Abstract
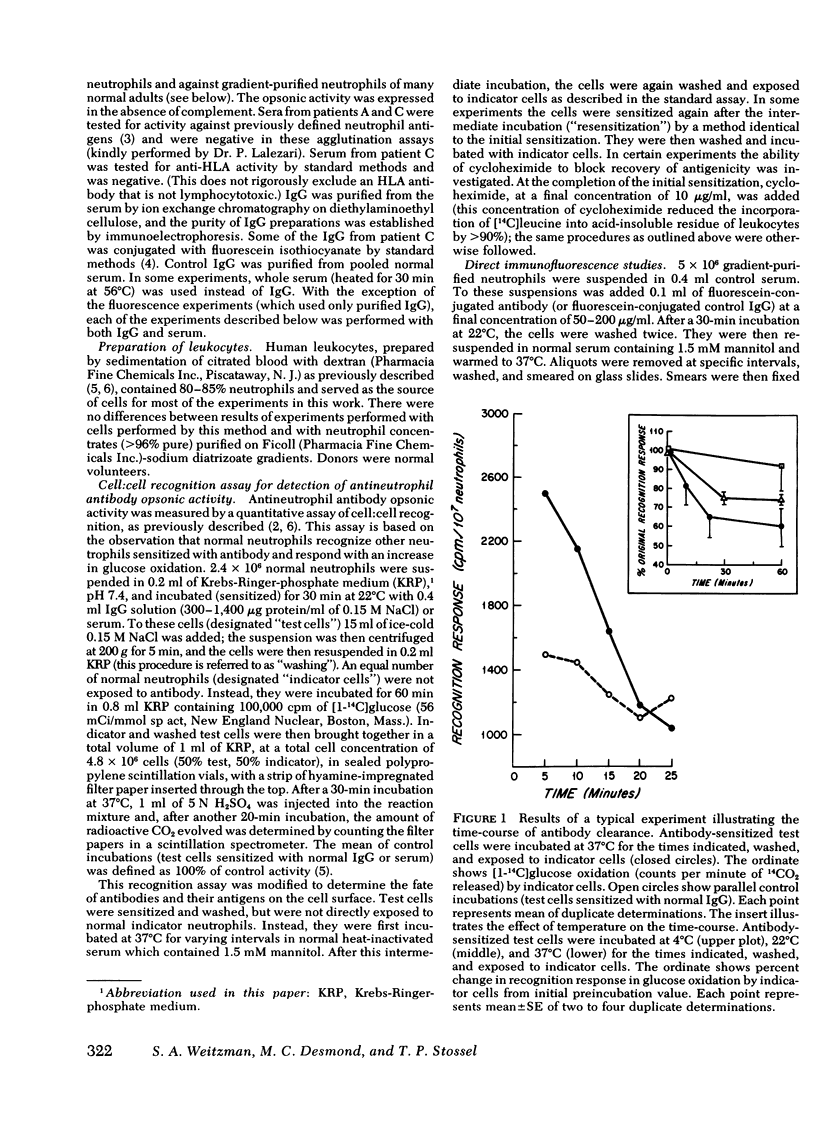
Turnover of membrane constituents appears important in many biologic processes. We studied this process in neutrophils by immunologic methods. The capacity of neutrophils to recognize other neutrophils coated with antibodies against membrane antigens was used to determine the changes that occur after attachment of the antibody to the neutrophil membrane. Neutrophils were sensitized for 30 min at 22°C with antibodies from three patients with antineutrophil autoantibodies. The sensitized neutrophils were recognized by normal neutrophils, which responded with an increase in glucose oxidation. If, after sensitization, the sensitized neutrophils were not immediately exposed to normal neutrophils, but instead were incubated at 37°C for varying times, the capacity to elicit a recognition response decayed and was gone by 30 min. Additionally, the capacity of the cells to be resensitized by reexposure to antibody also decayed during this period. However, after further incubation at 37°C, the neutrophils recovered the capacity to become sensitized; and this recovery was not inhibited by the addition of cycloheximide. Control incubations with normal immunoglobulin (Ig)G did not elicit a recognition response. The decay in recognition response was temperature dependent. Direct immunofluorescent studies with fluorescein-conjugated antineutrophil IgG revealed that the antibodies were cleared by aggregation and endocytosis. We conclude that: (a) neutrophils clear antibody from the cell surface by a temperature-dependent mechanism; (b) antigenicity is cleared concomitantly; (c) the mechanism of clearance involves internalization; and (d) with time, antigenicity reappears on the cell surface.
Full text
PDF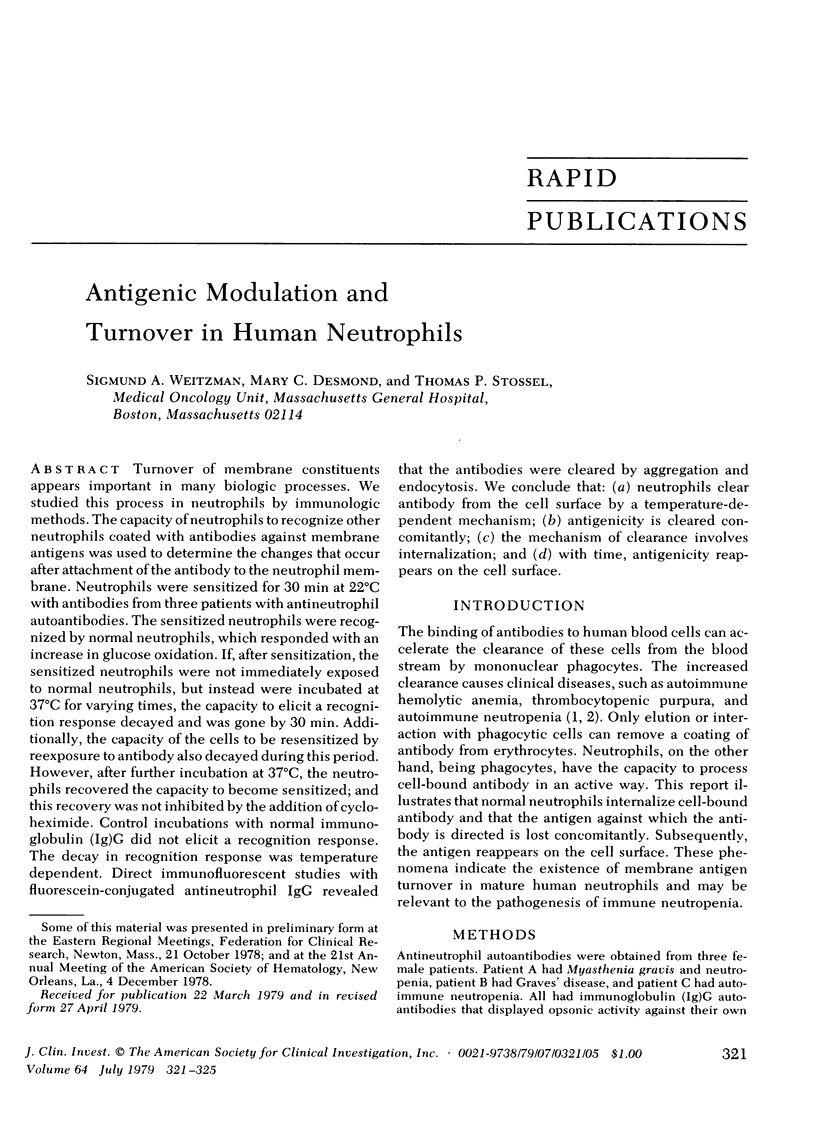
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Boxer L. A., Greenberg M. S., Boxer G. J., Stossel T. P. Autoimmune neutropenia. N Engl J Med. 1975 Oct 9;293(15):748–753. doi: 10.1056/NEJM197510092931505. [DOI] [PubMed] [Google Scholar]
- Kahn C. R. Membrane receptors for hormones and neurotransmitters. J Cell Biol. 1976 Aug;70(2 Pt 1):261–286. doi: 10.1083/jcb.70.2.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klock J. C., Stossel T. P. Detection, pathogenesis, and prevention of damage to human granulocytes caused by interaction with nylon wool fiber. Implications for filtration leukapheresis. J Clin Invest. 1977 Nov;60(5):1183–1190. doi: 10.1172/JCI108871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalezari P., Radel E. Neutrophil-specific antigens: immunology and clinical significance. Semin Hematol. 1974 Jul;11(3):281–290. [PubMed] [Google Scholar]
- Old L. J., Stockert E., Boyse E. A., Kim J. H. Antigenic modulation. Loss of TL antigen from cells exposed to TL antibody. Study of the phenomenon in vitro. J Exp Med. 1968 Mar 1;127(3):523–539. doi: 10.1084/jem.127.3.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stendahl O., Hed J., Kihlström E., Magnusson K. E., Tagesson C. Phagocytic internalization and the requirement for membrane perturbation. FEBS Lett. 1977 Sep 1;81(1):118–120. doi: 10.1016/0014-5793(77)80941-1. [DOI] [PubMed] [Google Scholar]
- Weitzman S. A., Stossel T. P. Drug-induced immunological neutropenia. Lancet. 1978 May 20;1(8073):1068–1072. doi: 10.1016/s0140-6736(78)90915-7. [DOI] [PubMed] [Google Scholar]