Abstract
Purpose: Caring for a family member with dementia is associated with chronic stress, which can have significant deleterious effects on caregivers. The purpose of the Balance Study was to compare a mindfulness-based stress reduction (MBSR) intervention to a community caregiver education and support (CCES) intervention for family caregivers of people with dementia. Design and Methods: We randomly assigned 78 family caregivers to an MBSR or a CCES intervention, matched for time and attention. Study participants attended 8 weekly intervention sessions and participated in home-based practice. Surveys were completed at baseline, postintervention, and at 6 months. Participants were 32- to 82-year-old predominately non-Hispanic White women caring for a parent with dementia. Results: MBSR was more effective at improving overall mental health, reducing stress, and decreasing depression than CCES. Both interventions improved caregiver mental health and were similarly effective at improving anxiety, social support, and burden. Implications: MBSR could reduce stress and improve mental health in caregivers of family members with dementia residing in the community.
Key Words: Chronic stress, Dementia, Complemen tary therapies, Mind-body therapies
Few tasks are more challenging than caring for a family member with dementia. Dementia is a progressive disorder leading to perceptual and cognitive decline that result in increased impairment, behavioral changes, and inability to function independently. Eventually, people with dementia require round-the-clock care—most often from family caregivers (Alzheimer’s Association, 2012). Caregiving is associated with a host of problems, including poor physical health leading to increased mortality, compromised immune function, emotional issues, social isolation, and mental health concerns such as depression and anxiety (Aschbacher et al., 2006; Ferrara et al., 2008; Pinquart & Sörensen, 2007; Schulz & Martire, 2004) The resulting chronic stress has significant deleterious effects on caregiver health and well-being (Kiecolt-Glaser et al., 2003; Schulz & Martire, 2004; Sörensen, Duberstein, Gill, & Pinquart, 2006). Interventions designed to help caregivers manage this stress are increasingly important as the number of people with dementia expands with the aging population (Alzheimer’s Association, 2012). New interventions such as mindfulness-based stress reduction (MBSR) may help caregivers manage the chronic stress of caring for a family member with dementia.
Current interventions for caregivers are often multidimensional in structure, providing psychological, social/emotional, and educational support. These programs often include a variety of components, such as education, counseling, support groups, problem solving, behavior management training, and respite or adult day care. The most widely studied interventions are psychoeducational and combine social support with caregiver education (Acton & Kang, 2001). Newer interventions such as Resources for Enhancing Alzheimer’s Caregivers Health (REACH) have gone much further, testing multiple theory-driven programs at differing sites based on strategies such as psychoeducational and skill-based training, technology, and home-based strategies (Belle et al., 2006; Elliott, Burgio, & Decoster, 2010; Gitlin et al., 2003). Although there is growing evidence that a number of these programs benefit caregivers, access to promising interventions can be limited due to economic, geographic, and policy barriers (Peacock & Forbes, 2003; Schulz et al., 2002; Sörensen, Pinquart, & Duberstein, 2002). Evidence supporting the long-term benefit of these programs is also somewhat limited.
People with dementia often have declining cognitive function and increasing behavioral problems over many years. For caregivers, this decline can lead to increasing stress, frustration, anxiety, depression, and health problems. Giving caregivers skills to manage the daily chronic stress and the emotional challenges of caregiving may provide a long-term benefit to the caregiver.
MBSR is a standardized program designed to reduce stress and manage difficult emotions through training in mindfulness (Bishop, 2002; Chambers, Gullone, & Allen, 2009). Mindfulness refers to a particular type of attention focused on the present moment, nonjudgmental awareness, and acceptance of that experience with a stance of openness and curiosity. It includes both formal practice (mindful movement, the body scan, sitting meditation) and informal practice (incorporating mindfulness into everyday life; Cullen, 2011). Rooted in Buddhist tradition, MBSR is a nonreligious program developed for patients with chronic pain and illness to help reduce stress and manage symptoms (Kabat-Zinn, 1990). Participants are encouraged to simply observe their thoughts and emotions, letting them pass without judgment or becoming caught up or immersed in them. The practice can facilitate responses to internal and external stimuli in a more reflective and less reactive and impulsive way. Training in mindfulness may enhance the range and use of coping skills through improved self-observation and reflection (Baer, 2003). It can also decrease ruminative thoughts about past or future events through focus on moment-to-moment awareness and acceptance (Borders, Earleywine, & Jajodia, 2010; Jain et al., 2007). These skills may help caregivers manage their stress responses to the long-term challenges of caregiving.
MBSR has been studied as a complementary therapy for stress and symptom management in a wide range of chronic medical conditions, including pain (McCracken, Gauntlett-Gilbert, & Vowles, 2007), cancer (Ledesma & Kumano, 2008; Lengacher et al., 2009), fibromyalgia (Grossman, Tiefenthaler-Gilmer, Raysz, & Kesper, 2007), rheumatoid arthritis (Pradhan et al., 2007), solid organ transplant (Gross et al., 2004,2010; Kreitzer, Gross, Ye, Russas, & Treesak, 2005), severe psoriasis (Kabat-Zinn et al., 1998), insomnia (Gross et al., 2011), and diabetes (Rosenzweig et al., 2007; Whitebird, Kreitzer, & O’Connor, 2009). It has also been used with caregivers of disabled children (Minor, Carlson, Mackenzie, Zernicke, & Jones, 2006) and incorporated into a new therapeutic approach called mindfulness-based cognitive therapy, which has shown promise in treating recurrent depression (Kuyken et al., 2008; Teasdale et al., 2000). In aggregate, studies of MBSR show decreases in medically related symptoms; improved functioning; and reduced stress, anxiety, and depression (Astin, Shapiro, Eisenberg, & Forys, 2003; Fjorback, Arendt, Ornbol, Fink, & Walach, 2011; Grossman, Niemann, Schmidt, & Walach, 2004; Hofmann, Sawyer, Witt, & Oh, 2010).
To date, we know of no other studies that have examined the use of MBSR for family caregivers of a person with dementia. Waelde, Thompson, and Gallager-Thompson (2004) conducted a pilot study for dementia caregiver stress using a program called Inner Resources, which has features similar to MBSR. Their findings suggest that this type of intervention may be feasible and effective for family caregivers. Lavretsky et al. (2012) in their recent study of yogic meditation for caregivers of family members with dementia found that a brief daily meditation practice led to improved mental and cognitive functioning and lower levels of depression in caregivers. They also found improvement in telomerase activity, suggesting improvements in stress-induced cellular aging.
The Balance Study was a randomized controlled trial that compared an MBSR intervention for family caregivers of a person with dementia with an active comparison group, a standard community caregiver education and social support (CCES) program. The purpose was twofold: (a) to examine the feasibility and acceptability of MBSR as an intervention for stress among caregivers of a family member with dementia and (b) to examine mental health outcomes. We hypothesized that caregivers in the MBSR intervention would have better outcomes than caregivers in the CCES intervention on measures of perceived stress, psychological health, and perceived caregiver burden.
Methods
Participants
The study was conducted from 2007 to 2010 in the upper Midwest at a nonprofit research center affiliated with a mixed-model health plan. Study participants were recruited through a health plan and its clinics, community outreach, paid advertising (i.e., print and radio ads), press coverage, and word of mouth (Whitebird et al., 2011). Participants were study eligible if, during a telephone screen, they self-identified as a primary caregiver of a community-dwelling family member who had memory loss consistent with dementia; were older than 21; spoke English; could read the course materials; were willing to attend all group sessions; had not participated in a community caregiver support program; had not practiced meditation, yoga, or tai chi in the previous year; had to score 5 or higher on a single-item measure of self-perceived stress (scale of 1–10); had no psychiatric hospitalizations or diagnoses of mental illness in the previous 2 years; had not been taking antipsychotic or anticonvulsion medication; and had no thoughts of harming themselves in the previous 6 months.
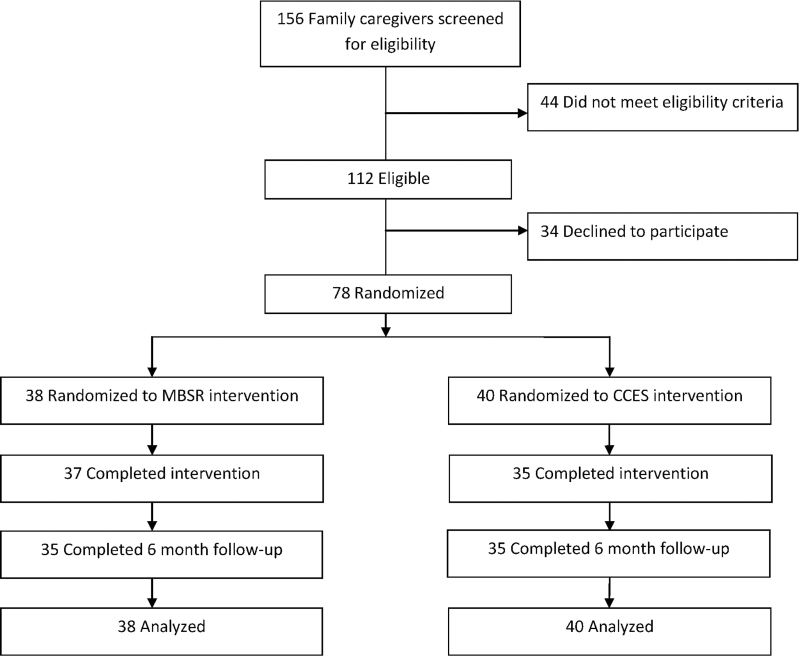
Of the 156 caregivers screened for the study, 112 were eligible and 78 agreed to participate, enrolled, and were randomly assigned to the MBSR or CCES intervention (Figure 1). Our target recruitment goal was 60 participants. Over recruitment was allowed to anticipate potential dropouts and variations in recruitment flow that affected group size across the 18-month recruitment period. Six of the 78 participants dropped out before completing the intervention because the spouse they had been caring for entered a nursing home or they had time constraints related to caregiving or dissatisfaction with random assignment to CCES.
Figure 1.
Participant flow through the study. CCES = community caregiver education and support and MBSR = mindfulness-based stress reduction.
Procedures
Participants received written study materials by mail and attended an orientation meeting at which they received additional study information, signed consent forms, completed a survey, and were randomly assigned using a computerized algorithm for simple randomization. They completed additional surveys postintervention (2 months) and 6 months following the baseline survey. Participants also completed a daily health behaviors calendar during the intervention period to track MBSR practice and stress reduction activities. The study was reviewed and approved by the HealthPartners and University of Minnesota Institutional Review Boards.
Intervention
The MBSR and CCES interventions were matched for time and attention and consisted of 8 weekly 2.5-hr in-person group sessions. Each intervention included a 5-hr retreat or wellness day that more intensively covered the same material delivered in the weekly sessions. The MBSR instructor was employed by the University of Minnesota Center for Spirituality and Healing and trained in MBSR through the Stress Reduction and Relaxation Clinic at the University of Massachusetts. The CCES group instructor was an experienced licensed social worker provided through a local nonprofit organization that has provided caregiver programs and services in the community for 30 years. There were five waves of MBSR/CCES intervention groups with an average of seven or eight participants per study group in each wave.
MBSR participants received instruction about concepts of mindfulness and practiced meditation and gentle yoga exercises each week. They received instruction on sitting and walking meditation, body scan meditation, and gentle Hatha yoga and stretching exercises and were given CDs and written material to help engage in home practice. Participants recorded their minutes of daily MBSR practice in their health behaviors calendar.
CCES participants received education on issues affecting family caregivers and group social and emotional support. Participants received educational information each week on topics such as dementia, legal and financial issues, community resources, communication, self-care, grief, and loss. They also participated in group-based discussions facilitated by the instructor about their experience as caregivers.
The study coordinator conducted weekly telephone support calls during the intervention and then monthly through month 6. The coordinator encouraged MBSR participants to practice daily and helped those with difficulties problem solve. The coordinator encouraged the CCES group to practice or implement what they were learning in their intervention.
Measures
We collected information on demographics, caregiver relationship, and length of time as a caregiver from all participants. The survey assessed psychosocial and caregiver burden at baseline, postintervention, and 6 months.
Stress.—
Stress was measured using the 10-item version of the Perceived Stress Scale (PSS). It is a self-reported measure of the degree to which situations were considered stressful during the previous month (Cohen, Kamarck, & Mermelstein, 1983; Cohen, & Williamson, 1988).
Mental Health.—
Depression symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CES-D), a 20-item measure that has been extensively studied and validated (McDowell & Newell, 2006). Anxiety was measured with the State-Trait Anxiety Inventory (STAI)—State Version Y subscale. The STAI is widely used in research and clinical practice and has demonstrated internal consistency and validity (Spelberger, 1983). Overall mental health was measured with the Short-Form-12 Health Survey (SF-12), which provides two composite scores: one for mental health (MCS-12) and one for physical health (PCS-12). It has been used extensively and demonstrates good reliability and validity (McDowell & Newell, 2006).
Caregiver Burden.—
Caregiver burden was assessed using the Montgomery Borgatta Caregiver Burden Scale, which contains three subscales: objective burden, subjective demand burden, and subjective stress burden (Montgomery, 2002; Montgomery, Borgatta, & Borgatta, 2000). Objective burden measures perceived infringement on or disruption of tangible aspects of the caregiver’s life. Subjective demand burden measures the extent to which the caregiver perceives care to be overly demanding. Subjective stress burden measures the emotional impact of caregiving responsibilities. Recent studies show reasonable reliability and validity for the subscales (Stone & Clements, 2009).
Social Support.—
Social support was measured using the Medical Outcomes Study Social Support Survey, which covers four categories of social support: emotional or informational support, tangible support, positive social interaction, and affectionate support. The scale has been extensively studied and demonstrates good reliability and validity (McDowell & Newell, 2006).
Analysis
Measures of central tendency and dispersion were calculated for prerandomization demographic characteristics and intervention adherence. The MBSR and CCES participants were compared on these measures using t tests or chi-square statistics as appropriate.
The primary analyses tested the hypothesis that MBSR and CCES participants would not differ on any of these measures before randomization, but that by postintervention (2 months) and 6 months, MBSR participants would report better outcomes. General linear mixed models (Verbeke & Molenberghs, 2000) using SAS PROC MIXED predicted each outcome measure from measurement time (baseline, postintervention, 6 months) and intervention (MBSR, CCES). Simple effects tests comparing MBSR with CCES participants were calculated to determine the time points at which the groups differed. The efficacy of MBSR relative to CCES in promoting psychological health among caregivers would be most strongly supported by significant time-by-intervention interactions coupled with significant MBSR–CCES postintervention and 6-month comparisons.
The mixed models specified up to three obser vations for each participant, random participant intercepts, unspecified covariance structure, and restricted maximum likelihood estimation (Littell, Milliken, Stroup, Wolfinger, & Schabenberger, 2006). We chose the mixed-model approach because, relative to a repeated measures ANOVA/ANCOVA approach, it ensured an intent-to-treat analysis that used all available observations from all randomized participants to estimate model parameters.
Results
Participants (n = 78) were 32- to 82-year-old predominately non-Hispanic White (97%) women (89%), most of them caring for a parent (Table 1). There were no observed demographic differences between the caregivers randomly assigned to MBSR relative to CCES. Adherence to each intervention included attendance at weekly groups and the retreat/wellness day; 83% of participants attended at least seven of the eight weekly group sessions, and 90% attended the retreat/wellness day (Table 2). Similarly, 88% of CCES and 92% of the MBSR participants completed the 6-month survey. MBSR participants practiced MBSR at home, an average of 6.8 sessions per week and averaged 29.4min per session over the 8-week intervention.
Table 1.
Characteristics of All Study Participants Randomly Assigned to Community Caregiver Education and Support (CCES) and Mindfulness-Based Stress Reduction (MBSR) Treatment Groups
| Total | CCES | MBSR | p Value | |
|---|---|---|---|---|
| N | 78 | 40 | 38 | |
| Age, M (SD) | 56.8 (9.9) | 56.4 (10.2) | 57.2 (9.6) | .69 |
| Female (%) | 88.5 | 90.0 | 86.8 | .66 |
| Race (%) | .33 | |||
| White | 98.7 | 97.5 | 100 | |
| American Indian | 1.3 | 2.5 | 0 | |
| Hispanic (%) | 1.3 | 2.5 | 0 | .33 |
| Non-Hispanic White (%) | 97.4 | 95.0 | 100 | .16 |
| Caregiver relationship (%) | .24 | |||
| Adult child | 74.4 | 80.0 | 68.4 | |
| Spouse, sibling, friend | 25.6 | 20.0 | 31.6 | |
| Months caregiving, M (SD) | 48.8 (39.3) | 46.7 (42.5) | 51.1 (36.0) | .63 |
| Marital status (%) | .72 | |||
| Married | 60.3 | 57.5 | 63.2 | |
| Never married | 23.1 | 22.5 | 23.7 | |
| Widowed or divorced | 16.7 | 20.0 | 13.2 | |
| Education (%) | .84 | |||
| High school/some college | 43.6 | 42.5 | 44.7 | |
| College | 34.6 | 37.5 | 31.6 | |
| Graduate school | 21.8 | 20.0 | 23.7 | |
| Employment (%) | .92 | |||
| Employed | 65.4 | 67.5 | 63.2 | |
| Out of work/unable to work | 5.1 | 5.0 | 5.3 | |
| Retired/homemaker | 39.5 | 27.5 | 31.6 |
Table 2.
Adherence to Evaluation and Randomly Assigned Intervention
| Total | CCES | MBSR | p Value | |
|---|---|---|---|---|
| Evaluation | ||||
| Baseline, n | 78 | 40 | 38 | |
| 2-month survey, n | 72 | 35 | 37 | |
| 6-month survey, n | 70 | 35 | 35 | |
| Intervention attendance | ||||
| Weekly sessions, M (SD) | 7.1 (1.6) | 6.8 (2.0) | 7.3 (1.1) | .16 |
| Retreat, wellness day, M (SD) | 0.9 (0.3) | 0.9 (0.4) | 1.0 (0.2) | .10 |
| Combined attendance, M (SD) | 8.0 (1.9) | 7.7 (2.3) | 8.3 (1.2) | .14 |
| Sessions per week of MBSR home practice, M (SD) | 6.8 (3.0) | |||
| Minutes per session per week of MBSR home practice, M (SD) | 29.4 (4.6) | |||
Notes: CCES = community caregiver education and support and MBSR = mindfulness-based stress reduction.
Two patterns of outcomes indicated support for the efficacy of MBSR. The first was observed for the MCS-12 mental health scale (Table 3). MBSR participants showed immediate improvement and reported better mental health than CCES participants postintervention (p = .007) and maintained this improvement. CCES participants reported very little change in their mental health over time, resulting in a significant difference between the groups at 6 months as well (p = .04). The second pattern supported the short-term efficacy of MBSR for perceived stress and depression. The MBSR and CCES participants were not different at baseline in their reports of perceived stress (p = .99) or depression (p = .58). Postintervention, MBSR participants reported lower stress (p = .007) and depression (p = .005) than CCES participants. At 6 months, however, the groups were no longer statistically distinguishable from each other (p stress = .07, p depression = .16). For both of these outcomes, MBSR participants reported improved mental health outcomes postintervention and maintained this improvement at 6 months, whereas CCES participants reported steady improvement that resulted in similar outcomes as MBSR participants at 6 months.
Table 3.
Observed Mean (SD) of Mental Health Measures at Baseline and 2 and 6 Months by Treatment Group, Cohen’s d for Mindfulness-Based Stress Reduction (MBSR)–Community Caregiver Education and Support (CCES) Difference, Significance of Simple Effects Test at Each Time Point, and Significance of Main and Interactive Effects
| CCES | MBSR | d | p Value | |
|---|---|---|---|---|
| Perceived stress | ||||
| Baseline | 21.2 (7.5) | 21.2 (4.7) | −.01 | .99 |
| 2 months | 19.3 (7.6) | 15.2 (5.8) | −.61 | .007 |
| 6 months | 16.7 (7.2) | 14.0 (4.5) | −.47 | .07 |
| Treatment group | .07 | |||
| Time | <.001 | |||
| Treatment group × time | .01 | |||
| Depression | ||||
| Baseline | 19.2 (11.8) | 17.9 (8.9) | −.13 | .58 |
| 2 months | 17.1 (11.2) | 10.6 (8.4) | −.66 | .005 |
| 6 months | 13.7 (9.5) | 10.5 (6.5) | −.39 | .16 |
| Treatment group | .05 | |||
| Time | <.001 | |||
| Treatment group × time | .07 | |||
| Anxiety | ||||
| Baseline | 47.4 (14.6) | 40.0 (12.7) | −.54 | .01 |
| 2 months | 41.7 (14.4) | 34.2 (10.7) | −.59 | .01 |
| 6 months | 41.1 (14.2) | 34.6 (10.4) | −.52 | .02 |
| Treatment group | .003 | |||
| Time | <.001 | |||
| Treatment group × time | .98 | |||
| MCS-12 | ||||
| Baseline | 40.4 (11.9) | 36.6 (8.8) | −.37 | .10 |
| 2 months | 40.8 (10.6) | 47.4 (9.2) | .66 | .007 |
| 6 months | 44.6 (10.9) | 49.7 (7.9) | .54 | .04 |
| Treatment group | .18 | |||
| Time | <.001 | |||
| Treatment group × time | <.001 | |||
| PCS-12 | ||||
| Baseline | 48.9 (10.7) | 53.5 (7.3) | .51 | .04 |
| 2 months | 48.1 (9.7) | 49.9 (9.1) | .19 | .36 |
| 6 months | 48.7 (11.0) | 51.0 (9.1) | .23 | .26 |
| Treatment group | .12 | |||
| Time | .03 | |||
| Treatment group × time | .35 | |||
| Caregiver burden | ||||
| Objective burden | ||||
| Baseline | 24.4 (3.9) | 24.8 (3.2) | .11 | .70 |
| 2 months | 23.3 (5.0) | 23.8 (3.6) | .11 | .58 |
| 6 months | 22.6 (5.2) | 22.1 (5.1) | −.11 | .67 |
| Treatment group | .84 | |||
| Time | <.001 | |||
| Treatment group × time | .63 | |||
| Subjective demand burden | ||||
| Baseline | 13.8 (3.7) | 13.0 (3.4) | −.22 | .31 |
| 2 months | 12.8 (3.5) | 12.0 (3.2) | −.25 | .24 |
| 6 months | 12.4 (3.0) | 11.0 (3.5) | −.42 | .09 |
| Treatment group | .07 | |||
| Time | .005 | |||
| Treatment group × time | .80 | |||
| Subjective stress burden | ||||
| Baseline | 16.9 (2.8) | 16.7 (2.3) | −.07 | .79 |
| 2 months | 15.6 (2.9) | 15.0 (2.3) | −.23 | .32 |
| 6 months | 14.7 (3.6) | 14.0 (3.5) | −.20 | .26 |
| Treatment group | .29 | |||
| Time | <.001 | |||
| Treatment group × time | .68 | |||
| Social support, total | ||||
| Baseline | 66.5 (20.8) | 63.5 (22.2) | −.14 | .61 |
| 2 months | 68.8 (21.8) | 71.1 (21.1) | .11 | .66 |
| 6 months | 73.0 (21.4) | 74.2 (21.0) | .06 | .84 |
| Treatment group | .95 | |||
| Time | .002 | |||
| Treatment group × time | .51 | |||
For each of the remaining outcomes, all participants reported improvement immediately following the intervention (i.e., anxiety) or steadily over time (i.e., objective burden, subjective demand, subjective stress, social support) such that there were no significant differences between MBSR and CCES participants at postintervention or 6 months, only significant improvement over time. Baseline differences in anxiety between MBSR and CCES participants remained stable as both improved consistently over time, whereas baseline differences in physical health diminished as MBSR participants improved slightly.
Discussion
We know of no other study that examined the use of MBSR for stress reduction in family caregivers of people with dementia residing in the community. Our study shows that MBSR is a feasible, acceptable intervention for caregivers based on study recruitment and retention; not only did we exceed our initial recruitment goal, we also retained most participants for the course of the study. Results show that MBSR was more effective than CCES at improving overall mental health, reducing stress, and decreasing depression postintervention (2 months), with both groups showing improvement in anxiety postintervention that was retained at 6 months. There were no differences between groups on social support or caregiver burden. The results suggest that MBSR could effectively reduce stress and improve mental health in caregivers of community-dwelling family members with dementia.
Improving the mental health and well-being of caregivers is becoming an increasingly important focus in dementia care as the number of families affected by dementia increases and the consequences of caregiving become clearer; these include poorer health (Pinquart & Sörensen, 2007; Schulz & Martire, 2004); declines in psychological, social, and emotional health (Ferrara et al., 2008); and increased mortality (Schulz & Beach, 1999). The participants in this study reported poorer overall mental health than the U.S. average on the mental health subscale of the SF-12 (Utah Department of Health, 2001). Participants in the MBSR group demonstrated significant improvement in their mental health scores immediately postintervention and sustained at 6 months. This was not the case for the CCES group, which showed little change in overall mental health scores (MCS-12) from baseline to postintervention and only slight improvement at 6 months, although their score on depression did show improvement at 6 months.
Stress is a major contributing factor to declining mental health and well-being, with chronic stress associated with increasing risk of depression, anxiety, and perception of burden (Clark, Bond, & Hecker, 2007; Cohen, Janicki-Deverts, & Miller, 2007). This is especially true for dementia care, where the trajectory can last a very long time and lead to higher levels of stress in the later stages (Pearlin, Mullan, Semple, & Skaff, 1990). A recent report (Cohen & Janicki-Deverts, 2011) using a U.S. sample showed mean PSS scores of 15.52 for men and 16.14 for women. This is far below the mean of 21.2 reported by study participants at baseline, who had been providing care for, on average, 4 years. There was little difference between the intervention groups on the PSS at baseline, with both groups reporting high levels of stress. However, there was a significant difference at postintervention as well as continued improvement seen at 6 months, with MBSR participants reporting less stress than CCES participants. Reported symptoms for depression and anxiety were also high at baseline for both groups, indicating mild to moderate levels of depression and elevated levels of anxiety. Similar to the trend we saw in stress, significant improvements were seen in depressive symptoms in the MBSR group at postintervention and in both groups by 6 months. Anxiety levels also improved in both groups postintervention and retained that improvement at 6 months.
The way in which MBSR affects mental health for caregivers is not entirely understood but likely has its basis in the foundational features of mindfulness and nonjudgmental awareness. This focus on present-moment experience and nonjudgmental acceptance has been shown to affect worry, rumination, and stress appraisal (Borders et al., 2010; Jain et al., 2007). Worry and rumination involve a focus on negative emotional states and thinking repetitively about their causes, meanings, and consequences, with a focus on past or future events rather than the present moment (Ramel, Goldin, & Carmona, 2004). Worry and rumination are also generally associated with higher levels of depression, anxiety, and negative mood (Nolen-Hoeksema, 2000). For those caring for a family member with dementia, worry and rumination over past events or a fearful future related to the trajectory of dementia can be significant.
Mindfulness and nonjudgmental acceptance of present-moment experience may also affect stress, depression, and anxiety through stress appraisal. In stress process theory (Folkman, 2008; Lazarus & Folkman, 1984), the appraisal of a stressful event is a cognitive process that distinguishes between the event and how we respond to it. How caregivers appraise the stress of caregiving is of increasing interest as interventions focus not only on altering stressors in the environment, such as dementia-related behavior problems, but also on how caregivers subjectively appraise those problems and how this affects mental health (Pearlin et al., 1990). In a study of caregiver appraisal, Mittleman and colleagues (2004) found that caregivers receiving a multicomponent counseling and support intervention significantly reduced their reaction ratings to dementia behaviors, resulting in decreased depression (Mittelman et al., 1995). MBSR may support the process of stress appraisal, leading to what Folkman (2008) has identified as meaning-focused coping, which in turn generates positive emotions in stress appraisal.
The improvements seen in mental health for caregivers in the MBSR intervention did not, however, extend to caregiver burden scores, which demonstrated only slight improvement in either intervention group. Caregiver burden is a challenging concept to both define and measure, given its multidimensional nature, which includes both subjective and objective components (Acton & Kang, 2001). The multiple features represented by the concept of burden may also require more of a multicomponent program targeted to the many dimensions of the caregiver experience associated with burden rather than an intervention such as MBSR directed singularly at stress reduction. Gitlin and colleagues (2003) highlighted this when discussing the multicomponent interventions of the REACH study; they concluded that caregivers benefit from a variety of approaches targeting the various aspects and unique experiences of the caregiver. They note that focusing on stress reduction, while it benefits overall mental health, stress, and depression, did not have a significant impact on caregiver burden. It should be noted however, that single-component interventions with a higher intensity of frequency and duration may also have a greater positive impact on the caregiver.
There are limitations to our study. Although results show short-term benefit in the use of MBSR for improving the mental health of caregivers, the long-term benefit has not been established and deserves further study. The daily practice of MBSR can also be a challenge to maintain over time, and identifying appropriate and needed support for continued practice will be critical to studying and understanding potential long-term outcomes. MBSR instructors trained to serve this population will also be critical. MBSR as a mind-body intervention can be challenging for caregivers to accept as a method of stress reduction. We experienced significant challenges in recruitment related to this reluctance, especially among minority populations. Our study population represents a predominately White caregiver group and may not reflect minority caregiver experiences (see also Whitebird et al., 2011). MBSR as an intervention for caregivers does, however, have many appealing features. It is a relatively low-cost intervention that is increasingly offered through a wide variety of organizations. This is important in an era when providing ongoing services for family caregivers is challenging due to the difficult economic and policy environment. MBSR also uses exercises and techniques that are easy to understand and, once learned, can be used every day to help calm and reduce emotional reactivity to frustrations that arise with dementia-related behaviors. This may help the caregiver marshal positive coping skills to manage the stress and challenge of caregiving.
There are many different approaches to improving mental health and reducing stress for caregivers. Multicomponent interventions offer an array of needed services but can also be expensive and geographically inaccessible for many caregivers. New interventions that do not depend on availability and funding of aging services in the community can offer important alternatives for caregivers seeking assistance with navigating the stress of caregiving. As Sörensen and colleagues (2002) note, caregivers have vastly different needs, and a one-size-fits-all approach may not be useful. MBSR offers a new and exciting opportunity to provide an innovative technique for stress reduction in one of the populations that need it most—those caring for a family member with dementia.
Funding
Research reported in this publication was supported by the National Center for Complementary and Alternative Medicine of the National Institutes of Health under award number R21AT003654. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Acton G. J., Kang J. (2001). Interventions to reduce the burden of caregiving for an adult with dementia: A meta-analysis. Research in Nursing and Health, 24, 349–360 Retrieved from http://onlinelibrary.wiley.com/doi/10.1002/nur.1036/abstract [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association (2012). 2012 Alzheimer’s disease facts and figures. Alzheimer’s and dementia: The Journal of the Alzheimer’s Association, 8, 131–168 Retrieved from http://www.alz.org/downloads/Facts_Figures_2012.pdf [DOI] [PubMed] [Google Scholar]
- Aschbacher K., von Känel R., Dimsdale J. E., Patterson T. L., Mills P. J., Mausbach B. T., et al. (2006). Dementia severity of the care receiver predicts procoagulant response in Alzheimer caregivers. American Journal of Geriatric Psychiatry, 14, 694–703. 10.1097/01.JGP.0000227969.36850.eb [DOI] [PubMed] [Google Scholar]
- Astin J. A., Shapiro S. L., Eisenberg D. M., Forys K. L. (2003). Mind-body medicine: State of the science, implications for practice. Journal of the American Board of Family Practice, 16, 131–147 Retrieved from http://www.jabfm.org/content/16/2/131.full.pdf [DOI] [PubMed] [Google Scholar]
- Baer R. A. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10, 125–143. 10.1093/clipsy.bpg015 [Google Scholar]
- Belle S. H., Burgio L., Burns R., Coon D., Czaja S. J., Gallagher-Thompson D., et al. (2006). Can providing support to dementia caregivers improve their quality of life? [Summaries for Patients]. Annals of Internal Medicine, 145, 727–738 Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2585490/pdf/nihms72020.pdf 17116917 [Google Scholar]
- Bishop S. R. (2002). What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine, 64, 71–83 Retrieved from http://www.psychosomaticmedicine.org/content/64/1/71.full.pdf [DOI] [PubMed] [Google Scholar]
- Borders A., Earleywine M., Jajodia A. (2010). Could mindfulness decrease anger, hostility, and aggression by decreasing rumination? Aggressive Behavior, 36, 28–44. 10.1002/ab.20327 [DOI] [PubMed] [Google Scholar]
- Chambers R., Gullone E., Allen N. B. (2009). Mindful emotion regulation: An integrative review. Clinical Psychology Review, 29, 560–57210.1016/j.cpr.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Clark M. S., Bond M. J., Hecker J. R. (2007). Environmental stress, psychological stress and allostatic load. Psychology, Health & Medicine, 12, 18–30. 10.1080/13548500500429338 [DOI] [PubMed] [Google Scholar]
- Cohen S., Williamson G. (1988). Percieved stress in a probability sample of the United States. In Sapcapam S., Oskamp S. (Eds.), The social psychology of health: Claremont Symposium on applied social psychology. Newbury Park, CA: Sage [Google Scholar]
- Cohen S., Janicki-Deverts D. (2011). Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006 and 2009 Retrieved from http://www.psy.cmu.edu/~scohen/Cohen_Janicki_PSS_JASP_2010.doc
- Cohen S., Janicki-Deverts D., Miller G. E. (2007). Psychological stress and disease. JAMA, 298, 1685–1687. 10.1001/jama.298.14.1685 [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396 Retrieved from http://hsb.sagepub.com/ [PubMed] [Google Scholar]
- Cullen M. (2011). Mindfulness-based interventions: An emerging phenomenon. Mindfulness, 2, 186–193. 10.1007/s12671-011-0058-1 [Google Scholar]
- Elliott A. F., Burgio L. D., Decoster J. (2010). Enhancing caregiver health: Findings from the resources for enhancing Alzheimer’s caregiver health II intervention. Journal of the American Geriatrics Society, 58, 30–3710.1111/j.1532-5415.2009.02631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrara M., Langiano E., Di Brango T., De Vito E., Di Cioccio L., Bauco C. (2008). Prevalence of stress, anxiety and depression in with Alzheimer caregivers. Health and Quality of Life Outcomes, 6, 93. 10.1186/1477-7525-6-93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjorback L. O., Arendt M., Ornbol E., Fink P., Walach H. (2011). Mindfulness-based stress reduction and mindfulness-based cognitive therapy: A systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica, 124, 102–119. 10.1111/j.1600-0447.2011.01704.x [DOI] [PubMed] [Google Scholar]
- Folkman S. (2008). The case for positive emotions in the stress process. Anxiety Stress Coping, 21, 3–14. 10.1080/10615800701740457 [DOI] [PubMed] [Google Scholar]
- Gitlin L. N., Belle S. H., Burgio L. D., Czaja S. J., Mahoney D., Gallagher-Thompson D., et al. (2003). Effect of multicomponent interventions on caregiver burden and depression: the REACH multisite initiative at 6-month follow-up. Psychology and Aging, 18, 361–374. 10.1037/0882-7974.18.3.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross C. R., Kreitzer M. J., Reilly-Spong M., Wall M., Winbush N. Y., Patterson R., et al. (2011). Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: A randomized controlled clinical trial. Explore (NY), 7, 76–87. 10.1016/j.explore.2010.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross C. R., Kreitzer M. J., Russas V., Treesak C., Frazier P. A., Hertz M. I. (2004). Mindfulness meditation to reduce symptoms after organ transplant: a pilot study. Alternative Therapies in Health and Medicine, 10, 58–66 Retrieved from http://www.alternative-therapies.com/index.cfm/fuseaction/archives.display/action/download/id/7261 [PubMed] [Google Scholar]
- Gross C. R., Kreitzer M. J., Thomas W., Reilly-Spong M., Cramer-Bornemann M., Nyman J. A., et al. (2010). Mindfulness-based stress reduction for solid organ transplant recipients: A randomized controlled trial. Alternative Therapies in Health and Medicine, 16, 30–38 Retrieved from www.alternative-therapies.com [PMC free article] [PubMed] [Google Scholar]
- Grossman P., Niemann L., Schmidt S., Walach H. (2004). Mindfulness-based stress reduction and health benefits. A meta-analysis. Journal of Psychosomatic Research, 57, 35–43. 10.1016/S0022-3999(03)00573-7 [DOI] [PubMed] [Google Scholar]
- Grossman P., Tiefenthaler-Gilmer U., Raysz A., Kesper U. (2007). Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychotherapy and Psychosomatics, 76, 226–233. 10.1159/ 000101501 [DOI] [PubMed] [Google Scholar]
- Hofmann S. G., Sawyer A. T., Witt A. A., Oh D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183. 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain S., Shapiro S. L., Swanick S., Roesch S. C., Mills P. J., Bell I., Schwartz G. E. (2007). A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine, 33, 11–21. 10.1207/s15324796abm3301_2 [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. (1990). Full Catastrophe Living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing [Google Scholar]
- Kabat-Zinn J., Wheeler E., Light T., Skillings A., Scharf M. J., Cropley T. G., et al. (1998). Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA). Psychosomatic Medicine, 60, 625–632 Retrieved from http://www.psychosomaticmedicine.org/content/60/5/625.full.pdf [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser J. K., Preacher K. J., MacCallum R. C., Atkinson C., Malarkey W. B., Glaser R. (2003). Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proceedings of the National Academy of Sciences of the United States of America, 100, 9090–9095. 10.1073/pnas.1531903100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreitzer M. J., Gross C. R., Ye X., Russas V., Treesak C. (2005). Longitudinal impact of mindfulness meditation on illness burden in solid-organ transplant recipients. Progress in Transplantation, 15, 166–172 Retrieved from http://natco.metapress.com/ [DOI] [PubMed] [Google Scholar]
- Kuyken W., Byford S., Taylor R. S., Watkins E., Holden E., White K., et al. (2008). Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. Journal of Consulting and Clinical Psychology, 76, 966–978. 10.1037/a0013786 [DOI] [PubMed] [Google Scholar]
- Lavretsky H., Epel E. S., Siddarth P., Nazarian N., Cyr N. S., Khalsa D. S., et al. (2012). A pilot study of yogic meditation for family dementia caregivers with depressive symptoms: effects on mental health, cognition, and telomerase activity. International Journal of Geriatric Psychiatry. 10.1002/gps.3790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R., Folkman S. (1984). Stress, appraisal, and coping. New York: Springer [Google Scholar]
- Ledesma D., Kumano H. (2008). Mindfulness-based stress reduction and cancer: A meta-analysis. Psycho-Oncology, 18, 571–579. 10.1002/pon.1400 [DOI] [PubMed] [Google Scholar]
- Lengacher C. A., Johnson-Mallard V., Post-White J., Moscoso M. S., Jacobsen P. B., Klein T. W., et al. (2009). Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-Oncology, 18, 1261–1272. 10.1002/pon.1529 [DOI] [PubMed] [Google Scholar]
- Littell R. C., Milliken G. A., Stroup W. W., Wolfinger R. D., Schabenberger O. (Eds.). (2006). SAS® for mixed models (2nd ed.). Cary, NC: SAS Institute Inc [Google Scholar]
- McCracken L. M., Gauntlett-Gilbert J., Vowles K. E. (2007). The role of mindfulness in a contextual cognitive-behavioral analysis of chronic pain-related suffering and disability. Pain, 131, 63–69. 10.1016/j.pain.2006.12.013 [DOI] [PubMed] [Google Scholar]
- McDowell I., Newell C. (2006). Measuring health: A guide to rating scales and questionnaires (3rd ed.). New York: Oxford University Press [Google Scholar]
- Minor H. G., Carlson L. E., Mackenzie M. J., Zernicke K., Jones L. (2006). Evaluation of a Mindfulness-Based Stress Reduction (MBSR) program for caregivers of children with chronic conditions. Social Work in Health Care, 43, 91–109. 10.1300/J010v43n01_06 [DOI] [PubMed] [Google Scholar]
- Mittelman M. S., Ferris S. H., Shulman E., Steinberg G., Ambinder A., Mackell J. A., Cohen J. (1995). A comprehensive support program: Effect on depression in spouse-caregivers of AD patients. Gerontologist, 35, 792–802. 10.1093/geront/35.6.792 [DOI] [PubMed] [Google Scholar]
- Mittelman M. S., Roth D. L., Haley W. E., Zarit S. H. (2004). Effects of a caregiver intervention on negative caregiver appraisals of behavior problems in patients with Alzheimer’s disease: results of a randomized trial. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 59, P27–P34. 10.1093/geront/35.6.792 [DOI] [PubMed] [Google Scholar]
- Montgomery R. J. V. (2002). Using and Interpreting the Montgomery Borgatta Caregiver Burden Scale Retrieved from http://www4.uwm.edu/hbssw/pdf/burden
- Montgomery R. J. V., Borgatta E. F., Borgatta M. L. (2000). Societal and family change in the burden of care. In Lui W. T., Kendig H. (Eds.), Who should care for the elderly? An East-West value divide. Singapore: The National University of Singapore Press [Google Scholar]
- Nolen-Hoeksema S. (2000). The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology, 109, 504–511. 10.1037/0021-843X.109.3.504 [PubMed] [Google Scholar]
- Peacock S. C., Forbes D. A. (2003). Interventions for caregivers of persons with dementia: a systematic review. Canadian Journal of Nursing Research, 35, 88–107 Retrieved from http://cjnr.mcgill.ca/archives.html# [PubMed] [Google Scholar]
- Pearlin L. I., Mullan J. T., Semple S. J., Skaff M. M. (1990). Caregiving and the stress process: an overview of concepts and their measures. Gerontologist, 30, 583–594. 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2007). Correlates of physical health of informal caregivers: a meta-analysis. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 62, P126–P137. 62/2/P126 [DOI] [PubMed] [Google Scholar]
- Pradhan E. K., Baumgarten M., Langenberg P., Handwerger B., Gilpin A. K., Magyari T., et al. (2007). Effect of Mindfulness-Based Stress Reduction in rheumatoid arthritis patients. Arthritis and Rheumatism, 57, 1134–1142. 10.1002/art.23010 [DOI] [PubMed] [Google Scholar]
- Ramel W., Goldin P. R., Carmona P. E. (2004). The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cognitive Therapy and Research, 28, 433–455. 10.1023/BCOTR.0000045557.15923.96 [Google Scholar]
- Rosenzweig S., Reibel D. K., Greeson J. M., Edman J. S., Jasser S. A., McMearty K. D., Goldstein B. J. (2007). Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Alternative Therapies in Health and Medicine, 13, 36–38 Retrieved from http://www.alternative-therapies.com [PubMed] [Google Scholar]
- Schulz R., Beach S. R. (1999). Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA, 282, 2215–2219. joc91040 [DOI] [PubMed] [Google Scholar]
- Schulz R., Martire L. M. (2004). Family caregiving of persons with dementia: prevalence, health effects, and support strategies. American Journal of Geriatric Psychiatry, 12, 240–249 Retrieved from http://journals.lww.com/ajgponline/pages/default.aspx [PubMed] [Google Scholar]
- Schulz R., O’Brien A., Czaja S., Ory M., Norris R., Martire L. M., et al. (2002). Dementia caregiver intervention research: in search of clinical significance. Gerontologist, 42, 589–602 Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2579772/pdf/nihms72032.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sörensen S., Duberstein P., Gill D., Pinquart M. (2006). Dementia care: mental health effects, intervention strategies, and clinical implications. Lancet Neurology, 5, 961–973. 10.1016/S1474-4422(06)70599-3 [DOI] [PubMed] [Google Scholar]
- Sörensen S., Pinquart M., Duberstein P. (2002). How effective are interventions with caregivers? An updated meta-analysis. Gerontologist, 42, 356–372. 10.1093/geront/42.3.356 [DOI] [PubMed] [Google Scholar]
- Spelberger C. D. (1983). Manual for the State-Trait Anxiety Inventory for Adults. Palo Alto, CA: Consulting Psychologists Press, Mind Garden Inc [Google Scholar]
- Stone L. J., Clements J. A. (2009). The effects of nursing home placement on the perceived levels of caregiver burden. Journal of Gerontological Social Work, 52, 193–214. 10.1080/01634370802609163 [DOI] [PubMed] [Google Scholar]
- Teasdale J. D., Segal Z. V., Williams J. M., Ridgeway V. A., Soulsby J. M., Lau M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68, 615–623. 10.1037/0022-006X.68.4.615 [DOI] [PubMed] [Google Scholar]
- Utah Department of Health (2001). Utah health status survey Retrieved November 21, 2011, from http://health.utah.gov/opha/publications/2001hss/sf12/SF12_Interpreting.pdf
- Verbeke G., Molenberghs G. (2000). Linear mixed models for longitudinal data. New York: Springer-Verlag [Google Scholar]
- Waelde L. C., Thompson L., Gallagher-Thompson D. (2004). A pilot study of a yoga and meditation intervention for dementia caregiver stress. Journal of Clinical Psychology, 60, 677–687. 10.1002/jclp.10259 [DOI] [PubMed] [Google Scholar]
- Whitebird R. R., Kreitzer M. J., Lewis B. A., Hanson L. R., Crain A. L., Enstad C. J., Mehta A. (2011). Recruiting and retaining family caregivers to a randomized controlled trial on mindfulness-based stress reduction. Contemporary Clinical Trials, 32, 654–661. 10.1016/j.cct.2011.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitebird R. R., Kreitzer M. J., O’Connor P. J. (2009). Mindfulness-based stress reduction and diabetes. Diabetes Spectrum, 22, 226–230. 10.2337/diaspect.22.4.226 [DOI] [PMC free article] [PubMed] [Google Scholar]