We can’t solve our problems by using the same kind of thinking we used when we created the problems.
Einstein
A growing phenomenon continues to fracture contemporary clinical medicine. We now have orthodox medicine, naturopathic medicine, ayurvedic medicine, environmental medicine, osteopathic medicine, complementary and alternative medicine, functional medicine, restorative medicine, and so on. Mainstream physicians generally believe that conventional medicine is scientific and that alternative medicine is unscientific1; alternative practitioners, on the other hand, generally believe that conventional practitioners are ill equipped to facilitate health and healing. Although each group shares a common desire to help patients and sincerely believes it has answers for the health care challenges of today and tomorrow, the expanding divide between professional health disciplines is confusing for patients and problematic for those crafting health policies. It behooves medical organizations to address the rift between conventional and alternative health care for the sake of patient well-being and the future of clinical medicine.
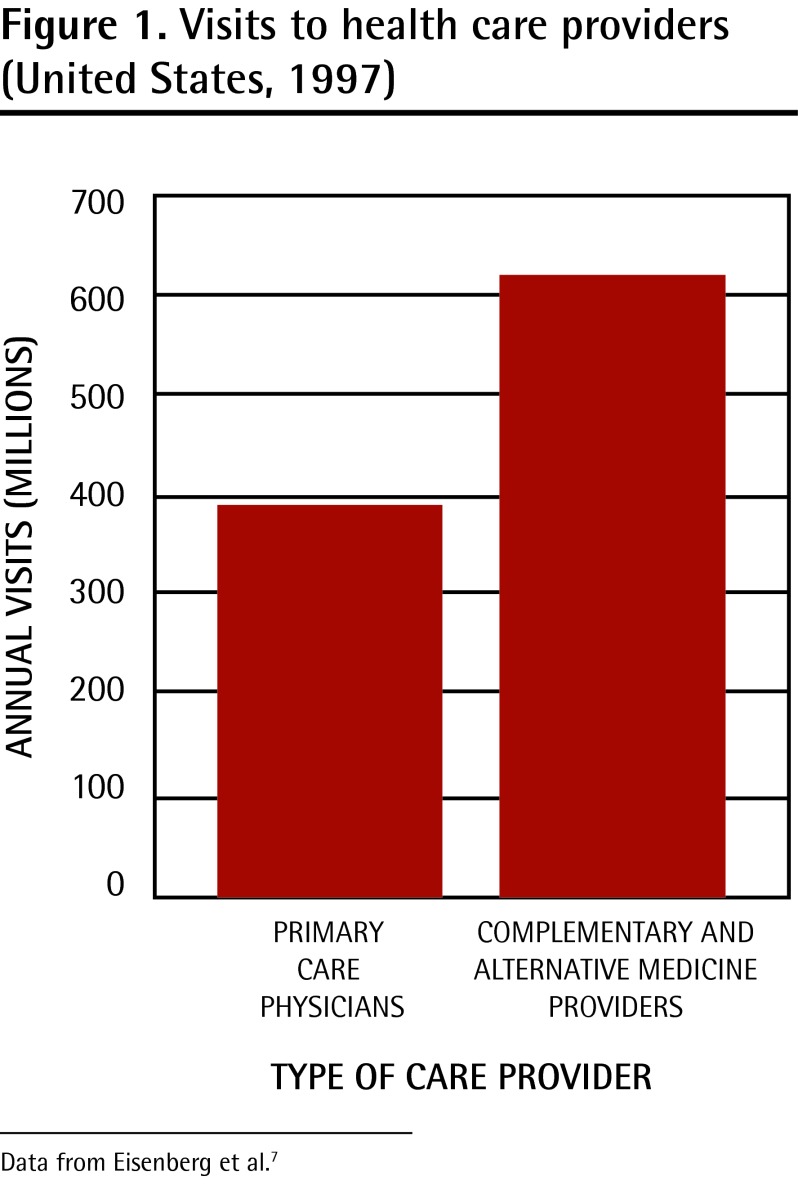
Fractures and splits are often a barometer of the level of dysfunction within an institution—this is certainly evident in contemporary health care with escalating rates of chronic disease,2,3 poor morale within the medical community,4 health care systems in disarray,5 alarming rates of medical errors,6 and so on. In this milieu, there are countless suffering patients scrambling to find solutions for their health concerns, and recent evidence suggests there are now more visits registered to nonallopathic practitioners in America than to conventional primary care physicians (Figure 1).7 In fact, the demand continues to escalate, with current reports estimating that $5.6 billion, or about $166 per capita, is spent annually on nonconventional health care in Canada.8 Physicians often feel slighted when patients seek help elsewhere, yet the escalating demand for nonallopathic approaches frequently represents dissatisfaction with outcomes obtained through conventional medicine. Rather than collaborating to optimize patient outcomes, however, disparate medical groups continue to allow tensions to divide them.
Figure 1.
Visits to health care providers (United States, 1997)
Data from Eisenberg et al.7
Divide between conventional and alternative medicine
A perspective from conventional medicine
Improvements in life expectancy during the past few decades are often heralded as evidence of the sufficiency and success of the conventional scientific medical model. With such achievement, physicians frequently fail to regard alternative health providers as “real doctors,” sometimes perceiving them as pretenders or charlatans who practise quackery with no scientific substantiation for their far-fetched interventions. Some physicians consistently disparage other health care disciplines, highlighting the glaring paucity of clinical trials and evidence-based science in many alternative interventions.1 In fact, the Canadian Medical Association recently summarized the view of many physicians that a nonallopathic approach to health care has “minimal scientific validity and that recommending it to patients achieves no clinical purpose and may be unethical.”9 Responding to the mounting interest in unconventional interventions from some physicians, the British Columbia Medical Association recently warned of “ethical challenges that arise when physicians form professional affiliations with alternative providers.”8
Conventional medical advocates have often alleged that the divisions within health care are destructive and expressed the sentiment that until “people themselves are better educated concerning the danger and iniquity of quackery, they must be protected from the forces that prey.”10 Some suggest that perhaps discourse in science and medicine should be constrained in order to avoid confusion for health consumers and to preclude loss of trust in conventional approaches and institutions. Recognizing that the scientific literature defines a “discipline’s objects of study, methodologies, and discursive conventions,”11 some seek to influence the policies of scientific journals in order to control the production of knowledge in a given field by requiring authors to stick to “dominant discursive conventions”11 in order to get published. Within this mindset, journals might disregard or reject submissions considered unconventional and limit what information can be categorized as credible knowledge, thus determining who has the power to speak about a given field of study.
In addition, some of the ongoing fodder for anti-alternative sentiment is provided through websites and publications originating from individuals with scientific training who customarily disparage unconventional attitudes and therapies in health care.12–14 Allegedly acting as sentinels to expose contemporary health fraud and “quackery,” their message is often vitriolic toward physicians who incorporate nonconventional approaches, all the while exhorting consumers to pursue conventional health care.12,13 Using scientific vernacular, such diatribes are effective in manufacturing doubt15 and maintaining unreceptive attitudes toward alternative care.
Rebuttal from advocates of alternative approaches
Alternative health practitioners, on the other hand, sometimes regard physicians as dupes who are deluded about their own prowess and deceived by the seductive charms of the pharmaceutical industry. Detractors of conventional medicine often cite studies confirming swelling rates of chronic illness,3 especially in children,2 in the face of unprecedented health care expenditures as evidence that mainstream approaches are failing. They frequently reference publications, such as the BMJ, that report that most therapies in conventional medicine lack solid scientific evidence16 and that many have never been adequately assessed.16,17 Recent research, for example, confirms that two-thirds of clinical practice recommendations put forth by the American College of Obstetricians and Gynecologists lack good or consistent scientific evidence.18 Further, the Institute of Medicine and others have reported that clinical practice guidelines detailing recommended practice algorithms in conventional medicine are often developed by committees whose members have substantial financial relations with industry.19–21
The most acerbic assertions against the conventional medical model, however, highlight the widespread medical blunders and complications within mainstream medical practice.6,22–26 The oft-quoted statistic, originally published in JAMA, is the sobering detail that after deaths from heart disease and cancer, iatrogenic illness from conventional medicine is now “the third leading cause of death in the United States,”27 with more deaths than occur from strokes, chronic respiratory diseases, Alzheimer disease, diabetes, accidents, or various others causes. In Canada, a landmark 2004 study by Baker et al found that there were 9250 to 23 750 preventable deaths in Canadian hospitals each year,28 and the American Healthgrades report disclosed that the incidence of medical harm is estimated to be many thousands of harmful or lethal errors daily,29 with a spike of fatal medication errors occurring in July owing, in part, to the arrival of new medical residents.30 Despite vigorous efforts of late to address the calamity of pervasive iatrogenic illness, the New England Journal of Medicine reports that rates of harm persist unabated with little evidence of widespread improvement.31 Some critics contend that such outcomes reflect clinical practices that are much more problematic than any form of alleged alternative quackery and consider it ironic that conventional health providers deem themselves principal members of “the scientific community.”8
Detractors of conventional health care point out that statistical improvements in life expectancy data, rather than validating contemporary health care, primarily reflect steep declines in infant mortality resulting from innovative neonatal care, combined with advanced interventions for trauma, cardiac events, and infectious disease; such acute care is widely esteemed. Overall, however, “the neglected epidemic of chronic disease,”32 rampant iatrogenic illness,27 and inattention to prevention33,34 have led critics to assert that mainstream medicine is failing as a results-oriented profession, and that integration of alternative approaches is required.
Finally, alternative medical practitioners assert that the vocal rancour from conventional medicine is disingenuous, self-serving, and unoriginal. In fact, a frequently referenced publication in JAMA highlights a 1987 US federal court judgment against the American Medical Association and other medical groups for seeking to establish a health care monopoly, citing systematic defamation, and publishing and distribution of propaganda specifically intended to ruin other health care professionals’ reputations.35 The American Medical Association was also admonished for coercing physicians to refuse collaboration with nonconventional practitioners such as osteopaths and naturopaths in the comanagement of patients.35
With unrelenting acrimony between competing health care disciplines, how do we proceed? A comprehensive analysis of any issue involves a study of its history; there are lessons to be gleaned from a glimpse into bygone medicine.
Snapshot of medical history
The advancement of medical knowledge with change in clinical practice has always been the result of challenging the status quo, evaluating shortcomings, and proposing new and alternative approaches. Hippocrates, the “father of scientific medicine,” challenged the metaphysical paradigm of clinical medicine circa 400 bce in order to move medicine from a religion to a science. In his foundational writings in the Hippocratic Corpus, alternative ideas were introduced about the causes of illness that shifted disease attribution from conventional beliefs involving metaphysical demons and spirits to identifiable determinants within the natural realm.36
Throughout medical history, however, alternative ideas about illness and clinical management have consistently been scoffed at, no matter how compelling the evidence.37–39 Transitions have been sluggish because of systemic reluctance to trade the shackles of orthodox belief for emerging unconventional evidence.38 Semmelweis’ historic hand-washing intervention to prevent puerperal sepsis was mocked for a generation before implementation,40 and Lind’s monumental discovery that citrus ingestion was the antidote for scurvy took more than 4 decades to be accepted.41 Mendel, the “father of genetics,” was considered a monster for his research suggesting transgenerational transmission.42 Warren and Marshall’s 2005 Nobel Prize in medicine occurred only after years of rebuke and ridicule following their discovery of the link between Helicobacter pylori and ulcers.43 Although each generation believes it is open minded, sophisticated, and free from the prejudices of bygone eras, conventional medicine has consistently rejected new or alternative ideas, and research that challenges traditional wisdom.39
Does this mean we should accept every new theory or uncanny intervention that emerges? Hardly. Ineffective, fraudulent, and dangerous therapies have also been peddled throughout medical history by misguided practitioners or charlatans delivering grandiose claims. The “quackery” movement of 18th-century Holland and the “snake oil” phenomenon of 19th-century America highlight examples of health care gone awry. Any move forward will require that we vigorously pursue scientific rigour to distinguish fact from fiction in clinical medicine and to protect the public from foolhardy offshoots and outlandish remedies while remaining open to innovative advances. The role of another historical determinant in the contemporary health care diaspora must also be considered.
During the past 150 years, the ubiquitous presence and influence of the “corporation” has emerged, coupled with increasingly aggressive use of intellectual property rights (IPR) law.44 Almost all so-called complementary or alternative therapies lie outside the domain of IPR law, and consequently are of little interest to industry. Corporations are inexorably drawn to products or services for which IPR law allows monopoly patent protection, thus markedly enhancing profitability and hence shareholder satisfaction. With enormous tentacles extending into research decisions,45 medical practice guidelines,21 scientific publications,46,47 university administrations,48 and government policy, the heavy thumbprint of commerce subtly yet profoundly influences attitudes among health care professionals toward clinical approaches.45–47,49,50
In review, alongside a mainstream reluctance to consider unfamiliar approaches and the covert shadow of corporate sway,39,51 a diverse spectrum of sincere health care providers is juxtaposed. Within this context, what primary principles might be incorporated to advance optimal health care?
Moving forward
First, unbiased scientific scrutiny needs to be applied to existing therapies as well as to novel initiatives. With alarming rates of iatrogenic illness, current approaches and new ideas in both allopathic and nonallopathic care merit equal examination and critical appraisal. Clinical medicine should be based on credible, untainted research and reporting, reproducible observation, competent and compassionate health care, as well as (and most important) favourable outcomes for patients and populations—not on arbitrary notions of what is allopathic and what is alternative. Effective, sound science should be supported; ineffectual interventions should be discarded. However, the rigid demand that randomized controlled trials be required for legitimacy of any alternative care is absurd. Randomized controlled trial evidence is lacking for many conventional health-promoting interventions such as the health efficacy of seat-belt use, alcohol avoidance in pregnancy, tobacco cessation for cancer prevention, and even parachute deployment while skydiving.52 Other forms of evidence, such as epidemiologic research, can also impart scientific validation.
Scottish legend Thomas Dewar once said, “Minds are like parachutes; they only function when open.” Much lip service is paid in academia to the importance of critical thinking, tolerance, impartiality, and independent thought. Yet, health care trainees are sometimes socialized to conform to status quo principles and to emerge as staunch protectors of their brand. All health disciplines need to be less defensive about their respective ideologies, and mainstream physicians should accept that exploration of innovative approaches is not a betrayal of conventional medicine. Careful consideration, scrutiny of scientific merit, and adoption of credible approaches should be the algorithm, not visceral dismissal of anything unfamiliar.
Regulatory bodies need to fulfil their mandate of protecting the public. The incessant morbidity and mortality figures associated with standard medical interventions6,22–27,31 discredit the profession and challenge the very legitimacy of existing regulatory institutions. Authorities should adopt an outcome-based assessment approach by monitoring the aftermath of health care, rather than scrutinizing practitioner adherence to evolving standard-of-care credos, subjective opinions from conventional experts, or dubious practice guidelines.21 Regulatory agencies are sometimes accused of intimidating physicians perceived to be thinking outside of the box; instead they should protect the community by demonstrating concerted vigilance and scrutiny of contributions made by health care practitioners to the state of individual and population health. Results are the measure of evidence and should be the grid whereby health care and regulatory bodies are evaluated—insufficient attention to outcomes in an age of evidence-based medicine is incongruous and illogical. Furthermore, conflict of interest should be eradicated within regulatory agencies by eliminating affiliation with the sway of corporate science.
Scientific journals must remain impartial, with decisions on merit governed by ideas and evidence, not ideologies. With ongoing resistance from scientific journals, Warren and Marshall struggled to publish their research data on H pylori and ulcers, leading them to conclude that gastroenterology was more about religion than science.43 All scientific approaches, not only those that fit a predetermined paradigm, should receive equal consideration. Peer reviewers should not be limited to those who exist within the confines of one approach and are philosophically opposed to iconoclastic ideas.
While good health care makes sense, it does not make money; there is an inherent tension when profit underlies the evidence supporting the approach to care. Health initiatives not furthering corporate interests do not receive the same support or research funding as approaches that predominantly rely on the “have an ill, take a pill” algorithm to health care. Most postgraduate medical education is supported, organized, and undertaken by vested interests.50,53 The medical community must become apprised of the reality of profit-motivated research45,46 as an obstacle to clinical approaches that promote healing rather than chronic care, and interventions that favour education not medication. The word doctor, after all, originates from the Latin docēre, which means to teach. Medical instruction at all stages should remain the purview of public interest, not vested interests.
Finally, knowledge translation needs to be expedited in our information age,38,39 and clinical medicine in all health care disciplines should keep up with sound science. No matter how attached health care providers are to their habitual clinical approaches, the stark reality is that new science often represents “the slaying of a beautiful hypothesis through an ugly fact.”38 In contradistinction to profuse evidence about disease origins,24 for example, much chronic disease care still presumes genomic predestination and persists in managing epiphenomena rather than addressing causative determinants within the exposome and epigenome.54–56 A historic paper in the American Journal of Cardiology highlights this state of affairs in relation to coronary artery disease,34 a leading cause of global morbidity and mortality. All safe and effective clinical approaches—mainstream, alternative, or any integrative permutation—should be committed to knowledge translation with expeditious adoption of credible emerging science.
Conclusion
It is neither expected nor necessary that physicians, naturopaths, nutritionists, holistic practitioners, and others sit together in a big circle, join hands, and sing “Kumbaya.” The reality that both worthwhile and disappointing outcomes routinely result from interventions originating from both conventional and alternative therapies might suggest that some measure of merit and malarkey emanates from various directions. Accordingly, existing approaches and new ideas in both conventional and alternative health care deserve equal scrutiny and critical appraisal. Fair and unbiased examination of all health disciplines and clinical practices, rather than reflexive disdain for nonfamiliar approaches, might facilitate rapid rejection of useless or fraudulent therapies and hasten the protracted period of translation and adoption of valuable clinical knowledge and skills. Mutual respect among health providers would ameliorate the current animosity and improve the comfort level for patients reluctant to disclose use of nonconventional care.57 It is instructive that some esteemed medical organizations have increasingly embraced non-conventional approaches—for example, the second edition of the Mayo Clinic Book of Alternative Medicine was recently released, advocating the integration of natural therapies and conventional medicine in clinical care.58
Challenging the status quo with adoption of new ideas and skills has always been, and remains, the customary path to scientific and clinical progress. Perhaps it is time to incorporate credible science and reputable evidence, whatever the source, into the practice of mainstream clinical medicine. Perhaps it is time to consider medicine without descriptors and to integrate outcome-based measures as the primary indicator of high-quality health care. Perhaps regulatory bodies should protect the public by securing compliance with health care that delivers safe and optimal results. Perhaps bridges rather than walls should be erected between fragmenting medical disciplines.
Footnotes
This article has been peer reviewed.
Competing interests
None declared
References
- 1.Dalen JE. “Conventional” and “unconventional” medicine: can they be integrated? Arch Intern Med. 1998;158(20):2179–81. doi: 10.1001/archinte.158.20.2179. [DOI] [PubMed] [Google Scholar]
- 2.Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood chronic conditions in the United States. JAMA. 2007;297(24):2755–9. doi: 10.1001/jama.297.24.2755. [DOI] [PubMed] [Google Scholar]
- 3.Sears ME, Genuis SJ. Environmental determinants of chronic diseaseand medical approaches: recognition, avoidance, supportive therapy, and detoxification. J Environ Public Health. 2012;2012:356798. doi: 10.1155/2012/356798. Epub 2012 Jan 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith R. Why are doctors so unhappy? There are probably many causes, some of them deep. BMJ. 2001;322(7294):1073–4. doi: 10.1136/bmj.322.7294.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Linden RA. The rise and fall of the American medical empire: a trench doctor’s view of the past, present, and future of the U.S. healthcare system. North Branch, MN: Sunrise River Press; 2010. pp. 44–117. [Google Scholar]
- 6.Institute of Medicine . To err is human: building a safer health system. Washington, DC: National Academy Press; 2000. [Google Scholar]
- 7.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280(18):1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 8.Belluz J. Alternative medicine worry hits boiling point. The Medical Post. 2011 Oct 4; [Google Scholar]
- 9.Gollom M. Doctors slam alternative medicine proposal. CBC News. 2011 Sep 12; Available from: www.cbc.ca/news/health/story/2011/09/09/alternative-medicine-guidelines.html. Accessed 2013 Apr 25. [Google Scholar]
- 10.Quackery abroad [JAMA 100 years ago] JAMA. 2012;307(21):2236. [Google Scholar]
- 11.McNabb R. Making all the right moves: Foucault, journals, and the authorization of discourse. J Sch Publ. 1999;31(1):20–41. [Google Scholar]
- 12.Barrett S. Quackwatch: your guide to quackery, health fraud, and intelligent decisions. Chapel Hill, NC: Quackwatch; 2013. Available from www.quackwatch.com. Accessed 2013 May 7. [Google Scholar]
- 13.Barrett S. National Council Against Health Fraud archive. Chapel Hill, NC: National Council Against Health Fraud; 2012. Available from: www.ncahf.org. Accessed 2012 May 22. [Google Scholar]
- 14.Novella S. Science-based medicine: exploring issues and controversies in the relationship between science and medicine. Science-Based Medicine; 2008. Available from: www.sciencebasedmedicine.org. Accessed 2012 Jun 6. [Google Scholar]
- 15.Michaels D. Doubt is their product. How industry’s assault on science threatens your health. New York, NY: Oxford University Press; 2008. [Google Scholar]
- 16.Smith R. Where is the wisdom...? BMJ. 1991;303(6806):798–9. doi: 10.1136/bmj.303.6806.798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prasad V, Cifu A, Ioannidis JP. Reversals of established medical practices: evidence to abandon ship. JAMA. 2012;307(1):37–8. doi: 10.1001/jama.2011.1960. [DOI] [PubMed] [Google Scholar]
- 18.Wright JD, Pawar N, Gonzalez JS, Lewin SN, Burke WM, Simpson LL, et al. Scientific evidence underlying the American College of Obstetricians and Gynecologists’ practice bulletins. Obstet Gynecol. 2011;118(3):505–12. doi: 10.1097/AOG.0b013e3182267f43. [DOI] [PubMed] [Google Scholar]
- 19.Institute of Medicine of the National Academies . Clinical practice guidelines we can trust. Washington, DC: National Academies Press; 2011. Available from: www.iom.edu/Reports/2011/Clinical-Practice-Guidelines-We-Can-Trust.aspx. Accessed 2011 Sep 18. [PubMed] [Google Scholar]
- 20.Sniderman AD, Furberg CD. Why guideline-making requires reform. JAMA. 2009;301(4):429–31. doi: 10.1001/jama.2009.15. [DOI] [PubMed] [Google Scholar]
- 21.Genuis SJ. The proliferation of clinical practice guidelines: professional development or medicine by numbers? J Am Board Fam Pract. 2005;18(5):419–25. doi: 10.3122/jabfm.18.5.419. [DOI] [PubMed] [Google Scholar]
- 22.Moore TJ, Weiss SR, Kaplan S, Blaisdell CJ. Reported adverse drug events in infants and children under 2 years of age. Pediatrics. 2002;110(5):e53. doi: 10.1542/peds.110.5.e53. [DOI] [PubMed] [Google Scholar]
- 23.McGavock H. Prescription-related illness—a scandalous pandemic. J Eval Clin Pract. 2004;10(4):491–7. doi: 10.1111/j.1365-2753.2003.00471.x. [DOI] [PubMed] [Google Scholar]
- 24.Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324(6):370–6. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 25.Leape LL. Error in medicine. JAMA. 1994;272(23):1851–7. [PubMed] [Google Scholar]
- 26.Nebehay S. Going into hospital far riskier than flying: WHO. Reuters. 2011 Jul 21; Available from: www.reuters.com/article/2011/07/21/us-safety-idUSTRE76K45R20110721. Accessed 2011 Jul 21. [Google Scholar]
- 27.Starfield B. Is US health really the best in the world? JAMA. 2000;284(4):483–5. doi: 10.1001/jama.284.4.483. [DOI] [PubMed] [Google Scholar]
- 28.Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170(11):1678–86. doi: 10.1503/cmaj.1040498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reed KD, May R. HealthGrades Patient Safety in American Hospitals Study. Denver, CO: Healthgrades Inc; 2011. Available from: http://hg-article-center.s3-websiteus-east-1.amazonaws.com/8b/76/afc5e3164c2ca8d8ed2ace1a7cd0/HealthGradesPatientSafetyInAmericanHospitalsStudy2011.pdf. Accessed 2013 Mar 24. [Google Scholar]
- 30.Phillips DP, Barker GE. A July spike in fatal medication errors: a possible effect of new medical residents. J Gen Intern Med. 2010;25(8):774–9. doi: 10.1007/s11606-010-1356-3. Epub 2010 May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Landrigan CP, Parry GJ, Bones CB, Hackbarth AD, Goldmann DA, Sharek PJ. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. 2010;363(22):2124–34. doi: 10.1056/NEJMsa1004404. [DOI] [PubMed] [Google Scholar]
- 32.Horton R. The neglected epidemic of chronic disease. Lancet. 2005;366(9496):1514. doi: 10.1016/S0140-6736(05)67454-5. [DOI] [PubMed] [Google Scholar]
- 33.Genuis SJ. An ounce of prevention. A pound of cure for an ailing health care system. Can Fam Physician. 2007;53:597–9. (Eng), 605–7 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 34.Esselstyn CB., Jr Is the present therapy for coronary artery disease the radical mastectomy of the twenty-first century? Am J Cardiol. 2010;106(6):902–4. doi: 10.1016/j.amjcard.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 35.Getzendanner S. Permanent injunction order against AMA. JAMA. 1988;259(1):81–2. [PubMed] [Google Scholar]
- 36.Adams F, translator. The genuine works of Hippocrates. New York, NY: William Wood and Company; 1891. [Google Scholar]
- 37.Genuis SJ. What’s out there making us sick? J Environ Public Health. 2012;2012:605137. doi: 10.1155/2012/605137. Epub 2011 Oct 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haynes B, Haynes GA. ACP Journal Club. What does it take to put an ugly fact through the heart of a beautiful hypothesis? Ann Intern Med. 2009;150(6):JC3–2. JC3–3. doi: 10.7326/0003-4819-150-6-200903170-02002. [DOI] [PubMed] [Google Scholar]
- 39.Doherty S. History of evidence-based medicine. Oranges, chloride of lime and leeches: barriers to teaching old dogs new tricks. Emerg Med Australas. 2005;17(4):314–21. doi: 10.1111/j.1742-6723.2005.00752.x. [DOI] [PubMed] [Google Scholar]
- 40.Nuland SB. The enigma of Semmelweis—an interpretation. J Hist Med Allied Sci. 1979;34(3):255–72. doi: 10.1093/jhmas/xxxiv.3.255. [DOI] [PubMed] [Google Scholar]
- 41.Bartholomew M. James Lind’s treatise of the scurvy (1753) Postgrad Med J. 2002;78(925):695–6. doi: 10.1136/pmj.78.925.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Henig RM. The monk in the garden: the lost and found genius of Gregor Mendel, the father of genetics. New York, NY: First Mariner Books; 2001. pp. 1–263. [Google Scholar]
- 43.Marshall B, editor. Helicobacter pioneers: firsthand accounts from the scientists who discovered helicobacters, 1892–1982. Victoria, Australia: Blackwell Publishing; 2002. [Google Scholar]
- 44.Gabel M, Bruner H. Globalinc.: an atlas of the multinational corporation. New York, NY: The New Press; 2003. pp. 1–165. [Google Scholar]
- 45.Angell M. The truth about the drug companies: how they deceive us and what to do about it. New York, NY: Random House; 2005. [Google Scholar]
- 46.Angell M. Is academic medicine for sale? N Engl J Med. 2000;342(20):1516–8. doi: 10.1056/NEJM200005183422009. [DOI] [PubMed] [Google Scholar]
- 47.Genuis SK, Genuis SJ. Exploring the continuum: medical information to effective clinical practice. Paper 1: the translation of knowledge into clinical practice. J Eval Clin Pract. 2006;12(1):49–62. doi: 10.1111/j.1365-2753.2005.00608.x. [DOI] [PubMed] [Google Scholar]
- 48.Healy DI. Conflicts of interest in Toronto: anatomy of a controversy at the interface of academia and industry. Perspect Biol Med. 2002;45(2):250–63. doi: 10.1353/pbm.2002.0028. [DOI] [PubMed] [Google Scholar]
- 49.Healy D. Pharmageddon. Los Angeles, CA: University of California Press; 2012. [Google Scholar]
- 50.Moynihan R, Heath I, Henry D. Selling sickness: the pharmaceutical industry and disease mongering. BMJ. 2002;324(7342):886–91. doi: 10.1136/bmj.324.7342.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tatsioni A, Bonitsis NG, Ioannidis JP. Persistence of contradicted claims in the literature. JAMA. 2007;298(21):2517–26. doi: 10.1001/jama.298.21.2517. [DOI] [PubMed] [Google Scholar]
- 52.Smith GC, Pell JP. Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials. BMJ. 2003;327(7429):1459–61. doi: 10.1136/bmj.327.7429.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moynihan R. Who pays for the pizza? Redefining the relationships between doctors and drug companies. 1: entanglement. BMJ. 2003;326(7400):1189–92. doi: 10.1136/bmj.326.7400.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Genuis SJ. Our genes are not our destiny: incorporating molecular medicine into clinical practice. J Eval Clin Pract. 2008;14(1):94–102. doi: 10.1111/j.1365-2753.2007.00808.x. [DOI] [PubMed] [Google Scholar]
- 55.Paoloni-Giacobino A. Post genomic decade—the epigenome and exposome challenges. Swiss Med Wkly. 2011;141:w13321. doi: 10.4414/smw.2011.13321. [DOI] [PubMed] [Google Scholar]
- 56.Rappaport SM. Discovering environmental causes of disease. J Epidemiol Community Health. 2012;66(2):99–102. doi: 10.1136/jech-2011-200726. [DOI] [PubMed] [Google Scholar]
- 57.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328(4):246–52. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 58.Mayo Foundation for Medical Education and Research . Mayo Clinic book of alternative medicine. 2nd ed. New York, NY: Time Inc.; 2010. pp. 6–206. [Google Scholar]