Abstract
Objective
Autism spectrum disorder (ASD) is associated with amplified emotional responses and poor emotional control, but little is known about the underlying mechanisms. This paper provides a conceptual and methodological framework for understanding compromised emotion regulation (ER) in ASD.
Method
After defining ER and related constructs, methods to study ER were reviewed with special consideration on how to apply these approaches to ASD. Against the backdrop of cognitive characteristics in ASD and existing ER theories, available research was examined to identify likely contributors to emotional dysregulation in ASD.
Results
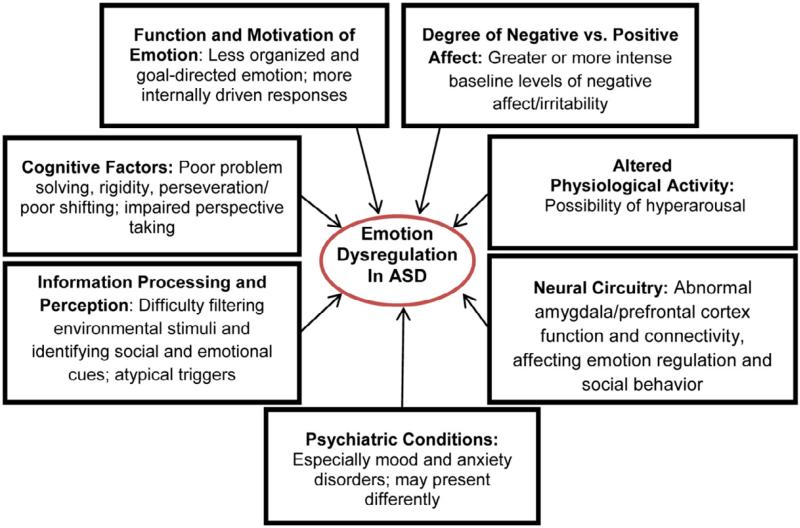
Little is currently known about ER in youth with ASD. Some mechanisms that contribute to poor ER in ASD may be shared with other clinical populations (e.g., physiological arousal, degree of negative and positive affect, alterations in the amygdala and prefrontal cortex), whereas other mechanisms may be more unique to ASD (e.g., differences in information processing/perception, cognitive factors (e.g., rigidity), less goal-directed behavior and more disorganized emotion in ASD).
Conclusions
Although assignment of concomitant psychiatric diagnoses is warranted in some cases, poor ER may be inherent in ASD and may provide a more parsimonious conceptualization for the many associated socio-emotional and behavioral problems in this population. Further study of ER in youth with ASD may identify meaningful subgroups of patients and lead to more effective individualized treatments.
Keywords: arousal, autism spectrum disorder, comorbidity, emotion regulation, psychiatric disorders
Autism spectrum disorder (ASD), a neurodevelopmental condition diagnosed on the basis of impairments in socialization and social communication, as well as the presence of restricted and repetitive behaviors,1 is estimated to affect 1 in 88 in school age children.2 Emerging consensus indicates that ASD involves disruptions in connectivity and processing across brain regions.3 Thus, the impairments associated with ASD are pervasive, including a significant impact on emotional functioning.3 Common associated problems include irritability, aggression, self-injury, anxiety, and impulsivity.4
Emotion regulation (ER) is a construct that may provide explanatory power for understanding the observed emotional and behavioral problems in ASD. ER is generally defined as the automatic or intentional modification of a person’s emotional state that promotes adaptive or goal-directed behavior.5 Individuals with ASD may fail to employ adaptive ER strategies and instead react impulsively to emotional stimuli with tantrums, aggression, or self-injury.6 Such behaviors are often interpreted as deliberate or defiant, but may be due to inadequate management of emotion.7
A common presenting complaint that exemplifies impaired ER in ASD includes intense reactions to stress or outbursts that are colloquially referred to as ‘meltdowns.’8 The concern about ‘meltdowns’ can be inferred by the popularity of resources on this topic. For example, using the search-words of ‘meltdown and autism’ on Amazon.com identified 50 books. By contrast, a PsychInfo search of peer-reviewed articles with ‘emotion regulation’ and ‘autism’ in the abstract produced only 15 articles (10/12/12). This suggests a marked discrepancy between the perceived importance of these problems in ASD and the empirical investigation of the phenomenon. This paper aims to accelerate research on the processes underlying the expression and experience of impaired ER in ASD.
TERMS AND CONCEPTS
The study of ER can be traced back to early research on temperament. Temperament is a broader construct than ER, encompassing biologically-based individual differences in affective, attentional, and motor reactivity or response.9 The scientific study of ER as a distinct construct emerged only a few decades ago.10-11 Since then, there has been a burgeoning of research and proposed clinical approaches devoted to ER.12
Despite its widespread use, the definition of ER is not straightforward. Emotions allow rapid appraisal of situations (external or internal stimuli) and preparation of subsequent actions to maintain wellbeing. Thus, emotions emanate from an individual’s evaluation of a stimulus.13-14 The initial strength (i.e., intensity, speed) of this emotional response is often referred to as emotional reactivity or emotionality.15 The term regulation implies efforts to modify or control the intensity of the emotional reaction, usually in the service of an individual goal.5 The relation of emotionality and ER has been debated, with some researchers supporting a clear distinction,16 and others contending that emotion/emotionality and ER are inseparable.17 It is also important to distinguish between mood (e.g., depression) and emotion (e.g., sadness). Mood is a stable and enduring state, whereas emotion is usually tied to the appraisal of a specific situation and a subsequent behavioral response.13
The emotional response involves multiple domains, such as behavior, subjective experience, and physiology. Definitions of ER have also included consideration of attention and motivation.18 A point of difference between emotionality and ER involves the integration of this information to control emotional responses through either unconscious or conscious processes. ER may decrease (i.e., down-regulate), increase (i.e., up-regulate), or simply maintain positive or negative emotions. These processes can be response-focused or occur prior to the emotional response (antecedent-focused).13
METHOD TO STUDY ER
Behavioral/Clinical Method
Few studies have examined ER assessment methods for individuals with ASD. A general recommendation for the measurement of ER is multi-method assessment.19-20 Widely used observational methods for children include requiring a child to wait to open a surprise,21 and free play in an unstructured setting.22. Another approach is the disappointment paradigm,23 during which the child receives an undesirable prize. In these methods, emotions are quantified based on ratings of facial and vocal indices.24 Other coded behaviors may include asking for information for reassurance and disruptive behaviors. The application of such approaches in children with ASD may be difficult to interpret if not evaluated in the context of the child’s baseline behaviors and emotional expressions. Abnormal use of nonverbal communication, which is a diagnostic criterion for ASD, may explain unusual or limited facial expressions. In addition, the observable behaviors reflecting self-regulation may differ. For example, adults with ASD have commented that self-stimulatory behaviors (e.g., rocking) or intense focus on routines/rituals/circumscribed interests can be used for self-soothing.25 By contrast, these same behaviors may reflect distress.26 Thus, an extended baseline period of observation and historical information may be needed to accurately classify behavior as manifestations of distress versus deliberate self-soothing. Finally, despite the value of observational methods in developmental research, these methods may miss internal components of ER.19
Interviews and questionnaires have been widely used in non-ASD populations to assess relevant internal processes. Advantages of interviews include the opportunity for the respondent to describe internal states and ER strategies in an open-ended manner. In addition, the examiner can ask for clarification or elaboration. Self-report questionnaires designed to study the internal processes of ER or putative cognitive biases related to emotional responses have also been used in non-ASD populations. However, there is limited research to support the psychometric properties or clinical utility of such self-report questionnaires in ASD. For example, a study of adolescents with ASD found no association between the Dysfunctional Attitudes Scale for Children and self-reported depressive symptoms.30 This finding stands in sharp contrast to consistent evidence of an association in non-ASD populations.27 Whether this difference is due to differences in the mechanism underlying depression in ASD or reflects poor validity of this questionnaire in ASD is not clear. Another limitation of self-report questionnaires in ASD is difficulty applying them to nonverbal individuals, individuals with intellectual disability, and young children. Taken together, these considerations imply that measures of ER validated in the general population warrant careful re-assessment in youth with ASD.
Biologically-Based Method
The autonomic nervous system (ANS) is relevant to understanding physiological processes of ER and offers the possibility of an objective assessment of ER.28 Heart rate variability (HRV; variation in interbeat intervals) is an index of autonomic flexibility.28,29 There are multiple measures of parasympathetically mediated HRV, such as respiratory sinus arrhymthmia (RSA).30 Studies examining RSA suggest that higher baseline levels of RSA are associated with flexible emotional responses.31-32 However, interpretation of changes in RSA from baseline differs depending on the context, which may be a particular consideration in ASD. Specifically, RSA suppression (i.e., decrease in RSA from baseline) may reflect effective coping in response to stressful situations.33 On the other hand, in contexts that are nonthreatening, effective ER is thought to be associated with an increase in RSA above baseline.34
Accumulated results from functional magnetic resonance imaging (fMRI) studies provide insight into the neural circuitry of ER in clinical and nonclinical populations.35 In ASD, the challenge of finding ecologically valid means of eliciting emotion in a neuroimaging scanner is difficult given the idiosyncratic nature of emotional triggers in this population.36 Once an emotion is elicited, it may be difficult to differentiate the emotional response from efforts to regulate emotion.17 To date, fMRI studies in ASD have predominantly used higher-functioning individuals, perhaps due to the difficulties involved in engaging subjects with intellectual disability and those with receptive language deficits in fMRI tasks.
ER RESEARCH IN ASD
Research in ASD has focused more on emotional experience rather than ER. In general, this research suggest that youth with ASD, compared to non-ASD controls, have poorly differentiated emotional responses, exhibit more negative and less positive affect, and experience the physiological consequences of emotion with limited cognitive insight.37 Children with high-functioning ASD tend to rely on overt cues to describe their emotion (e.g., I was sad because I was crying) and provide nonspecific accounts of their emotional experiences.38 Although limited by small sample sizes and the assessment of predominantly high-functioning samples, available research suggests that individuals with ASD generally lack the emotional insight needed for effective ER.
Survey data in a few small studies support the presence of poor ER in ASD.37,39 Moreover, although the link has yet to be empirically established, ER deficits in children with ASD likely partially contribute to increased use of psychiatric services. A year-long study of the health care costs and utilization of 33,582 children (3,053 with ASD) found that children with ASD had almost 12 times more psychiatric hospital days than children without ASD, at almost 11 times the cost.40 Similarly, as many as 60% of children with ASD are prescribed psychotropic medications despite scant evidence that any medication is effective for the core features of ASD.41,42
An emerging body of evidence supports the presence of inadequate ER strategies in ASD. For example, adults with ASD report less use of cognitive reappraisal and greater use of suppression than adults without ASD.39 This pattern persisted even after controlling for differences in emotional experiences and alexithymia (difficulty identifying and describing emotions).37 In addition, 2 separate observational studies of young children with ASD found that they were less likely to use adaptive coping strategies compared to children without ASD.43,44 No ER studies have included adolescents with ASD.
CONCEPTUALIZING POOR ER IN ASD
One possible explanation for inadequate ER in ASD is the co-occurrence of a psychiatric disorder that accounts for the deficit. Alternatively, poor ER may be intrinsic to ASD. It could also be that specific psychiatric disorders and ER deficits in ASD share clinical or neurobiological features in common, making it difficult to disentangle the source of the behavioral disturbance.
Psychiatric Comorbidity
There is a reciprocal relationship between maladaptive ER and psychiatric disorders, such that poor ER increases risk for developing a psychiatric disorder, and having a psychiatric disorder interferes with adaptive regulation. Additionally, poor ER is a common mechanism across many disorders, and its behavioral manifestation is often what prompts referral for treatment.20 The presence of emotion dysregulation in ASD is often interpreted as evidence of an additional psychiatric disorder.36,45 Among community samples, 71–80% of children with ASD have at least 1 concurrent psychiatric diagnosis, and 41% have 2 or more.46 Even higher rates are observed in clinically-referred samples. For example, children with ASD seen in a psychopharmacology clinic were diagnosed with an average of 6.4 concurrent psychiatric disorders using a standard psychiatric interview.47
However, co-occurring psychiatric disorders may be overdiagnosed in this population when using standard diagnostic measures. A study of 35 high-functioning adolescents with ASD found that the majority (~60%) of prior psychiatric diagnoses were not supported by a psychiatric interview that was modified to take ASD-related impairment into account.48 The results of this pilot study highlight the need for validated diagnostic measures in ASD to separate the behavioral correlates of ASD and symptoms of other psychiatric disorders.49
This issue of diagnostic boundaries shares some of the challenges of severe mood dysregulation and irritability in non-ASD samples.50 The new diagnostic category, Disruptive Mood Dysregulation Disorder, aims to differentiate individuals with impaired mood regulation from individuals with bipolar disorder. It is not yet clear how this diagnosis will apply to individuals with ASD and emotion dysregulation. In a study of 91 adolescents with ASD, over 25% of the ASD group had severe mood dysregulation, but the neurocognitive correlates associated with severe mood problems differed from non-ASD samples.45 Therefore, it may be that manifestations of emotion dysregulation in ASD are somewhat distinct from non-ASD youth.
Shared Risk Factors With Other Disorders
Impaired ER has been associated with several disorders, including anxiety and mood disorders and borderline personality disorder.51 Some of the mechanisms thought to underlie inadequate ER in these populations may have relevance to ASD as well. Below we consider the tripartite model of anxiety and depression and some key findings regarding the neural circuitry implicated in ER.
The Triparite Model
The tripartite model of anxiety and depression holds that general distress is a shared factor, but physiological hyperarousal is specific to anxiety and anhedonia is specific to depression.52 General distress, or high baseline levels of negative affect, may also play an important role in ASD. Indeed, greater irritability and lower positive affect have been observed in many infants who later develop ASD.53 Although mixed, some evidence suggests hyperarousal in ASD.54 In support of emotion dysregulation associated with physiological hyperarousal in ASD, multiple studies have shown increased basal HR and decreased basal HRV or RSA in individuals with ASD relative to healthy controls, suggesting decreased vagal regulation of the heart or sympathetic and limbic activation.55-58 If ASD is associated with physiological hyperarousal, the presence of anxiety in ASD is easier to understand and may inform treatment given a well-established connection between hyperarousal and anxiety in non-ASD samples.59 Although not always clearly articulated, the management of arousal is an element in most cognitive-behavioral therapy (CBT) approaches for anxiety.60 Encouraging results from studies of CBT in youth with ASD support the potential relevance of over-arousal in ASD.61 A focus on reducing arousal has also been successfully integrated into other ASD treatment programs, such as SCERTS.62
Affective Neuroscience
ER typically activates several areas of prefrontal cortex (PFC). The subgenual anterior cingulate cortex (ACC), for example, plays an important role in the modulation of affective experiences.63-64 The modulation of amygdala (involved in the experience of emotion) by ventromedial PFC (vmPFC, including ACC) is a prominent theme in affective neuroscience, with abnormalities in vmPFC/amygdala connectivity implicated in mood and anxiety disorders.35,64 ER roles have also been attributed to ventrolateral PFC, and more superior aspects of medial PFC.63 The distinct roles of each of these prefrontal areas to ER is an area of active investigation in nonclinical and mood/anxiety disorder samples.
Some aspects of the ER neuroscience literature fit well within current models of neural dysfunction in ASD. For example, abnormal PFC function is a recurring theme in neuroimaging studies of ASD, although often associated with abnormal perspective taking rather than ER.65-66 However, PFC deficits could possibly account for both impaired perspective-taking and ER deficits in ASD. A related area of interest is PFC/amygdala connectivity. The few studies that have explicitly examined this connectivity in ASD in the context of emotion have yielded inconsistent findings. Swartz et al.67 showed diminished connectivity, whereas Monk et al.68 found increased connectivity. Although the affective neuroscience literature generally implicates decreased connectivity between PFC and amygdala in populations with clinical anxiety, Monk et al.68 raise the intriguing possibility that PFC upregulates amygdala function in ASD, diminishing the capacity to adaptively regulate emotion. These data call for a more sophisticated model of PFC/amygdala connectivity that moves beyond a strictly inhibitory relationship—one that also considers findings of abnormal white matter development in ASD.69-70
The numerous reports of abnormal medial PFC activity in ASD are consistent with data on PFC contributions to ER and, by extension, findings of ER deficits in ASD. Although many of these reports implicate dorsal medial PFC deficits in ASD (Brodmann areas 9 and 1071), a growing number focus on the same vmPFC areas that are implicated in ER (namely orbitofrontal and subgenual anterior cingulate cortices;).67,72,73 Given the equivocality in findings on the PFC regions involved in ER within ASD, we contend that it will be important to examine ASD deficits and ER processes together. For example, the localization of ASD deficits to specific PFC areas implicated in ER may help us to understand individual differences in ER functions and behavior in ASD.
The preponderance of literature on amygdala and emotion dysregulation in non-ASD clinical samples implicates hyperactivation,63,64,68 whereas traditional models of amygdala dysfunction in ASD implicate hypoactivation.74 The putatively “social” and “emotional” functions of amygdala are likely to be highly related, but ASD is associated with anxiety and decreased amygdala activation (generally interpreted as relating to social anhedonia).75 However, there are a growing number of imaging studies that find hyperactivation of amygdala in ASD during emotional face perception.80-81 In one of the only ASD studies directly relating anxiety symptoms to brain function, Kleinhans et al.77 found a positive correlation between amygdala activation and social anxiety symptoms. Increased amygdala activation has recently been associated with patterns of eye gaze avoidance in ASD, leading to an intriguing confluence between amygdala function, anxiety, and social avoidance in ASD.78,79
Although further investigation into the parameters surrounding amygdala activation in ASD is needed, three points warrant mention. First, individual differences are integral to understanding brain function in ASD. Specifically, the level of anxiety in the ASD samples may influence the amygdala findings, thereby influencing interpretations of the “social” functions of amygdala. Second, recent studies68,76,78-80 underscore the importance of attentional mechanisms in examination of emotion systems in ASD. When given the opportunity, individuals with ASD and elevated anxiety may be more prone to avoid the most potent affective information in a visual display, thereby affecting signal in biological measures. Third, measurement of mood, anxiety, and emotionality in ASD research in general, and neuroimaging studies in particular, is essential to build the evidence base.
The case for amygdala and PFC involvement in ER dysregulation in ASD is strong. Nevertheless, more complex models are likely needed to fully understand the (atypical) development of ER abilities in ASD. In particular, the regulation of amygdala function likely involves more than PFC. Although the case of PFC regulation of amygdala is compelling (including extensive evidence from both human and animal studies), it has been argued persuasively that emotion processes (including ER) need to be understood in the context of broader networks and more complex modulatory connections between structures.81 Network approaches to understanding ER are highly relevant to ASD, given the evidence for broad abnormalities in multiple gray and white matter structures.66,69 Furthermore, there are many additional brain areas that may play an important role in the understanding of ER in ASD. For example, recent studies implicate the insula in the experience and anticipation of negative outcomes—functions that fit well within the ER framework.82-84 Both functional and structural imaging studies of ASD have identified abnormalities in this area73,85-87 Similar overlap can be identified in striate cortex, which plays an important role in reward components of ER72 and has been shown to function abnormally in ASD.75 Given that ER and ASD deficits involve multiple, interconnected brain circuits, the search for key structures is likely to require a great deal of future research.
Characteristics of ASD that Influence ER
The functionalist perspective of ER posits that a person consciously seeks to regulate positive and negative emotions in order to attain set goals.18 Clinical observations in ASD support a tendency to react to emotional stimuli intensely without clear goal-directedness. The few ER studies done to date in ASD suggest the use of suppression,37 resignation, and avoidance,44 which lends some support to the notion that ER in ASD lacks the motivational component thought to be integral to ER in non-ASD populations. This apparent lack of motivation for ER may be compounded by poor emotional insight and self-monitoring.
Adaptive ER strategies are contextually dependent and applied selectively, based on the situation. By contrast, maladaptive strategies tend to be universally applied.51 Given the problems with cognitive flexibility and difficulties in modulating behavior in people with ASD, greater use of maladaptive strategies and less effective implementation of adaptive strategies is not surprising. In addition, deficits in perspective taking88 may limit the ability to evaluate the responses of others, lead to misunderstanding and frustration, and hinder accurate reappraisal of a situation.37
Differences in information processing and perception in ASD, ranging from slower processing to a heightened sensitivity to environmental influences (e.g., sensory sensitivity, resistance to change) may also affect ER in ASD. For example, the drive to modulate sensory input to a comfortable level may override and interfere with ER. A lower threshold for sensory information (hypersensitivity) may lead to intense and easily triggered reactions, whereas hyposensitivity (higher sensory thresholds) may be associated with disruptive and dysregulated behavior.89 A recent study found that cortical responses to sensory stimuli in ASD are markedly unreliable, with large within-subject differences in amplitude across trials.90 This may help to explain observations of aberrant and inconsistent responses to sensory information among people with ASD. It also raises the question of whether evoked emotional responses are similarly unreliable (e.g., whether neural responses to emotion are variable across time). If so, this would interfere with the ability to identify and respond to emotional experiences appropriately.
DISCUSSION
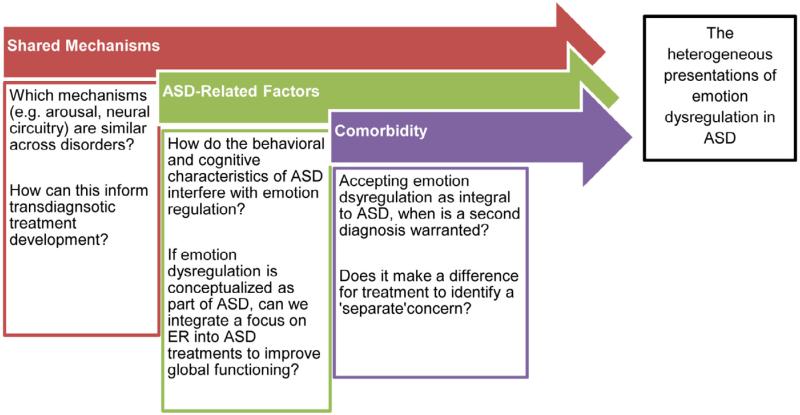
Despite the many challenges involved in studying ER in ASD, this area of inquiry has the potential to improve understanding of the neural circuitry of ASD itself as well as pave the way for new and more effective treatments. Therefore, ER warrants assessment in both clinical and research settings. However, many questions remain regarding the mechanisms that lead to impaired ER in ASD and the implications for treatment (see Figure 1). Our framework proposes that neural mechanisms shared with other psychiatric disorders, in combination with ASD-related behavioral and cognitive characteristics, interact to produce the heterogeneous presentations of emotion dysregulation in ASD (see Figure 2). The inclusion of ASD characteristics that are likely to influence ER disruption makes our model ASD-specific, yet we posit that ER is a dimensional construct that cuts across disorders (cf. Research Domain Criteria [RDoC]). It may be possible to develop transdiagnostic treatments for ER that are effective for many diagnostic populations, with modifications included to address the unique aspects of emotion dysregulation in ASD.
Figure 1.
Key research and clinical questions related to the processes that interact to produce impaired emotion regulation (ER) in autism spectrum disorder (ASD).
Figure 2.
Factors that may contribute to emotion dysregulation in autism spectrum disorder (ASD).
We propose that impaired ER may be intrinsic to ASD. However, this may increase risk for developing a psychiatric disorder and co-occurring psychiatric disorders contribute to the clinical picture in some cases. Nonetheless, the reported prevalence of concurrent psychiatric disorders in individuals with ASD may be overstated in order to explain the behavioral manifestations of emotion dysregulation.48 Impaired ER may be a more parsimonious explanation for the degree to which problems with anger and aggression (externalizing behaviors) as well as anxiety and depression (internalizing behaviors) are seen in ASD. A balance between understanding emotion dysregulation inherent to ASD (perhaps through the identification of subtypes) and the presence of a separate psychiatric disorder is needed. Situations marked by a new constellation of behaviors and symptoms that reflect a clear change in the individual’s functioning may call for a second diagnosis (e.g., an episodic mood disorder).49 Greater clarity will occur when we understand how the developmental, neural, cognitive, and behavioral features of these psychiatric disorders differ in ASD compared to the non-ASD population.
Research on ER in ASD is likely to require a multimethod approach,91 preferably combining physiological or neural measures with behavioral measures. An advantage of physiological and neuroimaging approaches is their ability to detect a response even if other factors (e.g., impaired language or insight, or alexithymia) limit the accuracy of self-report. Paradigms are needed to capture the often idiosyncratic emotional triggers in ASD. Self-reports have obvious pitfalls in ASD, but hold potential for obtaining information about specific manifestations of anxiety and internal processes. For this reason, there is a need to develop and validate self-report ER measures in ASD.
In order to understand ER in ASD, representative samples with a variety of emotional presentations (from blunted to labile) are needed. Longitudinal studies will help tease apart whether ER development in ASD is delayed versus deviant and will also identify age effects in ER. In addition, given the role of language in ER development,23 ASD samples spanning a range of language and intellectual abilities will be necessary. Integration of research into specialized inpatient psychiatry units that serve a high volume of children with ASD and other developmental disorders is one way to access large numbers of children with ASD and limited verbal ability.92 Treatment development studies related to ER should also include participants representing the full range of verbal and cognitive abilities.
As we await research on the feasibility and efficacy of psychosocial, pharmacological, and other (e.g., biofeedback) treatment approaches for impaired ER in ASD, clinicians must draw upon the extant research from other clinical populations and make adaptations when necessary for clients with ASD. To assess ER in a clinical context, careful observation of behavior may be most informative and applicable regardless of the individual’s verbal ability or cognitive function. For example, how does the individual react to disappointment (e.g., parent ‘forgot’ a favorite snack) or uncertainty (e.g., examiner asks individual to wait while she organizes papers), as well as positive emotions, such as receiving a reward? Such observational data, combined with parent- and self-report, may be feasible in most practice settings and provide information useful to case conceptualization. If it is determined that poor ER is an explanatory factor for the clinical presentation, psychoeducation for the patient and family on ER and adaptive and maladaptive strategies can be useful. In some cases, caregivers may not realize their reliance on a maladaptive strategy and that these strategies are modeled for the patient. Psychoeducation about ASD and ER can promote a validating environment and acceptance of the individual’s difficulties (similar to dialectical behavior therapy93) as well as recognition of the individual’s strengths. Other treatment strategies could include developing the client’s awareness of his/her own internal state in order to prepare for potentially difficult situations. Helping the individual to identify situations when an ER strategy should be used (flexibility in implementation) is essential in addition to specific ER skills (e.g., acceptance, reappraisal).
Approaching externalizing behaviors in ASD from the perspective of impaired ER also suggests alternate pharmacologic approaches, such as the use of alpha-2 agonists. Alpha-2 agonists decrease sympathetic tone, and thus can be conceptualized as targeted treatment for the emotional reactivity and hyperarousal that is characteristic of poor ER in ASD. Though there is insufficient evidence for alpha-2 agonists in ASD at this time,41 a large multi-site trial of a long acting alpha-2 agonist for children with ASD is underway, and may provide further evidence for this pathway.
Application of a validated dimensional measure reflecting an emotional and behavioral composite, termed “irritability,”94 in randomized clinical trials led to Food and Drug Administration (FDA) approval of two medications in children with DSM-IV-defined autistic disorder.95-96 These successful drug treatment programs point the way forward and suggest that validating other emotional profiles may also affirm important treatment targets. In addition, there is preliminary evidence that psychosocial interventions targeting ER skills can effectively reduce outbursts and negativity in young children with ASD,97 but much more work in this area is needed. Measures of ER that are reliable and valid across the full range of youth with ASD and sensitive to change have yet to be developed. Development of such a dimensional measure requires a better understanding of ER in the full ASD population, and moving beyond strict, categorical approaches.
Acknowledgments
This manuscript was supported by the National Institute of Child Health and Human Development grant K23HD060601 (C.A.M.), Slifka/Ritvo Award for Innovation in Autism Research (C.A.M.), AdvanceVT (S.W.W.), and the National Institute of Mental Health (NIMH) grant R01MH99021 (L.S.).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Dr. Herrington has received research funding from Shire Pharmaceuticals. Dr. Scahill has received research funding from NIMH, Roche, Pfizer, and Shire; has served as a consultant for Biomarin and Bracket; and has received royalties from Guilford Publications. Dr. Scarpa has received funding from Autism Speaks and has received royalties from Guilford Publications, Oxford Press, and from the sale of the Stress and Anger Management Program (STAMP) Treatment Manual through Jessica Kingsley Publishers. Dr. White has received royalties from Guilford Publications. Drs. Mazefsky and Seigel, and Ms. Maddox report no biomedical financial interests or potential conflicts of interest.
Contributor Information
Carla A. Mazefsky, University of Pittsburgh School of Medicine
John Herrington, Perelman School of Medicine at the University of Pennsylvania and Children’s Hospital of Philadelphia
Matthew Siegel, Spring Harbor Hospital and Tufts Medical Center
Angela Scarpa, Virginia Tech
Brenna B. Maddox, Virginia Tech
Lawrence Scahill, Emory University
Susan W. White, Virginia Tech
References
- 1.American Psychiatric Association . Text Revision. 4th Ed. Author; Washington, DC: 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 2.Autism and Developmental Disabiltiies Monitoring Network Prevalence of autism spectrum disorders. MMWR Surveill Summ. 2012;61(3):1–19. [PubMed] [Google Scholar]
- 3.Mazefsky CA, Minshew NJ. Clinical Pearl: The Spectrum of Autism-From Neuronal Connections to Behavioral Expression. Virtual Mentor. 2010;12(11):867–872. doi: 10.1001/virtualmentor.2010.12.11.cprl1-1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lecavalier L. Behavioral and emotional problems in young people with pervasive developmental disorders: Relative prevalence, effects of subject characteristics, and empirical classification. J Autism Dev Dis. 2006;36(8):1101–14. doi: 10.1007/s10803-006-0147-5. [DOI] [PubMed] [Google Scholar]
- 5.Thompson RA. Monographs of the Society for Research in Child Development. University of Chicago Press; Chicago, Illinois: 1994. Emotion regulation: A theme in search of definition; pp. 25–52. [PubMed] [Google Scholar]
- 6.Sofronoff K, Attwood T, Hinton S, Levin I. A randomized controlled trial of a cognitive behavioural intervention for anger management in children diagnosed with Asperger syndrome. J Autism Dev Dis. 2007;37(7):1203–14. doi: 10.1007/s10803-006-0262-3. [DOI] [PubMed] [Google Scholar]
- 7.Laurent AC, Otr L, Rubin E. Challenges in emotional regulation in asperger syndrome and high-functioning autism. Topics Lang Dis. 2004;4(24):286–297. [Google Scholar]
- 8.Baker J. No More Meltdowns. Future Horizons; Arlington, TX: 2008. [Google Scholar]
- 9.Derryberry D, Rothbart MK. Emotion, attention, and temperament. Cambridge University Press; Cambridge: pp. 132–166. [Google Scholar]
- 10.Campos JJ, Campos RG, Barrett KC. Emergent themes in the study of emotional development and emotion regulation. Dev Psychol. 1989;25(3):394–402. [Google Scholar]
- 11.Gross JJ. The Emerging Field of Emotion Regulation: An Integrative Review. Rev Gen Psychol. 1998;2(5):271–299. [Google Scholar]
- 12.Tamir M. The maturing field of emotion regulation. Emotion Rev. 2011;3(1):3–7. [Google Scholar]
- 13.Gross JTR. Handbook of Emotion Regulation. Guilford Press/Guilford Publications, Inc.; New York, NY: 2007. Emotion regulation: conceptual foundations; pp. 3–24. [Google Scholar]
- 14.Mauss IB, Robinson MD. Measures of emotion: a review. Cog Emotion. 2009;23(2):209–237. doi: 10.1080/02699930802204677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewis AR, Zinbarg RE, Durbin CE. Advances, problems, and challenges in the study of emotion regulation: a commentary. J Psychopath Beh Assess. 2010;32(1):83–91. [Google Scholar]
- 16.Cole PM, Martin SE, Dennis TA. Emotion regulation as a scientific construct: methodological challenges and directions for child development research. Child Dev. 2004;75(2):317–33. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- 17.Campos JJ, Frankel CB, Camras L. On the nature of emotion regulation. Child Dev. 2004;75(2):377–94. doi: 10.1111/j.1467-8624.2004.00681.x. [DOI] [PubMed] [Google Scholar]
- 18.Eisenberg N, Spinrad TL. Emotion-related regulation: sharpening the definition. Child Dev. 2004;75(2):334–9. doi: 10.1111/j.1467-8624.2004.00674.x. [DOI] [PubMed] [Google Scholar]
- 19.Adrian M, Zeman J, Veits G. Methodological implications of the affect revolution: a 35-year review of emotion regulation assessment in children. J Exp Child Psychol. 2011;110(2):171–97. doi: 10.1016/j.jecp.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 20.Berking M, Wupperman P. Emotion regulation and mental health: recent findings, current challenges, and future directions. Curr Opin Psychiatry. 2012;25(2):128–34. doi: 10.1097/YCO.0b013e3283503669. [DOI] [PubMed] [Google Scholar]
- 21.Cole PM, Teti LO, Zahn-Waxler C. Mutual emotion regulation and the stability of conduct problems between preschool and early school age. Dev Psychopath. 2003;15(1):1–18. [PubMed] [Google Scholar]
- 22.Denham SA, Blair KA, DeMulder E, et al. Preschool emotional competence: pathway to social competence? Child Dev. 2003;74(1):238–56. doi: 10.1111/1467-8624.00533. [DOI] [PubMed] [Google Scholar]
- 23.Saarni C. An observational study of children’s attempts to monitor their expressive behavior. Child Dev. 1984;55(4):1504. [Google Scholar]
- 24.Gruber J, Keltner D. Emotional Behavior and Psychopathology: A Survey of Methods and Concepts. In: Rottenberg JSJ, editor. Emotion and psychopathology: Bridging affective and clinical science. American Psychological Association; Washington, DC: 2007. pp. 35–52. [Google Scholar]
- 25.Lipsky D, Richards W. Managing Meltdowns: Using the S.C.A.R.E.D. Calming Technique with Children and Adults with Autism. Jessica Kingsley Publishers; Philadelphia, PA: 2009. [Google Scholar]
- 26.Magnuson KM, Constantino JN. Characterization of depression in children with autism spectrum disorders. J Dev Beh Ped. 2011;32:332–340. doi: 10.1097/DBP.0b013e318213f56c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenaway R, Howlin P. Dysfunctional attitudes and perfectionism and their relationship to anxious and depressive symptoms in boys with autism spectrum disorders. J Autism Dev Dis. 2010;40(10):1179–87. doi: 10.1007/s10803-010-0977-z. [DOI] [PubMed] [Google Scholar]
- 28.Appelhans BM, Luecken LJ. Heart rate variability as an index of regulated emotional responding. Rev Gen Psychol. 2006;10(3):229–240. [Google Scholar]
- 29.Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Dis. 2000;61(3):201–16. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- 30.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology Heart rate variability: Standards of measurement, physiologic interpretation, and clinical use. Circ. 1996;93:1043–1065. [PubMed] [Google Scholar]
- 31.Porges SW. Cardiorespiratory and cardiosomatic psychophysiology. Plenum; New York: 1986. Respiratory sinus arrhythmia: Physiological basis, quantitative methods, and clinical implications; pp. 101–116. [Google Scholar]
- 32.Suess PE, Porges SW, Plude DL. Cardiac vagal tone and sustained attention in school-age children. Psychophys. 1994;31:17–22. doi: 10.1111/j.1469-8986.1994.tb01020.x. [DOI] [PubMed] [Google Scholar]
- 33.Huffman LC, Bryan YE, Del Carmen R, Pedersen FA, Doussard-Roosevelt JA, Porges SW. Infant temperament and cardiac vagal tone: assessments at twelve weeks of age. Child Dev. 1998;69(3):624–35. [PubMed] [Google Scholar]
- 34.Hastings PD, Nuselovici JN, Utendale WT, Coutya J, McShane KE, Sullivan C. Applying the polyvagal theory to children’s emotion regulation: social context, socialization, and adjustment. Bio Psychol. 2008;79(3):299–306. doi: 10.1016/j.biopsycho.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 35.Monk CS. The development of emotion-related neural circuitry in health and psychopathology. Dev Psychopath. 2008;20(4):1231–50. doi: 10.1017/S095457940800059X. [DOI] [PubMed] [Google Scholar]
- 36.Mazefsky CA, Pelphrey KA, Dahl RE. The need for a broader approach to emotion regulation research in autism. Child Dev Perspect. 2012;6(1):92–97. doi: 10.1111/j.1750-8606.2011.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Samson AC, Huber O, Gross JJ. Emotion regulation in Asperger’s syndrome and high-functioning autism. Emotion. 2012;12(4):659–65. doi: 10.1037/a0027975. [DOI] [PubMed] [Google Scholar]
- 38.Losh M, Capps L. Understanding of emotional experience in autism: Insights from the personal accounts of high-functioning children with autism. Dev Psychol. 2006;42(5):809–818. doi: 10.1037/0012-1649.42.5.809. [DOI] [PubMed] [Google Scholar]
- 39.Jahromi LB, Bryce CI, Swanson J. The importance of self-regulation for the school and peer engagement of children with high-functioning autism. Res Autism Spectrum Dis. 2013;7(2):235–246. [Google Scholar]
- 40.Croen LA, Najjar DV, Ray GT, Lotspeich L, Bernal P. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics. 2006;118(4):1203–11. doi: 10.1542/peds.2006-0127. [DOI] [PubMed] [Google Scholar]
- 41.Siegel M. Psychopharmacology of autism spectrum disorder: evidence and practice. Child Adol Psychiatric Clin N Amer. 2012;21(4):957–73. doi: 10.1016/j.chc.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 42.McDougle CJ, Scahill L, Aman MG, et al. Risperidone for the core symptom domains of autism: results from the study by the autism network of the research units on pediatric psychopharmacology. Am J Psychiatry. 2005;162(6):1142–1148. doi: 10.1176/appi.ajp.162.6.1142. [DOI] [PubMed] [Google Scholar]
- 43.Konstantareas MM, Stewart K. Affect regulation and temperament in children with Autism Spectrum Disorder. J Autism Dev Dis. 2006;36(2):143–54. doi: 10.1007/s10803-005-0051-4. [DOI] [PubMed] [Google Scholar]
- 44.Jahromi LB, Meek SE, Ober-Reynolds S. Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. J Child Psychol Psychiatry. 2012;53(12):1250–8. doi: 10.1111/j.1469-7610.2012.02560.x. [DOI] [PubMed] [Google Scholar]
- 45.Simonoff E, Jones CRG, Pickles A, Happé F, Baird G, Charman T. Severe mood problems in adolescents with autism spectrum disorder. J Child Psychol Psychiatry. 2012;53(11):1157–66. doi: 10.1111/j.1469-7610.2012.02600.x. [DOI] [PubMed] [Google Scholar]
- 46.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Amer Acad Child Adol Psychiatry. 2008;47(8):921–9. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 47.Joshi G, Petty C, Wozniak J, et al. The heavy burden of psychiatric comorbidity in youth with autism spectrum disorders: a large comparative study of a psychiatrically referred population. J Autism Dev Dis. 2010;40(11):1361–70. doi: 10.1007/s10803-010-0996-9. [DOI] [PubMed] [Google Scholar]
- 48.Mazefsky CA, Oswald DP, Day TN, Eack SM, Minshew NJ, Lainhart JE. ASD, a psychiatric disorder, or both? Psychiatric diagnoses in adolescents with high-functioning ASD. J Clin Child Adol Psychol. 2012;41(4):516–23. doi: 10.1080/15374416.2012.686102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mazefsky CA, Filipink R, Link J, Lubetsky MJ. Medical evaluation and co-morbid psychiatric disorders. In: Lubetsky MJ, Handen BL, McGonigle JJ, editors. Autism Spectrum Disorder. Oxford University Press; 2011. [Google Scholar]
- 50.Leibenluft E. Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. AmJ psychiatry. 2011;168(2):129–42. doi: 10.1176/appi.ajp.2010.10050766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin Psychol Rev. 2010;30(2):217–37. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 52.Watson D, Clark LA, Weber K, et al. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abn Psychol. 1991;100(3):316–36. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 53.Rogers SJ. What are infant siblings teaching us about autism in infancy? Autism Res. 2009;2(3):125–37. doi: 10.1002/aur.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rogers SJ, Ozonoff S. Annotation: what do we know about sensory dysfunction in autism? A critical review of the empirical evidence. J Child Psychol Psychiatry. 2005;46(12):1255–68. doi: 10.1111/j.1469-7610.2005.01431.x. [DOI] [PubMed] [Google Scholar]
- 55.Vaughan Van Hecke A, Lebow J, Bal E, et al. Electroencephalogram and heart rate regulation to familiar and unfamiliar people in children with autism spectrum disorders. Child Dev. 2009;80(4):1118–33. doi: 10.1111/j.1467-8624.2009.01320.x. [DOI] [PubMed] [Google Scholar]
- 56.Ming X, Julu POO, Brimacombe M, Connor S, Daniels ML. Reduced cardiac parasympathetic activity in children with autism. Brain Dev. 2005;27(7):509–16. doi: 10.1016/j.braindev.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 57.Goodwin MS, Groden J, Velicer WF, et al. Cardiovascular arousal in individuals with autism. Focus Autism. 2006;21(2):100–123. [Google Scholar]
- 58.Bal E, Harden E, Lamb D, Van Hecke AV, Denver JW, Porges SW. Emotion recognition in children with autism spectrum disorders: relations to eye gaze and autonomic state. J Autism Dev Dis. 2010;40(3):358–70. doi: 10.1007/s10803-009-0884-3. [DOI] [PubMed] [Google Scholar]
- 59.White SW, Ollendick T, Albano AM, et al. Randomized controlled trial: multimodal anxiety and social skill intervention for adolescents with autism spectrum disorder. J Autism Dev Dis. 2013;43(2):382–94. doi: 10.1007/s10803-012-1577-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Beh Ther. 2004;35(2):205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 61.Scarpa A, White SW, Attwood T, editors. Cognitive-behavioral Interventions for Children and Adolescents with High-functioning Autism Spectrum Disorders. Guilford Publications; New York, NY: 2012. [Google Scholar]
- 62.Prizant BM, Wetherby AM, Rubin E, Laurent AC. The SCERTS Model. Infant Young Child. 2003;16(4):296–316. [Google Scholar]
- 63.Kross E, Davidson M, Weber J, Ochsner K. Coping with emotions past: the neural bases of regulating affect associated with negative autobiographical memories. Bio Psychiatry. 2009;65(5):361–6. doi: 10.1016/j.biopsych.2008.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kim MJ, Loucks RA, Palmer AL, et al. The structural and functional connectivity of the amygdala: from normal emotion to pathological anxiety. Beh Brain Res. 2011;223(2):403–10. doi: 10.1016/j.bbr.2011.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gallagher HL, Frith CD. Functional imaging of “theory of mind”. Trends Cogn Sci. 2003;7(2):77–83. doi: 10.1016/s1364-6613(02)00025-6. [DOI] [PubMed] [Google Scholar]
- 66.Herrington JD, Schultz R. Understanding Neuropsychiatric Disorders: Insights From Neuroimaging. Cambridge University Press; Cambridge: 2010. Neuroimaging of developmental disorders. [Google Scholar]
- 67.Swartz JR, Wiggins JL, Carrasco M, Lord C, Monk CS. Amygdala Habituation and Prefrontal Functional Connectivity in Youth With Autism Spectrum Disorders. J Am Acad Child Adolesc Psychiatry. 2013;52(1):84–93. doi: 10.1016/j.jaac.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Monk C. Neural circuitry of emotional face processing in autism spectrum disorders. JPsychiatry Neurosci. 2010;35(2):105–114. doi: 10.1503/jpn.090085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barnea-Goraly N, Kwon H, Menon V, Eliez S, Lotspeich L, Reiss AL. White matter structure in autism: preliminary evidence from diffusion tensor imaging. Biol Psychiatry. 2004;55(3):323–326. doi: 10.1016/j.biopsych.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 70.Ingalhalikar M, Parker D, Bloy L, Roberts TPL, Verma R. Diffusion based abnormality markers of pathology: toward learned diagnostic prediction of ASD. NeuroImage. 2011;57(3):918–27. doi: 10.1016/j.neuroimage.2011.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shalom D Ben. The medial prefrontal cortex and integration in autism. Neuroscientist. 2009;15(6):589–98. doi: 10.1177/1073858409336371. [DOI] [PubMed] [Google Scholar]
- 72.Pfeifer JH, Peake SJ. Self-development: integrating cognitive, socioemotional, and neuroimaging perspectives. Dev Cognitive Neurosci. 2012;2(1):55–69. doi: 10.1016/j.dcn.2011.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Watanabe T, Yahata N, Abe O, et al. Diminished medial prefrontal activity behind autistic social judgments of incongruent information. PloS one. 2012;7(6):e39561. doi: 10.1371/journal.pone.0039561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schultz RT. Developmental deficits in social perception in autism: the role of the amygdala and fusiform face area. IntJ Dev Neurosci. 2005;23(2-3):125–41. doi: 10.1016/j.ijdevneu.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 75.Chevallier C, Kohls G, Troiani V, Brodkin ES, Schultz RT. The social motivation theory of autism. Trends CognSci. 2012;16(4):231–9. doi: 10.1016/j.tics.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dalton KM, Nacewicz BM, Johnstone T, et al. Gaze fixation and the neural circuitry of face processing in autism. Nature Neurosci. 2005;8(4):519–26. doi: 10.1038/nn1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kleinhans NM, Richards T, Weaver K, et al. Association between amygdala response to emotional faces and social anxiety in autism spectrum disorders. Neuropsychologia. 2010;48(12):3665–70. doi: 10.1016/j.neuropsychologia.2010.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kliemann D, Dziobek I, Hatri A, Steimke R, Heekeren HR. Atypical reflexive gaze patterns on emotional faces in autism spectrum disorders. J Neurosci. 2010;30(37):12281–7. doi: 10.1523/JNEUROSCI.0688-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kliemann D, Dziobek I, Hatri A, Baudewig J, Heekeren HR. The role of the amygdala in atypical gaze on emotional faces in autism spectrum disorders. J Neurosci. 2012;32(28):9469–76. doi: 10.1523/JNEUROSCI.5294-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dalton KM, Nacewicz BM, Alexander AL, Davidson RJ. Gaze-fixation, brain activation, and amygdala volume in unaffected siblings of individuals with autism. Bio Psychiatry. 2007;61(4):512–20. doi: 10.1016/j.biopsych.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 81.Pfeifer JH, Allen NB. Arrested development? Reconsidering dual-systems models of brain function in adolescence and disorders. Trends Cogn Sci. 2012;16(6):322–9. doi: 10.1016/j.tics.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grinband J, Hirsch J, Ferrera VP. A neural representation of categorization uncertainty in the human brain. Neuron. 2006;49(5):757–63. doi: 10.1016/j.neuron.2006.01.032. [DOI] [PubMed] [Google Scholar]
- 83.Hasler G, Fromm S, Alvarez RP, Luckenbaugh DA, Drevets WC, Grillon C. Cerebral blood flow in immediate and sustained anxiety. J Neurosci. 2007;27(23):6313–9. doi: 10.1523/JNEUROSCI.5369-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sarinopoulos I, Grupe DW, Mackiewicz KL, et al. Uncertainty during anticipation modulates neural responses to aversion in human insula and amygdala. Cerebral Cortex. 2010;20(4):929–40. doi: 10.1093/cercor/bhp155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Doyle-Thomas KA, Kushki A, Duerden EG, et al. The effect of diagnosis, age, and symptom severity on cortical surface area in the cingulate cortex and insula in autism spectrum disorders. [published online July 25 2012] J Child Neurol. 2012 doi: 10.1177/0883073812451496. doi: 10.1177/0883073812451496. [DOI] [PubMed] [Google Scholar]
- 86.Shokouhi M, Williams JHG, Waiter GD, Condon B. Changes in the sulcal size associated with autism spectrum disorder revealed by sulcal morphometry. Autism Res. 2012;5(4):245–52. doi: 10.1002/aur.1232. [DOI] [PubMed] [Google Scholar]
- 87.Von dem Hagen EA, Stoyanova RS, Baron-Cohen S, Calder AJ. Reduced functional connectivity within and between “social” resting state networks in autism spectrum conditions [published online June 8, 2012] Soc Cog Affec Neurosci. doi: 10.1093/scan/nss053. doi: 10.1093/scan/nss053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Baron-Cohen S. Mindblindness: An essay on autism and theory of mind. 1997. [Google Scholar]
- 89.Dunn W, City K. The Impact of Sensory Processing Abilities on the Daily Lives of Young Children and Their Families: A Conceptual Model. Infant Young Child. 1997;9(4):24–35. [Google Scholar]
- 90.Dinstein I, Heeger DJ, Lorenzi L, Minshew NJ, Malach R, Behrmann M. Unreliable evoked responses in autism. Neuron. 2012;75(6):981–91. doi: 10.1016/j.neuron.2012.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Adrian M, Zeman J, Veits G. Methodological implications of the affect revolution: A 35-year review of emotion regulation assessment in children. J Exp Child Psychol. 2011;110(2):171–97. doi: 10.1016/j.jecp.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 92.Siegel M, Doyle K, Chemelski B, et al. Specialized inpatient psychiatry units for children with autism and developmental disorders: a United States survey. J Autism Dev Disord. 2012;42(9):1863–9. doi: 10.1007/s10803-011-1426-3. [DOI] [PubMed] [Google Scholar]
- 93.Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. Guilford Publications, Inc; 1993. p. 558. [Google Scholar]
- 94.Aman M, Singh N, Stewart A, et al. The aberrant behavior checklist: A behavior rating scale for the assessment of treatment effects. Am J Mental Def. 1985;89(5):485–91. [PubMed] [Google Scholar]
- 95.Network RU on PPA Risperdone in children with autism and serious behavioral problems. New Engl J Med. 2002;347(5):314–321. doi: 10.1056/NEJMoa013171. [DOI] [PubMed] [Google Scholar]
- 96.Owen R, Sikich L, Marcus RN, et al. Aripiprazole in the treatment of irritability in children and adolescents with autistic disorder. Pediatrics. 2009;124(6):1533–1540. doi: 10.1542/peds.2008-3782. [DOI] [PubMed] [Google Scholar]
- 97.Scarpa A, Reyes N. Improving emotion regulation with CBT in young children with high functioning autism spectrum disorders: A pilot study. Beh Cog Psychother. 2011;39(4):495–500. doi: 10.1017/S1352465811000063. [DOI] [PubMed] [Google Scholar]