Abstract
Background
On 11 March 2011, the Tohoku earthquake and tsunami struck off the coast of northeastern Japan. Within 3 weeks, an increased number of pneumonia admissions and deaths occurred in local hospitals.
Methods
A multicentre survey was conducted at three hospitals in Kesennuma City (population 74 000), northern Miyagi Prefecture. All adults aged ≥18 years hospitalised between March 2010 and June 2011 with community-acquired pneumonia were identified using hospital databases and medical records. Segmented regression analyses were used to quantify changes in the incidence of pneumonia.
Results
A total of 550 pneumonia hospitalisations were identified, including 325 during the pre-disaster period and 225 cases during the post-disaster period. The majority (90%) of the post-disaster pneumonia patients were aged ≥65 years, and only eight cases (3.6%) were associated with near-drowning in the tsunami waters. The clinical pattern and causative pathogens were almost identical among the pre-disaster and post-disaster pneumonia patients. A marked increase in the incidence of pneumonia was observed during the 3-month period following the disaster; the weekly incidence rates of pneumonia hospitalisations and pneumonia-associated deaths increased by 5.7 times (95% CI 3.9 to 8.4) and 8.9 times (95% CI 4.4 to 17.8), respectively. The increases were largest among residents in nursing homes followed by those in evacuation shelters.
Conclusions
A substantial increase in the pneumonia burden was observed among adults after the Tohoku earthquake and tsunami. Although the exact cause remains unresolved, multiple factors including population aging and stressful living conditions likely contributed to this pneumonia outbreak.
Keywords: Pneumonia, Respiratory Infection, Bacterial Infection
Key messages.
What is the key question?
Did the pneumonia incidence increase among the adult population after the Tohoku earthquake/tsunami, what were the characteristics of the disaster-associated pneumonia?
What is the bottom line?
Our survey in a well defined population of northern Miyagi Prefecture revealed that a marked increase in the incidence of pneumonia hospitalisations and pneumonia-associated deaths was observed during the 3-month period following the disaster, the vast majority of the victims were older people, only 3.6% were associated with near-drowning in the tsunami waters, and the clinical and microbiological characteristics of the post-disaster patients were similar to those of the pre-disaster patients.
Why read on?
Because this disaster affected a notably aging population with the highest baseline pneumonia incidence rate, the disaster caused a drastic increase in the number of admissions and placed a heavy burden on local hospitals. In addition to using the pneumococcal vaccine for disaster-affected populations, the provision of optimal living conditions, medical check-ups and oral hygiene care must be a priority for older people after natural disasters.
Introduction
On 11 March 2011, a magnitude 9.0 earthquake struck off the northeastern coast of Japan. Within an hour of the earthquake, devastating tsunamis swept over the east coast of the Tohoku Region, resulting in approximately 20 000 deaths and catastrophic damage to the local infrastructure and environment.1 2 As a result of the extensive destruction of homes, more than 400 000 displaced people were moved to emergency evacuation shelters that were not supplied with electricity, gas, water or food, despite sub-freezing winter temperatures.3 4
Previous studies showed that acute respiratory infections were frequently observed among people displaced by the 2001 earthquake in El Salvador,5 among those affected by the 2003 Bam earthquake in Iran6 and among people in Aceh Province affected by the 2004 Indian Ocean earthquake and tsunami.7 Furthermore, severe pneumonia associated with the aspiration of seawater, known as ‘tsunami lung’, was reported in areas affected by the Indian Ocean tsunami.8–10 However, these studies were conducted in resource-limited settings without reliable baseline data and lacked a standardised case definition. The impact of natural disasters, including tsunamis, on the risk of pneumonia remains largely unknown.
Within 3 weeks of the earthquake and tsunami on 11 March, a rapid increase in pneumonia hospitalisations and related deaths in northern Miyagi Prefecture was reported by mass media outlets.11 We undertook an investigation to elucidate the impact of the Tohoku earthquake/tsunami on the incidence of pneumonia-related hospitalisations and mortality among adults aged ≥18 years in Kesennuma. We also sought to describe the clinical characteristics of disaster-related pneumonia and investigate the potential causes of increased rates of pneumonia in the affected population.
Methods
Setting
Kesennuma is located on the northeastern coast of Miyagi Prefecture (figure 1). The city has a long, saw-toothed coastline with narrow, flat land facing the Pacific Ocean. The total population in February 2011 was 74 257 (source: Department of Vital Statistics, Kesennuma City). The city inhabitants included a substantial number of older adults: 30.2% (n=22 421) were aged ≥65 years and 8.9% (n=6618) were aged ≥80 years. These percentages were higher than the national averages (23% and 6.4%, respectively). At the time of the disaster, no national programme for the administration of the 23 valent polysaccharide pneumococcal vaccine (PPV23) existed in Japan, and its coverage among Kesennuma residents aged ≥65 years was <5%.
Figure 1.
Area affected by the Tohoku earthquake and tsunami, Kesennuma City, Miyagi Prefecture. The disaster area data were obtained from the overview map of tsunami-affected areas released by the Geospatial Information Authority of Japan (http://www.gsi.go.jp/BOUSAI/h23_tohoku.html).
At 14 : 46 local time on 11 March 2011, the earthquake shook Kesennuma. The first large tsunami wave hit Kesennuma within a half hour of the earthquake, resulting in the deaths of 1032 residents; an additional 324 residents were listed as missing. The majority (>90%) of the victims died from drowning.2
The tsunamis devastated buildings, cars, ships and all other structures. Major oil tanks in the port were damaged and leaked petroleum, leading to massive conflagrations in the city. The main road was demolished to the north and the south, and the city was isolated (figure 1). In the aftermath, residents fled to evacuation shelters, including schools and public halls, to relatives’ houses located on higher ground. The number of evacuees reached a peak on 17 March 2011 (20 105 individuals at 99 sites), while many other residents remained in their partially damaged houses.
In early April 2011, a considerable increase in pneumonia hospitalisations was reported from hospitals in northern Miyagi Prefecture. Media outlets reported that the outbreak may have been related to exposure to dried oil mist (ie, oil leaked from damaged storage tanks) or contaminated tsunami water.
Study design
In response to this outbreak, the Kesennuma City Hospital (KCH), the Kesennuma City Medical Association and Nagasaki University established an investigation team and initiated a multicentre survey on 12 May. The team identified three hospitals in Kesennuma that were providing inpatient care for patients with pneumonia before the disaster (KCH, 451 beds; Kesennuma Motoyoshi Hospital (KMH), 38 beds; and Ohtomo Hospital (OH), 78 beds). The team also identified an orthopaedic hospital and some clinics that had a small number of pneumonia admissions before the disaster (approximately 10 cases per year in total); however, their buildings were completely demolished, and their patients’ records were unavailable. Therefore, we did not include those cases.
Case ascertainment
For the study period (defined as 1 March 2010 to 30 June 2011), all patients who were hospitalised with a diagnosis of pneumonia were enumerated from existing hospitalisation databases. Working as a panel, three qualified pulmonologists reviewed medical charts and chest radiographs (CXRs) in September 2011 using a standardised case definition based on the British Thoracic Society guidelines.12 After reviewing the medical charts and CXRs, the panel's consensus CXR interpretations were recorded. Patients were classified as having any pneumonia if they showed pulmonary consolidation on CXR and any respiratory symptoms consistent with pneumonia. If a patient developed the disease 48 h after admission, the patient was classified as having hospital-acquired pneumonia and was excluded from further analysis. Repeated episodes of pneumonia in the same patient within a 2-week period were regarded as a single episode.
While inspecting hospitalisation records and CXRs, we realised that a considerable proportion of paper-based medical charts and CXRs in KMH were lost or damaged by the tsunami, and only discharge summaries were available. Therefore for analysis, the patients were classified into one of two pneumonia case categories: (1) confirmed pneumonia (full medical records were available and the presence of consolidation was confirmed by pulmonologists) and (2) probable pneumonia (detailed data and CXRs were not available, but the history described in the summary records was compatible with pneumonia). We defined pneumonia episodes as near-drowning related if patients were engulfed by the tsunami water on 11 March 2011, and their disease onset occurred within 4 weeks of the disaster.
Data collection
Demographic, clinical, radiographic, microbiological and evacuation site information was collected from the medical charts using a standardised abstraction form. The patients’ addresses before the disaster were extracted from the hospital database and converted to geographical coordinates. Patients with pneumonia who died in any of the three study hospitals were categorised as fatal cases. The severity of pneumonia was assessed using the CURB65 scoring system.13 Microbiological tests were routinely performed for clinically suspected cases throughout the study period at KCH, but they were not available at the other hospitals.
Data analysis
The demographic and clinical characteristics of the study patients were compared between the pre-disaster and post-disaster periods using χ2 and Fisher's exact tests. The near-drowning-related cases were excluded from this comparison because the cause of disease was clear. The factors associated with death were assessed using Poisson regression models with robust SEs.14 Pneumonia incidence and mortality rate calculations were limited to patients living in Kesennuma. The effects of the disaster, defined as a change in the weekly incidence of hospitalisations and associated deaths after the disaster (ie, the incidence rate ratios), were separately assessed using segmented generalised linear Poisson regression models allowing for overdispersion.15 The regression models included terms for the disaster and time trends before and after the disaster. The change in the population size due to the disaster was taken into account using the offset function. Partial correlograms were used to assess serial autocorrelation of the residuals and, since there was no detectable autocorrelation, the data were modelled assuming independence.
Ethics
This study was approved by the Institutional Review Board of KCH.
Results
Patients
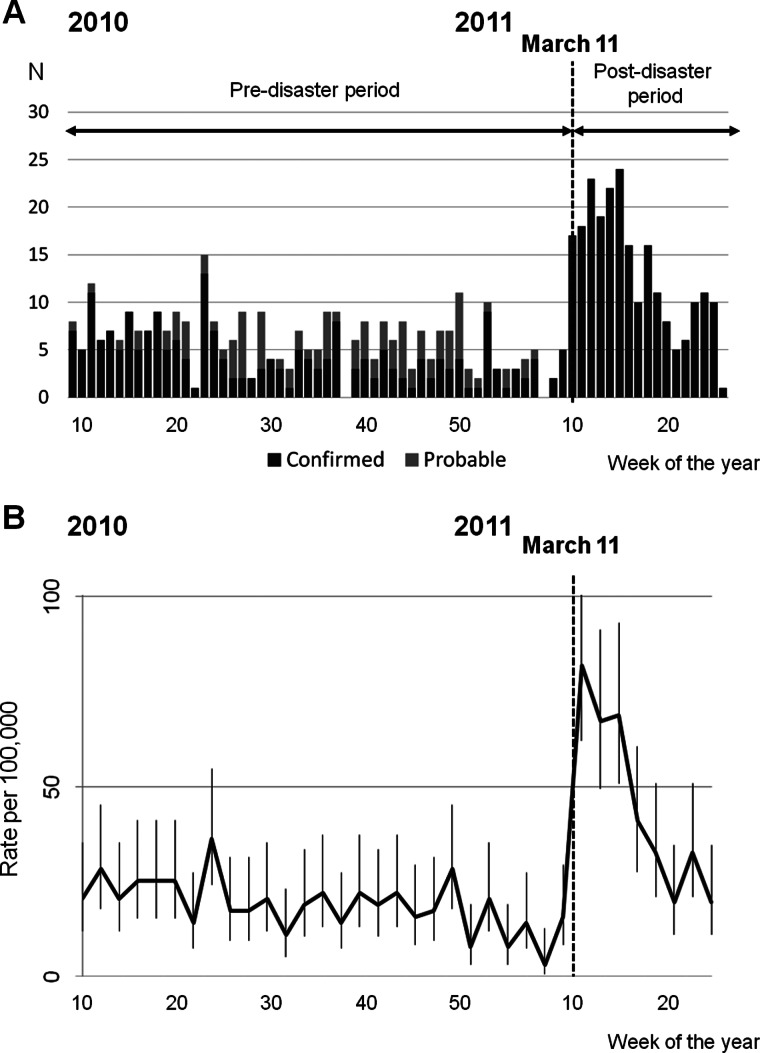
Over the course of the study period (1 March 2010 to 30 June 2011), a total of 550 pneumonia cases were identified from hospital and facility records. According to the patients’ disease onset, 225 confirmed cases and 100 probable cases occurred before 11 March and 225 confirmed cases occurred after 11 March (see online supplementary appendix figure 1). There was a sharp rise in the weekly number of pneumonia hospitalisations shortly after the disaster (figure 2A). A majority of the patients (95%) were city residents and their geographical distribution was similar across the study periods (see online supplementary appendix figure 2 ). When only city residents were included in the analysis, the highest incidence rate occurred during the first 2 weeks after the disaster, and the incidence declined to the baseline level by mid-June 2011 (figure 2B).
Figure 2.
Trend of pneumonia hospitalisations in Kesennuma City, March 2010 to June 2011. (A) Weekly number of confirmed and probable cases according to the date of onset. (B) Biweekly incidence rates (per 100 000 people) calculated according to the date of onset. Cases were limited to the residents of Kesennuma City. The vertical lines indicate 95% CI.
To understand changes in the incidence of pneumonia, we compared the periods before (1 March 2010–10 March 2011) and after (11 March–30 June 2011) the disaster (table 1). The demographic and clinical pictures of disaster-related pneumonia were similar to those of pre-disaster cases, except that a substantial proportion (27.7%) of post-disaster patients were living in evacuation shelters. Nearly 90% of patients were older adults aged ≥65 years. The patients who were identified from evacuation shelters were younger (average age 76.7 years vs 80 years, p=0.047), less likely to have underlying medical conditions (45% vs 59.9%, p=0.049) and less likely to have fatal pneumonia (10% vs 29.3%, p=0.003) than patients with pneumonia identified from residences and nursing homes.
Table 1.
Characteristics of confirmed pneumonia cases by residence, before and after the 2011 Tohoku earthquake and tsunami, Kesennuma City, Miyagi, Japan
| Pre-disaster period (1 March 2010–10 March 2011)† | Post-disaster period (11 March–30 June 2011)† | |||||||
|---|---|---|---|---|---|---|---|---|
| Residential category* | Residential category** | Pre-disaster vs post-disaster period p Value‡ | ||||||
| Characteristics | Total (n=225) | Home (n=193) | Nursing home (n=32) | Total (n=217) | Home (n=117) | Nursing home (n=40) | Evacuation shelter (n=60) | |
| Female sex (%) | 98 (43.6) | 77 (39.9) | 21 (65.6) | 93 (42.9) | 46 (39.3) | 26 (65) | 21 (35) | 0.882 |
| Age category (%) | ||||||||
| 18–49 years | 13 (5.8) | 12 (6.2) | 1 (3.1) | 4 (1.8) | 3 (2.6) | 0 (0) | 1 (1.7) | 0.161§ |
| 50–64 years | 21 (9.3) | 20 (10.4) | 1 (3.1) | 18 (8.3) | 10 (8.6) | 3 (7.5) | 5 (8.3) | |
| 65–79 years | 61 (27.1) | 56 (29) | 5 (15.6) | 67 (30.9) | 32 (27.4) | 6 (15) | 29 (48.3) | |
| ≥80 years | 130 (57.8) | 105 (54.4) | 25 (78.1) | 128 (59) | 72 (61.5) | 31 (77.5) | 25 (41.7) | |
| Duration of symptoms before admission (%) | ||||||||
| ≤2 days | 109 (48.4) | 91 (47.2) | 18 (56.3) | 114 (52.5) | 59 (50.4) | 25 (62.5) | 30 (50) | 0.434 |
| 3 days or more | 109 (48.4) | 96 (49.7) | 13 (40.6) | 98 (45.2) | 54 (46.2) | 14 (35) | 30 (50) | |
| Antibiotics prescribed before admission (%) | 32 (14.2) | 23 (11.9) | 9 (28.1) | 29 (13.4) | 7 (6) | 10 (25) | 12 (20) | 0.794 |
| With underlying conditions (%) | 129 (57.3) | 107 (55.4) | 22 (68.7) | 121 (55.8) | 64 (54.7) | 30 (75) | 27 (45) | 0.739 |
| CURB65 score (%) | ||||||||
| 3–5 (severe) | 26 (11.6) | 23 (11.9) | 3 (9.4) | 27 (12.4) | 10 (8.6) | 13 (32.5) | 4 (6.7) | 0.916 |
| 0–2 (less severe) | 186 (82.7) | 159 (82.4) | 27 (84.4) | 179 (82.5) | 97 (82.9) | 26 (65) | 56 (93.3) | |
| Deceased (%) | 39 (17.3) | 31 (16.1) | 8 (25) | 52 (24) | 28 (23.9) | 18 (45) | 6 (10) | 0.085 |
| Microbiological tests performed | 145 (64.4) | 129 (66.8) | 16 (50) | 139 (64.1) | 74 (63.3) | 22 (55) | 43 (71.7) | 0.932 |
| Positive for Streptococcus pneumoniae¶ | 15 (6.7) | 13 (6.7) | 2 (6.3) | 22 (10.1) | 9 (7.7) | 4 (10) | 9 (15) | 0.402 |
| Positive for Haemophilus influenzae | 3 (1.3) | 3 (1.5) | 0 (0) | 14 (6.5) | 7 (6) | 0 (0) | 7 (11.7) | 0.013§ |
| Positive for Klebsiella pneumoniae | 8 (3.6) | 6 (3.1) | 2 (6.2) | 11 (5.1) | 5 (4.3) | 4 (10) | 2 (3.3) | 0.698 |
*The characteristics differed by residential categories for gender (p=0.007) and pre-hospital antibiotic treatment (p=0.015).
†The pre-disaster and pos-disaster cases were categorised according to the date of onset. The near-drowning-related cases were excluded.
‡Characteristics were compared between the pre-disaster and post-disaster cases. χ2 tests were performed unless otherwise indicated.
§Fisher's exact test.
¶Either a bacterial culture was isolated or a rapid urinary antigen test was positive.
**The characteristics differed by residential categories for gender (p=0.006), age group (p=0.012), pre-hospital antibiotic treatment (p=0.002), presence of underlying conditions (p=0.012), clinical severity (p<0.001) and fatality (p<0.001).
The patients identified from nursing homes were predominantly women, older and more likely to have had underlying conditions than were patients from homes and evacuation shelters. The proportion of patients with severe pneumonia with CURB65 ≥3 was high among patients from nursing homes, and those patients were more likely to die in the post-disaster period than in the pre-disaster period.
Incidence rates
During the three and a half months following 11 March, the weekly incidence of pneumonia hospitalisations increased by 5.7 times (95% CI 3.9 to 8.4) from the baseline level (table 2). The age group specific ratios were similar across all generations, whereas the absolute increase in the incidence was substantially greater among older people, especially those aged ≥80 years (the rate difference, 156.3 (95% CI 90.8 to 221.9) per 100 000 per population-week). The admission rate ratio was highest among nursing home residents followed by the residents of evacuation shelters. For pneumonia-related deaths, the rate increased by 8.9 times (95% CI 4.4 to 17.8) from the baseline level, and the mortality rate ratio was highest among nursing home residents.
Table 2.
Incidence of pneumonia hospitalisations and pneumonia-associated mortality among people aged ≥18 years before and after the 2011 Tohoku earthquake and tsunami, Kesennuma City, Miyagi, Japan
| Pre-disaster period (1 March 2010–10 March 2011)* | Post-disaster period (11 March 2011–30 June 2011)* | ||||||
|---|---|---|---|---|---|---|---|
| Pop.† | N‡ | Weekly incidence rate§ (95% CI) | Pop.† | N‡ | Weekly incidence rate§ (95% CI) | Rate ratio (95% CI)¶ | |
| Pneumonia hospitalisations | |||||||
| Total | 63365 | 305 | 9.2 (8 to 10.4) | 61104 | 208 | 38.3 (28.6 to 48) | 5.7 (3.9 to 8.4) |
| Age category (years) | |||||||
| 18–49 | 23354 | 14 | 1 (0.4 to 1.5) | 22291 | 6 | 3.6 (-0.4 to 7.7) | 10 (1.9 to 54.3) |
| 50–64 | 17590 | 24 | 2.5 (1.3 to 3.6) | 17245 | 18 | 7.3 (0.6 to 14) | 6.1 (1.5 to 24.7) |
| 65–79 | 15803 | 85 | 10.6 (8.2 to 13.1) | 15241 | 62 | 62.6 (37.5 to 87.7) | 6.2 (3.3 to 11.5) |
| 80+ | 6618 | 182 | 52.3 (43.8 to 60.8) | 6327 | 122 | 193.3 (129.1 to 257.5) | 5.2 (3.2 to 8.5) |
| Residence location | |||||||
| Home | 62239 | 262 | 8.1 (7 to 9.2) | 54460 | 111 | 21 (12.9 to 29) | 2.7 (1.7 to 4.4) |
| Nursing home | 1126 | 43 | 57 (38.6 to 75.5) | 796 | 38 | 882.8 (481.3 to 1284.3) | 28.2 (11.7 to 68) |
| Evacuation shelter | – | – | – | 5848 | 59 | 328.7 (190.8 to 466.7) | 10.2 (6.2 to 16.9) |
| Pneumonia-associated deaths | |||||||
| Total | 63365 | 55 | 1.6 (1.2 to 2.1) | 61104 | 49 | 12.8 (7.5 to 18.1) | 8.9 (4.4 to 17.8) |
| Age category (years) | |||||||
| 18–79 | 56747 | 13 | 0.4 (0.2 to 0.7) | 54777 | 12 | 8.7 (3 to 14.4) | 18.6 (5.3 to 64.9) |
| 80- | 6618 | 42 | 12 (8.5 to 15.5) | 6327 | 37 | 66.3 (32.8 to 99.8) | 6.7 (3 to 14.8) |
| Residence location | |||||||
| Home | 62239 | 46 | 1.4 (1 to 1.8) | 54460 | 27 | 7.1 (2.7 to 11.5) | 4.8 (2 to 11.2) |
| Nursing home | 1126 | 9 | 12.4 (4.5 to 20.3) | 796 | 17 | 555.2 (216.6 to 893.7) | 40.6 (9.1 to 180.8) |
| Evacuation shelter | – | – | – | 5848 | 5 | 80.6 (0.2 to 160.9) | 11.6 (3.7 to 36.2) |
*The pre-disaster and post-disaster cases were categorised according to the date of onset. The near-drowning-related cases were excluded.
†Population in 28 February 2011 for the pre-disaster period and in 31 May 2011 for the post-disaster period. The population in each residential category reflects the period average. Data provided by Kesennuma City Hall.
‡Number of patients living in Kesennuma.
§Per 100 000 people. Weekly incidence rates were estimated using segmented generalised linear Poisson regression models allowing for time trends and the change in the population size.
¶Rate ratios were estimated using segmented generalised linear Poisson regression models. Rate ratios for evacuation shelter residents were estimated using the overall pre-disaster incidence as a reference.
Pneumonia aetiologies
Streptococcus pneumoniae, Haemophilus influenzae and Klebsiella pneumoniae were the leading causative pathogens identified in pre-disaster and post-disaster pneumonia cases. The positivity of H influenzae increased by fourfold after 11 March, especially among patients from evacuation shelters. Staphylococcus aureus was also found in patients throughout the study period, but its causative role was unclear (see online supplementary appendix table 1). None of the patients in this study were reported to have had positive rapid tests for influenza (the percentages tested before and after the disaster were 11.4% and 17.9%, respectively) or Legionella pneumophila serogroup 1 (28.4% and 35.5%, respectively).
Risk factors for death
Both before and after 11 March, a higher CURB65 score was significantly associated with an increased risk of death; the mortality also increased by age group, but the statistical evidence of this increase was weak. After the disaster, male gender and pre-hospital antibiotics use were associated with a higher risk of death after adjusting for other factors, and staying at an evacuation shelter was associated with a lower risk of death, although the significance was only marginal after adjustment. However, their effects on death were similar to the baseline figures (see online supplementary appendix table 2).
Near-drowning-related pneumonia
A history of exposure to tsunami water on 11 March was recorded in 10 patients. Among them, eight (3.6% of the disaster-related cases) were near-drowning-related pneumonia; seven were women, three were inside a car when engulfed by the tsunami, and one died from the disease. The median age was younger than that of other disaster-related pneumonia patients (62 years vs 79 years, p<0.001).
Discussion
In this report, we documented a substantial increase in the rate of pneumonia-related hospital admissions and deaths in Kesennuma among adults of all age groups soon after the Tohoku earthquake and tsunami. The clinical and microbiological characteristics of the post-disaster patients were similar to those of the pre-disaster patients. The vast majority of the victims were older people. Because this disaster affected a notably aging population with the highest baseline pneumonia incidence rate, the disaster caused a drastic increase in the number of admissions and placed a heavy burden on local hospitals.
Although the causal mechanism was not fully established, our findings suggested that multiple factors have contributed to this outbreak. The largest increase in the pneumonia burden was observed in nursing home residents, the majority of which were older people with physical and mental limitations and needed assistance with daily activities. A sudden change in their living environment after the disaster, such as a lack of appropriate nutrition, the loss of regular medicines and a shortage of caregivers, must have worsened their conditions.16 It should be noted that many caregivers were also victims who lost their families, friends and homes. This may have been reflected by the fact that the highest mortality rate among patients from nursing homes occurred in the early post-disaster period (results not shown). A high incidence was also observed in the residents of evacuation shelters. Crowding is a risk factor for S pneumoniae and H influenzae infection,17 18 and we found that these pathogens, particularly H influenzae, were isolated more frequently in patients from evacuation shelters.
The increased incidence observed in all residential places suggests that other factors which were shared by all survivors have also played an important role. First, hypothermia is known to increase the risk of subsequent infections, including pneumonia.19 20 On 11 March, it was snowing in northern Miyagi. All survivors were suddenly left without running water, gas, electricity or oil in freezing weather (−3 to −5°C at night; see online supplementary appendix figure 3). The majority of the evacuation shelters were not sufficiently equipped with heating and blankets immediately after the disaster. Second, people experience stress reactions after the disaster. Psychological stress weakens the immune system and may increase the risk of respiratory infections.21 22 Third, the medical supply systems have drastically changed. Soon after the disaster, more than a hundred relief teams arrived in Kesennuma and initiated care for survivors; this change may have increased the chance of identifying patients with pneumonia.
The abovementioned reasons also explain the decline in pneumonia cases after May; the temperature increase, improvements in living conditions (water, gas and electricity had been fully restored by the end of May), recovery of medical supplies, and the decline in the number of evacuees reduced the risks of pneumonia. However, in our study, it was impossible to know what factors have truly contributed to this outbreak.
Pneumonia outbreaks after natural disasters have never been documented in the past. In 2005, Nishikiori and colleagues conducted a cross-sectional survey (n=3533 individuals) in Sri Lanka after the Indian Ocean tsunami,23 and no deaths were reported between one week and two and a half months after the tsunami. The different findings in Sri Lanka may be explained by the difference in population structures. If we projected our age group-specific estimates onto a population in Sri Lanka, where the proportions of people aged ≥65 years and ≥80 years in 2004 were 7% and <0.5%, respectively, the overall impact on pneumonia admission and mortality would decrease by almost 80%. Therefore, it is plausible that the impact of disasters on pneumonia incidence was overlooked in developing countries with relatively young populations.
A comparable event may have been observed in Japan after the Hanshin-Awaji earthquake that occurred in Hyogo Prefecture (where 15% of the population were aged ≥65 years) in January 1995. Among 1948 patients admitted for illness during the first 15 days after the earthquake, 418 (21%) had pneumonia. Their average age was 66 years,24 although population-based impact estimates were unavailable. In contrast, no pneumonia outbreak was documented after Hurricane Katrina, which occurred during the summer.25 26 Freezing temperatures may be a critical factor in pneumonia outbreaks after a disaster.
In our study, eight cases of near-drowning-related pneumonia were identified. Pneumonia associated with the aspiration of tsunami water drew global attention after a series of melioidosis cases among the Indian Ocean tsunami survivors was reported.8–10 This condition has been sometimes referred to as ‘tsunami lung’, which is defined as pneumonia caused by the aspiration of tsunami water containing soil, oil and sewage.27 28 However, there is no evidence that this condition is distinct from seawater drownings unrelated to tsunami disasters. Furthermore, the clinical characteristics of victims of the Indian Ocean tsunami may not be comparable to those of patients in settings where Burkholderia pseudomallei is not endemic, as in our case. Natural disasters do not cause new diseases that are not endemic to the affected area.29–31 The term ‘tsunami lung’ must be used with caution to avoid media sensationalism.
The limitations of our study arise from the nature of hospital-based data collection. In Japan, 70% of the medical costs for people aged <70 years and 80–90% of the medical costs for people aged ≥70 years are covered by insurance,32 and all medical fees for the disaster-affected people were waived after 11 March.33 The cost was not a barrier to hospitalisation throughout the study period. Non-pneumonia diseases, such as heart failure, might have been misdiagnosed as pneumonia during the post-disaster period especially among older patients. However, the cases in this study were confirmed by experts using a standardised case definition, and the microbiological confirmation rate was similar between the pre-disaster and post-disaster period. Thus, the impact of misclassification and potential changes in admission criteria on our incidence estimates must be minimal. However, due to the limited microbiological data, the aetiology of our cases was not fully established.
Pneumonia and pneumonia-related deaths among older people have been overlooked in emergency preparedness and humanitarian responses, most likely because both are common events in this population. The key findings of our study are: disaster-affected people, especially those exposed to stressful living conditions, are at high risk of developing pneumonia and pneumonia-related death during the emergency phase of a disaster; and the pneumonia burden becomes substantial in areas with an aging population. This situation may arise in low-income and middle-income countries, as their populations are rapidly aging.34 In addition to using the PPV23 or pneumococcal conjugate vaccine for disaster-affected populations, the provision of optimal living conditions, medical check-ups and oral hygiene care must be a priority for older people after natural disasters.35
Supplementary Material
Acknowledgments
The authors are grateful to the staff at Kesennuma City Hospital for their technical support, and to Ms Michiko Sasaki of Kesennuma Motoyoshi Hospital for her field support.
Footnotes
Contributors: HD, MS and SO formulated the research question and designed the study. HD, MS and KA wrote research grants. HD, MS, JS, HO, KM, MI, WE and SO collected the clinical and demographic data. HD, MS, TK, MH and KA analysed the data. HD, MS, PEK, KM, TK, HO, MH, KH, KA and SO interpreted the findings. HD, MS, PEK, KA and SO wrote the report. HD and MS contributed equally.
Funding: This work was supported by the Kesennuma City Hospital, Nagasaki University, Daiwa Securities Health Foundation, and the Japanese Ministry of Education, Culture, Sports, Science & Technology (JSPS KAKENHI Grant Number 24790801). The study sponsors were not involved in the study design and the collection, analysis and interpretation of data, or the writing of the article or the decision to submit it for publication. The authors were independent from the study sponsors.
Competing interests: None.
Ethics approval: The Institutional Review Board of Kesennuma City Hospital.
Provenance and peer review: Not commissioned; internally peer reviewed.
Open Access: This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/3.0/
References
- 1.Nagamatsu S, Maekawa T, Ujike Y, et al. The earthquake and tsunami—observations by Japanese physicians since the 11 March catastrophe. Crit Care 2011;15:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Damage situation and police countermeasures associated with 2011 Tohoku district—off the Pacific Ocean Earthquake, March 28, 2012. National Police Agency of Japan; 2012. http://www.npa.go.jp/archive/keibi/biki/higaijokyo_e.pdf (accessed 10 Feb 2013). [Google Scholar]
- 3.McCurry J. Japan: the aftermath. Lancet 2011;377:1061–2 [DOI] [PubMed] [Google Scholar]
- 4.Cabinet Office Government of Japan Transition of the number of evacuees after the Great East Japan Earthquake. Cabinet Office, Government of Japan; http://www.cao.go.jp/shien/en/2-count/annex1-2.pdf (accessed 7 February 2013). [Google Scholar]
- 5.Woersching JC, Snyder AE. Earthquakes in El Salvador: a descriptive study of health concerns in a rural community and the clinical implications, part I. Disaster Manag Response 2003;1:105–9 [DOI] [PubMed] [Google Scholar]
- 6.Akbari ME, Farshad AA, Asadi-Lari M. The devastation of Bam: an overview of health issues 1 month after the earthquake. Public Health 2004;118:403–8 [DOI] [PubMed] [Google Scholar]
- 7.Guha-Sapir D, van Panhuis WG. Health impact of the 2004 Andaman Nicobar earthquake and tsunami in Indonesia. Prehosp Disaster Med 2009;24:493–9 [DOI] [PubMed] [Google Scholar]
- 8.Chierakul W, Winothai W, Wattanawaitunechai C, et al. Melioidosis in 6 tsunami survivors in southern Thailand. Clin Infect Dis 2005;41:982–90 [DOI] [PubMed] [Google Scholar]
- 9.Allworth AM. Tsunami lung: a necrotising pneumonia in survivors of the Asian tsunami. Med J Aust 2005;182:364. [DOI] [PubMed] [Google Scholar]
- 10.Athan E, Allworth AM, Engler C, et al. Melioidosis in tsunami survivors. Emerg Infect Dis 2005;11:1638–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pneumonia cases rise in Tohoku. The Japan Times. 2011 10 April. [Google Scholar]
- 12.Levy ML, Le Jeune I, Woodhead MA, et al. Primary care summary of the British Thoracic Society Guidelines for the management of community acquired pneumonia in adults: 2009 update. Endorsed by the Royal College of General Practitioners and the Primary Care Respiratory Society UK. Prim Care Respir J 2010;19:21–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chalmers JD, Singanayagam A, Akram AR, et al. Severity assessment tools for predicting mortality in hospitalised patients with community-acquired pneumonia. Systematic review and meta-analysis. Thorax 2010;65:878–83 [DOI] [PubMed] [Google Scholar]
- 14.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 2003;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27:299–309 [DOI] [PubMed] [Google Scholar]
- 16.Tanida N. What happened to elderly people in the great Hanshin earthquake. BMJ 1996;313:1133–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watanabe H, Batuwanthudawe R, Thevanesam V, et al. Possible prevalence and transmission of acute respiratory tract infections caused by Streptococcus pneumoniae and Haemophilus influenzae among the internally displaced persons in tsunami disaster evacuation camps of Sri Lanka. Intern Med 2007;46:1395–402 [DOI] [PubMed] [Google Scholar]
- 18.Dagan R, Gradstein S, Belmaker I, et al. An outbreak of Streptococcus pneumoniae serotype 1 in a closed community in southern Israel. Clin Infect Dis 2000;30:319–21 [DOI] [PubMed] [Google Scholar]
- 19.Pio A, Kirkwood BR, Gove S. Avoiding hypothermia, an intervention to prevent morbidity and mortality from pneumonia in young children. Pediatr Infect Dis J 2010;29:153–9 [DOI] [PubMed] [Google Scholar]
- 20.Laupland KB, Zahar JR, Adrie C, et al. Severe hypothermia increases the risk for intensive care unit-acquired infection. Clin Infect Dis 2012;54:1064–70 [DOI] [PubMed] [Google Scholar]
- 21.Baker DG, Nievergelt CM, O'Connor DT. Biomarkers of PTSD: neuropeptides and immune signaling. Neuropharmacology 2012;62:663–73 [DOI] [PubMed] [Google Scholar]
- 22.Luft BJ, Schechter C, Kotov R, et al. Exposure, probable PTSD and lower respiratory illness among World Trade Center rescue, recovery and clean-up workers. Psychol Med 2012;42:1069–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nishikiori N, Abe T, Costa DG, et al. Timing of mortality among internally displaced persons due to the tsunami in Sri Lanka: cross sectional household survey. BMJ 2006;332:334–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matsuoka T, Yoshioka T, Oda J, et al. The impact of a catastrophic earthquake on morbidity rates for various illnesses. Public Health 2000;114:249–53 [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention Mortality associated with Hurricane Katrina—Florida and Alabama, August–October 2005. MMWR Morb Mortal Wkly Rep 2006;55:239–42 [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention Morbidity surveillance after Hurricane Katrina—Arkansas, Louisiana, Mississippi, and Texas, September 2005. MMWR Morb Mortal Wkly Rep 2006;55:727–31 [PubMed] [Google Scholar]
- 27.Inoue Y, Fujino Y, Onodera M, et al. Tsunami lung. J Anesth 2012;26:246–9 [DOI] [PubMed] [Google Scholar]
- 28.Potera C. In disaster's wake: tsunami lung. Environ Health Perspect 2005;113:A734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Floret N, Viel JF, Mauny F, et al. Negligible risk for epidemics after geophysical disasters. Emerg Infect Dis 2006;12:543–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watson JT, Gayer M, Connolly MA. Epidemics after natural disasters. Emerg Infect Dis 2007;13:1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kouadio IK, Aljunid S, Kamigaki T, et al. Infectious diseases following natural disasters: prevention and control measures. Expert Rev Anti Infect Ther 2012;10:95–104 [DOI] [PubMed] [Google Scholar]
- 32.Ikegami N, Yoo BK, Hashimoto H, et al. Japanese universal health coverage: evolution, achievements, and challenges. Lancet 2011;378:1106–15 [DOI] [PubMed] [Google Scholar]
- 33.The Ministry of Health Law Medical fees for the disaster-affected people in Tohoku Region. The Ministry of Health, Labor and Welfare; 2011. http://www.med.or.jp/etc/eq201103/hoken/110311eq9.pdf (accessed 10 Feb 2013). [Google Scholar]
- 34.Lutz W, Sanderson W, Scherbov S. The coming acceleration of global population ageing. Nature 2008;451:716–19 [DOI] [PubMed] [Google Scholar]
- 35.Terpenning M. Geriatric oral health and pneumonia risk. Clin Infect Dis 2005;40:1807–10 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.