Summary
Hypermobility of the first ray, which is caused by an instability of the first metatarsocuneiform joint, is one of the factors that induces hallux valgus and can be caused by technical mistakes in ballet practice.
Correlation between ballet practice and hypermobility of the first ray.
Using a modified Klaue device, mobility of the first metatarsocuneiform joint was measured (hypermobility ≥ 10mm) in both dorsal and dorso-medial directions in 264 feet in 2 groups of people: ballet dancers (non professional) and a control group of non-dancers.
45° mobility is statistically higher than dorsal mobility, and mobility in the ballet dancer group is higher than in the control group, but there is no correlation between hours of ballet and en-pointe shoe practice, and hypermobility of the first ray.
First ray hypermobility, and even hallux valgus, in ballet practice is related to anatomical-hereditary factors and to incorrect technical execution.
Keywords: hypermobility, first ray, hallux valgus, ballet dancer, joint instability
Introduction
Hypermobility of the first ray is one of the predisposing factors for the development of hallux valgus (HV), especially if there are also extrinsic risk factors, such as an injury of the plantar ligament between the first metatarsal and cuneiform or a tendon-muscle imbalance1. Moreover, hallux valgus deformity causes further exacerbation of any preexisting hypermobility of the first ray2. In particular, there is a direct relationship between painful HV and hypermobility at the first metatarsus-cuneiform joint extension3 for which a pathogenic mechanism has been proposed. This mechanism links symptomatic HV with primary alterations in the forefoot load, which leads to an increased first metatarsus-phalangeal angle as one of the consequences.
Klaue has provided a quantitative definition of hypermobility: a first ray that moves dorsally more than 8–10 mm and lacks a precise point of maximum final extension3,4. Clinically, hallux valgus is a deformity in the transverse plane (increased intermetatarsal angle), but physiologically, the metatarsal-cuneiform articulation shows a certain degree of mobility even in the dorsal plane5. For this reason, clinical trials performed to date3,5–7 have only evaluated first ray hypermobility in the dorsal direction, even if during walking, the joint moves in the dorsal-medial direction at an angle of 45–60°8.
The etiology of hallux valgus in a particular group of subjects, such as ballet dancers, can be explained by several factors9:
- § “Constitutional” issues:
- - Egyptian Foot (the first toe is longer than the other four); a short first metatarsus, metatarsus primus varus.
- - Flat feet or ligamentous laxity of the feet in subjects with generalized hypermobility impedes the symmetrical distribution of load on the soles of the feet, resulting in a weight shift to the inside (due to the collapse of the medial arch) and the overload of the midfoot.
- - Altered biomechanics of the foot during the push phase of walking.
- In all of these cases, the dancer will support the weight of her body using the second or third toe and move the first one into valgus, with the subsequent development of HV. § Incorrect technique in the execution of the fundamentals of dance (triggers):
- - Rolling in (Fig. 1): if the ankle is not well supported in the en dehours position, it will cause foot pronation, with rotation of the first ray and consequent stress on the metatarsophalangeal joint, and finally injury to the capsular structures of the first toe.
- - Stress related to dance activity; tightly fitting dance shoes; starting the study of “en pointe shoes” too early.
Figure 1.
Rolling in.
Dance practice does not cause bunions more frequently than in the general female population9; it is rather related to heredity, which the use of pointe shoes can aggravate. In some cases, bunions in dancers can have an acute traumatic origin due to the rupture of the medial ligament of the 1MTT-P, which often can not be diagnosed at the time of the injury but only when the hallux valgus deviation occurs (becomes apparent?). In these cases, the best procedure is the suturing of the ligaments torn10.
HV-related pain is accentuated by walking, ballet practice, and forefoot-hugging shoes. In these cases, a rest period of a few days is recommended, during which pain can be reduced by the application of ice and local analgesics. After returning to ballet practice, the dancer must look for any technical error and correct it. Functional bandages during ballet practice give good results in pain reduction.
Materials and methods
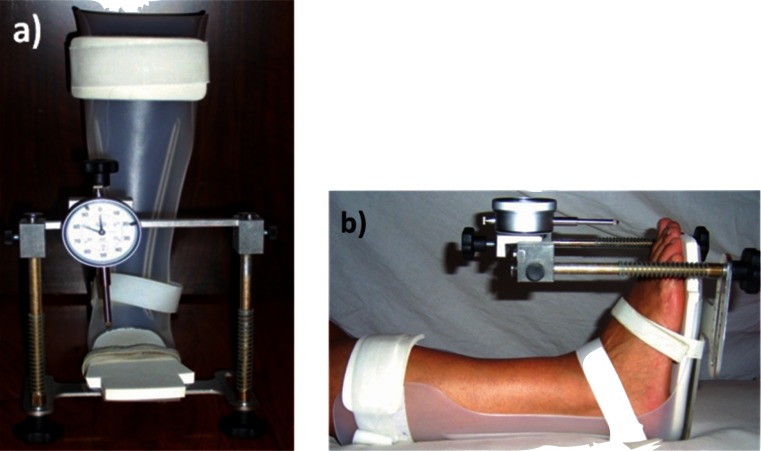
We used a modified Klaue device (Fig. 2a): a steel bracket was mounted on a foot and leg plexiglas orthosis thus allowing the positioning of the micrometer in a precise, quick, and easy manner.
Figure 2.
a) Modified Klaue device used in this study. b) The foot is placed in the orthosis at 90° to the leg, ankle in neutral position and it is immobilized in three points: calf, ankle, and midfoot.
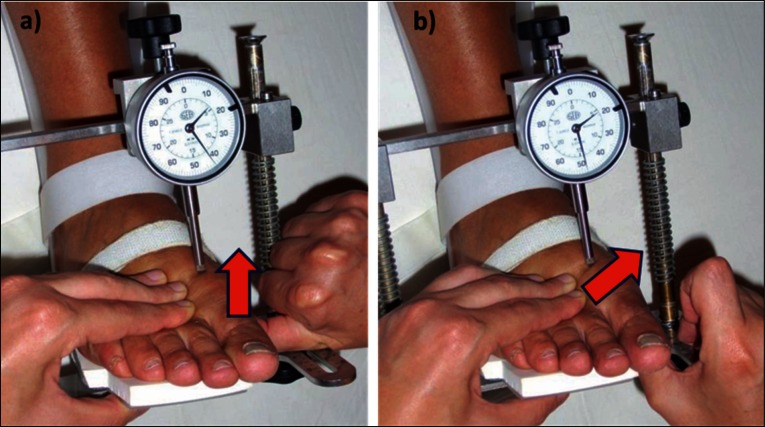
The foot is placed in the orthosis at 90° to the leg, ankle in neutral position and it is immobilized in three points: calf, ankle, and midfoot (Fig. 2b). The steel support is then adjusted in the three directions so that the tip of the micrometer touches the dorsal surface of the first metatarsal head. With one hand, the examiner immobilizes metatarsals II to V, and with the thumb of the other hand, exerts a force on the plantar side of the first metatarsal head in order to reach the maximum dorsal (Fig. 3a) and dorsal-medial (Fig. 3b) displacement. Five measurements in the dorsal direction and subsequently five measurements in the dorsal-medial direction are performed for each foot. The dial of the micrometer is able to measure the extent of mobility of the first ray in millimeters.
Figure 3.
With one hand, the examiner immobilizes metatarsals II to V, and with the thumb of the other hand, exerts a force on the plantar side of the first metatarsal head in order to reach the a) maximum dorsal and b) dorsal-medial displacement.
Every subject who participated in this study was informed in advance about the procedure and purpose of the study and gave his or her informed consent.
Subjects were between 15 and 34 years old, with no history of trauma or surgery associated with the foot examined, and no birth defects of the foot. Between November 2010 and July 2011, 264 feet (132 right and 132 left) of 132 subjects (2 M and 130 F), were evaluated in this study and the individuals participating were divided into two groups:
The Ballet Dancers Group (BD) included 132 feet of 66 subjects (1 M and 65 F) who study ballet as a hobby. For each subject of this group, the hours of dance practice and pointe shoe practice were calculated on the basis of hours per week and years of dance and pointe shoe practice.
The Ballet Dancers Control Group (CTRL_BD) included 132 feet of 66 subjects (1 M and 65 F) who do no ballet dancing.
Results
We assumed that the data collected were selected from populations distributed according to a normal curve and thus chose to use the Student’s t-test with a significance level of 5% (α = 0.05). Moreover, considering the first ray hypermobility mobility measurement values greater than or equal to 10 mm, each of the 6 groups of subjects evaluated was divided into 3 subgroups:
- Normal mobility of the first ray
- Hypermobility of only the dorso-medial first ray
- Hypermobility of both dorsal and dorso-medial first ray.
Subjects belonging to the Ballet Dancers (BD) Group and those belonging to the Control Ballet Dancers (CTRL_BD) Group were comparable in age and height, while weight and shoe size were significantly lower in BD compared to CTRL_BD (Tab. 1).
Table 1.
Differences between BD and CTRL_BD.
| N | Average | SD | Min | Max | p value | |
|---|---|---|---|---|---|---|
| AGE | 66 | −0.02 | 1.36 | −3.00 | 3.00 | 0.92846 |
| WEIGHT | 66 | −1.58 | 2.89 | −7.00 | 5.00 | <0.0001 |
| HIGHT | 66 | 0.67 | 3.22 | −5.00 | 10.00 | 0.0971 |
| SHOE N° | 66 | −0.38 | 0.91 | −2.00 | 2.00 | 0.0012 |
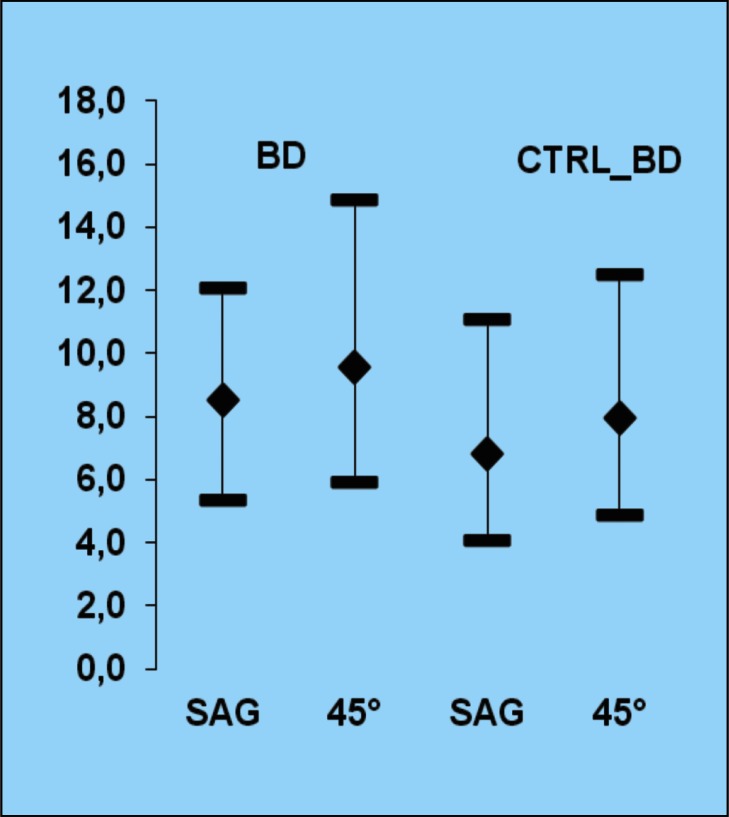
The average values of measurements in BD subjects were: 8.51 mm in the sagittal plane (direction?) and 9.56 mm at 45°, while the average values of measurements in CTRL_BD subjects were: 6.85 mm in the sagittal plane and 7.96 mm at 45° (Tab. 2; Fig. 4).
Table 2.
Measurements in BD Group and CTRL_BD Group.
| Group | Variable | N | Average | SD | Min | Max |
|---|---|---|---|---|---|---|
| BALLET | R_SAGIT | 66 | 8.50 | 1.58 | 5.39 | 12.08 |
| DANCER | L_SAG | 66 | 8.52 | 1.67 | 5.36 | 11.75 |
| R_45 | 66 | 9.53 | 1.77 | 6.11 | 14.86 | |
| L_45 | 66 | 9.60 | 1.79 | 5.91 | 13.70 | |
| TOT_SAGIT | 66 | 8.51 | 1.62 | 5.36 | 12.08 | |
| TOT_45 | 66 | 9.56 | 1.77 | 5.91 | 14.86 | |
|
| ||||||
| BALLET | R_SAGIT | 66 | 6.65 | 1.46 | 4.09 | 10.38 |
| DANCER | L_SAG | 66 | 7.06 | 1.49 | 4.39 | 11.07 |
| CONTROL | R_45 | 66 | 7.71 | 1.62 | 4.90 | 12.51 |
| L_45 | 66 | 8.21 | 1.75 | 5.16 | 12.47 | |
| TOT_SAGIT | 66 | 6.85 | 1.48 | 4.09 | 11.07 | |
| TOT_45 | 66 | 7.96 | 1.70 | 4.90 | 12.51 | |
Figure 4.
Average and lower and upper limits of measurements in sagittal and 45° directions of all cases of BD compared to their respective controls.
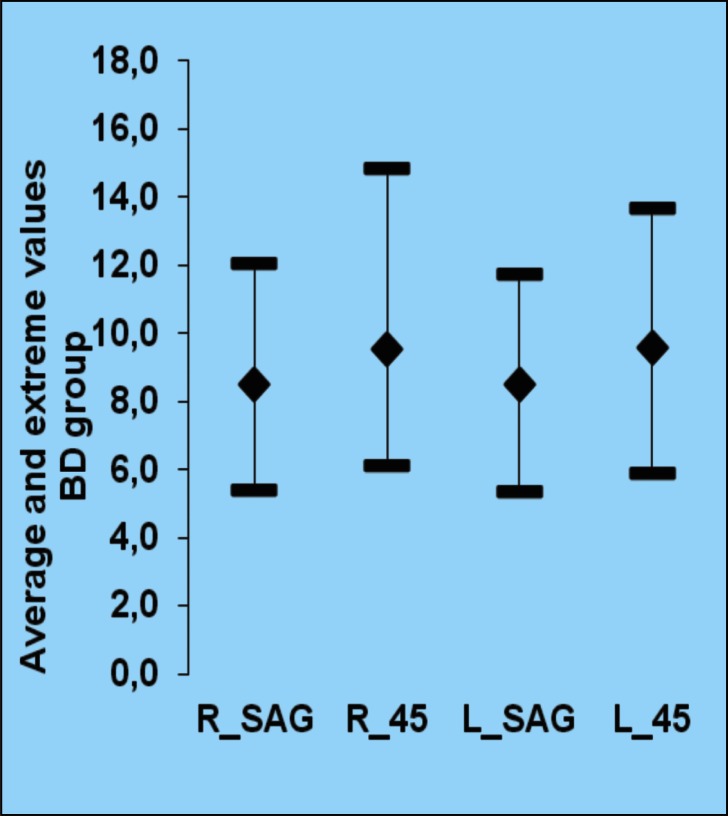
The Ballet Dancers Group (Fig. 5):
- Measurements obtained at 45° were significantly (p < 0.05) higher than those obtained in the sagittal plane. The difference was on average 3.1 mm on the right foot and 1.8 mm on the left.
- Measurements obtained on the left foot were not significantly higher (p > 0.10) compared to those obtained on the right. The difference was on average 0.02 mm for the sagittal plane and 0.07 mm at 45°.
Figure 5.
Average and extreme values in BD group: right and left foot, sagittal and 45° measurements.
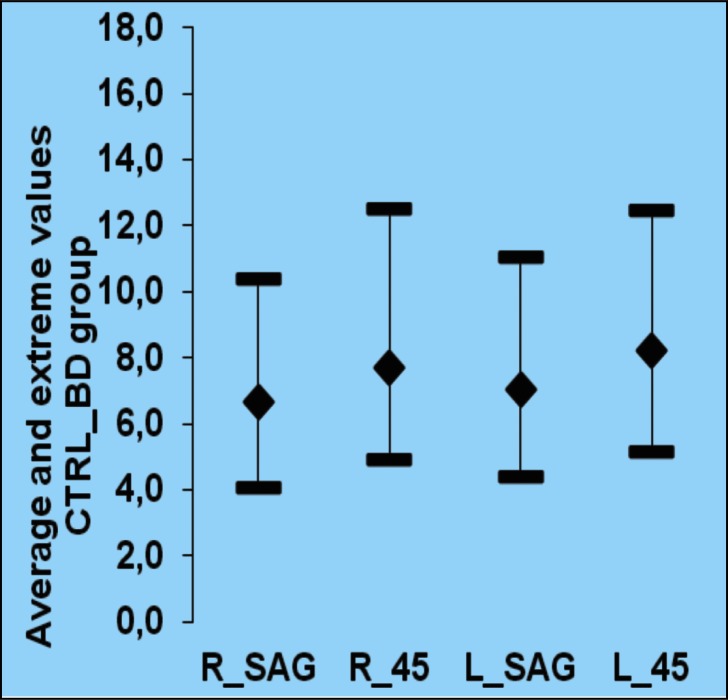
The Control Group (Fig. 6):
- Measurements obtained at 45° were significantly greater than those obtained in the sagittal plane (p < 0.05). The difference was on average 1.6 mm on the right foot and 1.15 mm on the left.
- Measurements obtained on the left foot were not significantly (p > 0.10) higher than those obtained on the right: on average 0.41mm in the sagittal plane and 0.5 mm at 45°.
Figure 6.
Average and extreme values in CTRL_BD group: right and left foot, sagittal and 45° measurements.
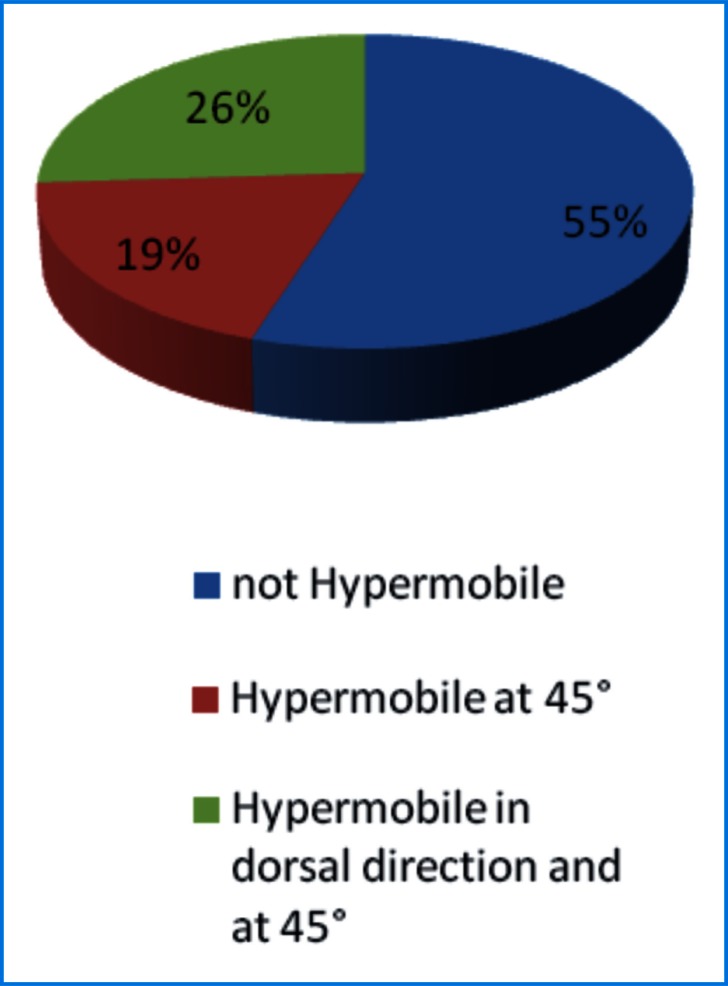
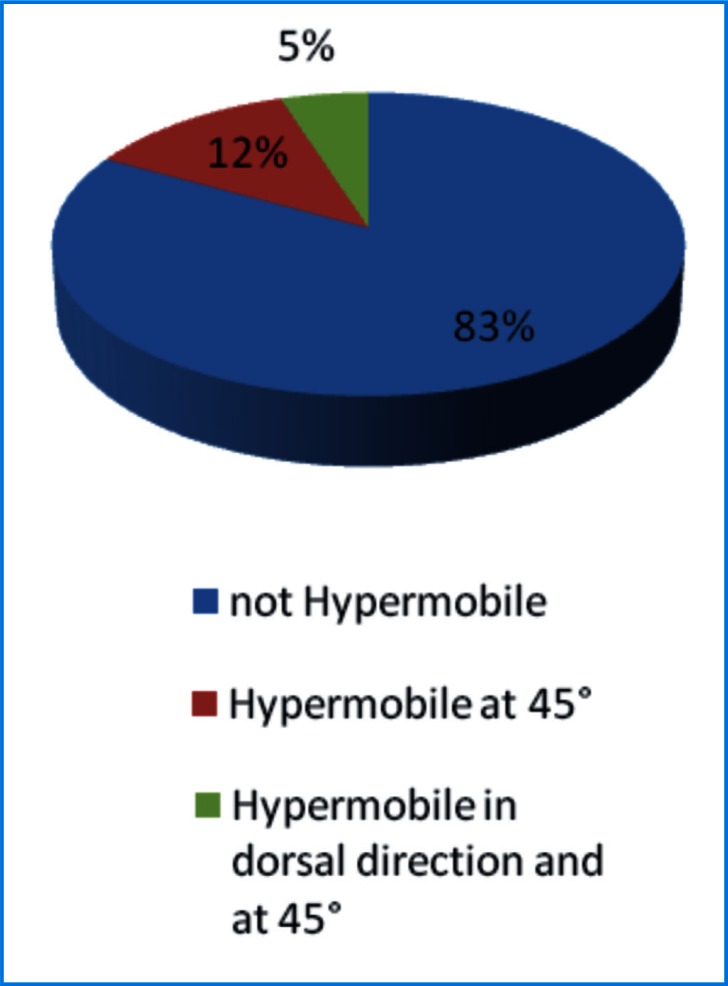
Figure 7 shows the percentage frequency of the three subgroups within the BD Group. Figure 8 shows the percentage frequency of the three subgroups within the CTRL_BD Group.
Figure 7.
Subgroups in BD group (1- not Hypermobile; 2- Hypermobile at 45°; 3- Hypermobile in dorsal direction and at 45°).
Figure 8.
Subgroup in CTRL_BD group.
Discussion
In both groups in this study, measurements performed at 45° are on average significantly higher than measurements in the sagittal direction. In the Ballet Dancers Group, both measurements in the sagittal plane and at 45° are significantly higher than their controls on both sides, right foot and left foot (Tab. 3).
Table 3.
Differences between BD and CTRL_BD.
| N | Average | SD | Min | Max | p value | |
|---|---|---|---|---|---|---|
| R_SAGIT | 66 | 1.85 | 2.26 | −3.42 | 6.72 | <0.0001 |
| R_45 | 66 | 1.82 | 2.46 | −3.91 | 7.78 | <0.0001 |
| L_SAG | 66 | 1.46 | 2.23 | −3.21 | 6.42 | <0.0001 |
| L_45 | 66 | 1.39 | 2.45 | −4.53 | 6.98 | <0.0001 |
To verify the presence of a correlation between the hours of dancing and en pointe shoes practice with possible first ray hypermobility, subjects of the Ballet Dancers Group were divided into two subgroups according to the average (or mean) hours of dancing and en pointe shoe practice carried out during their dance activity. In Tables 4 and 5, it is apparent that both measurements in sagittal and 45° planes, for both the right and the left foot, are almost identical in the two subgroups.
Table 4.
Differences in the two subgroups of BD group by the average hours of ballet practice.
| BALLET PRACTICE (total hours) | Variable | N | Average | SD | Min | Max |
|---|---|---|---|---|---|---|
| ≤ 2992 | BD R_SAGIT | 33 | 8.54 | 1.63 | 5.73 | 12.08 |
| BD R_45 | 33 | 9.72 | 1.83 | 6.42 | 14.86 | |
| BD L_SAG | 33 | 8.72 | 1.72 | 5.36 | 11.72 | |
| BD L_45 | 33 | 9.91 | 1.79 | 5.91 | 13.70 | |
|
| ||||||
| > 2992 | BD R_SAGIT | 33 | 8.46 | 1.56 | 5.39 | 10.95 |
| BD R_45 | 33 | 9.34 | 1.73 | 6.11 | 12.17 | |
| BD L_SAG | 33 | 8.32 | 1.62 | 5.55 | 11.75 | |
| BD L_45 | 33 | 9.29 | 1.76 | 6.13 | 12.80 | |
Table 5.
Differences in the two subgroups of BD group by the average hours of en pointe shoe practice.
| EN POINTE SHOES (total hours) | Variable | N | Average | SD | Min | Max |
|---|---|---|---|---|---|---|
| ≤ 440 | BD R_SAGIT | 32 | 8.48 | 1.73 | 5.73 | 12.08 |
| BD R_45 | 32 | 9.62 | 2.01 | 6.15 | 14.86 | |
| BD L_SAG | 32 | 8.47 | 1.58 | 5.36 | 11.72 | |
| BD L_45 | 32 | 9.66 | 1.76 | 6.13 | 13.70 | |
|
| ||||||
| > 440 | BD R_SAGIT | 29 | 8.44 | 1.50 | 5.39 | 10.86 |
| BD R_45 | 29 | 9.42 | 1.56 | 6.11 | 11.90 | |
| BD L_SAG | 29 | 8.53 | 1.62 | 5.55 | 11.56 | |
| BD L_45 | 29 | 9.56 | 1.74 | 6.58 | 12.80 | |
We can surmise that, although first ray hypermobility, and even hallux valgus, are closely related to ballet practice. This is not due to the amount of dancing hours with or without pointe shoes, but rather is related to anatomical-hereditary factors, and to incorrect technical execution (as explained above: “rolling in”).
In the Ballet Dancers Group, 26% (34 feet of 132) of the feet measured were hypermobile in both dorsal and dorso-medial 45° directions, and a further 19% (25 feet of 132) were hypermobile only in the dorsal-medial 45° direction. In all other groups, feet with a hypermobile first ray in both directions, or only in the dorso-medial direction, were no more than 30% of the total. Therefore, when considering the “hypermobile” category as including not only those with a first ray that can be moved 10 mm or more in the dorsal direction, but also those individuals with a first ray mobility achieved only in the dorso-medial (but not on the dorsal) direction, the sensitivity and specificity of the correlation between hypermobility and hallux valgus exceed 81%. This confirms that hypermobility of the first metatarsal-cuneiform joint is an important factor in the development and progression of hallux valgus5.
Measurement of the mobility of the first ray is recommended in preparation for treatment of forefoot deformities11. In particular, for hallux valgus with a hypermobile first ray, therapy should be directed to the alignment of the metatarsal heads, so as to correct the entire forefoot loading pattern altered by the lack of load on the medial part of the foot. The treatment of choice for first ray hypermobility is therefore surgery, except in the case of very young patients (where the epiphyses have not yet settled) or with generalized ligamentous laxity (and therefore subject to frequent recurrence)1. In addition, problems related to hypermobility of the first ray in ballet dancers must be resolved by correction of the technical errors that underlie them rather than the use of conservative or surgical treatment, which would be disabling for the dancers and are destined to fail12.
Conclusions
In both groups, a significantly greater mobility of the first ray in the dorsal-medial 45° direction was found as compared to the conventional measurement in the sagittal plane, along with the presence, particularly in the Ballet Dancers Groups, of a significant percentage of subjects with normal mobility in the dorsal direction, but hypermobile at 45°. Moreover, first ray hypermobility, and even hallux valgus, are related to ballet practice, due to anatomical-hereditary factors, and to an incorrect technical execution (“rolling in”).
References
- 1.Myerson MS, Badekas A. Hypermobility of the first ray. Foot Ankle Clin. 2000;5(3):469–484. [PubMed] [Google Scholar]
- 2.Smith BW, Coughlin MJ. The first metatarso-cuneiform joint, hypermobility, and hallux valgus: what does it all mean? Foot Ankle Surg. 2008;14:138–141. doi: 10.1016/j.fas.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 3.Klaue K, Sigvard TH, Masquelet AC. Clinical, quantitative assessment of first tarsometatarsal mobility in the sagittal plane and its relation to hallux valgus deformity. Foot Ankle. 1994;15(1):9–13. doi: 10.1177/107110079401500103. [DOI] [PubMed] [Google Scholar]
- 4.Klaue K. Hallux Valgus and Hypermobiler erster strahl-kausale behandlung durch tarsometatarsale reorientierungsarthrodese. Ther Umschau. 1991;48(12):817–823. [PubMed] [Google Scholar]
- 5.Faber FWM, Kleinrensink GJ, Vehoog MW. Mobility of the first tarsometatarsal joint in relation to hallux valgus deformity: anatomical and biomechanical aspects. Foot Ankle Int. 1999;20(10):951–956. doi: 10.1177/107110079902001007. [DOI] [PubMed] [Google Scholar]
- 6.Coughlin MJ, Jones CP. Hallux valgus and first ray mobility: a prospective study. J Bone Joint Surg. 2007;89:1887–1898. doi: 10.2106/JBJS.F.01139. [DOI] [PubMed] [Google Scholar]
- 7.Glasoe WM, Yack HJ, Saltzman CL. The reliability and validity of a first ray measurement device. Foot Ankle Int. 2000;21:240–246. doi: 10.1177/107110070002100310. [DOI] [PubMed] [Google Scholar]
- 8.Wanivenhaus A, Pretterklieber M. First tarsometatarsal joint: anatomical biomechanical study. Foot Ankle. 1989;9:153–157. doi: 10.1177/107110078900900401. [DOI] [PubMed] [Google Scholar]
- 9.Goulart M, O’Malley MJ, Hodgkins CW. Foot and ankle fractures in dancers. Clin Sports Med. 2008;27:295–304. doi: 10.1016/j.csm.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Hamilton WG, Bauman PA, Kahan JSG. Foot and Ankle Injuries in Dancers. Foot and Ankle Surgery. (8th edition) :1603–1620. [Google Scholar]
- 11.Donatelli RA. Abnormal biomechanics. In: Donatelli RA, editor. The Biomechanics of the Foot and Ankle. 2nd ed. Philadelphia, Pa: FA Davis Co; 1996. pp. 34–72. [Google Scholar]
- 12.Ahonen J. Biomechanics of the foot in dance. A literature review. J Dance Med Sci. 2008;12(3):99–108. [PubMed] [Google Scholar]