Abstract
A 52-year-old man underwent bilateral articular surface replacement (ASR) DePuy in June 2006. Following a right femoral neck fracture 4 days postoperatively, he underwent revision to a cemented C-stem DePuy, a taper sleeve adaptor and a 47 mm diameter cobalt chromium femoral head. The patient recovered well with satisfactory 5-year follow-up. In September 2011 the patient presented to the accident and emergency department with a 5-day history of feeling unwell with right lower quadrant pain. Examination of the right hip was unremarkable apart from painful adduction. Blood tests showed raised inflammatory markers and white cell count. MRI scan showed a right iliopsoas collection which appeared to communicate with the hip joint. The patient underwent a direct exchange of the right hip prosthesis. The intraoperative clinical picture was suggestive of atypical lymphocytic vasculitis and associated lesions. The patient recovered well and was discharged home. At his last clinic visit he was well and pain free.
Background
Atypical lymphocytic vasculitis and associated lesions (ALVAL) is a delayed type IV hypersensitivity reaction. It has been observed in patients with metal-on-metal total hip replacements (THRs)1 as a sequela of an adverse reaction to metal debris (ARMD).
The condition is historically relatively rare (0.3%) and previously it was unclear as to which patients were more likely to develop ALVAL. However, it had been suggested that patients with allergies to certain metals or with advanced renal dysfunction should avoid having metal-on-metal bearing implants.1 Some studies had also found that women were at a higher risk of developing ALVAL than men.2
Particular interest in ALVAL has developed over the last few years in view of the serious nature of the problems caused by metal debris from a new generation of metal-on-metal hip prostheses. Muscle necrosis, aseptic loosening and periprosthetic osteolysis have all been reported.
It is important for members of all medical specialties to be aware of this phenomenon so that a correct diagnosis and appropriate management can be implemented. We present a case of ALVAL in a patient complaining of acute abdominal pain.
Case presentation
A 52-year-old fit and healthy man who had bilateral articular surface replacement (ASR) DePuy, in June 2006 for osteoarthritis (figure 1). A 47 mm diameter ASR femoral component and a 54 mm outside diameter ASR cup were implanted on the right side. Four days postoperative he sustained a right femoral neck fracture with no history of trauma. Subsequently the patient underwent revision of the ASR femoral resurfacing to a cemented C-stem DePuy, a taper sleeve adaptor and a 47 mm diameter cobalt chromium femoral head. The patient recovered well and was discharged 2 days later with satisfactory 6 week and 1 year follow-up.
Figure 1.

Postoperative radiograph June 2006.
In March 2011, 5 years postoperative, radiographs were satisfactory, range of movement was excellent and the patient remained pain free.
At the end of September 2011 the patient presented to the accident and emergency department with a 5 day history of generally feeling unwell with right lower quadrant pain. Following a round of golf he had felt a spontaneous sharp pain in his right groin and abdomen, lost his balance and fell. He was admitted under the medics and on examination was found to be feverish with tender hepatomegaly. Blood tests showed his white cell count (13.5 ×109/l) and inflammatory markers (C reactive protein 207 mg/l) to be raised and his liver function tests deranged.
Examination revealed fever and a tender epigastrium. On examination the right hip was comfortable in flexion, had normal abduction but painful adduction.
Investigations
A pelvic CT scan was reported as showing a 5 cm diameter psoas abscess. Intravenous antibiotics were subsequently started and tentative arrangements for percutaneous drainage of the collection made.
Twenty-four hours after admission the patient was seen by the orthopaedic on-call team and for further clarification a MRI was performed showing a right iliopsoas collection (6×4×5 cm) which appeared to communicate with the hip joint (figure 2). Extensive metal debris was seen but there was no evidence of significant periprosthetic osteolysis.
Figure 2.
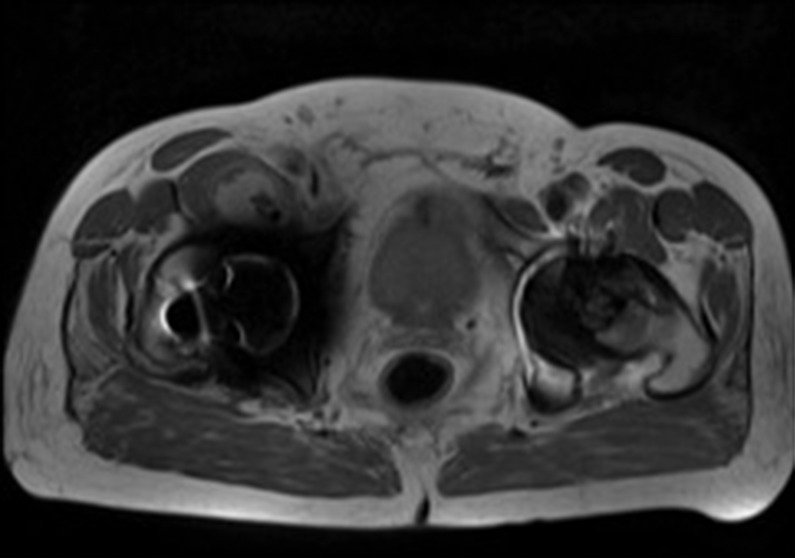
Right psoas collection.
Differential diagnosis
The initial medical differential diagnoses were (1) biliary sepsis, (2) urinary tract infection and (3) septic arthritis.
Following orthopaedic review by senior doctors and the MRI scan results the differential diagnoses were altered to (1) ALVAL and (2) infected THR.
Treatment
In light of the CT and MRI findings a diagnosis of ALVAL/ARMD was made and percutaneous drainage of the collection was cancelled. Arrangements were made for revision arthroplasty surgery and a week after admission the patient underwent a direct exchange of the right hip prosthesis. At surgery a white creamy collection was visualised within the hip joint (figure 3), there was black staining of the trunion (figure 4), macroscopic wear of the taper (figure 5) and granulomatous tissue in line with the psoas tendon.
Figure 3.
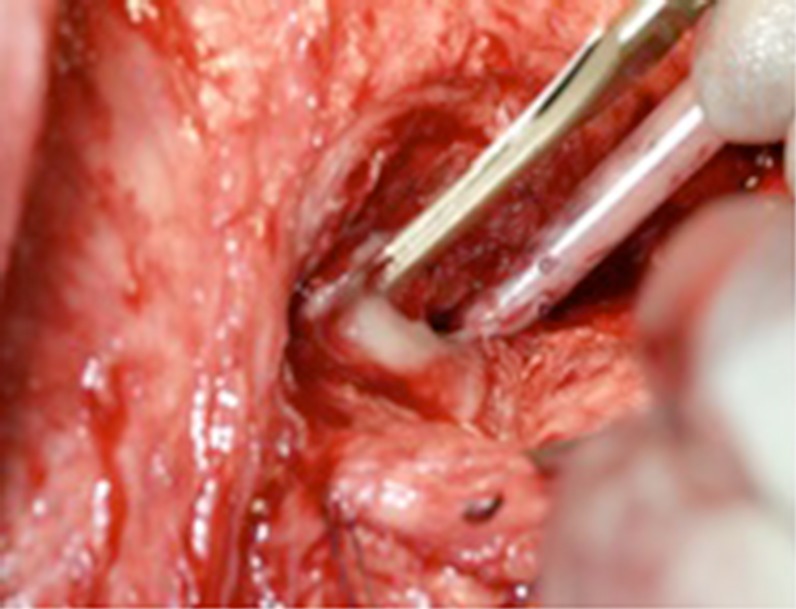
A white creamy collection visualised within the hip joint intraoperatively.
Figure 4.

Black staining of the trunion.
Figure 5.
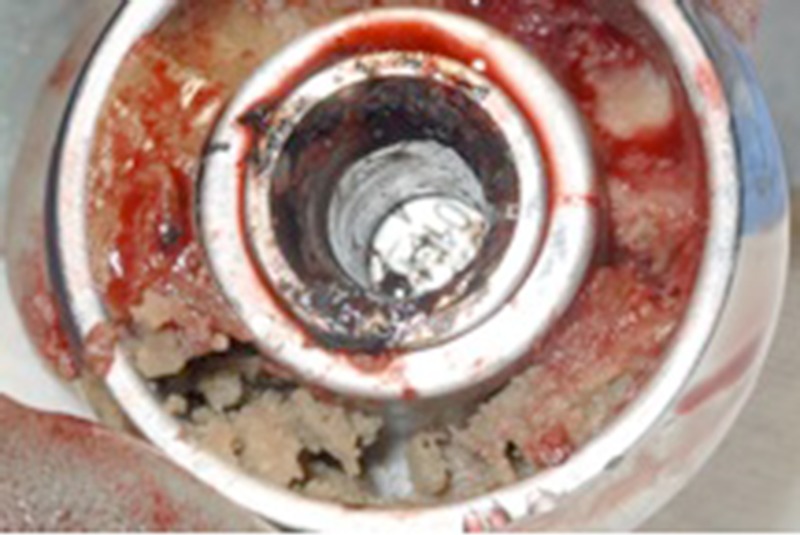
Macroscopic wear of the taper.
The intraoperative clinical picture was highly suggestive of ALVAL and not an infective process, psoas abscess or abdominal pathology. Five intraoperatrive tissue samples taken were sent for prolonged aerobic and anaerobic culture which subsequently revealed no evidence of infection.
The hip was revised to a Duraloc DePuy uncemented cup with a ceramic liner and a short stem Exeter Stryker cemented femoral stem with a 32 mm ceramic head (figure 6).
Figure 6.

Radiograph of the hip revised to a Duraloc DePuy uncemented cup with a ceramic liner and a short stem Exeter Stryker cemented femoral stem with a 32 mm ceramic head.
Serum cobalt (Co)/chromium (Cr) levels taken on admission triggered at the current Medicines and Healthcare products Regulatory Agency (MHRA) action levels; 7.00 µg/l (ppb) for Co, Cr. Co 6.14 µg/l (ppb) and Cr 9.00 µg/l (ppb) would suggest an excessive metal ion release in keeping with our diagnosis of ALVAL.
Outcome and follow-up
The patient recovered well and 5 days following surgery he was discharged home. At his last clinic visit he was well and pain free. Metal ion levels had normalised and a left hip MRI in December 2011 was normal.
Discussion
Metal-on-metal hip resurfacing arthroplasty was initially proposed for the younger patient with symptomatic osteoarthritis of the hip with high functional demands following surgery. Stated benefits of this proposal included durability, stability, similar anatomical mechanics to the original hip and preservation of a bone stock for potential future revisions.3 Of late there have been increasing numbers of metal-on-metal THR failures reported due to ALVAL and ARMD. Perivascular infiltration of T and B lymphocytes in the tissues around the prosthetic joint cause failure because of aseptic loosening and periprosthetic osteolysis.4
ALVAL can present in different ways. Common presentations include gradually worsening groin pain, hip pain with or without groin, or periprosthetic masses (pseudotumours).5–8 Asymptomatic patients with a failing bearing present an increasing problem and serial measurements of metal ions is a useful screening tool along with metal artefact reduction sequence (MARS) MRI.
The diagnosis of ALVAL remains a challenging one. It is thought that metal-on-metal implants release different quantities of metal ions over time from normal wear. However, serum levels of metal ions are of controversial value when trying to determine which patients are at risk of developing ALVAL. This is confusing as metal ions are believed to play a key part in eliciting the hypersensitivity reaction.1 7
It can be difficult clinically to differentiate ALVAL from infection as discussed in this paper. Aspiration of the hip joint with prolonged cultures of the aspirate is essential to exclude infection as the diagnosis.4 While some may be reticent in undertaking this procedure because of the potential risk of introducing infection into the joint we believe it is the only way to ascertain whether or not the joint is infected. The only definitive test for ALVAL is histological assessment of the affected tissues. Histology would differentiate the infected tissue from that tissue which has been subjected to a hypersensitivity reaction. Histological features include necrosis, evidence of bleeding, exudated fibrin, macrophages, plasma cells and perivascular lymphocytes.9
While patch testing has been used to assess allergic reaction to metal there is discrepancy between researchers as to whether dermal testing can be used reliably to assess a patient's likelihood of a systemic reaction to metal implant debris.7 9 10 Lymphocyte transformation testing, cytokine ELISA and leucocyte migration inhibition testing may be helpful preoperatively in finding patients at high risk of developing ALVAL.7 9 Currently these tests are expensive, not widely available and remain unproven in their accuracy as a screening tool.9
MARS MRI imaging is now increasingly commonly used to identify ALVAL11 in symptomatic patients or those asymptomatic patients with raised cobalt or chromium levels. One study using MARS MRI to diagnose pseudotumours associated with ALVAL found similar numbers of pseudotumours in both symptomatic and asymptomatic patients.12 However, even using this highly specific imaging technique there is still difficulty in differentiating between ALVAL and infection, especially in the early stages of the disease.11 ALVAL remains a diagnostic challenge which can result in a delay of treatment.
The use of multiple imaging modalities has been proposed by Tins13 who found that as ALVAL was not easily differentiated from infection using MRI, further CT imaging looking at bone changes was of additional benefit. Sepsis and ALVAL can occur within the same joint as the immune response potentiated by ALVAL can lead to an environment favourable for bacterial growth if left untreated.14
The pathological course of ALVAL is one of progressive soft tissue destruction such that at the hip there is increased joint instability and susceptibility to dislocation.15 ALVAL needs to be diagnosed and managed accordingly to prevent this progressive soft tissue destruction which would impair the success of any subsequent revision procedures.
Some researchers have raised the issue of causality. There has been suggestion that infection or aseptic loosening of a metal prosthesis causes the release of metal ions, which then elicits a hypersensitivity response instead of the other way round.16 17 Either way, surgeons have noted that the majority of patients who undergo revisions for ALVAL have immediate improvement in their symptoms postoperatively.8
Metal hypersensitivity with perivascular lymphocytic infiltration (PVLI) is not exclusive to metal-on-metal hip implants. PVLI has also been reported in total knee replacements and THRs with more traditional bearing surfaces (Co Cr on polyethylene)18 but the most severe reactions are still seen at revisions of metal-on-metal hip arthroplasty, as described in this paper. More recently, ALVAL has been documented in spinal surgery where metal-on-metal total disc replacements have been used.19
The use of metal-on-metal implants should be carefully considered. In 2012 the British Hip Society advised that large metal-on-metal THRs should no longer be used. This advice does not apply to hip resurfacings and they remain a viable option.
In conclusion, a high index of suspicion of ARMD and the potential for ALVAL should be considered in any patient with a metal-on-metal prosthesis who presents with hip, groin or lower abdominal pain with or without soft tissue swelling. This will then allow prompt referral to orthopaedic surgeons for further management.
Learning points.
Atypical lymphocytic vasculitis and associated lesions (ALVAL) is a delayed type IV hypersensitivity reaction seen in patients with metal-on-metal hip replacements.
ALVAL remains a diagnostic challenge requiring careful investigation.
Doctors should have a high index of suspicion for ALVAL in patients presenting with hip, groin or lower abdominal pain who have a metal-on-metal hip prosthesis in situ.
It is important to diagnose ALVAL early, as the pathological course is one of progressive soft tissue destruction leading to increased joint instability and susceptibility to dislocation.
The only definitive treatment for ALVAL is revision arthroplasty surgery of the affected joint.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Delaunay C, Petit I, Learmonth ID, et al. Metal-on-metal bearings total hip arthroplasty: the cobalt and chromium ions release concern. Orthop Traumatol Surg Res 2010;2013:894–904 [DOI] [PubMed] [Google Scholar]
- 2.Hinsch A, Vettorazzi E, Morlock MM, et al. Sex differences in the morphological failure patterns following hip resurfacing arthroplasty. BMC Med 2011;2013:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mabilleau G, Kwon YM, Pandit H, et al. Metal-on-metal hip resurfacing arthroplasty: a review of periprosthetic biological reactions. Acta Orthop 2008;2013:734–47 [DOI] [PubMed] [Google Scholar]
- 4.Meyer H, Kruger A, Roessner A, et al. [Allergic reactions as differential diagnoses for periprosthetic infection]. Orthopade 2012;2013:26–31 [DOI] [PubMed] [Google Scholar]
- 5.Counsell A, Heasley R, Arumilli B, et al. A groin mass caused by metal particle debris after hip resurfacing. Acta Orthop Belg 2008;2013:870–4 [PubMed] [Google Scholar]
- 6.Campbell P, Ebramzaheh E, Nelson S, et al. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res 2010;2013:2321–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watters TS, Cardona DM, Menon KS, et al. Aseptic lymphocyte-dominated vasculitis-associated lesion: a clinicopathologic review of an underrecognised cause of prosthetic failure. Am J Clin Pathol 2010;2013:886–93 [DOI] [PubMed] [Google Scholar]
- 8.Rajpura A, Porter ML, Gambhir AK, et al. Clinical experience of revision of metal on metal hip arthroplasty for aseptic lymphocyte dominated vasculitis associated lesions (ALVAL). Hip Int 2011;2013:43–51 [DOI] [PubMed] [Google Scholar]
- 9.Galbraith JG, Butler JS, Browne TJ, et al. Infection or metal hypersensitivity? The diagnostic challenege of failure in metal-on-metal bearings. Acta Orthop Belg 2011;2013:145–51 [PubMed] [Google Scholar]
- 10.Granchi D, Cenni E, Trisolino G, et al. Sensitivity to implant material in patients undergoing total hip replacement. J Biomed Mater Res B Appl Biomater 2006;2013:257–64 [DOI] [PubMed] [Google Scholar]
- 11.Anderson H, Toms AP, Cahir JG, et al. Grading the severity of soft tissue changes associated with metal-on-metal hip replacements: reliability of a MR grading system. Skeletal Radiol 2011;2013:303–7 [DOI] [PubMed] [Google Scholar]
- 12.Hart AJ, Satchithananda K, Liddle AD, et al. Pseudotumours in association with well-functioning metal-on-metal hip prostheses: a case control study using three-dimensional computed tomography and magnetic resonance imaging. J Bone Joint Surg Am 2012;2013:317–25 [DOI] [PubMed] [Google Scholar]
- 13.Tins B. Dislocation and spontaneous reduction of the femoral implant against the femoral neck in an infected metal on metal hip resurfacing with complex collection. Eur J Radiol 2011;2013:136–9 [DOI] [PubMed] [Google Scholar]
- 14.Donaldson JR, Miles J, Sri-Ram K, et al. The relationship between the presence of mattallosis and massive infection in metal-on-metal hip replacements. Hip Int 2010;2013:242–7 [DOI] [PubMed] [Google Scholar]
- 15.Theruvil B, Vasukutty N, Hancock N, et al. Dislocation of large metal-on-metal bearings an indicator of metal reaction? J Athroplasty 2010;2013:832–7 [DOI] [PubMed] [Google Scholar]
- 16.Rau C, Thomas P, Thomsen M. [ Metal sensitivity in patients with joint replacement arthroplasties before and after surgery]. Orthopade 2008;2013:102–10 [DOI] [PubMed] [Google Scholar]
- 17.Elves MW, Wilson JN, Scales JT, et al. Incidence of metal hypersensitivity in patients with total joint replacements. Br Med J 1975;2013:376–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ng VY, Lombardi AV, Jr, Berend KR, et al. Perivascular lymphocytic infiltration is not limited to metal-on-metal bearings. Clin Orthop Relat Res 2011;2013:523–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guyer RD, Shellock J, MacLennan B, et al. Early failure of metal-on-metal artificial disc prostheses associated with lymphocytic reaction: diagnosis and treatment experience in four cases. Spine (Phila Pa 1976) 2011;2013:E492–7 [DOI] [PubMed] [Google Scholar]


