Abstract
Objective
Physicians’ negative attitudes towards patients with obesity are well documented. Whether or how these beliefs may affect patient-physician communication is unknown. We aimed to describe the relationship between patient BMI and physician communication behaviors (biomedical, psychosocial/lifestyle, and rapport building) during typical outpatient primary care visits.
Design and Methods
Using audio-recorded outpatient encounters from 39 urban PCPs and 208 of their patients, we examined the frequency of communication behaviors using the Roter Interaction Analysis System. The independent variable was measured patient BMI and dependent variables were communication behaviors by the PCP within the biomedical, psychosocial/lifestyle, and rapport building domains. We performed a cross-sectional analysis using multilevel Poisson regression models to evaluate the association between BMI and physician communication.
Results
PCPs demonstrated less emotional rapport with overweight and obese patients (IRR 0.65, 95%CI 0.48–0.88, p=0.01; IRR 0.69, 95%CI 0.58–0.82, p<0.01, respectively) than for normal weight patients. We found no differences in PCPs’ biomedical or psychosocial/lifestyle communication by patient BMI.
Conclusions
Our findings raise the concern that low levels of emotional rapport in primary care visits with overweight and obese patients may weaken the patient-physician relationship, diminish patients’ adherence to recommendations, and decrease the effectiveness of behavior change counseling.
Keywords: Obesity, patient-provider, primary care, psychosocial research
Introduction
Patient-physician communication influences patient behavior (1), and good communication is essential to the patient-physician relationship. Studies have linked certain communication behaviors such as empathy, encouragement, and psychosocial talk with improved patient satisfaction and adherence (2). The physician’s attitude towards a patient influences how that physician communicates with that patient. For example, physicians who have less respect for particular patients provide less information and express a less positive affect (3). Obese patients may be particularly vulnerable to poor patient-physician communication, as prior studies have documented physicians’ negative attitudes towards patients with obesity (4–8). Physicians have less respect for obese patients (8), perceive obese patients as non-adherent to medications (6), and associate obesity with “laziness” and “worthlessness” (7). These attitudes may negatively influence how physicians communicate with their patients.
To date, the majority of literature examining physicians’ obesity bias relies on self-report by providers or patients (4–8). Self-reported measures may be subject to social desirability and recall bias. Whether these negative physician attitudes translate into measurable differences in communication and care is unclear, as we know of no studies to date that objectively examine whether physicians’ communication during clinical encounters differs with obese patients.
In this study, our aim was to describe the relationship between patient body mass index (BMI) and physician communication behaviors during typical outpatient primary care visits. We examined three well-established domains of medical interaction that relate to biomedical, psychosocial/lifestyle, and rapport building communication. We hypothesized that physicians would engage in more biomedical communication with obese patients, as obesity has been linked with increased number of comorbid conditions. We hypothesized that psychosocial/lifestyle communication would not be influenced by patient weight. Given the previous literature that documents physicians’ obesity bias, we hypothesized that visits with obese patients would reflect less positive and emotional engagement in rapport building communication.
Methods and Procedures
Design and Participants
We performed a cross-sectional analysis using audio recordings and baseline data from the Patient-Physician Partnership (Triple P) Study. The Triple P Study was a randomized controlled trial of a patient-physician communication intervention to improve patient adherence and blood pressure control (9). The study included urban, community-based primary care physicians (PCPs) seeing their established patients for routine follow up. PCPs were recruited from 15 practices in Baltimore, MD. Physicians had to see patients at least 20 hours per week and have no intention to leave the practice within 12 months of beginning of the patient recruitment period. Patients were recruited from the participating physicians’ panels. Patients had to be aged 18 years and older, have had an ICD9 diagnosis of hypertension in the preceding 12 months, and be able to provide contact information and consent to participate in the study. During the baseline assessment, a single outpatient encounter was audio-recorded for each patient. These visits were a part of ongoing clinical care, and not specifically scheduled for the study. In addition, both patients and physicians completed questionnaires that included demographic information. The baseline data was collected between 2003 and 2005.
The parent study included 42 physicians and 279 of their patients. For our analysis, we excluded any patients that did not have a recorded height or weight (n=9), those who did not have a patient encounter audio recorded (n=43), those who did not identify as black or white race (n=3), and underweight patients defined as a BMI<18.5 kg/m2 (n=1). We also excluded patients with encounters of unusually short or long visit duration, as we were concerned that these encounters might not represent a typical outpatient visit. We defined a short visit length as <5 minutes (n=7) and a long visit length as >30 minutes (n=8). Our final sample included 39 physicians and 208 of their patients.
The Johns Hopkins Institutional Review Board approved this study. Patients and providers provided written consent prior to inclusion in the study.
Measures
Our dependent variables were counts of physician communication behaviors expressed during a typical outpatient visit. To calculate these counts, the audiotapes of the patient encounters were analyzed using the Roter Interaction Analysis System (RIAS). RIAS is a coding system that assesses patient-physician communication with established reliability and validity (10). Trained coders assign each complete thought expressed by the patient or physician into 1 of 37 mutually exclusive and exhaustive codes. As in many other studies using the RIAS, a number of individual codes were combined into composites characterized by content domains: (a) biomedical as it relates to medical history, symptoms, therapeutic regimen and tests; (b) psychosocial/lifestyle as it relates to social relationships, psychological experiences, and lifestyle related habits and routines (e.g., diet, exercise, smoking, etc); and (c) rapport building communication related to positive, emotional, and social interaction. Codes can also be categorized in terms of interaction functions such as data gathering (open or closed questions), patient education and counseling, and rapport building. Table 1 displays the content domains and dialogue functions, as well as the RIAS codes and transcript examples. Additional information about the RIAS system can be found online (http://www.riasworks.com).
Table 1.
Physician communication behaviors with associated RIAS codes and examples
| Behaviors | RIAS Codes | Examples | |
|---|---|---|---|
| Biomedical | Medical Data Gathering |
|
“Are you having trouble with your breathing when you walk?” [Asks medical questions] |
| Medical Education and Counseling |
|
“Your blood pressure is elevated. I’m prescribing you a medication that you will take each day to control your blood pressure.” [Gives medical information] | |
| Psychosocial/Lifestyle | Psychosocial/Lifestyle Data Gathering |
|
“Do you have a regular exercise routine that you follow?” [Asks lifestyle questions] |
| Psychosocial/Lifestyle Education and Counseling |
|
“My favorite tip on eating healthier is that fruits and vegetables are delicious and should be eaten every day.” [Gives lifestyle information] | |
| Rapport Building | Positive Rapport Building |
|
“You are doing really well. Pretty soon, you’ll put me out of business.” [Compliments] |
| Emotional Rapport Building |
|
“I can see how frustrated you are by your slow progress – anyone would be.” [Empathy] | |
| Social Rapport Building |
|
“Did you see the football game last night?” [Social talk] |
We examined seven components of communication behavior within three content domains. The biomedical domain included two components: medical data gathering and medical education and counseling. The psychosocial/lifestyle domain similarly included related data gathering and patient education and counseling. The rapport building domain included three components: positive rapport building, emotional rapport building, and social rapport building. We also combined these three rapport building components to create an overall rapport building variable. These domains and components are well-established within the RIAS system, and have been used extensively in other health communication studies (3, 11–13).
The study’s independent variable was patient BMI, which was calculated using height and weight obtained from the medical chart. We categorized BMI into three groups according to the National Institutes of Health standards (14), which define normal range as 18.5–24.9 kg/m2, overweight as 25–29.9 kg/m2, and obese as ≥ 30 kg/m2.
We identified additional patient-related and physician-related variables that we used to characterize our study sample. Patient variables included age, sex, race, number of co-morbidities, depressive symptoms, physician familiarity with the patient, visit length, and race concordance with the physician. Race was dichotomized as black or white. Presence of depressive symptoms was defined as a CES-D score>16. Physician familiarity with the patient was assessed via a questionnaire that asked, “How well do you know this patient?” The responses were dichotomized as know very well/well or know less well. Physician covariates included age, sex, race, number of years in practice, and specialty. Physician race was categorized as black, white or other. Specialty was categorized as general internist, family practice, or general practitioner.
Statistical Analyses
Descriptive analyses of all variables were performed. Bivariate analyses of patient and physician characteristics by BMI category were performed using the adjusted Wald test for continuous variables or Pearson’s χ2 test for dichotomous or categorical variables. To assess how representative our sample was with the overall sample in the parent study, we compared patient and physician characteristics between our sample and the overall study sample using adjusted Wald test for continuous variables or Pearson’s χ2 test for dichotomous or categorical variables. We explored the distribution of counts for each communication behavior by creating box plots for the overall sample.
To account for clustering of patients by physician, we used multilevel Poisson regression models to evaluate the association between BMI and each component of physician communication. To best account for over-dispersion of variance at the patient level (level 1), we used the sandwich estimator for the standard errors with the multilevel Poisson model (15). The base models were adjusted for the number of co-morbidities and physician familiarity with the patient, as these variables were significantly different between BMI groups in the bivariate analyses. The base models were also adjusted for visit length, which influences the opportunity that physicians may have to engage in different types of communication (16). In the full models, we adjusted for all variables in the base model, as well as additional patient covariates that have been previously linked with differences in physician communication including patient age, patient race, patient sex, and depressive symptoms (3, 11–13). We found no difference in race concordance by BMI group, so we did not include it in the full model. We did a sensitivity analysis adding race concordance to the full model, which did not change results.
Results
The study sample included 39 urban primary care physicians and 208 of their patients. Table 2 shows the characteristics of physicians in our sample. There were no significant differences in physician characteristics by patient BMI group. Overall, patients’ mean age was 62.1 years (SD 12.3) with 65% female and 59% black. Patients’ mean BMI was 32.7 kg/m2 (SD 7.9). Table 3 shows the distribution of patient characteristics by BMI group. Overweight and obese patients had more co-morbid conditions (p=0.05) and were known less well by their physicians (p=0.03) as compared to normal weight patients. We found no significant differences between our sample for analysis and the overall study sample.
Table 2.
Physician characteristics for study sample
| Physicians (n=39) | |
|---|---|
| Age in years | |
| Mean (SD) | 42.9 (8.7) |
|
| |
| Sex | |
| Female | 21 (53%) |
|
| |
| Race | |
| White | 18 (45%) |
| Black | 10 (25%) |
| Asian | 12 (30%) |
|
| |
| Specialty | |
| Internal Medicine | 32 (82%) |
| Family Practice | 6 (15%) |
| General Practitioner | 1 (3%) |
|
| |
| Years in practice | |
| Mean (SD) | 11.2 (7.7) |
|
| |
| Number of patients | |
| Mean (SD) | 5.3 (3.4) |
Table 3.
Characteristics for normal range, overweight and obese patients in study sample
| Normal Range | Overweight | Obese | p-valuea | |
|---|---|---|---|---|
| BMI 18.5–24.9 kg/m2 (n=28) | BMI 25–29.9 kg/m2 (n=60) | BMI ≥30 kg/m2 (n=120) | ||
| Age in years | ||||
| Mean (SD) | 62.8 (12.5) | 64.2 (11.1) | 61.0 (12.7) | 0.41 |
|
| ||||
| Sex | ||||
| Female | 20 (71%) | 37 (62%) | 77 (64%) | 0.67 |
|
| ||||
| Race | ||||
| Black | 18 (64%) | 32 (53%) | 74 (62%) | 0.49 |
|
| ||||
| Education | ||||
| High school grad | 18 (64%) | 46 (77%) | 86 (72%) | 0.48 |
|
| ||||
| Insurance status | ||||
| Uninsured | 2 (7%) | 6 (10%) | 12 (10%) | 0.89 |
|
| ||||
| Number of co-morbid conditions | ||||
| 1–3 | 13 (48%) | 36 (63%) | 52 (44%) | 0.05 |
| ≥4 | 14 (52%) | 21 (37%) | 67 (56%) | |
|
| ||||
| Physician familiarity with the patient | ||||
| Know very well | 27 (96%) | 43 (72%) | 91 (76%) | 0.03 |
| or well | ||||
|
| ||||
| Depressive symptoms | ||||
| CES-D>16 | 8 (31%) | 12 (20%) | 37 (32%) | 0.28 |
|
| ||||
| Visit length in minutes | ||||
| Mean (SD) | 15.8 (5.1) | 14.5 (5.7) | 15.1 (5.6) | 0.41 |
|
| ||||
| Race concordance with physician | ||||
| Race concordant | 11 (39%) | 26 (43%) | 57 (48%) | 0.69 |
BMI, body mass index; CES-D, Centers for Epidemiologic Studies Depression Scale
p-value calculated using an adjusted Wald test for continuous variables and a Pearson’s χ2 for dichotomous and categorical variables.
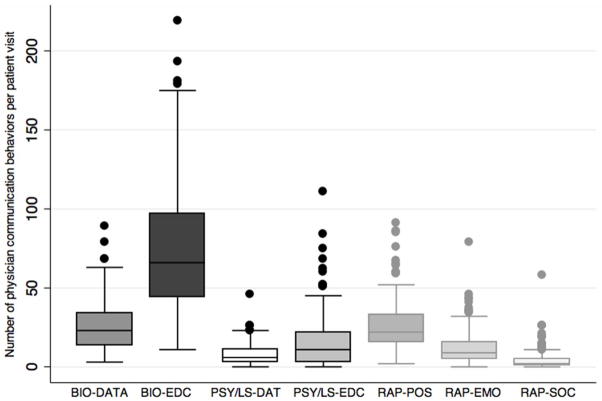
Figure 1 shows the box plots that illustrate the distribution of the physician communication behaviors. Overall, medical education and counseling dominated the discussion during the patient visits, while the rates of psychosocial/lifestyle data gathering and social rapport building were low.
Figure 1.
This figure illustrates the distribution of the physician communication behaviors in our overall sample. The box plots show the 25th percentile (Q1), median (Q2), and 75th percentile (Q3) for each communication behavior. The whiskers represent the 5th and 95th percentiles, and dots show all outliers. Communication behaviors are abbreviated as follows: BIO-DATA Biomedical data gathering; BIO-EDC Biomedical education and counseling; PSY/LS-DATA Psychosocial/lifestyle data gathering; PSY/LS-EDC Psychosocial/lifestyle education and counseling; RAP-POS Positive rapport building; RAP-EMO Emotional rapport building; RAP-SOC Social rapport building.
Table 4 shows the incidence rate ratios for the association of BMI with the physician communication behaviors for the full models. The results for all base models (data not displayed) were similar to the results of the full models shown in Table 4. There were no significant differences in any elements of physician biomedical or psychosocial/lifestyle communication behaviors, although physicians’ increased biomedical data gathering with obese patients approached statistical significance (IRR 1.20, 95%CI 0.99–1.46, p=0.06). Physicians’ built significantly less emotional rapport with the overweight and obese groups (IRR 0.65, 95%CI 0.48–0.88, p=0.01; IRR 0.69, 95%CI 0.58–0.82, p<0.01, respectively), but no differences were found in positive or social rapport. We also examined overall rapport by patient weight and found that physicians’ engaged in significantly less rapport building overall with overweight and obese patients (full model: IRR 0.80, 95%CI 0.70–0.91, p<0.01; IRR 0.85, 95%CI 0.75–0.97, p=0.01, respectively).
Table 4.
Incidence rate ratiosa of physician communication behaviors between overweight and obese patients compared to normal weight patients
| IRR (95% CI) | ||||
|---|---|---|---|---|
| Normal Range | Overweight | Obese | ||
| BMI 18.5–24.9 kg/m2 (n=28) | BMI 25–29.9 kg/m2 (n=60) | BMI ≥30 kg/m2 (n=120) | ||
| Biomedical | Medical Data Gathering | 1.00 | 1.18 (0.94–1.47) p=0.15 |
1.20 (0.99–1.46) p=0.06 |
|
| ||||
| Medical Education and Counseling | 1.00 | 1.08 (0.87–1.33) p=0.50 |
1.00 (0.81–1.22) p=0.99 |
|
|
| ||||
| Psychosocial/Lifestyle | Psychosocial/Lifestyle Data Gathering | 1.00 | 0.78 (0.53–1.15) p=0.21 |
0.82 (0.57–1.19) p=0.30 |
|
| ||||
| Psychosocial/Lifestyle Education and Counseling | 1.00 | 1.00 (0.66–1.53) p=0.98 |
0.88 (0.58–1.33) p=0.54 |
|
|
| ||||
| Rapport Building | Positive Rapport Building | 1.00 | 0.92 (0.81–1.05) p=0.22 |
0.96 (0.85–1.08) P=0.48 |
|
| ||||
| Emotional Rapport Building | 1.00 | 0.65 (0.48–0.88) p=0.01 |
0.69 (0.58–0.82) p<0.01 |
|
|
| ||||
| Social Rapport Building | 1.00 | 0.62 (0.34–1.11) p=0.11 |
0.86 (0.43–1.70) p=0.66 |
|
IRR, incidence rate ratio; BMI, body mass index
Multilevel Poisson regression model adjusted for patient age, sex, race, depressive symptoms, number of co-morbidities, physician familiarity with the patient, and visit length.
Discussion
Our study raises the question of what should be considered optimal communication between physicians and their obese patients. Physicians must balance the use of biomedical communication that is essential in the medical management of obesity-related chronic diseases with the demands for psychosocial/lifestyle communication to enact the U.S. Preventive Services Task Force (USPSTF) guidelines to counsel obese patients to lose weight (17). In addition, physicians must include rapport building to support the patients’ behavior changes required to manage comorbidities and lose weight. Caring for obese patients presents a challenge for physicians on how to prioritize biomedical, psychosocial/lifestyle, and rapport building communication during the limited time allotted for a typical outpatient visit.
In our study, we found that physicians’ focused predominantly on biomedical communication regardless of patient BMI. The duration of the outpatient visits also did not differ significantly by patient BMI. Previous studies have reported that physicians may feel overwhelmed by the multi-morbidity associated with obesity (18–20), so we found it surprising that physicians in our sample did not spend more time with obese patients or engage them in more biomedical communication to address multi-morbidity. We found that the obese patients in our sample had a greater number of co-morbid conditions as compared to normal weight patients; yet providers did not pay increased attention to education and counseling of these patients in regard to medical conditions or therapeutic regimens. Moreover, we found that psychosocial/lifestyle communication comprised less of the physician dialogue regardless of patient BMI. It is unclear whether equal rates of psychosocial/lifestyle communication should be considered ideal. Given that all patients in our sample had hypertension, all would warrant some lifestyle counseling regardless of weight. Therefore, our observed equal rates of psychosocial/lifestyle communication in this sample may be interpreted as equal treatment rather than a communication or relationship disparity attributable to obesity bias. In a general population, it may be reasonable to consider increased rates of psychosocial/lifestyle communication ideal for obese patients, given the USPSTF guidelines encouraging providers to perform weight loss counseling that incorporates both lifestyle and related psychosocial issues to obese patients (17).
In regards to rapport, physicians engaged most in positive rapport building and least often in social rapport building, neither of which differed by patient BMI. However, we did find that physicians were significantly less likely to build emotional rapport with overweight and obese patients. Given the lower levels of emotional rapport building with these patients, we have concerns about the nature of the relationships between overweight and obese patients with their physicians. Emotional rapport building includes statements of empathy, legitimation, concern, reassurance, partnership, and self-disclosure, which is considered essential to creating a patient-centered experience (21). Elements of emotional rapport including empathy, reassurance, listening, shared decision making, and patient centeredness have more often been linked with improved patient satisfaction and adherence, as compared to positive or social rapport elements (2). Empathy has also been associated with improved clinical outcomes (22), fewer malpractice claims (23), and decreased physician burnout (24). In light of the burgeoning obesity epidemic, patients want and need help from their primary care physicians in the complex and difficult realm of lifestyle change and weight management. Previous studies have found that patients were more likely to change their dietary habits, increase exercise and attempt to lose weight when their physicians expressed more empathy (25–26), which is a key component of emotional rapport. Patients want information and treatment, but they also need the emotional support and attention that could support them through the challenges that accompany weight loss and the establishment of a healthy lifestyle.
Given the importance of emotional rapport building in lifestyle behavior change, our results raise the question of why physicians are not engaging in this behavior. The lower rates of emotional rapport may reflect negative attitudes that physicians hold towards obese patients (6–8). Another study found that obesity was a patient characteristic that elicited negative feelings from primary care providers (27). These negative feelings may interfere with primary care providers’ willingness or ability to engage on an emotional level with these patients. In our study, physicians were more likely to report that they were less familiar with their obese patients than those of normal weight, which may further support the notion that these patient-physician relationships operate at an emotional distance. Future studies should evaluate whether differences in communication are linked with negative physician attitudes towards patients with obesity.
Our study has several limitations. First, our results may not generalize to all overweight and obese patients, as our sample came from an urban, predominantly ethnic minority population. Second, we had a relatively small sample size, which may have impacted our power to detect more subtle differences in communication such as biomedical data gathering during visits with obese patients. Future studies should be designed to confirm our results, and be adequately powered to evaluate for such associations. As this study was a secondary analysis of previously collected data, we could not make such adjustments. Third, we did not collect information regarding the reason for the patient visit; however, we did adjust for co-morbidities, which likely minimized communication differences that might have occurred due to the reason for the visit. Fourth, we were unable to account for the duration of patient-physician relationship as a potential confounder. However, we adjusted our analyses for physician ratings of familiarity with the patient, which may be considered a subjective proxy for duration. Fifth, we did not directly evaluate physician obesity bias, so we could not determine whether physicians’ attitudes about obesity account for the differences in emotional rapport building identified in this study. Finally, unmeasured site characteristics, such as pre-established limits of time or resources to manage overweight and obese patients, may have affected our findings.
Notwithstanding these limitations, this study is the first examining physician communication behaviors by weight and highlights patient-physician communication as an important area for future investigation. Our study has several strengths, as we used an objective measure of BMI and a validated method of assessing patient-physician communication. Furthermore, our study may suggest communication skills training tailored to address obesity as an area for intervention development. In one study, communication skills training improved the rapport building capabilities of medical students (28). In another study, physicians who received communication skills training increased their rapport building, as well as other clinical behaviors such as screening rates for health behaviors such as smoking and depression (29). Another recent study designed and tested a general empathy training protocol with residents (30). After this training, residents were rated more highly empathic by patients. These studies were not specifically focused on expressing empathy or building rapport with obese patients; however, they demonstrate how protocols might be developed to foster emotional rapport building between physicians and patients. Future interventions may want to address communication and rapport building skills through continuing medical education training, as a possible means to improve patient-physician communication for patients with obesity.3
Acknowledgments
The Triple P study was supported by a grant from the National Heart, Lung, and Blood Institute (R01HL069403). The National Heart, Lung, and Blood Institute also provided support through the following grants: LAC by K24HL083113, and MCB by 5R01HL088511. KAG was supported by a training grant from the Health Resources and Service Administration (T32HP10025-16-00) and a trainee award from the National Heart, Lung, and Blood Institute Centers for Population Health and Health Disparities (P50HL0105187). We presented our results as an oral presentation, which was selected as a finalist for the Mack Lipkin Sr. Award at the 2011 national meeting of the Society of General Internal Medicine in Phoenix, AZ on May 6, 2011. In addition, we presented our results as a poster at the International Conference on Communication in Healthcare in Chicago, IL on October 16, 2011.
Footnotes
Disclosure
The authors declare no conflicts of interest.
References
- 1.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 2.Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15:25–38. [PubMed] [Google Scholar]
- 3.Beach MC, Roter DL, Wang NY, Duggan PS, Cooper LA. Are physicians’ attitudes of respect accurately perceived by patients and associated with more positive communication behaviours? Patient Educ Couns. 2006;62:347–54. doi: 10.1016/j.pec.2006.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 5.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 6.Huizinga MM, Bleich SN, Beach MC, Clark JM, Cooper LA. Disparity in physician perception of patients’ adherence to medications by obesity status. Obesity (Silver Spring) 2010;18:1932–7. doi: 10.1038/oby.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwartz MB, Chambliss HO, Brownell KD, Blair DN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–1039. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- 8.Huizinga MM, Cooper LA, Bleich SN, Clark JM, Beach CM. Physician respect for patients with obesity. J Gen Intern Med. 2009;24:1236–1239. doi: 10.1007/s11606-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper LA, Roter DL, Bone LR, et al. A randomized controlled trial of interventions to enhance patient-physician partnership, patient adherence and high blood pressure control among ethnic minorities and poor persons: study protocol NCT00123045. Implement Sci. 2009;4:7. doi: 10.1186/1748-5908-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46:243–51. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- 11.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139:907–15. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 12.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–90. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beach MC, Saha S, Korthuis PT, et al. Differences in patient-provider communication for Hispanic compared to non-Hispanic white patients in HIV care. J Gen Intern Med. 2010;25:682–7. doi: 10.1007/s11606-010-1310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NHLBI Obesity education initiative expert panel. [accessed October 24, 2011];Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. 1998 Sep; NIH publication No. 98-4083. http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf.
- 15.Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using Stata. Stata Press; College Station, Texas: 2008. pp. 394–5. [Google Scholar]
- 16.Deveugele M, Derese A, De Bacquer D, van den Brink-Muinen A, Bensing J, De Maeseneer J. Consultation in general practice: a standard operating procedure? Patient Educ Couns. 2004;54:227–33. doi: 10.1016/S0738-3991(03)00239-8. [DOI] [PubMed] [Google Scholar]
- 17.McTigue KM, Harris R, Hemphill B, et al. Screening and interventions for obesity in adults: summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;139:933–49. doi: 10.7326/0003-4819-139-11-200312020-00013. [DOI] [PubMed] [Google Scholar]
- 18.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24:546–52. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 19.Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians’ weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79:156–61. doi: 10.1097/00001888-200402000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Alexander SC, Ostbye T, Pollak KI, Gradison M, Bastian LA, Brouwer RJ. Physicians’ beliefs about discussing obesity: results from focus groups. Am J Health Promot. 2007;21:498–500. doi: 10.4278/0890-1171-21.6.498. [DOI] [PubMed] [Google Scholar]
- 21.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. National Academies Press; Washington, DC: 2001. [PubMed] [Google Scholar]
- 22.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz CG. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–64. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 23.Hickson GB, Federspiel CF, Pichert JW, Miller CS, Gauld-Jaeger J, Bost P. Patient complaints and malpractice risk. J Am Med Assoc. 2002;287:2951–7. doi: 10.1001/jama.287.22.2951. [DOI] [PubMed] [Google Scholar]
- 24.Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. J Am Med Assoc. 2009;302:1284–93. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 25.Pollak KI, Ostebye T, Alexander SC, et al. Empathy goes a long way in weight loss discussions. J Fam Pract. 2007;56:1031–6. [PubMed] [Google Scholar]
- 26.Cox ME, Yancy WS, Coffman CJ, et al. Effects of counseling techniques on patients’ weight-related attitudes and behaviors in a primary care clinic. Patient Educ Couns. 2011 doi: 10.1016/j.pec.2011.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klein D, Najman J, Kohrman AF, Munro C. Patient characteristics that elicit negative response from family physicians. J Fam Pract. 1982;14:881–8. [PubMed] [Google Scholar]
- 28.Windish DM, Price EG, Clever SL, Magaziner JL, Thomas PA. Teaching medical students the important connection between communication and clinical reasoning. J Gen Intern Med. 2005;20:1108–13. doi: 10.1111/j.1525-1497.2005.0244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zabar S, Hanley K, Stevens DL, et al. Can interactive skills-based seminars with standardized patients enhance clinicians’ prevention skills? Measure the impact of a CME program. Patient Educ Couns. 2010;80:248–52. doi: 10.1016/j.pec.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 30.Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27:1280–6. doi: 10.1007/s11606-012-2063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]