Summary
Rotator cuff tears are a common cause of pain and shoulder dysfunction. The prevalence of the rotator cuff tears increases with the age reaching the 80% in patients aged more than 80 year. Symptomatic shoulders usually are initially treated conservatively and then, in case of poor outcomes, with surgery. Different parameters are still used to decide between the conservative or surgical treatment in patients with rotator cuff tears. Aim of the current study is to characterize the various features used in decision making and to validate a “Prediction Score” that let us know which patients could have a good and stable outcome with non operative treatment. We enrolled 60 patients (mean age 52 years) with symptomatic rotator cuff tears who were assigned to conservative treatment and were evaluated at 6,9 and 12 months follow-up. We developed a score based on 18 clinical and radiographic parameters. 27 patients (“non conservative”) (45%) with a mean prediction score of 16.1 ± 1.7 interrupted the conservative treatment, while 33 patients (“conservative”) (55%) with an average prediction score of 11.3 ± 1.8 remained conservatively treated at last follow-up. The conservative patients were 14 years older than non conservative patients. According to the results of this study we identified a value of 13 points as a “cut-off” score to predict good results by conservative management of rotator cuff tear. These outcomes support the assumption that a predictive prognostic score may guarantee a rational approach in the management of subjects with RC tears, especially in elderly who continue to have the higher rate of recurrence and therefore could be well treated with standard conservative therapies.
Keywords: shoulder, rotator cuff, conservative treatment, prediction score
Introduction
Degenerative tear of the rotator cuff (RC) is a very common cause of pain and deficit of the shoulder. A high rate of patients after fifty years of age are affected by a RC tear and the most of them are asymptomatic (1–7). The prevalence of the RC tear increases with the age reaching the 80% in patients aged more than 80 years (8). Symptomatic shoulders in patients affected by RC tears usually are initially treated conservatively and then, in case of poor outcomes, with surgery (9–12). Often a symptomatic rotator cuff tear is associated with an asymptomatic cuff tear in the contralateral shoulder (13). The clinical outcome of the surgical treatment is still controversial due to the high percentage of recurrence tears (14–17). The factors determining the rerupture of the cuff have been described (18–20). On the contrary, the rate of successful conservative treatment varies from less than 50% to greater than 90%, in short or long term follow-up, with a wide variety of methods, duration of treatment and evaluation tools (10,11,21–23). Different parameters are still used to chooce the conservative or surgical treatment in patients with rotator cuff tears. Aim of the study is to characterize the various features used in decision making and to validate a prognostic score to predict which patients could have a good and stable outcomes with non operative treatment.
Patients and methods
Because all participating subjects followed a standard of care this study did not undergo institutional review board approval. All patients consented to voluntarily take part in this research. In January 2006, 60 consecutive patients with rotator cuff tears were prospectively enrolled. All the patients had a symptomatic rotator cuff tear. RC tears were detected with MRI (24). We excluded patients with the following associated lesions: glenohumeral osteoarthritis, A/C joint arthritis or dislocations, nerve palsy, previous shoulder surgery, calcifying tendonitis, gleno-humeral instability, SLAP lesions, rheumatoid arthritis, fractures, wheel-chair users. We also excluded subjects with cognitive limitations. Demographic data of the patients are reported in Table 1.
Table 1.
Demographic data of the population enrolled in the study.
| Variable | Data |
|---|---|
| Patients (N°) | 60 |
| Mean age, (years + SD) | 52 + 6.3 |
| Gender (M/F) (%) | 24(40)/36(60) |
| Dominant arm (right/left) (%) | 50(83)/10(17) |
| Clinical tools | Constant-Murley score VAS score |
| Conservative therapies | Rehabilitation, Laser, NSAIDs |
| Follow-ups (months) | 6 months |
| 9 months | |
| 12 months |
All cases were evaluated at baseline (enrolling time), and at 6, 9 and 12 months by three independent clinicians with expertise in shoulder surgery. The Constant-Murley score (CS) (26) was used to evaluate the outcomes in the clinical examinations. Subjective satisfaction was graded on a nominal scale (0–100) as: excellent (80–100), good (60-sual analogic scale (VAS), asking the patients “How severe is your pain” using a 10 mm line with 0 (no pain) on the left and 10 (worse pain) on the right. All the patients were followed in our unit by a therapist team who set a 6 months schedule divided in 4 phases similiar to other standard protocols of rehabilitation (10, 26):
Phase 1: pain control and self assisted excercises
Phase 2: passive soft tissue streching, active mobilization in water pool
Phase 3: strengthening exercises for humeral positioners and anterior deltoid
Phase 4: maintenance program with active and passive mobilization including home exercises.
The program included 2 weeks (3 sessions/week) of assisted mobilization in the scapular plane, external and internal rotation; from the 3rd week began active mobilization in water-pool (3 sessions/week for 1 mounth) including assisted exercises for humeral depressors, and external/internal rotators. After completing the cycle of hydrotherapy, continued supervised strengthening exercises with elastic band for anterior deltoid, humeral positioners and internal/external rotators (2 sessions/week); in this phase the patients were instructed to begin home rehabilitation including active self-assisted mobilization, streching and strengthening exercises. In subjects with positive drop-sign, exercises for external rotation were not included in the schedule. Starting from the 4th mounths, all the patients followed a program of home exercises to reinforce the humeral depressor/deltoid anterior, external/internal rotators and scapular pivot.
All patients received 10 applications of Laser therapy at the end of every section of physiotherapy in the 1st mounth; antiflogistic non steroid drugs (NSAIDs) were assumpted in case of acute pain. None had steroid injections. We developed a score based on the following 18 parameters (Table 2): age, working activity, working compensation (WC), overhead sports, trauma, shoulder pain, previous rehabilitation, rotator cuff (RC) tear, drop sign, LHB tear or instability, acromion-humeral distance, scapular dyskinesis, muscle atrophy, fatty infiltration, stiffness, active range of motion (ROM), bilateral tear. The drop-sign (27) was assessed placing the the shoulder at 0° of abduction and 45° of external rotation (Fig. 1A), then the examiner ask the patient to maintain it in this position when he left the arm. The test is positive when the forearm drops back to 0° of external rotation (Fig. 1B). Scapular dyskinesis (28) was evaluated on the patients standing with the shoulder flexed at 90° (Fig. 2). Passive stiffness was assessed in supine using a standard goniometer, active motion was measured in standing position. The questionnarie was administered to every patients at the baseline in order to obtain a mean of the scores attributed by the three surgeons.
Table 2.
Clinical and radiographic prognostic features of the rotator cuff prediction score.
| Prognostic features | points |
|---|---|
| Age | |
| > 60 years | 0 |
| < 60 years | 1 |
| Working activity | |
| light | 0 |
| heavy | 1 |
| Working compensation | |
| Yes | 0 |
| No | 1 |
| Overhead sport | |
| Yes | 1 |
| No | 0 |
| Shoulder trauma | |
| < 6 months | 1 |
| > 6 months | 0 |
| Previous rehabilitation | |
| Yes | 1 |
| No | 0 |
| RC tear | |
| complete | 1 |
| partial | 0 |
| Subscapularis tear | |
| Yes | 1 |
| No | 0 |
| Bilateral tear | |
| Yes | 0 |
| No | 1 |
| Drop sign | |
| Yes | 0 |
| No | 1 |
| LHB | |
| Nomal | 0 |
| Rupture | 0 |
| Instability | 1 |
| AH interval | |
| > 7 mm | 1 |
| < 7 mm | 0 |
| Scapular dyskinesis | |
| Yes | 0 |
| No | 1 |
| RC muscle atrophy | |
| Grade I | 3 |
| Grade II | 2 |
| Grade III | 1 |
| Grade IV | 0 |
| RC fatty infiltration | |
| Grade 0 or I | 2 |
| Grade II | 1 |
| Grade III | 0 |
| Passive stiffness | |
| None or mild | 2 |
| Moderate | 1 |
| Severe | 0 |
| Active ROM | |
| > 90% | 0 |
| < 90% | 1 |
Figure 1.
A–B Clinical assessment of “drop sign”. When the examiner place the shoulder at 45° of external rotation (A) and it drop back to 0° (B) the test is positive.
Figure 2.
Patient’s position to evaluate scapular dyskinesis.
No further scores were taken at follow-up examinations to avoid changing of the patients’ treatment management. All the patients followed the previous reported rehabilitation program without variations based on the results of the score.
Statistical analysis
To ensure reliability of the final outcome scores, the pre-and post-rehabilitation program CS attributed by the three examiners were analyzed using Pearson’s intraclass correlation coefficient (ICC) to determine the realibility of repeated values collected between testers. Data were averaged out among the different results (p<0.001). Student’s t-test was used to highlight significant differences between pre- and post-rehabilitation program scores.
Results
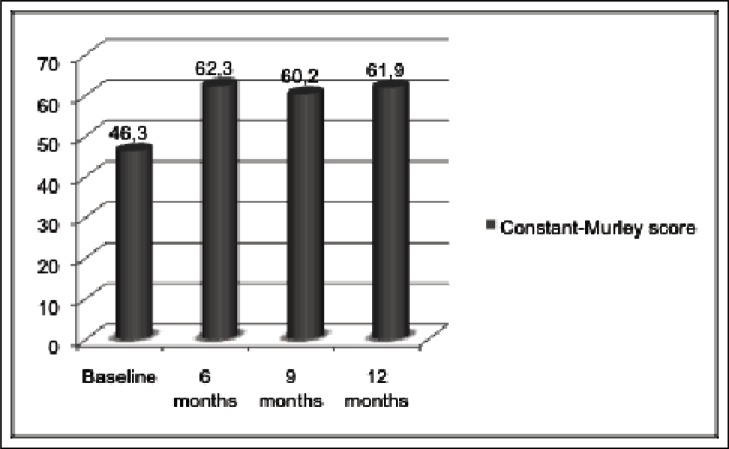
The mean age of the patients enrolled was 52 years, with 20 patients younger than 60 years (min: 40, max: 59) and 40 patients older than 60 years (min: 60, max: 80). The average CS increased significantly at all 3 follow-ups (p < 0.01) (Fig. 3); the analysis of active ROM showed a significant improvement of forward elevation and abduction (p < 0.01), the internal and external rotation remain unchanged (p > 0.05) (Table 3).
Figure 3.
Constant-Murley score of the study population at all three follow-ups.
Table 3.
Values of active ROM at all three follow-ups versus baseline.
| Follow-up | |||||||
|---|---|---|---|---|---|---|---|
| Active ROM | Baseline | 6 months | P value | 9 months | P value | 12 months | P value |
| FE (°) | 108 + 3.2 | 160 + 4.9 | 0.00895 | 150 + 6.2 | 0.00987 | 145 + 5.8 | 0.00992 |
| Abduction (°) | 92 + 2.8 | 150 + 4.3 | 0.00793 | 145 + 7.1 | 0.00679 | 140 + 6.1 | 0.00785 |
| ER(°) | 45 + 5.2 | 42 + 4.9 | 0.0673 | 47 + 3.6 | 0.0753 | 46 + 5.6 | 0.0691 |
| IR(°) | 50 + 6.4 | 52 + 3.7 | 0.0642 | 48 + 4.7 | 0.0629 | 54 + 3.5 | 0.0747 |
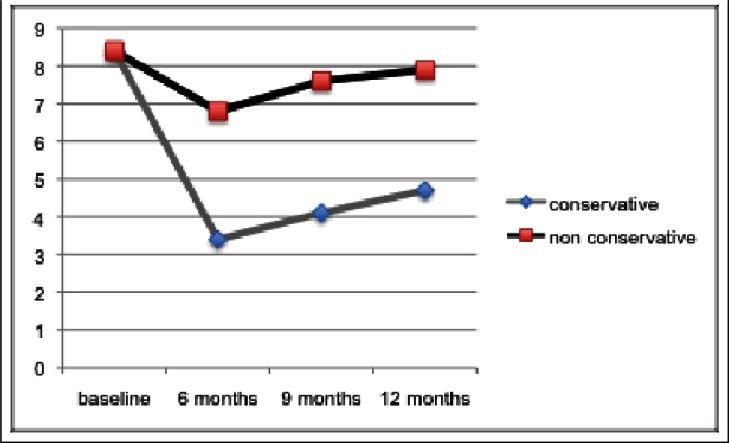
FE: forward elevation; ER: external rotation; IR: internal rotation
The conservative treatment was interrupted by 27 patients (45%) who underwent to surgical procedure. We considered failed the conservative treatment when the patients complained for persistent pain at rest and were unable to perform daily living activity. At 6 months 40 subjects (67%) were very satisfied with a mean CS of 72±6.9 (P=0.00863) and 20 cases (33%) had worse score with an average 52.1±4.5 (P=0.0692); 16 of these underwent surgical therapy. At 9 months 36 patients (60%) referred good subjective satisfaction with an average CS of 69.8±5.1 (P =0.00895) while poor outcomes were found in 8 cases (13%) with a mean CS of 50.2+4.7 (P=0.0626); 6 subjects were surgically managed. Higher values of the CS (68.5±3.9) (P =0.00961) were registered in 33 patients (55%) at 12 months, lower scores (50.9±3.6) (P =0.0649) were recorded in 5 cases (8%) who underwent to surgical treatment. The course of VAS score is described in Figure 4. The analysis of the prediction score in the study population showed a mean value of 13.5±2.7 (min: 8, max: 19). Among the 33 patients who remained conservatively treated at last follow-up the average prediction score was 11.3±1.8 while the values registered in the 27 patients surgically managed were 16.1±1.7.
Figure 4.
Course of pain score in the “conservative” and “non conservative” subjects from baseline to 12 months
Among the 33 patients who reported good outcome after 12 months of conservative treatment, the mean age was 68 years and only 3 of them were under 60 years. The remaining 27 patients who did not continue the conservative therapy, had a mean age of 54 years with only 10 of these were older than 60 years. The values of Pearson’s ICC recorded at each follow-up were closed to 1 (0.987; 0.978; 0.983) indicating a good interobserver correlation.
Discussion
RC injuries are a widespread problem that affect shoulder function and related patients’ quality of life (1, 29, 30). Furher-more, the effects of shoulder pain due to RC tear are emphasized by aging and the following increased functional demands in elderly (31). Therefore, chronic RC pathology has become an issue of social interest for the considerable disability, poor quality of life and the expensive utilization of health care resources (32, 33). The decision to undertake a conservative (34) rather than surgical (35) treatment is controversial (36), especially for symptomatic degenerative RC ruptures (30, 37). Another aspect concerns the asymptomatic rotator cuff tears (38) that pass from subclinic condition in 10% in the fourth decade to 50% in the sixth decade and about 80% in the eight decade of life (39). Patients fifty years and older with a subclinical or asymptomatic RC tears develop a painful and weak shoulder within 5 years (1). Whereas the objective of non-surgical treatment is aimed to obtain pain relief and improving in shoulder function, there is no clear evidence about which treatments are most suitable and what they entail (10, 22, 34). Common conservative treatment include oral analgesics and NSAIDs, steroid injections, massage and exercises therapy, instrumental interventions (Laser, TENS, Ultrasounds), but there are few studies to support this kind of non surgical therapies (37,40–42). Arthroscopic and open repair of the RC showed satisfactory outcomes for pain and shoulder function, as recently reported by Millett et al. (43), who registered, after arthroscopic rotator cuff repair, a survivorship (defined as a shoulder requiring additional surgery) of 94% at 5 years and 83% at 10 years with a statistical significant improvement in mean ASES score; however, most of the results of arthroscopy included mid-term follow-up studies (12, 44, 45) and therefore the outcomes are not as well established as for long-term open procedure (46, 47). It should be also noted that, despite the good clinical results for pain relief and abilty to perform daily living activity, ultrasound (45, 47) and MRI (48, 49) findings demonstrated an high rate of recurrent defects. The factors affecting tendon healing included the patient’s age at the time of the operation, the size and extent of the tear, and the presence of fatty degeneration in the rotator cuff muscle (47, 48). The decision to start a surgical procedure remains a choice of the surgeon in accordance with the patient and at the same time, there are no guidelines that can direct the cases to be submitted to conservative treatment. Although several older (11, 50–55) and recent (29, 36, 56–60) research articles reported the outcomes of conservative therapy in patients with symptomathyc full-thickness rotator cuff tears, few of these studies (52, 55, 59) have indicated the criteria for non surgical treatment. As results, we still have little understanding about which factors are related to good outcomes after conservative interventions. Since it is not possible to establish uniform criteria, the common treatment strategy is tailored to the individual case. According to the aforementioned considerations, we have identified the prognostic factors implicated in the selection of subjects could have satisfactory results by conservative treatment and on the basis of them we built a prediction score. With regard to the various parameters examined in the prediction score, we need to make some observations that emerge from tha current literature. The age is the most commonly used parameter in the decision making for the surgery of degenerative (9, 10, 23, 48, 61) and traumatic (62, 63) rupture of the rotator cuff. Poor results are found in patients aged 63 years and older (61, 64). Heavy work, especially if associated with repetitive movements of the arm above the equatorial plane, are often responsible for cuff injuries. Patients with work related injuries should be surgically treated but they have worse outocome compared to those of standard population and the difference are even greater when manual labour are involved (65, 66). Similarly, overhead sports can induce rotator cuff weakness or injuries and LHB pathology due to overuse syndrome (67, 68). Another important feature influencing the decision making of subjects with rotator cuff tears is made up by working compensation patients who have been recognized as having inferior surgical outcomes respect to the non-WC patients (69). About the timing for rotator cuff repair, recent research findings have demonstred that traumatic tears with a delayed surgery within 3 months (62, 63) achieve better satisfatctory outcomes than chronic tears70, similarly the long duration of the symptoms represent an adverse prognostic factor for surgical approach (11). A previous history of non operative treatment is associated with unsatisfactory results in case of new conservative treatment (71). Although the surgical approach of partial RC tears is controversial, the rehabilitation seems to give better outcomes compared with full-thickness tendon tears and the prognosis become worse when a complete subscapularis lesion is associated (27, 72). Massive RC tears, including the whole external rotators, have been showed to not achieve good outcomes with non surgical measures and therefore a latissimus dorsi tendon transfer is recommended (73). Various pathologies affecting the LHB, including tendinitis, instability and incomplete tears, have been indicated as source of pain at rest and during the daily living activities; the inflammation of the LHB is attributed to surrounding RC pathologies and characterized as secondary process (74). LHB tendinitis and instability don’t respond to common conservative therapies and should be treated with surgical intervention (75). An alteration of scapulohumeral rhythm, due to the fatigue of scapular stabilizers, can induce shoulder dysfunction with an associated decrease in rotator cuff strength (28, 76). In case of type II scapular dyskinesis associated with a cuff tear, surgical results may be negatively affected (77). Preoperative imaging, including X-ray, MRI and CT scans, can provide essential prognostic informations, in fact, it has been demonstred that a superior migration of the humeral head due to a complete lesion of the postero-superior RC associated with muscle atrophy and the fatty infiltration, complicate the surgical treatment with an high rate of recurrent tears, persistent pain and disability (19, 78–82). When the cuff lesion is associated with a controlateral tear and the range of motion is passively and actively limited, a conservative treatment should be preferred (83, 84).
In order to the specific features of the prediction score, some findings need to be emphasized from our study. About half of the population enrolled (“conservative”) continued the conservative therapy at last follow-up referring a good satisfaction, pain improvement and an acceptable quality of life. This subgroup conservatively treated, had a complete RC tear that was bilateral in 1 case and involved the upper portion of the subscapularis in 2 cases. Spontaneous rupture of the LHB was observed in 10 cases while only 2 patients were heavy workers and other 2 cases had a work-related injury; in 9 subjects with a positive drop-sign, we found a posterior superior cuff lesion with A/H interval lower than 7 mm. The MRI showed a grade III of muscle atrophy and relative fatty infiltration in 18 cases. In 30 out of 33 subjects, the active shoulder motion was higher than 90% with an an associated type II scapular dyskinesis. It was interesting to note that the 33 conservative patients were older than the remaining 27 subjects (“non conservative”) who preferred to stop the protocol due to persistent pain and disability. The prediction score in the conservative patients ranged from 10.6 to 12.8, resulting lower compared with non conservative subgroup in which the average values were recorded 5 point higher (range: 15.2 – 17.3). Since the patients who benefit from conservative treatment had a score lower than 13 points, we identified this values as a “cut-off” score to predict a good results by conservative management of RC tear. Patients with an intermediate score ranging from 14 to 15 points, referred good satisfaction at an early follow-up but the outcomes have deteriorated over time so that only 5 out of 12 followed the conservative treatment after 12 months.
Some weak point are noteworthy in this study: 1) since this is a prognostic study the sample size of the study population could be too small to give definitive conclusions, 2) the clinical tool (Constant-Murley score) used to assess the patients is not adjusted and there is no comparison with other clinical scores to get supplemental data to analyze and discuss, 3) conservative treatment included rehabilitation, Laser therapy and NSAIDs, excluding steroid injections that are commonly used in the treatment of painful RC tears, 4) the sensitivity, specificity and accuracy of the prediction score “cut-off” was not calculated.
Although these limitations, the outcomes of our study support the assumption that a predictive prognostic score may guarantee a rational approach in the management of subjects with RC tears, expecially in elderly who continue to have the higher rate of recurrence and therefore could be well treated with standard conservative therapies. Specifically for the point 4, we think that further realibility studies are required to validate the prediction score as common clinical tool to use in the clinical practice.
References
- 1.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10:199–203. doi: 10.1067/mse.2001.113086. [DOI] [PubMed] [Google Scholar]
- 2.Schibany N, Zehetgruber H, Kainberger F, Wurnig C, Ba-Ssalamah A, Herneth AM, Lang T, Gruber D, Breitenseher MJ. Rotator cuff tears in asymptomatic individuals: a clinical and ultrasonographic screening study. Eur J Rad. 2004;5:236–238. doi: 10.1016/S0720-048X(03)00159-1. [DOI] [PubMed] [Google Scholar]
- 3.Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulder. J Bone Joint Surg Am. 1995;77:10–15. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Milgrom C, Schaffler M, Gilbert S, Van Holsbeeck M. Rotator cuff changes in asymptomatic adults: The effect of age, hand dominance and gender. Journal Bone Joint Surg Br. 1995;77:296–298. [PubMed] [Google Scholar]
- 5.Kelly BT, Williams RJ, Cordasco FA, Backus SI, Otis JC, Weiland DE, Altchek DW, Craig EV, Wickiewicz TL, Warren RF. Differential patterns of muscle activation in patients with symptomatic and asymptomatic rotator cuff tears. J Shoulder Elbow Surg. 2005;14:165–171. doi: 10.1016/j.jse.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 6.Ditsios KT, Yamaguchi K, Teefey AS, Middleton WD, Hildebolt C, Galatz LM. The demographics and morphology of rotator cuff disease: A comparison of asymptomatic and symptomatic shoulder. Journal Bone Joint Surg Br. 2004;86-B:175. doi: 10.2106/JBJS.E.00835. [DOI] [PubMed] [Google Scholar]
- 7.Jerosch J, Muller T, Castro WH. The incidence of rotator cuff rupture. An anatomic study. Acta Orthop. Belg. 1991;57:124–129. [PubMed] [Google Scholar]
- 8.Tempelhof S, Rupp S, Romain S. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8:296–299. doi: 10.1016/s1058-2746(99)90148-9. [DOI] [PubMed] [Google Scholar]
- 9.Rockwood CA, jr, Basamania C, Wirth MA. Nonoperative treatment of full-thickness rotator cuff tears. J Bone Joint Surg Am. 1997;79:404. [Google Scholar]
- 10.Goldberg BA, Nowinski RJ, Matsen FA., III Outcome of nonoperative management of full-thickness rotator cuff tears. Clinical Orthop Rel Res. 2001;382:99–107. doi: 10.1097/00003086-200101000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Bokor DJ, Hawkis RJ, Huckell GH, Angelo RL, Schickendants MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res. 1993;294:103–110. [PubMed] [Google Scholar]
- 12.Murray TF, Jr, Lajtai G, Mileski RM, Snyder SJ. Arthroscopic repair of medium to large full-thickness rotator cuff tears: outcome at 2- to 6-year follow-up. J Shoulder Elbow Surg. 2002;11:19–24. doi: 10.1067/mse.2002.120142. [DOI] [PubMed] [Google Scholar]
- 13.Maritz NGJ, Oschman Z. An ultrasonographic study of the asymptomatic controlateral shoulder in patients with a confirmed symptomatic rotator cuff tear. Journal Bone Joint Surg Br. 2005;87-B:275. [Google Scholar]
- 14.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The Outcome and Repair Integrity of Completely Arthroscopically Repaired Large and Massive Rotator Cuff Tears. J Bone Joint Surg Am. 2004;86:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Klepps S, Bishop J, Lin J, Cahlon O, Strauss A, Hayes P, Flatow EL. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716–1722. doi: 10.1177/0363546504265262. [DOI] [PubMed] [Google Scholar]
- 16.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Jost B, Pfirrmann CWA, Gerber C. Clinical Outcome After Structural Failure of Rotator Cuff Repairs. J Bone Joint Surg. 2000;82:304–314. doi: 10.2106/00004623-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Kane SM, Dave A, Haque A, Langston K. The incidence of rotator cuff disease in smoking and nonsmoking patients: a cadaveric study. Orthopedics. 2006;29:363–366. doi: 10.3928/01477447-20060401-17. [DOI] [PubMed] [Google Scholar]
- 19.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clinic Orthop Rel Res. 1997;344:275–283. [PubMed] [Google Scholar]
- 20.Walch G, Maréchal E, Maupas J, Liotard JP. Traitement chirurgical des ruptures de la coiffe des rotateurs. Facteurs de pronostic. Rev Chir Orthop Rep. 1992;78:379–388. [PubMed] [Google Scholar]
- 21.Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for Rotator Cuff Repair A Systematic Review. Clin Orthop Rel Res. 2006;455:52–63. doi: 10.1097/BLO.0b013e31802fc175. [DOI] [PubMed] [Google Scholar]
- 22.Hawkins RH, Dunlop R. Nonoperative treatment of rotator cuff tears. Clin Orthop Rel Res. 1995;321:178–88. [PubMed] [Google Scholar]
- 23.Itoi E, Tabata S. Incomplete rotator cuff tears: Result of operative treatment. Clin orthop. 1992;248:128–135. [PubMed] [Google Scholar]
- 24.Balich SM, Sheley RC, Brown TR, Sauser DD, Quinn SF. MR imaging of the rotator cuff tendon: interobserver agreement and analysis of interpretive errors. Radiology. 1997;204:191–194. doi: 10.1148/radiology.204.1.9205245. [DOI] [PubMed] [Google Scholar]
- 25.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop. 1987;214:160–164. [PubMed] [Google Scholar]
- 26.Ainsworth R. Physiotherapy rehabilitation in patients with massive, irreparable rotator cuff tears. Musculoskeletal Care. 2006;4:140–151. doi: 10.1002/msc.85. [DOI] [PubMed] [Google Scholar]
- 27.Walch G, Bohulahia A, Calderone S, Robinson AH. The ‘dropping and’ hornblower’ signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br. 1998;80:624–628. doi: 10.1302/0301-620x.80b4.8651. [DOI] [PubMed] [Google Scholar]
- 28.Merolla G, De Santis E, Sperling JW, Campi F, Paladini P, Porcellini G. Infraspinatus strenght assessment before and after scapular muscles rehabilitation in professional volleyball players with scapular dyskinesis. J Shoulder Elbow Surg. 2010;19:1256–1264. doi: 10.1016/j.jse.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 29.Zingg PO, Jost B, Sukthankar A, Buhler M, Phirrmann CW, Gerber C. Clinical and structural outcomes of non operative management of massive rotator cuff tears. J Bone Joint Surg. 2007;89:1928–1934. doi: 10.2106/JBJS.F.01073. [DOI] [PubMed] [Google Scholar]
- 30.Lambers Heerspink FO, Hoogeslag RA, Diercks RL, van den Akker-Scheek I, van Raay JJ. Clinical and radiological outcome of conservative vs. surgical treatment of atraumatic degenerative rotator cuff rupture: design of a randomized controlled trial. BMC Musculoskelet Disord. 2011;26:12–25. doi: 10.1186/1471-2474-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fehringer EV, Sun J, VanOeveren LS, Keller BK, Matsen FA., III Fullthickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elbow Surg. 2008;17:881–885. doi: 10.1016/j.jse.2008.05.039. [DOI] [PubMed] [Google Scholar]
- 32.Smith KL, Harryman DT, 2nd, Antoniou J, Campbell B, Sidles JA, Matsen FA., 3rd A prospective, multipractice study of shoulder function and health status in patients with documented rotator cuff tears. J Shoulder Elbow Surg. 2000;9:395–402. doi: 10.1067/mse.2000.108962. [DOI] [PubMed] [Google Scholar]
- 33.Roquelaure Y, Mariel J, Fanello S, Boissiere JC, Chiron H, Dano C, Bureau D, Penneau-Fontbonne D. Active epidemiological surveillance of musculoskeletal disorders in a shoe factory. Occup Environ Med. 2002;59:452–458. doi: 10.1136/oem.59.7.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dalton SE. The conservative management of rotator cuff disorders. Br J Rheumatol. 1994;33:663–667. doi: 10.1093/rheumatology/33.7.663. [DOI] [PubMed] [Google Scholar]
- 35.Coghlan AJ, Rachelle B, Sally G, Johnston VR, Bell NS. Surgery for rotator cuff disease. Cochrane Database Syst Rev. 2008;(1):CD005619. doi: 10.1002/14651858.CD005619.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Williams GR, Rockwood CA, Bigliani LU, Iannotti JP, Stanwood W. Rotator cuff tear: Why do we repair them? J Bone Joint Surg Am. 2004;12:2764–2776. [PubMed] [Google Scholar]
- 37.Bruce A, Goodyear-Smith F. Corticosteroid injections for painful shoulder: a meta-analysis. Br J Gen Pract. 2005;55:224–228. [PMC free article] [PubMed] [Google Scholar]
- 38.Lehman C, Cuomo F, Kummer FJ, Zuckerman JD. The incidence of full thickness rotator cuff tears in a large cadaveric population. Bull Hosp Jt Dis. 1995;54:30–31. [PubMed] [Google Scholar]
- 39.Sher JS, Uribe JW, Posada A, Murphy JB, Zlatkin MB. Abnormal findings on magnetic resonance imaging of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10–15. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Coburn S, Wee E, Green S, Harris A, Forbes A, Buchbinder R. Efficacy and cost-effectiveness of a physiotherapy program for chronic rotator cuff pathology: a protocol for a randomised, double-blind, placebo-controlled trial. BMC Musculoskelet Disord. 2007;31:8–86. doi: 10.1186/1471-2474-8-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Calis HT, Berberoglu N, Calis M. Are ultrasound, laser and exercise superior to each other in the treatment of subacromial impingement syndrome? A randomized clinical trial. Eur J Phys Rehabil Med. 2011;47:1–6. [PubMed] [Google Scholar]
- 42.Dorrestijn O, Greving K, van der Veen WJ, van der Meer K, Diercks RL, Winters JC, Stevens M. Patients with shoulder complaints in general practice: consumption of medical care. Rheumatology. 2011;50:389–395. doi: 10.1093/rheumatology/keq333. [DOI] [PubMed] [Google Scholar]
- 43.Millett PJ, Horan MP, Maland KE, Hawkins RJ. Long term survivorship and outcomes after surgical repair and survivorship of full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2011;20:591–597. doi: 10.1016/j.jse.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 44.Gartsman GM, Khan M, Hammerman SM. Arthroscopic repair of full-thickness tears of the rotator cuff. J Bone Joint Surg Am. 1998;80:832–840. doi: 10.2106/00004623-199806000-00007. [DOI] [PubMed] [Google Scholar]
- 45.Nho SJ, Brown BS, Lyman S, Adler RS, Altcheck DW, Macgillivray JD. Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg. 2009;18:13–20. doi: 10.1016/j.jse.2008.05.045. [DOI] [PubMed] [Google Scholar]
- 46.Calvert PT, Packer NP, Stoker DJ, Bayley JI, Kessel L. Arthrography of the shoulder after operative repair of the torn rotator cuff. J Bone Joint Surg Br. 1986;68:147–150. doi: 10.1302/0301-620X.68B1.3941132. [DOI] [PubMed] [Google Scholar]
- 47.Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff: correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–989. [PubMed] [Google Scholar]
- 48.Cho NS, Rhee YG. The factors affecting the clinical aoutcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg. 2009;1:96–104. doi: 10.4055/cios.2009.1.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gusmer PB, Potter HG, Donovan WD, O'Brien SJ. MR imaging of the shoulder after rotator cuff repair. AJR. 1997;168:559–563. doi: 10.2214/ajr.168.2.9016248. [DOI] [PubMed] [Google Scholar]
- 50.Brown JT. Early assessment of supraspinatus tears. Porcine infiltration as a guide to treatment. J Bone Joint Surg Br. 1949;31:423–425. [PubMed] [Google Scholar]
- 51.McLaughlin HL. Rupture of the rotator cuff. J Bone Joint Surg Am. 1962;44:979–983. [Google Scholar]
- 52.Rowe CR. Rupture of the rotator cuff. Selection of cases for conservative treatment. Surg Clin North Am. 1963;43:1531–1534. doi: 10.1016/s0039-6109(16)37140-7. [DOI] [PubMed] [Google Scholar]
- 53.Wallace WA, Wiley AM. The long-term results of conservative management of full-thickness tears of the rotator cuff. J Bone Joint Surg Br. 1986;68:162. [Google Scholar]
- 54.Bartolozzi A, Andreychik D, Ahmad S. Determinants of outcome in the treatment of rotator cuff disease. Clin Orthop Relat Res. 1994;308:90–97. [PubMed] [Google Scholar]
- 55.Itoi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop Relat Res. 1995;275:165–173. [PubMed] [Google Scholar]
- 56.Tanaka M, Itoi E, Sato K, Hamada J, Hintachi S, tojo Y, Honda M, Tabata S. factors related to successful outcome of conservative treatment for rotator cuff tears. Ups J Med Sci. 2010;115:193–200. doi: 10.3109/03009734.2010.493246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Baydar M, Akalin E, El O, Gulbahar S, Bircan C, Akgul O, et al. The efficacy of conservative treatment in patients with full-thickness rotator cuff tears. Rheumatol Int. 2009;29:623–628. doi: 10.1007/s00296-008-0733-2. [DOI] [PubMed] [Google Scholar]
- 58.Koubaa S, Ben Salah FZ, Lebib S, Miri I, Ghorbel S, Dziri C. Conservative management of full-thickness rotator cuff tears. A prospective study of 24 patients. Ann Readapt Med Phys. 2006;49:62–67. doi: 10.1016/j.annrmp.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 59.Minagawa H, Itoi E, Saito I. Conservative treatment of rotator cuff tears. Rheumatology. 2001;25:509–9. [Google Scholar]
- 60.Wirth MA, Basamania C, Rockwood CA. Nonoperative management of full thickness tears of rotator cuff. Orthop Clin North Am. 1997;28:59–67. doi: 10.1016/s0030-5898(05)70264-9. [DOI] [PubMed] [Google Scholar]
- 61.Oh JH, Kim SH, Kang JY, Oh CH, Gong HS. Effect of age on functional and structural outcome after rotator cuff repair. Am J sports Med. 2010;38:672–678. doi: 10.1177/0363546509352460. [DOI] [PubMed] [Google Scholar]
- 62.Bjornsson HC, Norlin R, Johansson K, Adolfsson LE. The influence of age, delay of repair, and tendon involvement in acute rotator cuff tears: structural and clinical outcomes after repair of 42 shoulders. Acta Orthop. 2011;82:187–92. doi: 10.3109/17453674.2011.566144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Petersen SA, Murphy TP. The timing of rotator cuff repair for the restoration of function. J Shoulder Elbow Surg. 2011;20:62–68. doi: 10.1016/j.jse.2010.04.045. [DOI] [PubMed] [Google Scholar]
- 64.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 65.Novè-Josserand L, liotard JP, godeneche A, Neyton L, Borel F, Rey B, Noel E, Walch G. Occupational outcome after surgery in patients with rotator cuff tear due to a work related injury or occupational disease. A series of 262 cases. Orthop Traumatol Surg Res. 2011;97:361–366. doi: 10.1016/j.otsr.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 66.McKee MD, Yoo DJ. The effect of surgery for rotator cuff disease on general health status. Results of a prospective trial. J Bone Joint Surg. 2000;82-A:970–979. doi: 10.2106/00004623-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 67.Greiwe RM, Ahmad CS. Management of the throwing shoulder: cuff, labrum and internal impingement. Orthop Clin North Am. 2010;41:309–323. doi: 10.1016/j.ocl.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 68.Wilk KE, Meister K, Andrews JR. Current Concepts in the Rehabilitation of the Overhead Throwing Athlete. AM J Sports Med. 2002;30:136–151. doi: 10.1177/03635465020300011201. [DOI] [PubMed] [Google Scholar]
- 69.Bathia S, Piasecki DP, Nho SJ, Romeo AA, Cole BJ, Nicholson GP, Boniquit N, Verma NN. Early return to work in workers' compensation patients after arthroscopic full-thickness rotator cuff repair. Arthroscopy. 2010;26:1027–1034. doi: 10.1016/j.arthro.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 70.Bassett RW, Cofield RH. Acute tears of the rotator cuff. The timing of surgical repair. Clin Orthop. 1983;175:18–24. [PubMed] [Google Scholar]
- 71.Michener LA, Walsworth MK, Burnet EN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: asystematic review. J Hand Ther. 2004;17:152–164. doi: 10.1197/j.jht.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 72.McConville OR, Iannotti JP. Partial-thickness tears of the rotator cuff: evaluation and management. J Am Acad Orthop Surg. 1999;7:32–43. doi: 10.5435/00124635-199901000-00004. [DOI] [PubMed] [Google Scholar]
- 73.Gerber C. Latissimus dorsi transfer for irreparable tears of the rotator cuff. Clin Orthop Rel Res. 1992;275:152–160. [PubMed] [Google Scholar]
- 74.Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581–592. doi: 10.1016/j.arthro.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 75.Walch G, Edwards TB, Boulahia A, Novè-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of the rotator cuff tears: clinical and radiographic results of 307 caees. J Shoulder Elbow Surg. 2005;14:238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 76.Merolla G, De Santis E, campi F, Paladini P, Porcellini G. Supraspinatus and Infraspinatus weakness in overhead athletes with scapular dyskinesis: strenght assessment before and after restoration of scapular musculature scapular balance. Musculoskeletal Surg. 2010;94:119–125. doi: 10.1007/s12306-010-0082-7. [DOI] [PubMed] [Google Scholar]
- 77.Kibler WB, Uhl TL, Maddux JW, Brooks PV, Zeller B, McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11:550–556. doi: 10.1067/mse.2002.126766. [DOI] [PubMed] [Google Scholar]
- 78.Nové-Josserand L, Lévigne C, Noël E, Walch G. The acromio-humeral interval. A study of the factors influencing its height. Re Chir Orthop Reparatrice Appar Mot. 1996;82:379–385. [PubMed] [Google Scholar]
- 79.Warner JJ, Higgins L, Parsons IM, 4th, Dowdy P. Diagnosis and management of anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2001;10:37–46. doi: 10.1067/mse.2001.112022. [DOI] [PubMed] [Google Scholar]
- 80.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty Muscle degeneration in cuff ruptures, Pre and postoperative evaluation by CT scan. Clin Orthop Rel Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 81.Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscle of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. doi: 10.1016/s1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 82.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair of completely artthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 83.Tauro JC. Stiffness and rotator cuff tears: incidence, arthroscopic findings, and treatment results. Arthroscopy. 2006;22:581–586. doi: 10.1016/j.arthro.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 84.Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears. A prospective long term study. J Bone Joint Surg Am. 2001;83:71–77. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]