891841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Revelo XS, Waldron MR. Effects of in vitro insulin and 2,4-thiazolidinedione on the function of neutrophils harvested from blood of cows in different physiological states. Journal of Dairy Science. 2010;93(9):3990–4005. doi: 10.3168/jds.2009-2922. [DOI] [PubMed] [Google Scholar]
- 73.Marx N, Bourcier T, Sukhova GK, Libby P, Plutzky J. PPARγ activation in human endothelial cells increases plasminogen activator inhibitor type-1 expression: PPARγ as a potential mediator in vascular disease. Arteriosclerosis, Thrombosis, and Vascular Biology. 1999;19(3):546–551. doi: 10.1161/01.atv.19.3.546. [DOI] [PubMed] [Google Scholar]
- 74.Tudor C, Feige JN, Pingali H, et al. Association with coregulators is the major determinant governing peroxisome proliferator-activated receptor mobility in living cells. Journal of Biological Chemistry. 2007;282(7):4417–4426. doi: 10.1074/jbc.M608172200. [DOI] [PubMed] [Google Scholar]
- 75.Zoete V, Grosdidier A, Michielin O. Peroxisome proliferator-activated receptor structures: ligand specificity, molecular switch and interactions with regulators. Biochimica et Biophysica Acta. 2007;1771(8):915–925. doi: 10.1016/j.bbalip.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 76.Bugge A, Mandrup S. Molecular mechanisms and genome-wide aspects of PPAR subtype specific transactivation. PPAR Research. 2010;2010 doi: 10.1155/2010/169506.169506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sheldrick ELR, Derecka K, Marshall E, et al. Peroxisome-proliferator-activated receptors and the control of levels of prostaglandin-endoperoxide synthase 2 by arachidonic acid in the bovine uterus. Biochemical Journal. 2007;406(1):175–183. doi: 10.1042/BJ20070089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Litherland NB, Bionaz M, Wallace RL, Loor JJ, Drackley JK. Effects of the peroxisome proliferator-activated receptor-α agonists clofibrate and fish oil on hepatic fatty acid metabolism in weaned dairy calves1. Journal of Dairy Science. 2010;93(6):2404–2418. doi: 10.3168/jds.2009-2716. [DOI] [PubMed] [Google Scholar]
- 79.Liu Y, Zhu Y, Rannou F, et al. Laminar flow activates peroxisome proliferator-activated receptor-γ in vascular endothelial cells. Circulation. 2004;110(9):1128–1133. doi: 10.1161/01.CIR.0000139850.08365.EC. [DOI] [PubMed] [Google Scholar]
- 80.Albrecht E, Gotoh T, Ebara F, et al. Cellular conditions for intramuscular fat deposition in Japanese Black and Holstein steers. Meat Science. 2011;89(1):13–20. doi: 10.1016/j.meatsci.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 81.Muhlhausler BS, Morrison JL, McMillen IC. Rosiglitazone increases the expression of peroxisome proliferator-activated receptor-γ target genes in adipose tissue, liver, and skeletal muscle in the sheep fetus in late gestation. Endocrinology. 2009;150(9):4287–4294. doi: 10.1210/en.2009-0462. [DOI] [PubMed] [Google Scholar]
- 82.Schoenberg KM, Overton TR. Effects of plane of nutrition and 2, 4-thiazolidinedione on insulin responses and adipose tissue gene expression in dairy cattle during late gestation. Journal of Dairy Science. 2011;94(12):6021–6035. doi: 10.3168/jds.2011-4533. [DOI] [PubMed] [Google Scholar]
- 83.Invernizzi G, Kadegowda AKG, Bionaz M, et al. Palmitate affects larger gene networks in MACT cells compared with trans-10,cis-12-CLA or PPAR-gamma activation via Rosiglitazone. Journal of Dairy Science. 2009;92(article 321) [Google Scholar]
- 84.Schoenberg KM, Perfield KL, Farney JK, et al. Effects of prepartum 2,4-thiazolidinedione on insulin sensitivity, plasma concentrations of tumor necrosis factor-alpha and leptin, and adipose tissue gene expression. Journal of Dairy Science. 2011;94(11):5523–5532. doi: 10.3168/jds.2011-4501. [DOI] [PubMed] [Google Scholar]
- 85.Sharma S, Sun X, Rafikov R, et al. PPAR-gamma regulates carnitine homeostasis and mitochondrial function in a lamb model of increased pulmonary blood flow. PLoS One. 2012;7(article e41555) doi: 10.1371/journal.pone.0041555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Khan MJ, Graugnard DE, Loor JJ. Endocannabinoid and PPARα signaling gene network expression in liver of peripartal cows fed two levels of dietary energy prepartum. Journal of Dairy Science. 2010;93(artcile 1124) [Google Scholar]
- 87.Delerive P, Martin-Nizard F, Chinetti G, et al. Peroxisome proliferator-activated receptor activators inhibit thrombin- induced endothelin-1 production in human vascular endothelial cells by inhibiting the activator protein-1 signaling pathway. Circulation Research. 1999;85(5):394–402. doi: 10.1161/01.res.85.5.394. [DOI] [PubMed] [Google Scholar]
- 88.Wang Y, Wang Y, Yang Q, et al. Effects of bezafibrate on the expression of endothelial nitric oxide synthase gene and its mechanisms in cultured bovine endothelial cells. Atherosclerosis. 2006;187(2):265–273. doi: 10.1016/j.atherosclerosis.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 89.Cho DH, Choi YJ, Jo SA, Jo I. Nitric oxide production and regulation of endothelial nitric-oxide synthase phosphorylation by prolonged treatment with troglitazone: evidence for involvement of peroxisome proliferator-activated receptor (PPAR) γ-dependent and PPARγ-independent signaling pathways. Journal of Biological Chemistry. 2004;279(4):2499–2506. doi: 10.1074/jbc.M309451200. [DOI] [PubMed] [Google Scholar]
- 90.Werner C, Gensch C, Pöss J, Haendeler J, Böhm M, Laufs U. Pioglitazone activates aortic telomerase and prevents stress-induced endothelial apoptosis. Atherosclerosis. 2011;216(1):23–34. doi: 10.1016/j.atherosclerosis.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 91.Soret B, Lee HJ, Finley E, Lee SC, Vernon RG. Regulation of differentiation of sheep subcutaneous and abdominal preadipocytes in culture. Journal of Endocrinology. 1999;161(3):517–524. doi: 10.1677/joe.0.1610517. [DOI] [PubMed] [Google Scholar]
- 92.Hayashida K, Kume N, Minami M, Kataoka H, Morimoto M, Kita T. Peroxisome proliferator-activated receptor α ligands increase lectin-like oxidized low density lipoprotein receptor-1 expression in vascular endothelial cells. Annals of the New York Academy of Sciences. 2001;947:370–372. doi: 10.1111/j.1749-6632.2001.tb03965.x. [DOI] [PubMed] [Google Scholar]
- 93.White HM, Koser SL, Donkin SS. Differential regulation of bovine pyruvate carboxylase promoters by fatty acids and peroxisome proliferator-activated receptor-α agonist. Journal of Dairy Science. 2011;94(7):3428–3436. doi: 10.3168/jds.2010-3960. [DOI] [PubMed] [Google Scholar]
- 94.Sommer M, Wolf G. Rosiglitazone increases PPARγ in renal tubular epithelial cells and protects against damage by hydrogen peroxide. American Journal of Nephrology. 2007;27(4):425–434. doi: 10.1159/000105125. [DOI] [PubMed] [Google Scholar]
- 95.Schoenberg KM, Giesy SL, Harvatine KJ, et al. Plasma FGF21 is elevated by the intense lipid mobilization of lactation. Endocrinology. 2011;152:4652–4661. doi: 10.1210/en.2011-1425. [DOI] [PubMed] [Google Scholar]
- 96.Vanden Heuvel JP. Peroxisome proliferator-activated receptors: a critical link among fatty acids, gene expression and carcinogenesis. The Journal of Nutrition. 1999;129(2):575S–580S. doi: 10.1093/jn/129.2.575S. [DOI] [PubMed] [Google Scholar]
- 97.Wright HM, Clish CB, Mikami T, et al. A synthetic antagonist for the peroxisome proliferator-activated receptor γ inhibits adipocyte differentiation. Journal of Biological Chemistry. 2000;275(3):1873–1877. doi: 10.1074/jbc.275.3.1873. [DOI] [PubMed] [Google Scholar]
- 98.Dworzanski T, Celinski K, Korolczuk A, et al. Influence of the peroxisome proliferator-activated receptor gamma (PPAR-γ) agonist, rosiglitazone and antagonist, biphenol-a-diglicydyl ether (BADGE) on the course of inflammation in the experimental model of colitis in rats. Journal of Physiology and Pharmacology. 2010;61(6):683–693. [PubMed] [Google Scholar]
- 99.Rakic B, Sagan SM, Noestheden M, et al. Peroxisome proliferator-activated receptor α antagonism inhibits hepatitis C virus replication. Chemistry and Biology. 2006;13(1):23–30. doi: 10.1016/j.chembiol.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 100.Xu HE, Stanley TB, Montana VG, et al. Structural basis for antagonist-mediated recruitment of nuclear co-repressors by PPARα . Nature. 2002;415(6873):813–817. doi: 10.1038/415813a. [DOI] [PubMed] [Google Scholar]
- 101.Shearer BG, Steger DJ, Way JM, et al. Identification and characterization of a selective peroxisome proliferator-activated receptor β/δ (NR1C2) antagonist. Molecular Endocrinology. 2008;22(2):523–529. doi: 10.1210/me.2007-0190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Shearer BG, Wiethe RW, Ashe A, et al. Identification and characterization of 4-chloro-N-(2- {[5-trifluoromethyl)- 2-pyridyl] sulfonyl} ethyl)benzamide (GSK3787), a selective and irreversible peroxisome proliferator-activated receptor δ (PPARδ) antagonist. Journal of Medicinal Chemistry. 2010;53(4):1857–1861. doi: 10.1021/jm900464j. [DOI] [PubMed] [Google Scholar]
- 103.de Dios ST, Hannan KM, Dilley RJ, Hill MA, Little PJ. Troglitazone, but not rosiglitazone, inhibits Na/H exchange activity and proliferation of macrovascular endothelial cells. Journal of Diabetes and Its Complications. 2001;15(3):120–127. doi: 10.1016/s1056-8727(01)00141-6. [DOI] [PubMed] [Google Scholar]
- 104.Fukunaga Y, Itoh H, Doi K, et al. Thiazolidinediones, peroxisome proliferator-activated receptor γ agonists, regulate endothelial cell growth and secretion of vasoactive peptides. Atherosclerosis. 2001;158(1):113–119. doi: 10.1016/s0021-9150(01)00430-0. [DOI] [PubMed] [Google Scholar]
- 105.Ohyama M, Matsuda K, Torii S, et al. The interaction between vitamin a and thiazolidinedione on bovine adipocyte differentiation in primary culture. Journal of Animal Science. 1998;76(1):61–65. doi: 10.2527/1998.76161x. [DOI] [PubMed] [Google Scholar]
- 106.Torii SI, Kawada T, Matsuda K, Matsui T, Ishihara T, Yano H. Thiazolidinedione induces the adipose differentiation of fibroblast-like cells resident within bovine skeletal muscle. Cell Biology International. 1998;22(6):421–427. doi: 10.1006/cbir.1998.0270. [DOI] [PubMed] [Google Scholar]
- 107.Kushibiki S, Hodate K, Shingu H, et al. Insulin resistance induced in dairy steers by tumor necrosis factor alpha is partially reversed by 2,4-thiazolidinedione. Domestic Animal Endocrinology. 2001;21(1):25–37. doi: 10.1016/s0739-7240(01)00102-3. [DOI] [PubMed] [Google Scholar]
- 108.Cappon GD, Liu RCM, Frame SR, Hurtt ME. Effects of the rat hepatic peroxisome proliferator, Wyeth 14,643, on the lactating goat. Drug and Chemical Toxicology. 2002;25(3):255–266. doi: 10.1081/dct-120005888. [DOI] [PubMed] [Google Scholar]
- 109.Smith KL, Butler WR, Overton TR. Effects of prepartum 2,4-thiazolidinedione on metabolism and performance in transition dairy cows. Journal of Dairy Science. 2009;92(8):3623–3633. doi: 10.3168/jds.2008-1508. [DOI] [PubMed] [Google Scholar]
- 110.Smith KL, Stebulis SE, Waldron MR, Overton TR. Prepartum 2,4-thiazolidinedione alters metabolic dynamics and dry matter intake of dairy cows. Journal of Dairy Science. 2007;90(8):3660–3670. doi: 10.3168/jds.2006-650. [DOI] [PubMed] [Google Scholar]
- 111.Bocos C, Gottlicher M, Gearing K, et al. Fatty acid activation of peroxisome proliferator-activated receptor (PPAR) Journal of Steroid Biochemistry and Molecular Biology. 1995;53(1–6):467–473. doi: 10.1016/0960-0760(95)00093-f. [DOI] [PubMed] [Google Scholar]
- 112.Duplus E, Forest C. Is there a single mechanism for fatty acid regulation of gene transcription? Biochemical Pharmacology. 2002;64(5-6):893–901. doi: 10.1016/s0006-2952(02)01157-7. [DOI] [PubMed] [Google Scholar]
- 113.Gottlicher M, Widmark E, Li Q, Gustafsson JA. Fatty acids activate a chimera of the clofibric acid-activated receptor and the glucocorticoid receptor. Proceedings of the National Academy of Sciences of the United States of America. 1992;89(10):4653–4657. doi: 10.1073/pnas.89.10.4653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hostetler HA, Petrescu AD, Kier AB, Schroeder F. Peroxisome proliferator-activated receptor α interacts with high affinity and is conformationally responsive to endogenous ligands. Journal of Biological Chemistry. 2005;280(19):18667–18682. doi: 10.1074/jbc.M412062200. [DOI] [PubMed] [Google Scholar]
- 115.Bonilla S, Redonnet A, Noël-Suberville C, Pallet V, Garcin H, Higueret P. High-fat diets affect the expression of nuclear retinoic acid receptor in rat liver. The British Journal of Nutrition. 2000;83(6):665–671. doi: 10.1017/s0007114500000842. [DOI] [PubMed] [Google Scholar]
- 116.Huang H, Starodub O, McIntosh A, Kier AB, Schroeder F. Liver fatty acid-binding protein targets fatty acids to the nucleus. Real time confocal and multiphoton fluorescence imaging in living cells. Journal of Biological Chemistry. 2002;277(32):29139–29151. doi: 10.1074/jbc.M202923200. [DOI] [PubMed] [Google Scholar]
- 117.Wolfrum C, Borrmann CM, Börchers T, Spener F. Fatty acids and hypolipidemic drugs regulate peroxisome proliferator-activated receptors α- and γ-mediated gene expression via liver fatty acid binding protein: a signaling path to the nucleus. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(5):2323–2328. doi: 10.1073/pnas.051619898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Khan SA, Vanden Heuvel JP. Reviews: current topics role of nuclear receptors in the regulation of gene expression by dietary fatty acids (review) Journal of Nutritional Biochemistry. 2003;14(10):554–567. doi: 10.1016/s0955-2863(03)00098-6. [DOI] [PubMed] [Google Scholar]
- 119.Vanden Heuvel JP, Thompson JT, Frame SRSR, Gillies PJ. Differential activation of nuclear receptors by perfluorinated fatty acid analogs and natural fatty acids: a comparison of human, mouse, and rat peroxisome proliferator-activated receptor-α, -β, and -γ, liver X receptor-β, and retinoid X receptor-α . Toxicological Sciences. 2006;92(2):476–489. doi: 10.1093/toxsci/kfl014. [DOI] [PubMed] [Google Scholar]
- 120.Zachut M, Arieli A, Lehrer H, Livshitz L, Yakoby S, Moallem U. Effects of increased supplementation of n-3 fatty acids to transition dairy cows on performance and fatty acid profile in plasma, adipose tissue, and milk fat. Journal of Dairy Science. 2010;93(12):5877–5889. doi: 10.3168/jds.2010-3427. [DOI] [PubMed] [Google Scholar]
- 121.Or-Rashid MM, Fisher R, Karrow N, AlZahal O, McBride BW. Plasma fatty acid profile of gestating ewes supplemented with docosahexaenoic acid. Canadian Journal of Animal Science. 2009;89:138–138. doi: 10.2527/jas.2009-1895. [DOI] [PubMed] [Google Scholar]
- 122.Peltier S, Portois L, Malaisse WJ, Carpenter YA. Fatty acid profile of plasma and liver lipds in mice depleted in long-chain polyunsaturated (n-3) fatty acids. International Journal of Molecular Medicine. 2008;22(4):559–563. [PubMed] [Google Scholar]
- 123.Ma J, Folsom AR, Eckfeldt JH, et al. Short- and long-term repeatability of fatty acid composition of human plasma phospholipids and cholesterol esters. The American Journal of Clinical Nutrition. 1995;62(3):572–578. doi: 10.1093/ajcn/62.3.572. [DOI] [PubMed] [Google Scholar]
- 124.Itoh T, Fairall L, Amin K, et al. Structural basis for the activation of PPARγ by oxidized fatty acids. Nature Structural and Molecular Biology. 2008;15(9):924–931. doi: 10.1038/nsmb.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hostetler HA, Huang H, Kier AB, Schroeder F. Glucose directly links to lipid metabolism through high affinity interaction with peroxisome proliferator-activated receptor α . The Journal of Biological Chemistry. 2008;283(4):2246–2254. doi: 10.1074/jbc.M705138200. [DOI] [PubMed] [Google Scholar]
- 126.Blanquicett C, Kang BY, Ritzenthaler JD, Jones DP, Hart CM. Oxidative stress modulates PPARγ in vascular endothelial cells. Free Radical Biology and Medicine. 2010;48(12):1618–1625. doi: 10.1016/j.freeradbiomed.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Borniquel S, Valle I, Cadenas S, Lamas S, Monsalve M. Nitric oxide regulates mitochondrial oxidative stress protection via the transcriptional coactivator PGC-1alpha. The FASEB Journal. 2006;20(11):1889–1891. doi: 10.1096/fj.05-5189fje. [DOI] [PubMed] [Google Scholar]
- 128.Kanata S, Akagi M, Nishimura S, et al. Oxidized LDL binding to LOX-1 upregulates VEGF expression in cultured bovine chondrocytes through activation of PPAR-γ . Biochemical and Biophysical Research Communications. 2006;348(3):1003–1010. doi: 10.1016/j.bbrc.2006.07.133. [DOI] [PubMed] [Google Scholar]
- 129.Bionaz M, Baumrucker CR, Shirk E, et al. Characterization of Madin-Darby bovine kidney cell line for peroxisome proliferator-activated receptors: temporal response and sensitivity to fatty acids. Journal of Dairy Science. 2009;92(9):4715–4715. doi: 10.3168/jds.2007-0789. vol. 91, p. 2808, 2008. [DOI] [PubMed] [Google Scholar]
- 130.Lee JH, Banerjee A, Ueno Y, Ramaiah SK. Potential relationship between hepatobiliary osteopontin and peroxisome proliferator-activated receptor α expression following ethanol-associated hepatic injury in vivo and in vitro. Toxicological Sciences. 2008;106(1):290–299. doi: 10.1093/toxsci/kfn165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Oyama Y, Akuzawa N, Nagai R, Kurabayashi M. PPARγ ligand inhibits osteopontin gene expression through interference with binding of nuclear factors to A/T-rich sequence in THP-1 cells. Circulation Research. 2002;90(3):348–355. doi: 10.1161/hh0302.105098. [DOI] [PubMed] [Google Scholar]
- 132.Kishimoto M, Fujiki R, Takezawa S, et al. Nuclear receptor mediated gene regulation through chromatin remodeling and histone modifications. Endocrine Journal. 2006;53(2):157–172. doi: 10.1507/endocrj.53.157. [DOI] [PubMed] [Google Scholar]
- 133.Thompson GM, Trainor D, Biswas C, LaCerte C, Berger JP, Kelly LJ. A high-capacity assay for PPARγ ligand regulation of endogenous aP2 expression in 3T3-L1 cells. Analytical Biochemistry. 2004;330(1):21–28. doi: 10.1016/j.ab.2004.03.061. [DOI] [PubMed] [Google Scholar]
- 134.Ji P, Osorio JS, Drackley JK, Loor JJ. Overfeeding a moderate energy diet prepartum does not impair bovine subcutaneous adipose tissue insulin signal transduction and induces marked changes in peripartal gene network expression. Journal of Dairy Science. 2012;95:4333–4351. doi: 10.3168/jds.2011-5079. [DOI] [PubMed] [Google Scholar]
- 135.Kadegowda AKG, Bionaz M, Thering B, Piperova LS, Erdman RA, Loor JJ. Identification of internal control genes for quantitative polymerase chain reaction in mammary tissue of lactating cows receiving lipid supplements. Journal of Dairy Science. 2009;92(5):2007–2019. doi: 10.3168/jds.2008-1655. [DOI] [PubMed] [Google Scholar]
- 136.Bustin SA, Benes V, Garson JA, et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clinical Chemistry. 2009;55(4):611–622. doi: 10.1373/clinchem.2008.112797. [DOI] [PubMed] [Google Scholar]
- 137.Kersten S, Seydoux J, Peters JM, Gonzalez FJ, Desvergne B, Wahli W. Peroxisome proliferator-activated receptor α mediates the adaptive response to fasting. The Journal of Clinical Investigation. 1999;103(11):1489–1498. doi: 10.1172/JCI6223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Schlegel G, Keller J, Hirche F, et al. Expression of genes involved in hepatic carnitine synthesis and uptake in dairy cows in the transition period and at different stages of lactation. BMC Veterinary Research. 2012;8(article 28) doi: 10.1186/1746-6148-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.van Dorland HA, Richter S, Morel I, Doherr MG, Castro N, Bruckmaier RM. Variation in hepatic regulation of metabolism during the dry period and in early lactation in dairy cows. Journal of Dairy Science. 2009;92(5):1924–1940. doi: 10.3168/jds.2008-1454. [DOI] [PubMed] [Google Scholar]
- 140.Carriquiry M, Weber WJ, Fahrenkrug SC, Crooker BA. Hepatic gene expression in multiparous Holstein cows treated with bovine somatotropin and fed n-3 fatty acids in early lactation. Journal of Dairy Science. 2009;92(10):4889–4900. doi: 10.3168/jds.2008-1676. [DOI] [PubMed] [Google Scholar]
- 141.Kuhla B, Gors S, Metges CC. Hypothalamic orexin A expression and the involvement of AMPK and PPAR-gamma signalling in energy restricted dairy cows. Archiv für Tierzucht-Archives of Animal Breeding. 2011;54:567–579. [Google Scholar]
- 142.Brennan KM, Michal JJ, Ramsey JJ, Johnson KA. Body weight loss in beef cows: I. The effect of increased β-oxidation on messenger ribonucleic acid levels of uncoupling proteins two and three and peroxisome proliferator-activated receptor in skeletal muscle. Journal of Animal Science. 2009;87(9):2860–2866. doi: 10.2527/jas.2008-1302. [DOI] [PubMed] [Google Scholar]
- 143.Janovick-Guretzky NA, Dann HM, Loor JJ, Drackley JK. Prepartum plane of dietary energy alters hepatic expression of inflammatory and fatty acid oxidation genes in dairy cows. The FASEB Journal. 2007;21:A374–A374. [Google Scholar]
- 144.Bispham J, Gardner DS, Gnanalingham MG, Stephenson T, Symonds ME, Budge H. Maternal nutritional programming of fetal adipose tissue development: differential effects on mRNA abundance for uncoupling proteins, peroxisome proliferator activated and prolactin receptors. Endocrinology. 2005;146(9):3943–3949. doi: 10.1210/en.2005-0246. [DOI] [PubMed] [Google Scholar]
- 145.Muhlhausler BS, Duffield JA, McMillen IC. Increased maternal nutrition stimulates peroxisome proliferator activated receptor-γ, adiponectin, and leptin messenger ribonucleic acid expression in adipose tissue before birth. Endocrinology. 2007;148(2):878–885. doi: 10.1210/en.2006-1115. [DOI] [PubMed] [Google Scholar]
- 146.Rattanatray L, MacLaughlin SM, Kleemann DO, Walker SK, Muhlhausler BS, McMillen IC. Impact of maternal periconceptional overnutrition on fat mass and expression of adipogenic and lipogenic genes in visceral and subcutaneous fat depots in the postnatal lamb. Endocrinology. 2010;151(11):5195–5205. doi: 10.1210/en.2010-0501. [DOI] [PubMed] [Google Scholar]
- 147.García-Rojas P, Antaramian A, González-Dávalos L, et al. Induction of peroxisomal proliferator-activated receptor γ and peroxisomal proliferator-activated receptor γ coactivator 1 by unsaturated fatty acids, retinoic acid, and carotenoids in preadipocytes obtained from bovine white adipose tissue. Journal of Animal Science. 2010;88(5):1801–1808. doi: 10.2527/jas.2009-2579. [DOI] [PubMed] [Google Scholar]
- 148.Loor JJ, Bionaz M, Invernizzi G. Systems biology and animal nutrition: insights from the dairy cow during growth and the lactation cycle. In: te Pas MFW, Woelders H, Bannink A, editors. Systems Biology and Livestock Science. Hoboken, NJ, USA: Wiley-Blackwell; 2011. pp. 215–246. [Google Scholar]
- 149.Ji P. Transcriptional Adaptation of Adipose Tissue in Dairy Cows in Response to Energy Overfeeding. Urbana, Ill, USA: University of Illinois; 2011. [Google Scholar]
- 150.Lim D, Kim NK, Park HS, et al. Identification of candidate genes related to bovine marbling using protein-protein interaction networks. International Journal of Biological Sciences. 2011;7:992–1002. doi: 10.7150/ijbs.7.992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Drackley JK, Overton TR, Douglas GN. Adaptations of glucose and long-chain fatty acid metabolism in liver of dairy cows during the periparturient period. Journal of Dairy Science. 2001;84:E100–E112. [Google Scholar]
- 152.Bionaz M, Loor JJ. Ruminant metabolic systems biology: reconstruction and integration of transcriptome dynamics underlying functional responses of tissues to nutrition and physiological state. Gene Regulation and Systems Biology. 2012;6:109–125. doi: 10.4137/GRSB.S9852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bauman DE, Harvatine KJ, Lock AL. Nutrigenomics, rumen-derived bioactive fatty acids, and the regulation of milk fat synthesis. Annual Review of Nutrition. 2011;31:299–319. doi: 10.1146/annurev.nutr.012809.104648. [DOI] [PubMed] [Google Scholar]
- 154.Monaco E, Lima A, Bionaz M, et al. Morphological and transcriptomic comparison of adipose and bone marrow derived porcine stem cells. Journal of Tissue Engineering and Regenerative Medicine. 2009;2:20–33. [Google Scholar]
- 155.Sertznig P, Seifert M, Tilgen W, Reichrath J. Peroxisome proliferator-activated receptors (PPARs) and the human skin: importance of PPARs in skin physiology and dermatologic diseases. American Journal of Clinical Dermatology. 2008;9(1):15–31. doi: 10.2165/00128071-200809010-00002. [DOI] [PubMed] [Google Scholar]
- 156.Corl BA, Butler ST, Butler WR, Bauman DE. Short communication: regulation of milk fat yield and fatty acid composition by insulin. Journal of Dairy Science. 2006;89(11):4172–4175. doi: 10.3168/jds.S0022-0302(06)72462-6. [DOI] [PubMed] [Google Scholar]
- 157.McFadden JW, Corl BA. Activation of liver X receptor (LXR) enhances de novo fatty acid synthesis in bovine mammary epithelial cells. Journal of Dairy Science. 2010;93(10):4651–4658. doi: 10.3168/jds.2010-3202. [DOI] [PubMed] [Google Scholar]
- 158.Oppi-Williams C, Suagee JK, Corl BA. Regulation of lipid synthesis by liver X receptor alpha and sterol regulatory element-binding protein 1 in mammary epithelial cells. Journal of Dairy Science. 2013;96(1):112–121. doi: 10.3168/jds.2011-5276. [DOI] [PubMed] [Google Scholar]
- 159.Ma L, Corl BA. Transcriptional regulation of lipid synthesis in bovine mammary epithelial cells by sterol regulatory element binding protein-1. Journal of Dairy Science. 2012;95:3743–3755. doi: 10.3168/jds.2011-5083. [DOI] [PubMed] [Google Scholar]
- 160.Rudolph MC, McManaman JL, Phang T, et al. Metabolic regulation in the lactating mammary gland: a lipid synthesizing machine. Physiological Genomics. 2007;28(3):323–336. doi: 10.1152/physiolgenomics.00020.2006. [DOI] [PubMed] [Google Scholar]
- 161.Bionaz M, Loor JJ. Comparative MammOmics of milk fat synthesis in Mus musculus vs. Bos Taurus. Journal of Dairy Science. 2008;91:566–567. [Google Scholar]
- 162.Shu DP, Chen BL, Hong J, et al. Global transcriptional profiling in porcine mammary glands from late pregnancy to peak lactation. Omics. 2012;16:123–137. doi: 10.1089/omi.2011.0116. [DOI] [PubMed] [Google Scholar]
- 163.Lin X, Loor JJ, Herbein JH. Trans10,cis12-18:2 is a more potent inhibitor of de novo fatty acid synthesis and desaturation than cis9,trans11-18:2 in the mammary gland of lactating mice. The Journal of Nutrition. 2004;134(6):1362–1368. doi: 10.1093/jn/134.6.1362. [DOI] [PubMed] [Google Scholar]
- 164.Bishop-Bailey D, Bystrom J. Emerging roles of peroxisome proliferator-activated receptor-β/δ in inflammation. Pharmacology and Therapeutics. 2009;124(2):141–150. doi: 10.1016/j.pharmthera.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 165.Hauner H. The mode of action of thiazolidinediones. Diabetes/Metabolism Research and Reviews. 2002;18(2):S10–S15. doi: 10.1002/dmrr.249. [DOI] [PubMed] [Google Scholar]
- 166.Perdomo MC, Santos JE, Badinga L. Trans-10, cis-12 conjugated linoleic acid and the PPAR-gamma agonist rosiglitazone attenuate lipopolysaccharide-induced TNF-alpha production by bovine immune cells. Domestic Animal Endocrinology. 2011;41(3):118–125. doi: 10.1016/j.domaniend.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 167.Ahmed W, Orasanu G, Nehra V, et al. High-density lipoprotein hydrolysis by endothelial lipase activates PPARα: a candidate mechanism for high-density lipoprotein-mediated repression of leukocyte adhesion. Circulation Research. 2006;98(4):490–498. doi: 10.1161/01.RES.0000205846.46812.be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mitterhuemer S, Petzl W, Krebs S, et al. Escherichia coli infection induces distinct local and systemic transcriptome responses in the mammary gland. BMC Genomics. 2010;11(1, article 138) doi: 10.1186/1471-2164-11-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Moyes KM, Drackley JK, Morin DE, et al. Gene network and pathway analysis of bovine mammary tissue challenged with Streptococcus uberis reveals induction of cell proliferation and inhibition of PPAR signaling as potential mechanism for the negative relationships between immune response and lipid metabolism. BMC Genomics. 2009;10, article 542 doi: 10.1186/1471-2164-10-542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Jiang L, Sørensen P, Røntved C, Vels L, Ingvartsen KL. Gene expression profiling of liver from dairy cows treated intra-mammary with lipopolysaccharide. BMC Genomics. 2008;9, article 443 doi: 10.1186/1471-2164-9-443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Loor JJ, Moyes KM, Bionaz M. Functional adaptations of the transcriptome to mastitis-causing pathogens: the mammary gland and beyond. Journal of Mammary Gland Biology and Neoplasia. 2011;16(4):305–322. doi: 10.1007/s10911-011-9232-2. [DOI] [PubMed] [Google Scholar]
- 172.Graugnard DE, Moyes KM, Trevisi E, et al. Liver lipid content and inflammometabolic indices in peripartal dairy cows are altered in response to prepartal energy intake and postpartal intramammary inflammatory challenge. Journal of Dairy Science. 2013;96:918–935. doi: 10.3168/jds.2012-5676. [DOI] [PubMed] [Google Scholar]
- 173.Lu B, Moser A, Shigenaga JK, Grunfeld C, Feingold KR. The acute phase response stimulates the expression of angiopoietin like protein 4. Biochemical and Biophysical Research Communications. 2010;391(4):1737–1741. doi: 10.1016/j.bbrc.2009.12.145. [DOI] [PubMed] [Google Scholar]
- 174.Koltes DA, Spurlock DM. Adipose tissue angiopoietin-like protein 4 messenger RNA changes with altered energy balance in lactating Holstein cows. Domestic Animal Endocrinology. 2012;43(4):307–316. doi: 10.1016/j.domaniend.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 175.Bertoni G, Trevisi E, Han X, Bionaz M. Effects of inflammatory conditions on liver activity in puerperium period and consequences for performance in dairy cows. Journal of Dairy Science. 2008;91(9):3300–3310. doi: 10.3168/jds.2008-0995. [DOI] [PubMed] [Google Scholar]
- 176.Bionaz M, Trevisi E, Calamari L, Librandi F, Ferrari A, Bertoni G. Plasma paraoxonase, health, inflammatory conditions, and liver function in transition dairy cows. Journal of Dairy Science. 2007;90(4):1740–1750. doi: 10.3168/jds.2006-445. [DOI] [PubMed] [Google Scholar]
- 177.Shahzad K, Sumner-Thomson J, McNamara JP, Loor JJ. Analysis of bovine adipose transcriptomics data during the transition from pregnancy to early lactation using two bioinformatics approaches. Journal of Dairy Science. 2011;94(article M258) [Google Scholar]
- 178.Kersten S. Regulation of lipid metabolism via angiopoietin-like proteins. Biochemical Society Transactions. 2005;33(5):1059–1062. doi: 10.1042/BST20051059. [DOI] [PubMed] [Google Scholar]
- 179.Kharitonenkov A, Shiyanova TL, Koester A, et al. FGF-21 as a novel metabolic regulator. The Journal of Clinical Investigation. 2005;115(6):1627–1635. doi: 10.1172/JCI23606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Hondares E, Rosell M, Gonzalez FJ, Giralt M, Iglesias R, Villarroya F. Hepatic FGF21 expression is induced at birth via PPARα in response to milk intake and contributes to thermogenic activation of neonatal brown fat. Cell Metabolism. 2010;11(3):206–212. doi: 10.1016/j.cmet.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Cho DH, Choi YJ, Jo SA, et al. Troglitazone acutely inhibits protein synthesis in endothelial cells via a novel mechanism involving protein phosphatase 2A-dependent p70 S6 kinase inhibition. American Journal of Physiology—Cell Physiology. 2006;291(2):C317–C326. doi: 10.1152/ajpcell.00491.2005. [DOI] [PubMed] [Google Scholar]
- 182.Mandard S, Müller M, Kersten S. Peroxisome proliferator-activated receptor α target genes. Cellular and Molecular Life Sciences. 2004;61(4):393–416. doi: 10.1007/s00018-003-3216-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.White HM, Koser SL, Donkin SS. Gluconeogenic enzymes are differentially regulated by fatty acid cocktails in Madin-Darby bovine kidney cells. Journal of Dairy Science. 2012;95(3):1249–1256. doi: 10.3168/jds.2011-4644. [DOI] [PubMed] [Google Scholar]
- 184.Andrikopoulos S, Blair AR, Deluca N, Fam BC, Proietto J. Evaluating the glucose tolerance test in mice. American Journal of Physiology—Endocrinology and Metabolism. 2008;295(6):E1323–E1332. doi: 10.1152/ajpendo.90617.2008. [DOI] [PubMed] [Google Scholar]
- 185.Bionaz M, Loor JJ. Gene networks driving bovine mammary protein synthesis during the lactation cycle. Bioinformatics and Biology Insights. 2011;5:83–98. doi: 10.4137/BBI.S7003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Bionaz M, Periasamy K, Rodriguez-Zas SL, et al. Old and new stories: revelations from functional analysis of the bovine mammary transcriptome during the lactation cycle. PloS One. 2012;7(article e33268) doi: 10.1371/journal.pone.0033268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Berger J, Moller DE. The mechanisms of action of PPARs. Annual Review of Medicine. 2002;53:409–435. doi: 10.1146/annurev.med.53.082901.104018. [DOI] [PubMed] [Google Scholar]
- 188.Viswakarma N, Jia Y, Bai L, et al. Coactivators in PPAR-regulated gene expression. PPAR Research. 2010;2010:21 pages. doi: 10.1155/2010/250126.250126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Lengi AJ, Corl BA. Factors influencing the differentiation of bovine preadipocytes in vitro. Journal of Animal Science. 2010;88(6):1999–2008. doi: 10.2527/jas.2009-2439. [DOI] [PubMed] [Google Scholar]
- 190.Drackley JK. ADSA foundation scholar award: biology of dairy cows during the transition period: the final frontier? Journal of Dairy Science. 1999;82(11):2259–2273. doi: 10.3168/jds.s0022-0302(99)75474-3. [DOI] [PubMed] [Google Scholar]
- 191.Holtenius P, Holtenius K. A model to estimate insulin sensitivity in dairy cows. Acta Veterinaria Scandinavica. 2007;49(1, article 29) doi: 10.1186/1751-0147-49-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Trevisi E, Amadori M, Archetti I, Lacetera N, Bertoni G. Inflammatory response and acute phase proteins in the transition period of high-yielding dairy cows. In: Veas F, editor. Acute Phase Proteins as Early Non-Specific Biomarkers of Human and Veterinary Diseases. Rijeka, Croatia: InTech; 2011. [Google Scholar]
- 193.Allen MS, Bradford BJ, Harvatine KJ. The cow as a model to study food intake regulation. Annual Review of Nutrition. 2005;25:523–547. doi: 10.1146/annurev.nutr.25.050304.092704. [DOI] [PubMed] [Google Scholar]
- 194.Bobe G, Young JW, Beitz DC. Invited review: pathology, etiology, prevention, and treatment of fatty liver in dairy cows. Journal of Dairy Science. 2004;87(10):3105–3124. doi: 10.3168/jds.S0022-0302(04)73446-3. [DOI] [PubMed] [Google Scholar]
- 195.Holtenius P, Holtenius K. New aspects of ketone bodies in energy metabolism of dairy cows: a review. Zentralblatt für Veterinärmedizin. Reihe A. 1996;43(10):579–587. doi: 10.1111/j.1439-0442.1996.tb00491.x. [DOI] [PubMed] [Google Scholar]
- 196.Walsh RB, Walton JS, Kelton DF, LeBlanc SJ, Leslie KE, Duffield TF. The effect of subclinical ketosis in early lactation on reproductive performance of postpartum dairy cows. Journal of Dairy Science. 2007;90(6):2788–2796. doi: 10.3168/jds.2006-560. [DOI] [PubMed] [Google Scholar]
- 197.Drackley JK, Dann HM, Douglas GN, et al. Physiological and pathological adaptations in dairy cows that may increase susceptibility to periparturient diseases and disorders. Italian Journal of Animal Science. 2005;4(4):323–344. [Google Scholar]
- 198.Sordillo LM, Contreras GA, Aitken SL. Metabolic factors affecting the inflammatory response of periparturient dairy cows. Animal Health Research Reviews / Conference of Research Workers in Animal Diseases. 2009;10(1):53–63. doi: 10.1017/S1466252309990016. [DOI] [PubMed] [Google Scholar]
- 199.Bragt MCE, Popeijus HE. Peroxisome proliferator-activated receptors and the metabolic syndrome. Physiology and Behavior. 2008;94(2):187–197. doi: 10.1016/j.physbeh.2007.11.053. [DOI] [PubMed] [Google Scholar]
- 200.Guo L, Tabrizchi R. Peroxisome proliferator-activated receptor gamma as a drug target in the pathogenesis of insulin resistance. Pharmacology and Therapeutics. 2006;111(1):145–173. doi: 10.1016/j.pharmthera.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 201.Bionaz M. Studi sui Rapporti fra Funzionalità Epatica e Fenomeni Infiammatori al Parto: Conseguenze sulle Performance Produttive e Riproduttive. Piacenza, Italy: Università cattolica del Sacro Cuore.; 2004. [Google Scholar]
- 202.Andersen JB, Ridder C, Larsen T. Priming the cow for mobilization in the periparturient period: effects of supplementing the dry cow with saturated fat or linseed. Journal of Dairy Science. 2008;91(3):1029–1043. doi: 10.3168/jds.2007-0437. [DOI] [PubMed] [Google Scholar]
- 203.Gruffat D, Durand D, Graulet B, Bauchart D. Regulation of VLDL synthesis and secretion in the liver. Reproduction Nutrition Development. 1996;36(4):375–389. doi: 10.1051/rnd:19960404. [DOI] [PubMed] [Google Scholar]
- 204.Allen MS, Bradford BJ, Oba M. Board-invited review: the hepatic oxidation theory of the control of feed intake and its application to ruminants. Journal of Animal Science. 2009;87(10):3317–3334. doi: 10.2527/jas.2009-1779. [DOI] [PubMed] [Google Scholar]
- 205.Bernabucci U, Ronchi B, Basiricò L, et al. Abundance of mRNA of apolipoprotein B100, apolipoprotein E, and microsomal triglyceride transfer protein in liver from periparturient dairy cows. Journal of Dairy Science. 2004;87(9):2881–2888. doi: 10.3168/jds.S0022-0302(04)73418-9. [DOI] [PubMed] [Google Scholar]
- 206.Katoh N. Relevance of apolipoproteins in the development of fatty liver and fatty liver-related peripartum diseases in dairy cows. Journal of Veterinary Medical Science. 2002;64(4):293–307. doi: 10.1292/jvms.64.293. [DOI] [PubMed] [Google Scholar]
- 207.Contreras GA, Sordillo LM. Lipid mobilization and inflammatory responses during the transition period of dairy cows. Comparative Immunology, Microbiology and Infectious Diseases. 2011;34(3):281–289. doi: 10.1016/j.cimid.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 208.Ball RK, Friis RR, Schoenenberger CA, Doppler W, Groner B. Prolactin regulation of beta-casein gene expression and of a cytosolic 120-kd protein in a cloned mouse mammary epithelial cell line. The EMBO Journal. 1988;7(7):2089–2095. doi: 10.1002/j.1460-2075.1988.tb03048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Hsieh CW, Huang C, Bederman I, et al. Function of phosphoenolpyruvate carboxykinase in mammary gland epithelial cells. Journal of Lipid Research. 2011;52(7):1352–1362. doi: 10.1194/jlr.M012666. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1: Summary of the studies where activation of PPAR isotypes was performed in ruminants using synthetic agonists or other known natural ligands (e.g., 15-deoxy-Δ12,14-prostaglandin J2 for PPARγ). The studies are sorted by year of publication.
Supplementary Table 2: Factors affecting the expression of PPAR isotype genes in various ruminant tissues/cells.


