Abstract
BACKGROUND
Telemedicine can facilitate communication between primary care clinicians and specialists. Generalists who use telemedicine for consultation (teleconsultation) may be able to practice more independently and reduce the number of formal referrals to specialists. In the United States, a federally funded human immunodeficiency virus (HIV) teleconsultation service (HIV Warmline) offers clinicians live telephone access to HIV specialists; however, its impact on clinicians’ self-perceived clinical competence and referral rates has not been studied.
OBJECTIVE
To determine if primary care clinicians who used the HIV Warmline felt more capable of managing HIV in their own practices.
DESIGN
Online survey.
PARTICIPANTS
Primary care physicians and mid-level practitioners who used the HIV Warmline for teleconsultation between 1/2008 and 3/2010.
MAIN MEASURES
Participants compared the HIV Warmline to other methods of obtaining HIV clinical support, and then rated its impact on their confidence in their HIV skills and their referral patterns.
KEY RESULTS
Respondents (N = 191, 59 % response rate) found the HIV Warmline to be quicker (65 %), more applicable (70 %), and more trustworthy (57 %) than other sources of HIV information. After using the HIV Warmline, 90 % had improved confidence about caring for HIV, 67 % stated it changed the way they managed HIV, and 74 % were able to avoid referring patients to specialists. All valued the availability of live, free consultation.
CONCLUSIONS
Primary care clinicians who called the HIV Warmline reported increased confidence in their HIV care and less need to refer patients to specialists. Teleconsultation may be a powerful tool to help consolidate HIV care in the primary care setting, and could be adapted for use with a variety of other medical conditions. The direct impact of teleconsultation on actual referral rates, quality of care and clinical outcomes needs to be studied.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-013-2332-5) contains supplementary material, which is available to authorized users.
KEY WORDS: telemedicine, primary care, consultation, infectious disease, HIV, AIDS
INTRODUCTION
The United States healthcare system is in need of innovations to strengthen primary care and reduce the overuse of specialists.1–5 A variety of practice changes have been suggested to redress the primary–specialty care balance, with many in various stages of investigation or implementation.6,7 One important strategy is the use of information technology to facilitate communication between primary care clinicians and specialists.8,9 An emerging tool is that of “teleconsultation”—the use of email, telephone, video, or mobile device to obtain specialty consultation at a distance. It has been suggested that teleconsultation could help primary care clinicians practice more independently and thereby reduce the number of formal referrals to specialists.10,11 In addition, teleconsultation might enable clinicians without local specialist resources to build their knowledge base and eventually expand their scope of practice, offering services their patients would not otherwise be able to receive.12 As a tool for consolidating medical care in the primary care setting, teleconsultation may be ideal for use in the Patient Centered Medical Home and other primary care-centered health system models.
There are an increasing number and variety of telemedicine programs used to deliver specialty consultation, commonly in fields such as radiology, dermatology, neurology and cardiology. A few of these programs are geared specifically toward increasing the skill and knowledge base of primary care clinicians and have been generally well accepted by those who use them.12–22 However, there are few data about how these interventions impact the scope of practice, quality of care, or the subsequent use of specialist services by primary care clinicians, and we are aware of only one study that has measured patient outcomes.23
To better understand the effect of teleconsultation on primary care clinicians’ self-perceived clinical competence and its impact on their utilization of specialist resources, we surveyed users of a long-standing teleconsultation service, the National Human Immunodeficiency Virus (HIV) Telephone Consultation Service (the HIV Warmline) at the University of California, San Francisco. Since 1992, the HIV Warmline has provided clinicians with real-time, free, telephone consultations with HIV experts. The HIV Warmline is available nation-wide and more than half of callers are primary care clinicians. Both primary care and specialist clinicians have rated the service highly on satisfaction surveys.24 However, until our current survey, clinicians had not been studied formally to examine the service’s impact on their self-reported HIV-related practice patterns. We sought to determine whether primary care clinicians experienced a subjective improvement in confidence about their HIV clinical skills and whether this would reduce their perceived need to refer patients to HIV specialists. Positive findings would support the idea that teleconsultation can expand the comprehensiveness of care delivered by primary care clinicians, thereby reducing the need to rely on expensive, and sometimes scarce specialty resources.
We chose to study the HIV Warmline for three reasons: first, the service is a well established and successful program, allowing us to evaluate users’ experience without having to account for the instabilities faced by many newer programs. Second, as a national service, the results of the study may be more generalizable than studies without a national scope. Third, HIV is an ideal condition to study the primary-specialty care balance, since this balance is already in the process of shifting from an expert-centered model of care to a primary care-centered model of care: over the next few years a sizeable portion of HIV care is expected to be reallocated to primary care clinicians, because of the expanding primary care needs of patients with HIV and the decreasing availability of HIV specialists.25–27 This naturally occurring shift makes HIV an excellent arena in which to study interventions that support primary care clinicians in delivering more in-depth medical care, a concept which could then be expanded from HIV to other diseases.
METHODS
Study Population
We surveyed primary care clinicians who had used the federally-funded National HIV Telephone Consultation Service (HIV Warmline) for consultation on the management of HIV-infected patients.
The HIV Warmline (1-800-933-3413) is a national telephone service that provides free clinical consultation to healthcare providers managing HIV-infected patients. Established in 1992, the service is part of the National HIV/AIDS Clinicians’ Consultation Center (NCCC) at the University of California, San Francisco (UCSF), San Francisco General Hospital and is funded by the Health Resources and Services Administration (HRSA), with supplementary funding from the Centers for Disease Control and Prevention (CDC). The HIV Warmline is staffed by UCSF physicians and clinical pharmacists with expertise in HIV care. Clinicians with any level of HIV experience can call between 9 AM and 8 PM EST and speak directly with an HIV specialist. Clinical recommendations are based on national HIV treatment guidelines28,29 supplemented by current research and expert opinion. The most common topic of consultation is management of antiretroviral therapy (56 %), followed by clinical issues relating to HIV disease (29 %).30
Users of the HIV Warmline include physicians (60 %, with approximately 2/3 primary care and 1/3 infectious diseases specialists); nurse practitioners and physician assistants (20 %); nurses, pharmacists, and others (20 %).24 The service maintains an electronic record of consultations and stores contact information for callers.
We searched the HIV Warmline’s electronic database to identify primary care clinicians who had called with a clinical question between 1 January 2008 and 31 March 2010. Primary care clinicians were defined as family physicians, general internal medicine physicians, general practitioners, obstetricians/gynecologists, nurse practitioners and physician assistants. Pediatricians were excluded, since most pediatric HIV care in the United States is delivered in highly specialized settings. Callers without an email address on file, those who opted out of receiving surveys, and those with a pre-existing relationship to HIV Warmline staff were excluded.
In April 2010, we emailed an invitation to complete the online survey via Survey Monkey. No incentive was offered to participants. Reminder emails were sent twice, at 1-week intervals. One month later, non-respondents and those with undeliverable emails were sent a paper copy of the survey by postal mail.
Measurements
The survey consisted of 18 questions covering demographic information (including professional training and current clinical practice characteristics), and an evaluation of the HIV Warmline service. The evaluation component used a 5-point Likert scale (1 = lowest, 5 = highest) to rate responses in three areas: 1) a comparison of the HIV Warmline to other methods of obtaining HIV information; 2) identification of aspects of the HIV Warmline most important to users; and 3) an evaluation of the subjective impact the service has had on their HIV practice patterns. The full survey instrument is available in the online appendix.
We formulated survey questions based on prior surveys of HIV providers31–34 and pilot tested the instrument with colleagues. We used acceptance of Medicaid as a surrogate measure for care of underserved communities. The measure, “self-identified expertise,” has been used in previous studies and has been shown to correlate well with HIV-infected (HIV+) patient caseload, HIV knowledge, and referral rates among generalist-trained physicians.30 We defined “level of HIV service” as the degree of comprehensiveness of care provided to HIV + patients, ranging from no care (“I do not provide care for HIV infected patients”) to complete care (“I provide comprehensive services, including HIV medication therapy, at all stages of disease”). For non-respondents, we obtained demographic details directly from the HIV Warmline database, including profession, specialty, practice setting, HIV + patient load, and number of calls to the HIV Warmline.
Analysis
We present demographic information descriptively. For questions using the 5-point Likert scale, we dichotomized the scale, comparing Likert values 1–3 (strongly negative to neutral) to Likert values 4–5 (positive to strongly positive). For each question, we present point estimates for the percentage of respondents in the higher category, along with 95 % confidence intervals.
We performed bivariate and multivariate logistic regression (including the pre-specified variables of profession, specialty, practice type, urban versus rural locale, HIV + patient load, level of HIV service, and self-defined expertise) to examine the relationship between provider characteristics and the impact of the HIV Warmline on clinicians’ self-perceived clinical competence and practice patterns. For multilevel categorical predictors, we used chi square tests to assess heterogeneity or linear trend (using orthogonal contrasts), as appropriate. Missing data were dropped from the analyses using pairwise deletion.
We performed several analyses to address potential sources of bias. To address volunteer response bias, we compared demographic characteristics of respondents to non-respondents and those of email to paper survey respondents. We anticipated that repeat callers would be more likely to respond to the survey and would be more likely to be positive in their evaluation than one-time callers; to address this potential bias, we performed chi square tests to compare the responses of one-time to repeat callers on key questions. We followed this with a sensitivity analysis, assuming that non-respondents would rate the HIV Warmline low on the dichotomized Likert scale on all questions.
All statistical tests were performed using Stata 11 (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX).
The University of California San Francisco Committee on Human Research approved this study.
RESULTS
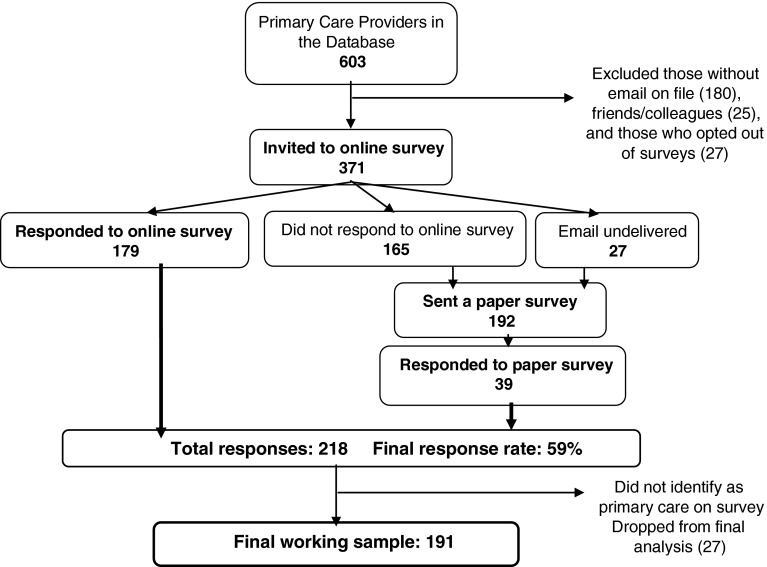
Online and subsequent paper invitations were sent to 371 participants; 218 completed the survey for a response rate of 59 % (Fig. 1). For the final analysis, we excluded 27 respondents who did not identify as primary care clinicians on their survey, yielding a working sample of 191 participants.
Figure 1.
Participant enrollment flow chart.
Caller Demographic Information
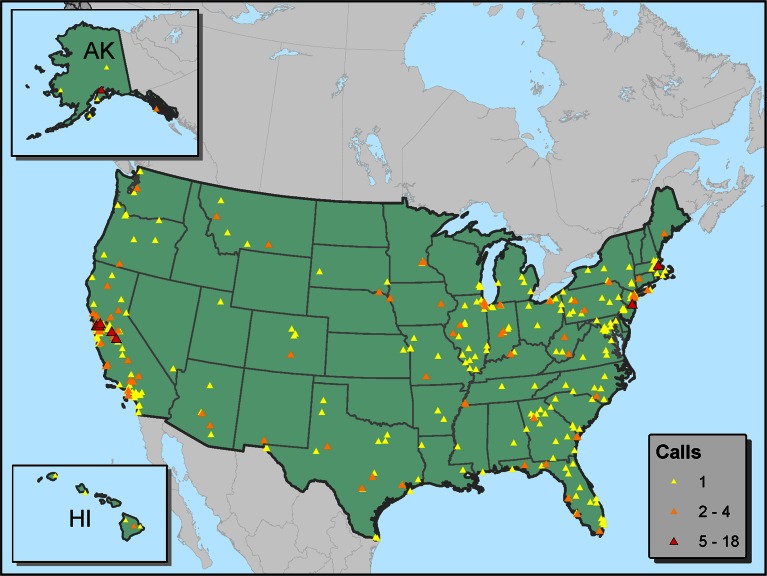
Calls came from 45 states and the U.S. territories of Guam, Puerto Rico and Trinidad and Tobago (Fig. 2). Respondents called between one and 61 times each, with a median of one call and a mean of 5.1 calls. Sixty one percent of respondents called more than once.
Figure 2.
Distribution of calls to the HIV warmline from primary care clinicians (includes respondents and non-respondents, January 2008 to March 2010).
Two thirds of respondents were physicians, and more than half of all respondents practiced family medicine (Table 1). The average number of years in practice was 15.5 (range 0–43 years). The most common practice setting was a community or public health clinic; 76 % reported working in a setting that accepts Medicaid. Twenty five percent of callers worked in rural areas. Although half of respondents cared for more than 25 HIV-infected patients and 62 % provided comprehensive care to HIV + patients at all stages of disease, only 39 % considered themselves to be HIV experts.
Table 1.
Subject Characteristics
| Characteristic | n (%) |
|---|---|
| Professional Degree (N = 188) | |
| MD | 126 (67) |
| NP/PA | 62 (33) |
| Primary Specialty or Focus of Practice (N = 191) | |
| Family Medicine | 98 (51) |
| General Internal Medicine | 60 (31) |
| General Practice | 15 (8) |
| Other Primary Care | 18 (9) |
| Practice Type (N = 190) | |
| Community Clinic/Public Health Clinic | 74 (39) |
| Private Practice | 38 (20) |
| University or Hospital Associated Clinic | 23 (12) |
| Correctional Facility | 24 (13) |
| Other | 31 (16) |
| Practice Locale (N = 190) | |
| Urban | 113 (60) |
| Suburban | 29 (15) |
| Rural | 48 (25) |
| Current HIV + Patient Load (N = 190) | |
| > 25 Patients | 94 (49) |
| 6–25 Patients | 40 (21) |
| 1–5 Patients | 41 (22) |
| 0 Patients | 15 (8) |
| Level of Service Provided for HIV + Patients (N = 189) | |
| Provide comprehensive services at all stages of disease | 118 (62) |
| Provide comprehensive services, but refer if complications | 37 (20) |
| Provide services until need for HIV medication, then refer | 11 (6) |
| Provide services only for conditions not related to HIV | 15 (8) |
| I do not provide care for HIV-infected patients | 8 (4) |
| Self-Defined HIV Expert? (N = 190) | |
| Yes | 74 (39) |
| No | 116 (61) |
Evaluation of the HIV Warmline
Overall, callers found the HIV Warmline to be faster to use, more applicable to their particular situation and more trustworthy than their other most-commonly used HIV resource (Table 2). They most valued being able to talk to a consultant live and free of charge. Sixty four percent of respondents felt that their patient’s health had improved as a direct result of using the HIV Warmline and 98 % planned to use the service again, including 61 out of the 62 one-time callers. Table 3 provides a selection of comments from respondents, highlighting specific benefits of the service.
Table 2.
Assessment of HIV Warmline Services
| Question | % Likert 4–5 (95 % CI) |
|---|---|
| “Compared to your other most commonly used HIV resource…:” | “More or Much More” |
| How QUICKLY does the HIV Warmline provide you with an answer to your question? | 65.4 % (0.58, 0.72) |
| How APPLICABLE to your particular clinical situation is the information from the HIV Warmline? | 69.7 % (0.63, 0.76) |
| How TRUSTWORTHY is the information from the HIV Warmline? | 57.3 % (0.50, 0.64) |
| “How important are the following features of the HIV Warmline?” | “Very or Extremely Important” |
| Live consultants | 98.4 % (0.97, 1.00) |
| Free service | 93.0 % (0.89, 0.97) |
| Advice Based on Federal HIV Practice Guidelines | 76.1 % (0.70, 0.82) |
| Confidential service | 69.4 % (0.63, 0.76) |
| “To what extent do you agree with the following statements?” | “Agree, or Strongly Agree” |
| The HIV Warmline has helped me stay up-to-date with HIV care. | 77.3 % (0.71, 0.83) |
| Using the HIV Warmline has changed the way I manage HIV. | 67.2 % (0.60, 0.74) |
| Using the HIV Warmline has improved my confidence about caring for HIV-infected patients. | 90.3 %(0.86, 0.95) |
| The HIV Warmline has helped me manage HIV without having to refer the patient elsewhere. | 74.3 % (0.68, 0.81) |
Table 3.
Specific Benefits of HIV Warmline Consultation
| Comment | Theme(s) |
|---|---|
| “In a rural practice, patients appreciate services like yours to maintain up to date information/consultation through their primary care provider.” | Isolated provider |
| Staying up to date with HIV medicine | |
| “You are providing a fabulous service, especially to docs like me in a prison where it is hard to find good HIV specialists who will see prisoners.” | Isolated provider |
| “The HIV Warmline is great for complex HIV issues because my patients cannot travel long distances and thus I must manage all aspect of their HIV disease.” | Isolated provider |
| Complex cases | |
| “As a midlevel practitioner I can’t imagine working in HIV medicine without it.” | Mid-level provider |
| “I have a few less than 25 patients, and it’s nice to be able to get answers to simple questions that would be a bit embarrassing to ask, and for complex questions where I prefer the advice of the Warmline to my local ID consultants.” | Low volume provider |
| Concern about appearing unqualified in front of local colleagues | |
| “By the time I call the Warmline, I have already used the Stanford HIV Resistance Database, but want a second opinion.” | Experienced provider |
| Complex cases | |
| “I find the Warmline useful when there is not consensus among my colleagues, when study data is conflicting, and when existing data is unclear or difficult, at least for me, to interpret.” | Help synthesizing multiple sources of information |
| Complex cases | |
| “I found the service excellent, and not replaceable with on-line research.” | Superior to on-line resources |
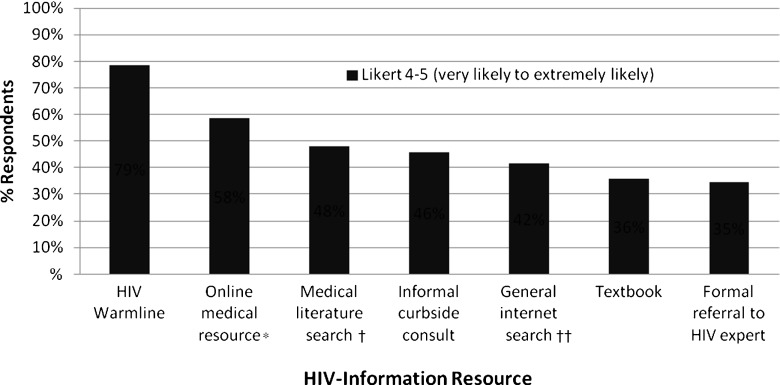
Respondents were asked how likely they were to use a variety of HIV information resources (Fig. 3). The HIV Warmline was rated as very or extremely likely to be used by 79 %. Only 35 % stated that they were very or extremely likely to consult a textbook or make a formal referral to an HIV expert.
Figure 3.
Likelihood of using various HIV-information resources. * e.g. UpToDate, Medscape, etc. † e.g. Pubmed, etc. ††e.g. Google, Yahoo, etc.
Impact on HIV Practice Patterns
A significant majority of respondents (90 %) experienced improvement in confidence about caring for HIV; 74 % stated they were able to manage the patient without referring for specialty care because of their use of the HIV Warmline (Table 2). On multivariate analysis (data not shown), few differences were noted on the impact of the HIV Warmline to increase confidence or reduce referrals among different subgroups of clinicians. In fact, only offering a higher level of HIV service was associated with a reduction in referrals (plinear trend = 0.002). This effect was not observed for clinicians caring for larger panels of HIV + patients (p = 0.08), nor for those who consider themselves HIV experts (p = 0.36).
Evaluation of Potential Sources of Bias We compared demographic information between respondents and non-respondents and found no statistically significant differences in profession, specialty, practice setting, or HIV + patient load. There were no statistically significant differences between those who completed email or paper surveys.
Non-respondents were more likely to be one-time callers (56 %) compared to respondents (38 %, p = 0.001). We performed chi square tests to examine differences in the experience of the HIV Warmline between one-time and repeat callers. While most responses were similar, statistically significant differences were observed for two questions: repeat callers were more likely to experience an increase in confidence about their HIV care (94 % vs. 84 %, p = 0.04), and they were more likely to state that the service had helped them stay up to date with HIV care (83 % vs. 64 %, p = 0.006). The sensitivity analysis showed that if all non-respondents had rated the HIV Warmline low, 45 % would have experienced increased confidence and 36 % would have experienced a decreased need to refer.
DISCUSSION
This survey of primary care clinicians who used the HIV Warmline for teleconsultation shows it to be a valuable and well-received tool, increasing clinicians’ confidence in their own HIV care and reducing their need to refer patients to specialists. Clinicians found the service to be both efficient and reliable, and affirmed that they altered their HIV management based on the consultants’ recommendations. Although these measures are subjective and cannot be generalized widely, the high degree of enthusiasm among respondents suggests that teleconsultation could be a favored mechanism of support for clinicians who are similar to those in our sample.
Survey respondents largely preferred the HIV Warmline to other sources of HIV information and consultation, finding it to be quick, effective, and trustworthy. The most important feature was the availability of live consultants. An earlier study we conducted24 suggests some possible reasons for this, including the speed of getting an answer, the ability to have a more detailed dialog about complicated cases than is practical in writing, and the reassurance that comes from developing trust in the consultant during the conversation. The second most important feature to callers was the fact that the service is free of charge. This contributes greatly to the accessibility of the service and lowers the bar for many who might be reluctant to try it for the first time.
We saw no difference in the impact of HIV Warmline consultation on different types of clinicians with one exception: providers who already deliver more comprehensive HIV care saw a greater reduction in referral rates. This finding might reflect the pre-existing commitment of those clinicians to deliver full-spectrum care and their interest in using consultation to further decrease their referral rates. There were no differences between urban and rural clinicians, nor between midlevel providers and physicians. The general lack of differential effect suggests that expert telephonic consultation can be helpful for a wide variety of clinicians.
Our study has some weaknesses. Most importantly, users of the HIV Warmline are a self-selected group, making generalization a challenge. However, even if our findings only apply to users similar to those in our survey, it is likely that sufficient numbers of such clinicians exist to make dissemination of the model worth exploring. This is especially true given that teleconsultation does not require users to be collocated in time or space. An additional limitation is that the survey did not collect information about patients, nor about the complexity of the cases discussed. However, our earlier work noted that patients discussed on the HIV Warmline are roughly representative of the national HIV epidemic and that the complexity of calls spans the clinical spectrum (with 60 % of antiretroviral calls related to drug resistance, generally considered among the most complex of HIV topics).24 Thus, HIV Warmline consultation should be appropriate for the full range of questions posed by primary care clinicians. Our survey is also vulnerable to respondent bias despite the nearly 60 % response rate. To estimate the magnitude of this bias, we compared demographic details of respondents to non-respondents and found no differences, suggesting that respondents were representative of our target population. We did find that respondents were more likely to be repeat callers, which would tend to bias the results towards a more favorable review of the service. However, we found few differences in the answers to survey questions between one-time and repeat callers, with the exception that repeat callers felt more confident and more up-to-date with HIV care. It is also notable that even one-time callers reported high levels of satisfaction with HIV Warmline consultation, including 84 % experiencing an improvement in their confidence about HIV care and 98 % stating that they would use the service again (although we acknowledge a potential source of measurement error, given that some of our apparent one-time callers may be repeat callers, having called before 2008). Finally, our sensitivity analysis showed that even if all non-respondents rated the HIV Warmline poorly, 45 % would still experience an increase in confidence and 36 % would refer less often, suggesting that use of the HIV Warmline would translate into concrete changes in primary care practice, even if our survey was biased to overstate the effect size.
The HIV Warmline provides a real-world example of teleconsultation as a tool to strengthen primary care. Our study shows that primary care clinicians who used the service found it to be an efficient and effective way of obtaining HIV consultation, increasing their confidence about HIV care and reducing referrals to HIV specialists. Although fewer referrals may not lead directly to improved care, our findings support the concept that teleconsultation can help consolidate care in the primary care setting, leading to fewer gaps in care, decreased spending on specialty care, and increased access to services for many patients. Further evaluation of the service’s impact on objective measures of quality of care, referral rates, and cost effectiveness are needed, along with an examination of the program’s readiness for dissemination within and beyond HIV. Teleconsultation should continue to be studied as an important contribution of health information technology to primary care redesign.
Electronic supplementary material
(PDF 165 kb)
Acknowledgements
Contributors
No additional contributors.
Funders
The National HIV/AIDS Clinicians’ Consultation Center administers the HIV Warmline at the University of California San Francisco and is supported by the Health Resources and Services Administration (HRSA) HIV/AIDS Bureau’s AIDS Education and Training Centers (AETCs) (Grant No. H4AHA01082).
Dr. Waldura is supported in part by a National Institutes of Health Award Number KL2RR024130 from the National Center for Research Resources.
Dr. Dehlendorf is supported by Grant Number K23HD067197 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health.
Prior Presentations
A preliminary version of our findings was presented as a poster at 2010 Ryan White Grantee Meeting and 13th Annual Clinical Conference in Washington D.C., August 2010.
Conflict of Interest
Drs. Waldura and Goldschmidt and Ms. Neff receive salary support from the National HIV/AIDS Clinicians’ Consultation Center, which administers the HIV Warmline as a grant-support project of the Department of Family and Community Medicine at the University of California, San Francisco.
Abbreviations
- HIV
Human immunodeficiency virus
- AIDS
Acquired immunodeficiency syndrome
REFERENCES
- 1.Agency for Healthcare Research and Quality. Research at the Interface of Primary and Specialty Care. Conference Summary. 1995; http://www.ahrq.gov/research/interovr.htm. Accessed Dec. 19, 2012.
- 2.Selby JV, Grumbach K, Quesenberry CP, Jr, Schmittdiel JA, Truman AF. Differences in resource use and costs of primary care in a large HMO according to physician specialty. Health Serv Res. 1999;34(2):503–518. [PMC free article] [PubMed] [Google Scholar]
- 3.Bodenheimer T, Grumbach K, Berenson RA. A lifeline for primary care. N Engl J Med. 2009;360(26):2693–2696. doi: 10.1056/NEJMp0902909. [DOI] [PubMed] [Google Scholar]
- 4.Stange KC, Ferrer RL. The paradox of primary care. Ann Fam Med. 2009;7(4):293–299. doi: 10.1370/afm.1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Starfield B. Primary care, specialist care, and chronic care: can they interlock? Chest. 2010;137(1):8–10. doi: 10.1378/chest.09-1441. [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint principles of the patient centered medical home. 2007. http://www.pcpcc.net/node/14. Accessed Dec. 19, 2012.
- 7.Craig C ED, Whittington J. Care Coordination Model: Better Care at Lower Cost for People with Multiple Health and Social Needs. IHI Innovation Series white paper. 2011. http://www.ihi.org/knowledge/Pages/IHIWhitePapers/IHICareCoordinationModelWhitePaper.aspx. Accessed Dec. 19, 2012.
- 8.Bates DW, Bitton A. The future of health information technology in the patient-centered medical home. Health Aff (Millwood).29(4):614–621 [DOI] [PubMed]
- 9.Chen AH, Yee HF., Jr Improving primary care-specialty care communication: lessons from San Francisco’s safety net: comment on “Referral and consultation communication between primary care and specialist physicians”. Arch Intern Med. 2011;171(1):65–67. doi: 10.1001/archinternmed.2010.484. [DOI] [PubMed] [Google Scholar]
- 10.Forrest CB. A typology of specialists’ clinical roles. Arch Intern Med. 2009;169(11):1062–1068. doi: 10.1001/archinternmed.2009.114. [DOI] [PubMed] [Google Scholar]
- 11.Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: early insights. Issue Brief (Commonw Fund). 2011;23:1–14. [PubMed] [Google Scholar]
- 12.Arora S, Kalishman S, Thornton K, et al. Expanding access to hepatitis C virus treatment–Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology. 2010;52(3):1124–1133. doi: 10.1002/hep.23802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smego RA, Khakoo RA, Burnside CA, Lewis MJ. The benefits of telephone-access medical consultation. J Rural Health. 1993;9(3):240–245. doi: 10.1111/j.1748-0361.1993.tb00517.x. [DOI] [PubMed] [Google Scholar]
- 14.Scalvini S, Rivadossi F, Comini L, Muiesan ML, Glisenti F. Telemedicine: the role of specialist second opinion for GPs in the care of hypertensive patients. Blood pressure. 2011;20(3):158–165. doi: 10.3109/08037051.2010.542646. [DOI] [PubMed] [Google Scholar]
- 15.Angstman KB, Adamson SC, Furst JW, Houston MS, Rohrer JE. Provider satisfaction with virtual specialist consultations in a family medicine department. Health Care Manager. 2009;28(1):14–18. doi: 10.1097/HCM.0b013e318196def8. [DOI] [PubMed] [Google Scholar]
- 16.Bradstock SE, Wilson AJ, Cullen MJ, Barwell KL. Telephone-based psychiatry advice service for general practitioners. Med J Aust. 2005;183(2):90. doi: 10.5694/j.1326-5377.2005.tb06932.x. [DOI] [PubMed] [Google Scholar]
- 17.Bujnowska-Fedak MM, Staniszewski A, Steciwko A, Puchala E. System of telemedicine services designed for family doctors’ practices. Telemed J E Health. 2000;6(4):449–452. doi: 10.1089/15305620050503933. [DOI] [PubMed] [Google Scholar]
- 18.Hollins J, Veitch C, Hays R. Interpractitioner communication: telephone consultations between rural general practitioners and specialists. Aust J Rural Heal. 2000;8(4):227–231. doi: 10.1046/j.1440-1584.2000.00285.x. [DOI] [PubMed] [Google Scholar]
- 19.Holt N, Crawford MA. Medical Information Service via Telephone. The pioneer of physician consultation services. Ann N Y Acad Sci. 1992;670(1):155–162. doi: 10.1111/j.1749-6632.1992.tb26086.x. [DOI] [PubMed] [Google Scholar]
- 20.MacFarlane A, Harrison R, Murray E, Wallace P. A qualitative study of communication during joint teleconsultations at the primary-secondary care interface. J Telemed Telecare. 2006;12(Suppl 1):24–26. doi: 10.1258/135763306777978425. [DOI] [PubMed] [Google Scholar]
- 21.Norris TE, Hart GL, Larson EH, et al. Low-bandwidth, low-cost telemedicine consultations in rural family practice. J Am Board Fam Pract. 2002;15(2):123–127. [PubMed] [Google Scholar]
- 22.Roland M, Bewley B. Boneline: evaluation of an initiative to improve communication between specialists and general practitioners. J publ health med. 1992;14(3):307–309. [PubMed] [Google Scholar]
- 23.Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199–2207. doi: 10.1056/NEJMoa1009370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Waldura JF, Neff S, Goldschmidt RH. Teleconsultation for clinicians who provide human immunodeficiency virus care: experience of the national HIV telephone consultation service. Telemed J E Health. 2011;17(6):472–477. doi: 10.1089/tmj.2010.0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.HIV Medicine Association. The looming crisis in HIV care: who will provide the care? 2010. http://www.idsociety.org/Search.aspx?&lcid=9&q=looming&tz=America%2FLos_Angeles. Accessed Dec. 19, 2012.
- 26.Health Resources and Services Administration. Workforce Capacity in HIV. CAREAction Newsletter. 2010(April). http://hab.hrsa.gov/newspublications/careactionnewsletter/april2010.pdf. Accessed Dec. 19, 2012.
- 27.Katz MH. Human immunodeficiency virus is (once again) a primary care disease. Arch Intern Med. 2011;171(8):719–720. doi: 10.1001/archinternmed.2011.130. [DOI] [PubMed] [Google Scholar]
- 28.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. http://aidsinfo.nih.gov/contentfiles/lvguidelines/AdultandAdolescentGL.pdf. Accessed Dec. 19, 2012.
- 29.Thompson MA, Aberg JA, Hoy JF, Telenti A, Benson C, Cahn P, Eron JJ, Gunthard HF, Hammer SH, Reiss P, Richman DD, Rizzardini G, Thomas DL, Jacobsen DM, Volberding PA. Antiretroviral Treatment of Adult HIV Infection: 2012 Recommendations of the International Antiviral Society–USA Panel. JAMA. 2012;308(4):387–402. doi: 10.1001/jama.2012.7961. [DOI] [PubMed] [Google Scholar]
- 30.Landon BE, Wilson IB, Wenger NS, et al. Specialty training and specialization among physicians who treat HIV/AIDS in the United States. J Gen Intern Med. 2002;17(1):12–22. doi: 10.1046/j.1525-1497.2002.10401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liljestrand P. HIV care: continuing medical education and consultation needs of nurses, physicians, and pharmacists. J Assoc Nurses AIDS Care. 2004;15(2):38–50. doi: 10.1177/1055329003252053. [DOI] [PubMed] [Google Scholar]
- 32.Cook PF, Friedman R, Lord A, Bradley-Springer LA. Outcomes of multimodal training for healthcare professionals at an AIDS education and training center. Eval Health Prof. 2009;32(1):3–22. doi: 10.1177/0163278708328736. [DOI] [PubMed] [Google Scholar]
- 33.Culyba RJ, McGee BT, Weyer D. Changing HIV clinical knowledge and skill in context: the impact of longitudinal training in the Southeast United States. J Assoc Nurses AIDS Care. 2011;22(2):128–139. doi: 10.1016/j.jana.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 34.Landon BE, Wilson IB, Cohn SE, et al. Physician specialization and antiretroviral therapy for HIV. J Gen Intern Med. 2003;18(4):233–241. doi: 10.1046/j.1525-1497.2003.20705.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 165 kb)