Abstract
Objective
Define surgical outcomes of specific donor sites for free tissue transfer in head and neck reconstruction.
Design
Retrospective cohort review
Setting
Academic tertiary care center.
Patients
A review of free tissue transfer procedures performed at a university-based tertiary care facility from October 2004 to April 2011. A total of 1051 patients underwent 6 types of free flaps: fasciocutaneous radial forearm (53%), osteocutaneous radial forearm (16%), rectus abdominus (11%), fibula (10%), anterior lateral thigh (7%), and latissimus dorsi (2%).
Main Outcome Measures
Demographic data was collected and outcomes measured were: length of hospital stay, flap viability, and major complications (infection, fistula, and hematoma).
Results
Of the 1051 flaps performed, the most common operative site was oral cavity (40% n=414) followed by hypopharynx/larynx (22%, n=234), cutaneous (20%, n=206), oropharynx (9%, n= 98), mid-face (7%, n= 76), and skull base (2%, n=23). The median hospital stay was 7.9 days (range 1-76) and the overall failure rate was 2.8%. Cutaneous defects required the shortest length of hospitalization (5.8 days, P< .0001), a low free flap failure rate (1.5%, n= 3), and limited major complications (6%, n= 12). Conversely, oropharynx defects were associated with the longest hospitalization (8.9 days). While midface defects had a high incidence of complications (15%, n= 11, P=.10). Defects above the angle of the mandible had higher overall complications when compared to below. Similarly, reconstruction for primary or recurrent cancer had a total failure rate of 2.5% while secondary reconstruction and radionecrosis had a failure rate of 4.0% (P=.29). Additionally, there was no statistical difference between outcomes based on donor site.
Conclusions
This review demonstrates that certain subsets of patients are at higher risk for complications after free tissue transfer. Patients undergoing free flap reconstruction for cutaneous defects have substantially shorter hospital stays and are at lower risk of flap complications, while reconstruction for radionecrosis or secondary reconstruction tend to have higher overall flap failure rates.
Keywords: Reconstruction, head and neck, free flap, outcomes
INTRODUCTION
Since the development of free tissue transfer and microsurgical techniques in the 1980s, microvascular free flap tissue transfers have largely become the gold standard for reconstruction of complex head and neck defects.1-3 One distinct advantage of free tissue transfer is its utility (surface area, volume, vascularity, diversity of tissue type) when compared to local or regional tissue transfer. As a result, a large variety of defect dimensions and locations can be reconstructed, allowing for larger oncologic resections, improved tissue coverage and lower patient morbidity.
Over time, there have been significant changes in reconstructive techniques, with gravitation towards a narrower set of donor sites and a reduction in complication rates.4,5 The selection and outcomes of free tissue transfers in head and neck reconstructions were evaluated in this study. Outcomes were based on donor and recipient site, indication for reconstruction, and the use of an osteocutaneous versus a fasciocutaneous transfer. Despite the widespread use of this technique in the head and neck, not all free flap donor sites or recipient sites are equivalent. Furthermore, a single percentile to describe failure rates is misleading. We evaluated patients who presented for a microvascular free flap reconstruction of a complex head and neck defect in order to better understand the potential risks and benefits of each type of free tissue transfer.
METHODS
Patient Selection
Institutional review board approval was obtained for review of a prospectively compiled database. All patients who presented between October 2004 and April 2011 for a microvascular free flap reconstruction of a head and neck defect were included (n=1051). The selection of the donor site depended on the defect (cutaneous, soft tissue, or bone), patient comorbidities (diabetes mellitus, cardiac disease, immunosuppression), and surgeon preference. Demographic characteristics examined included: surgical indication, duration of hospital stay, and complications. Complications were classified as either microvascular (partial or total flap loss) or non-microvascular complications (infection requiring surgical intervention, donor or recipient site hematoma, and fistula formation). Additional comorbidities were not analyzed despite their known impact on complications and flap outcome.
Statistical Analyses
Descriptive variables were summarized by mean (± SD) for continuous variables and %, n for categorical variables. A student’s t-test was used to compare differences in means between groups. A one-way ANOVA was used to analyze relationships between categorical factors and continuous responses. A contingency analysis was used to analyze relationships between categorical factors and responses. Univariate analyses were performed using the Pearson bivariate correlation coefficient. Multivariate analyses were performed to analyze the combined effects of multiple variables on various outcomes. A P-value of < .05 was considered statistically significant. Statistical analysis was performed using Jmp 9.0.2 software (SAS, Cary, NC).
RESULTS
Patient and Flap Characteristics
The mean age of the patients was 61.9 (range, 3-97) with the majority of the patients being male (74%, n=780). The vast majority of patients were Caucasian (81%, n=854), with the remaining being Black (18%, n=187) or Hispanic (1%, n=8). A total of 1051 microvascular free flap reconstructions were performed. Indications for reconstruction included defect following resection of a primary or recurrent malignancy (83%, n=876), a secondary reconstruction (14%, n=143), or radionecrosis (3%, n=32) (Table 1).
Table 1.
Patient characteristics.
| Characteristic | % (n=1051) |
|---|---|
| Age (range) | 61.9 (3-97) |
| Gender | |
| Male | 74 (780) |
| Female | 26 (26) |
| Race | |
| Caucasian | 81 (854) |
| Black | 18 (187) |
| Hispanic | 1 (8) |
| Other | 0.1 (2) |
| Surgical Indication | |
| Primary Lesion | 40 (421) |
| Recurrent Lesion | 43 (455) |
| Secondary Reconstruction | 14 (143) |
| Osteoradionecrosis | 3(32) |
The most common defect site was the oral cavity (40%, n=414), followed by hypopharynx/larynx (22%, n=234), cutaneous (20%, n=206), oropharynx (9%, n= 98), mid-face (7%, n= 76), and skull base (2%, n=23) (Table 2). The distribution of microvascular free flaps used for reconstruction of the defects was as follows: fasciocutaneous radial forearm (53%, n=557), osteocutaneous radial forearm (16%, n=163), myocutaneous vertical rectus abdominus (11%, n=120), osteocutaneous fibula (10%, n=109), myocutaneous anterior lateral thigh (7%, n=77), and myofascial latissimus dorsi (2%, n=25) (Figure 1). There was a significant correlation between the type of free flap used for the reconstruction and the location of the defect (P<.0001). The majority of myofascial latissimus dorsi (92%, n=23) and myocutaneous anterior lateral thigh (53%, n=41) free flaps were used to construct cutaneous defects, while the majority of osteocutaneous radial forearm (60%, n=98) and fibular (99%, n=108) free flaps were used to reconstruct oral cavity defects. The majority of fasciocutaneous radial forearm free flaps were used for reconstruction of the hypopharynx/larynx (37%, n=206) and the oral cavity (28%, n=158). Finally, the myocutaneous vertical rectus abdominis free flap was most commonly used for reconstruction of oral cavity (30%, n=36) and cutaneous (28%, n=33) defects. Stratification by defect subsite showed that fasciocutaneous radial forearm free flap was the most common donor site for cutaneous (48%, n=98), oral cavity (38%, n=158), oropharynx (75%, n=73), hypopharynx/larynx (88%, n=206), and skull base (52%, n=12) defects. The most likely free flap for reconstruction of midface defects was the osteocutaneous radial forearm free flap (62%, n=98).
Table 2.
Characteristics of microvascular free flap reconstructions.
| % (n) | Total 100 (1051) |
LD 2 (25) |
VRAM 11 (120) |
RFFF 53 (557) |
OCRFFF 16 (163) |
F 10 (109) |
ALT 7 (77) |
|---|---|---|---|---|---|---|---|
| Defect Site | |||||||
| Cutaneous | 20 (206) | 92 (23) | 28 (33) | 18 (98) | 6 (10) | 1 (1) | 53 (41) |
| Midface | 7 (76) | - | 12.5 (15) | 2 (10) | 29 (47) | - | 5 (4) |
| Oral Cavity | 40 (414) | - | 30 (36) | 28 (158) | 60 (98) | 99 (108) | 18 (14) |
| Oropharynx | 9 (98) | - | 13 (16) | 13 (73) | 2 (4) | - | 7 (5) |
| Hyopopharynx/ Larynx |
22 (234) | - | 12.5 (15) | 37 (206) | 1 (2) | - | 14 (11) |
| Skullbase | 2 (23) | 8 (2) | 4 (5) | 2 (12) | 1 (2) | - | 3 (2) |
LD, latissimus dorsi; VRAM, vertical rectus abdominis myocutaneous; RFFF, radial forearm free flap; OCRFFF, osteocutaneous radial forearm free flap; F, fibula; ALT, anterior lateral thigh.
Figure 1.
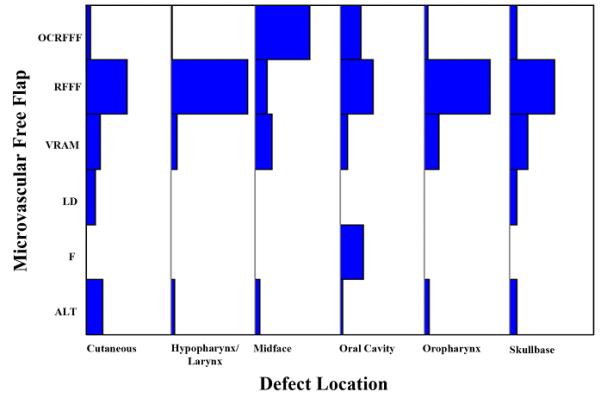
Distribution of microvascular free flaps by location of the defect.
LD, latissimus dorsi; VRAM, vertical rectus abdominis myocutaneous; RFFF, radial forearm free flap; OCRFFF, osteocutaneous radial forearm free flap; F, fibula; ALT, anterior lateral thigh.
A comparison of the patient ages stratified by ranges (Figure 2) and type of free flap used for the reconstruction was found to be significant (P<.0001). When a Student’s t-test was used to compare paired means of the patient ages, there was significant difference between fibular (57.2 years of age, ±15) and latissimus dorsi (69.5 years of age, ±12; P<.0001), anterior lateral thigh (65.6 years of age, ± 12; P<.0001), rectus abdominis (63 years of age, ± 12; P=.0006), and osteocutaneous radial forearm (62.9 years of age, ± 15; P=.0003). There was also a significant difference in the ages of patients being reconstructed with a latissimus dorsi free flap compared to fasciocutaneous radial forearm (61.4 years of age, ±12; P=.0017), osteocutaneous radial forearm (P=.016) and rectus abdominis (P=.018) free flap reconstructions. In addition, there was a significant difference in the ages of patients reconstructed with a fasciocuteanous radial forearm and anterior lateral thigh free flap (P=.006) (Figure 3).
Figure 2.
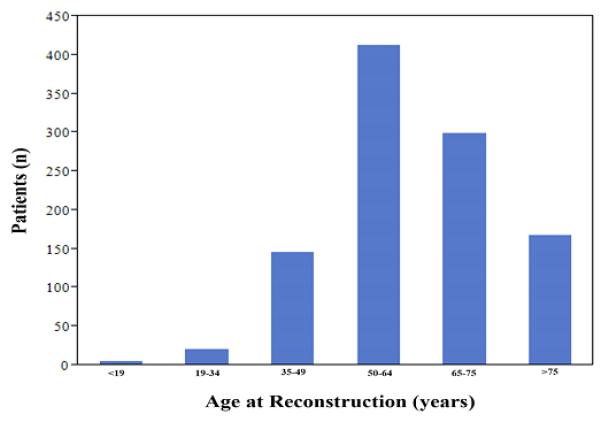
Distribution of patients according to their age at time of the reconstruction.
Figure 3.
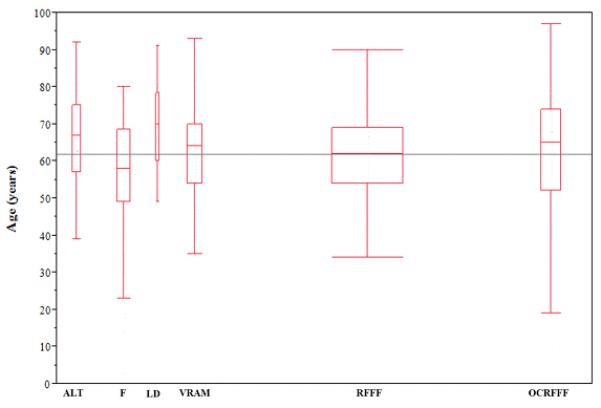
Age of patients undergoing microvascular free flap reconstructions.
LD, latissimus dorsi; VRAM, vertical rectus abdominis myocutaneous; RFFF, radial forearm free flap; OCRFFF, osteocutaneous radial forearm free flap; F, fibula; ALT, anterior lateral thigh.
Trends in microvascular reconstructions were observed over time (Figure 4). For analysis purposes, reconstructions performed in 2004 and 2011 were excluded since 12 months of data was not available for these two years. At our institution, there has been a reduction in anterior lateral thigh and fibular free flap reconstructions, with rectus abdominis and latissimus dorsi reconstructions remaining fairly consistent, and an increase in the fasciocutaneous and osteocutaneous radial forearm free flap reconstructions performed (Figure 4). These trends were found to be statistically significant on contingency analysis (P<.0001).
Figure 4.
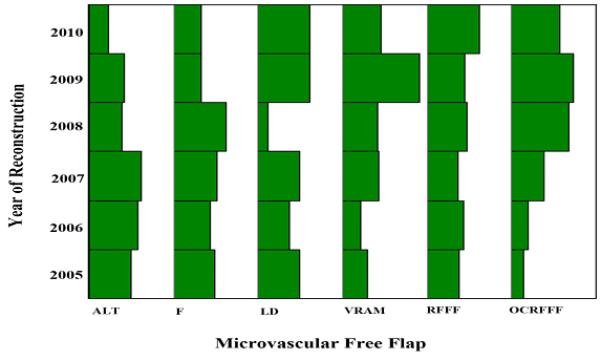
Trends in microvascular free flap reconstructions over time.
LD, latissimus dorsi; VRAM, vertical rectus abdominis myocutaneous; RFFF, radial forearm free flap; OCRFFF, osteocutaneous radial forearm free flap; F, fibula; ALT, anterior lateral thigh.
Length of Hospital Stay
The median length of hospital stay (LOS) was 7 days (range, 1-76) and the mean was 7.9 (±3.4). A comparison of LOS by location of the defects was found to the significantly different by one way ANOVA (P<.0001). Cutaneous defects required the shortest duration of hospitalization (5.8 d, P <.0001). Comparison of paired means by Student’s t-test found significant difference in LOS between cutaneous defects (5.8 d ±3.4) and defects of the midface (8.0 d ±6.0; P=.002.), oral cavity (8.2 d ±4.0; P<.0001), oropharynx (8.9 d ±5.0; P<.0001), hypopharynx/larynx (8.6 d ±7.2; P<.0001), and skull base (8.7 d ±3.7; P=.008).
A comparison of LOS by type of microvascular free flap used for reconstruction found no statistical difference by one way ANOVA (P =.35; Figure 5). However, when a Student’s t-test was used to compare paired means, there was a significant difference between LOS following an osteocutaneous fibular (8.8 d) and osteocutaneous radial forearm (7.4 d) free flap reconstruction (P =.035) and trended toward significance between osteocutaneous fibular and anterior lateral thigh (7.4 d ±5.7) free flap reconstruction (P =.064).
Figure 5. Length of hospitalization (≤ 30 days) by microvascular free flap reconstruction.
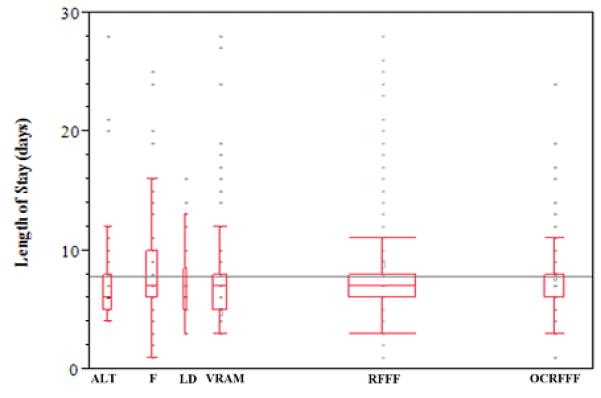
LD, latissimus dorsi; VRAM, vertical rectus abdominis myocutaneous; RFFF, radial forearm free flap; OCRFFF, osteocutaneous radial forearm free flap; F, fibula; ALT, anterior lateral thigh.
The age of the patients was found to not affect LOS (P=.39). An overall comparison of the LOS by the year of the reconstruction was not significant (P=0.34). However, when a Student’s t-test was used to compare paired means, there was noted to be a trend over time to sending patients home earlier. We noted a significant difference between LOS in 2009 (7.3 d ±3.9) and 2005 (8.5 d ±6.1; P=0.029) and 2006 (8.5 d ±5.2; P=.027), suggesting a reduction in hospital stay over time.
Microvascular Complications
A total flap loss occurred in 2.8% (n=29) of cases and a partial flap loss was seen in 1.0% (n=10) (Table 3). Flap failure rates did not differ by the type of microvascular free flap used for the reconstruction (P=.30). Flap survival was not affected by the location of the defect (P=.61) or patient age (P=.90). Total free flap failure rates were 3.2% for muscular free flaps (n=222), 2.9% for fasciocutaneous free flaps (n=557) or and 2.2% for osteocutaneous free flaps (n=272) (P=.79). Free flap reconstruction for defects that resulted from radionecrosis had higher free flap failure rates (6.3%, n=2), compared to repair of composite resections for malignancy (P=.04). Furthermore, reconstructions after composite resection for primary cancer (3.1%, n=13) or recurrence (2.0%, n=9) trended toward lower failure rate compared to secondary reconstructions (3.5%, n=5) (P=.06). However, there was no significant difference in free flap failure rates when stratified by cause of defect (P=.40).
Table 3.
Post-operative complications.
| Total % (n=1051) |
LD % (n=25) |
VRAM % (n=120) |
RFFF % (n=557) |
OCRFFF % (n=163) |
F % (n=109) |
ALT % (n=77) |
|
|---|---|---|---|---|---|---|---|
| None | 90 (943) | 88 (22) | 86 (103) | 90 (503) | 88 (143) | 91 (99) | 95 (73) |
| Major | 10 (108) | 12 (3) | 14 (17) | 10 (54) | 12 (20) | 9 (10) | 4 (4) |
| Flap Loss | |||||||
| Partial | 1 (10) | 0 (0) | 0 (0) | 0.5 (3) | 1 (2) | 4 (4) | 1 (1) |
| Complete | 3 (29) | 4 (1) | 3 (4) | 3 (16) | 3 (4) | 2 (2) | 3 (2) |
LD, latissimus dorsi; VRAM, vertical rectus abdominis myocutaneous; RFFF, radial forearm free flap; OCRFFF, osteocutaneous radial forearm free flap; F, fibula; ALT, anterior lateral thigh.
Non-Microvascular Complications
The non-free flap related surgical complication rate was 10%. This included hematoma formation (3%, n=30), recipient or donor site infection (4%, n=40), and fistula (3%, n=29). The incidence of a major complication was not affected by patient age (P=.65) or location of the defect (P=.10). The incidence of major complications stratified by donor site are as follows: myocutaneous rectus abdominis (14%, n=17) free flap, myofascial latissimus dorsi (12%, n=3), osteocutaneous radial forearm (12%, n=20), anterior lateral thigh (4%, n=77) and fibular (9%, n=10) free flap reconstructions (Table 3). However, type of free flap reconstruction was not found to statistically correlate with incidence of a major complication (P=.39).
DISCUSSION
The versatility of free tissue transfers allows reconstruction of most complex defects; however, it carries significant risks, including longer operative times, donor site morbidity, recipient site complications and free flap failure, and longer hospital stays. As a result, careful consideration and evaluation is necessary prior to reconstruction. Several variables dictate donor site selection including tissue composition, extent of defect, distance from recipient vessels, and surgeon preference. Post-operative care pathways on surgical wards, intraoperative set-up time, and surgeon familiarity often make it desirable to identify a relatively narrow set of free flap donor sites. Although previous studies in free tissue transfer have evaluated risks based on preexisting medical comorbities, here we focus on the surgical factors that may influence outcomes. This study sought to evaluate these trends and outcomes for a large cohort of microvascular free flap reconstructions of the head and neck.
The overall microvascular free flap failure rate was low (3%) with limited complications (10%). This failure rate is similar to previous publications, citing failure rates from 2% to 9%.1,6-10 In comparable large cohort studies (classified as over 1,000 free flaps), average microvascular free flap failure has ranged from 3.4% to 4.2%.1,6,7 Favorable reconstruction outcomes in the current study may be related to our reliance on a limited number of donor sites (in our case the majority being radial forearm) for improved tissue survival and lower complications, a trend that is in agreement with other publications on this topic .4,6
Stratification of surgical characteristics revealed that outcomes in free tissue transfer are recipient site, flap type, and donor site dependent. Cutaneous defects had shorter length of stay (mean 5.8 days) and lower complication rates (6%) relative to defects of the midface which were associated with more than double the number of complications (15%) (P=.02) and longer hospital stays (mean 8.0 days) (P=.0002). Because cutaneous defects do not involve violation of the mucosal surfaces, the wounds are not exposed to salivary contamination. In addition to the sterility of the surgical field, access to the defect, shorter insetting time, and ease of post-operative monitoring are all favorable in cutaneous defects. It is not entirely clear why skull base and midface defects tended to have higher complication rates. It is often more difficult to achieve volume match and adequate flap closure is more challenging, which is perhaps in part due to the three dimensional nature of the defects. However, it may be that because cervical recipient vessels were most commonly used for the anastomosis there may have been additional gravitational effect contributing to vessel compromise. Additionally, passage of the vessels lateral to and overlying the mandible may increase the compressive forces on the vessels, also contributing to free flap failure. The result of these differences is evident in this study, with higher complications, higher flap failure, and longer hospital stays associated with defects above the angle of the mandible.
While the majority of our patients were reconstructed with a fasciocutaneous free flap (74%), 26% underwent reconstruction with an osteocutaneous free flap. Interestingly, this series showed that osteocutaneous tissue transfers had fewer free flap failures than fasciocutaneous. Although osteocutaneous transfers had a slightly lower failure rate (2.2% versus 2.9%) (P=.039), the rates of complications associated with the procedures were similar (11% and 10%) (P=.53). The failure rates and overall complication rates between fasciocutaneous and the osteocutaneous radial forearm free flap were not statistically different, suggesting that there was a limited increase in risk associate with bone reconstruction when using this flap. Our reduction in osteocutaneous failure rates is partly a reflection of the utility of the osteocutaneous radial forearm flap. Traditionally, fibula transfers encompassed the majority of osteocutaneous flaps in the head and neck.11,12 By taking advantage of the radial forearm vasculature, ease of harvest, and versatility of the graft, radial forearm free flaps have proven to be as reliable as fibula transfers. While total failure rate is slightly lower in fibula reconstruction (1.8% compared to 2.5%) (P=.42), overall microvascular complications are higher with fibula transfer (5.8% compared to 3.5%) (P=.46) as well as increased hospital stay (P=.34). However, none of these differences proved statistically significant. The use of the osteocutaneous radial forearm free flap has gradually increased over time and its indications have expanded, especially after it became clear that, despite its limited bone stock, the flap resulted in solid boney reconstruction.11
Secondary bone reconstructions were associated with higher complication rates. Exposure of hardware, especially secondary to radionecrosis, was commonly associated with both the fibula and osteocutaneous forearm transfers. Since it is not specifically associated with the free tissue transfer, it was excluded as a variable from this analysis, but has been evaluated previously by our group. 11,13,14
In this series, a total of 877 patients required reconstruction for primary or recurrent malignancy and 175 for radionecrosis or secondary reconstruction. Microvascular free flap failure rates for defects that resulted from radionecrosis had higher free flap failure rates (6.3%, n=2), compared to repair of composite resections for malignancy (P=.04). This data is consistent with previous studies, indicating that radionecrosis carry a higher risk of flap related complications. We also found radionecrosis was associated with lower rates of free flap survival, consistent with findings reported in the current literature.13,15-17
CONCLUSION
Interestingly, in our evaluation of 1051 microvascular free flap reconstructions, the majority of parameters investigated were found to be equivocal. Survival of a microvascular free flap was not affected by location of the defect, age of the patient, or type of free flap used for the reconstruction. Furthermore, the type of microvascular free flap used for the reconstruction did not affect the incidence of complications or length of hospitalization. Cutaneous defects were associated with shorter lengths of hospitalization relative to other defect locations. Comparison of osteocutaneous free flap reconstructions found longer lengths of hospitalization following fibular reconstructions relative to radial forearm. While several variables are considered in the selection of a donor site for free flap reconstructions, outcomes at our institution were not found to differ significantly when stratified by donor site, defect location, or indication for reconstruction. There was a significant relationship between patient age and donor site selection, with latissimus dorsi free flap reconstructions being selected more frequently in older patients.
Acknowledgements
This work was supported by grants from the National Institute of Health (R01 CA142637-01 and 2T32 CA091078-09). No potential conflicts of interest were disclosed.
REFERENCES
- 1.Nakatsuka T, Harii K, Asato H, et al. Analytic review of 2372 free flap transfers for head and neck reconstruction following cancer resection. J Reconstr Microsurg. 2003;19:363–368. doi: 10.1055/s-2003-42630. discussion 369. [DOI] [PubMed] [Google Scholar]
- 2.Rinaldo A, Shaha AR, Wei WI, Silver CE, Ferlito A. Microvascular free flaps: a major advance in head and neck reconstruction. Acta Otolaryngol. 2002;122:779–784. [PubMed] [Google Scholar]
- 3.Seidenberg B, Hurwitt ES. Immediate reconstruction of the cervical esophagus by a revascularized isolated jejunal segment. Surg Forum. 1958;9:413–416. [PubMed] [Google Scholar]
- 4.Rosenthal E, Carroll W, Dobbs M, Scott Magnuson J, Wax M, Peters G. Simplifying head and neck microvascular reconstruction. Head Neck. 2004;26:930–936. doi: 10.1002/hed.20076. [DOI] [PubMed] [Google Scholar]
- 5.Disa JJ, Cordeiro PG. Mandible reconstruction with microvascular surgery. Semin Surg Oncol. 2000;19:226–234. doi: 10.1002/1098-2388(200010/11)19:3<226::aid-ssu4>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 6.Pohlenz P, Klatt J, Schon G, Blessmann M, Li L, Schmelzle R. Microvascular free flaps in head and neck surgery: complications and outcome of 1000 flaps. Int J Oral Maxillofac Surg. 2012 doi: 10.1016/j.ijom.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Eckardt A, Meyer A, Laas U, Hausamen JE. Reconstruction of defects in the head and neck with free flaps: 20 years experience. Br J Oral Maxillofac Surg. 2007;45:11–15. doi: 10.1016/j.bjoms.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 8.le Nobel GJ, Higgins KM, Enepekides DJ. Predictors of complications of free flap reconstruction in head and neck surgery: Analysis of 304 free flap reconstruction procedures. Laryngoscope. 2012 doi: 10.1002/lary.22454. [DOI] [PubMed] [Google Scholar]
- 9.Genden EM, Rinaldo A, Suarez C, Wei WI, Bradley PJ, Ferlito A. Complications of free flap transfers for head and neck reconstruction following cancer resection. Oral Oncol. 2004;40:979–984. doi: 10.1016/j.oraloncology.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Haughey BH, Wilson E, Kluwe L, et al. Free flap reconstruction of the head and neck: analysis of 241 cases. Otolaryngol Head Neck Surg. 2001;125:10–17. doi: 10.1067/mhn.2001.116788. [DOI] [PubMed] [Google Scholar]
- 11.Virgin FW, Iseli TA, Iseli CE, et al. Functional outcomes of fibula and osteocutaneous forearm free flap reconstruction for segmental mandibular defects. Laryngoscope. 120:663–667. doi: 10.1002/lary.20791. [DOI] [PubMed] [Google Scholar]
- 12.Disa JJ, Pusic AL, Hidalgo DH, Cordeiro PG. Simplifying microvascular head and neck reconstruction: a rational approach to donor site selection. Ann Plast Surg. 2001;47:385–389. doi: 10.1097/00000637-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Dean NR, McKinney SM, Wax MK, Louis PJ, Rosenthal EL. Free flap reconstruction of self-inflicted submental gunshot wounds. Craniomaxillofac Trauma Reconstr. 4:25–34. doi: 10.1055/s-0031-1272899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dean NR, Wax MK, Virgin FW, Magnuson JS, Carroll WR, Rosenthal EL. Free flap reconstruction of lateral mandibular defects: indications and outcomes. Otolaryngol Head Neck Surg. 146:547–552. doi: 10.1177/0194599811430897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curi MM, Oliveira dos Santos M, Feher O, Faria JC, Rodrigues ML, Kowalski LP. Management of extensive osteoradionecrosis of the mandible with radical resection and immediate microvascular reconstruction. J Oral Maxillofac Surg. 2007;65:434–438. doi: 10.1016/j.joms.2005.12.068. [DOI] [PubMed] [Google Scholar]
- 16.Militsakh ON, Wallace DI, Kriet JD, Tsue TT, Girod DA. The role of the osteocutaneous radial forearm free flap in the treatment of mandibular osteoradionecrosis. Otolaryngol Head Neck Surg. 2005;133:80–83. doi: 10.1016/j.otohns.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 17.Futran ND, Farwell DG, Smith RB, Johnson PE, Funk GF. Definitive management of severe facial trauma utilizing free tissue transfer. Otolaryngol Head Neck Surg. 2005;132:75–85. doi: 10.1016/j.otohns.2004.08.013. [DOI] [PubMed] [Google Scholar]


