Abstract
BACKGROUND AND OBJECTIVES:
Hypothermia contributes to neonatal mortality and morbidity, especially in preterm and low birth weight infants in developing countries. Plastic bags covering the trunk and extremities of very low birth weight infants reduces hypothermia. This technique has not been studied in larger infants or in many resource-limited settings. The objective was to determine if placing preterm and low birth weight infants inside a plastic bag at birth maintains normothermia.
METHODS:
Infants at 26 to 36 weeks’ gestational age and/or with a birth weight of 1000 to 2500 g born at the University Teaching Hospital in Lusaka, Zambia, were randomized by using a 1:1 allocation and parallel design to standard thermoregulation (blanket or radiant warmer) care or to standard thermoregulation care plus placement inside a plastic bag at birth. The primary outcome measure was axillary temperature in the World Health Organization–defined normal range (36.5–37.5°C) at 1 hour after birth.
RESULTS:
A total of 104 infants were randomized. At 1 hour after birth, infants randomized to plastic bag (n = 49) were more likely to have a temperature in the normal range as compared with infants in the standard thermoregulation care group (n = 55; 59.2% vs 32.7%; relative risk 1.81; 95% confidence interval 1.16–2.81; P = .007). The temperature at 1 hour after birth in the infants randomized to plastic bag was 36.5 ± 0.5°C compared with 36.1 ± 0.6°C in standard care infants (P < .001). Hyperthermia (>38.0°C) did not occur in any infant.
CONCLUSIONS:
Placement of preterm/low birth weight infants inside a plastic bag at birth compared with standard thermoregulation care reduced hypothermia without resulting in hyperthermia, and is a low-cost, low-technology tool for resource-limited settings.
Keywords: hypothermia/prevention and control, infant newborn, infant premature, diseases/prevention and control, perinatal care/methods
What’s Known on This Subject:
Preterm neonates in resource-poor settings frequently develop hypothermia. Plastic bags or wraps are a low-cost intervention for the prevention of hypothermia in infants in developed countries.
What This Study Adds:
For preterm infants born in a resource-poor health facility, placement in a plastic bag at birth can reduce the incidence of hypothermia at 1 hour after birth.
Annually, about 3 million infants die during the neonatal period worldwide.1 More than 80% of these neonatal deaths can be attributed to infection, birth asphyxia, complications of premature delivery, including hypothermia, and congenital anomalies.2 Hypothermia has long been recognized as a serious risk to newborns, especially premature and low birth weight infants,3–6 and is a problem in both the developed7 and the developing world.1,8–10 Neonatal hypothermia has been associated with increased risk of infection, coagulation defects, acidosis, delayed fetal-to-newborn circulatory adjustment, hyaline membrane disease, brain hemorrhage, increased oxygen consumption, and increased mortality.3,5,11–13 Infants are most at risk for hypothermia in the first few minutes to hours after birth, when they are first removed from the thermally regulated intrauterine environment.5,12,14 Hypothermia can occur in infants of all countries, including tropical climates.8,9,15,16
The World Health Organization (WHO) recommendations to prevent hypothermia include a warm delivery room (25°C), immediate drying, and resuscitation under radiant warmers, skin-to-skin contact with the mother, or an incubator.17 Low-cost technologies used to prevent hypothermia in preterm and very low birth weight infants in the developed world could be extended to the developing world.
Evaporative heat loss is the major cause of heat loss in newborn infants during the first 30 minutes after birth.18 Insensible water loss and an immature skin barrier contribute to the increased risk of hypothermia in infants.5,19 Polyethylene occlusive wrapping or plastic bags used at birth in the delivery room reduce hypothermia in extremely low and very low birth weight infants.20–24 It is thought that plastic bags reduce evaporative/convective heat losses, insensible water loss, and the need for metabolic heat production.17,25,26 McCall et al,27 in a Cochrane review (including 3 studies of polyethylene wrappings used within 10 minutes of birth in infants <32 weeks’ gestation), concluded that the use of plastic wraps or bags decreases hypothermia soon after birth and recommended future research to determine the feasibility of their use in poorer countries where cost is a concern. The Neonatal Resuscitation Program recommends the use of a plastic bag as a means to prevent hypothermia in infants born at <29 weeks’ gestation.28 The International Liaison Committee on Resuscitation consensus statement recommends the use of a plastic bag in addition to standard techniques in the delivery room for very low birth weight infants.29
Plastic bags may be an affordable option for developing countries. The current trial was designed to test the hypothesis that use of low-cost plastic (polyethylene) bags starting at birth reduces hypothermia without causing hyperthermia at 1 hour after birth in preterm and low birth weight infants. This trial enrolled more mature and larger infants than previously studied because in resource-limited settings these infants are at high risk of hypothermia.
Methods
Study Design
In this single-center randomized controlled trial conducted at the tertiary University Teaching Hospital in Lusaka, Zambia, a standard thermoregulation care strategy (control group) was compared with a strategy including standard thermoregulation care plus placement of the newborn in a low-cost polyethylene bag (intervention group). The study was approved by the institutional review boards of the University of Alabama at Birmingham, Oregon Health & Science University, and University Teaching Hospital in Lusaka, Zambia (Clinicaltrials.gov identifier NCT01403623).
Infants born at the hospital were eligible for inclusion if they were between 26 weeks 0 days and 36 weeks 6 days of gestation at birth according to the best obstetrical estimate (using last menstrual period, fundal height, and ultrasound as assessed by the obstetric team) or if their birth weight was between 1000 and 2500 g. Infants were excluded if they had an abdominal wall defect, myelomeningocele, other major congenital anomaly, or obvious skin disorders. Mothers of eligible infants were identified on admission to the labor and delivery unit and approached for consent before delivery or within 10 minutes after delivery if previous consent was not possible. Written informed consent from the mother was obtained for each infant. Enrollment occurred from August through October 2011. Infants were randomized during both day and night shifts.
In a 1:1 allocation and parallel design, infants were randomly assigned to 1 of the 2 treatment groups at birth. Randomization occurred at birth or within the first 10 minutes after birth. Twins and higher-order multiples were randomized individually. Randomization was blinded and done by using sealed numbered envelopes assigned by a random number generator. Study investigators kept the sealed envelopes and opened them at the birth of the infant. Blinding of the intervention was not possible.
The University Teaching Hospital in Lusaka is a tertiary referral, teaching hospital in the capital of Zambia. There are approximately 11 000 to 13 000 annual births, almost exclusively from high-risk referrals. The ward is staffed by midwives, obstetrics-gynecology residents, and attending obstetricians. There is ultrasound and cesarean delivery capability. Electronic fetal monitoring during labor is not available. There is a NICU staffed by dedicated nurses, pediatric residents, pediatricians, and neonatologists. There are nearly 3000 preterm and term infants admitted annually to the NICU, with a mortality rate of ∼40%. There is incubator, radiant warmer, intravenous fluid, oxygen supplementation, ventilator, and intravenous medication capability. The nursery and NICU have space heaters to achieve a goal room temperature of 25°C, but this is difficult to maintain with open doors and windows. Lusaka has a tropical climate close to the equator, but has a range of ambient temperature from August through October of 17 to 35°C because of its high altitude (4265 feet above sea level).
Control Groups
Infants randomized to the control group were delivered and immediately set on their mother’s abdomen, then dried with blankets and stimulated on the mother’s abdomen while the cord was cut and placenta delivered. If further resuscitation was required, a small nursery in the labor and delivery unit with radiant warmer and other supplies was available. If the infant was delivered by cesarean, the infant was initially dried and stimulated under a radiant warmer in the operating room and then transferred to the nursery in the labor and delivery unit. Resuscitation practices followed the WHO Essential Newborn Care and Helping Babies Breathe training course protocols. Infants were transferred to the nursery, where they were weighed, wrapped (with blankets provided by the family, usually a terry cloth towel and large fleece blanket), covered with a hat, and placed either under a radiant warmer or in an open crib, depending on availability. An initial axillary temperature was obtained at the time of weighing in the nursery and a repeat axillary temperature was obtained at 1 hour after birth. Temperature measurements were obtained with a digital thermometer.
Per hospital practice, mothers and infants were discharged from the hospital as early as 6 hours postpartum if the infant was not admitted to the NICU. If the infants were born in the afternoon, evening, or night, they were discharged from the hospital the next morning. Infants were admitted to the NICU if they had a birth weight <1400 g, had respiratory distress, or had other abnormal signs requiring observation or treatment. Very low birth weight infants were routinely discharged from the hospital from the NICU when they attained a weight of >1500 g and were otherwise medically stable, including normal temperatures in an open crib.
Intervention Group
Infants randomized to the intervention group received the same care, except they were placed inside a plastic bag (nonmedical low-cost [3 cents per bag] linear low-density polyethylene bag measuring 10 × 8 × 24 in. and 1.2 mil [mil is a thousandth of an inch] thick) covering the trunk and extremities. Placement in the plastic bag occurred after brief drying on the mother’s abdomen while the cord was being cut and the infant was handed to the pediatrician or assistant and no later than 10 minutes after birth. The infants remained in the plastic bag for at least 1 hour after birth, at which time the axillary temperature was measured. The bag was removed at 1 hour of age if the infant’s temperature was in the normal range (36.5–37.5°C) or higher. Infants with a temperature below the normal range remained in the plastic bag until a normal temperature was obtained.
All study data were collected by 2 of the authors (A.L. and J.B.W.) and 2 research assistants trained by those authors. Temperature measurements were all taken with the same 3 digital thermometers. Hard copies of the study data were controlled by the investigators and kept in locked offices and kept password protected when transferred to digital files.
Outcomes
The primary outcome was normothermia at 1 hour. Temperatures were classified per WHO guidelines. Normothermia was defined per WHO guidelines as an axillary temperature of 36.5 to 37.5°C (97.7–99.5°F). The temperature was obtained with a digital thermometer placed under the arm of the infant. Hypothermia was defined as a temperature <36.5°C (97.7°F). Hyperthermia was defined as a temperature >38.0°C (100.4°F). The temperature was obtained with a digital thermometer placed in the axilla. Prespecified secondary outcomes on patients admitted to the NICU included hypotension, hypoglycemia, seizures during the first 24 hours after birth, respiratory distress syndrome, bronchopulmonary dysplasia, pneumothorax, sepsis, major brain injury (defined as intraventricular hemorrhage Grade 3 or 4 or periventricular leukomalacia), necrotizing enterocolitis, bowel perforation, pulmonary hemorrhage, and death before discharge.
Statistical Analysis
The sample size was estimated based on historical data from the study center showing a baseline hypothermia rate of 60% in this birth weight range.1,8,30 We hypothesized a 30% absolute risk reduction (50% relative reduction) of hypothermia with the use of the plastic bag. With a preset confidence level of 95%, power of 80%, and using a continuity correction method, a sample size of 50 infants per group was determined to be sufficient to detect a difference between groups.
Descriptive statistics were used to compare baseline characteristics of the study groups. Continuous variables were compared with Student’s t test. Proportions were compared using Mantel-Haenszel χ2/Fisher’s exact statistics. For risk analysis of the primary outcome, risk ratio and confidence intervals for this point estimate were calculated using contingency tables. All data were analyzed with SPSS 17.0 for Windows (IBM SPSS Statistics, IBM Corporation, Chicago, IL). All statistical tests were 2-tailed, and P values <.05 were considered statistically significant.
Results
Study Participants
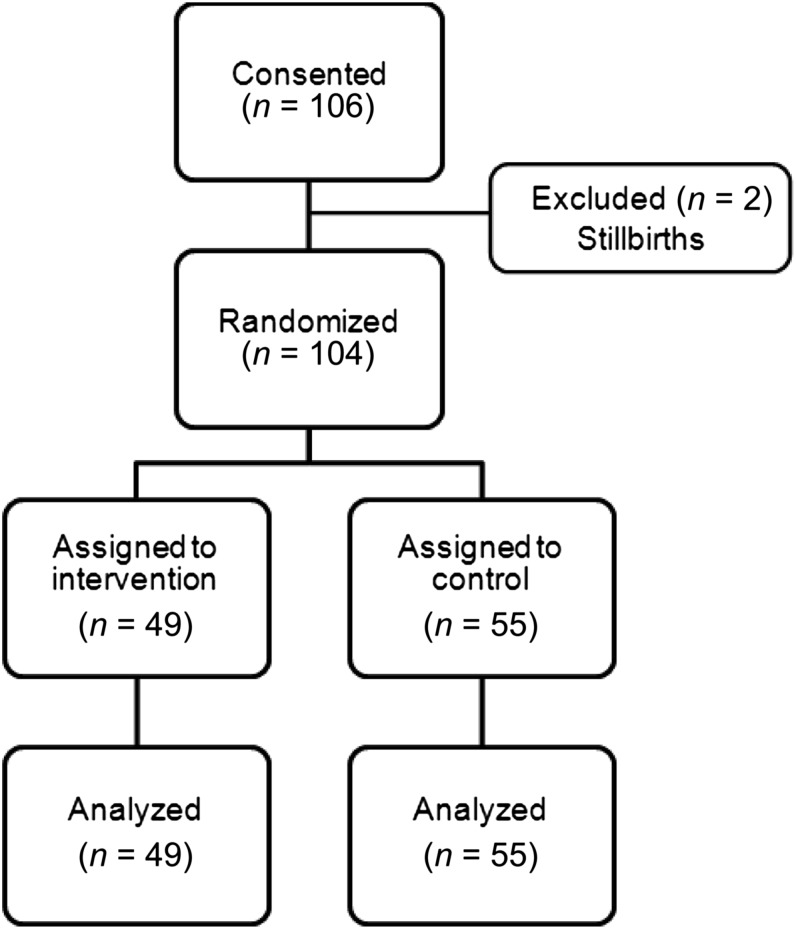
A total of 104 infants were randomized (Fig 1). All but 2 infants were randomized at birth; 2 were randomized within the 10-minute limit. All infants had primary outcome data. The baseline characteristics of infants randomized to the intervention and control groups were similar (Table 1). Of all the infants in the trial, 86 (83%) had a temperature <36.5oC at 10 minutes after birth. Ten infants in the intervention group were <32 weeks’ gestation (20%) and 14 infants in the control group (29%) were <32 weeks’ gestation.
FIGURE 1.
Consort diagram.
TABLE 1.
Baseline Characteristics
| Intervention Group (n = 49) | Control Group (n = 55) | |
|---|---|---|
| Mean birth weight, kg (SD) | 2.20 (0.56) | 2.11 (0.52) |
| Median gestational age, wk (IQR) | 34 (32–36) | 34 (31–36) |
| Gestational age <32 wk (%) | 10 (20) | 14 (29) |
| Male gender, n (%) | 27 (55.1) | 28 (50.9) |
| Vaginal delivery, n (%) | 42 (85.7) | 51 (92.7) |
| NICU admission, n (%) | 14 (28.5) | 9 (16.4) |
| Hypothermia at 10 min, n (%) | 41 (83.7) | 45 (81.8) |
IQR, interquartile range.
Primary Outcome
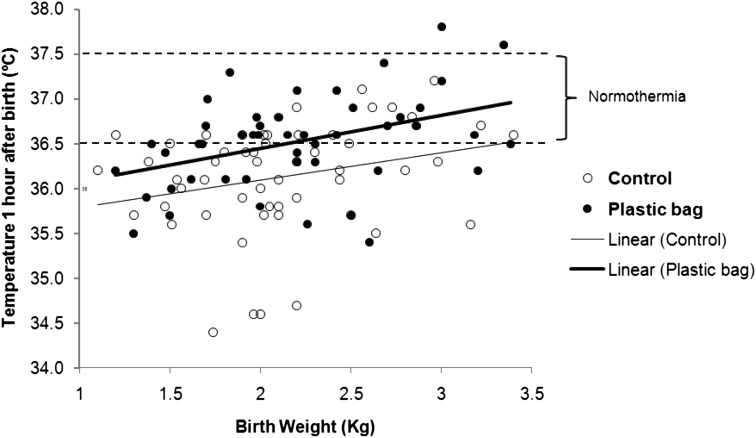
Of the 49 infants in the intervention (plastic bag) group, 29 (59%) compared with 18 (33%) of 55 infants in the control group had a temperature in the normal range at 1 hour after birth (relative risk 1.81 with 95% confidence interval 1.16–2.81, P = .007). The mean temperature at 1 hour for infants in the intervention group was 36.5 ± 0.5oC compared with 36.1 ± 0.6oC in control infants (P < .001). The risk of hypothermia had an absolute risk reduction of 26% when a plastic bag was used (number needed to treat = 4). Temperature at 1 hour was correlated with birth weight, with hypothermia being more common in the smallest infants (Fig 2). The duration of use of the plastic bag in hypothermic infants ranged from 80 to 120 minutes. None of the infants in either group had hyperthermia. None of the infants developed skin side effects attributable to the plastic bags.
FIGURE 2.
Temperature 1 hour after birth in infants randomized to a plastic bag or control group plotted by birth weight. The dotted lines are the limits of normothermia. More infants randomized to a plastic bag compared with control infants had normal temperatures. The effect happened across the birth weight strata. Hyperthermia (>38°C) was not seen.
Secondary Outcomes
Most infants were discharged from the hospital with their mothers in <24 hours. Twenty-three of the 104 infants (14 in the intervention group and 9 in the control group, P = .13) were admitted to the NICU unrelated to the trial interventions. Among infants admitted to the NICU, no significant differences were found in mean temperature after 24 hours of admission, length of hospital stay, or death (7 [14%] of 49 in the intervention group versus 3 [5%] of 55 in the control group, P = .13). Hypotension, hypoglycemia, seizures in the first 24 hours after birth, bronchopulmonary dysplasia, pneumothorax, major brain injury, bowel perforation, or pulmonary hemorrhage were not documented in any of the study infants during their NICU admission.
Discussion
This trial shows that placement of the trunk and extremities of preterm/low birth weight infants in a plastic bag at birth or shortly after birth decreased hypothermia at 1 hour after birth without increasing the risk of hyperthermia. More than 80% of all the infants in the study were hypothermic at 10 minutes after birth, when the first temperature was taken, documenting the high prevalence of this problem, even though most of the infants were more mature or had a higher birth weight than infants for whom plastic bags or wrappings are recommended based on trials in developed countries (<29 weeks’ gestation). Although a reduction in hypothermia was observed, this resulted from a relatively small difference in the actual mean temperatures (36.1 vs 36.5°C).
A limitation of the trial is the short duration of the intervention. The duration of the intervention was selected to prevent hyperthermia, as well as other unlikely hazards of placement inside a plastic bag, such as skin damage or suffocation. Another limitation to this study is the inaccuracy of pregnancy dating, which is common in low-resource countries and may explain the high proportion of infants >2500 g birth weight. We cannot exclude the possibility that term infants were enrolled. The trial was not powered to detect a difference between the groups with regard to the secondary outcomes. The birth weight and gestational age entry criteria allowed us to enroll infants with a low prevalence of these outcomes and therefore we have to conclude that these data do not provide evidence of treatment effect on these clinical outcomes. These outcomes were used as safety measures. The decision to admit an infant to the NICU was made shortly after birth, largely related to the birth weight or respiratory status. Thus, the admission rate is unlikely to be dependent on the trial intervention.
Another limitation is the lack of control of the environmental temperature in the delivery rooms and resuscitation areas. The hospital did not have central air-conditioning or heating, and strict control of the ambient temperature was not possible. This could affect the infants’ temperatures31 and the study could not control for it. However, even though ambient temperature can affect the temperature of the newborn, the plastic bags were able to reduce hypothermia without causing hyperthermia in this stressful environment. Infants were dried at birth per WHO guidelines, but this may not be necessary when plastic bags are used.20–24
Just as we found in the current trial, hyperthermia has not been reported in previous randomized controlled trials of plastic wrappings.20,21,24 Furthermore, there is in vitro evidence that indicates that plastic bags should not cause hyperthermia.32
We studied plastic bags against normal thermoregulation practices, not against skin-to-skin contact with the mother, specifically because preterm and low birth weight infants frequently have to be separated from their mothers soon after birth. Data have been published regarding the thermoregulation benefits of skin-to-skin contact with the mother.33,34 The WHO Essential Newborn Care curriculum includes skin-to-skin contact with the mother in the first few hours after birth for thermoregulation and early breast feeding.35 However, in a large study, hypothermia occurred in 43% and 49% of normal birth weight and low birth weight infants despite a 75% rate of skin-to-skin contact with the mother during the first 24 hours after birth.36
The use of plastic bags or polyethylene wrapping in very low birth weight infants in the delivery room is a common practice in the developed world. Previous studies have shown that plastic bags or wrappings reduce hypothermia in infants at <29 weeks’ gestation.21,24 Although infants down to 26 weeks and 1000 g were included in our trial, they constituted a small proportion of the enrolled infants. Larger infants also have trouble maintaining a normal temperature in the early minutes to hours after birth, and the current trial demonstrates that plastic bags may also reduce hypothermia in these infants. The relatively high prevalence of hypothermia, even in the larger infants enrolled in the current trial suggests that these infants may benefit from placement inside a plastic bag shortly after birth.
There are limited data from high-level evidence studies on thermoregulation in preterm/low birth weight infants in developing countries. A randomized controlled trial, which enrolled 110 infants of 24 to 34 weeks’ gestation in a NICU in Malaysia, showed that although plastic wrapping increased temperatures, 78% of the infants in the treatment group became hypothermic even though the incidence of hypothermia was slightly reduced.37
Hypothermia has long been linked to an increased risk of mortality.1,3,4,8,9,30 It is an accepted and logical standard of care in NICUs and labor wards around the world to provide thermal protection to newborns, and admission temperature can be used to gauge the success of resuscitation. Larger randomized controlled studies are needed to determine if improving the temperature immediately after birth improves any other long-term outcomes.
This randomized controlled trial supports the hypothesis that placement of preterm and low birth weight infants inside a plastic bag soon after birth reduces hypothermia and increases normothermia without causing hyperthermia or other complications. Because of the high rate of hypothermia in the population studied, these results may be most generalizable to populations with high rates of hypothermia. Placement of infants at birth in a plastic bag is a low-cost and promising intervention for infants born in limited-resource settings where there is limited availability of radiant warmers and incubators.
Acknowledgments
We thank Monica Collins RN, BSN, MaEd, and Becky Brazeel, CPS, CAP, from the University of Alabama at Birmingham; Clement C. Mwamba and Lydia Mapala from the University of Zambia; Franco Mudekwa from the Lusaka Nursing Institute; and all the nurse midwives at University Teaching Hospital in Lusaka for their help in completing this project.
Glossary
- WHO
World Health Organization
Footnotes
Dr Leadford conceptualized and designed the trial, implemented and carried out data collection, analyzed and drafted the initial paper, and revised the final manuscript; Dr Warren designed the trial, and implemented and conducted data collection; Dr Manasyan designed, implemented, and carried out data collection; Drs Chomba and Schelonka designed the trial; Dr Salas designed the trial and conducted the analysis; Dr Carlo conceptualized and designed the trial, analyzed the results, drafted the initial paper, and revised the final manuscript; and all authors reviewed and approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01403623).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development Global Network for Women’s and Children’s Health Research (HD043464), Perinatal Health and Human Development Research Program of the University of Alabama at Birmingham, and Children’s of Alabama Centennial Scholar Fund. Funded by the National Institutes of Health (NIH).
References
- 1.Liu L, Johnson HL, Cousens S, et al. Child Health Epidemiology Reference Group of WHO and UNICEF . Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–2161 [DOI] [PubMed] [Google Scholar]
- 2.Lawn JE, Kerber K, Enweronu-Laryea C, Cousens S. 3.6 million neonatal deaths—what is progressing and what is not? Semin Perinatol. 2010;34(6):371–386 [DOI] [PubMed] [Google Scholar]
- 3.Silverman WA, Fertig JW, Berger AP. The influence of the thermal environment upon the survival of newly born premature infants. Pediatrics. 1958;22(5):876–886 [PubMed] [Google Scholar]
- 4.Day RL, Caliguiri L, Kamenski C, Ehrlich F. Body temperature and survival of premature infants. Pediatrics. 1964;34:171–181 [PubMed] [Google Scholar]
- 5.Klaus MH, Fanaroff AA. Care of the High-Risk Neonate. 6th ed. St. Louis, MO: W. B. Saunders Company; 2001 [Google Scholar]
- 6.Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Neonatal hypothermia and associated risk factors among newborns of southern Nepal. BMC Med. 2010;8:43 [DOI] [PMC free article] [PubMed]
- 7.Laptook AR, Salhab W, Bhaskar B, Neonatal Research Network . Admission temperature of low birth weight infants: predictors and associated morbidities. Pediatrics. 2007;119(3). Available at: www.pediatrics.org/cgi/content/full/119/3/e643 [DOI] [PubMed] [Google Scholar]
- 8.Kambarami R, Chidede O. Neonatal hypothermia levels and risk factors for mortality in a tropical country. Cent Afr J Med. 2003;49(9-10):103–106 [PubMed] [Google Scholar]
- 9.Sodemann M, Nielsen J, Veirum J, Jakobsen MS, Biai S, Aaby P. Hypothermia of newborns is associated with excess mortality in the first 2 months of life in Guinea-Bissau, West Africa. Trop Med Int Health. 2008;13(8):980–986 [DOI] [PubMed] [Google Scholar]
- 10.Kumar V, Shearer JC, Kumar A, Darmstadt GL. Neonatal hypothermia in low resource settings: a review. J Perinatol. 2009;29(6):401–412 [DOI] [PubMed] [Google Scholar]
- 11.Hill JR, Rahimtulla KA. Heat balance and the metabolic rate of new-born babies in relation to environmental temperature; and the effect of age and of weight on basal metabolic rate. J Physiol. 1965;180(2):239–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bissinger RL, Annibale DJ. Thermoregulation in very low-birth-weight infants during the golden hour: results and implications. Adv Neonatal Care. 2010;10(5):230–238 [DOI] [PubMed] [Google Scholar]
- 13.Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Risk of mortality associated with neonatal hypothermia in southern Nepal. Arch Pediatr Adolesc Med. 2010;164(7):650–656 [DOI] [PubMed] [Google Scholar]
- 14.Dahm LS, James LS. Newborn temperature and calculated heat loss in the delivery room. Pediatrics. 1972;49(4):504–513 [PubMed] [Google Scholar]
- 15.Byaruhanga R, Bergstrom A, Okong P. Neonatal hypothermia in Uganda: prevalence and risk factors. J Trop Pediatr. 2005;51(4):212–215 [DOI] [PubMed] [Google Scholar]
- 16.Moss W, Darmstadt GL, Marsh DR, Black RE, Santosham M. Research priorities for the reduction of perinatal and neonatal morbidity and mortality in developing country communities. J Perinatol. 2002;22(6):484–495 [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization, Department of Reproductive Health and Research. Thermal Protection of the Newborn: A Practical Guide. Geneva, Switzerland. 1997. [Google Scholar]
- 18.Hammarlund K, Nilsson GE, Oberg PA, Sedin G. Transepidermal water loss in newborn infants. V. Evaporation from the skin and heat exchange during the first hours of life. Acta Paediatr Scand. 1980;69(3):385–392 [DOI] [PubMed] [Google Scholar]
- 19.MacDonald MG, Mullett MD, Seshia MM. Avery’s Neonatalogy, Pathophysiology and Management of the Newborn. 6th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2005 [Google Scholar]
- 20.Vohra S, Frent G, Campbell V, Abbott M, Whyte R. Effect of polyethylene occlusive skin wrapping on heat loss in very low birth weight infants at delivery: a randomized trial. J Pediatr. 1999;134(5):547–551 [DOI] [PubMed] [Google Scholar]
- 21.Vohra S, Roberts RS, Zhang B, Janes M, Schmidt B. Heat Loss Prevention (HeLP) in the delivery room: a randomized controlled trial of polyethylene occlusive skin wrapping in very preterm infants. J Pediatr. 2004;145(6):750–753 [DOI] [PubMed] [Google Scholar]
- 22.Cramer K, Wiebe N, Hartling L, Crumley E, Vohra S. Heat loss prevention: a systematic review of occlusive skin wrap for premature neonates. J Perinatol. 2005;25(12):763–769 [DOI] [PubMed] [Google Scholar]
- 23.Carroll PD, Nankervis CA, Giannone PJ, Cordero L. Use of polyethylene bags in extremely low birth weight infant resuscitation for the prevention of hypothermia. J Reprod Med. 2010;55(1-2):9–13 [PubMed] [Google Scholar]
- 24.Knobel RB, Wimmer JE, Jr, Holbert D. Heat loss prevention for preterm infants in the delivery room. J Perinatol. 2005;25(5):304–308 [DOI] [PubMed] [Google Scholar]
- 25.Baumgart S, Engle WD, Fox WW, Polin RA. Effect of heat shielding on convective and evaporative heat losses and on radiant heat transfer in the premature infant. J Pediatr. 1981;99(6):948–956 [DOI] [PubMed] [Google Scholar]
- 26.Baumgart S. Reduction of oxygen consumption, insensible water loss, and radiant heat demand with use of a plastic blanket for low-birth-weight infants under radiant warmers. Pediatrics. 1984;74(6):1022–1028 [PubMed] [Google Scholar]
- 27.McCall EM, Alderdice F, Halliday HL, Jenkins JG, Vohra S. Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. Cochrane Database Syst Rev. 2010;(3):CD004210. [DOI] [PubMed] [Google Scholar]
- 28.Kattwinkel J, ed. Neonatal Resuscitation. 6th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2011 [Google Scholar]
- 29.Perlman JM, Kattwinkel J, Richmond S, et al. International Liaison Committee on Resuscitation . The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: pediatric basic and advanced life support. Pediatrics. 2006;117(5). Available at: www.pediatrics.org/cgi/content/full/117/5/e955 [DOI] [PubMed] [Google Scholar]
- 30.Christensson K, Bhat GJ, Eriksson B, Shilalukey-Ngoma MP, Sterky G. The effect of routine hospital care on the health of hypothermic newborn infants in Zambia. J Trop Pediatr. 1995;41(4):210–214 [DOI] [PubMed] [Google Scholar]
- 31.Mullany LC, Katz J, Khatry SK, Leclerq SC, Darmstadt GL, Tielsch JM. Incidence and seasonality of hypothermia among newborns in southern Nepal. Arch Pediatr Adolesc Med. 2010;164(1):71–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agourram B, Bach V, Tourneux P, Krim G, Delanaud S, Libert JP. Why wrapping premature neonates to prevent hypothermia can predispose to overheating. J Appl Physiol. 2010;108(6):1674–1681 [DOI] [PubMed] [Google Scholar]
- 33.Conde-Agudelo A, Belizán JM, Diaz-Rossello J. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst Rev. 2011;(3):CD002771. [DOI] [PubMed] [Google Scholar]
- 34.Moore ER, Anderson GC, Bergman N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2007;(3):CD003519. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization, Department of Reproductive Health and Research. Essential newborn care. Geneva, Switzerland. 2010. Available at: www.who.int/maternal_child_adolescent/documents/newborncare_course/en/index.html. Accessed April 30, 2013
- 36.Darmstadt GL, Kumar V, Yadav R, et al. Introduction of community-based skin-to-skin care in rural Uttar Pradesh, India. J Perinatol. 2006;26(10):597–604 [DOI] [PubMed] [Google Scholar]
- 37.Rohana J, Khairina W, Boo NY, Shareena I. Reducing hypothermia in preterm infants with polyethylene wrap. Pediatr Int. 2011;53(4):468–474 [DOI] [PubMed] [Google Scholar]