ABSTRACT
Purpose: To explore the feasibility and efficacy of using a power training exercise programme for the quadriceps femoris (QF) in elderly women with knee osteoarthritis (OA). Method: A one-group quasi-experimental design with pre- and post-intervention measurements was conducted on 17 older adult women with knee OA pain. A bilateral QF exercise programme (24 sessions over 8 weeks) consisting of 3 series of 10 repetitions of flexion-extension as fast as possible at 40% of their one-repetition maximum (1RM) was performed in an outpatient physiotherapy clinic. The primary outcome measures were the knee function and associated problems using the Knee injury Osteoarthritis Outcome Score (KOOS) questionnaire and the weekly mean pain score from pain diaries using a visual analogue scale (VAS). QF strength (QFS), power (QFP) and work (QFW) were measured with an isokinetic dynamometer as secondary outcomes. Results: Significant improvements (p<0.05) were noted on the five categories of the KOOS. Significant decrease (p<0.01) was noted in pain intensity on VAS. QFP and QFW increased significantly on both sides (p<0.05). Exercise compliance was 99.5% for 16 participants. Conclusions: A short power-training exercise programme is a feasible training modality for patients with knee OA, and significant functional improvements can be achieved. Further studies must be conducted to better understand the effects of the programme parameters and the generalizability of the findings.
Key Words: exercise therapy, muscle strength, osteoarthritis, quadriceps muscle, resistance training
RÉSUMÉ
Objectif : Analyser la faisabilité d'utiliser un programme d'entrainement en puissance des quadriceps cruraux (QC) et son efficacité chez des personnés âgées atteintes d'arthrose. Méthodologie : Devis quasi expérimental avec mesures pré et post intervention sur un groupe de 17 femmes de plus de 65 ans avec douleur au genou causée par l'arthrose. Programme individuel d'exercices bilatéraux pour les QC (24 séances en 8 semaines) comprenant 3 séries de 10 répétitions de flexion-extension à 40 % de la force maximum à une répétition (1RM) exécutées a vitesse maximale et réalisé sous supervision en clinique externe de physiothérapie. Les principales mesures de résultat étaient la fonction du genou et les problèmes connexes, à l'aide du questionnaire KOOS (Knee injury Osteoarthritis Outcome Score) et la douleur moyenne hebdomadaire calculée à partir des valeurs de douleur sur une échelle visuelle analogue (EVA) consignées dans un journal de la douleur. La force des QC (FQC), la puissance (PQC) et le travail musculaire (TQC) ont été mesurés à l'aide d'un dynamomètre isocinétique et consignés comme résultats secondaires. Résultats : Des améliorations appréciables (p<0,05) ont été observées dans cinq catégories du KOOS. Une diminution considérable (p<0,01) a été notée dans l'intensité de la douleur à l'EVA. La puissance des QC et le travail musculaire des QC se sont considérablement accrus des deux côtés (p<0,05). Le programme d'exercices a été observé par 99,5 % des 16 participantes. Conclusions : Un programme court d'exercice en puissance est une modalité d'entrainement envisageable pour les patients avec arthrose du genou et permet des améliorations fonctionnelles appréciables. D'autres études devront être réalisées afin de mieux comprendre les effets des paramètres du programme et la généralisation des conclusions.
Mots clés : arthrose, entraînement en résistance, force musculaire, muscles quadriceps, thérapie par l'exercice
Knee osteoarthritis (OA) affects 10%–15% of adults over age 60 and can limit activity and mobility in significant ways.1 Clinical management of knee OA currently revolves around providing symptom-reducing therapies such as analgesics, exercises, intra-articular injections, and surgery.2 Results from large-scale clinical trials have demonstrated that muscle-strengthening regimens based on resistance training can lead to significant improvements in older adults3 and older adults with knee OA.4 These regimens typically use moderate- to high-resistance (50%–80% of maximal strength or one repetition maximum [1RM]) contractions, performed slowly, and target improvement in strength or the capacity to generate a force.5 In recent years, interest in high-velocity resistance training or so-called power training as a training modality for older adults has been growing in the physical rehabilitation literature.6–14 With power training, contractions are performed as fast as possible generally with lower resistance than traditional resistance training, and the goal is to improve the ability to produce force rapidly.12 Power training has been shown to be well tolerated by older adults with no disability.10
The rationale for the use of power training is based on observations showing that muscle power in older adults is a better predictor of mobility than muscle strength15–17 and that mobility activities (e.g., rising from a chair, climbing stairs, walking, and attending to domestic needs) depend more on power than on strength.18–24 From an intervention standpoint, two recent systematic reviews concluded that power training in older adults offers a slight advantage over resistance training in terms of gains in muscle characteristics (power and strength) and function. Steib and colleagues reviewed 29 trials, involving a total of 1,313 participants, that showed that while higher training intensities (60%–80% of 1RM) in resistance training are superior to lower intensities for improving maximal strength, they are not necessarily better than power training for improving functional performance among older adults.25 Tschopp and colleagues reviewed 11 trials, involving a total of 377 participants, that showed a small to medium effect on functional outcomes in favour of power training over resistance training.26 Although these results offer support for the use of power training in older adults, the effect of different training volumes and frequencies, the dose–response relationship of power training, and the impact of power training on functional outcomes in older adults are still largely undocumented.
In people with knee OA, tolerance for power training and the benefits of its use have not been explored extensively. When we performed our study, no published research had yet to examine the effect of power training in older adults with knee OA. More recently, Sayers and colleagues27 have shed some light on the topic. Using a single-blind, three-group randomized trial with 33 participants, they found that for older adults with knee OA, power training and resistance training performed 3 times per week for 12 weeks resulted in similar improvements in function. While power training improved muscle power and muscle speed to a greater extent than resistance training, the researchers did not observe significant differences in improvement in function and pain between training modalities.
As most published studies on power training in older adults have focused on people with no impairments and have used dynamometric exercise machines, our objective in this pilot study was to explore the feasibility and efficacy of a power-training exercise programme with elastic bands for the quadriceps femoris (QF) in older adults with knee OA.
Method
The study was approved by the Institutional Review Board of the Centre de Santé et de Services Sociaux Sherbrooke—Institut Universitaire de Gériatrie de Sherbrooke (CSSS-IUGS), and informed consent was obtained from all participants.
Participants
Seventeen community-dwelling women between 50 and 70 years of age with unilateral or bilateral OA knee pain were recruited through newspaper advertising. Inclusion criteria were a score ≤90 points in the 5 categories (pain; other symptoms; activities of daily living; quality of life; and function, sports, and recreational activities) of the Knee injury and Osteoarthritis Outcome Score (KOOS)28 questionnaire and radiological knee damage graded as stage 1 or stage 2 on the Kellgren–Lawrence scale.29 Exclusion criteria were acute or terminal phase illness; heart attack, unstable illness, or lower-limb fracture or amputation within 6 months before the start of the trial; participation in a regular exercise programme more than once a week; knee arthroplasty; and neuromuscular illness or intake of drugs affecting neuromuscular function.
Procedures
Interested individuals were first cleared by a physician for participation in the study. The physician then graded each participant's radiological knee damage on the Kellgren–Lawrence scale,29 and the participant completed the KOOS questionnaire to determine initial study eligibility. All eligible participants then completed a pre-intervention assessment (week 1) during which descriptive data such as body mass index (BMI) and depressive symptoms (Geriatric Depression Scale, or GDS)30 were measured. Participants' bilateral isometric and isokinetic concentric quadriceps femoris strength (QFS), power (QFP), and work (QFW) were measured using the Biodex System 3 (Biodex, Shirley, NY). Participants took part in an 8-week power training programme (weeks 2–9) during which they were asked to record in a journal their daily pain scores on a VAS and their daily analgesic intake. During week 10, participants again completed the KOOS questionnaire and their post-intervention bilateral isometric and isokinetic concentric QFS, QFP and QFW were measured with the Biodex System 3.
Power training protocol
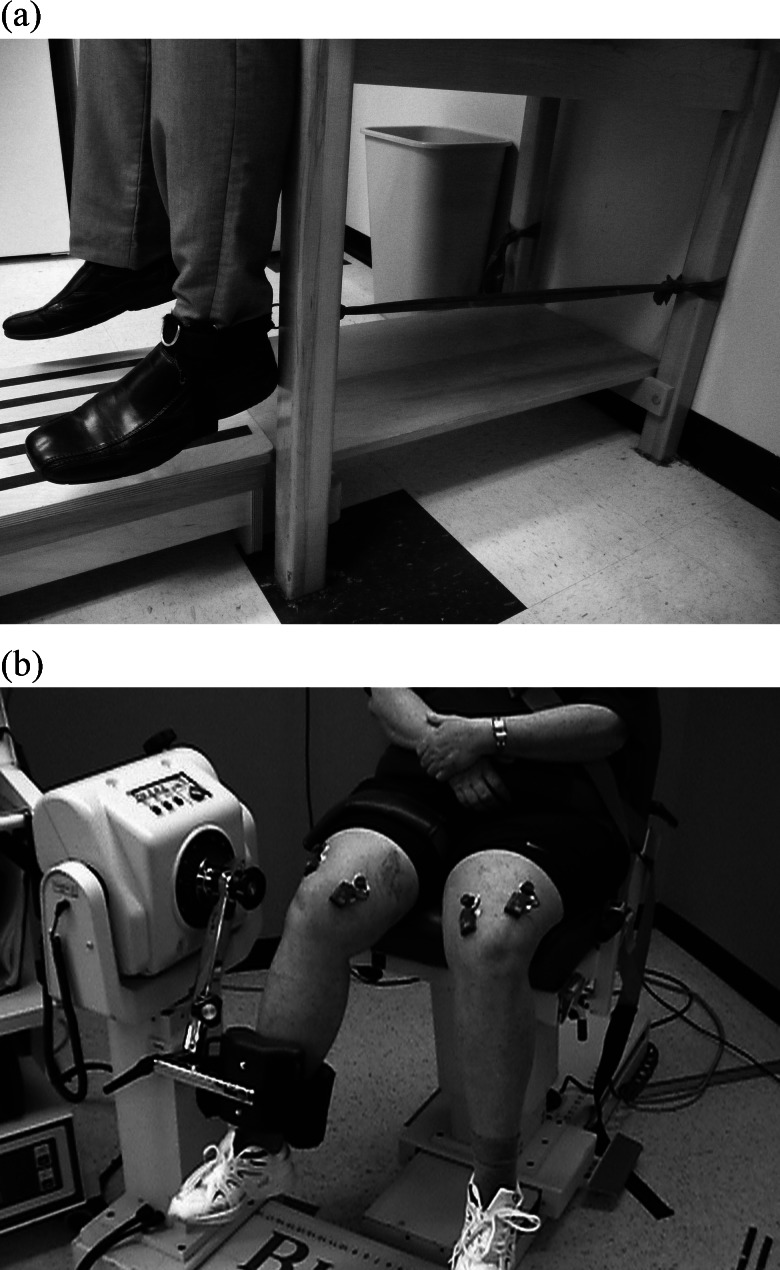
Our study explored the efficacy of an 8-week power training exercise programme (24 sessions) for the QF, using elastic bands. Previous studies13,14,27 have demonstrated that power training at 40% of 1RM significantly improved muscle performance and function compared to higher resistance (80% of 1RM) in older adults. Therefore, our bilateral QF reinforcement exercise programme consisted of 3 series of 10 repetitions with elastic resistance bands representing 40% of the average of 3 1RM measured every 2 weeks. To establish the 1RM, participants performed three 5-second maximum voluntary isometric contractions at 90° knee flexion with a Nicholas dynamometer (Lafayette Instrument, Lafayette, Indiana). During training, each participant was seated with his or her knee at 90°, and an elastic band was attached perpendicularly to a loop fixed at the ankle (Figure 1a). The colour and length of elastic band used to perform the exercises was determined using the Page table,31,32 which describes the resistance, in pounds, of the type of elastic band used and how the resistance varies according to the elongation of the bands, so that the proper elastic resistance band can be selected. Sessions lasted approximately 30 minutes, 3 times a week for 8 weeks, and were performed under direct one-on-one supervision of a licensed physical therapist.
Figure 1.
(a) Power training position with elastic bands; (b) Patient positioned on isokinetic dynamometer (Biodex 3).
Measures
Knee injury and Osteoarthritis Outcome Score (KOOS)
Participants' pre- and post-intervention self-reported knee function was evaluated using the KOOS.28 The KOOS score criterion is based on a total of 100 points for each of five categories: pain, other symptoms, activities of daily living, quality of life, and function, sports and recreational activity. A total score of 100 indicates no problems; a total score of 0 indicates important problems. The French version of the KOOS used in our study is a valid, reliable, and responsive instrument for people with knee OA.33 Ornetti and colleagues found intra-class correlation coefficients ranging from 0.755 to 0.914 for the KOOS subscale measurements, indicating good to excellent reproducibility;33 responsiveness was high, with standardized response means ranging from 0.89 to 1.93.33 An improvement ≥10 points is considered the minimal clinically important difference that can be observed.28
Quadriceps femoris strength, power, and work
Following a 5-minute warm up on a stationary bike, bilateral isometric and isokinetic concentric QFS, QFP, and QFW were measured pre- and post-intervention, using an isokinetic dynamometer (Biodex System 3) calibrated according to the manufacturer's standards. All QFS, QFP, and QFW assessments were carried out by the same person. Participants sat with the backrest at a 95° angle, safely secured and stabilized with safety belts. The lateral epicondyle of the femur was placed in line with the centre axis of the dynamometer, with a cushion stabilizing the tibia distally (see Figure 1b).
Following one practice contraction, three 10-second non-painful maximum voluntary isometric contractions at 30° knee flexion were recorded. Bilateral isokinetic evaluation of the QF was performed at an angular speed of 180°/second. Participants were instructed to perform 10 successive knee extensions at maximum effort. The return to flexion was performed at an angular speed of 300°/second. Following five practice contractions, three trials were recorded, with a 1-minute rest period between trials. QFS corresponds to the peak torque recorded during maximum voluntary isometric contractions (newton metre, Nċm). QFP corresponds to the work performed per time unit (watt, W); it is the product of the moment of force and angular speed. QFW corresponds to the integration of the surface below the curve of the moments of force (joule, J).13 The Biodex System 3 provides reliable measures of torque and velocity; the validity of the isometric torque was acceptable for research purposes, and concentric velocity measures are valid up to 300°/second.34
Body mass index (BMI) and depression
Measures of BMI and depression were taken as descriptive data. Participants' BMI was calculated from height and weight measured during the first visit. During the first week participants also completed the Geriatric Depression Scale (GDS),30 a 30-item (yes/no) self-administered questionnaire used to identify depression in older adults. A score of 0–9 is considered normal; a score of 10–19 indicates mild depression, and a score of 20–30 indicates severe depression.
Daily knee pain and medication use
We gave participants a diary in which they were asked to enter the type and amount of analgesic taken each day. The diary also included a 100 mm Visual Analog Scale (VAS) on which participants rated their daily knee pain at the time most convenient for them during the 8-week intervention. We recorded the mean weekly pain score in millimetres, computed from the VAS. Boonstra and colleagues assessed the reliability and validity of the VAS for disability in people with chronic musculoskeletal pain;35 they concluded that the reliability of the VAS is moderate to good, but its validity is questionable, since the measure is weakly correlated with other disability instruments.35
Data analysis
Because Shapiro–Wilk test results showed that the data were not normally distributed, we performed Wilcoxon signed-rank tests to assess both the direction of difference and the relative amount of difference pre- and post-intervention for QFS, QFP, QFW, and all five subcategories of the KOOS. Differences were considered statistically significant at p<0.05.
Results
A total of 17 female participants started the programme; one had to withdraw due to a fall at home at week 7. No potential participants were excluded based on the criteria specified above. Participant characteristics are summarized in Table 1. The mean age of the 16 participants who completed the programme was 60.3 (SD 6) years; mean BMI was 28.5 (SD 6) kg/m2, and mean GDS score was 5/30 (SD 4/30). No participants were found to be morbidly obese (BMI >35) or to have mild or severe depression (GDS score ≥10). At the end of the study, 382 of the 384 planned interventions had been carried out; that is, exercise compliance was 99.5%. Only two interventions with two different participants were cancelled, one because of weather conditions and the other because of a viral infection.
Table 1.
Patient Characteristics (n=16)
| Characteristic | Mean (SD), range |
|---|---|
| Age, y | 60.3 (6), 51–70 |
| Height, cm | 159.2 (4.5), 153–168 |
| Weight, kg | 72.2 (15.4), 51.1–100 |
| BMI, kg/m2 | 28.5 (6), 19.7–38.1 |
| GDS score, 30 | 5 (4), 0–10 |
BMI=body mass index; GDS=Geriatric Depression Scale.
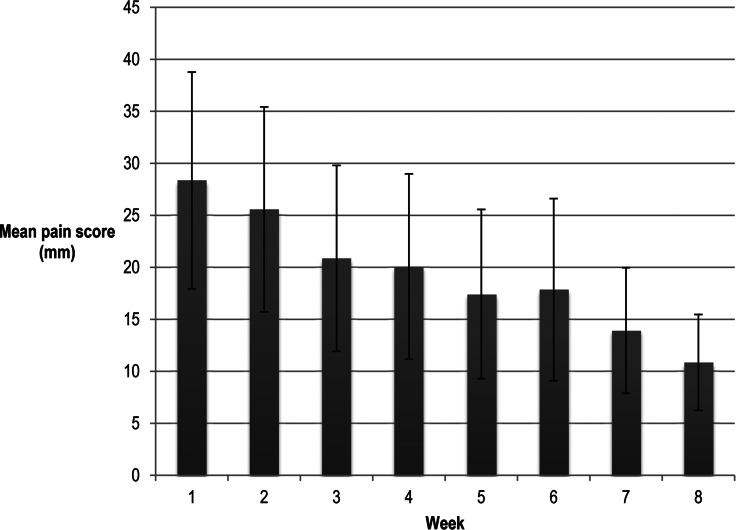
Significant improvements were noted on all five categories of the KOOS (pain, p=0.001; other symptoms, p=0.001; ADL, p=0.001; FSR, p=0.008; QOL, p=0.005; see Table 2). All these scores improved by at least 10 points, indicating that the minimal clinically important difference was observed.28 Participants' mean weekly VAS scores decreased significantly in intensity from week 1 to week 8 (p<0.01), as shown in Figure 2. Daily analgesic consumption did not vary during the experiment, as measured by qualitative evaluation of participants' medication diaries. Pre- and post-intervention bilateral isometric and isokinetic concentric quadriceps function and self-reported functional status are reported in Table 2. QFP (left, p=0.031; right, p=0.030) and QFW (left, p=0.004; right, p=0.001) increased significantly on both sides in isokinetic conditions; isometric QFS (left, p=0.12; right, p=0.59) did not change significantly during the same period.
Table 2.
Pre and Post Measurements of Quadriceps Femoris Strength, Power and Work, and Self-Reported Knee Function
| Variables | Mean (SD) measurements |
Pre/post difference (SD), %* |
p-value† | |
|---|---|---|---|---|
| Pre | Post | |||
| Muscle physiological properties | ||||
| Isometric peak torque, Nċm Left QF |
57.84 (15.11) |
63.92 (18.61) |
11.68 (27.54) |
0.12 |
| Right QF | 62.40 (15.65) | 66.27 (21.89) | 7.84 (36.38) | 0.59 |
| Maximal power, W Left QF |
171.19 (50.95) |
186.77 (50.09) |
10.76 (15.90) |
0.03 |
| Right QF | 182.49 (39.24) | 195.44 (32.78) | 8.73 (13.70) | 0.03 |
| Total work done, J Left QF |
1440.37 (439.94) |
1758.61 (546.09) |
23.96 (25.34) |
0.004 |
| Right QF | 1547.57 (319.19) | 1961.45 (518.62) | 29.39 (38.57) | 0.001 |
| KOOS scores | ||||
| Pain | 53.65 (14.93) | 69.97 (12.51) | 16.32 (11.20) | 0.001 |
| Other Symptoms | 58.48 (16.12) | 71.21 (11.25) | 12.72 (11.66) | 0.001 |
| ADL | 58.00 (17.26) | 73.99 (14.20) | 15.99 (11.07) | 0.001 |
| FSR | 24.06 (15.94) | 39.38 (23.18) | 15.31 (18.57) | 0.008 |
| QOL | 31.64 (11.29) | 48.05 (17.64) | 16.41 (18.24) | 0.005 |
Pre/post differences were calculated for each participant; mean and SD were obtained from these data. Differences in muscle physiological properties are given as percentages to describe the proportional amount of change; KOOS pre/post differences are out of 100, the total possible KOOS score.
Statistical significance for all tests was set at p<0.05.
Nċm=newtonċmetre; W=watt; J=joule; ADL=activities of daily living; FSR=function, sports, and recreational activities; QOL=quality of life QF=quadriceps femoris.
Figure 2.
Mean weekly pain score on the visual analogue scale, with error bars representing the SD.
Discussion
Power training is not a customary physiotherapy treatment approach for people with knee OA. Legitimate concerns have been expressed about its applicability for this population because high-velocity resistance training could exacerbate pain symptoms, which would be detrimental. Results from our pilot study, however, suggest that this approach is feasible, given our participants' regular attendance and the absence of pain exacerbation during the training programme (no adverse events were reported, and no changes in the amount of analgesic use were observed from the medication diaries). However, the small sample size limits the generalizability of these findings. In addition, the patients recruited to the study were highly motivated to participate in the training programme, which may have affected their tolerance to pain exacerbation. Level of disability may have also affected their tolerance to the programme, as participants in this pilot study were not severely affected by knee OA (i.e., all were at stage 1 or 2 on the Kellgren–Lawrence scale).29
We found significant gains in QFP and QFW and improvements in participants' self-reported functional status after 24 training sessions, and these gains were found to be both statistically and clinically significant, indicating an important difference in participants' conditions following the training protocol. These results are similar to previous findings from large-scale clinical trials, which demonstrated that muscle-strengthening regimens based on resistance training can lead to significant improvements in pain and function for knee OA.4 Improvement in muscle power, pain, and function were similar to those reported for people with knee OA undergoing a 12-week power-training programme in a recently published study.27 The fact that these gains were achieved after a relatively short programme (24 sessions in 8 weeks) suggests that power training for patients with knee OA is not only well tolerated but can produce significant gains within a short time. Indeed, previous studies on resistance training and power training in older adults25 and older adults with knee OA4,27 obtained their positive results with a much higher training dose. Because compliance with exercise programmes diminishes, or at least can become more difficult to maintain, as programme duration increases, the 8-week programme proposed here seems to offer participants a good balance between time commitment and benefits. The majority of resistance-training exercise programmes for older adults use dynamometric equipment; the use of elastic bands to provide resistance in the power-training exercise programme described here increases the generalizability of this approach, particularly as a home-based programme.
One of the major strengths of our study is that it used a variety of valid instruments, including a VAS, the KOOS questionnaire, and the Biodex protocol, which are often the core outcomes measured in intervention studies for people with knee OA. While we observed significant changes in the outcomes measured by these instruments, which points to potential efficacy, it would be important for future studies to consider physical performance outcome measures such as the stair-climb test, the timed up-and-go test, or the 6-minute walk test, to gain a better appreciation of the functional impact of power training.
Limitations
Results from this pilot study are encouraging, but they should be interpreted in light of the limitations of the study design and the population recruited. In addition to the small sample size, a limitation of the study was the absence of a control group and the fact that all participants were women. We made these choices in the context of the objectives and constraints of a pilot study. Interpretation of the results obtained should thus be limited to the population studied.
Conclusion
This pilot study shows that power training 3 times a week for 8 weeks is a feasible and promising treatment modality for women aged 50 to 70 years old with stage 1 or 2 knee OA. Given the positive results our participants saw and the feasibility of the exercise regimen described, clinical application of this mode of resistance training should be considered in the management of people with knee OA. However, further studies must be conducted to better understand the most effective programme parameters and the dose response relative to traditional resistance training used with this population.
Key Messages
What is already known on this topic
Knee osteoarthritis (OA) affects between 10% and 15% of adults over age 60 and can lead to important activity and mobility limitations. Muscle-strengthening regimens based on resistance training can lead to significant improvements in pain and function for people with knee OA.
What this study adds
Power training with elastic bands is a feasible and promising treatment modality for older women with knee OA. Demonstrated improvements in participants' muscle power, pain, and self-reported functional status were achieved with a relatively short (3×/wk for 8 wk) one-on-one supervised training programme that could be adapted as a home-based programme.
Physiotherapy Canada 2013; 65(2);176–182; doi:10.3138/ptc.2012-05
References
- 1.Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26(3):355–69. doi: 10.1016/j.cger.2010.03.001. http://dx.doi.org/10.1016/j.cger.2010.03.001. Medline:20699159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jüni P, Reichenbach S, Dieppe P. Osteoarthritis: rational approach to treating the individual. Best Pract Res Clin Rheumatol. 2006;20(4):721–40. doi: 10.1016/j.berh.2006.05.002. http://dx.doi.org/10.1016/j.berh.2006.05.002. Medline:16979535. [DOI] [PubMed] [Google Scholar]
- 3.Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;(3):CD002759. doi: 10.1002/14651858.CD002759.pub2. Medline:19588334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Latham N, Liu CJ. Strength training in older adults: the benefits for osteoarthritis. Clin Geriatr Med. 2010;26(3):445–59. doi: 10.1016/j.cger.2010.03.006. http://dx.doi.org/10.1016/j.cger.2010.03.006. Medline:20699165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.ACSM. ACSM's guidelines for exercise testing and prescription. 6th ed. Baltimore (MD): Wolters Kluwer; 2000. [Google Scholar]
- 6.Bottaro M, Machado SN, Nogueira W, et al. Effect of high versus low-velocity resistance training on muscular fitness and functional performance in older men. Eur J Appl Physiol. 2007;99(3):257–64. doi: 10.1007/s00421-006-0343-1. http://dx.doi.org/10.1007/s00421-006-0343-1. Medline:17146693. [DOI] [PubMed] [Google Scholar]
- 7.de Vos NJ, Singh NA, Ross DA, et al. Effect of power-training intensity on the contribution of force and velocity to peak power in older adults. J Aging Phys Act. 2008;16(4):393–407. doi: 10.1123/japa.16.4.393. Medline:19033601. [DOI] [PubMed] [Google Scholar]
- 8.Henwood TR, Riek S, Taaffe DR. Strength versus muscle power-specific resistance training in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2008;63(1):83–91. doi: 10.1093/gerona/63.1.83. http://dx.doi.org/10.1093/gerona/63.1.83. Medline:18245765. [DOI] [PubMed] [Google Scholar]
- 9.Orr R, de Vos NJ, Singh NA, et al. Power training improves balance in healthy older adults. J Gerontol A Biol Sci Med Sci. 2006;61(1):78–85. doi: 10.1093/gerona/61.1.78. http://dx.doi.org/10.1093/gerona/61.1.78. Medline:16456197. [DOI] [PubMed] [Google Scholar]
- 10.Porter MM. Power training for older adults. Appl Physiol Nutr Metab. 2006;31(2):87–94. doi: 10.1139/h05-034. http://dx.doi.org/10.1139/h05-034. Medline:16604125. [DOI] [PubMed] [Google Scholar]
- 11.Reid KF, Callahan DM, Carabello RJ, et al. Lower extremity power training in elderly subjects with mobility limitations: a randomized controlled trial. Aging Clin Exp Res. 2008;20(4):337–43. doi: 10.1007/bf03324865. Medline:18852547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sayers SP. High-speed power training: a novel approach to resistance training in older men and women. A brief review and pilot study. J Strength Cond Res. 2007;21(2):518–26. doi: 10.1519/R-20546.1. Medline:17530980. [DOI] [PubMed] [Google Scholar]
- 13.Sayers SP. High velocity power training in older adults. Curr Aging Sci. 2008;1(1):62–7. doi: 10.2174/1874609810801010062. http://dx.doi.org/10.2174/1874609810801010062. Medline:20021374. [DOI] [PubMed] [Google Scholar]
- 14.Sayers SP, Gibson K. A comparison of high-speed power training and traditional slow-speed resistance training in older men and women. J Strength Cond Res. 2010;24(12):3369–80. doi: 10.1519/JSC.0b013e3181f00c7c. http://dx.doi.org/10.1519/JSC.0b013e3181f00c7c. Medline:21068681. [DOI] [PubMed] [Google Scholar]
- 15.Kidde J, Marcus R, Dibble L, et al. Regional muscle and whole-body composition factors related to mobility in older individuals: a review. Physiother Can. 2009;61(4):197–209. doi: 10.3138/physio.61.4.197. http://dx.doi.org/10.3138/physio.61.4.197. Medline:20808481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puthoff ML, Janz KF, Nielson D. The relationship between lower extremity strength and power to everday walking behaviors in older adults with functional limitations. J Geriatr Phys Ther. 2008;31(1):24–31. doi: 10.1519/00139143-200831010-00005. http://dx.doi.org/10.1519/00139143-200831010-00005. Medline:18489805. [DOI] [PubMed] [Google Scholar]
- 17.Puthoff ML, Nielsen DH. Relationships among impairments in lower-extremity strength and power, functional limitations, and disability in older adults. Phys Ther. 2007;87(10):1334–47. doi: 10.2522/ptj.20060176. http://dx.doi.org/10.2522/ptj.20060176. Medline:17684086. [DOI] [PubMed] [Google Scholar]
- 18.Bean JF, Kiely DK, LaRose S, et al. Is stair climb power a clinically relevant measure of leg power impairments in at-risk older adults? Arch Phys Med Rehabil. 2007;88(5):604–9. doi: 10.1016/j.apmr.2007.02.004. http://dx.doi.org/10.1016/j.apmr.2007.02.004. Medline:17466729. [DOI] [PubMed] [Google Scholar]
- 19.Clark DJ, Patten C, Reid KF, et al. Muscle performance and physical function are associated with voluntary rate of neuromuscular activation in older adults. J Gerontol A Biol Sci Med Sci. 2011;66(1):115–21. doi: 10.1093/gerona/glq153. http://dx.doi.org/10.1093/gerona/glq153. Medline:20829294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cuoco A, Callahan DM, Sayers S, et al. Impact of muscle power and force on gait speed in disabled older men and women. J Gerontol A Biol Sci Med Sci. 2004;59(11):1200–6. doi: 10.1093/gerona/59.11.1200. http://dx.doi.org/10.1093/gerona/59.11.1200. Medline:15602076. [DOI] [PubMed] [Google Scholar]
- 21.Herman S, Kiely DK, Leveille S, et al. Upper and lower limb muscle power relationships in mobility-limited older adults. J Gerontol A Biol Sci Med Sci. 2005;60(4):476–80. doi: 10.1093/gerona/60.4.476. http://dx.doi.org/10.1093/gerona/60.4.476. Medline:15933387. [DOI] [PubMed] [Google Scholar]
- 22.Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev. 2012;40(1):4–12. doi: 10.1097/JES.0b013e31823b5f13. http://dx.doi.org/10.1097/JES.0b013e31823b5f13. Medline:22016147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reid KF, Naumova EN, Carabello RJ, et al. Lower extremity muscle mass predicts functional performance in mobility-limited elders. J Nutr Health Aging. 2008;12(7):493–8. doi: 10.1007/BF02982711. http://dx.doi.org/10.1007/BF02982711. Medline:18615232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Runge M, Rittweger J, Russo CR, et al. Is muscle power output a key factor in the age-related decline in physical performance? A comparison of muscle cross section, chair-rising test and jumping power. Clin Physiol Funct Imaging. 2004;24(6):335–40. doi: 10.1111/j.1475-097X.2004.00567.x. http://dx.doi.org/10.1111/j.1475-097X.2004.00567.x. Medline:15522042. [DOI] [PubMed] [Google Scholar]
- 25.Steib S, Schoene D, Pfeifer K. Dose-response relationship of resistance training in older adults: a meta-analysis. Med Sci Sports Exerc. 2010;42(5):902–14. doi: 10.1249/MSS.0b013e3181c34465. http://dx.doi.org/10.1249/MSS.0b013e3181c34465. Medline:19996996. [DOI] [PubMed] [Google Scholar]
- 26.Tschopp M, Sattelmayer MK, Hilfiker R. Is power training or conventional resistance training better for function in elderly persons? a meta-analysis. Age Ageing. 2011;40(5):549–56. doi: 10.1093/ageing/afr005. http://dx.doi.org/10.1093/ageing/afr005. Medline:21383023. [DOI] [PubMed] [Google Scholar]
- 27.Sayers SP, Gibson K, Cook CR. Effect of high-speed power training on muscle performance, function, and pain in older adults with knee osteoarthritis: a pilot investigation. Arthritis Care Res (Hoboken) 2012;64(1):46–53. doi: 10.1002/acr.20675. http://dx.doi.org/10.1002/acr.20675. Medline:22012877. [DOI] [PubMed] [Google Scholar]
- 28.Roos EM, Roos HP, Lohmander LS, et al. Knee injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. Medline:9699158. [DOI] [PubMed] [Google Scholar]
- 29.Kellgren J, Lawrence J. Atlas of standard radiographs. Oxford: Blackwell Scientific; 1963. [Google Scholar]
- 30.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. http://dx.doi.org/10.1016/0022-3956(82)90033-4. Medline:7183759. [DOI] [PubMed] [Google Scholar]
- 31.Hughes C, Page P. Scientific basis of exercise resistance. In: Page P, Ellenbecker T, editors. The scientific and clinical application of elastic resistance. Champaign (IL): Human Kinetics; 2003. pp. 1–25. [Google Scholar]
- 32.Page P, Labbe A, Topp R. Clinical force production of Thera Band® elastic bands. J Orthop Sports Phys Ther. 2000;30(1):A47–8. [Google Scholar]
- 33.Ornetti P, Parratte S, Gossec L, et al. Cross-cultural adaptation and validation of the French version of the Knee injury and Osteoarthritis Outcome Score (KOOS) in knee osteoarthritis patients. Osteoarthritis Cartilage. 2008;16(4):423–8. doi: 10.1016/j.joca.2007.08.007. http://dx.doi.org/10.1016/j.joca.2007.08.007. Medline:17905602. [DOI] [PubMed] [Google Scholar]
- 34.Drouin JM, Valovich-mcLeod TC, Shultz SJ, et al. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur J Appl Physiol. 2004;91(1):22–9. doi: 10.1007/s00421-003-0933-0. http://dx.doi.org/10.1007/s00421-003-0933-0. Medline:14508689. [DOI] [PubMed] [Google Scholar]
- 35.Boonstra AM, Schiphorst Preuper HR, Reneman MF, et al. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. 2008;31(2):165–9. doi: 10.1097/MRR.0b013e3282fc0f93. http://dx.doi.org/10.1097/MRR.0b013e3282fc0f93. Medline:18467932. [DOI] [PubMed] [Google Scholar]