Abstract
Background
More than 25% of Medicare patients hospitalized for heart failure are readmitted within 30 days. The contributions of numeracy and health literacy to recidivism for patients with acute heart failure (AHF) are not known.
Methods and Results
A cohort of patients with AHF who presented to four emergency departments between January 2008 and September 2011. Research assistants administered subjective measures of numeracy and health literacy; thirty-day follow up was performed by phone interview. Recidivism was defined as any unplanned return to the emergency department or hospital within 30-days of the index emergency department visit for AHF. Multivariable logistic regression adjusting for patient age, gender, race, insurance status, hospital site, days eligible for recidivism, chronic kidney disease, abnormal hemoglobin, and low ejection fraction evaluated the relationships between numeracy and health literacy with 30-day recidivism. Of the 709 patients included in the analysis, 390 (55%) had low numeracy skills and 258 (37%) had low literacy skills. Low numeracy was associated with increased odds of recidivism within 30 days (adjusted odds ratio (OR) 1.41, 95% confidence interval 1.00-1.98, P=0.048). For low health literacy, adjusted OR of recidivism was 1.17 (95% CI 0.83-1.65, P=0.37).
Conclusions
Low numeracy was associated with greater odds of 30-day recidivism. Further investigation is warranted to determine whether addressing numeracy and health literacy may reduce 30-day recidivism for patients with acute heart failure.
Keywords: emergency, heart failure, heart failure readmission follow-up studies
Health literacy, or “the degree to which individuals can obtain, process, and understand basic health information and services needed to make appropriate health decisions,”1 and numeracy2, or “the ability to use and understand numbers in daily life,”3 are key elements of disease self-management. Unfortunately, low numeracy and health literacy are common1,4-7, associated with worse health outcomes8, and costly9, accounting for up to 5% of health care costs annually10. Furthermore, healthcare providers are often unaware of their patients’ low literacy levels11, 12.
Heart failure is a common cause of hospital admission and is associated with frequent rehospitalizations13-15. Estimated US costs exceeded $39 billion in 201016, much of it due to emergency department visits and hospitalizations13, 17. Hospitalization for acute heart failure represents an important inflection point in a patient’s clinical course. More than 25% of patients admitted for heart failure are readmitted to the hospital within 30 days and importantly, many readmissions are for non-heart failure related causes13. In addition, mortality increases with each subsequent re-hospitalization; median survival is 2.5 years after a first hospitalization and 6 months after a fourth hospitalization18, 19. Identifying factors associated with recidivism, or recurrent emergency department visits and unplanned hospitalizations, is an important step toward improving outcomes for patients with acute heart failure.
Previous small and retrospective studies suggest that patients with chronic heart failure and low health literacy may be at higher risk for emergency care, hospitalization, and death20-22. However, the relationships between numeracy and health literacy with recidivism after an episode of acute heart failure are not well understood. Therefore, the goal of this study was to evaluate the relationship between both numeracy and health literacy with 30-day recidivism, defined as an emergency department visit or unplanned hospitalization, after an acute heart failure-associated emergency department visit. We hypothesized that lower numeracy and health literacy would both be associated with greater odds of recidivism.
Methods
We conducted a multicenter, prospective cohort study of adult patients who presented to four hospital-based emergency departments with acute heart failure between January 2008 and September 2011. Patients with a clinical diagnosis of acute heart failure who were able to provide informed consent and who completed assessments of numeracy or health literacy were eligible for inclusion. This study was approved by each of the four local institutional review boards.
Study Population
All patients greater than 18 years of age who presented to the emergency department were screened for dyspnea, cough, and acute pulmonary edema. Treating physicians then determined whether potentially eligible patients met additional clinical criteria for acute heart failure based on the modified Framingham criteria (Table 123, 24). Patients who passed both screens and who could be enrolled within three hours of first physician contact were approached for consent. After consent, research assistants administered numeracy and health literacy scales25-29; they then collected detailed sociodemographic and medical history data, which was verified by medical record review. The results of the numeracy and health literacy screen were not provided to the patient or providers. Patients who received a clinical diagnosis of acute heart failure by treating physicians were included in the analysis. Patients meeting the following criteria were excluded: initiation of palliative care during the 30-day follow-up period; hospital admission for the entire follow-up period; and unknown date of death. Patients with an unknown date of death were excluded because it was unknown whether these patients had an opportunity to experience recidivism.
Table 1.
Cohort Inclusion Criteria: Modified Framingham Criteria
| Major Criteria | Minor Criteria |
|---|---|
| History of heart failure | Extremity edema |
| Paroxysmal nocturnal dyspnea | Night cough |
| Pulmonary interstitial edema on CXR | Dyspnea on exertion |
| Rales | Hepatomegaly |
| Cardiomegaly | Pleural effusion |
| S3 gallop | Tachycardia ≥130 bpm |
| Jugular venous distension | |
| Positive hepatojugular reflex |
2 Major or 1 Major and 2 Minor Criteria are required to establish a preliminary diagnosis of heart failure by the Framingham criteria.
Data collection
Patients were enrolled as convenience samples at four hospitals: two tertiary care hospitals with approximately 55,000 and 90,000 annual adult emergency department visits (Hospital 1 and 2, respectively), and two community hospitals with approximately 33,000 and 47,000 annual adult emergency department visits (Hospital 3 and 4, respectively). Hospital 1, 3, and 4 enrolled patients 16 hours a day, seven days a week; Hospital 2 enrolled patients 24 hours a day, seven days a week. Study data were collected and managed using Research Electronic Data Capture (REDcap) tools30.
Numeracy and Health Literacy
We used two validated instruments to measure numeracy and health literacy. The subjective numeracy scale27, 28 and the subjective health literacy scale26 assess numeracy and health literacy, respectively, by asking subjects about their perceived abilities and attitudes related to numeracy and health literacy. These scales have been validated against objective measures of literacy and numeracy, including the Short Test of Functional Health Literacy in Adults (S-TOFHLA) and the Rapid Estimate of Adult Literacy in Medicine (REALM)25, 26, and the Wide Range Achievement Test Mathematical subtest (WRAT-4)27, 28, respectively. Additionally, the numeracy scale and the health literacy scale were validated in a general adult emergency department population and were shown to add information above and beyond patient demographics and level of education29.
The numeracy scale consists of eight written items on a 6-point Likert-like scale, four regarding perceived skills using numbers, and four addressing preferences regarding the use of numbers (Table 2)27, 28. On a scale from 8 to 48, higher scores indicated higher subjective numeracy skills. In a previous study of a general adult emergency department patient population, this numeracy scale had a Cronbach’s alpha of 0.8229. The health literacy scale consists of three oral items on a 5-point Likert–like scale addressing patient perceptions regarding their health literacy (Table 2)26. On a scale from 3 to 15, higher scores indicated higher subjective health literacy skills. This health literacy scale demonstrated a Cronbach’s alpha of 0.74 in a general emergency department population29.
Table 2.
| Subjective Numeracy Scale | How good are you at working with fractions? |
| How good are you at working with percentages? | |
| How good are you at calculating a 15% tip? | |
| How good are you at figuring out how much a shirt will cost if it is 25% off? | |
| When reading the newspaper, how helpful do you find tables and graphs that are parts of a story? | |
| When people tell you the chance of something happening, do you prefer that they use words or numbers? | |
| When you hear a weather forecast, do you prefer predictions using percentages or predictions using only words? | |
| How often do you find numerical information to be useful? | |
|
| |
| Subjective Health Literacy Scale | How often do you have problems learning about your medical condition because of difficulty understanding written information? |
| How confident are you filling out medical forms by yourself? | |
| How often do you have someone help you read hospital materials? | |
Measures of Recidivism
Patients were contacted by phone 30 days after the initial emergency department visit for acute heart failure. Outcomes were obtained by patient or caregiver report, with confirmation by review of medical records and the Social Security Death Index. The primary outcome was 30-day recidivism, defined as ≥ 1 emergency department visit or unplanned hospitalization for any cause within 30 days of the index emergency department visit.
Statistical Analysis
Descriptive statistics are presented as medians and interquartile ranges (IQR) or frequency and percentages. Demographics were compared using the Chi-square test, Fisher’s exact test, or Wilcoxon’s rank sum test, as appropriate. Unadjusted and adjusted logistic regression with 95% confidence intervals (CIs) was used to evaluate the associations between numeracy and health literacy with 30-day recidivism. Thirty-day recidivism was examined as a dichotomous outcome; one or more recidivism events within the 30-day follow-up period were categorized as positive, while no recidivism in the follow-up period was categorized as negative. For patients with any missing component of the recidivism outcome, the missing components were conservatively coded as negative if the status of recidivism was unclear. Numeracy and health literacy are related but unique skills, with only moderate correlation 29; therefore, numeracy and health literacy were evaluated in separate regression models. Planned secondary analysis evaluated these scales dichotomized to indicate low numeracy and low health literacy. Because the prevalence of low numeracy and health literacy varies among different patient populations, cut points on the scales indicating skill levels (inadequate, marginal, adequate) have not been firmly established. For the purposes of this study and based on the sensitivity and specificity of these tests in a general emergency department population, low numeracy was defined as a score less than 34, or approximately high school numeracy level on the WRAT-4; low health literacy was defined as a health literacy score less than 12, or approximately a high school reading level as measured by the S-TOFHLA. In these analyses, continuous numeracy and health literacy scores were reversed so that higher scores indicated decreasing numeracy and health literacy skills. Values for missing data on the numeracy or health literacy scales were imputed as the mean score of the completed items.
The number of predictors was limited by the general rule of thumb allowing 15 events per predictor degree of freedom31, 32. Covariates thought to reflect healthcare access, disease severity, and resource utilization in patients with heart failure were determined a priori based on review of existing literature and clinical judgment, including age, gender, race, insurance status, history of chronic kidney disease, abnormal hemoglobin on presentation (less than 13 g/dL or greater than or equal to 17 g/dL), and ejection fraction (EF) less than 30%33-35. Hospital site was also included in the model. The maximum number of days patients were eligible for recidivism was also included as a covariate and was defined as the number of days within the 30-day follow-up period that patients were alive and not admitted to the hospital and therefore were at risk for recidivism. Local polynomial smoothed lines with 95% CI were used to generate figures illustrating the relationships between numeracy and health literacy with predicted probability of 30-day recidivism, based on the adjusted multiple logistic regression models. In these figures, higher numeracy and health literacy scores indicate higher numeracy and health literacy skills. Previously, a small subset of this data was analyzed to evaluate whether numeracy or health literacy were associated with a composite outcome of prolonged hospitalization, death, and recidivism within 30 days; because of the exploratory nature of our analysis, no adjustment for Type I error was made for this analysis. A p value less than 0.05 was considered statistically significant. All analyses were performed using Stata/IC 11.2 (Copyright © 2009, College Station, TX, USA).
Results
Among the four study hospitals, 737 patients were enrolled (Figure 1); of these, 28 patients were excluded, including five who were admitted to the hospital for the duration of the follow up period, 16 who were placed on palliative care, and seven who died but the date of death was missing, leaving 709 patients in the analysis. Enrollment at each participating hospital included 303 subjects at Hospital 1, 108 subjects at Hospital 2, 10 at Hospital 3, and 288 at Hospital 4. The follow-up rate at 30 days was 98%; two subjects had incomplete data for the primary composite outcome and were included in the analysis as not having experienced recidivism. Clinical characteristics of subjects, comparing those who experienced recidivism within 30 days against those who did not, are found in Table 3. Details regarding clinical outcomes are found in Table 4.
Figure 1.
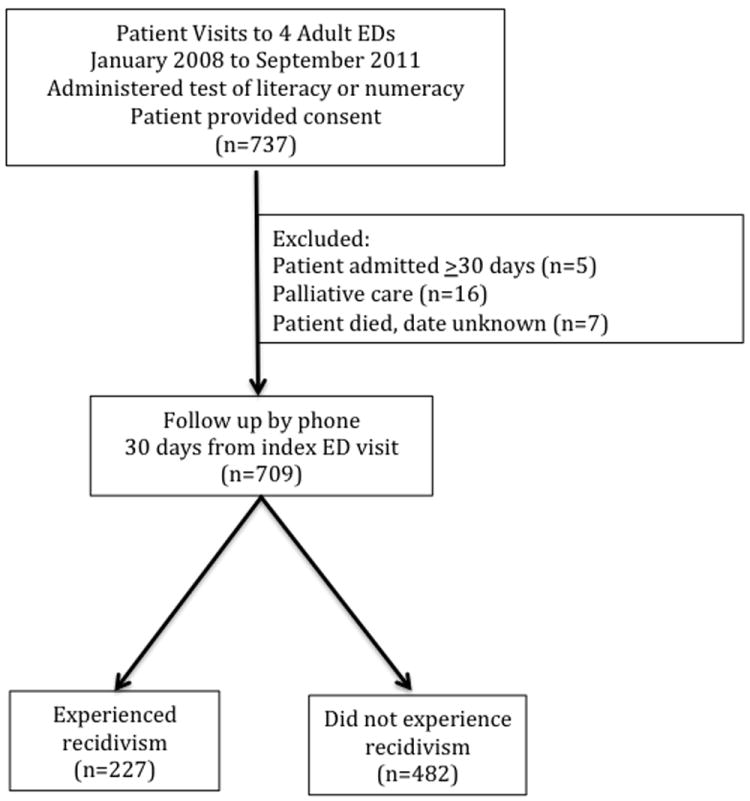
Inclusion and Exclusion Criteria
Table 3.
Clinical Characteristics
| Experienced Recidivism (n=227) | Did Not Experience Recidivism (n=482) | P | |
|---|---|---|---|
| Demographic | |||
| Age, median years (IQR) | 60 (52-71) | 62 (52-72) | 0.50 |
| Men, No. (%) | 136 (60) | 262 (54) | 0.17 |
| White, No. (%) | 113 (50) | 262 (54) | 0.26 |
| Insurance status | |||
| Private/Group, No. (%) | 54 (24) | 128 (27) | 0.10 |
| Federal or State Insurance, No. (%) | 151 (66) | 293 (61) | |
| Self-pay, No. (%) | 22 (10) | 60 (12) | |
| Education | |||
| ≤High School, No. (%) | 165 (74) | 296 (62) | 0.02 |
| College, No. (%) | 48 (21) | 134 (28) | |
| Post Graduate, No.(%) | 12 (5) | 49 (10) | |
| Clinical | |||
| Chronic Kidney Disease, No. (%) | 73 (32) | 83 (17) | <0.001 |
| Hgb<13 or ≥17, No. (%) | 154 (68) | 268 (56) | 0.002 |
| EF<30%, No. (%) | 52 (23) | 129 (27) | 0.49 |
| Numeracy | |||
| Subjective Numeracy, median (IQR) | 30 (22-36) | 32 (24-39) | 0.02 |
| Low Subjective Numeracy, No. (%) | 138 (61) | 252 (52) | 0.04 |
| Literacy | |||
| Subjective Literacy, median (IQR) | 13 (9-15) | 13 (10-15) | 0.06 |
| Low Subjective Literacy, No. (%) | 92 (41) | 166 (35) | 0.13 |
| Disposition | |||
| Discharged from the ED, No. (%) | 17 (8) | 30 (6) | 0.52 |
| Days admitted, median (IQR) | 3 (1-5) | 3 (2-5) | 0.44 |
Abbreviations: IQR, interquartile range; No., number; Hgb, hemoglobin; EF, ejection fraction; ED, emergency department
Table 4.
Outcomes, by recidivism type (n=709)
| Any Outcome, No. (%) | 227 (32) |
| ED visit, for AHF, No. (%) | 62 (9) |
| ED visit, not for AHF, No. (%) | 163 (23) |
| Unscheduled hospitalization, for AHF, No. (%) | 59 (3) |
| Unscheduled hospitalization, not for AHF, No. (%) | 121 (17) |
| Subjects with any unverified outcomes | 4 (0.6) |
Abbreviations: No., number; ED, emergency department; AHF, acute heart failure
Overall, 668 subjects took both the numeracy and literacy scales, 35 took only the health literacy scale, and six took only the numeracy scale. Twenty-five subjects left one item blank on either the numeracy or health literacy scale and the missing values were imputed as the mean score of the completed items. Three hundred ninety (55%) of patients had low numeracy skills, or a numeracy score less than 34, and 258 (38%) had low health literacy skills, or a health literacy score less than 12. Two hundred twenty-seven (32%) patients experienced at least one recidivism event; of these 62 (9%) returned to the emergency department for acute heart failure and 59 (8%) were admitted for acute heart failure. The remaining 155 patients experienced recidivism for conditions other than acute heart failure, including dyspnea not caused by acute heart failure (23%), chest pain (13%), other cardiovascular complaints (15%), infection (11%), complications related to other comorbid conditions (19%), and fall or trauma (6%).
Results of the regression analyses are found in Table 5. For patients with low numeracy, the adjusted odds ratio (OR) of recidivism within 30 days was 1.41 (95% confidence interval (CI) 1.00-1.98, P = 0.048); for patients with low health literacy, the adjusted OR of recidivism within 30 days was 1.17 (95% CI 0.83-1.65, P = 0.37). Per point decrease on the 41-point health numeracy scale, the adjusted OR of 30-day recidivism was 1.02 (95% CI 1.00-1.04, P = 0.04). Per point decrease on the 13-point health literacy scale, the adjusted OR of 30-day recidivism was 1.05 (95% CI 1.00-1.10, P = 0.05). Figure 2 and Figure 3 illustrate the relationships between predicted 30-day recidivism and numeracy and health literacy, respectively.
Table 5.
Odds of Experiencing Emergency Department or Hospital Recidivism with 30 days for Adult Emergency Department Patients with Acute Heart Failure, by Decreasing Subjective Numeracy and Subjective Health Literacy*
| Unadjusted OR (95% CI) | P | Adjusted OR (95% CI)+ | P | |
|---|---|---|---|---|
| Numeracy (n=674) | 1.02 (1.00-1.04) | 0.013 | 1.02 (1.01-1.04) | 0.037 |
| Low Numeracy (n=674) | 1.42 (1.03-1.95) | 0.034 | 1.41 (1.00-1.98) | 0.048 |
| Health Literacy (n=702) | 1.06 (1.01-1.11) | 0.011 | 1.05 (1.00-1.10) | 0.052 |
| Low Health Literacy (n=702) | 1.29 (0.93-1.78) | 0.129 | 1.17 (0.83-1.65) | 0.371 |
Abbreviations: OR, odds ratio; CI, confidence interval
Numeracy and health literacy scores were reverse scored, thus OR is per unit decrease in numeracy and health literacy skills
Adjusted for age, gender, race, insurance, presence of diabetes, chronic kidney disease, abnormal hemoglobin, low ejection fraction, study site, and maximum number of days known to be eligible for recidivism
Figure 2.
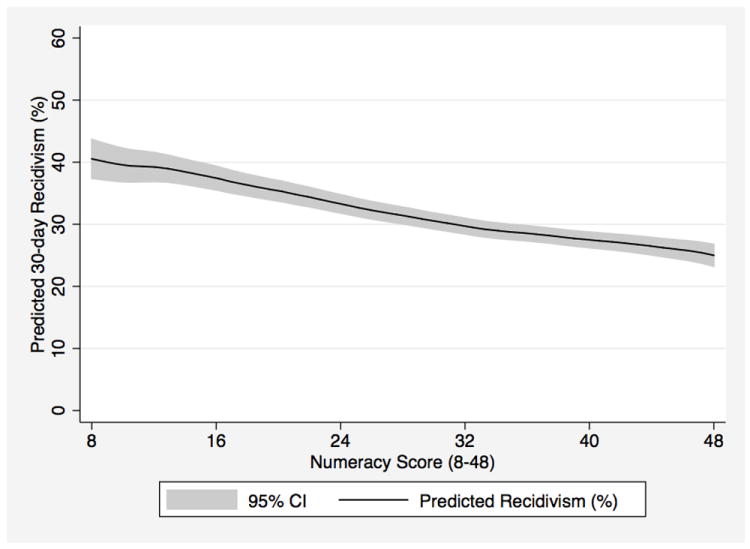
Numeracy and Predicted 30-day Emergency Department and Hospital Recidivism*, n=673
* Adjusted for age, gender, race, insurance, presence of diabetes, chronic kidney disease, abnormal hemoglobin, low ejection fraction, study site, and maximum number of days known to be eligible for recidivism; higher Numeracy Scores indicate higher numeracy skills
Figure 3.
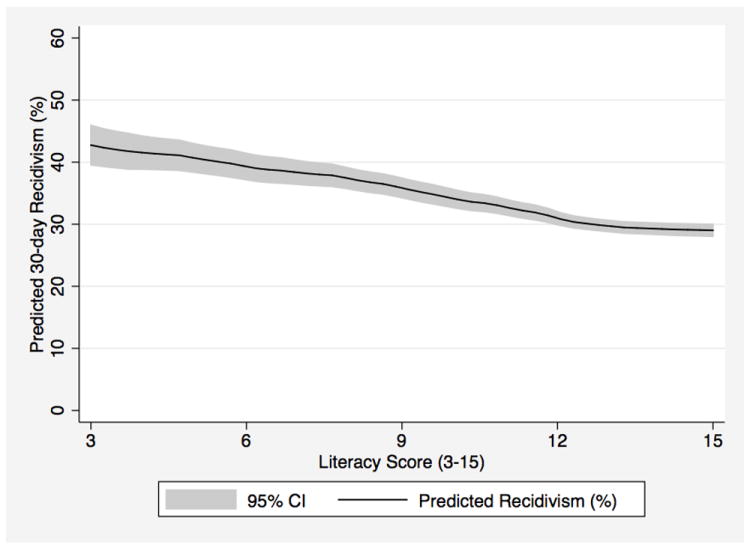
Literacy and Predicted 30-day Emergency Department and Hospital Recidivism*, n=702
* Adjusted for age, gender, race, insurance, presence of diabetes, chronic kidney disease, abnormal hemoglobin, low ejection fraction, study site, and maximum number of days known to be eligible for recidivism; higher Literacy Scores indicate higher health literacy skills
Discussion
To our knowledge, this is the first large, multi-center, prospective study of a diverse patient population to show that numeracy is associated with 30-day recidivism for patients with acute heart failure.
An 8-point decrease on the numeracy scale, or a 1-point change on each of the 8 questions, would be expected to confer 16% higher odds of experiencing recidivism. Thus, while the magnitude of association between numeracy and recidivism may appear small per point on the scale, the differences between individuals are significant, as are the disparities on a population level. Annually, more than $17 billion is spent on heart failure in the US, much of it due to costs associated with rehospitalizations13. An intervention addressing numeracy may reduce rehospitalizations and should be tested to evaluate its impact on costs associated with heart failure.
Approximately 55% of patients in this study had low numeracy skills, and 37% had low health literacy skills. This is similar prior to research, in which 36% of the general population had basic or below-basic health literacy skills36, and after pooling multiple studies, 26% of patients had low health literacy37. The ability to determine which of two quantities is larger is considered a basic numeracy skill, and finding values on a table is considered an intermediate numeracy skill38. Patients with heart failure are expected to weigh themselves daily, monitor sodium intake, and in some cases titrate diuretics to adjust for water weight gain. These patients often have multiple comorbidities and take multiple medications requiring titration. The ability to use and understand numbers is a necessary component of effective disease self-management, and it may outweigh the importance of general health literacy for diseases that require relatively complex mathematical skills for disease self-management.
It is noteworthy that many of the return emergency department visits and unscheduled hospitalizations were not directly related to acute heart failure. These findings are similar to prior research in which acute heart failure was the cause of readmission for 16% of patients with heart failure, where 22% of readmissions were related to other cardiovascular complaints and the remaining 62% of admissions were for other complaints13, 39. This is likely a reflection of the multiple comorbid conditions associated with acute heart failure, further reinforcing the importance of clear health communication for vulnerable patients with complex medical conditions. The potentially important role of numeracy in predicting readmissions for conditions other than heart failure, which constitute a significant portion of readmissions after hospitalization for acute heart failure, warrants further investigation.
Prior research has shown that patients with low numeracy and health literacy skills have worse clinical outcomes40, 41, are less likely to use preventive services, and lack the skills necessary for disease self-management 42-44. These patients are also more likely to be hospitalized45, 46, have higher mortality47, and report lower quality of life48. In addition, specifically for patients with heart failure, lower health literacy has been linked to worse clinical outcomes and more frequent emergency department visits. Lower medication adherence and lower health literacy may have contributed to emergency department visits for 192 patients with chronic heart failure22. During the evaluation of a pharmacy intervention for 61 patients with chronic heart failure, lower medication adherence and lower health literacy were associated with ED visits for cardiovascular complaints49. In addition, a recent retrospective cohort study of 1,492 patients with chronic heart failure in the Kaiser Permanente Colorado health system found that lower subjective health literacy was associated with increased all-cause mortality but not with hospitalizations20.
Strengths and Limitations
The strengths of this study include the size of the cohort and the unique focus on patients with acute heart failure and who are therefore most at risk for poor clinical outcomes and most likely to benefit from interventions aimed at improving chronic disease self-management.
While our study suggests that low numeracy is associated with increased 30-day recidivism, the results should be interpreted in the context of several limitations. We utilized subjective measures of numeracy and health literacy rather than objective measures such as the S-TOFHLA, REALM, or the WRAT. Objective measures are time consuming, must be administered by research assistants, are often not well received by patients27, 28, and are difficult to use in a clinical setting. The subjective measures of numeracy and health literacy used in this study were both validated in a general emergency department patient population29. Education level is thought to be in the causal pathway leading to low numeracy and health literacy skill levels and was therefore not included as a covariate in the models50; the potential independent contribution of education to the relationships between numeracy and health literacy with 30-day recidivism are not addressed in this analysis. Employment status was not included as a covariate in an effort to avoid overfitting the model. The exact relationship between numeracy and health literacy is unclear. The two are related, but it is thought that many patients with high health literacy may have low numeracy skills. We used a dichotomous composite outcome to indicate the burden of 30-day recidivism. Because patients who experienced multiple unplanned hospital admissions for acute heart failure were categorized the same as patients who returned to the emergency department once, our findings may underestimate the burden and severity of 30-day recidivism. Patients were screened for inclusion based on the chief complaints of dyspnea, cough, and acute pulmonary edema, which may not identify all patients with acute heart failure such as those who with orthopnea, atrial fibrillation, or edema; thus, it is possible that a small number of patients with acute heart failure may not have been screened for inclusion in this study. The diagnosis of acute heart failure was made by treating physicians, either in the emergency department or after admission to the hospital. Diagnoses were extracted by chart review and were left entirely to treating clinicians, who were not aware of study goals. While diagnostic error is possible, using clinical diagnoses makes the results of the study more generalizable to “real world” circumstances.
Conclusions
For patients with acute heart failure, lower subjective numeracy is associated with increased odds of recidivism to the emergency department or hospital within 30 days. Subjective health literacy may also play a role, but there was no evident association between health literacy and 30-day recidivism for patients with acute heart failure in this cohort of patients. The United States has made improving health literacy a top priority51, and the Centers for Medicare and Medicaid Services’ has emphasized reducing readmissions. As part of the effort to improve patient-centered outcomes and break the cascade of events that leads to suboptimal clinical outcomes, numeracy’s potential role in the high-cost, high-risk events of emergency department and hospital recidivism should be evaluated in future interventions aimed at improving the quality of care for patients with heart failure.
Clinical Summary.
Using a prospective cohort study of 709 patients who presented to the four hospital-based emergency departments (EDs) with signs and symptoms of acute heart failure, weinvestigated the relationships between subjective numeracy and health literacy with 30-day recidivism to the ED or hospital. Low numeracy was common (55% of patients), as was low health literacy (38% of patients); approximately 32% of patients returned to the ED or hospital within 30 days of the index ED visit. After adjusting for demographics and disease severity, low numeracy was associated with increased odds of returning to the ED or hospital within 30 days (adjusted odds ratio 1.41, 95% confidence interval 1.00-1.98, p=0.0048). Subjective health literacy may also play a role, but we did not detect a relationship in this cohort of patients with acute heart failure. Although this study did not investigate how numeracy may be associated with recidivism, we hypothesize that patients with low numeracy may have a difficulty understanding medical instructions, adhering to medication recommendations, and performing disease self-management tasks. For the many patients with heart failure who are high risk for hospitalization and re-hospitalization, addressing numeracy may be a key component of future efforts to improve patient-centered outcomes and break the cascade of events that leads to suboptimal clinical outcomes.
Acknowledgments
Sources of Funding
This work was supported by the Office of Academic Affiliations, Department of Veterans Affairs, VA National Quality Scholars; the National Heart, Lung, and Bone Institute grants R01 HL088459 and K23 HL085387; and National Center for Research Resources/National Institutes of Health CTSA grant UL1 RR024975-01.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the views of the Department of Veterans Affairs.
Footnotes
Disclosures
None.
References
- 1.Institute of medicine. Health literacy: A prescrition to end confusion. Washington, DC: The National Academies Press; 2004. [Google Scholar]
- 2.Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: Theory and practice. Ann Behav Med. 2008;35:261–274. doi: 10.1007/s12160-008-9037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rothman RL, Montori VM, Cherrington A, Pignone MP. Perspective: The role of numeracy in health care. J Health Commun. 2008;13:583–595. doi: 10.1080/10810730802281791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Health literacy: Report of the council on scientific affairs. Ad hoc committee on health literacy for the council on scientific affairs, american medical association. JAMA. 1999;281:552–557. [PubMed] [Google Scholar]
- 5.Ginde AA, Clark S, Goldstein JN, Camargo CA., Jr Demographic disparities in numeracy among emergency department patients: Evidence from two multicenter studies. Patient Educ Couns. 2008;72:350–356. doi: 10.1016/j.pec.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 6.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 7.Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, Nurss JR. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–1682. [PubMed] [Google Scholar]
- 8.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: An updated systematic review. Annals of internal medicine. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 9.Howard DH, Gazmararian J, Parker RM. The impact of low health literacy on the medical costs of medicare managed care enrollees. Am J Med. 2005;118:371–377. doi: 10.1016/j.amjmed.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 10.Eichler K, Wieser S, Brugger U. The costs of limited health literacy: A systematic review. International journal of public health. 2009;54:313–324. doi: 10.1007/s00038-009-0058-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly PA, Haidet P. Physician overestimation of patient literacy: A potential source of health care disparities. Patient education and counseling. 2007;66:119–122. doi: 10.1016/j.pec.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Powell CK, Kripalani S. Brief report: Resident recognition of low literacy as a risk factor in hospital readmission. Journal of general internal medicine. 2005;20:1042–1044. doi: 10.1111/j.1525-1497.2005.0220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. The New England journal of medicine. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 14.Gheorghiade M, Pang PS. Acute heart failure syndromes. J Am Coll Cardiol. 2009;53:557–573. doi: 10.1016/j.jacc.2008.10.041. [DOI] [PubMed] [Google Scholar]
- 15.Ross JS, Chen J, Lin Z, Bueno H, Curtis JP, Keenan PS, Normand SL, Schreiner G, Spertus JA, Vidan MT, Wang Y, Krumholz HM. Recent national trends in readmission rates after heart failure hospitalization. Circulation Heart Failure. 2010;3:97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics--2011 update: A report from the american heart association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCaig LF, Burt CW. National hospital ambulatory medical care survey: 2002 emergency department summary. Adv Data. 2004:1–34. [PubMed] [Google Scholar]
- 18.Lee DS, Austin PC, Stukel TA, Alter DA, Chong A, Parker JD, Tu JV. “Dose-dependent” impact of recurrent cardiac events on mortality in patients with heart failure. The American journal of medicine. 2009;122:162–169. e161. doi: 10.1016/j.amjmed.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 19.Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. American heart journal. 2007;154:260–266. doi: 10.1016/j.ahj.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 20.Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, Matlock DD, Magid DJ, Masoudi FA. Health literacy and outcomes among patients with heart failure. JAMA: The Journal of the American Medical Association. 2011;305:1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DeWalt DA, Malone RM, Bryant ME, Kosnar MC, Corr KE, Rothman RL, Sueta CA, Pignone MP. A heart failure self-management program for patients of all literacy levels: A randomized, controlled trial [isrctn11535170] BMC Health Serv Res. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther. 2009;85:651–658. doi: 10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in framingham heart study subjects. Circulation. 1993;88:107–115. doi: 10.1161/01.cir.88.1.107. [DOI] [PubMed] [Google Scholar]
- 24.McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: The framingham study. The New England journal of medicine. 1971;285:1441–1446. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- 25.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–594. [PubMed] [Google Scholar]
- 26.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, Bradley KA, Nugent SM, Baines AD, Vanryn M. Validation of screening questions for limited health literacy in a large va outpatient population. J Gen Intern Med. 2008;23:561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: Development of the subjective numeracy scale. Med Decis Making. 2007;27:672–680. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- 28.Zikmund-Fisher BJ, Smith DM, Ubel PA, Fagerlin A. Validation of the subjective numeracy scale: Effects of low numeracy on comprehension of risk communications and utility elicitations. Med Decis Making. 2007;27:663–671. doi: 10.1177/0272989X07303824. [DOI] [PubMed] [Google Scholar]
- 29.McNaughton C, Wallston KA, Rothman RL, Marcovitz DE, Storrow AB. Short, subjective measures of numeracy and general health literacy in an adult emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2011;18:1148–1155. doi: 10.1111/j.1553-2712.2011.01210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (redcap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harrell FE, Jr, Lee KL, Califf RM, Pryor DB, Rosati RA. Regression modelling strategies for improved prognostic prediction. Stat Med. 1984;3:143–152. doi: 10.1002/sim.4780030207. [DOI] [PubMed] [Google Scholar]
- 32.Steyerberg E. Clinical prediction models - a practical approach to development, validation, and updating. New York City, NY: Springer; 2009. [Google Scholar]
- 33.Pocock SJ, Wang D, Pfeffer MA, Yusuf S, McMurray JJ, Swedberg KB, Ostergren J, Michelson EL, Pieper KS, Granger CB. Predictors of mortality and morbidity in patients with chronic heart failure. European heart journal. 2006;27:65–75. doi: 10.1093/eurheartj/ehi555. [DOI] [PubMed] [Google Scholar]
- 34.Go AS, Yang J, Ackerson LM, Lepper K, Robbins S, Massie BM, Shlipak MG. Hemoglobin level, chronic kidney disease, and the risks of death and hospitalization in adults with chronic heart failure: The anemia in chronic heart failure: Outcomes and resource utilization (anchor) study. Circulation. 2006;113:2713–2723. doi: 10.1161/CIRCULATIONAHA.105.577577. [DOI] [PubMed] [Google Scholar]
- 35.Unroe KT, Greiner MA, Hernandez AF, Whellan DJ, Kaul P, Schulman KA, Peterson ED, Curtis LH. Resource use in the last 6 months of life among medicare beneficiaries with heart failure, 2000-2007. Archives of internal medicine. 2011;171:196–203. doi: 10.1001/archinternmed.2010.371. [DOI] [PubMed] [Google Scholar]
- 36.Kirsch IS, Jungeblut A, Jenkins L, Kolstad A. Adult literacy in America: A first look at the results of the national adult literacy survey (NCES 1993-275) 3. Washington, DC: National Center for Education Statistics, US Dept of Education; 2002. [Google Scholar]
- 37.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20:175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy (NCES 2006-483) Washington, DC: National Center for Education Statistics, US Dept of Education; 2006. [Google Scholar]
- 39.Dunlay SM, Redfield MM, Weston SA, Therneau TM, Hall Long K, Shah ND, Roger VL. Hospitalizations after heart failure diagnosis a community perspective. Journal of the American College of Cardiology. 2009;54:1695–1702. doi: 10.1016/j.jacc.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.DeWalt DA, Dilling MH, Rosenthal MS, Pignone MP. Low parental literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007;7:25–31. doi: 10.1016/j.ambp.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 42.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–1015. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 43.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among medicare enrollees in a managed care organization. Med Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 45.Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, Ren J, Peel J. Functional health literacy and the risk of hospital admission among medicare managed care enrollees. Am J Public Health. 2002;92:1278–1283. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13:791–798. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cavanaugh KL, Wingard RL, Hakim RM, Eden S, Shintani A, Wallston KA, Huizinga MM, Elasy TA, Rothman RL, Ikizler TA. Low health literacy associates with increased mortality in esrd. J Am Soc Nephrol. 2010;21:1979–1985. doi: 10.1681/ASN.2009111163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. American Journal of Public Health. 1997;87:1027–1030. doi: 10.2105/ajph.87.6.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hope CJ, Wu J, Tu W, Young J, Murray MD. Association of medication adherence, knowledge, and skills with emergency department visits by adults 50 years or older with congestive heart failure. Am J Health Syst Pharm. 2004;61:2043–2049. doi: 10.1093/ajhp/61.19.2043. [DOI] [PubMed] [Google Scholar]
- 50.DeWalt DA, Pignone MP. Reading is fundamental: The relationship between literacy and health. Archives of internal medicine. 2005;165:1943–1944. doi: 10.1001/archinte.165.17.1943. [DOI] [PubMed] [Google Scholar]
- 51.Koh HK, Berwick DM, Clancy CM, Baur C, Brach C, Harris LM, Zerhusen EG. New federal policy initiatives to boost health literacy can help the nation move beyond the cycle of costly ‘crisis care’. Health Aff (Millwood) 2012 doi: 10.1377/hlthaff.2011.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]


