Abstract
Skin homeostasis is maintained, in part, through regulation of gene expression orchestrated by type II nuclear hormone receptors in a cell and context specific manner. This group of transcriptional regulators is implicated in various cellular processes including epidermal proliferation, differentiation, permeability barrier formation, follicular cycling and inflammatory responses. Endogenous ligands for the receptors regulate actions during skin development and maintenance of tissue homeostasis. Type II nuclear receptor signaling is also important for cellular crosstalk between multiple cell types in the skin. Overall, these nuclear receptors are critical players in keratinocyte and melanocyte biology and present targets for cutaneous disease management.
Mechanisms of action for type II nuclear receptors
Transcriptional control of gene expression is achieved, in part, through protein factors bound to regulatory elements present on the chromatin. The type II nuclear receptors (NR), belonging to the superfamily of steroid-thyroid hormone nuclear receptors, contribute to the cellular responses of physiological demands [1] [2] [3] [4]. Transcriptional modulation is achieved by structural adjustments initiated through ligand binding. Present throughout the animal kingdom, this family of environmental sensors contributes both positively and negatively to gene expression. This differential regulation is useful in organismal development and homeostasis, though it is also implicated in a variety of pathological conditions. The present review will only detail the contributions of type II NRs towards epidermal and follicular development and homeostasis, and in skin diseases. Particular emphasis is given on melanocyte biology and in melanomagenesis arising from altered signaling between keratinocytes and melanocytes, while highlighting the potential therapeutic value of these pliable receptors.
Type II NRs belong to a larger family of steroid hormone receptors, all sharing similarities in domain structure (Fig. 1) [5] [6]. Distinct variations in domain sequence has allowed for the diversification and specialization currently present within the family [7]. The DNA binding domain is highly conserved across the family and contains two zinc finger motifs. These domains recognize and bind short response elements, allowing for both homo- and hetero-dimerization combinations. Two activation domains called AF-1 and AF-2 assist the receptors in dimerization and DNA binding. Variability is more evident within the carboxyl terminal ligand binding domain, where individual receptors have evolved to bind a variety of signaling molecules [8]. Receptors for which ligand specificity has yet to be determined are labeled as orphan receptors. Endogenous ligands for NRs known to be expressed in skin include: all-trans retinoic acid (RA) and 9-cis RA for retinoic acid receptor (RAR) [9] [10], 9-cis RA for retinoid-X-receptor (RXR) [2] [11], 1,25-dihydroxyvitamin D3 (1,25-(OH)2D3) for vitamin D receptor (VDR) [12], fatty acids/lipids for peroxisome proliferator-activated receptor (PPAR) [13] [14] [15] [16], oxysterols for liver X receptor (LXR) [17] and triiodothyronine for thyroid receptor (TR) [18].
Figure 1. Schematic representation of functional domains in type II nuclear receptors.

Transcriptional activation function 1 (AF-1) domain initiates at the amino terminus, followed by the DNA-binding domain (DBD). A flexible hinge region (H) assists in DNA binding, dimerization and transactivation functions. Variable ligand-binding domains (LBD) and a second activation function (AF-2) are present at the carboxyl terminus.
A distinguishing feature of type II NRs is the promiscuity displayed by RXR. All NRs from this class form heterodimers with an isoform of RXR (α/β/γ) and regulate gene expression in a ligand dependent fashion. RXRα is able to heterodimerize with some 15 NR family members and occupy direct repeat response elements present on the promoters of target genes [19] [20] [21] [22] [23]. The nonsteroidal ligands of RXR/NR heterodimers dictate the organization of complexes associated with the receptors. Serial combinations of regulatory proteins allow chromatin remodeling and recruitment of basal factors to initiate and/or repress transactivation (Fig. 2) [24] [25]. Coactivators include ATP-dependent chromatin remodelers, histone acetyltrasferases and the Mediator complex [26] [27] [28] [29] [30]. Corepressors comprise the N-CoR/SMRT assembly and histone deacetylases [31] [32] [33] [34]. The large numbers of regulatory factors, as well as tissue specific localization, allow NRs to influence a diverse range of gene expression in a cell and tissue specific manner. For example, the PPARγ cofactor PGC-1 is present in adipose tissue but not fibroblasts, allowing a cell-type specific activation of genes related to adaptive thermogenesis [35]. Post-translational modifications of co-factors such as phosphorylation, methylation, sumoylation and ubiquitination are also known to contribute to the extensive specificity of NR regulation [36].
Figure 2. Putative mechanisms of transcriptional regulation by type II nuclear receptors.
Repression of gene expression by nuclear receptor heterodimers involves association with co-repressor protein complexes, including NCoR/SMRT and histone deacetylases (HDAC). Positive transactivation occurs after ligand binding when co-repressor complexes are replaced by co-activator proteins such as ATP-dependant chromatin remodelers (ADCR), histone acetyltransferases (HAT) and the Mediator complex (MC). DBD, DNA-binding domain; LBD, ligand-binding domain; NRRE, nuclear receptor response element; TSS, transcriptional start site.
Skin morphogenesis, epidermal homeostasis and hair cycling
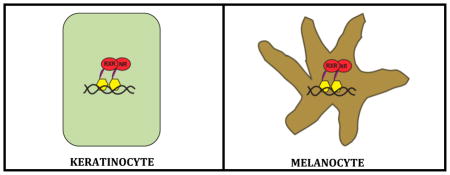
Skin is the largest organ in the body and is comprised of multiple cell types such as epidermal keratinocytes, dermal fibroblasts and hypodermal adipocytes, besides Langerhans cells, melanocytes and endothelial cells. It utilizes both autocrine and paracrine signaling for development and maintenance of tissue homeostasis [37]. The outermost epidermal layer provides a protective barrier to environmental and physical stresses and constantly progresses through cycles of proliferation and differentiation. Basal keratinocytes located on the innermost epidermal basement membrane (separating epidermis from the underlying dermis) generate daughter cells, which undergo committed differentiation that give rise to ordered layers of suprabasal early- and late-differentiated keratinocytes. Appendages such as hair follicles and sebaceous glands (SGs) are invaginated into the mesenchymal-derived dermal layer. Different resident multipotent skin stem cell (SC) niches contribute to the renewal, maintenance and repair of the epidermal tissues of the skin, including interfollicular epidermis (IFE), hair follicles and SGs [38]. Epidermal SCs play a crucial role in maintaining tissue homeostasis by supplying new daughter cells to replace those constantly lost during turnover or following injury. Bulge SCs are known to maintain normal follicle homeostasis and can also contribute to the formation of IFE following skin injury and during wound healing. Melanocytes are also located within the hair follicles where they primarily contribute pigmentation to coat color. In humans, IFE melanocyte populations rely on keratinocytic paracrine signaling for assistance in photoprotection from solar ultraviolet irradiation [39].
Type II nuclear receptor signaling contributes to the perpetual renewal of keratinocytic layers, maintenance of the epidermal permeability barrier (EPB) and follicular cycling. Impaired expression or function of these receptors is implicated in aberrant proliferation and/or differentiation of epidermal tissue and alopecia (hair loss). The promiscuous role that RXRs play in type II NR signaling hints to the impact that impaired RXR expression or activity influences receptor signal transduction. Although many of RXRs heterodimer partners are implicated in a wide variety of skin diseases, in many cases these pathologies could instead be associated with compromised RXR mediated gene regulation. Regardless, only studies that have specifically indicated a specific role for RXR function will be discussed here. RXRs play a critical and varied role in epidermal differentiation and EPB maintenance. RXRα, the primary isoform in skin and hair follicles, has stronger expression levels compared to RARs, and RXRα/RARγ heterodimer appears to be the major retinoid transducing element in epidermal biology [40] [41] [42]. RXRα/RARγ heterodimerization is also critical in the development and formation of epidermal lamellar granules by repression of target genes, as RARγ agonists promote lamellar granule defects in murine skin. Similarly, RXRα/PPARβ/δ heterodimers are equally important to stratum corneum homeostasis through activation of gene transcription [43].
The importance of vitamin A signaling to cutaneous homeostasis has long been observed. Although, comprehensive studies have investigated multiple proteins along this pathway in skin (such as retinoic acid binding proteins), this review will focus primarily on RARs in human and rodent skin, particularly the role of RARγ [40] [44]. RA is widely used as a therapeutic against various skin diseases due to its inhibitory effects on keratinocytic terminal differentiation, besides regulating keratinocyte proliferation and apoptosis, through modulation of RAR target genes [45]. Management of keratin expression, which in turn dictates status of epidermal differentiation, is a known regulatory mechanism of cutaneous RARs [46] [47] [48]. Unfortunately, the use of pan-retinoids is limited due to unwanted side effects such as skin irritation, hypertriglyceridemia, bone toxicity and teratogenicity [49] [50]. In order to utilize these efficacious compounds in a dermatological setting, receptor-selective retinoids in parallel with prophylactic lipid management therapies may provide clinical benefits with decreased risk of toxicities.
Early studies have elucidated the synthesis of pre-hormone 25-hydroxycholecalciferol (calcifediol) by murine epidermal basal cells that acts in a paracrine manner for the CYP27B1 and VDR expressing differentiated keratinocytes [51]. Typical of the type II nuclear receptors, 1,25(OH)2D3-induced VDR activation inhibited proliferation and promoted differentiation of keratinocytes, though VDR/RXRα heterodimers can transactivate keratinocytic genes independent of 1,25(OH)2D3 binding [52]. DeltaNp63alpha, a critical regulator of epidermal biology, is known to directly control VDR expression in murine skin and mediate its function in a ligand-independent manner [53]. Mice bearing a targeted ablation of VDR present a large number of pathological properties in the skin, including progressive alopecia and dermal cysts as well as decreased expression of epidermal differentiation markers [54] [55]. By expressing in discrete epidermal locations, VDR-interacting coactivators contributed divergent roles towards keratinocyte proliferation and differentiation [56] [57]. VDR and its associated cofactors also contributed to lipid production and epidermal barrier formation. Genetic network analysis has implicated VDR as a necessary regulator of skin barrier formation and predicts the phenotype characterized in the VDR-null mice [58]. Many epidermal genes induced by WNT/β-catenin contain VDR response elements and were activated independently of TCF/LEF, implying that it is part of a TCF/LEF-independent aspect of WNT signaling [59]. Likewise, depletion of follicular keratinocyte populations in VDR-null mice was linked to aberration of the canonical WNT pathway [60].
Alopecia is a commonplace in hereditary resistance to 1,25(OH)2D3 and VDR expression is seen in the outer root sheath keratinocytes and dermal papilla of follicles, increasing during late anagen and catagen [61]. The transcriptional repressor hairless (HR) co-localized with VDR in the outer root sheath of hair and has been shown to inhibit target genes leading to hair cycle progression [62]. Another VDR cofactor and critical subunit of the transcriptional coactivator complex Mediator (MED), MED1, has been recently linked to hair cycling and epidermal proliferation and differentiation. Selective ablation of MED1 in keratinocytes presents a similar phenotype to VDR or HR ablation [63]. miR-125b is a known repressor of skin differentiation in the bulge region of the hair follicle and expressing miR-125b in SC progeny significantly downregulated VDR activity [64].
PPARβ/δ expression was seen in both basal and suprabasal layers of the normal human epidermis, while PPARα and PPARγ expression was confined to suprabasal epidermal cells and was linked to squamous differentiation [65]. PPARs are transcriptionally regulated by AP-1, C/EBP family members and p63, the master regulator of epidermal morphogenesis and differentiation [66] [67]. Mechanistically, inhibition of the PKC/MAPK pathway through PPAR-mediated PKCα-ubiqutitination has been implicated in reduction of epidermal proliferation [68]. All PPAR isoforms were expressed in human hair follicle cells while PPARγ ablation in mice mimicked a human scarring alopecia phenotype [69] [70].
The ability of LXRs to act as environmental cholesterol sensors enables them to contribute to consistent epidermal turnover which support a sound EPB. LXRα/β are expressed in all layers of the human epidermis, as well as in the outer root sheath and SG, and the LXR agonists oxysterols act on epidermal keratinocytes by reducing proliferation and inducing differentiation [71]. One proposed mechanism of LXR mediated induction of keratinocytic differentiation is influencing the binding of transcriptional complex AP-1 to target genes. ChIP-on-chip studies investigating LXRβ/RXRα binding in human keratinocytes revealed a strong correlation to AP-1 response elements, with up to 77% of all LXRβ/RXRα binding sites associated with AP-1 motifs [72]. This could indicate LXR involvement in the pathogenesis of certain diseases that present with abnormal keratinocytic differentiation and/or compromised barrier function.
Thyroid-stimulating hormone receptor signaling is commonly associated with cutaneous biology, though TR ligand binding is also known to contribute to epidermal homeostasis. Resistance to thyroid hormones is a syndrome with a wide variety of symptoms and is connected to TRβ mutations in in both mice and humans [73] [74]. Follicular TRβ is the predominant isoform expressed within human skin and one phenotype of the disease linked to aberrant TRβ signaling is alopecia [75] [76]. In support of a role for TRβ in hair cycle homeostasis, thyroid hormones and TRβ-selective thyromimetics are able to induce hair growth in both murine and simian models, as well as stimulate intrafollicular melanin production [77] [78]. TRs bind to conserved keratin response elements located in the promoter region of epidermal keratin genes and can directly control their transcription. One proposed mechanism of these genes involves transcriptional repression in the presence of a liganded TR receptor. In this scenario, proteins typically seen as components of a co-activator/histone acetylase complex display repressive tendencies in the presence of liganded receptors while co-repressors act as activators when unliganded TRs are present on the keratin response element [79]. Transcriptome analyses from epidermal keratinocytes treated with either thyroid hormone or vehicle display only a small number of genes that are differentially expressed. Among the suppressed genes (integrin β4, plectin, collagen XVII, MMP1/3/14) there was significant association to the blistering skin disease epidermolysis bullosa, implying an inhibitory role of thyroid signaling to extracellular matrix maintenance [80].
Inflammatory skin diseases
Cutaneous inflammatory disorders are characterized by inflammation of the skin that can lead to patient discomfort or disfigurement. Psoriasis is a genetic-based cutaneous syndrome that involves epidermal hyperproliferation, compromised EPB and an infiltrative immune response. It is present in up to 5% of the population, affects both sexes equally and is able to manifest within the first two decades of life [81]. As it is currently incurable, primary treatment options focus on the control of symptoms and include the use of topical corticosteroids, phototherapy and moisturizing creams [82]. As proof of concept that type II NR activation is a feasible therapeutic approach, acitretin and calcipotriol are widely utilized for psoriasis. Atopic dermatitis (AD) is another chronic inflammatory skin disease that is characterized by dry and itchy skin, persistent infections and very early onset [83]. AD is linked to other atopic diseases such as asthma and allergic rhinitis, and defective EPB function, environmental insults or genetic background are predisposing factors for this heterogeneous disease [84] [85]. Treatment options are similar to those for psoriasis, while preventing future allergic reactions is also important. Unfortunately, the roots of these diseases may be too deeply embedded in immune functions to be eradicated. Due to early onset and lifelong activity, the use of chronic corticosteroid therapy is discouraged. Knowledge regarding transcriptional regulation by key factors of EPB and epidermal proliferation gene networks enhances our retinue of therapeutic strategies in these diseases. NR ligands may be useful to modulate multiple pathways in order to lessen side effects and/or concentrations of the more efficacious compounds.
Mice with an epidermal-specific ablation of RXRα (RXRαep−/−) presented epidermal hyperplasia, alopecia, dermal cysts and a cutaneous inflammatory response [86] [87]. Likewise, mice lacking both RXRα and RXRβ in keratinocytes (RXRαβep−/−) developed a chronic dermatitis similar to human AD patients, elevated serum IgE/IgG and cytokine production associated with Th2-type response. Importantly, thymic stromal lymphopoietin (TSLP) was strongly upregulated from the basal keratinocytes, potentially influencing the systemic AD phenotype in these mice [88]. To further support the hypothesis that loss of RXRα contributed to a derepressive mechanism on gene expression leading to inflammatory responses, expression of RXRα has been reported to decrease in human psoriatic lesions, with levels in progressive disease further reduced compared to stable stages [89].
Use of the anti-proliferative, pro-differentiative properties of 1,25(OH)2D3 is not ideal due to harmful calcemic effects. Therefore, synthetic deltanoids represent the best way to initiate VDR activation for therapeutic or investigative purposes. It was previously discussed that keratinocytic RXRα/β ablation upregulates production of TSLP leading to an AD-like phenotype in the mouse. Interestingly, topical application of deltanoids also induces TSLP in epidermal keratinocytes, suggesting the role of RXR/VDR heterodimers in regulating TSLP expression in this cell type. That evidence suggests a role for VDR antagonists in the treatment of human AD patients [90]. Conversely, deltanoids were shown to significantly improve allergen-triggered eczema in a mouse model through increasing populations of FOXP3-expressing regulatory T cells [91]. Further evidences are needed to determine how VDR transactivation can initiate anti-inflammatory mechanisms if deltanoids are to become accepted therapy for hyperproliferative epidermal disorders in the clinic.
The anti-inflammatory actions of PPARα offer additional treatment modalities for reoccurring skin conditions such as AD and psoriasis. Stimulation of epidermal differentiation and reduction of proliferation can potentially treat these conditions without severe side effects brought on by glucocorticoids (GC). PPARα−/− mice (with a germline deletion of the Pparα gene) subjected to antigen sensitization exhibit increased epidermal thickening and inflammatory responses compared to wild-type controls, potentially through the loss of IL-2-mediated induction of Treg populations [92]. PPARα−/− skin also display heightened levels of both Th2- and Th1-related responses, as well as enhanced NF-κB signaling. Furthermore, PPARα expression is downregulated in lesional skin of human AD patients compared to non-atopic individuals [93]. Topical application of PPARα agonists reduces the hyperplastic response in mouse skin brought on by TPA treatment, in part through the reduction of inflammatory cytokines. Similar results were seen in oxazolone (OX)-induced allergic dermatitis mouse models, and importantly, combination therapy of PPARα agonists and GCs for severe dermatitis prevented GC-induced side effects and inhibited rebound flares [94] [95]. Conversely, activation of PPARβ/δ may trigger psoriasis pathogenesis within the skin and treatment strategies may include antagonism of this signaling pathway. PPARβ/δ is upregulated at both the mRNA and protein level in psoriatic lesions compared to nonlesional skin in human patients and eicosanoid accumulations within the lesions can activate PPARβ/δ [96] [97]. Also, topical antagonists targeted to cutaneous PPARβ/δ demonstrated efficacy in a psoriatic mouse model [98]. Alongside other physiological defects, PPARβ/δ-null mice exhibit an elevated epidermal hyperplastic response after TPA administration and delayed barrier recovery following acute barrier disruption [99] [100]. An increase in the release of inflammatory cytokines after wound healing in murine skin requires upregulation of PPARβ/δ that is otherwise undetected in normal skin. Interestingly, this pro-inflammatory cascade initiates production of endogenous PPARβ/δ ligands, reinforcing the activation of PPARβ/δ after skin injury [101] [102]. PPARβ/δ is also linked to UV-induced premature senescence via upregulation of PTEN that attenuates reactive oxygen species in keratinocytes [103]. Likewise, epidermal PPARγ signaling is also a target for the UV-induced inflammatory response. UV irradiation of human keratinocytes produces potent PPARγ agonistic activity and enhances COX-2 expression in these cells. Furthermore, PPARγ activation was seen as a general consequence to various oxidative stressors in human sebocytes [104] [105].
An increased accessibility of environmental antigens through epidermal tissue can activate cutaneous immune responses that potentially drive inflammation. Creation and maintenance of the EPB is a multistep process involving lipid production and lamellar body formation and LXR activation appears to hold key functions in many of these stages [106] [107]. EPB function is tightly linked to cholesterol levels in the epidermis and LXR has been shown to regulate the storage and efflux of lipid species. Members of the ATP-binding cassette transporter family such as ABCA1, ABCA12 and ABCG1, as well as the glycerol channel AQP3, are transcriptionally regulated by oxysterols [108] [109] [110] [111]. Environmental toxins present in cigarette smoke have been linked to several skin diseases including psoriasis and melanoma [112] [113]. Translocation of LXR to the nucleus in HaCaT cells after exposure to cigarette smoke facilitated an increase in cholesterol trafficking as a result of increased ABCA1 expression [114]. The ability of the synthetic LXR agonist T1317 to prevent physical changes inherent to photoaging and chronological skin aging has been investigated. T1317 inhibited the expression of cytokines and metalloproteinases in cell-based models of skin aging. Furthermore, LXRβ-null murine skin mimics some of the characteristics seen in chronologically aged human skin and the topically applied agonist reduced UV-induced skin thickness and wrinkle formation in a mouse model [115].
The anti-inflammatory actions of LXR activators have been demonstrated in both irritant and oxazolone (OX)-induced allergic dermatitis mouse models, in part through the inhibition of proinflammatory cytokines that are specific to LXRβ [116] [117]. Similarly, global gene expression studies using primary human keratinocytes from psoriatic lesions, non-affected skin of the same patients and healthy control subjects, indicates a role for LXRα in regulating inflammatory response. Along the same line, knocking down LXRα in human keratinocytes lead to a genomic profile similar to that seen in psoriatic skin lesions [118]. Even if LXRs are not directly involved in disease pathogenesis, the receptors might still be utilized as therapeutic tools to modulate cellular lipid levels. For example, a human sebaceous cell line treated with LXRα agonists increased lipid synthesis and induced the lipogenic gene SREBP-1, potentially useful for the treatment of seborrhea and acne [119]. Selective LXR agonists that are isoform and tissue-specific could provide localized and specific cutaneous effects that do not influence other LXR receptor pools [120] [121].
Epidermal carcinogenesis
Non-melanoma skin cancers arise from both the basal and squamous cells of the epidermis. Basal cell carcinoma (BCC) is the most common neoplasm related to the Caucasian population and its incidence rate is increasing yearly [122]. Though considered malignant due to its ability to invade deep into tissue, it rarely metastasizes from the primary location. Risk factors include fair skin disposed to freckling, family history of BCC and exposure to ultraviolet radiation. Patients with BCC also tend to be prone to other types of skin cancer including malignant melanoma [123]. Disease progression typically arises from UV-induced actinic keratosis or mutations in the hedgehog signaling pathway. Surgical excision is the treatment of choice though pathway specific compounds such as vismodegib provide additional therapy options [124]. Cutaneous squamous cell carcinoma (SCC) is the second leading cause of skin cancer, yet unlike BCC it tends to exhibit metastatic behavior [125]. Again, exposure to ultraviolet radiation is the predominant risk factor for this disease, though immunosuppressed patients are at increased risk for metastatic spread [126]. Treatment options include surgical removal, radiation therapy and in certain cases chemotherapeutics such as 5-fluorouracil or imiquimod [127]. Investigations into pathways regulating keratinocytic proliferation and differentiation may lead to additional treatment options useful in treating these disfiguring diseases.
The transcription factor KLF4 is required for proper EPB formation in mice and dysregulated KLF4 activity is shown to be oncogenic [128]. KLF4 regulates expression of RXRα and KLF4-induced malignant transformation is sensitive to retinoids in vitro. Importantly, rexinoid application drastically prevented formation of SCC in a KLF4-activated transgenic mouse line [129]. These results suggest existence of a crosstalk between RXR and KLF4 signaling, where KLF4-mediated expression of RXRα contributes to tumor suppressor activity within the epidermis. RXRαep−/− mice, selectively lacking RXRα in epidermal keratinocytes, subjected to a 7,12-dimethylbenz(a)anthracene (DMBA)/12-O-tetradecanolyphoral-13-acetate (TPA) induced two-step chemical carcinogenic protocol developed higher numbers of epidermal tumors compared to control mice [130]. The RXRαep−/− papillomas progressed towards SCC in a murine model, further validating the role of RXRα as a cutaneous tumor suppressor.
Both keratinocytes and melanocytes downregulated expression of RARs when subjected to UV exposure, potentially initiating cellular responses to ionizing radiation through the removal of repressive transcriptional controls [131] [132] [133]. A similar downregulation of RAR in mouse skin was seen after application of TPA, as well as when normal human skin progresses through premalignant actinic keratosis to invasive SCC [134] [135] [136]. A loss of RARγ expression exacerbated carcinogenic effects of tumor promoters and enhances malignant transformation [137] [138]. Topical application of RA during the promotion stage of carcinogen treatment in mice reduced the yield of papilloma and carcinoma formation [139]. Likewise, the RARβ/γ retinoid tazarotene displayed anti-tumoral activity when topically applied to BCC and may inhibit psoriatic proinflammatory gene networks [140] [141] [142]. Above results indicate important roles of retinoids and retinoid receptors in the control of epidermal homeostasis and prevention of hyper-proliferative diseases and skin cancer.
The regulatory nature of VDR in hair cycle progression and barrier formation is critical to maintain skin homeostasis, therefore defects in the transactivating function of the receptor allow pathological conditions to manifest. Multiple VDR polymorphisms have been associated with a broad spectrum of cutaneous disease, including SCC, BCC and vitiligo [143] [144] [145] [146] [147] [148]. Indeed, inactivation of VDR in mice enhanced sensitivity to both chemical and solar-induced skin carcinogenesis, potentially through activation of the hedgehog pathway [149] [150].
Due to evidence of PPAR signaling in the development of aberrant growths in differing tissue types, studies have investigated the role of these receptors in cutaneous neoplasms. Tumor formation and size were increased after chemical carcinogen application in PPARβ/δ−/− mice, while those selectively lacking PPARγ in epidermal keratinocytes show an increase in benign tumors, SCC and BCCs [130] [151]. Ligand activation of PPARβ/δ inhibits chemically induced skin tumorigenesis, most likely through induction of keratinocytic differentiation, and the addition of COX-2 inhibitors may result in synergistic efficacy [152] [153].
In mice, TRβ expression is detected in normal and TPA-treated hyperplastic skin. Loss of TRβ expression is seen in benign papillomas generated by the DMBA/TPA protocol and completely abrogated in subsequent SCC formation. Importantly, skin tumors from mice lacking both TRα and TRβ were more likely to develop in situ carcinoma and SCC than those from wildtype mice, supporting TRs role as a tumor suppressor [154]. In order to determine the role TRs have in the hyperproliferative response, TRα/β-double null mice were subjected to both TPA and RA treatments [155] [156]. Reduced hyperplasia with a decreased expression of cyclin D1 was seen in the TRα/β−/− skin after TPA treatment. That profile was correlated with increases in cell cycle inhibitors p19 and p27, as well as induction of proinflammatory cytokines and phosphorylation of p65/NF-κB and STAT3. This phenotype is opposite to that seen in PPARβ/δ−/− mice and elucidates the combinatorial mechanisms RXR/NR heterodimers regulate within the skin. Similarly, a typical retinoid response requires the presence of ligand-bound TR in mouse skin. Decreases in skin hyperplasia and expression of keratins 5/6, alongside increased transcription of inflammatory and chemotactic cytokines, are also seen in TRα/β−/− mice treated with 9-cis RA. Since TPA and retinoids are modulating separate signaling cascades, it is possible that TRs are involved in the cellular responses to both these compounds.
Melanocyte homeostasis and melanomagenesis
Melanocytes are neural crest-derived pigment producing cells that contribute photoprotective properties to the skin. Cutaneous melanoma is the deadliest form of skin cancer, with a diagnosis of metastasis indicating a median survival rate of less than a year [157]. Solar ultraviolet irradiation, especially childhood sun exposure, is an important etiological risk factor of melanoma [158]. Surgical excision prevents growth of the primary lesion, yet once transformed melanocytes spread to distal organs and this disease is refractory to current therapeutics. Recent evidence supports the use of MAPK inhibitors and immunomodulatory treatments with the goal of increasing lifespan [159] [160]. Therefore, any research directed towards key regulators of melanocytic activity could potentially open up new avenues for disease management.
Type II NR-mediated signaling via RXR dimerization is essential to melanocyte biology. RXRα and β expression has been detected in B16 and S91 murine melanoma cells, with RXRβ being the predominant isoform [161] [162]. Interestingly, loss of melanocytic RXRα expression was seen in human primary and metastatic melanoma compared to benign nevi, indicating the importance of this signaling pathway to the differentiation of these cell types [163]. RARβ expression was also downregulated in melanoma and its RA-induced expression was linked to growth inhibition and differentiation in these cells. Sequential occupation of the RA response element located on the Rarβ promoter by RXR/RXR and RXR/RAR combinations is believed to be a molecular switch responsible for Rarβ transcriptional activation in these cells. Since ligand activation of RXR heterodimeric partners regulates transcriptional activity of target genes involved with differentiation and growth arrest, it is possible that combinatorial activation of both dimer partners may assist in melanoma therapy. Rexinoid treatment alongside glitazones (PPARγ agonists) have displayed efficacy against melanomagenesis in in vitro and xenograft models, potentially through the inhibition of matrix metalloproteases and increases in S100A2 calcium binding activity [164] [165] [166].
Our own work has demonstrated the role of keratinocytic RXRα in manipulating melanocyte activation and proliferation through modulation of the cutaneous microenvironment [167]. RXRα/NR heterodimer binding regulates transcriptional repression of soluble mitogens and cytokines, making it a critical factor in the ultraviolet radiation (UVR) induced cellular responses. The loss of keratinocytic RXRα in RXRαep−/− mice relieves transcriptional repression and allows overexpression of keratinocytic soluble factors that act on melanocytic cell-surface receptors. Higher numbers of epidermal melanocytes were seen after UVR exposure in RXRαep−/− mice compared to controls, suggesting contribution of soluble factors in the cellular microenvironment for melanocyte activation and migration out of the hair follicle. Indeed, increased expression of Edn1, Fgf2 and Kitlg, that are known to be upregulated by keratinocytes and influence melanocyte activation, migration and proliferation, were seen in RXRαep−/− skin post-UVR [167]. Interestingly, in a two-step carcinogenesis model, RXRαep−/− mice developed a higher number of dermal melanocytic growths (nevi) compared to control mice, implicating contribution of keratinocyte-derived factors in melanomagenesis. Only nevi from RXRα mutant mice progressed to melanoma-like tumors, suggesting that RXRα-mediated distinct non-cell autonomous actions suppressed nevi formation and melanoma progression in mice [130]. Similarly, VDR−/− mice undergoing identical treatments also developed higher numbers of melanocytic lesions, indicating RXRα/VDR heterodimerization may be the causative factors, at least in part, in these non-cell autonomous events [130]. Finally, the loss of keratinocytic RXRα alongside an activated-CDK4 mutation enhanced the metastatic transformation of cutaneous melanoma after chemical carcinogenesis. Expression of Edn1, Hgf, Fgf2, Pomc and Kitlg were all upregulated in the skin of RXRαep−/−/CDK4R24C/R24C bigenic mice. Direct binding of RXRα on the promoter of Edn1 and Hgf was also seen in ex vivo primary murine keratinocytes. Gene expression analyses on mRNA isolated from melanocytic lesions from the bigenic skin using laser-capture microdissection demonstrated reduced apoptotic and enhanced invasive responses within bigenic melanomas. Loss of epidermal RXRα was also seen in human melanoma progression and could potentially be utilized as a therapeutic biomarker [168]. These results indicated a crucial role of RXRα/NR signaling in melanocytic homeostasis and in cellular responses to tumor promotion.
All RAR isoforms were expressed in melanocytes and treatment of retinoids, particularly RARγ-specific agonists, inhibits growth and initiates apoptosis in melanoma cells [169] [170] [171]. RA treatment increases expression of RARβ and PKCα while stimulating AP-1 transcriptional activity in melanoma cells. RARα specific agonists were most effective in upregulating RARβ levels and combinatorial RAR/RXR activation demonstrate the strongest induction of both PKCα and AP-1 function in murine melanoma cells [172] [173] [174]. Loss of RARs, especially RARβ and its tumor suppressor activities, was observed during melanomagenesis and could account for RA resistance in this disease [163] [175] [176]. That disruption of RARβ or RARγ signaling in benign nevi may predispose a lesion towards malignant transformation. Co-treatment of retinoids with histone deacetylases also counteracted the epigenetic silencing of RARβ often seen in RA resistant melanoma cell lines and provides increased antitumor activity [177]. Another mechanism implicated in RA-resistant melanoma cells is an increase in intracellular reactive oxygen species (ROS) that is inversely related to RAR activity. RA-sensitivity was restored when ROS levels were lowered, potentially through improved RXR/RAR promoter binding activity [178]. RA treatment in combination with polyl:C synergistically increased the toll-like receptor 3 chemokine responses in human melanoma cells and induced migration of antigen-presenting cells [179]. Decreased expression of collagenolytic-enzymes and alterations in mobility-associated cell surface receptors were consequences of RAR activation in melanoma cells [180] [181]. Further evidence of RARγ-mediated inhibition of melanoma invasion came from microarray analysis of murine melanoma cells treated with RARγ agonists, which identified the sulfotransferase CHST10 as being directly regulated by RARγ through RA response elements located in its promoter region. CHST10 synthesizes a HNK-1 carbohydrate that was involved with cell adhesion in the nervous system and RA-mediated embryonic plasticity [182]. Altogether, RAR-specific agonists present a potential therapeutic candidate for the treatment of metastatic melanoma if mechanisms of RA resistance can be elucidated and exploited.
Skin is both a target and producer of 1,25(OH)2D3, the secosteroid ligand of VDR and regulation of melanocyte homeostasis is a physiological role that is attributed to VDR signaling. The use of vitamin D analogs to combat vitiligo depigmentation has been well reviewed [183]. It is hoped that Vitamin D agonists might protect melanocyte loss in this disease through inhibition of immune response and modulating calcium flux. VDR activation may also promote re-pigmentation processes by upregulating melanogenic cytokines that drive pigment production. Due to insufficient knowledge on what drives the etiology of this disease, any research implicating driver mutations is important for developing effective therapeutics. Genomic DNA isolated from vitiligo patients, as well as age and sex-matched controls, demonstrated the TaqI VDR polymorphism is a risk factor for the disease. Haplotype BsmI/ApaI/TaqI/FokI/Cdx2 was also overrepresented in those patients [148].
The use of low-calcemic deltanoids for treatment of melanocytic lesions is another potential candidate for future therapies. Sunlight generates DNA damage within melanocytes yet also produces anti-proliferative 1,25(OH)2D3 ligands. This physiological dichotomy provides endogenous regulation of melanomagenesis and may offer directions on how to manage cutaneous melanoma. Human melanoma cell lines have been shown to posses different expression levels of VDR and different growth inhibitory responses to 1,25(OH)2D3. Importantly, melanoma cells demonstrate increased sensitivity to deltanoids compared to normal melanocytes [184]. Similar to some other type II NRs, a loss of VDR expression was seen during the progression of melanocytic lesions and that attenuated VDR signaling was linked to decreased overall survival time [185]. Likewise, a retrospective cohort study of large numbers of melanoma patients associated higher serum 1,25(OH)2D3 levels with thinner presenting melanomas and improved survival from melanoma [186]. In addition to investigations associating VDR polymorphisms to keratinocytic pathologies, extensive studies have shown VDR mutations as a critical contributing factor towards melanoma susceptibility and outcome, in particular the BsmI, FokI and TaqI polymorphisms [187] [188] [189]. Not all melanoma cell lines were sensitive to 1,25(OH)2D3 treatment though. Resistance to 1,25(OH)2D3 treatment may be attributed to epigenetic mechanisms that abrogate VDR signaling in those cell lines. An inverse relationship has been shown to exist between VDR mRNA expression and level of microRNA miR-125b, most likely through posttranscriptional regulation of VDR by miR-125b interacting with a recognition element in the 3′-UTR of human VDR mRNA. Treatment of these cells with a DNA methyltransferase inhibitor reduces expression of miR-125b and may prove efficacious alongside other chemical therapies [190] [191]. In short, aberrant VDR signaling appears to contribute significantly to the development of melanoma in humans and 1,25(OH)2D3 analogs may provide additional targeted chemotherapeutics in the treatment of that disease.
Due to importance of lipid metabolism in skin homeostasis, PPAR signaling in skin has been thoroughly investigated, including its role in melanocyte homeostasis. All PPAR isoforms are expressed in human melanocytes, though PPARγ signaling appears to be a primary possible drug target for melanoma. Two common PPARγ polymorphisms implicated in susceptibility of the malignant disease were evaluated as influences in melanoma risk, though it appeared that inactivating mutations do not appear to be a significant risk factor for the disease [192]. Recently a link was shown between α-MSH signaling and PPARγ nuclear translocation that reduced proliferation rates and increased melanogenesis through the Pi(4,5)P2/Plcβ pathway [193]. Glitazones are known to activate PPARγ and promote melanocyte differentiation. One mechanism to induce melanocyte differentiation is through β-catenin mediated upregulation of MITF levels. Phenotypic changes that occured in melanoma cells post-ciglitazone treatment include dendritic morphology and increased tyrosinase functions, possibly linked to large increases of Mitf promoter activity. β-catenin protein levels in ciglitazone-treated murine melanoma cells followed the same trend of transient increase followed by gradual decrease pattern as seen with MITF, suggesting that depleted levels of nuclear β-catenin was influencing the downregulation of MITF activity in these cells [194]. In addition to its pro-differentiative properties, inhibition of proliferation was seen in melanoma cells after ciglitazone treatment and is also associated with induction of apoptosis [195]. PPARγ agonists regulate the WNT3A/β-catenin signaling pathway and inhibits human melanoma cell proliferation through direct inhibition of β-catenin activity [196]. Though PPAR functions as a tumor suppressor at times, two studies screening large numbers of melanocytic lesions determined that both PPARγ and COX-2 expression was increased during progression from benign nevi to metastatic melanoma and may indicate therapy response levels of this disease [197] [198]. That conflicting role of PPARγ in tumorigenesis has yet to be elucidated but provides an exciting investigative target in the treatment of metastatic melanoma.
Few reports demonstrate a role of LXR activation in melanocytes, though known LXR target genes are important in melanocyte biology. LXRα appears to be the predominant isoform and could provide LXR-oriented strategies of melanoma therapy. LXRα expression was also localized adjacent to the follicular dermal papilla, suggesting a contribution to hair follicle melanocyte activity [199]. LXRα expression was seen in both human melanocytes and in melanoma cells. Moreover, LXRα mRNA and protein levels were increased in melanocytes present in the skin surrounding vitiligo lesions compared to normal skin, suggesting LXRα is modulating the melanocytic response to this disorder [200] [201]. Interestingly, LXRα has been linked to immunoevasion of melanoma through inhibition of dendritic cell (DC) migration to lymphoid organs. Production of LXR ligands from both human and mouse tumors were shown to hinder CCR7 expression on DCs that is required for lymphoid homing. Conditioned media from the human melanoma cell line MSR3 was shown to inhibit CCR7 expression in DCs, though not affecting other aspects of DC activation. Also, the media from MSR3, as well as from another melanoma cell line MR255, was able to activate LXRα reporter constructs, suggesting the presence of ligands expressed in the media. Use of the sulfotransferase enzyme SULT2B1b, which inactivates natural oxysterols, was able to protect CCR7 inhibition from the conditioned media. Similarly, mice receiving bone marrow transplants from an LXRα-null line demonstrated an enhanced ability of tumor rejection [202]. Altogether, studies indicate an important immuno-modulatory role of LXR signaling in melanocytic lesions and in melanoma primarily mediated by LXRα. Additional studies are required to establish the receptor functions in melanocyte homeostasis and in melanomagenesis.
Evidence for a role of TR in melanocyte biology is limited, though thyroid-stimulating hormone expression is seen in epidermal melanocytes. Of note, one study involving patients with uveal melanoma demonstrated that 60% of the cohort contained a loss of heterozygosity in the TRβ alleles in both the ciliary body and choroidal melanomas [203]. Further in vivo studies are needed to determine how TR signaling is impaired in epidermal diseases and in skin cancer, as well as the severity of any non-autonomous actions that affect the malignant transformation of melanocytic cells.
Conclusion
RXR/NR signaling makes important contributions to both the development and homeostasis of keratinocyte and melanocyte biology (Table 1). The ability of epidermal tissue to maintain a rigorous cycle of proliferation and differentiation utilizes complex transduction pathways that rely on tight transcriptional control of key target genes. Ligand activated regulation of gene transcription and/or repression by type II NR heterodimers is one example of how skin is able to continually replenish itself while at the same time inhibiting neoplastic transformation. Extensive research presents a scenario where type II NRs are critical tumor suppressors that regulate the sequential differentiation of maturing keratinocytes. With the exception of TR, which does not appear to play a major role in skin biology, loss of RXR/NR activity through inactivating mutations or epigenetic silencing leads to hyperproliferation and immune responses. Likewise, activation of NR heterodimers through endogenous ligand binding, or exogenous topical application of synthetic agonists, typically provides anti-inflammatory actions. Modulation of these receptors could provide supplemental therapy for inflammatory skin disease that is usually treated with potent GCs. The development of tissue specific NR ligands may provide additional relief for diseases such as psoriasis and AD that are not currently curable. RXR/VDR regulation of genes such as TSLP provides strong drug targets that could significantly alter the micro-environmental milieu that drives skin inflammation. Abolishing keratinocytic derived paracrine signaling utilized by melanocytes and immune cells may provide additional options in curative techniques for skin diseases including melanoma. Overall, RXR/NR signaling has evolved as extensive and dominant signaling networks within skin, the largest organ and most important barrier to environmental damages and insults. Utilizing these regulatory checkpoints through the use of synthetic ligands will be an important focus of cutaneous research in the immediate future.
Table 1.
Description of pathologies associated with alteration of skin keratinocytes and melanocytes homeostasis and mechanisms influenced by type II nuclear receptor signaling. Summary of references from the primary literature reviewed regarding keratinocyte or melanocyte-associated NR signaling. AD, atopic dermatitis; BCC, basal cell carcinoma; EPB, epidermal permeability barrier; Hh, hedgehog; SC, stratum corneum; SCC, squamous cell carcinoma; TSLP, thymic stromal lymphopoietin; UVR, ultraviolet radiation.
| ||
|---|---|---|
| RXR | ||
| Pathology | Mechanism | Ref. |
| EPB defects | Lamellar granule formation in epidermis | 43 |
| Alopecia | Follicular destruction and hair cycling defects, epidermal hyperplasia | 86, 87 |
| AD | TSLP derepression and Th2-type inflammation | 88, 90 |
| Psoriasis | Stage-related loss of expression | 89 |
| SCC | Cell-autonomous suppression of epidermal tumorigenesis and progression | 130 |
| Stage-related loss of expression | 136 | |
| Melanoma | Stage-related loss of expression | 163, 175 |
| Growth and invasion arrest by NR ligands | 164 | |
| Growth arrest by NR ligands | 165, 166, 172 | |
| Keratinocyte-derived paracrine effects in melanomagenesis | 130, 167, 168 | |
| RAR | ||
|---|---|---|
| Pathology | Mechanism | Ref |
| EPB defects | Lamellar granules formation in epidermis | 43 |
| Aging | UVR-induced loss of expression | 131, 132 |
| AD | TSLP derepression and Th2-type inflammation | 90 |
| Psoriasis | Negative gene regulation via retinoids | 140 |
| SCC | Stage-related loss of expression induces malignant progression | 136, 138 |
| BCC | Anti-proliferative and pro-apoptotic effects of retinoids | 141 |
| BCC | Tumor suppressor activities of basal RAR signaling | 142 |
| Melanoma | Stage-related loss of expression | 163, 175 |
| Epigenetic silencing of RARβ | 176 | |
| Anti-proliferative and pro-differentiative properties | 165, 169, 172, 174 | |
| Induction of apoptosis by retinoids | 170, 171 | |
| Regulation of cell surface receptors | 180, 182 | |
| Modulates HLA-DR expression on melanoma | 169 | |
| Increase in chemokine and IFNβ secretion | 179 | |
| VDR | ||
|---|---|---|
| Pathology | Mechanism | Ref |
| EPB defects | VDR genetic network linked to EPB function, inflammation | 58 |
| Alopecia | VDR−/− mice display progressive hair loss | 55 |
| Alopecia | VDR drives mammalian hair cycle through gene repression | 62 |
| AD | TSLP derepression and Th2-type inflammation | 58, 90 |
| AD | Low-calcemic VDR agonist improves allergen-induced eczema | 91 |
| SCC | VDR polymorphisms linked to SCC development, tumor susceptibility | 58, 143, 147 |
| SCC | VDR−/− mice susceptible to carcinogen-induced SCC through Hh pathway | 149, 150 |
| BCC | VDR polymorphisms linked to BCC development | 146, 147 |
| BCC | VDR−/− mice susceptible to carcinogen-induced BCC through Hh pathway | 150 |
| Vitiligo | VDR polymorphisms linked to vitiligo susceptibility | 148 |
| VDR targets the epidermal melanin unit | 183 | |
| Melanoma | Stage-related loss of expression of VDR | 185, 186 |
| miRNA associated epigenetic silencing | 190, 191 | |
| Anti-proliferative and pro-differentiative properties of vitamin D analogs | 184 | |
| VDR polymorphisms linked to melanoma development | 187, 188, 189 | |
| PPAR | ||
|---|---|---|
| Pathology | Mechanism | Ref |
| EPB formation | Lamellar granules formation | 43 |
| PPAR agonists regulate involucrin and CD36 expression | 65 | |
| PPARβ/δ is required for EPB homeostasis | 100 | |
| Activators stimulates lipid synthesis and processing | 107 | |
| Regulate expression of cholesterol and water transporters | 109, 110, 111 | |
| Alopecia | PPARγ ablation in hair follicles displays a scarring alopecia phenotype | 69 |
| Aging | PPARδ/γ provides resistance to UV-induced cellular senescence through PTEN upregulation | 103 |
| PPARγ is necessary for production of UV-induced epidermal prostaglandins | 104 | |
| AD | PPAR regulates IL-2-mediated Treg induction | 92 |
| PPAR negatively regulates skin inflammation through TH1 and TH2 responses | 93 | |
| PPAR agonists as therapy in murine AD models | 94, 95, 117 | |
| Psoriasis | Activation of epidermal PPAR linked to psoriatic gene regulation | 96, 97 |
| Inhibition of PPAR signaling as therapy for psoriasis | 98 | |
| SCC | Loss of expression induces malignant progression | 130 |
| Inhibition of PPAR signaling as therapy for SCC | 152, 153 | |
| BCC | Loss of expression during progression | 130 |
| Melanoma | Growth and invasion arrest by PPARγ ligands | 164 |
| Growth arrest by PPARγ, RAR and RXR agonists | 165, 166 | |
| PPAR-mediated downregulation of β-catenin downregulates MITF | 194 | |
| Growth arrest and induction of apoptosis by PPARγ ligands | 195 | |
| PPARγ agonists inhibit proliferation and modulate Wnt/β-catenin mediated signaling | 196 | |
| LXR | ||
|---|---|---|
| Pathology | Mechanism | Ref |
| EPB defects | LXR/AP-1 crosstalk in lipid production and barrier formation | 72 |
| EPB formation | Acidification of SC | 106 |
| EPB formation | Activators stimulates lipid synthesis and processing | 107 |
| EPB formation | Regulate expression of cholesterol and water transporters | 108, 109, 110, 111 |
| Aging | Cigarette smoke inhibits LXR translocation | 114 |
| Aging | Phenotype of chronically aged skin | 115 |
| AD | LXR agonists display anti-inflammatory effects | 116, 117 |
| Psoriasis | Loss of LXRα expression stimulates psoriatic gene profile | 118 |
| Vitiligo | Increased expression in vitiligo perilesional skin | 201 |
| Melanoma | LXR ligands inhibit CCR7 expression on maturing DCs and their migration to lymphoid organs | 202 |
References
- 1.Evans RM. The steroid and thyroid hormone receptor superfamily. Science. 1988;240:889–95. doi: 10.1126/science.3283939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mangelsdorf DJ, Ong ES, Dyck JA, Evans RM. Nuclear receptor that identifies a novel retinoic acid response pathway. Nature. 1990;345:224–9. doi: 10.1038/345224a0. [DOI] [PubMed] [Google Scholar]
- 3.Mangelsdorf DJ, Thummel C, Beato M, Herrlich P, Schutz G, Umesono K, Blumberg B, Kastner P, Mark M, Chambon P, Evans RM. The nuclear receptor superfamily: the second decade. Cell. 1995;83:835–9. doi: 10.1016/0092-8674(95)90199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chambon P. A decade of molecular biology of retinoic acid receptors. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 1996;10:940–54. [PubMed] [Google Scholar]
- 5.Escriva H, Langlois MC, Mendonca RL, Pierce R, Laudet V. Evolution and diversification of the nuclear receptor superfamily. Annals of the New York Academy of Sciences. 1998;839:143–6. doi: 10.1111/j.1749-6632.1998.tb10747.x. [DOI] [PubMed] [Google Scholar]
- 6.Kumar R, Thompson EB. The structure of the nuclear hormone receptors. Steroids. 1999;64:310–9. doi: 10.1016/s0039-128x(99)00014-8. [DOI] [PubMed] [Google Scholar]
- 7.Laudet V. Evolution of the nuclear receptor superfamily: early diversification from an ancestral orphan receptor. Journal of molecular endocrinology. 1997;19:207–26. doi: 10.1677/jme.0.0190207. [DOI] [PubMed] [Google Scholar]
- 8.Bourguet W, Germain P, Gronemeyer H. Nuclear receptor ligand-binding domains: three-dimensional structures, molecular interactions and pharmacological implications. Trends in pharmacological sciences. 2000;21:381–8. doi: 10.1016/s0165-6147(00)01548-0. [DOI] [PubMed] [Google Scholar]
- 9.Giguere V, Ong ES, Segui P, Evans RM. Identification of a receptor for the morphogen retinoic acid. Nature. 1987;330:624–9. doi: 10.1038/330624a0. [DOI] [PubMed] [Google Scholar]
- 10.Petkovich M, Brand NJ, Krust A, Chambon P. A human retinoic acid receptor which belongs to the family of nuclear receptors. Nature. 1987;330:444–50. doi: 10.1038/330444a0. [DOI] [PubMed] [Google Scholar]
- 11.Heyman RA, Mangelsdorf DJ, Dyck JA, Stein RB, Eichele G, Evans RM, Thaller C. 9-cis retinoic acid is a high affinity ligand for the retinoid X receptor. Cell. 1992;68:397–406. doi: 10.1016/0092-8674(92)90479-v. [DOI] [PubMed] [Google Scholar]
- 12.Simpson RU, DeLuca HF. Characterization of a receptor-like protein for 1,25-dihydroxyvitamin D3 in rat skin. Proceedings of the National Academy of Sciences of the United States of America. 1980;77:5822–6. doi: 10.1073/pnas.77.10.5822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forman BM, Tontonoz P, Chen J, Brun RP, Spiegelman BM, Evans RM. 15-Deoxy-delta 12, 14-prostaglandin J2 is a ligand for the adipocyte determination factor PPAR gamma. Cell. 1995;83:803–12. doi: 10.1016/0092-8674(95)90193-0. [DOI] [PubMed] [Google Scholar]
- 14.Kliewer SA, Lenhard JM, Willson TM, Patel I, Morris DC, Lehmann JM. A prostaglandin J2 metabolite binds peroxisome proliferator-activated receptor gamma and promotes adipocyte differentiation. Cell. 1995;83:813–9. doi: 10.1016/0092-8674(95)90194-9. [DOI] [PubMed] [Google Scholar]
- 15.Kliewer SA, Sundseth SS, Jones SA, Brown PJ, Wisely GB, Koble CS, Devchand P, Wahli W, Willson TM, Lenhard JM, Lehmann JM. Fatty acids and eicosanoids regulate gene expression through direct interactions with peroxisome proliferator-activated receptors alpha and gamma. Proceedings of the National Academy of Sciences of the United States of America. 1997;94:4318–23. doi: 10.1073/pnas.94.9.4318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Forman BM, Chen J, Evans RM. Hypolipidemic drugs, polyunsaturated fatty acids, and eicosanoids are ligands for peroxisome proliferator-activated receptors alpha and delta. Proceedings of the National Academy of Sciences of the United States of America. 1997;94:4312–7. doi: 10.1073/pnas.94.9.4312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janowski BA, Willy PJ, Devi TR, Falck JR, Mangelsdorf DJ. An oxysterol signalling pathway mediated by the nuclear receptor LXR alpha. Nature. 1996;383:728–31. doi: 10.1038/383728a0. [DOI] [PubMed] [Google Scholar]
- 18.Samuels HH, Tsai JS, Casanova J. Thyroid hormone action: in vitro demonstration of putative receptors in isolated nuclei and soluble nuclear extracts. Science. 1974;184:1188–91. doi: 10.1126/science.184.4142.1188. [DOI] [PubMed] [Google Scholar]
- 19.Leid M, Kastner P, Lyons R, Nakshatri H, Saunders M, Zacharewski T, Chen JY, Staub A, Garnier JM, Mader S, et al. Purification, cloning, and RXR identity of the HeLa cell factor with which RAR or TR heterodimerizes to bind target sequences efficiently. Cell. 1992;68:377–95. doi: 10.1016/0092-8674(92)90478-u. [DOI] [PubMed] [Google Scholar]
- 20.Kliewer SA, Umesono K, Mangelsdorf DJ, Evans RM. Retinoid X receptor interacts with nuclear receptors in retinoic acid, thyroid hormone and vitamin D3 signalling. Nature. 1992;355:446–9. doi: 10.1038/355446a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Willy PJ, Umesono K, Ong ES, Evans RM, Heyman RA, Mangelsdorf DJ. LXR, a nuclear receptor that defines a distinct retinoid response pathway. Genes & development. 1995;9:1033–45. doi: 10.1101/gad.9.9.1033. [DOI] [PubMed] [Google Scholar]
- 22.Chandra V, Huang P, Hamuro Y, Raghuram S, Wang Y, Burris TP, Rastinejad F. Structure of the intact PPAR-gamma-RXR-nuclear receptor complex on DNA. Nature. 2008;456:350–6. doi: 10.1038/nature07413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orlov I, Rochel N, Moras D, Klaholz BP. Structure of the full human RXR/VDR nuclear receptor heterodimer complex with its DR3 target DNA. The EMBO journal. 2012;31:291–300. doi: 10.1038/emboj.2011.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glass CK, Rosenfeld MG. The coregulator exchange in transcriptional functions of nuclear receptors. Genes & development. 2000;14:121–41. [PubMed] [Google Scholar]
- 25.Perissi V, Rosenfeld MG. Controlling nuclear receptors: the circular logic of cofactor cycles. Nature reviews Molecular cell biology. 2005;6:542–54. doi: 10.1038/nrm1680. [DOI] [PubMed] [Google Scholar]
- 26.Dilworth FJ, Fromental-Ramain C, Yamamoto K, Chambon P. ATP-driven chromatin remodeling activity and histone acetyltransferases act sequentially during transactivation by RAR/RXR In vitro. Molecular cell. 2000;6:1049–58. doi: 10.1016/s1097-2765(00)00103-9. [DOI] [PubMed] [Google Scholar]
- 27.De Luca A, Severino A, De Paolis P, Cottone G, De Luca L, De Falco M, Porcellini A, Volpe M, Condorelli G. p300/cAMP-response-element-binding-protein (‘CREB’)-binding protein (CBP) modulates co-operation between myocyte enhancer factor 2A (MEF2A) and thyroid hormone receptor-retinoid X receptor. The Biochemical journal. 2003;369:477–84. doi: 10.1042/BJ20020057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blanco JC, Minucci S, Lu J, Yang XJ, Walker KK, Chen H, Evans RM, Nakatani Y, Ozato K. The histone acetylase PCAF is a nuclear receptor coactivator. Genes & development. 1998;12:1638–51. doi: 10.1101/gad.12.11.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fondell JD, Ge H, Roeder RG. Ligand induction of a transcriptionally active thyroid hormone receptor coactivator complex. Proceedings of the National Academy of Sciences of the United States of America. 1996;93:8329–33. doi: 10.1073/pnas.93.16.8329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rachez C, Lemon BD, Suldan Z, Bromleigh V, Gamble M, Naar AM, Erdjument-Bromage H, Tempst P, Freedman LP. Ligand-dependent transcription activation by nuclear receptors requires the DRIP complex. Nature. 1999;398:824–8. doi: 10.1038/19783. [DOI] [PubMed] [Google Scholar]
- 31.Underhill C, Qutob MS, Yee SP, Torchia J. A novel nuclear receptor corepressor complex, N-CoR, contains components of the mammalian SWI/SNF complex and the corepressor KAP-1. The Journal of biological chemistry. 2000;275:40463–70. doi: 10.1074/jbc.M007864200. [DOI] [PubMed] [Google Scholar]
- 32.Yoon HG, Chan DW, Huang ZQ, Li J, Fondell JD, Qin J, Wong J. Purification and functional characterization of the human N-CoR complex: the roles of HDAC3, TBL1 and TBLR1. The EMBO journal. 2003;22:1336–46. doi: 10.1093/emboj/cdg120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miyata KS, McCaw SE, Meertens LM, Patel HV, Rachubinski RA, Capone JP. Receptor-interacting protein 140 interacts with and inhibits transactivation by, peroxisome proliferator-activated receptor alpha and liver-X-receptor alpha. Molecular and cellular endocrinology. 1998;146:69–76. doi: 10.1016/s0303-7207(98)00196-8. [DOI] [PubMed] [Google Scholar]
- 34.Lee CH, Wei LN. Characterization of receptor-interacting protein 140 in retinoid receptor activities. The Journal of biological chemistry. 1999;274:31320–6. doi: 10.1074/jbc.274.44.31320. [DOI] [PubMed] [Google Scholar]
- 35.Puigserver P, Wu Z, Park CW, Graves R, Wright M, Spiegelman BM. A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell. 1998;92:829–39. doi: 10.1016/s0092-8674(00)81410-5. [DOI] [PubMed] [Google Scholar]
- 36.Hermanson O, Glass CK, Rosenfeld MG. Nuclear receptor coregulators: multiple modes of modification. Trends in endocrinology and metabolism: TEM. 2002;13:55–60. doi: 10.1016/s1043-2760(01)00527-6. [DOI] [PubMed] [Google Scholar]
- 37.Fuchs E, Raghavan S. Getting under the skin of epidermal morphogenesis. Nature reviews Genetics. 2002;3:199–209. doi: 10.1038/nrg758. [DOI] [PubMed] [Google Scholar]
- 38.Fuchs E. Scratching the surface of skin development. Nature. 2007;445:834–42. doi: 10.1038/nature05659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nishimura EK. Melanocyte stem cells: a melanocyte reservoir in hair follicles for hair and skin pigmentation. Pigment cell & melanoma research. 2011;24:401–10. doi: 10.1111/j.1755-148X.2011.00855.x. [DOI] [PubMed] [Google Scholar]
- 40.Fisher GJ, Talwar HS, Xiao JH, Datta SC, Reddy AP, Gaub MP, Rochette-Egly C, Chambon P, Voorhees JJ. Immunological identification and functional quantitation of retinoic acid and retinoid X receptor proteins in human skin. The Journal of biological chemistry. 1994;269:20629–35. [PubMed] [Google Scholar]
- 41.Billoni N, Gautier B, Mahe YF, Bernard BA. Expression of retinoid nuclear receptor superfamily members in human hair follicles and its implication in hair growth. Acta dermato-venereologica. 1997;77:350–5. doi: 10.2340/0001555577350355. [DOI] [PubMed] [Google Scholar]
- 42.Feng X, Peng ZH, Di W, Li XY, Rochette-Egly C, Chambon P, Voorhees JJ, Xiao JH. Suprabasal expression of a dominant-negative RXR alpha mutant in transgenic mouse epidermis impairs regulation of gene transcription and basal keratinocyte proliferation by RAR-selective retinoids. Genes & development. 1997;11:59–71. doi: 10.1101/gad.11.1.59. [DOI] [PubMed] [Google Scholar]
- 43.Calleja C, Messaddeq N, Chapellier B, Yang H, Krezel W, Li M, Metzger D, Mascrez B, Ohta K, Kagechika H, Endo Y, Mark M, Ghyselinck NB, Chambon P. Genetic and pharmacological evidence that a retinoic acid cannot be the RXR-activating ligand in mouse epidermis keratinocytes. Genes & development. 2006;20:1525–38. doi: 10.1101/gad.368706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chapellier B, Mark M, Messaddeq N, Calleja C, Warot X, Brocard J, Gerard C, Li M, Metzger D, Ghyselinck NB, Chambon P. Physiological and retinoid-induced proliferations of epidermis basal keratinocytes are differently controlled. The EMBO journal. 2002;21:3402–13. doi: 10.1093/emboj/cdf331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee DD, Stojadinovic O, Krzyzanowska A, Vouthounis C, Blumenberg M, Tomic-Canic M. Retinoid-responsive transcriptional changes in epidermal keratinocytes. Journal of cellular physiology. 2009;220:427–39. doi: 10.1002/jcp.21784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tomic M, Jiang CK, Epstein HS, Freedberg IM, Samuels HH, Blumenberg M. Nuclear receptors for retinoic acid and thyroid hormone regulate transcription of keratin genes. Cell regulation. 1990;1:965–73. doi: 10.1091/mbc.1.12.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Navarro JM, Casatorres J, Jorcano JL. Elements controlling the expression and induction of the skin hyperproliferation-associated keratin K6. The Journal of biological chemistry. 1995;270:21362–7. doi: 10.1074/jbc.270.36.21362. [DOI] [PubMed] [Google Scholar]
- 48.Virtanen M, Sirsjo A, Vahlquist A, Torma H. Keratins 2 and 4/13 in reconstituted human skin are reciprocally regulated by retinoids binding to nuclear receptor RARalpha. Experimental dermatology. 2010;19:674–81. doi: 10.1111/j.1600-0625.2010.01079.x. [DOI] [PubMed] [Google Scholar]
- 49.Chandraratna RA. Future trends: a new generation of retinoids. Journal of the American Academy of Dermatology. 1998;39:S149–52. doi: 10.1016/s0190-9622(98)70313-5. [DOI] [PubMed] [Google Scholar]
- 50.Altucci L, Gronemeyer H. The promise of retinoids to fight against cancer. Nature reviews Cancer. 2001;1:181–93. doi: 10.1038/35106036. [DOI] [PubMed] [Google Scholar]
- 51.Rizk-Rabin M, Zineb R, Zhor B, Michele G, Jana P. Synthesis of and response to 1,25 dihydroxycholecalciferol by subpopulations of murine epidermal keratinocytes: existence of a paracrine system for 1,25 dihydroxycholecalciferol. Journal of cellular physiology. 1994;159:131–41. doi: 10.1002/jcp.1041590117. [DOI] [PubMed] [Google Scholar]
- 52.Ellison TI, Eckert RL, MacDonald PN. Evidence for 1,25-dihydroxyvitamin D3-independent transactivation by the vitamin D receptor: uncoupling the receptor and ligand in keratinocytes. The Journal of biological chemistry. 2007;282:10953–62. doi: 10.1074/jbc.M609717200. [DOI] [PubMed] [Google Scholar]
- 53.Kommagani R, Leonard MK, Lewis S, Romano RA, Sinha S, Kadakia MP. Regulation of VDR by deltaNp63alpha is associated with inhibition of cell invasion. Journal of cell science. 2009;122:2828–35. doi: 10.1242/jcs.049619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yoshizawa T, Handa Y, Uematsu Y, Takeda S, Sekine K, Yoshihara Y, Kawakami T, Arioka K, Sato H, Uchiyama Y, Masushige S, Fukamizu A, Matsumoto T, Kato S. Mice lacking the vitamin D receptor exhibit impaired bone formation, uterine hypoplasia and growth retardation after weaning. Nature genetics. 1997;16:391–6. doi: 10.1038/ng0897-391. [DOI] [PubMed] [Google Scholar]
- 55.Xie Z, Komuves L, Yu QC, Elalieh H, Ng DC, Leary C, Chang S, Crumrine D, Yoshizawa T, Kato S, Bikle DD. Lack of the vitamin D receptor is associated with reduced epidermal differentiation and hair follicle growth. The Journal of investigative dermatology. 2002;118:11–6. doi: 10.1046/j.1523-1747.2002.01644.x. [DOI] [PubMed] [Google Scholar]
- 56.Oda Y, Uchida Y, Moradian S, Crumrine D, Elias PM, Bikle DD. Vitamin D receptor and coactivators SRC2 and 3 regulate epidermis-specific sphingolipid production and permeability barrier formation. The Journal of investigative dermatology. 2009;129:1367–78. doi: 10.1038/jid.2008.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bikle DD, Teichert A, Arnold LA, Uchida Y, Elias PM, Oda Y. Differential regulation of epidermal function by VDR coactivators. The Journal of steroid biochemistry and molecular biology. 2010;121:308–13. doi: 10.1016/j.jsbmb.2010.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Quigley DA, To MD, Perez-Losada J, Pelorosso FG, Mao JH, Nagase H, Ginzinger DG, Balmain A. Genetic architecture of mouse skin inflammation and tumour susceptibility. Nature. 2009;458:505–8. doi: 10.1038/nature07683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Palmer HG, Anjos-Afonso F, Carmeliet G, Takeda H, Watt FM. The vitamin D receptor is a Wnt effector that controls hair follicle differentiation and specifies tumor type in adult epidermis. PloS one. 2008;3:e1483. doi: 10.1371/journal.pone.0001483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cianferotti L, Cox M, Skorija K, Demay MB. Vitamin D receptor is essential for normal keratinocyte stem cell function. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:9428–33. doi: 10.1073/pnas.0702884104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reichrath J, Schilli M, Kerber A, Bahmer FA, Czarnetzki BM, Paus R. Hair follicle expression of 1,25-dihydroxyvitamin D3 receptors during the murine hair cycle. The British journal of dermatology. 1994;131:477–82. doi: 10.1111/j.1365-2133.1994.tb08547.x. [DOI] [PubMed] [Google Scholar]
- 62.Haussler MR, Haussler CA, Whitfield GK, Hsieh JC, Thompson PD, Barthel TK, Bartik L, Egan JB, Wu Y, Kubicek JL, Lowmiller CL, Moffet EW, Forster RE, Jurutka PW. The nuclear vitamin D receptor controls the expression of genes encoding factors which feed the “Fountain of Youth” to mediate healthful aging. The Journal of steroid biochemistry and molecular biology. 2010;121:88–97. doi: 10.1016/j.jsbmb.2010.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Oda Y, Hu L, Bul V, Elalieh H, Reddy JK, Bikle DD. Coactivator MED1 ablation in keratinocytes results in hair-cycling defects and epidermal alterations. The Journal of investigative dermatology. 2012;132:1075–83. doi: 10.1038/jid.2011.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang L, Stokes N, Polak L, Fuchs E. Specific microRNAs are preferentially expressed by skin stem cells to balance self-renewal and early lineage commitment. Cell stem cell. 2011;8:294–308. doi: 10.1016/j.stem.2011.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Westergaard M, Henningsen J, Svendsen ML, Johansen C, Jensen UB, Schroder HD, Kratchmarova I, Berge RK, Iversen L, Bolund L, Kragballe K, Kristiansen K. Modulation of keratinocyte gene expression and differentiation by PPAR-selective ligands and tetradecylthioacetic acid. The Journal of investigative dermatology. 2001;116:702–12. doi: 10.1046/j.1523-1747.2001.01329.x. [DOI] [PubMed] [Google Scholar]
- 66.Di-Poi N, Desvergne B, Michalik L, Wahli W. Transcriptional repression of peroxisome proliferator-activated receptor beta/delta in murine keratinocytes by CCAAT/enhancer-binding proteins. The Journal of biological chemistry. 2005;280:38700–10. doi: 10.1074/jbc.M507782200. [DOI] [PubMed] [Google Scholar]
- 67.Pozzi S, Boergesen M, Sinha S, Mandrup S, Mantovani R. Peroxisome proliferator-activated receptor-alpha is a functional target of p63 in adult human keratinocytes. The Journal of investigative dermatology. 2009;129:2376–85. doi: 10.1038/jid.2009.92. [DOI] [PubMed] [Google Scholar]
- 68.Kim DJ, Murray IA, Burns AM, Gonzalez FJ, Perdew GH, Peters JM. Peroxisome proliferator-activated receptor-beta/delta inhibits epidermal cell proliferation by down-regulation of kinase activity. The Journal of biological chemistry. 2005;280:9519–27. doi: 10.1074/jbc.M413808200. [DOI] [PubMed] [Google Scholar]
- 69.Karnik P, Tekeste Z, McCormick TS, Gilliam AC, Price VH, Cooper KD, Mirmirani P. Hair follicle stem cell-specific PPARgamma deletion causes scarring alopecia. The Journal of investigative dermatology. 2009;129:1243–57. doi: 10.1038/jid.2008.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ruge F, Glavini A, Gallimore AM, Richards HE, Thomas CP, O’Donnell VB, Philpott MP, Porter RM. Delineating immune-mediated mechanisms underlying hair follicle destruction in the mouse mutant defolliculated. The Journal of investigative dermatology. 2011;131:572–9. doi: 10.1038/jid.2010.379. [DOI] [PubMed] [Google Scholar]
- 71.Komuves LG, Schmuth M, Fowler AJ, Elias PM, Hanley K, Man MQ, Moser AH, Lobaccaro JM, Williams ML, Mangelsdorf DJ, Feingold KR. Oxysterol stimulation of epidermal differentiation is mediated by liver X receptor-beta in murine epidermis. The Journal of investigative dermatology. 2002;118:25–34. doi: 10.1046/j.0022-202x.2001.01628.x. [DOI] [PubMed] [Google Scholar]
- 72.Shen Q, Bai Y, Chang KC, Wang Y, Burris TP, Freedman LP, Thompson CC, Nagpal S. Liver X receptor-retinoid X receptor (LXR-RXR) heterodimer cistrome reveals coordination of LXR and AP1 signaling in keratinocytes. The Journal of biological chemistry. 2011;286:14554–63. doi: 10.1074/jbc.M110.165704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Usala SJ, Tennyson GE, Bale AE, Lash RW, Gesundheit N, Wondisford FE, Accili D, Hauser P, Weintraub BD. A base mutation of the C-erbA beta thyroid hormone receptor in a kindred with generalized thyroid hormone resistance. Molecular heterogeneity in two other kindreds. The Journal of clinical investigation. 1990;85:93–100. doi: 10.1172/JCI114438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Forrest D, Hanebuth E, Smeyne RJ, Everds N, Stewart CL, Wehner JM, Curran T. Recessive resistance to thyroid hormone in mice lacking thyroid hormone receptor beta: evidence for tissue-specific modulation of receptor function. The EMBO journal. 1996;15:3006–15. [PMC free article] [PubMed] [Google Scholar]
- 75.Billoni N, Buan B, Gautier B, Gaillard O, Mahe YF, Bernard BA. Thyroid hormone receptor beta1 is expressed in the human hair follicle. The British journal of dermatology. 2000;142:645–52. doi: 10.1046/j.1365-2133.2000.03408.x. [DOI] [PubMed] [Google Scholar]
- 76.Guran T, Bircan R, Turan S, Bereket A. Alopecia: association with resistance to thyroid hormones. Journal of pediatric endocrinology & metabolism : JPEM. 2009;22:1075–81. doi: 10.1515/jpem.2009.22.11.1075. [DOI] [PubMed] [Google Scholar]
- 77.van Beek N, Bodo E, Kromminga A, Gaspar E, Meyer K, Zmijewski MA, Slominski A, Wenzel BE, Paus R. Thyroid hormones directly alter human hair follicle functions: anagen prolongation and stimulation of both hair matrix keratinocyte proliferation and hair pigmentation. The Journal of clinical endocrinology and metabolism. 2008;93:4381–8. doi: 10.1210/jc.2008-0283. [DOI] [PubMed] [Google Scholar]
- 78.Li JJ, Mitchell LH, Dow RL. Thyroid receptor agonists for the treatment of androgenetic alopecia. Bioorganic & medicinal chemistry letters. 2010;20:306–8. doi: 10.1016/j.bmcl.2009.10.109. [DOI] [PubMed] [Google Scholar]
- 79.Jho SH, Vouthounis C, Lee B, Stojadinovic O, Im MJ, Brem H, Merchant A, Chau K, Tomic-Canic M. The book of opposites: the role of the nuclear receptor co-regulators in the suppression of epidermal genes by retinoic acid and thyroid hormone receptors. The Journal of investigative dermatology. 2005;124:1034–43. doi: 10.1111/j.0022-202X.2005.23691.x. [DOI] [PubMed] [Google Scholar]
- 80.Tomic-Canic M, Stojadinovic O, Lee B, Walsh R, Blumenberg M. Nexus between epidermolysis bullosa and transcriptional regulation by thyroid hormone in epidermal keratinocytes. Clinical and translational science. 2008;1:45–9. doi: 10.1111/j.1752-8062.2008.00015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Benoit S, Hamm H. Childhood psoriasis. Clinics in dermatology. 2007;25:555–62. doi: 10.1016/j.clindermatol.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 82.Menter A, Gottlieb A, Feldman SR, Van Voorhees AS, Leonardi CL, Gordon KB, Lebwohl M, Koo JY, Elmets CA, Korman NJ, Beutner KR, Bhushan R. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 1. Overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. Journal of the American Academy of Dermatology. 2008;58:826–50. doi: 10.1016/j.jaad.2008.02.039. [DOI] [PubMed] [Google Scholar]
- 83.Leung DY, Nicklas RA, Li JT, Bernstein IL, Blessing-Moore J, Boguniewicz M, Chapman JA, Khan DA, Lang D, Lee RE, Portnoy JM, Schuller DE, Spector SL, Tilles SA. Disease management of atopic dermatitis: an updated practice parameter. Joint Task Force on Practice Parameters. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology. 2004;93:S1–21. doi: 10.1016/s1081-1206(10)61385-3. [DOI] [PubMed] [Google Scholar]
- 84.Kapoor R, Menon C, Hoffstad O, Bilker W, Leclerc P, Margolis DJ. The prevalence of atopic triad in children with physician-confirmed atopic dermatitis. Journal of the American Academy of Dermatology. 2008;58:68–73. doi: 10.1016/j.jaad.2007.06.041. [DOI] [PubMed] [Google Scholar]
- 85.Cork MJ, Danby SG, Vasilopoulos Y, Hadgraft J, Lane ME, Moustafa M, Guy RH, Macgowan AL, Tazi-Ahnini R, Ward SJ. Epidermal barrier dysfunction in atopic dermatitis. The Journal of investigative dermatology. 2009;129:1892–908. doi: 10.1038/jid.2009.133. [DOI] [PubMed] [Google Scholar]
- 86.Li M, Indra AK, Warot X, Brocard J, Messaddeq N, Kato S, Metzger D, Chambon P. Skin abnormalities generated by temporally controlled RXRalpha mutations in mouse epidermis. Nature. 2000;407:633–6. doi: 10.1038/35036595. [DOI] [PubMed] [Google Scholar]
- 87.Li M, Chiba H, Warot X, Messaddeq N, Gerard C, Chambon P, Metzger D. RXR-alpha ablation in skin keratinocytes results in alopecia and epidermal alterations. Development. 2001;128:675–88. doi: 10.1242/dev.128.5.675. [DOI] [PubMed] [Google Scholar]
- 88.Li M, Messaddeq N, Teletin M, Pasquali JL, Metzger D, Chambon P. Retinoid X receptor ablation in adult mouse keratinocytes generates an atopic dermatitis triggered by thymic stromal lymphopoietin. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:14795–800. doi: 10.1073/pnas.0507385102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Feng S, Lin L, Wu Q, Zhou W, Shao C. Study on the expression of RXRalpha in patients with psoriasis vulgaris. European journal of dermatology : EJD. 2006;16:33–8. [PubMed] [Google Scholar]
- 90.Li M, Hener P, Zhang Z, Kato S, Metzger D, Chambon P. Topical vitamin D3 and low-calcemic analogs induce thymic stromal lymphopoietin in mouse keratinocytes and trigger an atopic dermatitis. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:11736–41. doi: 10.1073/pnas.0604575103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hartmann B, Riedel R, Jorss K, Loddenkemper C, Steinmeyer A, Zugel U, Babina M, Radbruch A, Worm M. Vitamin D receptor activation improves allergen-triggered eczema in mice. The Journal of investigative dermatology. 2012;132:330–6. doi: 10.1038/jid.2011.296. [DOI] [PubMed] [Google Scholar]
- 92.Dubrac S, Elentner A, Schoonjans K, Auwerx J, Schmuth M. Lack of IL-2 in PPAR-alpha-deficient mice triggers allergic contact dermatitis by affecting regulatory T cells. European journal of immunology. 2011;41:1980–91. doi: 10.1002/eji.201041357. [DOI] [PubMed] [Google Scholar]
- 93.Staumont-Salle D, Abboud G, Brenuchon C, Kanda A, Roumier T, Lavogiez C, Fleury S, Remy P, Papin JP, Bertrand-Michel J, Terce F, Staels B, Delaporte E, Capron M, Dombrowicz D. Peroxisome proliferator-activated receptor alpha regulates skin inflammation and humoral response in atopic dermatitis. The Journal of allergy and clinical immunology. 2008;121:962–8. e6. doi: 10.1016/j.jaci.2007.12.1165. [DOI] [PubMed] [Google Scholar]
- 94.Sheu MY, Fowler AJ, Kao J, Schmuth M, Schoonjans K, Auwerx J, Fluhr JW, Man MQ, Elias PM, Feingold KR. Topical peroxisome proliferator activated receptor-alpha activators reduce inflammation in irritant and allergic contact dermatitis models. The Journal of investigative dermatology. 2002;118:94–101. doi: 10.1046/j.0022-202x.2001.01626.x. [DOI] [PubMed] [Google Scholar]
- 95.Hatano Y, Elias PM, Crumrine D, Feingold KR, Katagiri K, Fujiwara S. Efficacy of combined peroxisome proliferator-activated receptor-alpha ligand and glucocorticoid therapy in a murine model of atopic dermatitis. The Journal of investigative dermatology. 2011;131:1845–52. doi: 10.1038/jid.2011.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Westergaard M, Henningsen J, Johansen C, Rasmussen S, Svendsen ML, Jensen UB, Schroder HD, Staels B, Iversen L, Bolund L, Kragballe K, Kristiansen K. Expression and localization of peroxisome proliferator-activated receptors and nuclear factor kappaB in normal and lesional psoriatic skin. The Journal of investigative dermatology. 2003;121:1104–17. doi: 10.1046/j.1523-1747.2003.12536.x. [DOI] [PubMed] [Google Scholar]
- 97.Romanowska M, Reilly L, Palmer CN, Gustafsson MC, Foerster J. Activation of PPARbeta/delta causes a psoriasis-like skin disease in vivo. PloS one. 2010;5:e9701. doi: 10.1371/journal.pone.0009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hack K, Reilly L, Palmer C, Read KD, Norval S, Kime R, Booth K, Foerster J. Skin-targeted inhibition of PPAR beta/delta by selective antagonists to treat PPAR beta/delta-mediated psoriasis-like skin disease in vivo. PloS one. 2012;7:e37097. doi: 10.1371/journal.pone.0037097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Peters JM, Lee SS, Li W, Ward JM, Gavrilova O, Everett C, Reitman ML, Hudson LD, Gonzalez FJ. Growth, adipose, brain, and skin alterations resulting from targeted disruption of the mouse peroxisome proliferator-activated receptor beta(delta) Molecular and cellular biology. 2000;20:5119–28. doi: 10.1128/mcb.20.14.5119-5128.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Man MQ, Barish GD, Schmuth M, Crumrine D, Barak Y, Chang S, Jiang Y, Evans RM, Elias PM, Feingold KR. Deficiency of PPARbeta/delta in the epidermis results in defective cutaneous permeability barrier homeostasis and increased inflammation. The Journal of investigative dermatology. 2008;128:370–7. doi: 10.1038/sj.jid.5701026. [DOI] [PubMed] [Google Scholar]
- 101.Tan NS, Michalik L, Noy N, Yasmin R, Pacot C, Heim M, Fluhmann B, Desvergne B, Wahli W. Critical roles of PPAR beta/delta in keratinocyte response to inflammation. Genes & development. 2001;15:3263–77. doi: 10.1101/gad.207501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tan NS, Michalik L, Desvergne B, Wahli W. Genetic- or transforming growth factor-beta 1-induced changes in epidermal peroxisome proliferator-activated receptor beta/delta expression dictate wound repair kinetics. The Journal of biological chemistry. 2005;280:18163–70. doi: 10.1074/jbc.M412829200. [DOI] [PubMed] [Google Scholar]
- 103.Ham SA, Hwang JS, Yoo T, Lee H, Kang ES, Park C, Oh JW, Lee HT, Min G, Kim JH, Seo HG. Ligand-activated PPARdelta inhibits UVB-induced senescence of human keratinocytes via PTEN-mediated inhibition of superoxide production. The Biochemical journal. 2012;444:27–38. doi: 10.1042/BJ20111832. [DOI] [PubMed] [Google Scholar]
- 104.Zhang Q, Southall MD, Mezsick SM, Johnson C, Murphy RC, Konger RL, Travers JB. Epidermal peroxisome proliferator-activated receptor gamma as a target for ultraviolet B radiation. The Journal of biological chemistry. 2005;280:73–9. doi: 10.1074/jbc.M409795200. [DOI] [PubMed] [Google Scholar]
- 105.Zhang Q, Seltmann H, Zouboulis CC, Konger RL. Involvement of PPARgamma in oxidative stress-mediated prostaglandin E(2) production in SZ95 human sebaceous gland cells. The Journal of investigative dermatology. 2006;126:42–8. doi: 10.1038/sj.jid.5700028. [DOI] [PubMed] [Google Scholar]
- 106.Fluhr JW, Crumrine D, Mao-Qiang M, Moskowitz DG, Elias PM, Feingold KR. Topical liver x receptor activators accelerate postnatal acidification of stratum corneum and improve function in the neonate. The Journal of investigative dermatology. 2005;125:1206–14. doi: 10.1111/j.0022-202X.2005.23964.x. [DOI] [PubMed] [Google Scholar]
- 107.Man MQ, Choi EH, Schmuth M, Crumrine D, Uchida Y, Elias PM, Holleran WM, Feingold KR. Basis for improved permeability barrier homeostasis induced by PPAR and LXR activators: liposensors stimulate lipid synthesis, lamellar body secretion, and post-secretory lipid processing. The Journal of investigative dermatology. 2006;126:386–92. doi: 10.1038/sj.jid.5700046. [DOI] [PubMed] [Google Scholar]
- 108.Jiang YJ, Lu B, Kim P, Elias PM, Feingold KR. Regulation of ABCA1 expression in human keratinocytes and murine epidermis. Journal of lipid research. 2006;47:2248–58. doi: 10.1194/jlr.M600163-JLR200. [DOI] [PubMed] [Google Scholar]
- 109.Jiang YJ, Lu B, Kim P, Paragh G, Schmitz G, Elias PM, Feingold KR. PPAR and LXR activators regulate ABCA12 expression in human keratinocytes. The Journal of investigative dermatology. 2008;128:104–9. doi: 10.1038/sj.jid.5700944. [DOI] [PubMed] [Google Scholar]
- 110.Jiang YJ, Lu B, Tarling EJ, Kim P, Man MQ, Crumrine D, Edwards PA, Elias PM, Feingold KR. Regulation of ABCG1 expression in human keratinocytes and murine epidermis. Journal of lipid research. 2010;51:3185–95. doi: 10.1194/jlr.M006445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jiang YJ, Kim P, Lu YF, Feingold KR. PPARgamma activators stimulate aquaporin 3 expression in keratinocytes/epidermis. Experimental dermatology. 2011;20:595–9. doi: 10.1111/j.1600-0625.2011.01269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fortes C, Mastroeni S, Leffondre K, Sampogna F, Melchi F, Mazzotti E, Pasquini P, Abeni D. Relationship between smoking and the clinical severity of psoriasis. Archives of dermatology. 2005;141:1580–4. doi: 10.1001/archderm.141.12.1580. [DOI] [PubMed] [Google Scholar]
- 113.Kessides MC, Wheless L, Hoffman-Bolton J, Clipp S, Alani RM, Alberg AJ. Cigarette smoking and malignant melanoma: a case-control study. Journal of the American Academy of Dermatology. 2011;64:84–90. doi: 10.1016/j.jaad.2010.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sticozzi C, Pecorelli A, Belmonte G, Valacchi G. Cigarette Smoke Affects ABCAl Expression via Liver X Receptor Nuclear Translocation in Human Keratinocytes. International journal of molecular sciences. 2010;11:3375–86. doi: 10.3390/ijms11093375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chang KC, Shen Q, Oh IG, Jelinsky SA, Jenkins SF, Wang W, Wang Y, LaCava M, Yudt MR, Thompson CC, Freedman LP, Chung JH, Nagpal S. Liver X receptor is a therapeutic target for photoaging and chronological skin aging. Mol Endocrinol. 2008;22:2407–19. doi: 10.1210/me.2008-0232. [DOI] [PubMed] [Google Scholar]
- 116.Fowler AJ, Sheu MY, Schmuth M, Kao J, Fluhr JW, Rhein L, Collins JL, Willson TM, Mangelsdorf DJ, Elias PM, Feingold KR. Liver X receptor activators display anti-inflammatory activity in irritant and allergic contact dermatitis models: liver-X-receptor-specific inhibition of inflammation and primary cytokine production. The Journal of investigative dermatology. 2003;120:246–55. doi: 10.1046/j.1523-1747.2003.12033.x. [DOI] [PubMed] [Google Scholar]
- 117.Hatano Y, Man MQ, Uchida Y, Crumrine D, Mauro TM, Feingold KR, Elias PM, Holleran WM. Murine atopic dermatitis responds to peroxisome proliferator-activated receptors alpha and beta/delta (but not gamma) and liver X receptor activators. The Journal of allergy and clinical immunology. 2010;125:160–9. e1–5. doi: 10.1016/j.jaci.2009.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gupta DS, Kaul D, Kanwar AJ, Parsad D. Psoriasis: crucial role of LXR-alpha RNomics. Genes and immunity. 2010;11:37–44. doi: 10.1038/gene.2009.63. [DOI] [PubMed] [Google Scholar]
- 119.Hong I, Lee MH, Na TY, Zouboulis CC, Lee MO. LXRalpha enhances lipid synthesis in SZ95 sebocytes. The Journal of investigative dermatology. 2008;128:1266–72. doi: 10.1038/sj.jid.5701134. [DOI] [PubMed] [Google Scholar]
- 120.Bookout AL, Jeong Y, Downes M, Yu RT, Evans RM, Mangelsdorf DJ. Anatomical profiling of nuclear receptor expression reveals a hierarchical transcriptional network. Cell. 2006;126:789–99. doi: 10.1016/j.cell.2006.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Viennois E, Mouzat K, Dufour J, Morel L, Lobaccaro JM, Baron S. Selective liver X receptor modulators (SLiMs): what use in human health? Molecular and cellular endocrinology. 2012;351:129–41. doi: 10.1016/j.mce.2011.08.036. [DOI] [PubMed] [Google Scholar]
- 122.Diepgen TL, Mahler V. The epidemiology of skin cancer. The British journal of dermatology. 2002;146(Suppl 61):1–6. doi: 10.1046/j.1365-2133.146.s61.2.x. [DOI] [PubMed] [Google Scholar]
- 123.Wong CS, Strange RC, Lear JT. Basal cell carcinoma. BMJ. 2003;327:794–8. doi: 10.1136/bmj.327.7418.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sekulic A, Migden MR, Oro AE, Dirix L, Lewis KD, Hainsworth JD, Solomon JA, Yoo S, Arron ST, Friedlander PA, Marmur E, Rudin CM, Chang AL, Low JA, Mackey HM, Yauch RL, Graham RA, Reddy JC, Hauschild A. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. The New England journal of medicine. 2012;366:2171–9. doi: 10.1056/NEJMoa1113713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Johnson TM, Rowe DE, Nelson BR, Swanson NA. Squamous cell carcinoma of the skin (excluding lip and oral mucosa) Journal of the American Academy of Dermatology. 1992;26:467–84. doi: 10.1016/0190-9622(92)70074-p. [DOI] [PubMed] [Google Scholar]
- 126.Rowe DE, Carroll RJ, Day CL., Jr Prognostic factors for local recurrence, metastasis, and survival rates in squamous cell carcinoma of the skin, ear, and lip. Implications for treatment modality selection. Journal of the American Academy of Dermatology. 1992;26:976–90. doi: 10.1016/0190-9622(92)70144-5. [DOI] [PubMed] [Google Scholar]
- 127.Love WE, Bernhard JD, Bordeaux JS. Topical imiquimod or fluorouracil therapy for basal and squamous cell carcinoma: a systematic review. Archives of dermatology. 2009;145:1431–8. doi: 10.1001/archdermatol.2009.291. [DOI] [PubMed] [Google Scholar]
- 128.Segre JA, Bauer C, Fuchs E. Klf4 is a transcription factor required for establishing the barrier function of the skin. Nature genetics. 1999;22:356–60. doi: 10.1038/11926. [DOI] [PubMed] [Google Scholar]
- 129.Jiang W, Deng W, Bailey SK, Nail CD, Frost AR, Brouillette WJ, Muccio DD, Grubbs CJ, Ruppert JM, Lobo-Ruppert SM. Prevention of KLF4-mediated tumor initiation and malignant transformation by UAB30 rexinoid. Cancer biology & therapy. 2009;8:289–98. doi: 10.4161/cbt.8.3.7486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Indra AK, Castaneda E, Antal MC, Jiang M, Messaddeq N, Meng X, Loehr CV, Gariglio P, Kato S, Wahli W, Desvergne B, Metzger D, Chambon P. Malignant transformation of DMBA/TPA-induced papillomas and nevi in the skin of mice selectively lacking retinoid-X-receptor alpha in epidermal keratinocytes. The Journal of investigative dermatology. 2007;127:1250–60. doi: 10.1038/sj.jid.5700672. [DOI] [PubMed] [Google Scholar]
- 131.Wang Z, Boudjelal M, Kang S, Voorhees JJ, Fisher GJ. Ultraviolet irradiation of human skin causes functional vitamin A deficiency, preventable by all-trans retinoic acid pre-treatment. Nature medicine. 1999;5:418–22. doi: 10.1038/7417. [DOI] [PubMed] [Google Scholar]
- 132.Boudjelal M, Wang Z, Voorhees JJ, Fisher GJ. Ubiquitin/proteasome pathway regulates levels of retinoic acid receptor gamma and retinoid X receptor alpha in human keratinocytes. Cancer research. 2000;60:2247–52. [PubMed] [Google Scholar]
- 133.Andersson E, Rosdahl I, Torma H, Vahlquist A. Differential effects of UV irradiation on nuclear retinoid receptor levels in cultured keratinocytes and melanocytes. Experimental dermatology. 2003;12:563–71. doi: 10.1034/j.1600-0625.2003.00090.x. [DOI] [PubMed] [Google Scholar]
- 134.Kumar R, Shoemaker AR, Verma AK. Retinoic acid nuclear receptors and tumor promotion: decreased expression of retinoic acid nuclear receptors by the tumor promoter 12-O-tetradecanoylphorbol-13-acetate. Carcinogenesis. 1994;15:701–5. doi: 10.1093/carcin/15.4.701. [DOI] [PubMed] [Google Scholar]
- 135.Darwiche N, Celli G, Tennenbaum T, Glick AB, Yuspa SH, De Luca LM. Mouse skin tumor progression results in differential expression of retinoic acid and retinoid X receptors. Cancer research. 1995;55:2774–82. [PubMed] [Google Scholar]
- 136.Xu XC, Wong WY, Goldberg L, Baer SC, Wolf JE, Ramsdell WM, Alberts DS, Lippman SM, Lotan R. Progressive decreases in nuclear retinoid receptors during skin squamous carcinogenesis. Cancer research. 2001;61:4306–10. [PubMed] [Google Scholar]
- 137.Rudd CJ, Mansbridge JN, Suing KD, Dawson MI. Correlation of the ability of retinoids to inhibit promoter-induced anchorage-independent growth of JB6 mouse epidermal cells with their activation of retinoic acid receptor gamma. Cancer letters. 1993;73:41–9. doi: 10.1016/0304-3835(93)90186-d. [DOI] [PubMed] [Google Scholar]
- 138.Chen CF, Goyette P, Lohnes D. RARgamma acts as a tumor suppressor in mouse keratinocytes. Oncogene. 2004;23:5350–9. doi: 10.1038/sj.onc.1207682. [DOI] [PubMed] [Google Scholar]
- 139.Tennenbaum T, Lowry D, Darwiche N, Morgan DL, Gartsbein M, Hansen L, De Luca LM, Hennings H, Yuspa SH. Topical retinoic acid reduces skin papilloma formation but resistant papillomas are at high risk for malignant conversion. Cancer research. 1998;58:1435–43. [PubMed] [Google Scholar]
- 140.Nagpal S, Thacher SM, Patel S, Friant S, Malhotra M, Shafer J, Krasinski G, Asano AT, Teng M, Duvic M, Chandraratna RA. Negative regulation of two hyperproliferative keratinocyte differentiation markers by a retinoic acid receptor-specific retinoid: insight into the mechanism of retinoid action in psoriasis. Cell growth & differentiation : the molecular biology journal of the American Association for Cancer Research. 1996;7:1783–91. [PubMed] [Google Scholar]
- 141.Orlandi A, Bianchi L, Costanzo A, Campione E, Giusto Spagnoli L, Chimenti S. Evidence of increased apoptosis and reduced proliferation in basal cell carcinomas treated with tazarotene. The Journal of investigative dermatology. 2004;122:1037–41. doi: 10.1111/j.0022-202X.2004.22414.x. [DOI] [PubMed] [Google Scholar]
- 142.So PL, Fujimoto MA, Epstein EH., Jr Pharmacologic retinoid signaling and physiologic retinoic acid receptor signaling inhibit basal cell carcinoma tumorigenesis. Molecular cancer therapeutics. 2008;7:1275–84. doi: 10.1158/1535-7163.MCT-07-2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Han J, Colditz GA, Hunter DJ. Polymorphisms in the MTHFR and VDR genes and skin cancer risk. Carcinogenesis. 2007;28:390–7. doi: 10.1093/carcin/bgl156. [DOI] [PubMed] [Google Scholar]
- 144.Carless MA, Kraska T, Lintell N, Neale RE, Green AC, Griffiths LR. Polymorphisms of the VDR gene are associated with presence of solar keratoses on the skin. The British journal of dermatology. 2008;159:804–10. doi: 10.1111/j.1365-2133.2008.08745.x. [DOI] [PubMed] [Google Scholar]
- 145.Raimondi S, Johansson H, Maisonneuve P, Gandini S. Review and meta-analysis on vitamin D receptor polymorphisms and cancer risk. Carcinogenesis. 2009;30:1170–80. doi: 10.1093/carcin/bgp103. [DOI] [PubMed] [Google Scholar]
- 146.Lesiak A, Norval M, Wodz-Naskiewicz K, Pawliczak R, Rogowski-Tylman M, Sysa-Jedrzejowska A, Sobjanek M, Wlodarkiewicz A, Narbutt J. An enhanced risk of basal cell carcinoma is associated with particular polymorphisms in the VDR and MTHFR genes. Experimental dermatology. 2011;20:800–4. doi: 10.1111/j.1600-0625.2011.01328.x. [DOI] [PubMed] [Google Scholar]
- 147.Kostner K, Denzer N, Koreng M, Reichrath S, Graber S, Klein R, Tilgen W, Vogt T, Reichrath J. Association of genetic variants of the vitamin D receptor (VDR) with cutaneous squamous cell carcinomas (SCC) and basal cell carcinomas (BCC): a pilot study in a German population. Anticancer research. 2012;32:327–33. [PubMed] [Google Scholar]
- 148.Aydingoz IE, Bingul I, Dogru-Abbasoglu S, Vural P, Uysal M. Analysis of Vitamin D Receptor Gene Polymorphisms in Vitiligo. Dermatology. 2012 doi: 10.1159/000339340. [DOI] [PubMed] [Google Scholar]
- 149.Ellison TI, Smith MK, Gilliam AC, MacDonald PN. Inactivation of the vitamin D receptor enhances susceptibility of murine skin to UV-induced tumorigenesis. The Journal of investigative dermatology. 2008;128:2508–17. doi: 10.1038/jid.2008.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Teichert AE, Elalieh H, Elias PM, Welsh J, Bikle DD. Overexpression of hedgehog signaling is associated with epidermal tumor formation in vitamin D receptor-null mice. The Journal of investigative dermatology. 2011;131:2289–97. doi: 10.1038/jid.2011.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kim DJ, Akiyama TE, Harman FS, Burns AM, Shan W, Ward JM, Kennett MJ, Gonzalez FJ, Peters JM. Peroxisome proliferator-activated receptor beta (delta)-dependent regulation of ubiquitin C expression contributes to attenuation of skin carcinogenesis. The Journal of biological chemistry. 2004;279:23719–27. doi: 10.1074/jbc.M312063200. [DOI] [PubMed] [Google Scholar]
- 152.Bility MT, Devlin-Durante MK, Blazanin N, Glick AB, Ward JM, Kang BH, Kennett MJ, Gonzalez FJ, Peters JM. Ligand activation of peroxisome proliferator-activated receptor beta/delta (PPAR beta/delta) inhibits chemically induced skin tumorigenesis. Carcinogenesis. 2008;29:2406–14. doi: 10.1093/carcin/bgn219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhu B, Bai R, Kennett MJ, Kang BH, Gonzalez FJ, Peters JM. Chemoprevention of chemically induced skin tumorigenesis by ligand activation of peroxisome proliferator-activated receptor-beta/delta and inhibition of cyclooxygenase 2. Molecular cancer therapeutics. 2010;9:3267–77. doi: 10.1158/1535-7163.MCT-10-0820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Martinez-Iglesias O, Garcia-Silva S, Tenbaum SP, Regadera J, Larcher F, Paramio JM, Vennstrom B, Aranda A. Thyroid hormone receptor beta1 acts as a potent suppressor of tumor invasiveness and metastasis. Cancer research. 2009;69:501–9. doi: 10.1158/0008-5472.CAN-08-2198. [DOI] [PubMed] [Google Scholar]
- 155.Contreras-Jurado C, Garcia-Serrano L, Gomez-Ferreria M, Costa C, Paramio JM, Aranda A. The thyroid hormone receptors as modulators of skin proliferation and inflammation. The Journal of biological chemistry. 2011;286:24079–88. doi: 10.1074/jbc.M111.218487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Garcia-Serrano L, Gomez-Ferreria MA, Contreras-Jurado C, Segrelles C, Paramio JM, Aranda A. The thyroid hormone receptors modulate the skin response to retinoids. PloS one. 2011;6:e23825. doi: 10.1371/journal.pone.0023825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Chin L, Garraway LA, Fisher DE. Malignant melanoma: genetics and therapeutics in the genomic era. Genes & development. 2006;20:2149–82. doi: 10.1101/gad.1437206. [DOI] [PubMed] [Google Scholar]
- 158.Hodis E, Watson IR, Kryukov GV, Arold ST, Imielinski M, Theurillat JP, Nickerson E, Auclair D, Li L, Place C, Dicara D, Ramos AH, Lawrence MS, Cibulskis K, Sivachenko A, Voet D, Saksena G, Stransky N, Onofrio RC, Winckler W, Ardlie K, Wagle N, Wargo J, Chong K, Morton DL, Stemke-Hale K, Chen G, Noble M, Meyerson M, Ladbury JE, Davies MA, Gershenwald JE, Wagner SN, Hoon DS, Schadendorf D, Lander ES, Gabriel SB, Getz G, Garraway LA, Chin L. A landscape of driver mutations in melanoma. Cell. 2012;150:251–63. doi: 10.1016/j.cell.2012.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Flaherty KT, Puzanov I, Kim KB, Ribas A, McArthur GA, Sosman JA, O’Dwyer PJ, Lee RJ, Grippo JF, Nolop K, Chapman PB. Inhibition of mutated, activated BRAF in metastatic melanoma. The New England journal of medicine. 2010;363:809–19. doi: 10.1056/NEJMoa1002011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbe C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ. Improved survival with ipilimumab in patients with metastatic melanoma. The New England journal of medicine. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Desai DS, Niles RM. Expression and regulation of retinoid X receptors in B16 melanoma cells. Journal of cellular physiology. 1995;165:349–57. doi: 10.1002/jcp.1041650216. [DOI] [PubMed] [Google Scholar]
- 162.Spanjaard RA, Sugawara A, Ikeda M, Chin WW. Evidence that retinoid X receptors mediate retinoid-dependent transcriptional activation of the retinoic acid receptor beta gene in S91 melanoma cells. The Journal of biological chemistry. 1995;270:17429–36. doi: 10.1074/jbc.270.29.17429. [DOI] [PubMed] [Google Scholar]
- 163.Chakravarti N, Lotan R, Diwan AH, Warneke CL, Johnson MM, Prieto VG. Decreased expression of retinoid receptors in melanoma: entailment in tumorigenesis and prognosis. Clinical cancer research : an official journal of the American Association for Cancer Research. 2007;13:4817–24. doi: 10.1158/1078-0432.CCR-06-3026. [DOI] [PubMed] [Google Scholar]
- 164.Papi A, Rocchi P, Ferreri AM, Guerra F, Orlandi M. Enhanced effects of PPARgamma ligands and RXR selective retinoids in combination to inhibit migration and invasiveness in cancer cells. Oncology reports. 2009;21:1083–9. doi: 10.3892/or_00000327. [DOI] [PubMed] [Google Scholar]
- 165.Klopper JP, Sharma V, Berenz A, Hays WR, Loi M, Pugazhenthi U, Said S, Haugen BR. Retinoid and thiazolidinedione therapies in melanoma: an analysis of differential response based on nuclear hormone receptor expression. Molecular cancer. 2009;8:16. doi: 10.1186/1476-4598-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Klopper JP, Sharma V, Bissonnette R, Haugen BR. Combination PPARgamma and RXR Agonist Treatment in Melanoma Cells: Functional Importance of S100A2. PPAR research. 2010;2010:729876. doi: 10.1155/2010/729876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wang Z, Coleman DJ, Bajaj G, Liang X, Ganguli-Indra G, Indra AK. RXRalpha ablation in epidermal keratinocytes enhances UVR-induced DNA damage, apoptosis, and proliferation of keratinocytes and melanocytes. The Journal of investigative dermatology. 2011;131:177–87. doi: 10.1038/jid.2010.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Hyter S, Bajaj G, Liang X, Barbacid M, Ganguli-Indra G, Indra AK. Loss of nuclear receptor RXRalpha in epidermal keratinocytes promotes the formation of Cdk4-activated invasive melanomas. Pigment cell & melanoma research. 2010;23:635–48. doi: 10.1111/j.1755-148X.2010.00732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Schadendorf D, Worm M, Jurgovsky K, Dippel E, Michel S, Charpentier B, Bernardon J, Reichert U, Czarnetzki B. Retinoic Acid receptor-gamma-selective retinoids exert antiproliferative effects on human-melanoma cell-growth in-vitro. International journal of oncology. 1994;5:1325–31. doi: 10.3892/ijo.5.6.1325. [DOI] [PubMed] [Google Scholar]
- 170.Zhang H, Satyamoorthy K, Herlyn M, Rosdahl I. All-trans retinoic acid (atRA) differentially induces apoptosis in matched primary and metastatic melanoma cells -- a speculation on damage effect of atRA via mitochondrial dysfunction and cell cycle redistribution. Carcinogenesis. 2003;24:185–91. doi: 10.1093/carcin/24.2.185. [DOI] [PubMed] [Google Scholar]
- 171.Pan M, Geng S, Xiao S, Ren J, Liu Y, Li X, Li Z, Peng Z. Apoptosis induced by synthetic retinoic acid CD437 on human melanoma A375 cells involves RIG-I pathway. Archives of dermatological research. 2009;301:15–20. doi: 10.1007/s00403-008-0902-x. [DOI] [PubMed] [Google Scholar]
- 172.Desai SH, Boskovic G, Eastham L, Dawson M, Niles RM. Effect of receptor-selective retinoids on growth and differentiation pathways in mouse melanoma cells. Biochemical pharmacology. 2000;59:1265–75. doi: 10.1016/s0006-2952(00)00269-0. [DOI] [PubMed] [Google Scholar]
- 173.Boskovic G, Desai D, Niles RM. Regulation of retinoic acid receptor alpha by protein kinase C in B16 mouse melanoma cells. The Journal of biological chemistry. 2002;277:26113–9. doi: 10.1074/jbc.M201185200. [DOI] [PubMed] [Google Scholar]
- 174.Huang Y, Boskovic G, Niles RM. Retinoic acid-induced AP-1 transcriptional activity regulates B16 mouse melanoma growth inhibition and differentiation. Journal of cellular physiology. 2003;194:162–70. doi: 10.1002/jcp.10199. [DOI] [PubMed] [Google Scholar]
- 175.Boehm N, Samama B, Cribier B, Rochette-Egly C. Retinoic-acid receptor beta expression in melanocytes. European journal of dermatology : EJD. 2004;14:19–23. [PubMed] [Google Scholar]
- 176.Fan J, Eastham L, Varney ME, Hall A, Adkins NL, Chetel L, Sollars VE, Georgel P, Niles RM. Silencing and re-expression of retinoic acid receptor beta2 in human melanoma. Pigment cell & melanoma research. 2010;23:419–29. doi: 10.1111/j.1755-148X.2010.00702.x. [DOI] [PubMed] [Google Scholar]
- 177.Kato Y, Salumbides BC, Wang XF, Qian DZ, Williams S, Wei Y, Sanni TB, Atadja P, Pili R. Antitumor effect of the histone deacetylase inhibitor LAQ824 in combination with 13-cis-retinoic acid in human malignant melanoma. Molecular cancer therapeutics. 2007;6:70–81. doi: 10.1158/1535-7163.MCT-06-0125. [DOI] [PubMed] [Google Scholar]
- 178.Demary K, Wong L, Liou JS, Faller DV, Spanjaard RA. Redox control of retinoic acid receptor activity: a novel mechanism for retinoic acid resistance in melanoma cells. Endocrinology. 2001;142:2600–5. doi: 10.1210/endo.142.6.8201. [DOI] [PubMed] [Google Scholar]
- 179.Szabo A, Osman RM, Bacskai I, Kumar BV, Agod Z, Lanyi A, Gogolak P, Rajnavolgyi E. Temporally designed treatment of melanoma cells by ATRA and polyI: C results in enhanced chemokine and IFNbeta secretion controlled differently by TLR3 and MDA5. Melanoma research. 2012 doi: 10.1097/CMR.0b013e328357076c. [DOI] [PubMed] [Google Scholar]
- 180.Hendrix MJ, Wood WR, Seftor EA, Lotan D, Nakajima M, Misiorowski RL, Seftor RE, Stetler-Stevenson WG, Bevacqua SJ, Liotta LA, et al. Retinoic acid inhibition of human melanoma cell invasion through a reconstituted basement membrane and its relation to decreases in the expression of proteolytic enzymes and motility factor receptor. Cancer research. 1990;50:4121–30. [PubMed] [Google Scholar]
- 181.Lee JH, Kishikawa M, Kumazoe M, Yamada K, Tachibana H. Vitamin A enhances antitumor effect of a green tea polyphenol on melanoma by upregulating the polyphenol sensing molecule 67-kDa laminin receptor. PloS one. 2010;5:e11051. doi: 10.1371/journal.pone.0011051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Zhao X, Graves C, Ames SJ, Fisher DE, Spanjaard RA. Mechanism of regulation and suppression of melanoma invasiveness by novel retinoic acid receptor-gamma target gene carbohydrate sulfotransferase 10. Cancer research. 2009;69:5218–25. doi: 10.1158/0008-5472.CAN-09-0705. [DOI] [PubMed] [Google Scholar]
- 183.Birlea SA, Costin GE, Norris DA. Cellular and molecular mechanisms involved in the action of vitamin D analogs targeting vitiligo depigmentation. Current drug targets. 2008;9:345–59. doi: 10.2174/138945008783954970. [DOI] [PubMed] [Google Scholar]
- 184.Slominski AT, Kim TK, Janjetovic Z, Tuckey RC, Bieniek R, Yue J, Li W, Chen J, Nguyen MN, Tang EK, Miller D, Chen TC, Holick M. 20-Hydroxyvitamin D2 is a noncalcemic analog of vitamin D with potent antiproliferative and prodifferentiation activities in normal and malignant cells. American journal of physiology Cell physiology. 2011;300:C526–41. doi: 10.1152/ajpcell.00203.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Brozyna AA, Jozwicki W, Janjetovic Z, Slominski AT. Expression of vitamin D receptor decreases during progression of pigmented skin lesions. Human pathology. 2011;42:618–31. doi: 10.1016/j.humpath.2010.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Newton-Bishop JA, Beswick S, Randerson-Moor J, Chang YM, Affleck P, Elliott F, Chan M, Leake S, Karpavicius B, Haynes S, Kukalizch K, Whitaker L, Jackson S, Gerry E, Nolan C, Bertram C, Marsden J, Elder DE, Barrett JH, Bishop DT. Serum 25-hydroxyvitamin D3 levels are associated with breslow thickness at presentation and survival from melanoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2009;27:5439–44. doi: 10.1200/JCO.2009.22.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Denzer N, Vogt T, Reichrath J. Vitamin D receptor (VDR) polymorphisms and skin cancer: A systematic review. Dermato-endocrinology. 2011;3:205–10. doi: 10.4161/derm.3.3.16519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Mandelcorn-Monson R, Marrett L, Kricker A, Armstrong BK, Orlow I, Goumas C, Paine S, Rosso S, Thomas N, Millikan RC, Pole JD, Cotignola J, Rosen C, Kanetsky PA, Lee-Taylor J, Begg CB, Berwick M. Sun exposure, vitamin D receptor polymorphisms FokI and BsmI and risk of multiple primary melanoma. Cancer epidemiology. 2011;35:e105–10. doi: 10.1016/j.canep.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Orlow I, Roy P, Reiner AS, Yoo S, Patel H, Paine S, Armstrong BK, Kricker A, Marrett LD, Millikan RC, Thomas NE, Gruber SB, Anton-Culver H, Rosso S, Gallagher RP, Dwyer T, Kanetsky PA, Busam K, From L, Begg CB, Berwick M. Vitamin D receptor polymorphisms in patients with cutaneous melanoma. International journal of cancer Journal international du cancer. 2012;130:405–18. doi: 10.1002/ijc.26023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Essa S, Denzer N, Mahlknecht U, Klein R, Collnot EM, Tilgen W, Reichrath J. VDR microRNA expression and epigenetic silencing of vitamin D signaling in melanoma cells. The Journal of steroid biochemistry and molecular biology. 2010;121:110–3. doi: 10.1016/j.jsbmb.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 191.Essa S, Reichrath S, Mahlknecht U, Montenarh M, Vogt T, Reichrath J. Signature of VDR miRNAs and epigenetic modulation of vitamin D signaling in melanoma cell lines. Anticancer research. 2012;32:383–9. [PubMed] [Google Scholar]
- 192.Mossner R, Meyer P, Jankowski F, Konig IR, Kruger U, Kammerer S, Westphal G, Boettger MB, Berking C, Schmitt C, Brockmoller J, Ziegler A, Stapelmann H, Kaiser R, Volkenandt M, Reich K. Variations in the peroxisome proliferator-activated receptor-gamma gene and melanoma risk. Cancer letters. 2007;246:218–23. doi: 10.1016/j.canlet.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 193.Maresca V, Flori E, Camera E, Bellei B, Aspite N, Ludovici M, Catricala C, Cardinali G, Picardo M. alpha-Melanocyte Stimulating Hormone/Peroxisome Proliferator Activated Receptor-gamma: a new connection in B16-F10 melanoma cells. Pigment cell & melanoma research. 2012 doi: 10.1111/j.1755-148X.2012.01042.x. [DOI] [PubMed] [Google Scholar]
- 194.Grabacka M, Placha W, Urbanska K, Laidler P, Plonka PM, Reiss K. PPAR gamma regulates MITF and beta-catenin expression and promotes a differentiated phenotype in mouse melanoma S91. Pigment cell & melanoma research. 2008;21:388–96. doi: 10.1111/j.1755-148X.2008.00460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Liu Y, Meng Y, Li H, Li J, Fu J, Liu Y, Chen XG. Growth inhibition and differentiation induced by peroxisome proliferator activated receptor gamma ligand rosiglitazone in human melanoma cell line A375. Med Oncol. 2006;23:393–402. doi: 10.1385/mo:23:3:393. [DOI] [PubMed] [Google Scholar]
- 196.Smith AG, Beaumont KA, Smit DJ, Thurber AE, Cook AL, Boyle GM, Parsons PG, Sturm RA, Muscat GE. PPARgamma agonists attenuate proliferation and modulate Wnt/beta-catenin signalling in melanoma cells. The international journal of biochemistry & cell biology. 2009;41:844–52. doi: 10.1016/j.biocel.2008.08.037. [DOI] [PubMed] [Google Scholar]
- 197.Lee C, Ramirez JA, Guitart J, Diaz LK. Expression of cyclooxygenase-2 and peroxisome proliferator-activated receptor gamma during malignant melanoma progression. Journal of cutaneous pathology. 2008;35:989–94. doi: 10.1111/j.1600-0560.2007.00939.x. [DOI] [PubMed] [Google Scholar]
- 198.Meyer S, Vogt T, Landthaler M, Berand A, Reichle A, Bataille F, Marx AH, Menz A, Hartmann A, Kunz-Schughart LA, Wild PJ. Cyclooxygenase 2 (COX2) and Peroxisome Proliferator-Activated Receptor Gamma (PPARG) Are Stage-Dependent Prognostic Markers of Malignant Melanoma. PPAR research. 2009;2009:848645. doi: 10.1155/2010/848645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Russell LE, Harrison WJ, Bahta AW, Zouboulis CC, Burrin JM, Philpott MP. Characterization of liver X receptor expression and function in human skin and the pilosebaceous unit. Experimental dermatology. 2007;16:844–52. doi: 10.1111/j.1600-0625.2007.00612.x. [DOI] [PubMed] [Google Scholar]
- 200.Chen M, Beaven S, Tontonoz P. Identification and characterization of two alternatively spliced transcript variants of human liver X receptor alpha. Journal of lipid research. 2005;46:2570–9. doi: 10.1194/jlr.M500157-JLR200. [DOI] [PubMed] [Google Scholar]
- 201.Kumar R, Parsad D, Kaul D, Kanwar A. Liver X receptor expression in human melanocytes, does it have a role in the pathogenesis of vitiligo? Experimental dermatology. 2010;19:62–4. doi: 10.1111/j.1600-0625.2009.00940.x. [DOI] [PubMed] [Google Scholar]
- 202.Villablanca EJ, Raccosta L, Zhou D, Fontana R, Maggioni D, Negro A, Sanvito F, Ponzoni M, Valentinis B, Bregni M, Prinetti A, Steffensen KR, Sonnino S, Gustafsson JA, Doglioni C, Bordignon C, Traversari C, Russo V. Tumor-mediated liver X receptor-alpha activation inhibits CC chemokine receptor-7 expression on dendritic cells and dampens antitumor responses. Nature medicine. 2010;16:98–105. doi: 10.1038/nm.2074. [DOI] [PubMed] [Google Scholar]
- 203.Sisley K, Curtis D, Rennie IG, Rees RC. Loss of heterozygosity of the thyroid hormone receptor B in posterior uveal melanoma. Melanoma research. 1993;3:457–61. doi: 10.1097/00008390-199311000-00009. [DOI] [PubMed] [Google Scholar]



