Abstract
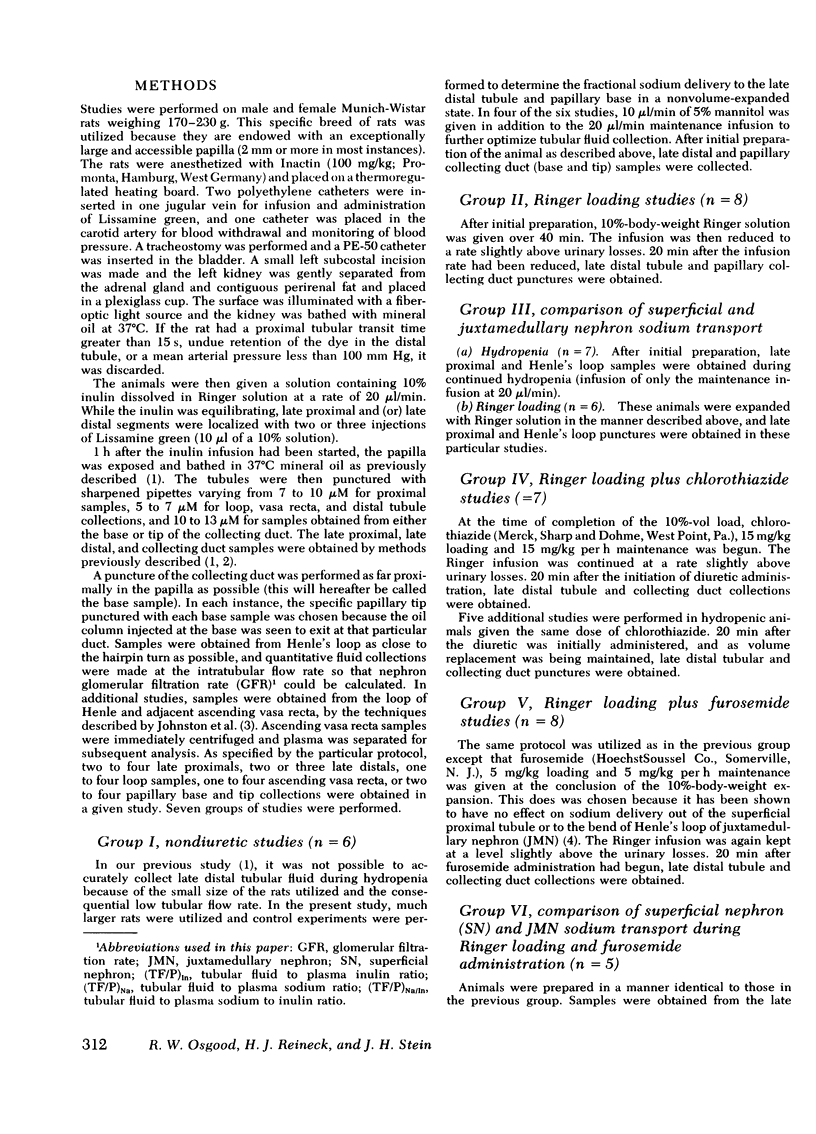
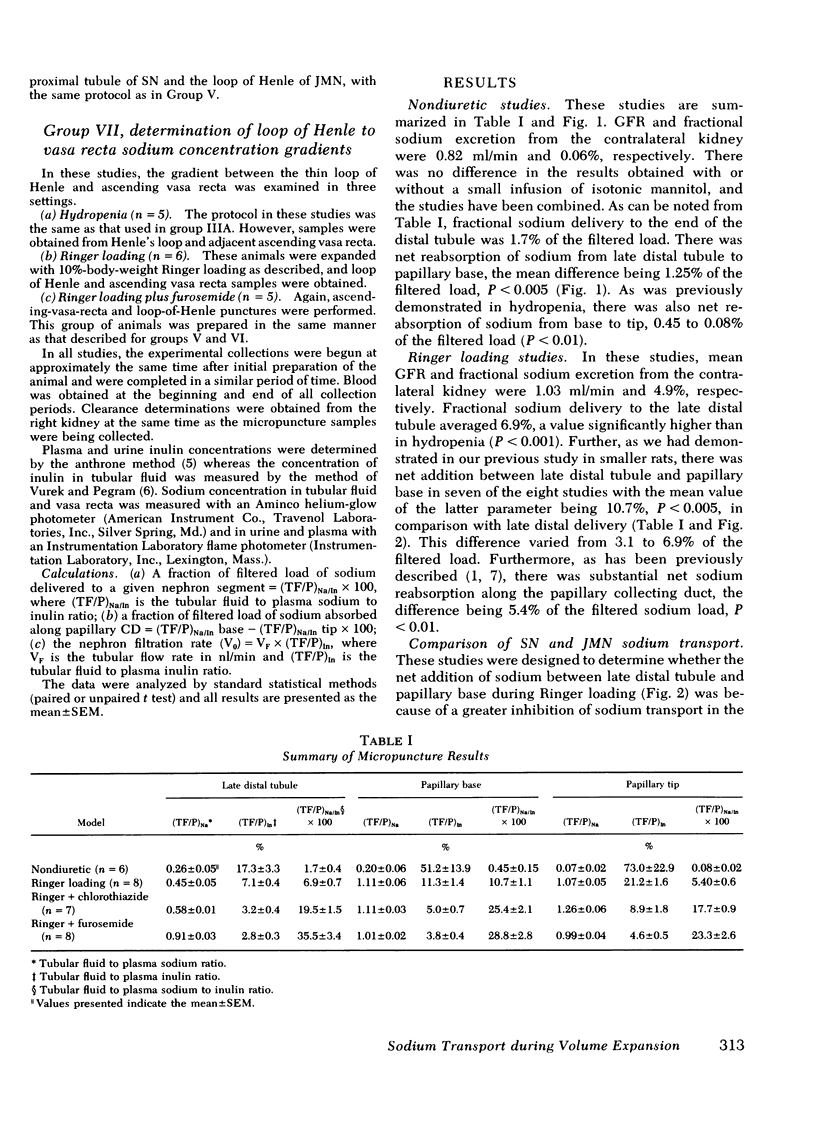
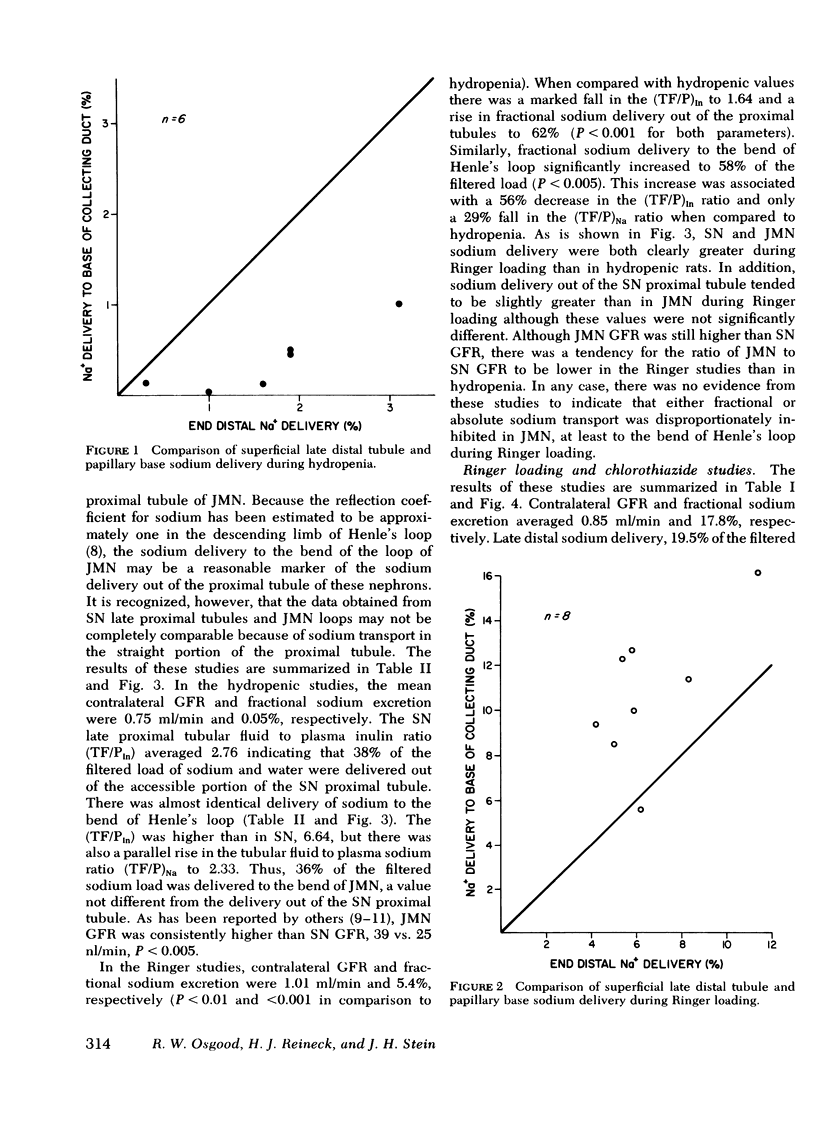
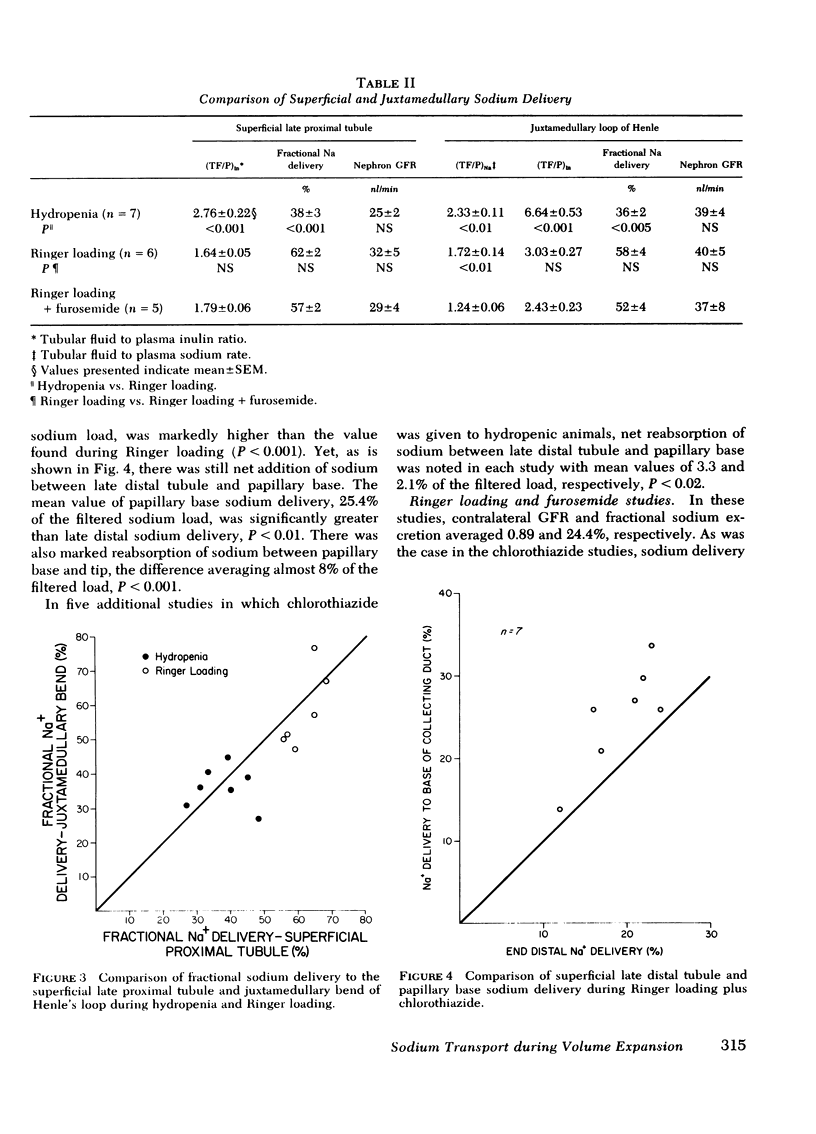
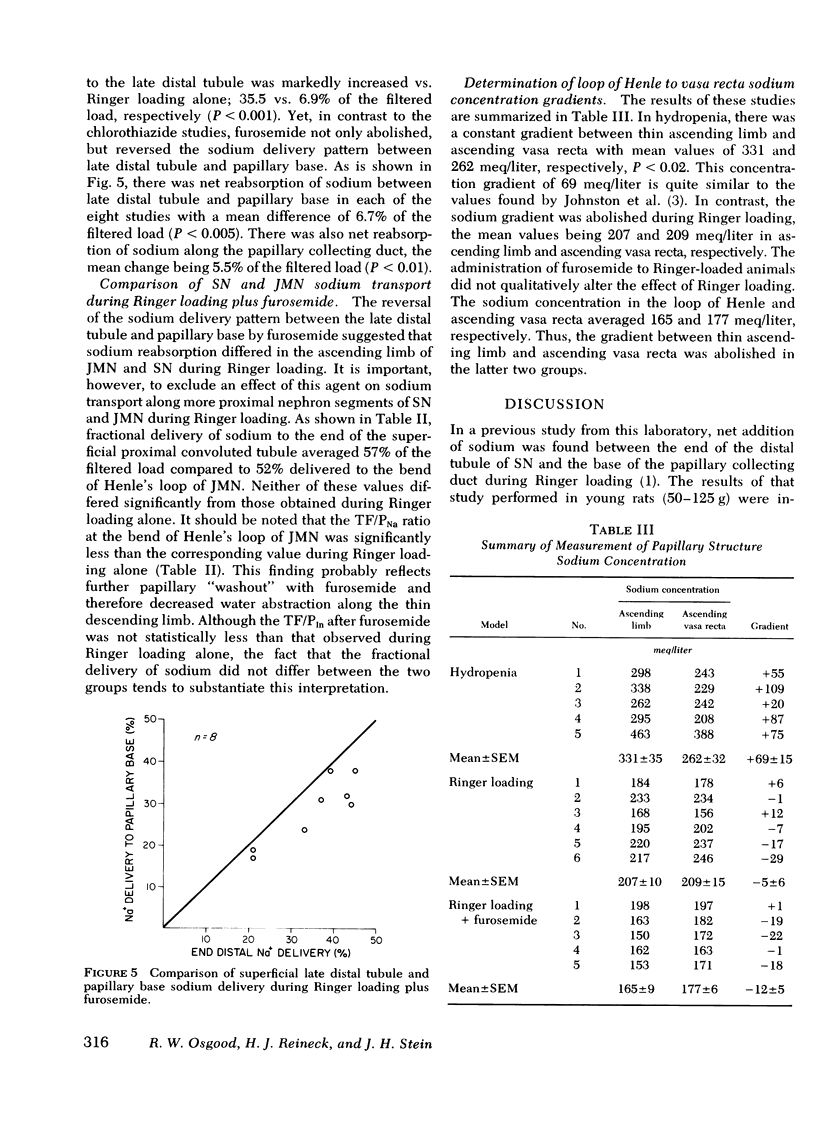
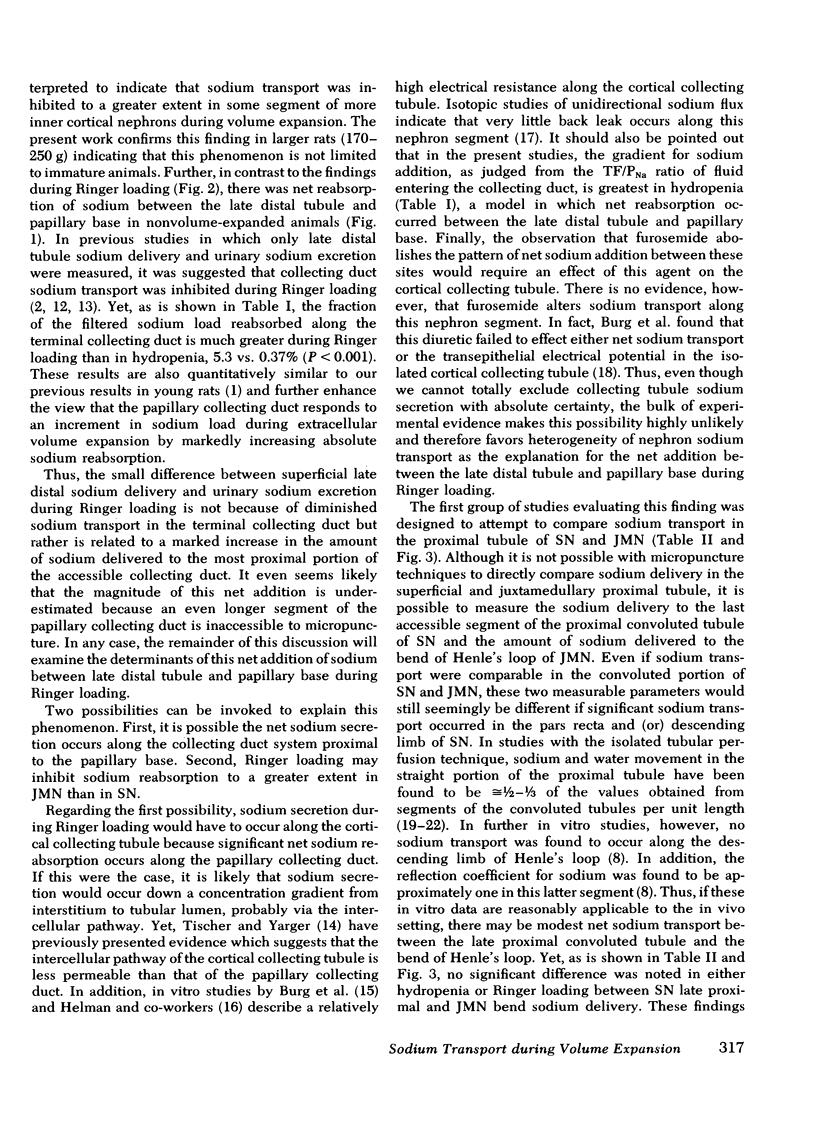
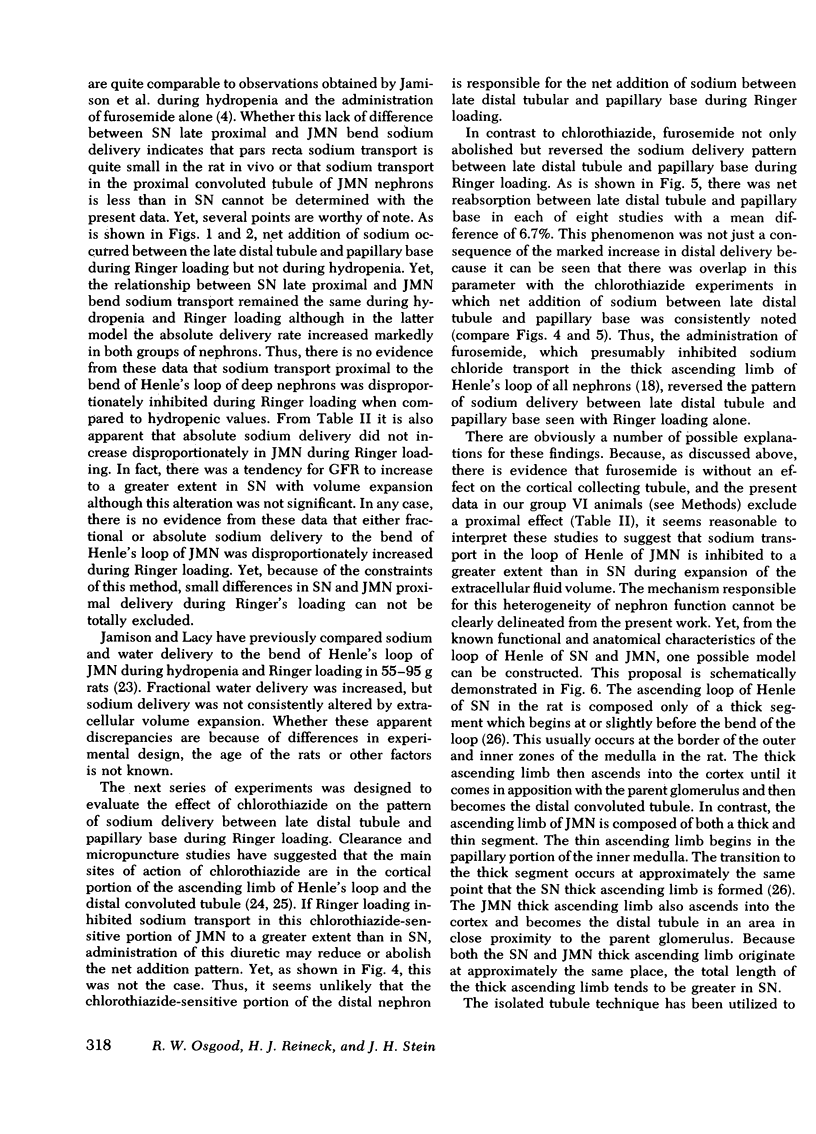
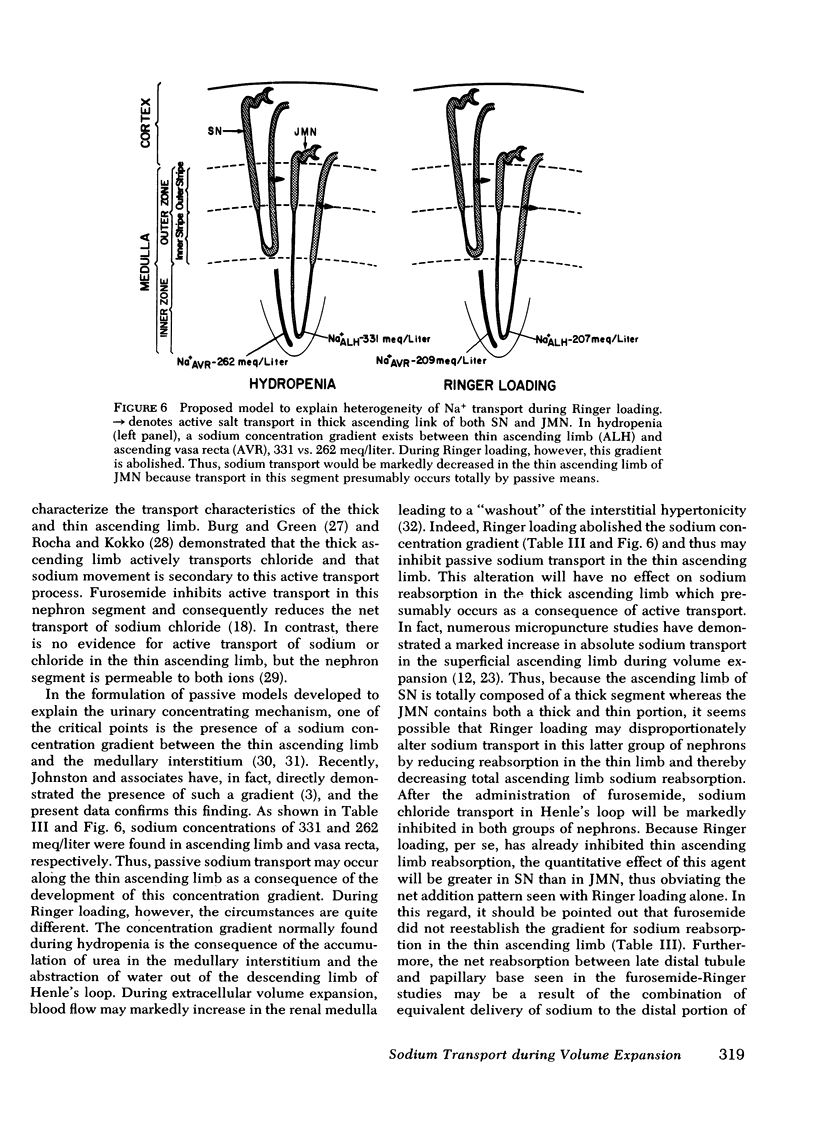
The present studies were designed to further investigate the possibility of heterogeneity of nephron function during Ringer loading in the rat, and to determine the specific nephron segment responsible for this finding. As in previous studies from this laboratory with smaller rats (50-125 g), net addition of sodium between late distal tubule and papillary base (6.9 vs. 10.4% of the filtered load, respectively, P <0.005) was found in more mature rats (170-230 g). In contrast, there was net reabsorption of sodium between these two segments in nonvolume-expanded animals, 1.70 vs. 0.45% of the filtered sodium load, P <0.005. Because nephron heterogeneity of sodium transport during extracellular volume expansion is the most likely explanation for these findings, further studies were performed to determine the specific juxtamedullary nephron segment responsible for the net addition pattern between late distal tubule and papillary base in Ringer-loaded animals. First, a comparison was made of sodium delivery to the late proximal tubule of superficial nephrons vs. the delivery rate to the bend of Henle's loop of juxtamedullary nephrons in both hydropenia and Ringer loading. Fractional sodium delivery was quite comparable between the superficial and juxtamedullary nephrons in both hydropenia and Ringer loading although the absolute level was much greater in both groups of nephrons in the Ringer studies. Chlorothiazide (15 mg/kg loading and 15 mg/kg per h) given during Ringer loading markedly increased late distal sodium delivery, 19% of the filtered load, but did not prevent net addition of sodium at the papillary base. In contrast, furosemide (5 mg/kg loading and 5/mg/kg per h) given during Ringer loading completely reversed the segmental pattern, 35.5 and 28.8% at late distal tubule and papillary base, respectively, P <0.005. These studies demonstrate that the net addition of sodium between late distal tubule and papillary base during Ringer loading is not limited to immature rats and that the segmental pattern does not occur in non-volume-expanded animals. Further, the reversal of the net addition pattern with furosemide, but not chlorothiazide, and the comparable proximal nephron delivery rates in Ringer loading suggest that the loop of Henle of juxtamedullary nephrons reabsorbs less sodium than the same portion of superficial nephrons in this setting. A model is proposed to explain this finding.
Full text
PDF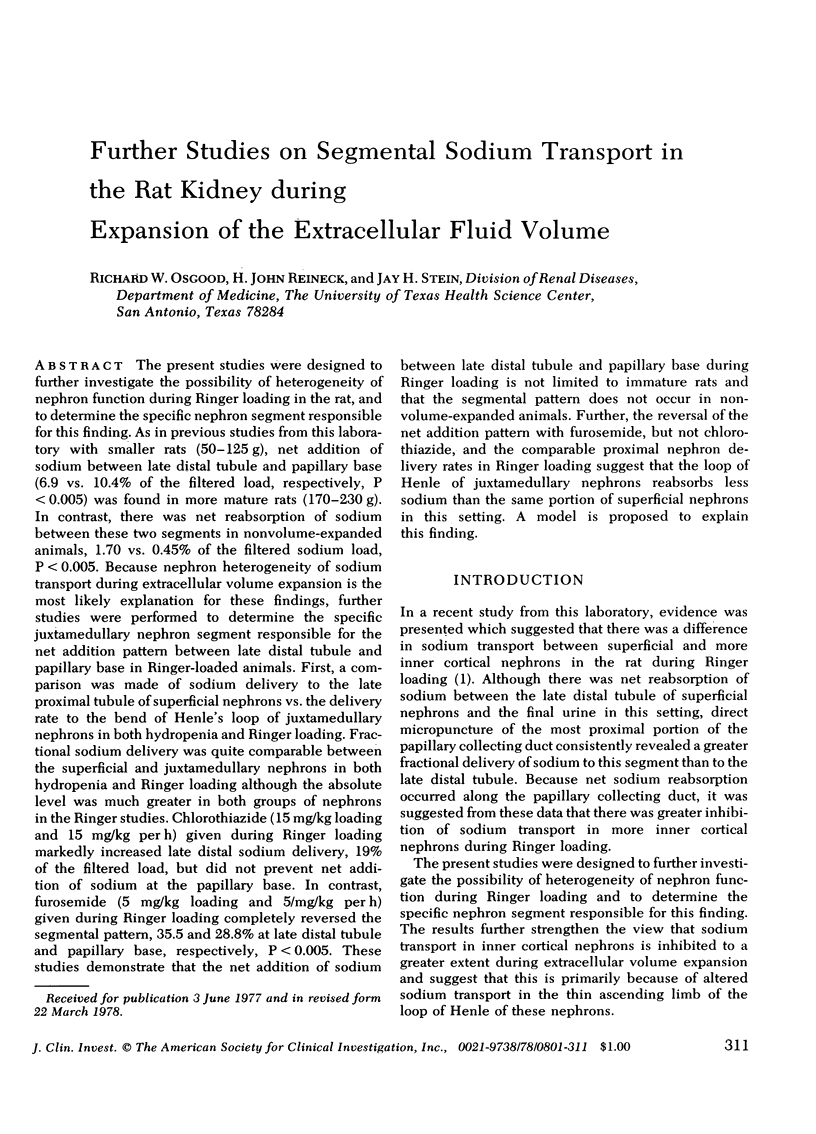
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Burg M. B., Green N. Function of the thick ascending limb of Henle's loop. Am J Physiol. 1973 Mar;224(3):659–668. doi: 10.1152/ajplegacy.1973.224.3.659. [DOI] [PubMed] [Google Scholar]
- Burg M. B., Issaacson L., Grantham J., Orloff J. Electrical properties of isolated perfused rabbit renal tubules. Am J Physiol. 1968 Oct;215(4):788–794. doi: 10.1152/ajplegacy.1968.215.4.788. [DOI] [PubMed] [Google Scholar]
- Burg M., Patlak C., Green N., Villey D. Organic solutes in fluid absorption by renal proximal convoluted tubules. Am J Physiol. 1976 Aug;231(2):627–637. doi: 10.1152/ajplegacy.1976.231.2.627. [DOI] [PubMed] [Google Scholar]
- Burg M., Stoner L., Cardinal J., Green N. Furosemide effect on isolated perfused tubules. Am J Physiol. 1973 Jul;225(1):119–124. doi: 10.1152/ajplegacy.1973.225.1.119. [DOI] [PubMed] [Google Scholar]
- Diezi J., Michoud P., Aceves J., Giebisch G. Micropuncture study of electrolyte transport across papillary collecting duct of the rat. Am J Physiol. 1973 Mar;224(3):623–634. doi: 10.1152/ajplegacy.1973.224.3.623. [DOI] [PubMed] [Google Scholar]
- EARLEY L. E., KAHN M., ORLOFF J. The effects of infusions of chlorothiazide on urinary dilution and concentration in the dog. J Clin Invest. 1961 May;40:857–866. doi: 10.1172/JCI104320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FUHR J., KACZMARCZYK J., KRUTTGEN C. D. Eine einfache colorimetrische Methode zur Inulinbestimmung für Nieren-Clearance-Untersuchungen bei Stoffwechselgesunden und Diabetikern. Klin Wochenschr. 1955 Aug 1;33(29-30):729–730. doi: 10.1007/BF01473295. [DOI] [PubMed] [Google Scholar]
- Frindt G., Burg M. B. Effect of vasopressin on sodium transport in renal cortical collecting tubules. Kidney Int. 1972 Apr;1(4):224–231. doi: 10.1038/ki.1972.32. [DOI] [PubMed] [Google Scholar]
- Hamburger R. J., Lawson N. L., Dennis V. W. Effects of cyclic adenosine nucleotides on fluid absorption by different segments of proximal tubule. Am J Physiol. 1974 Aug;227(2):396–401. doi: 10.1152/ajplegacy.1974.227.2.396. [DOI] [PubMed] [Google Scholar]
- Helman S. I., Grantham J. J., Burg M. B. Effect of vasopressin on electrical resistance of renal cortical collecting tubules. Am J Physiol. 1971 Jun;220(6):1825–1832. doi: 10.1152/ajplegacy.1971.220.6.1825. [DOI] [PubMed] [Google Scholar]
- Horster M., Thurau K. Micropuncture studies on the filtration rate of single superficial and juxtamedullary glomeruli in the rat kidney. Pflugers Arch Gesamte Physiol Menschen Tiere. 1968;301(2):162–181. doi: 10.1007/BF00362733. [DOI] [PubMed] [Google Scholar]
- Imai M., Kokko J. P. Effect of peritubular protein concentration on reabsorption of sodium and water in isolated perfused proxmal tubules. J Clin Invest. 1972 Feb;51(2):314–325. doi: 10.1172/JCI106816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai M., Kokko J. P. Sodium chloride, urea, and water transport in the thin ascending limb of Henle. Generation of osmotic gradients by passive diffusion of solutes. J Clin Invest. 1974 Feb;53(2):393–402. doi: 10.1172/JCI107572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamison R. L., Lacy F. B. Effect of saline infusion on superficial and juxtamedullary nephrons in the rat. Am J Physiol. 1971 Sep;221(3):690–697. doi: 10.1152/ajplegacy.1971.221.3.690. [DOI] [PubMed] [Google Scholar]
- Jamison R. L., Lacy F. B., Pennell J. P., Sanjana V. M. Potassium secretion by the decending limb or pars recta of the juxtamedullary nephron in vivo. Kidney Int. 1976 Apr;9(4):323–332. doi: 10.1038/ki.1976.38. [DOI] [PubMed] [Google Scholar]
- Jamison R. L. Micropuncture study of superficial and juxtamedullary nephrons in the rat. Am J Physiol. 1970 Jan;218(1):46–55. doi: 10.1152/ajplegacy.1970.218.1.46. [DOI] [PubMed] [Google Scholar]
- Johnston P. A., Battilana C. A., Lacy F. B., Jamison R. L. Evidence for a concentration gradient favoring outward movement of sodium from the thin loop of Henle. J Clin Invest. 1977 Feb;59(2):234–240. doi: 10.1172/JCI108633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamura S., Imai M., Seldin D. W., Kukko J. P. Characteristics of salt and water transport in superficial and juxtamedullary straight segments of proximal tubules. J Clin Invest. 1975 Jun;55(6):1269–1277. doi: 10.1172/JCI108046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokko J. P., Rector F. C., Jr Countercurrent multiplication system without active transport in inner medulla. Kidney Int. 1972 Oct;2(4):214–223. doi: 10.1038/ki.1972.97. [DOI] [PubMed] [Google Scholar]
- Kokko J. P. Sodium chloride and water transport in the descending limb of Henle. J Clin Invest. 1970 Oct;49(10):1838–1846. doi: 10.1172/JCI106401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunau R. T., Jr, Weller D. R., Webb H. L. Clarification of the site of action of chlorothiazide in the rat nephron. J Clin Invest. 1975 Aug;56(2):401–407. doi: 10.1172/JCI108105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landwehr D. M., Klose R. M., Giebisch G. Renal tubular sodium and water reabsorption in the isotonic sodium chloride-loaded rat. Am J Physiol. 1967 Jun;212(6):1327–1333. doi: 10.1152/ajplegacy.1967.212.6.1327. [DOI] [PubMed] [Google Scholar]
- Rocha A. S., Kokko J. P. Sodium chloride and water transport in the medullary thick ascending limb of Henle. Evidence for active chloride transport. J Clin Invest. 1973 Mar;52(3):612–623. doi: 10.1172/JCI107223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solez K., Kramer E. C., Fox J. A., Heptinstall R. H. Medullary plasma flow and intravascular leukocyte accumulation in acute renal failure. Kidney Int. 1974 Jul;6(1):24–37. doi: 10.1038/ki.1974.74. [DOI] [PubMed] [Google Scholar]
- Sonnenberg H. Renal response to blood volume expansion: distal tubular function and urinary excretion. Am J Physiol. 1972 Oct;223(4):916–924. doi: 10.1152/ajplegacy.1972.223.4.916. [DOI] [PubMed] [Google Scholar]
- Stein J. H., Osgood R. W., Boonjarern S., Cox J. W., Ferris T. F. Segmental sodium reabsorption in rats with mild and severe volume depletion. Am J Physiol. 1974 Aug;227(2):351–359. doi: 10.1152/ajplegacy.1974.227.2.351. [DOI] [PubMed] [Google Scholar]
- Stein J. H., Osgood R. W., Boonjarern S., Ferris T. F. A comparison of the segmental analysis of sodium reabsorption during Ringer's and hyperoncotic albumin infusion in the rat. J Clin Invest. 1973 Sep;52(9):2313–2323. doi: 10.1172/JCI107420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein J. H., Osgood R. W., Kunau R. T., Jr Direct measurement of papillary collecting duct sodium transport in the rat. Evidence for heterogeneity of nephron function during Ringer loading. J Clin Invest. 1976 Oct;58(4):767–773. doi: 10.1172/JCI108527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson J. L. Concentration of urine in a central core model of the renal counterflow system. Kidney Int. 1972 Aug;2(2):85–94. doi: 10.1038/ki.1972.75. [DOI] [PubMed] [Google Scholar]
- Stumpe K. O., Lowitz H. D., Ochwadt B. Function of juxtamedullary nephrons in normotensive and chronically hypertensive rats. Pflugers Arch. 1969;313(1):43–52. doi: 10.1007/BF00586327. [DOI] [PubMed] [Google Scholar]


