Abstract
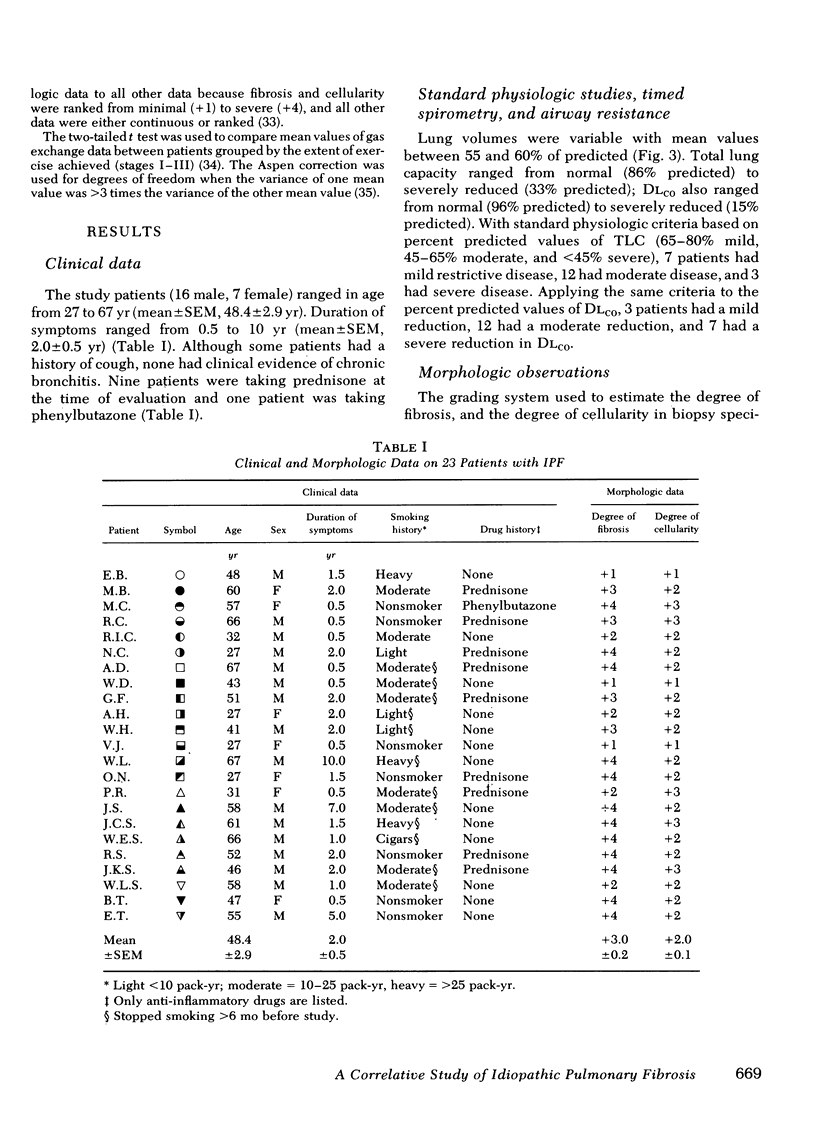
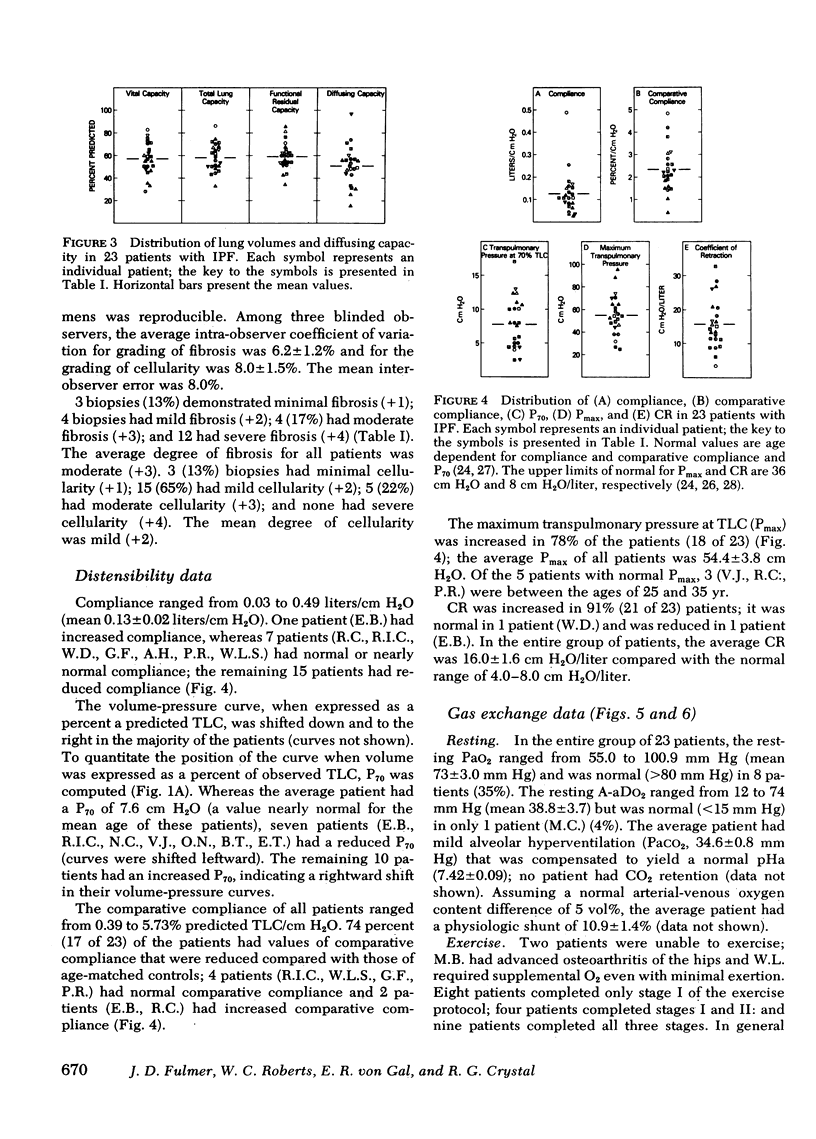
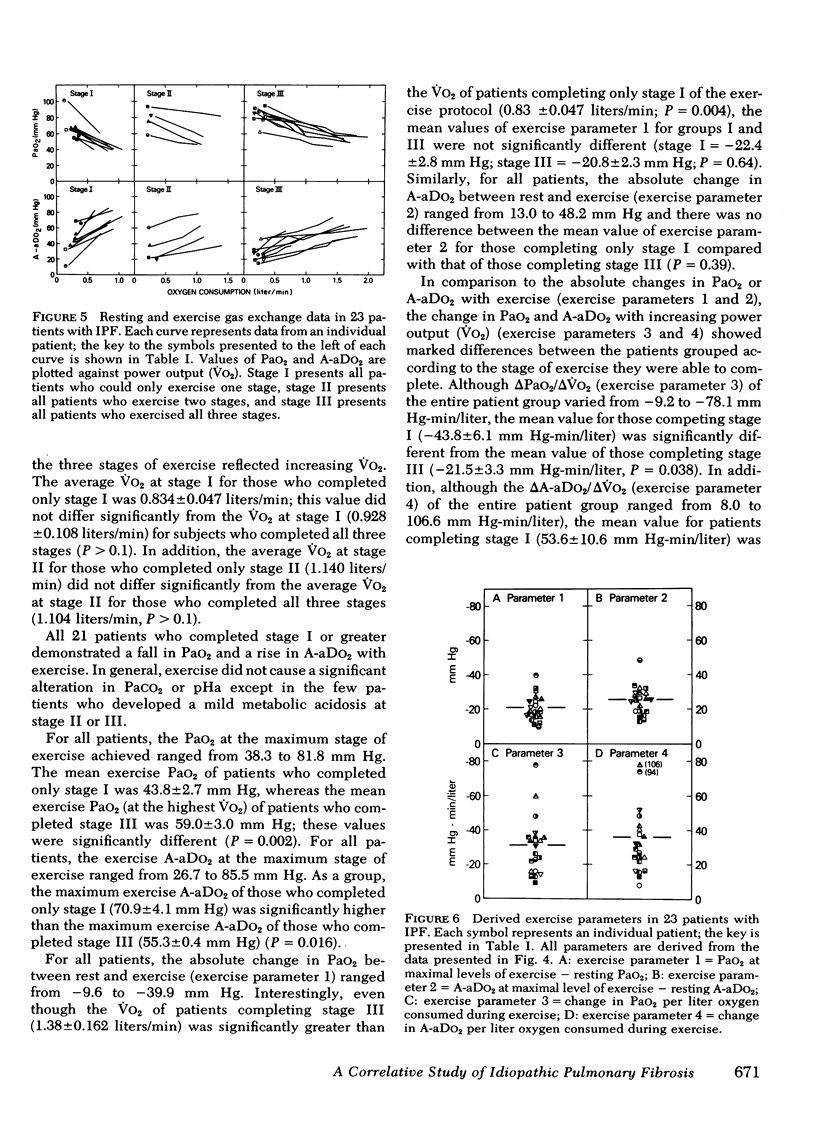
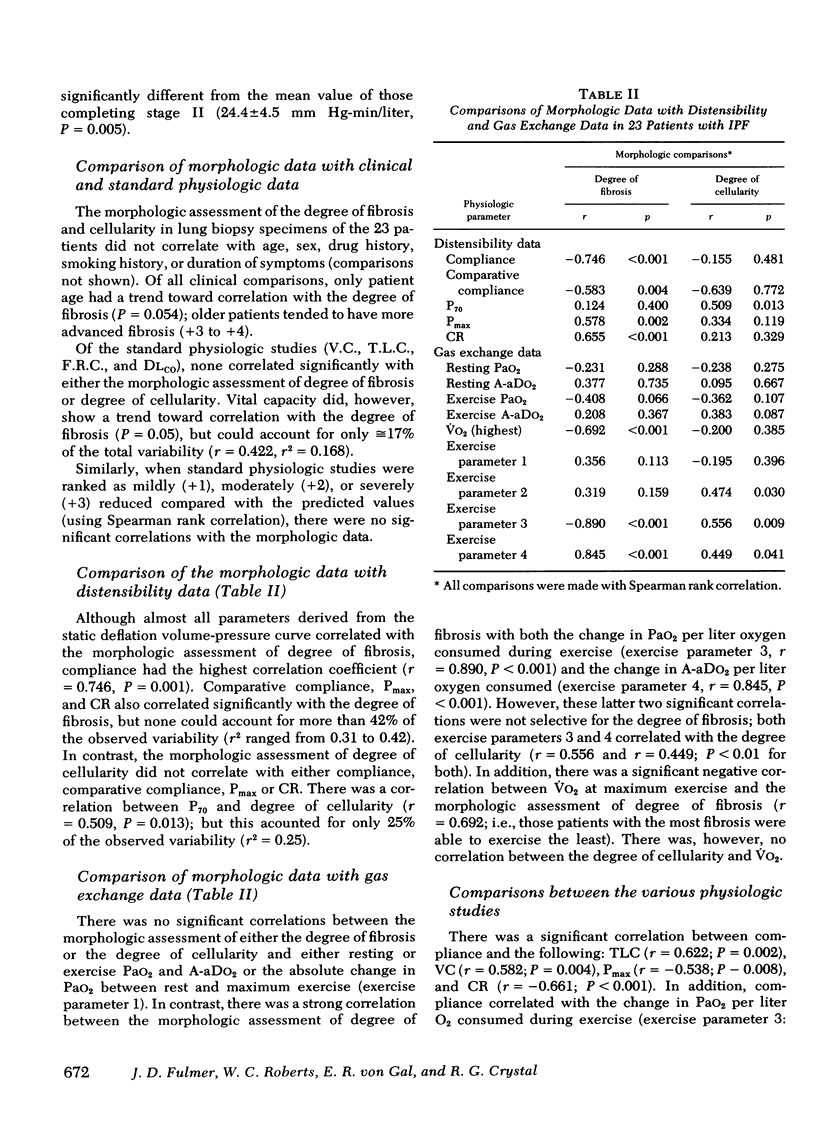
Idiopathic pulmonary fibrosis (IPF) is a progressive disease of lung parenchyma characterized by a chronic inflammatory cellular infiltration and varying degrees of interstitial fibrosis. Current data indicate that the severity of fibrosis and the degree of cellularity determine, in part, the prognosis of IPF and the response to therapy. Whereas lung biopsy gives the best assessement of fibrosis and cellularity, physiologic studies are used to stage and monitor the disease process. To determine which physiologic studies correlate best with severity of fibrosis and degree of cellularity, these parameters were graded in lung biopsies of 23 patients with IPF and compared with a variety of physiologic studies. Although vital capacity, total lung capacity, and diffusing capacity are commonly used as objective monitors of the disease process, none of these parameters correlated with either the severity of fibrosis or the degree of cellularity in biopsy specimens. In contrast, almost all parameters of lung distensibility correlated with the morphologic assessment of degree of fibrosis; compliance had the best correlation. Parameters of distensibility, however, correlated poorly with the degree of cellularity. In comparison, gas exchange during exercise correlated with both morphologic parameters; the exercise-induced changes in arterial oxygen pressure per liter of oxygen consumed had a high correlation with the degree of fibrosis (r = 0.89; P less than 0.001) and correlated to a lesser extent with the degree of cellularity (r = 0.56; P = 0.009). In contrast, neither the resting arterial oxygen tension nor the arterial oxygen tension at maximal exercise correlated with the morphologic assessment of degree of fibrosis or the degree of cellularity. These morphologic-physiologic comparisons suggest that (a) lung volumes and diffusing capacity are poor monitors of both the degree of fibrosis and the degree of cellularity; (b) the fibrotic process contributes, at least in part, to parameters of lung distensibility, and both fibrosis and cellularity contribute to gas exchange alterations during exercise; and (c) parameters of lung distensibility and exercise-induced gas exchange alterations may be useful in staging the severity of disease in IPF.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- AUSTRIAN R., McCLEMENT J. H., RENZETTI A. D., Jr, DONALD K. W., RILEY R. L., COURNAND A. Clinical and physiologic features of some types of pulmonary diseases with impairment of alveolar-capillary diffusion; the syndrome of "alveolar-capillary block". Am J Med. 1951 Dec;11(6):667–685. doi: 10.1016/0002-9343(51)90019-8. [DOI] [PubMed] [Google Scholar]
- Benson M. K., Hughes D. T. Serial pulmonary function tests in fibrosing alveolitis. Br J Dis Chest. 1972 Jan;66(1):33–44. [PubMed] [Google Scholar]
- Brown C. H., Turner-Warwick M. The treatment of cryptogenic fibrosing alveolitis with immunosuppressant drugs. Q J Med. 1971 Apr;40(158):289–302. doi: 10.1093/oxfordjournals.qjmed.a067271. [DOI] [PubMed] [Google Scholar]
- Carrington C. B., Gaensler E. A., Coutu R. E., FitzGerald M. X., Gupta R. G. Natural history and treated course of usual and desquamative interstitial pneumonia. N Engl J Med. 1978 Apr 13;298(15):801–809. doi: 10.1056/NEJM197804132981501. [DOI] [PubMed] [Google Scholar]
- Crystal R. G., Fulmer J. D., Roberts W. C., Moss M. L., Line B. R., Reynolds H. Y. Idiopathic pulmonary fibrosis. Clinical, histologic, radiographic, physiologic, scintigraphic, cytologic, and biochemical aspects. Ann Intern Med. 1976 Dec;85(6):769–788. doi: 10.7326/0003-4819-85-6-769. [DOI] [PubMed] [Google Scholar]
- DUBOIS A. B., BOTELHO S. Y., COMROE J. H., Jr A new method for measuring airway resistance in man using a body plethysmograph: values in normal subjects and in patients with respiratory disease. J Clin Invest. 1956 Mar;35(3):327–335. doi: 10.1172/JCI103282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies D., Crowther J. S., MacFarlane A. Idiopathic progressive pulmonary fibrosis. Thorax. 1975 Jun;30(3):316–325. doi: 10.1136/thx.30.3.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FINLEY T. N., SWENSON E. W., COMROE J. H., Jr The cause of arterial hypoxemia at rest in patients with "alveolarcapillary block syndrome". J Clin Invest. 1962 Mar;41:618–622. doi: 10.1172/JCI104517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulmer J. D., Roberts W. C., von Gal E. R., Grystal R. G. Small airways in idiopathic pulmonary fibrosis. Comparison of morphologic and physiologic observations. J Clin Invest. 1977 Sep;60(3):595–610. doi: 10.1172/JCI108811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOLDMAN H. I., BECKLAKE M. R. Respiratory function tests; normal values at median altitudes and the prediction of normal results. Am Rev Tuberc. 1959 Apr;79(4):457–467. doi: 10.1164/artpd.1959.79.4.457. [DOI] [PubMed] [Google Scholar]
- Gaensler E. A., Wright G. W. Evaluation of respiratory impairment. Arch Environ Health. 1966 Feb;12(2):146–189. doi: 10.1080/00039896.1966.10664355. [DOI] [PubMed] [Google Scholar]
- Gibson G. J., Pride N. B. Pulmonary mechanics in fibrosing alveolitis: the effects of lung shrinkage. Am Rev Respir Dis. 1977 Oct;116(4):637–647. doi: 10.1164/arrd.1977.116.4.637. [DOI] [PubMed] [Google Scholar]
- HAMER J. CAUSE OF LOW ARTERIAL OXYGEN SATURATION IN PULMONARY FIBROSIS. Thorax. 1964 Nov;19:507–514. doi: 10.1136/thx.19.6.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HERBERT F. A., NAHMIAS B. B., GAENSLER E. A., MACMAHON H. E. Pathophysiology of interstitial pulmonary fibrosis. Report of 19 cases and follow-up with corticosteroids. Arch Intern Med. 1962 Nov;110:628–648. doi: 10.1001/archinte.1962.03620230074012. [DOI] [PubMed] [Google Scholar]
- Horwitz A. L., Hance A. J., Crystal R. G. Granulocyte collagenase: selective digestion of type I relative to type III collagen. Proc Natl Acad Sci U S A. 1977 Mar;74(3):897–901. doi: 10.1073/pnas.74.3.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones N. L. Pulmonary gas exchange during exercise in patients with chronic airway obstruction. Clin Sci. 1966 Aug;31(1):39–50. [PubMed] [Google Scholar]
- Jones N. L. The place of exercise testing in the investigation of patients with respiratory disorders. Bull Eur Physiopathol Respir. 1977 May-Jun;13(3):425–439. [PubMed] [Google Scholar]
- LIVINGSTONE J. L., LEWIS J. G., REID L., JEFFERSON K. E. DIFFUSE INTERSTITIAL PULMONARY FIBROSIS.A CLINICAL, RADIOLOGICAL, AND PATHOLOGICAL STUDY BASED ON 45 PATIENTS. Q J Med. 1964 Jan;33:71–103. [PubMed] [Google Scholar]
- Lapp N. L., Seaton A., Kaplan K. C., Hunsaker M. R., Morgan W. K. Pulmonary hemodynamics in symptomatic coal miners. Am Rev Respir Dis. 1971 Sep;104(3):418–426. doi: 10.1164/arrd.1971.104.3.418. [DOI] [PubMed] [Google Scholar]
- Lemen R., Benson M., Jones J. G. Absolute pressure measurements with hand-dipped and manufactured esophageal balloons. J Appl Physiol. 1974 Oct;37(4):600–603. doi: 10.1152/jappl.1974.37.4.600. [DOI] [PubMed] [Google Scholar]
- MALMBERG R., BERGLUND E., ANDER L. IDIOPATHIC INTERSTITIAL FIBROSIS OF THE LUNGS. II. REVERSIBILITY OF RESPIRATORY DISTURBANCES DURING STEROID ADMINISTRATION. Acta Med Scand. 1965 Jul;178:59–66. [PubMed] [Google Scholar]
- MEAD J. Mechanical properties of lungs. Physiol Rev. 1961 Apr;41:281–330. doi: 10.1152/physrev.1961.41.2.281. [DOI] [PubMed] [Google Scholar]
- MILIC-EMILI J., MEAD J., TURNER J. M., GLAUSER E. M. IMPROVED TECHNIQUE FOR ESTIMATING PLEURAL PRESSURE FROM ESOPHAGEAL BALLOONS. J Appl Physiol. 1964 Mar;19:207–211. doi: 10.1152/jappl.1964.19.2.207. [DOI] [PubMed] [Google Scholar]
- McCarthy D., Cherniack R. M. Regional ventilation-perfusion and hypoxia in cryptogenic fibrosing alveolitis. Am Rev Respir Dis. 1973 Feb;107(2):200–208. doi: 10.1164/arrd.1973.107.2.200. [DOI] [PubMed] [Google Scholar]
- Morris J. F., Koski A., Johnson L. C. Spirometric standards for healthy nonsmoking adults. Am Rev Respir Dis. 1971 Jan;103(1):57–67. doi: 10.1164/arrd.1971.103.1.57. [DOI] [PubMed] [Google Scholar]
- NAIMARK A., WASSERMAN K., MCILROY M. B. CONTINUOUS MEASUREMENT OF VENTILATORY EXCHANGE RATIO DURING EXERCISE. J Appl Physiol. 1964 Jul;19:644–652. doi: 10.1152/jappl.1964.19.4.644. [DOI] [PubMed] [Google Scholar]
- RUBIN E. H., LUBLINER R. The Hamman-Rich syndrome: review of the literature and analysis of 15 cases. Medicine (Baltimore) 1957 Dec;36(4):397–463. doi: 10.1097/00005792-195712000-00001. [DOI] [PubMed] [Google Scholar]
- Scadding J. G. Diffuse pulmonary alveolar fibrosis. Thorax. 1974 May;29(3):271–281. doi: 10.1136/thx.29.3.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scadding J. G., Hinson K. F. Diffuse fibrosing alveolitis (diffuse interstitial fibrosis of the lungs). Correlation of histology at biopsy with prognosis. Thorax. 1967 Jul;22(4):291–304. doi: 10.1136/thx.22.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlueter D. P., Immekus J., Stead W. W. Relationship between maximal inspiratory pressure and total lung capacity (coefficient of retraction) in normal subjects and in patients with emphysema, asthma, and diffuse pulmonary infiltration. Am Rev Respir Dis. 1967 Oct;96(4):656–665. doi: 10.1164/arrd.1967.96.4.656. [DOI] [PubMed] [Google Scholar]
- Seaton A., Lapp N. L., Morgan W. K. Lung mechanics and frequency dependence of compliance in coal miners. J Clin Invest. 1972 May;51(5):1203–1211. doi: 10.1172/JCI106914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stack B. H., Choo-Kang Y. F., Heard B. E. The prognosis of cryptogenic fibrosing alveolitis. Thorax. 1972 Sep;27(5):535–542. doi: 10.1136/thx.27.5.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanek V., Widimský J., Kasalický J., Navrátil M., Daum S., Levinský L. The pulmonary gas exchange during exercise in patients with pulmonary fibrosis. Scand J Respir Dis. 1967;48(1):11–22. [PubMed] [Google Scholar]
- Turner J. M., Mead J., Wohl M. E. Elasticity of human lungs in relation to age. J Appl Physiol. 1968 Dec;25(6):664–671. doi: 10.1152/jappl.1968.25.6.664. [DOI] [PubMed] [Google Scholar]
- Wagner P. D., Dantzker D. R., Dueck R., de Polo J. L., Wasserman K., West J. B. Distribution of ventilation-perfusion ratios in patients with interstitial lung disease. Chest. 1976 Feb;69(2 Suppl):256–257. doi: 10.1378/chest.69.2_supplement.256-a. [DOI] [PubMed] [Google Scholar]
- Wasserman K., Whipp B. J. Excercise physiology in health and disease. Am Rev Respir Dis. 1975 Aug;112(2):219–249. doi: 10.1164/arrd.1975.112.2.219. [DOI] [PubMed] [Google Scholar]
- Whipp B. J., Wasserman K. Alveolar-arterial gas tension differences during graded exercise. J Appl Physiol. 1969 Sep;27(3):361–365. doi: 10.1152/jappl.1969.27.3.361. [DOI] [PubMed] [Google Scholar]
- Yernault J. C., Englert M. Static mechanical lung properties in young adults. Bull Physiopathol Respir (Nancy) 1974 Jul-Aug;10(4):435–450. [PubMed] [Google Scholar]
- Yernault J. C., de Jonghe M., de Coster A., Englert M. Pulmonary mechanics in diffuse fibrosing alveolitis. Bull Physiopathol Respir (Nancy) 1975 Mar-Apr;11(2):231–244. [PubMed] [Google Scholar]


