A meta-analysis of four randomized trials comparing laparoscopic versus open repair of perforated ulcer did not demonstrate significant superiority of the laparoscopic or open approach.
Keywords: Peptic ulcer disease, Perforated peptic ulcer, Gastric ulcer, Duodenal ulcer, Laparoscopy, Meta-analysis
Abstract
Background and Objectives:
Laparoscopic treatment of perforated peptic ulcer (PPU) has been introduced as an alternative procedure to open surgery. It has been postulated that the minimally invasive approach involves less operative stress and results in decreased morbidity and mortality.
Methods:
We conducted a meta-analysis of randomized trials to test this hypothesis. Medline, EMBASE, and the Cochrane Central Register of Randomized Trials databases were searched, with no date or language restrictions.
Results:
Our literature search identified 4 randomized trials, with a cumulative number of 289 patients, that compared the laparoscopic approach with open sutured repair of perforated ulcer. Analysis of outcomes did not favor either approach in terms of morbidity, mortality, and reoperation rate, although odds ratios seemed to consistently support the laparoscopic approach. Results did not determine the comparative efficiency and safety of laparoscopic or open approach for PPU.
Conclusion:
In view of an increased interest in the laparoscopic approach, further randomized trials are considered essential to determine the relative effectiveness of laparoscopic and open repair of PPU.
INTRODUCTION
Laparoscopic repair of perforated peptic ulcer (PPU) was first reported with the introduction of laparoscopy.1,2 Nevertheless, the use of the procedure in routine practice has been rather limited during the 1990s, largely because of the low incidence of PPU after identification of Helicobacter pylori as a prime factor, and because of the effectiveness of pharmacologic treatment in eradication of the bacterium and prevention of ulcer recurrence.3 Nevertheless, several studies have reported the use of the laparoscopic approach in clinical practice. Minimally invasive treatment of PPU involves entering the abdominal cavity after establishing a pneumoperitoneum, closure of the gastric defect, and lavage of the abdomen. Closure of the defect is facilitated either by direct suturing with or without placement of an omental patch or by introduction of biological glue with or without placement of a gelatin sponge.4,5 The concept of sutured closure is the laparoscopic counterpart to the open technique, whereas nonsutured repair does not require laparoscopic suturing skills and has the advantage of shorter operative time.6
The decreasing incidence of PPU has diminished the use of the laparoscopic treatment of this condition.7 Clinical data mostly report retrospective studies, whereas prospective trials are primarily uncontrolled,8 thereby providing a low level of evidence. In view of experimental data demonstrating the efficacy of pneumoperitoneum compared with laparotomy in experimental models of intra-abdominal sepsis,9 the laparoscopic approach to PPU is of considerable interest.
The present study reviews the current literature to identify the highest-quality studies and performs a comparative analysis of the clinical outcomes in laparoscopic and open sutured treatment of peptic ulcer perforation. A meta-analysis of randomized controlled trials was undertaken to examine the relative risks of morbidity and mortality for both the laparoscopic and open approaches.
MATERIALS AND METHODS
Study Protocol and Eligibility Criteria
An ad hoc study protocol was designed to address inclusion criteria and methods of analysis. Randomized controlled trials providing operative outcome data of laparoscopic sutured and open sutured repair of PPU were considered for inclusion. The primary outcome measure of the present meta-analysis was the relative risk of in-hospital mortality, whereas secondary outcome measures included operative morbidity, duration of surgery, postoperative pain, and length of in-hospital stay. Data sources were searched with no language or date restrictions. Only published material was included, whereas study abstracts presented in medical congresses and indexed in peer-reviewed journals were evaluated for content.
Data Sources and Study Selection
The electronic databases of the National Library of Medicine (Medline; provider Ovid, from 1966 to July 2012), Excerpta Medica (EMBASE; provider Elsevier, from 1980 to July 2012), and the Cochrane Central Register of Controlled Trials were searched to identify relevant articles. The following search terms were used: “laparoscopy (MeSH)” AND “repair OR closure” AND “gastric OR duodenal” AND “ulcer (MeSH).” Study abstracts were reviewed and full-text articles on pertinent subjects were obtained. A second-level search included the reference lists of eligible studies and the bibliography of all relevant systematic reviews. Study eligibility was assessed independently by 2 authors in an unblinded manner. Disagreements between reviewers were resolved by consensus. The last search was run on July 14, 2012.
Data Collection and Indexing
Data were independently retrieved by the 2 reviewers upon selection of studies to include in this work. For this purpose, an electronic database was developed using Microsoft Excel (Microsoft Corp, Redmond, WA) and refined accordingly. Data items extracted from each study included author, year of publication, country of origin, period of treatment, number of participating centers, number of included patients, number of patients who received treatment, number of patients for whom operative and postoperative data were available, number of patients in each treatment arm, inclusion criteria, exclusion criteria, randomization method, blinded method (if applicable), number of patients who were evaluated after treatment, male-to-female ratio, mean age, mean American Society of Anesthesiologists score, mean Boey score, type of surgery (simple repair with or without omental patch), and mean size of perforation. Outcome measures extracted from each study included duration of surgery, conversion rate, visual analog score (VAS) at 24, 48, and 72 hours after surgery, diet toleration time, absolute number of major complications, absolute number of minor complications, and duration of in-hospital stay. Major complications included suture line leakage, peritoneal abscess/collection, pancreatitis, fascial dehiscence, pneumonia or respiratory failure, and severe cardiac and cerebrovascular events. Wound infection or wound abscess, urinary tract infection, prolonged ileus, and incisional hernia were considered minor complications. If data were not reported, or were insufficient, the authors were contacted by e-mail, provided with information on the study, and invited to provide additional information. VAS at 48 and 72 hours after surgery were only provided by one study. A meta-analytical model for the continuous variables of duration of hospital stay and time to tolerate oral diet could not be applied because respective mean values were not provided.
Quality Assessment and Methods of Analysis
The Jadad score was calculated for each study to assess methodologic quality of the included trials. This 5-point scoring system takes a number of criteria into account, such as the randomization process, the blind assessment of investigated treatments, and reporting of dropouts.10 A Jadad score of 1 to 2 was considered poor quality, a score of 2 to 3 was considered fair, and a score of 4 to 5 indicated good methodologic quality.
Study-specific estimates were combined using random-effects or fixed-effects models as appropriate. Weighted mean differences with 95% confidence intervals were calculated to assess the size of the effect of each type of procedure on continuous variables. Pooled odds ratios with 95% CI were calculated to measure the effect of each type of procedure on categoric variables. Heterogeneity among trials was assessed using Cochrane's Q-statistic, a null hypothesis test with a value of P<.05 to indicate the presence of significant heterogeneity. Publication bias was assessed using Egger regression intercept. Statistical analysis was performed using Comprehensive Meta Analysis Version 2.0 (Biostat, Englewood, NJ). Statistical expertise was provided by one of the study authors. The present meta-analysis conformed to the Preferred Reporting Items for Systematic reviews and Meta-Analyses statement standards, a methodologic protocol based on essential criteria for transparent reporting.11
RESULTS
Search Results and Selection of Studies
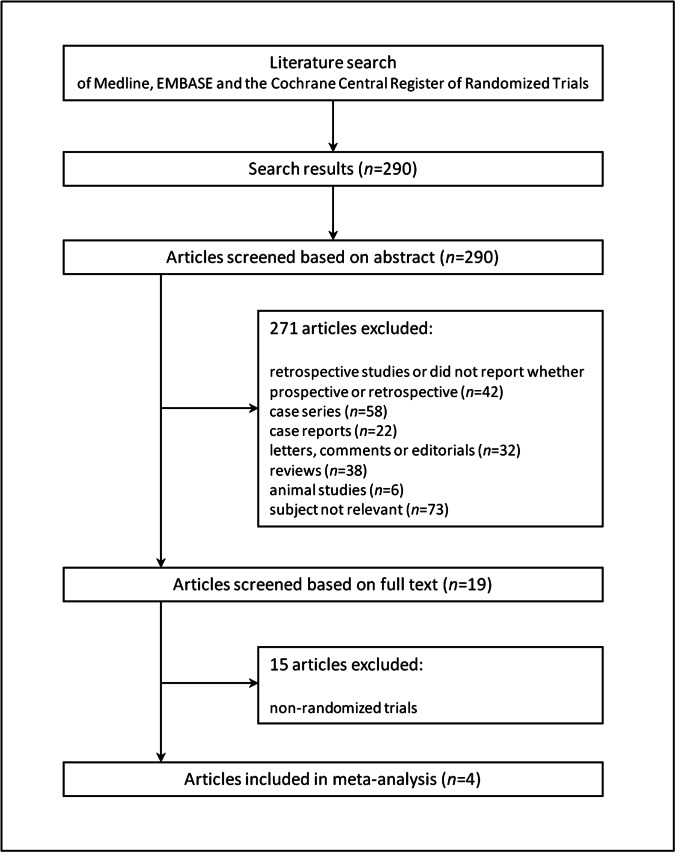
The electronic search of the databases returned 290 results (Figure 1). On the basis of the abstracts, 271 records were discarded because they were either confirmed retrospective studies or they did not report whether they were prospective or retrospective (n=42); case series (n=58); case reports (n=22); letters, comments, or editorials (n=32); reviews (n=38); animal studies (n=6); or studies with unrelated subjects (n=73). Nineteen prospective studies with a control arm were identified and their full texts retrieved. Four randomized controlled trials fulfilling the eligibility criteria were identified and included in the meta-analysis.12–15 Manual search of the reference lists reported in the included studies and relevant systematic reviews did not identify any further eligible studies.
Figure 1.
Flow chart of search history.
Characteristics of Included Studies
Table 1 reports the characteristics of the included randomized trials. All 4 studies were randomized controlled trials published in the English language between 1996 and 2009. One was a multicentric study with 9 participating centers.15 Three articles originated from China and one from the Netherlands, whereas 2 studies were designed by the same author team and reported on different study groups in distinct periods.12,13 One study focused its results on biochemical evaluation of stress-associated factors rather than on clinical outcomes.13 Nevertheless, this study was included in the analysis because it provided data on duration of surgery. Of 289 patients, 151 were included in the laparoscopic sutured repair arm and 138 in the open sutured repair arm. One study also compared the outcome of laparoscopic and open sutureless techniques, although respective data on treatments were excluded from this analysis.12 The main inclusion criteria entailed patients with the clinical diagnosis of PPU, whereas patients with bleeding ulcers and prior surgery in the upper abdomen were excluded by 3 studies. Male patients were predominant in the 3 studies that reported gender distribution, with an overall ratio of 1.5:1. The mean age was 54 years in the 2 studies reporting relevant data. In 3 studies, an omental patch was sutured on the repair site,12–14 whereas in 1 study, this was not included as a routine step for both laparoscopic and open procedures.15 Data on VAS, time to tolerate oral diet, and length of in-hospital stay could not be analyzed because several studies failed to report respective mean values or absolute numbers.
Table 1.
Characteristics of Randomized Trials
| Author | Year of Publication | Country | No. of Participating Centers | Period of Treatment | Inclusion Criteria | Exclusion Criteria | Jadad Score |
|---|---|---|---|---|---|---|---|
| Lau, et al.12 | 1996 | China | 1 | August 1992–September 1994 | Clinical diagnosis of PPU | 1. Complicated ulcer 2. Bleeding ulcer 3. Prior abdominal surgery 4. Severe cardiopulmonary disease |
3 |
| Lau et al.13 | 1998 | China | 1 | September 1995–July 1996 | Age between 17 and 69 years | 1. Bleeding ulcer 2. Immunosuppression |
2 |
| Siu et al.14 | 2002 | China | 1 | January 1994–June 1997 | 1. Clinical diagnosis of PPU 2. Age >16 years |
1. Bleeding ulcer 2. Prior abdominal surgery 3. Gastric outlet obstruction |
3 |
| Bertleff et al.15 | 2009 | The Netherlands | 9 | March 1999–July 2005 | Clinical diagnosis of PPU | 1. Prior upper abdominal surgery 2. Pregnancy |
3 |
A blinded approach was not applied in any of the studies, and one study did not specify any method of randomization.13 Hereby, 3 studies were considered to be of fair quality, with a Jadad score of 3, and 1 study was poor quality, reaching a Jadad score of only 2. All reported results adhered to the intention-to-treat concept in all studies. Data collected from patients who underwent conversion to open surgery were analyzed as data of the laparoscopic cohort.
Synthesis of Results and Outcome
Table 2 illustrates demographic data of the study populations, and Table 3 summarizes outcome measures.
Table 2.
Demographic and Operative Data of the Studied Patient Populations
| Author | No. of Patients (Lap/Open) | Age (Lap/Open) | Male-to-Female Ratio | ASA Score (Lap/Open) | Boey Score (Lap/Open) | Size of Perforation (mm) (Lap/Open) | Omental Patch | Conversion Rate |
|---|---|---|---|---|---|---|---|---|
| Lau et al.12 | 45 (24/21) | 52 (52/53) | 4.6:1 | NR | 0.27 (0.29/0.24) | NR (6 mm/5 mm) | Yes | 25% (6/24) |
| Lau et al.13 | 22 (12/10) | NR | NR | NR | NR | NR | Yes | 25% (3/12) |
| Siu et al.14 | 121 (63/58) | 55 (54/56) | 4.3:1 | 1.72 (1.7/1.7) | 0.28 (0.24/0.33) | 5.0 (5.2/4.7) | Yes | 14% (9/63) |
| Bertleff et al.15 | 101 (52/49) | NR (66/59)* | 1.5:1 | NR (1.0/1.5)* | NR | NR (10.0/7.0)* | Mixed cases | 8% (4/52) |
NR, not reported; ASA, American Society of Anesthesiologists; lap, laparoscopic.
Numerical data are reported as mean values, unless otherwise indicated.
Median values.
Table 3.
Summary Data of Outcome Measures
| Author | Operative Time (Min) (Lap/Open) | VAS† (Lap/Open) | Days After Surgery to Tolerate Oral Diet (Lap/Open) | Minor Complications, (Lap/Open), n (%) | Major Complications (Lap/Open), n (%) | Reoperation, (Lap/Open), n (%) | Duration of In-Hospital Stay (d) (Lap/Open) | Mortality (Lap/Open), n (%) |
|---|---|---|---|---|---|---|---|---|
| Lau et al.12 | 87 (113/57) | NR (4/5)* | NR (4/4)* | 2/4 (8/19) | 2/1 (8/5) | 0/1 (0/5) | NR (5/5)* | 0/1 (0/5) |
| Lau et al.13 | NR (96/35)* | NR | NR | NR | NR | NR | NR | NR |
| Siu et al.14 | 47 (42/52) | 4.9 (3.5/6.4) | NR (4/5)* | 7/14 (11/24) | 3/8 (5/14) | 5/1 (8/5) | NR (6/7)* | 1/3 (2/5) |
| Bertleff et al.15 | NR (75/50)* | (3.8/5.2)* | NR | NR | NR | NR | NR (6.5/8)* | 2/4 (4/8) |
n, absolute number; NR, not reported; lap, laparoscopic.
Numerical data are reported as mean values, unless otherwise indicated.
Median values.
24 hours after surgery.
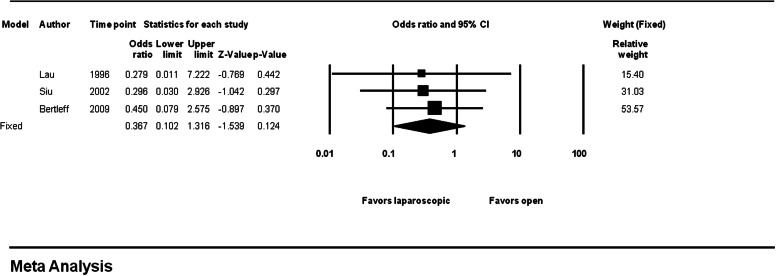
Mortality
There were 3 deaths in the laparoscopic group and 8 deaths in the open group, giving rates of 2% and 6%, respectively (OR 0.36, 95% CI 0.10–1.32, P=.124). There was no evidence of between-study heterogeneity (P=.945) (Figure 2).
Figure 2.
Forest plot of mortality for laparoscopic and open repair of perforated ulcer.
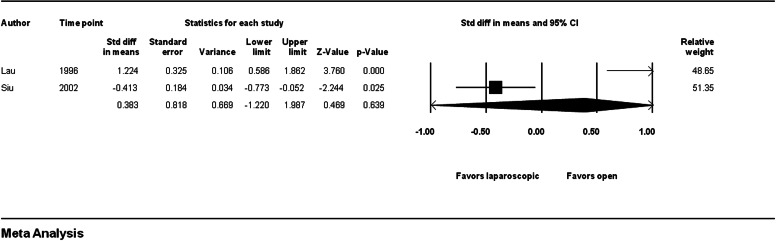
Operative Time
Mean duration of surgery was 62 minutes for the laparoscopic group and 53 minutes for the open group (weighted mean difference 0.38, 95% CI 1.22–1.99, P= .639). There was significant evidence of between-study heterogeneity (P<.001) (Figure 3).
Figure 3.
Forest plot of operative time for laparoscopic and open repair of perforated ulcer.
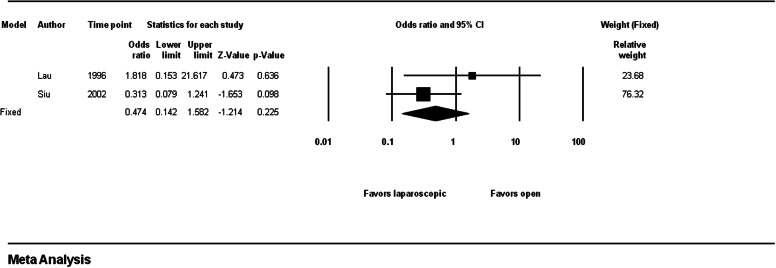
Major Complications
Incidence of major complications was 6% in the laparoscopic group and 11% in the open surgery group (OR 0.47, 95% CI 0.14–1.58, P=.225). The level of between-study heterogeneity was low (P=.223) (Figure 4).
Figure 4.
Forest plot of major complications for laparoscopic and open repair of perforated ulcer.
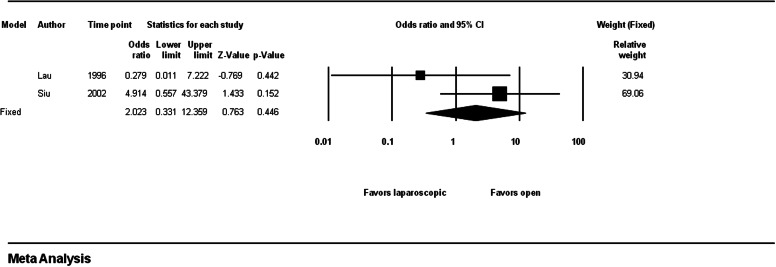
Reoperation
One percent of patients of the laparoscopic group and 8% of patients of the open group underwent repeated surgery (OR 2.02, 95% CI 0.33–12.36, P=.446). Between-study heterogeneity was low (P=.151) (Figure 5).
Figure 5.
Forest plot of rate of reoperation for laparoscopic and open repair of perforated ulcer.
DISCUSSION
The present meta-analysis does not support favorable outcomes for minimally invasive treatment of PPU over its open surgery counterpart, as reported in the currently studied variables. Several limitations have to be taken into account to evaluate these results. Our literature search identified only 4 randomized trials. Three of these studies were of fair methodologic quality, whereas the rest failed to provide adequate data for statistical evaluation. The cumulative study population was low, and the strength of the analysis was therefore limited.
The set of available data demonstrated homogeneous results for the outcome variables of mortality, complications, and reoperation rate. All studies adhered to the intention-to-treat principle, thereby rendering the outcome for laparoscopic repair more reliable. Statistical significance could not be reached for any of these variables, although odd ratios were consistently in favor of the laparoscopic repair, suggesting a potential type II statistical error. Similarly, the laparoscopic approach resulted in a lower rate of minor complications (10% vs 23%, data not shown). These results are consistent with a meta-analytical approach of nonrandomized trials, which may reflect the standard health care delivery setting.8
Early evidence from prospective studies demonstrated longer operating times for laparoscopic repair of PPU. Two randomized studies provided relevant data, which were contradictory, however. Longer duration of surgery was reported by Lau et al12 in their trial conducted between 1992 and 1994, whereas a significantly reduced mean operating time was demonstrated in a more recent study by Siu et al,14 which introduced substantial heterogeneity into the analysis. It has been suggested that acquaintance with the laparoscopic concept and laparoscopic suturing skills may result in a reduction in the duration of surgery over time.8 A prospective analysis of more than 100 cases of laparoscopic treatment of PPU performed by surgical trainees has reported an acceptable mean operating time of 65 minutes, although most the study population consisted of low-risk patients.16 Peritoneal lavage is a factor of prolonged duration of surgery, although this has now been replaced with high-volume irrigation systems.8,17
Open repair of PPU remains the gold-standard treatment. It is simple and effective and provides long-term regression of the disease when combined with eradication of H pylori and recess of nonsteroidal anti-inflammatory medication.18,19 In these patients, mortality is frequently associated with underlying sepsis and inflammatory response, which correlates with patient risk factors rather than surgical complications.20 Considering the mitigated inflammatory reaction after elective laparoscopic procedures or laparoscopy for perforated appendicitis,21,22 a minimally invasive approach to this emergency condition seems appealing. Outcomes of 3 randomized trials on in-hospital mortality were consistently favorable of the laparoscopic approach, although statistical significance could not be reached. The maximum relative weight was provided by the study by Bertleff et al,15 which reported a higher peritonitis index for the laparoscopic cohort. Although there is evidence suggesting a decreased amount of operative stress in patients with peritonitis undergoing laparoscopic surgery, the true benefit of laparoscopic repair in specific patients remains to be identified. Centers with adequate experience and a community-based evaluation of laparoscopic repair of PPU have recognized old age, poor anesthesiologic status, and delayed presentation as predictive factors for mortality.23–25 Comparative data on laparoscopic and open repair of PPU in patients stratified according to risk factors as ASA score and Boey score are still unavailable.
Systemic and procedure-related complications are a matter of concern in septic patients undergoing upper abdominal surgery. The theoretic advantage of laparoscopic treatment in terms of morbidity cannot be confirmed in the present analysis. The largest available randomized trial, which enrolled more than 100 patients, demonstrated a lower morbidity rate for the laparoscopic approach (5% vs 14%), but the data were not statistically significant.14 This finding correlates with a cumulative evaluation of prospective and retrospective studies in 2005.8 Because half of the studies included in this analysis were published before 2000, when laparoscopy experience was still limited, evaluation of surgery-related morbidity in the modern era of laparoscopy is a field for future investigation. Suture-site leakage is still an issue, and concerns have been raised regarding laparoscopic suturing of friable ulcer edges. An analysis of risk factors found that 84% of patients with a history of symptoms lasting longer than 9 hours developed leakage after laparoscopic repair.26 Nevertheless, high-quality comparative data of laparoscopic and open repair with regard to suture failure and intra-abdominal abscess are not available.
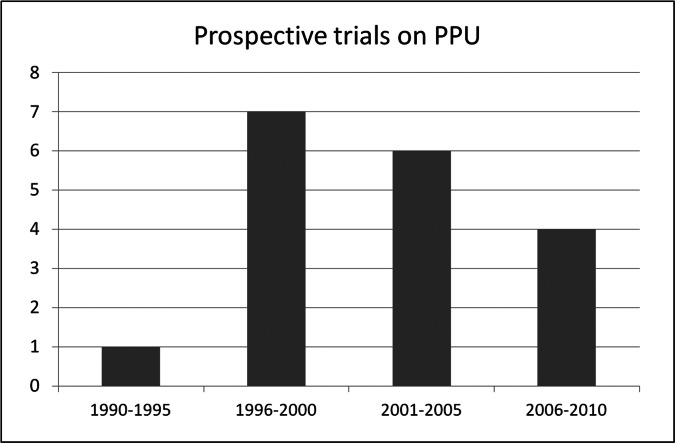
Although the laparoscopic approach to PPU may offer significant advantages over open repair with regard to postoperative morbidity and mortality, the evidence of its efficacy is still inconclusive. A population-based study from China reported an increase in the frequency of laparoscopic repair of PPU.27 Interestingly, our literature review has retrieved a decreasing number of published prospective trials from 1996 to date (Figure 6). In view of the low incidence of ulcer perforation, interinstitutional collaboration is strongly recommended to evaluate the effect of laparoscopic repair of PPU on the setting of a randomized study.
Figure 6.
Absolute numbers of prospective studies on laparoscopic treatment of PPU published from 1990 to 2010.
Current evidence does not clearly demonstrate the advantages of laparoscopic versus open repair of PPU for any of the examined outcome measures. Growing interest in the laparoscopic approach may encourage the design of additional randomized trials to analyze its efficacy compared with the open approach.
Contributor Information
Stavros A. Antoniou, Center for Minimally Invasive Surgery, Hospital Neuwerk, Mönchengladbach, Germany..
George A. Antoniou, Department of Vascular and Endovascular Surgery, Manchester Royal Infirmary, Central Manchester University Hospitals NHS Foundation Trust, Manchester, UK..
Oliver O. Koch, Department of General Surgery, Hospital Zell am See, Zell am See, Austria..
Rudolph Pointner, Department of General Surgery, Hospital Zell am See, Zell am See, Austria..
Frank A. Granderath, Center for Minimally Invasive Surgery, Hospital Neuwerk, Mönchengladbach, Germany..
References:
- 1. Nathanson LK, Easter WT, Cushieri A. Laparoscopic repair/peritoneal toilet of perforated duodenal ulcer. Surg Endosc. 1990;4:232–233 [DOI] [PubMed] [Google Scholar]
- 2. Mouret P, François Y, Vignal J, Barth X, Lombard-Platet R. Laparoscopic treatment of perforated peptic ulcer. Br J Surg. 1990;77:1006. [DOI] [PubMed] [Google Scholar]
- 3. Coghlan JG, Gilligan D, Humphries H, et al. Campylobacter pylori and recurrence of duodenal ulcers—a 12-month follow-up study. Lancet. 1987;2:1109–1111 [DOI] [PubMed] [Google Scholar]
- 4. Bhogal RH, Athwal R, Durkin D, Deakin M, Cheruvu CN. Comparison between open and laparoscopic repair of perforated peptic ulcer disease. World J Surg. 2008;32:2371–2374 [DOI] [PubMed] [Google Scholar]
- 5. Ates M, Sevil S, Bakircioglu E, Colak C. Laparoscopic repair of peptic ulcer perforation without omental patch versus conventional open repair. J Laparoendosc Adv Surg Tech. 2007;17:615–619 [DOI] [PubMed] [Google Scholar]
- 6. Lau WY, Leung KL, Zhu XL, Lam YH, Chung SC, Li AK. Laparoscopic repair of perforated peptic ulcer. Br J Surg. 1995;82:814–816 [DOI] [PubMed] [Google Scholar]
- 7. Bashinskaya B, Nahed BV, Redjal N, Kahle KT, Walcott BP. Trends in peptic ulcer disease and the identification of Helicobacter pylori as a causative organism: Population-based estimates from the US nationwide inpatient sample. J Glob Infect Dis. 2011;3:366–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lunevicius R, Morkevicius M. Systematic review comparing laparoscopic and open repair for perforated peptic ulcer. Br J Surg. 2005;92:1195–1207 [DOI] [PubMed] [Google Scholar]
- 9. Karantonis FF, Nikiteas N, Perrea D, et al. Evaluation of the effects of laparotomy and laparoscopy on the immune system in intra-abdominal sepsis–a review. J Invest Surg. 2008;21:330–339 [DOI] [PubMed] [Google Scholar]
- 10. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12 [DOI] [PubMed] [Google Scholar]
- 11. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lau WY, Leung KL, Kwong KH, et al. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. 1996;224:131–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lau JY, Lo SY, Ng EK, Lee DW, Lam YH, Chung SC. A randomized comparison of acute phase response and endotoxemia in patients with perforated peptic ulcers receiving laparoscopic or open patch repair. Am J Surg. 1998;175:325–327 [DOI] [PubMed] [Google Scholar]
- 14. Siu WT, Leong HT, Law BK, et al. Laparoscopic repair for perforated peptic ulcer: A randomized controlled trial. Ann Surg. 2002;235:313–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bertleff MJ, Halm JA, Bemelman WA, et al. Randomized clinical trial of laparoscopic versus open repair of the perforated peptic ulcer: the LAMA Trial. World J Surg. 2009;33:1368–1373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Siu WT, Chau CH, Law BK, Tang CN, Ha PY, Li MK. Routine use of laparoscopic repair for perforated peptic ulcer. Br J Surg. 2004;91:481–484 [DOI] [PubMed] [Google Scholar]
- 17. Lagoo S, McMahon RL, Kahikara M, Pappas TN, Eubanks S. The sixth decision regarding perforated duodenal ulcer. JSLS. 2002;6:359–368 [PMC free article] [PubMed] [Google Scholar]
- 18. Ng EK, Lam YH, Sung JJ, et al. Eradication of Helicobacter pylori prevents recurrence of ulcer after simple closure of duodenal ulcer perforation: Randomized controlled trial. Ann Surg. 2000;231:153–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tomtitchong P, Siribumrungwong B, Vilaichone RK, Kasetsuwan P, Matsukura N, Chaiyakunapruk N. Systematic review and meta-analysis: Helicobacter pylori eradication therapy after simple closure of perforated duodenal ulcer. Helicobacter. 2012;17:148–152 [DOI] [PubMed] [Google Scholar]
- 20. Boey J, Choi SK, Poon A, Alagaratnam TT. Risk stratification in perforated duodenal ulcers. A prospective validation of predictive factors. Ann Surg. 1987;205:22–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sammour T, Kahokehr A, Chan S, Booth RJ, Hill AG. The humoral response after laparoscopic versus open colorectal surgery: A meta-analysis. J Surg Res. 2010;164:28–37 [DOI] [PubMed] [Google Scholar]
- 22. Schietroma M, Piccione F, Carlei F, et al. Peritonitis from perforated appendicitis: stress response after laparoscopic or open treatment. Am Surg. 2012;78:582–590 [PubMed] [Google Scholar]
- 23. Druart ML, Van Hee R, Etienne J, et al. Laparoscopic repair of perforated duodenal ulcer. A prospective multicenter clinical trial. Surg Endosc. 1997;11:1017–1020 [DOI] [PubMed] [Google Scholar]
- 24. Wong DC, Siu WT, Wong SK, Tai YP, Li MK. Routine laparoscopic single-stitch omental patch repair for perforated peptic ulcer: Experience from 338 cases. Surg Endosc. 2009;23:457–458 [DOI] [PubMed] [Google Scholar]
- 25. Kuwabara K, Matsuda S, Fushimi K, Ishikawa KB, Horiguchi H, Fujimori K. Community-based evaluation of laparoscopic versus open simple closure of perforated peptic ulcers. World J Surg. 2011;35:2485–2492 [DOI] [PubMed] [Google Scholar]
- 26. Lunevicius R, Morkevicius M. Risk factors influencing the early outcome results after laparoscopic repair of perforated duodenal ulcer and their predictive value. Langenbecks Arch Surg. 2005;390:413–420 [DOI] [PubMed] [Google Scholar]
- 27. Lam CM, Yuen AW, Chik B, Wai AC, Fan ST. Laparoscopic surgery for common surgical emergencies: A population-based study. Surg Endosc. 2005;19:774–779 [DOI] [PubMed] [Google Scholar]