Abstract
Epithelial-mesenchymal transition (EMT) is an essential process that drives polarized, immotile mammary epithelial cells (MECs) to acquire apolar, highly migratory fibroblastoid-like features. EMT is an indispensable process that is associated with normal tissue development and organogenesis, as well as with tissue remodeling and wound healing. In stark contrast, inappropriate reactivation of EMT readily contributes to the development of a variety of human pathologies, particularly those associated with tissue fibrosis and cancer cell invasion and metastasis, including that by breast cancer cells. Although metastasis is unequivocally the most lethal aspect of breast cancer and the most prominent feature associated with disease recurrence, the molecular mechanisms whereby EMT mediates the initiation and resolution of breast cancer metastasis remains poorly understood. Transforming growth factor-β (TGF-β) is a multifunctional cytokine that is intimately involved in regulating numerous physiological processes, including cellular differentiation, homeostasis, and EMT. In addition, TGF-β also functions as a powerful tumor suppressor in MECs, whose neoplastic development ultimately converts TGF-β into an oncogenic cytokine in aggressive late-stage mammary tumors. Recent findings have implicated the process of EMT in mediating the functional conversion of TGF-β during breast cancer progression, suggesting that the chemotherapeutic targeting of EMT induced by TGF-β may offer new inroads in ameliorating metastatic disease in breast cancer patients. Here we review the molecular, cellular, and microenvironmental factors that contribute to the pathophysiological activities of TGF-β during its regulation of EMT in normal and malignant MECs.
Keywords: Epithelial-mesenchymal Transition, Metastasis, Signal Transduction, Transforming growth factor-β, Tumor Microenvironment
Introduction
Epithelial-mesenchymal transition (EMT) is a complex process whereby polarized epithelial cells transition into apolar fibroblastoid-like cells, a phenomenon that underlies tissue morphogenesis and organogenesis in the embryo, as well as tissue remodeling and repair in adults (1–3). Moreover, the inappropriate reactivation of developmental EMT programs plays a significant role in the pathology of fibrotic diseases and cancer, including those of the breast. Epithelial cell sheets manifest as tightly packed cell monolayers that compose the skin and line the internal cavities (e.g., airways and gastrointestinal tract), and in doing so, form a barrier that protects the host from environmental insults. In a similar fashion, mammary epithelial cells (MECs) exhibit a cobblestone appearance and are linked through the actions of numerous cell-cell complexes, including desmosomes, adherens, gap, and tight junctions (4). Collectively, these junctional structures provide MECs with their characteristic apical-basolateral polarity and cortical actin architecture. In stark contrast, mesenchymal cells lack cell-cell junctional complexes, leading to their apolar morphologies and enhanced migratory activities through the extracellular matrix (ECM). The plasticity of MECs enables them to dedifferentiate during EMT, and in doing so, transitioning MECs forego their cobblestone morphologies and instead acquire a spindle-shaped appearance characteristic of mesenchymal cells. In undertaking this phenotypic and morphologic transition, MECs first experience a disruption and delocalization of tight junction complexes (e.g., zonula occluden-1 (ZO-1), claudin, and occludin), which is succeeded by the loss of E-cadherin expression and activity that results in the stabilization and nuclear accumulation of β-catenin. This process is also characterized by the dramatic remodeling of the cytoskeleton and its formation of actin stress fibers as transitioning cells acquire migratory mesenchymal phenotypes (1–3). Thus, EMT reflects the initiation of a complex cascade of genetic and epigenetic events that culminate in MECs discarding their expression of epithelial gene signatures (e.g., E-cadherin, β4 integrin, and ZO-1) and acquiring those of mesenchymal cells [e.g., N-cadherin, vimentin, α-smooth muscle actin (α-SMA)]. Moreover, the process of EMT is highly metastable and is readily subject to phenotypic and morphologic reversion by mesenchymal-epithelial transition (MET), the molecular mechanisms of which are poorly understood and will not be discussed further herein (see (5, 6)). These general steps exhibited by transitioning MECs underlie both the biological and pathological episodes of EMT, which recently have been categorized into three distinct subtypes – i.e., a) embryonic and developmental EMT, which is referred to as type 1 EMT; b) tissue regeneration and fibrotic EMT, which is referred to as type 2 EMT; and c) cancer progression and metastatic EMT, which is known as type 3 EMT (2).
Here we review recent findings that directly impact our understanding of the role transforming growth factor-β (TGF-β) plays in regulating the initiation and resolution of individual subtypes of EMT. In addition, we also discuss the clinical implications afforded by chemotherapeutic targeting of TGF-β effectors coupled to type 3 EMT and their potential to suppress breast cancer progression and the oncogenic activities of TGF-β, particularly its induction of EMT and metastasis in developing mammary carcinomas.
TGF-β and EMT Subtypes
TGF-β Signaling and Epithelial Plasticity
TGF-β is a multifunctional cytokine and a powerful tumor suppressor that governs essentially every aspect of the physiology and homeostasis of MECs, including their ability to proliferate, migrate, differentiate, and survive (7–9). During mammary tumorigenesis, a variety of genetic and epigenetic events conspire to circumvent the cytostatic and tumor suppressing activities of TGF-β, thereby enhancing the development and progression of evolving mammary neoplasms (1, 7, 8). Even more remarkably, neoplastic MECs that have acquired resistance to the cytostatic activities of TGF-β often exhibit oncogenic behaviors when stimulated by TGF-β. This phenotypic switch in TGF-β function during tumorigenesis is known as the “TGF-β Paradox,” which represents the most important and unanswered question concerning the pathophysiological actions of this pleiotropic cytokine (10). Interestingly, the differentiation and migration of mammary stem cells results in the production of both the outer myoepithelial and inner luminal layers that ultimately give rise to mature mammary glands (11–13), suggesting that the process of EMT is in someway linked to the generation and maintenance of stem cell populations. Numerous studies have established TGF-β as a master regulator of EMT in normal and malignant MECs (1, 14, 15), while more recent findings have associated TGF-β stimulation of EMT with the acquisition of “stemness” in transitioning MECs (16, 17), and with the selection and expansion of breast cancer stem cells (18, 19). Along these lines, we and others have established EMT as being a vital component underlying the initiation of oncogenic TGF-β signaling in normal and malignant MECs (1, 14, 20). Thus, identifying the molecular mechanisms whereby EMT is induced by TGF-β is paramount to maintaining mammary gland homeostasis, and to suppressing the development and progression of mammary tumors.
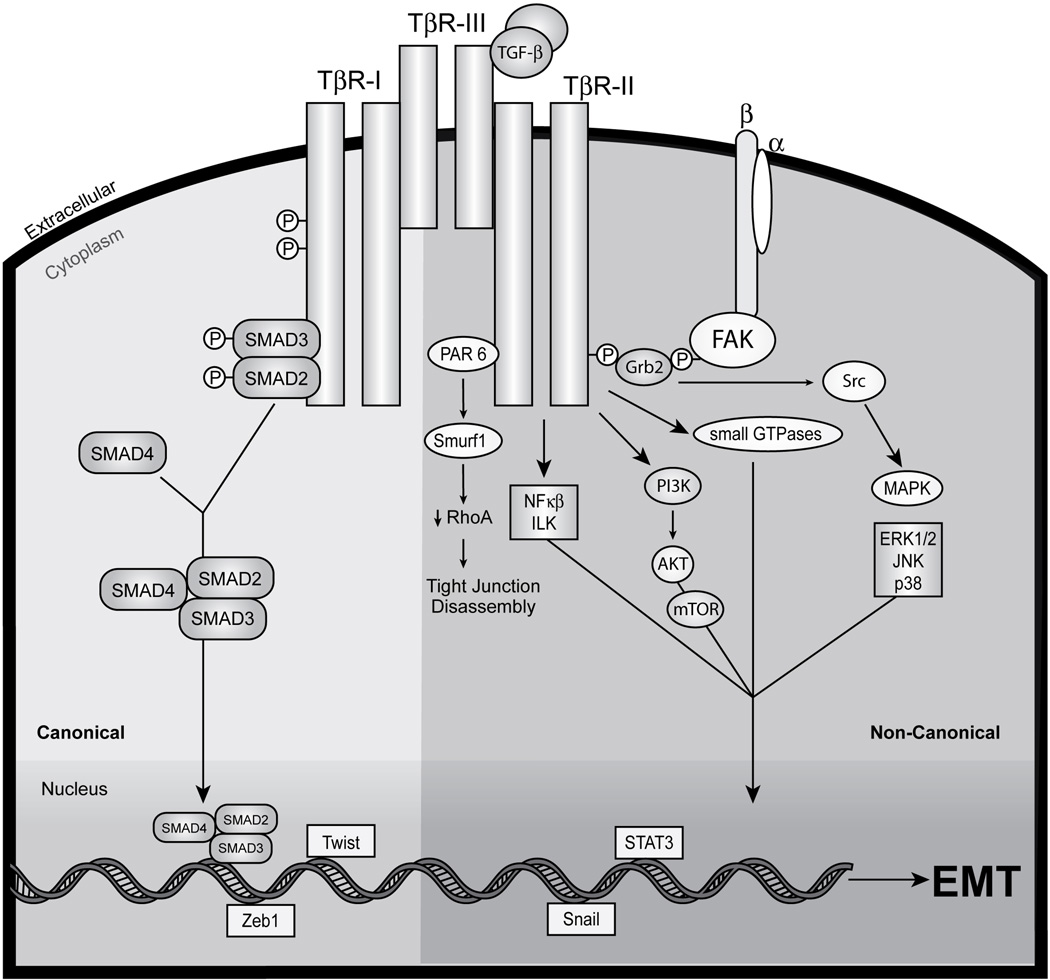
The mechanisms through which TGF-β initiates its pathophysiological activities and initiation of EMT are shown schematically in Figure 1. Indeed, transmembrane signaling stimulated by TGF-β commences by its binding to the high-affinity transmembrane Ser/Thr receptor protein kinases, TGF-β type I (TβR-I) and type II (TβR-II). Mammals express three distinct TGF-β isoforms termed TGF-β1, TGF-β2, and TGF-β3, which function analogously in vitro, but give rise to more than 30 distinct phenotypes upon their genetic deletion in mice (21). In addition, whereas TGF-βs 1 and 3 can bind directly to TβR-II, TGF-β2 requires assistance from the accessory TGF-β receptor, TGF-β type III (TβR-III). In all of these scenarios, the ligation of TGF-β to TβR-II facilitates its transphosphorylation and activation of TβR-I, which subsequently phosphorylates and activates the latent transcription factors, Smads 2 and 3. Once phosphorylated, receptor-activated Smads 2 and 3 associate with the common Smad, Smad4, at which point these heteromeric complexes translocate en masse into the nucleus to regulate the expression of TGF-β-responsive genes. In addition, the amplitude and duration of Smad2/3-based signaling transpires through their physical interaction with a plethora of transcription factors, and with a variety of transcriptional activators and co-repressors in a gene- and cell-specific manner (see (22, 23)). The capacity of Smad2/3 to impact MEC behavior is also governed by their association with a number of adapter molecules, including SARA (24), Hgs (25), and Dab2 (26–28). Likewise, upregulated expression of the inhibitory Smad, Smad7, also limits the extent of Smad2/3 signaling by competitively inhibiting their phosphorylation by TβR-I (29–31), and by promoting the internalization and degradation of TβR-I (32, 33). Moreover, the anti-TGF-β activity of Smad7 is augmented by its interaction with the adaptor protein STRAP (34), and conversely, is attenuated by its association with either AMSH2 (35) or Arkadia (36–38). Collectively, TGF-β signals propagated through Smad2/3 are referred to as “canonical” TGF-β signaling, and their specific role in regulating EMT induced by TGF-β is discussed below.
Figure 1.
Schematic depicting the canonical and noncanonical TGF-β signaling systems coupled to EMT in MECs. Transmembrane signaling by TGF-β ensues through its binding and activation of the Ser/Thr protein kinase receptors, TβR-I and TβR-II. Indeed, TGF-β binding to either TβR-III or TβR-II enables the recruitment and transphosphorylation of TβR-I, resulting its activation and subsequent phosphorylation the receptor-activated Smads, Smad2 and Smad3. Once activated, Smad2/3 form heterocomplexes with common the Smad, Smad4, which collectively translocate en masse to the nucleus to regulate the expression of TGF-β-responsive genes in concert with an ever expanding list of transcriptional coactivators and repressors. This branch of the bifurcated TGF-β signaling system represents the “canonical” or “Smad2/3-dependent” TGF-β pathway (left). Alternatively, TGF-β also activates a variety of “noncanonical” or “Smad2/3-independent” effectors, including Par6, NF-κB, ILK, FAK, Src, a variety of small GTPases, members of the MAP kinase family (e.g., ERK1/2, JNK, and p38 MAPK), and the PI3K:AKT:mTOR signaling axis (right). Activation of members of the Snail, ZEB, or bHLH family of transcription factors promote EMT by transcriptionally repressing the production of E-cadherin transcripts (bottom). Imbalances between canonical and noncanonical TGF-β signaling pathways have recently been identified and established as casual aberrancies underlying the initiation of oncogenic TGF-β signaling and its initiation of EMT in normal and malignant MECs. See text for details.
Besides its ability to activate canonical Smad2/3-dependent pathways, TGF-β also regulates MEC behavior and the induction of EMT via the stimulation of numerous “noncanonical” effector systems, including (i) small GTP-binding proteins (e.g., Ras, Rho, and Rac1); (ii) phosphoinositide-3-kinase (PI3K), AKT, and mTOR; (iii) MAP kinases (e.g., p38 MAPK, ERK1/2, and JNK); and (iv) NF-κB and Cox-2 (39–51). In addition, although inactivating mutations and decreased expression of TβR-I and TβR-II have been identified and characterized in human cancers, the occurrence of these mutagenic events is in fact quite rare. However, the loss of TβR-III expression does correlate with increased breast cancer tumorigenicity and decreased patient survival (52, 53), suggesting an important tumor suppressing function for this accessory receptor. Indeed, the functional loss of TβR-III coincides with EMT and enhances cell migration and invasion (54, 55). The coupling of TGF-β to these receptors and their noncanonical effectors is depicted schematically in Figure 1, as is our understanding of how integrins and proteins associated with focal adhesion complexes cooperate with TGF-β in regulating the behaviors and EMT status of normal and malignant MECs (45, 46, 56–60). The specific role of these noncanonical TGF-β effectors in regulating EMT in normal and malignant MECs is presented in the succeeding sections, while future studies clearly need to address the relative contribution of TβR-I, TβR-II, and TβR-III in mediating activation of canonical and noncanonical TGF-β signaling systems.
EMT Subtypes Coupled to TGF-β
The process of EMT occurs in a variety of distinct biological and pathological settings, including during normal embryogenesis and tissue morphogenesis, during tissue remodeling and repair, and during fibrosis and cancer progression. Although the underlying molecular mechanisms that define the pathophysiological activities of EMT in distinct cellular contexts are likely to be overlapping and redundant, the diversity of biological outcomes engendered by EMT is nonetheless highly specialized and has resulted in the classification of three distinct subtypes of EMT (2). For instance, type 1 EMT is activated during embryogenesis and tissue morphogenesis, leading to the generation of mesenchymal cells that ultimately give rise to secondary epithelial structures. In contrast, type 2 EMT is normally activated during tissue regeneration and repair, and abnormally during tissue fibrosis resulting from dysregulated inflammatory reactions. Finally, type 3 EMT is activated by cancer cells, including those of the breast (1), to facilitate their acquisition of invasive and metastatic phenotypes, and ultimately to establish secondary sites of lethal tumor outgrowth. In the succeeding sections, we highlight the molecular mechanisms and biological settings whereby TGF-β participates in regulating individual EMT subtypes, particularly type 3 EMT during mammary tumorigenesis.
Type 1 EMT
Developmental or type 1 EMT is associated with embryogenesis and its accompanying organogenesis and tissue morphogenesis, both of which require epithelial-derived mesenchymal cells to undergo MET during the formation of new epithelial structures (Fig. 2). In stark contrast to types 2 and 3 EMT, this developmental mode of EMT results in the production of multipotent mesenchymal cells and is not associated with tissue fibrosis and inflammation, or with the aberrant migration of cancer cells. Interestingly, members of the TGF-β superfamily play important regulatory roles during type 1 EMT, particularly during the processes of gastrulation, palate fusion, and neural crest and endocardial cushion formation (61). Indeed, type 1 EMT is first initiated during embryogenesis to promote gastrulation, which results in the formation of the ectoderm, mesoderm, and endoderm from the invaginating primitive streak (2, 4). This process requires Wnt signaling inputs to render primitive streak cells competent to undergo EMT in response to the TGF-β superfamily members, Nodal and Vg1 (62–65), both of which are essential for primitive streak and mesoderm formation in gastrulating embryos (66–70).
Figure 2.
Type 1 EMT in development and embryogenesis. Following fertilization, the zygote undergoes several rounds of cleavage to form a dense spheroid structure, which then undergoes blastulation to from a hollowed blastula. During gastrulation, TGF-β provides inductive EMT signals that elicits the formation of an invaginating structure that generates the three multipotent germ layers, namely the mesoderm, endoderm, and ectoderm. The mesoderm gives rise to muscle, skeleton, and connective tissue, while the endoderm gives rise to internal organs, such as the liver, colon, and stomach. The outer ectodermal layer generates the epidermis and ocular lens, as well as produces the mammary gland. The ectoderm also gives rise to the primordial nervous system via neurulation and neural crest formation, a process that dependent upon EMT induced by TGF-β. Finally, TGF-β stimulation of EMT during organogenesis is essential for the faithful development of the kidney, and of the endocardial cushion and subsequent atrioventricular valve formation. The role of TGF-β in regulating type 1 EMT during mammary gland branching and invasion is discussed in the text.
Type 1 EMT is also initiated during neurulation and occurs in the neural plate to facilitate the formation of the neural tube, which ultimately gives rise to the spine and brain. As the neural tube fuses, EMT also occurs in neural crest cells and facilitates their migration and dissemination throughout the embryo where they ultimately contribute to the generation of numerous specialized tissues, including the adrenal medulla and the peripheral nervous and skeletal systems (4, 71). Bone morphogenic proteins (BMPs) belong to the TGF-β superfamily and are essential to the induction of EMT during neurulation (72, 73). Similarly, TGF-β signaling also oversees the latter stages of heart and secondary palate formation (4, 74). For instance, myocardial cells actively secrete an ECM that separates the endocardium from the myocardium, which also induces endocardial cells to undergo EMT and migrate into the endocardial cushion to facilitate atrioventricular valve formation (4). Experiments performed in chicks and mice have identified important roles during development for all three TGF-β isoforms, of which TGF-β2 appears to play a dominant role in stimulating EMT in endocardial cells (75–77). Similarly, TGF-β3 is essential in mediating secondary palate formation, which requires midline epithelial seam cells to undergo EMT to complete oral palate fusion and closure (78, 79). Importantly, TβR-III expression is essential for EMT induced during the formation of both the heart and secondary palate (80, 81).
At present, a role for type 1 EMT in mediating mammary gland development has yet to be described; however, branching morphogenesis of normal MEC organoids in 3D–organotypic cultures showed that these structures exhibit a loss in polarity and acquire mesenchymal characteristics at invading branch tips, findings that point to a role of type 1 EMT in mammary gland development (82, 83). In addition, inappropriate reactivation of embryonic and type 1 EMT programs have been associated with the development and progression of mammary tumors (61). Indeed, aberrantly elevated expression of the Six1 homeoprotein not only elicits the formation of mammary tumors (84), but also stimulates breast cancer EMT and metastasis in part via a TGF-β-dependent mechanism (85). Thus, thoroughly defining the role of TGF-β during type 1 EMT will be critical to the development of novel chemotherapeutics capable of circumventing these activities during the inappropriate reactivation of type 1 EMT programs in mammary tumors.
Type 2 EMT
The initiation of type 2 EMT is essential in maintaining tissue homeostasis through its ability to induce wound healing and tissue remodeling in response to noxious insults. An important distinction between type 1 and type 2 EMT is that the latter is governed by inflammatory reactions, whose cessation resolves the EMT phenotype following wound repair (2). A corollary states that chronic inflammation underlies the initiation of tissue and organ fibrosis, which eventually elicits organ dysfunction and destruction if left unabated. As depicted in Fig. 3, the process of wound healing involves the orchestrated activities of numerous cell types to facilitate the re-epithelialization of denuded areas (86). In fact, signaling by TGF-β and the ECM are essential in promoting the activation and differentiation of myofibroblasts, which are the key cells involved in the repair of damaged epithelium and scar formation (86). Working in concert with epithelial and endothelial cells, activated myofibroblasts secrete matrix metalloproteinases (MMPs) that digest injured tissues and facilitate the synthesis of a provisional ECM (87, 88). Exposure of platelets and infiltrating immune cells to provisional ECM components elicits platelet degranulation, angiogenesis, and wound contraction, of which the latter response is mediated by myofibroblasts during the final stages of re-epithelialization (86, 87, 89). Under normal circumstances, the inflammatory reactions within healed wounds resolve, thereby terminating type 2 EMT and stimulating the elimination of myofibroblasts via apoptosis (88). However, sustained myofibroblast activation in conjunction with chronic inflammation underlies the initiation of fibrotic disorders due to unresolved type 2 EMT reactions (86, 87). Myofibroblasts represent a specialized cell type that exhibit traits reminiscent of smooth muscle cells, particularly the expression of α-smooth muscle actin (α-SMA; (90, 91)). As a group, myofibroblasts derive from fibroblasts, from circulating progenitor cells, and from epithelial cells following their completion of EMT, which is typically assessed by monitoring the extent of α-SMA expression in fully transitioned cells (1). Exacerbated α-SMA expression is also indicative of fibrotic states and fibroproliferative disorders (92–94), as well as correlates with increased tumor invasion and decreased survival rates in cancer patients (95). Not surprisingly, α-SMA expression is induced by TGF-β via the concerted signaling inputs of Smad2/3, RhoA/Rock, and ERK1/2 (96–99). Furthermore, integrin activation by laminin, fibronectin, and collagen also cooperates with TGF-β to induce EMT and myofibroblasts activation, an event coupled to the formation of β-catenin:Smad2 signaling complexes (100–102). Thus, in addition to its role in promoting type 2 EMT, aberrant TGF-β signaling also supports chronic inflammatory reactions that promote the establishment of fibroproliferative disorders in humans.
Figure 3.
Type 2 EMT in wound healing and tissue regeneration. Normal epithelia that arose from type 1 EMT during development experience a noxious event or injury that triggers endothelial and epithelial cells to produce factors that mediate coagulation and clot formation. These events, coupled with enhanced MMP production facilitate the recruitment of immune cells and platelets to denuded wounds, leading to the production of provisional ECM and activation of angiogenesis. TGF-β enhances the healing process by inducing EMT in myofibroblasts, which drives their differentiation, activation, and migration into denuded wounds to facilitate wound restitution, closure, and re-epithelialization. The role of TGF-β in regulating type 2 EMT during mammary gland fibrosis is discussed in the text.
At present, the overall importance of fibrotic reactions in promoting mammary tumorigenesis remains to be determined definitively. However, mammographically dense and fibrotic breast tissue have been linked to the increased incidence of mammary tumorigenesis (103, 104). Along these lines, radiation therapy of breast cancers is associated with the development of fibrosis (105), and with the initiation of EMT via a TGF-β-dependent mechanism (106). Moreover, mammary tumorigenesis is often accompanied by intense desmoplastic and fibrotic reactions, which elicit the formation of rigid tumor microenvironments that (i) enhance the selection and expansion of developing neoplasms, particularly that of late-stage metastatic tumors, and (ii) predict for poor clinical outcomes in patients with breast cancer (107–109). Interestingly, these aberrant cellular activities are highly reminiscent of those attributed to TGF-β (110), suggesting that TGF-β stimulation of EMT and fibrosis may promote the development and progression of mammary tumors. This supposition is bolstered by a recent study showing that inhibiting the cross-linking of collagen during mammary fibrosis reduces breast cancer progression in mice (111). Collectively, these findings suggest that chemotherapeutic targeting of the EMT inducing activities of TGF-β may offer a novel two-pronged approach to alleviate breast cancer progression – namely, the inactivation of pathologic type 2 (i.e., fibrotic) and type 3 EMT (see below).
Mechanisms of Type 3 EMT Induced by TGF-β
The initiation of type 3 EMT is essential in facilitating cancer progression and metastasis, including that by mammary tumors (1, 2). In addition, type 3 EMT is primarily distinguished from its type 1 and 2 counterparts by the cellular context in which this phenotypic transition transpires – namely, type 3 EMT occurs in oncogenically transformed cells that house a variety of genetic and epigenetic abnormalities that conspire with the molecular cascade that underlies EMT to elicit metastatic dissemination. Even more remarkably, TGF-β stimulation of EMT has been associated with the selection and expansion of breast cancer stem cells (16–19), which by their nature exhibit robust resistance to traditional cancer chemotherapies (112). In the succeeding sections, we present our understanding of the molecular, cellular, and microenvironmental factors that contribute to the initiation of type 3 EMT by TGF-β in breast cancer cells.
Canonical TGF-β Signaling During EMT
Although the activities attributed to Smad2 and Smad3 during TGF-β signaling are commonly conjoined in the scientific literature, recent findings indicate that these latent transcription factors do in fact mediate distinct biological activities in response to TGF-β (113). These disparate functions mediated by Smads 2 and 3 also extend to EMT, which is inhibited by Smad2 and stimulated by Smad3. For instance, Smad2-deficiency enhances the development and progression of squamous cell carcinomas by elevating Snail expression and its induction of EMT (114), as well as elicits the acquisition of mesenchymal and fibrotic morphologies in hepatocytes (115). Interestingly, oncogenic Ras cooperates with Smads 2 and 3 to drive the formation of spindle cells and their subsequent acquisition of EMT and metastatic phenotypes (116). TGF-β stimulation of EMT in kidney cells results in the attenuated expression of SARA, an adapter molecule that facilitates the presentation of Smad2/3 to TβR-I (24). Moreover, depleting cells of SARA increased the ubiquitination and degradation of Smad2, leading to the acquisition of EMT phenotypes (117). In stark contrast, Smad3-deficiency (i) prevented TGF-β stimulation of EMT in lens (118) and renal (119) epithelial cells; (ii) reduced the EMT and migratory abilities of keratinocytes to TGF-β (120, 121); and (iii) preserved an epithelial phenotype in hepatocytes stimulated by TGF-β (115). Thus, these studies implicate a pro-EMT function associated with Smad3 activation, which is mirrored by the activation of Smad4 in pancreatic cells undergoing EMT induced by TGF-β (122). Consistent with its designation as an inhibitory Smad, over expression of Smad7 is sufficient to abrogate the ability of TGF-β to induce EMT in epithelial cells of the breast (123), liver (124), and lens (125). Collectively, these studies demonstrate that the expression and activities of TGF-β-regulated Smads are critical to the initiation and resolution of EMT in diverse epithelial cell lineages.
Smad2/3 activation also figures prominently in mediating TGF-β stimulation of EMT in MECs. Indeed, TGF-β signaling through Smads 2, 3, and 4 induce an EMT transcriptional program in normal MECs, a physiological reaction that is blocked by overexpression of Smad7 (123). Interestingly, chronic TGF-β signaling elicits a metastable EMT phenotype in normal MECs that is characterized by reduced Smad2/3 signaling, leading to MEC resistance to the cytostatic and apoptotic activities of TGF-β (126). Thus, EMT may underlie the conversion of TGF-β function from that of a tumor suppressor to a tumor promoter in mammary tumors (see below). Along these lines, Smad4-deficiency not only prevented TGF-β stimulation of EMT in normal and malignant MECs, but also alleviated its induction of bone metastasis by breast cancer cells in mice (127). Furthermore, targeting and inactivating Smad2/3 signaling using aptamer technology was observed to neutralize the ability of TGF-β to induce EMT in normal MECs (128). Interestingly, Smad2 signaling has recently been shown to promote EMT in MECs by enhancing the DNA binding activity of the DNA methyltransferase, DNMT1, leading to chronic epigenetic silencing of epithelial-associated genes (129). Finally, a recent study established that the aberrant coupling of TGF-β to BMP-regulated Smads (e.g., Smads 1 and 5) during mammary tumorigenesis confers a pro-migratory phenotype in breast cancer cells (130). Although a role for this unusual coupling event in mediating EMT by TGF-β was not investigated, it is nonetheless tempting to speculate that inappropriate cross-talk between TGF-β superfamily members may contribute to the pathophysiological outcomes of EMT initiated by TGF-β. Future studies will need to address this question, as well as define the underlying relationship between Smad-dependent and -independent signaling during TGF-β stimulation of EMT in MECs (see below).
Noncanonical TGF-β Signaling During EMT
The aberrant amplification of noncanonical TGF-β signaling systems plays a salient role in mediating the ability of TGF-β to induce EMT in normal and malignant MECs, and in underlying the initiation of the “TGF-β Paradox.” The function of noncanonical TGF-β effectors in coupling this cytokine to EMT and metastasis are discussed in the succeeding sections.
Rho-family GTPases
Oncogenic TGF-β signaling is often associated with the dysregulated activity of the Rho GTPase family, which includes RhoA/B/C, Rac1, and Cdc42 (1, 14, 20). This family of small GTP-binding proteins are anchored to the plasma membrane where they regulate dynamic changes in cell adhesion, morphology, and motility in part by modulating the formation of filopodia (e.g., Cdc42), lamellipodia (e.g., Rac1), and actin stress fibers (e.g., RhoA) (131, 132). For instance, RhoA activation mediates the dissolution of adhesion complexes at cell-cell junctions, while that of Rac1 actually promotes the formation of these same complexes (133, 134). Additionally, constitutive activation of Cdc42 by TβR-III inhibits directional migration induced by TGF-β (135). Interestingly, the expression and activation of RhoC enhances the invasion and EMT of breast (136), prostate (137), and colon (138) cancer cells. The ability of TGF-β to induce EMT in MECs requires the activation of RhoA and its downstream effector, p160ROCK (41). In addition, the coupling of TGF-β to RhoA and RhoC also correlates with altered expression of E-cadherin and α-SMA during EMT (96, 139). Recently, TβR-II-mediated phosphorylation of Par6 was shown to underlie the ubiquitination and degradation of RhoA, leading to the dissolution of tight junctions during the acquisition of EMT and metastatic phenotypes in breast cancer cells (140, 141). Along these lines, upregulation of miR-155 by canonical TGF-β signaling was observed to promote EMT in MECs by targeting the destruction of RhoA mRNA (142). In start contrast, reduced RhoA expression mediated by miR-31 was found to suppress, not promote, breast cancer metastasis (143, 144), suggesting an intricate and complex role for RhoA and its relatives in regulating the initiation of EMT and metastasis.
PI3K, AKT, and mTOR
Oncogenic TGF-β signaling and its stimulation of EMT also requires the activities of phosphoinositide 3-kinase (PI3K) and Akt, both of which confer proliferative and survival advantages to developing carcinomas (145). In addition, PI3K and Akt also mediate TGF-β stimulation of EMT in MECs (40), an event that arises directly from TGF-β receptor signaling inputs, or indirectly through their transactivation of the receptors for EGF (146) and PDGF (147). Interestingly, co-administration of TGF-β and EGF elicits an exaggerated EMT through the activation of ERK1/2 and PI3K/Akt (148). Somewhat surprisingly, pharmacological inhibition of PI3K/Akt had no effect on the morphologic and phenotypic characteristics of EMT; however, this same treatment regimen did alleviate the ability of TGF-β and EGF to induce cell migration and invasion (148), suggesting that the morphologic and motile features of EMT may in fact be distinct physiological entities. Along these lines, inactivating mTOR pharmacologically with rapamycin prevents TGF-β from increasing the physical size of MECs, as well as from stimulating their migration and invasion (42). As above, mTOR antagonism failed to impact the morphological features of EMT, which suggests that mTOR may facilitate the synergistic effects of TGF-β and EGF on EMT. Collectively, these studies highlight the essential function of the PI3K/Akt/mTOR pathway in promoting EMT and metastasis stimulated by TGF-β, while future studies need to clarify the underlying dissociation between “fibroblastoid-like” phenotypes and cell motility.
Nuclear Factor-κB
Nuclear factor-κB (NF-κB) plays a prominent role in regulating the initiation and resolution of inflammatory reactions, and in promoting the growth, angiogenesis, invasion, and survival of developing carcinomas (149). In nontransformed tissues, TGF-β typically inhibits the activation of NF-κB (49, 50, 150), presumably by inducing the expression of IκBα (151), and by promoting the formation of TβR-III:β-arrestin2 complexes that prevent IκBα degradation (152). In stark contrast, mammary tumorigenesis converts TGF-β from an inhibitor to a stimulator of NF-κB activity by inducing the formation of TβR-I:xIAP:TAB1:TAK1:IKKβ complexes (49, 50, 153). Furthermore, activation of this noncanonical effector system by TGF-β was found to be essential for its induction of EMT in normal and malignant MECs (49, 50, 153, 154), and for its stimulation of mammary tumor development via activation of the innate immune system (49). Moreover, the coupling of TGF-β to NF-κB activation underlies the ability for Ras-transformed breast cancer cells to colonize the lung (47, 155), and elicits the initiation of an autocrine Cox-2:PGE2:EP2 receptor signaling cascade that not only induces EMT in normal and malignant MECs, but also stimulates breast cancer metastasis (50, 51). Finally, TGF-β stimulation of NF-κB in post-EMT cells stimulates their migration by establishing a SDF-1/CXCR4 signaling axis (156). Collectively, these studies highlight the importance of NF-κB to the induction of EMT by TGF-β, while future studies need to assess the relative contribution of these events to enhanced survival and chemoresistance exhibited by post-EMT breast cancer cells.
MAP Kinases
The propensity of TGF-β to induce pathological EMT and metastasis is also associated with its stimulation of members of the MAP kinase family of protein kinases, including ERKs, JNKs, and p38 MAPKs (39, 157–159). For instance, pharmacological inhibition of MEK1/2 prevents TGF-β from stimulating EMT and its characteristic formation of actin stress fibers and delocalization of E-cadherin and ZO-1 from the cell surface in MECs (158). Similarly, methods that disrupt the coupling of TGF-β to JNK activation prevent the morphological and transcriptional changes associated with EMT (160, 161). Along these lines, there exists a dynamic interplay between TGF-β and its production of various ECM components, which subsequently potentiate the activation of MAP kinase pathways during EMT. For instance, the expression of type I collagen activates PI3K, Akt, and JNK to induce EMT (162, 163). Moreover, TGF-β in conjunction with vitronectin signaling is necessary in mediating TβR-II phosphorylation by Src, a phosphotransferase reaction operant in activating p38 MAPK and EMT in MECs (23, 45). Likewise, the coupling of TGF-β to ERK1/2 and p38 MAPK activation is dependent upon the localization of TGF-β receptors to lipid rafts, not clathrin-coated pits, and as such, cholesterol-depleting methodologies are sufficient to block cell migration and EMT stimulated by TGF-β (164). Collectively, these studies implicate MAP kinases as crucial mediators linking the ability of TGF-β and ECM components to promote EMT.
Integrin-linked Kinase
The coupling of TGF-β to its noncanonical effectors during type 3 EMT is further exacerbated upon the activation of integrin-linked kinase (ILK), which is a Ser/Thr protein kinase coupled to the activation of small GTPases, PI3K/Akt, and MAP kinases (165–167). ILK activation also leads to the inhibition of GSK-3β activity, which stabilizes β-catenin and facilitates its nuclear accumulation during EMT (166). Indeed, elevated expression of ILK in MECs is associated with their decreased expression of E-cadherin and increased invasion (168), and with their oncogenic transformation by hyperactive ERK1/2 and Akt (169). Along these lines, ILK-deficiency prevented TGF-β from stimulating cell migration and invasion in part by uncoupling this cytokine from regulation of the uPA/PAI-1 system (170). Finally, TGF-β stimulation of Smad2/3 induces PINCH-1 expression, which interacts physically with ILK during the initiation of EMT and its consequential loss of E-cadherin and ZO-1 expression (171). Collectively, these findings suggest that ILK interfaces integrin signaling with that of TGF-β, resulting in aberrant protease activation that drives the acquisition of EMT, invasive, and metastatic phenotypes.
Integrins and Focal Adhesion Signaling During EMT
Integrins and EMT Stimulated by TGF-β
Communication within cell microenvironments is controlled in part by integrins, which govern cell adhesion, migration, and invasion, as well as cell proliferation and survival (172, 173). Cells undergoing neoplastic transformation exhibit dramatically altered integrin expression profiles, as well as altered integrin affinities for ECM substrates, both of which enhance cancer cell invasion and metastasis (174). As a receptor family, integrins are unique in their capacity to physically link the ECM to cytoskeletal system within cells, thus enabling the efficient propagation of mechanotransduction in a bidirectional manner (111, 175). In addition, focal adhesion kinase (FAK) serves as a molecular bridge that links integrins to the receptors to EGF and PDGF, thereby conferring cell migration activities to these growth factors (176, 177). Integrins also play an important role in eliciting EMT and cell migration stimulated by TGF-β. For instance, αvβ6 and αvβ8 integrins bind latent TGF-β complexes and elicit the presentation of TGF-β to its cell surface receptors (178), presumably by promoting matrix metalloproteinase (MMP)-14 activation (27, 179). Along these lines, TGF-β induces the expression of α3β1 and αvβ3 integrins, which confer migration and invasion properties to MECs (45, 46, 56, 157). Administering neutralizing β1 integrin antibodies to MECs uncoupled TGF-β from the activation of p38 MAPK and the induction of EMT (157). In addition, genetic or pharmacologic inactivation of αvβ3 integrin in normal and malignant MECs prevented TGF-β from inducing EMT and pulmonary metastasis (45, 46, 56). Mechanistically, upregulated β3 integrin expression stimulated by TGF-β results in the FAK-dependent formation of β3 integrin:TβR-II complexes that promote the activation of Src and its phosphorylation of TβR-II at Y284 (56, 180). Upon its phosphorylation, Y284 coordinates the recruitment and binding of the SH2-domain proteins, Grb2 and ShcA, which promote p38 MAPK activation and the initiation of EMT (45, 46, 56). Importantly, measures that disrupt this oncogenic TGF-β signaling axis completely abrogate the ability of TGF-β to induce EMT, and to promote the metastasis of breast cancer cells to the lung (46, 180, 181) and bone (182). Recently, we observed an interesting interplay between β1 and β3 integrins in regulating MEC response to TGF-β, such that genetic inactivation of β1 integrin in MECs elicits a compensatory upregulation of β3 integrin expression that impacts the coupling of TGF-β to EMT and cell motility (J.G. Parvani and W.P. Schiemann, unpublished observation). These findings implicate “integrin switching” as a potentially dangerous mechanism that may enable metastatic breast cancers to escape integrin-based chemotherapies. Future studies clearly need to investigate the validity of this hypothesis, as well as to identify the repertoire of integrins capable of regulating the diverse pathophysiological activities of TGF-β in normal and malignant MECs.
Nonreceptor Protein Tyrosine Kinases and Adapter Molecules of Focal Adhesion Complexes
As mentioned above, EMT and oncogenic TGF-β signaling transpires through a β3 integrin:FAK:Src:phospho-Y284-TβR-II:Grb2:p38 MAPK signaling axis that forms constitutively in basal-like breast cancer cells (45, 46, 56, 180, 182). The importance of this αvβ3 integrin-based signaling axis in promoting the oncogenic activities of TGF-β in other genetically distinct breast cancer subtypes remains unexplored; however, a number of recent studies have identified essential functions for a variety of focal adhesion complex proteins in mediating the coupling of TGF-β to EMT and metastasis. Indeed, in addition to its ability to coordinate the formation of β3 integrin:TβR-II complexes, FAK expression and activity are essential in coupling TGF-β to EMT and p38 MAPK activation, and to inducing pulmonary metastasis of breast cancer cells (180). Adjuvant FAK chemotherapy also inhibited breast cancer growth by suppressing the ability of macrophages to infiltrate the primary mammary tumor (180), suggesting that the tumor promoting activities of FAK manifest in carcinoma cells and their associated stromal compartment. Along these lines, FAK is essential in mediating TGF-β stimulation of E-cadherin redistribution and α-SMA expression during EMT (183, 184). In addition, the phosphorylation and activation of p130Cas functions as a molecular rheostat that governs the balance between canonical and noncanonical TGF-β signaling inputs. Indeed, activated p130Cas forms a heteromeric complex with Smad3 and TβR-I, which diminishes the phosphorylation of Smad3 and uncouples TGF-β from regulation of cell cycle progression (185). Interestingly, breast cancer patients whose tumors express abnormally high levels of p130Cas exhibit tamoxifen- and adriamycin-resistance, as well as diminished time to disease recurrence (186, 187). Likewise, elevated p130Cas expression significantly reduced the latency of mammary tumor formation driven by transgenic expression of Her2/Neu (188). We recently observed elevated p130Cas expression to mark the development of metastasis in breast cancers, and to skew the balance of TGF-β signaling from canonical to noncanonical effectors in metastatic MECs (189).
Similar to p130Cas, the adapter molecules Hic5 and Dab2 also promote the coupling of TGF-β to its noncanonical effectors during EMT. Indeed, Hic5 is a member of the paxillin superfamily that functions in the cytoplasm as a component of focal adhesion complexes (190), and in the nucleus as a transcriptional co-activator of the androgen receptor (191). Polarized MECs express low levels of Hic5, which are increased rapidly during EMT via a RhoA/ROCK-dependent pathway (190, 192). Interestingly, the LIM domain of Hic5 binds and inactivates Smad3 and Smad7 in prostate cancer cells (193, 194), which collectively diminishes Smad-dependent gene expression (i.e., targeting Smad3) in the context of enhanced TGF-β receptor signaling (i.e., targeting Smad7). Whether Hic-5 possesses similar anti-Smad activity in breast cancers remains unknown; however, it is tempting to speculate that Hic5 may cooperate with p130Cas in amplifying the coupling of TGF-β to its noncanonical effectors.
Finally, the adaptor molecule, Dab2 (Disabled-2) regulates the dynamics associated with the remodeling of the actin cytoskeleton during MEC adhesion and migration (195). In contrast to p130Cas and Hic5, Dab2 associates with TGF-β receptors and facilitates their activation of Smad2/3 (26), as well as that of TAK1 and JNK, which stimulate fibronectin expression and cell migration during EMT (160, 196). In addition, TGF-β stimulation of EMT assembles Dab2:β1 integrin complexes that induce FAK activation. Mechanistically, translation of Dab2 mRNA is strongly repressed in polarized MECs by the actions of hnRNP E1, which binds structural elements in the 3’UTR of Dab2 transcripts. When activated by TGF-β, Akt2 phosphorylates and releases hnRNP E1 from Dab2 mRNA, thereby enabling the production of Dab2 and its initiation of EMT in MECs (197). Future studies need to identify other genes targeted by this novel post-transcriptional regulon, as well as to define their role in mediating the pathophysiological outcomes of EMT stimulated by TGF-β.
Gene Regulation-Coupled to EMT Induced by TGF-β
The ultimate phenotypic change associated with the activation of canonical and noncanonical TGF-β signaling inputs derives from altered patterns of gene expression and repression that transpire in a cell- and context-specific manner. In the succeeding sections, we highlight the important transcriptional mediators operant in driving and fine-tuning the EMT transcriptome targeted by TGF-β in normal and malignant MECs.
Nuclear Transcription Factors Targeted by TGF-β During EMT
Members of the Snail (SNAI1 and SNAI2/Slug), ZEB (ZEB1 and ZEB2/SIP1), basic helix-loop-helix (Twist), and Six family of homeobox (Six1) transcription factors are considered to be master regulators of EMT, including that stimulated by TGF-β (198, 199). As a group, these transcription factors play essential roles in mediating type I EMT during embryogenesis and tissue morphogenesis; however, their inappropriate reactivation of developmental EMT programs during tumorigenesis is considered a hallmark of disease progression and metastasis initiation (61). Indeed, activated Snail molecules readily form complexes with Smads 3 and 4 that collectively target conserved E-box sequences in the promoters for E-cadherin, occludin, and claudin, which strongly represses their expression and inactivates adherens (i.e., E-cadherin) and tight junction (i.e., occludins and claudin) complexes during EMT (200, 201). Similar targeting and inactivation of E-cadherin is associated with all of the aforementioned transcription factors, whose underlying roles in mediating the pathophysiology of EMT has been the subject of several recent reviews (see (198, 199)). Interestingly, dysregulated Myc expression has been observed to function cooperatively with Smad4 to induce an EMT-related transcriptional profile in normal and malignant MECs (202). Likewise, the reactivation of fibulin-5 expression in transitioning MECs initiated a positive-feedback loop that sensitized MECs to the EMT-promoting activities of TGF-β, an event dependent upon the synergistic induction of Twist expression by fibulin-5 and TGF-β (203). In addition, TGF-β stimulation of Smad3 results in upregulated Mdm2 expression, which destabilizes p53 during the initiation of breast cancer EMT and metastasis (204). Smad3/4 signaling also promotes the expression of HMGA2, which stimulates the EMT transcriptional program by inducing the expression of Snail, Slug, and Twist, while simultaneously repressing that of Id2 (205). Finally, members of the homeobox family of transcription factors have also been implicated in mediating EMT induced by TGF-β. For instance, inappropriate LBX1 (ladybird homeobox 1) expression drives EMT and its expansion of breast cancer stem cells by stimulating the expression of TGF-β2, Snail, and ZEBs 1 and 2 (206). Similarly, aberrant reactivation of the homeoprotein Six1 promotes the acquisition of EMT and metastatic phenotypes in breast cancer cells in part by upregulating the messages transduced through the TGF-β signaling system (85). Collectively, these findings highlight the role of developmental EMT pathways that enhance the oncogenic activities of TGF-β during mammary tumorigenesis.
Estrogen Receptor-α
Estrogen receptor (ER) status has long been recognized as an important prognostic marker in developing breast cancers, particularly in terms of its diagnostic and therapeutic value. Indeed, the loss of ER-α expression during mammary tumorigenesis is associated with poor clinical outcomes, and with increased likelihood of breast cancer metastasis and disease recurrence (207). More recently, ER-α has been linked to the initiation of EMT through its ability to activate metastasis associated protein 3 (MTA3) in MECs (208, 209). Mechanistically, MTA3 serves as a subunit of the Mi-2/NuRD chromatin remodeling complex, which represses the expression of Snail (208). Thus, mammary tumors that have lost expression of ER-α exhibit reduced MTA3 activity that results in the inappropriate expression of Snail and its subsequent stimulation of EMT (208, 209). This process is further enhanced by the ability of Snail to repress ER-α expression, and to induce the expression of components of the TGF-β signaling system (e.g., TGF-β2 and TβR-II; (208)), thereby creating a powerful positive feedback loop to further potentiate the acquisition and stabilization of EMT phenotypes. Moreover, ER-α interacts physically with Smad3 and inhibits its ability to regulate gene expression (210). Thus, the loss of ER-α expression and activity may play a prominent role in engendering the initiation of oncogenic TGF-β signaling in normal and malignant MECs (8). In fact, aberrant cytoplasmic localization of ER-α has recently been proposed as a novel histopathological marker to identify sarcomatoid breast cancers in vivo (211). Future studies clearly need to elucidate molecular mechanisms that underlie the dynamic relationship between ER-α and TGF-β in regulating EMT, and to identify novel biomarkers capable of staging and stratifying breast cancer patients on the basis of their EMT, ER-α, and TGF-β status.
TGF-β and microRNAs
Recent studies have implicated the aberrant expression of numerous microRNA (miRs) in the initiation of EMT, and in the development and progression of mammary tumors (212–214). Indeed, members of the miR-200 family of microRNAs maintain polarized epithelial phenotypes by repressing the expression of the EMT-inducing transcription factors ZEB1 and ZEB2/SIP-1. Accordingly, monitoring the expression of miR-200 family members can be used to distinguish well-differentiated and immotile tumors that express E-cadherin from their poorly-differentiated and highly motile counterparts that express vimentin (215). In addition, TGF-β abrogates the expression of miR-200 family members, leading to the expression of ZEB1 and ZEB2 and their consequential downregulation of E-cadherin expression to initiate EMT (216, 217). Not surprisingly, miR-200 family member expression is frequently downregulated in invasive and metastatic mammary tumors, particularly those possessing mesenchymal-type breast cancer cells (216). Once expressed, ZEB1 can further repress the expression of miR-200 family members, thereby stabilizing the EMT phenotype in transitioning MECs (218).
The stimulation of EMT by TGF-β also transpires through its regulation of additional miRs. Indeed, TGF-β stimulation of normal MECs elicits their upregulated expression of miR-155 via a Smad4-dependent pathway. Once expressed, miR-155 participates in EMT by downregulating RhoA expression, leading to the dissolution of tight junctions (142). Along these lines, upregulated expression of miR-21 induced by TGF-β abrogates the expression of several tumor suppressors, including a) peroxisome proliferator-activated receptor; b) tissue inhibitor of metalloproteinase-3; c) programmed cell death 4; and d) AT-rich interactive domain 1A (219). Additionally, miR-21 expression also participates in the initiation of EMT by downregulating the expression of tropomyosin, leading to enhanced breast cancer motility, invasion, and anchorage-independent growth (220, 221). Thus, the coupling of TGF-β to the regulation of miR expression and activity affords news avenues to potentially manipulate the pathophysiology associated with type 3 EMT in mammary tumors. As such, future studies need to rapidly and accurately define the cellular targets of EMT-associated miRs, and to determine the molecular mechanisms operant in regulating their expression in transitioning MECs.
DNA Hypermethylation
Hypermethylation and silencing of the E-cadherin promoter has been linked to the initiation of EMT, migration, and invasion in breast cancer cells (222–224). More recently, TGF-β signaling was observed to maintain DNA methylation patterns during EMT, resulting in the silencing of E-cadherin (CDH1), the tight junction genes CGN and CLDN4, and the protease KLK10/NES1. Mechanistically, overexpressing Smad7 in MECs or rendering them deficient in Smad2 inhibited the activity of the DNA methyltransferase, DNMT1, which suppressed EMT and cell motility by restoring E-cadherin expression (129). Along these lines, miR-200c and its relative, miR-141, normally inhibit the initiation of EMT and metastasis in MECs by suppressing the expression of ZEB1/2 (216, 217). However, during mammary tumorigenesis, aberrant DNA methylation inactivates expression of these miR-200 family members, leading to the acquisition of EMT and metastatic phenotypes in developing and progressing mammary tumors (225). Moreover, E-cadherin-deficiency that arises during EMT may in fact function as an initiating signal coupled to the expanded and directed hypermethylation of genes normally operant in suppressing mammary tumorigenesis (226). For instance, hypermethylation of the E-cadherin promoter marks Ras-transformed MECs that have undergone a stable EMT induced by serum versus a transient EMT induced by TGF-β (226). Collectively, these studies establish an essential role for DNA methylation in facilitating type 3 EMT stimulated by TGF-β, and in differentially stabilizing the EMT phenotype in response to varying stimuli.
Microenvironmental Inputs During EMT Stimulated by TGF-β
Tissue homeostasis in the breast is maintained by the balanced integration of signaling inputs derived from various tissue and cell architectures, and from their supporting microenvironment and ECM. Indeed, whereas normal mammary tissue specification requires reciprocal signaling inputs from distinct cell types and matrix proteins, the phenotype of developing mammary carcinomas is similarly dictated by the dynamic interplay between malignant cells and their accompanying stroma, which houses fibroblasts, endothelial cells, and a variety of infiltrating immune and progenitor cells (227–229). Along these lines, desmoplasia and fibrosis during mammary tumorigenesis can drive disease progression in a manner that mimics the oncogenic activities of TGF-β (110, 230), suggesting that the interactions between MECs and their supporting stromal constituents play pivotal roles in regulating EMT and metastasis stimulated by TGF-β. Recent findings pertaining to the connections between the microenvironment and EMT are summarized in the following sections.
Adherens Junctions and EMT
A hallmark of EMT is the dissolution of cell-cell junctions, particularly adherens junctions which derive from the homotypic interactions between adjacent E-cadherin molecules housed on neighboring MECs. Similar to integrins, the cytoplasmic domain of E-cadherin is tethered to the cytoskeleton through a heteromeric complex consisting of the α-, β-, and γ-catenins, which collectively serve in marking differentiated MECs and suppressing their tumorigenesis (231, 232). Interestingly, the process of EMT is often characterized by “cadherin switching,” a term referring to the ability of E-cadherin expression and activity to give way to that of N-cadherin as MECs acquire mesenchymal phenotypes (233). Functional inactivation of E-cadherin transpires through a variety of mechanisms, including hypermethylation and epigenetic silencing of its promoter (234), as well as protease-mediated cleavage and shedding of its ectodomain (231). In rare cases, mutational inactivation of the E-cadherin gene, CDH1, has been observed and linked to increased risk for cancer development in affected individuals (235). However, transcriptional repression is by far the most common mechanism employed by transitioning MECs to downregulate their expression of E-cadherin. Indeed, TGF-β stimulation of EMT represses E-cadherin expression primarily by targeting the expression of Snail, ZEB, and bHLH family members (see above). Moreover, upregulated expression of the mesenchymal cadherins, N-cadherin and cadherin-11, occur concomitantly the loss of E-cadherin expression and correlate with increased tumor invasiveness and poor clinical outcomes (236–239). At present, the dynamic relationship between E- and N-cadherin in mediating TGF-β stimulation of EMT and metastasis remains unresolved, as does the manner through which bifurcated TGF-β signals coupled selectively to epithelial versus mesenchymal transcriptional programs influence the pathophysiological outcomes of EMT induced by TGF-β (50, 180).
Neuronal Cell Adhesion Molecule and EMT
Neuronal cell adhesion molecule (NCAM) belongs to the immunoglobulin superfamily and mediates calcium-independent cell-cell adhesion (240). Inappropriate NCAM expression has been associated with cancer progression and poor prognosis in cancers of the pancreas and colorectal system (233, 240). In addition, TGF-β stimulation of EMT in MECs significantly upregulates their expression of NCAM, a reaction that requires the activation of Smad4 and inactivation of E-cadherin. Mechanistically, NCAM translocates to lipid rafts and activates a p59fyn:FAK:β1 integrin signaling axis that promotes EMT and cell invasion (241). Interestingly, EMT induced by TGF-β also activates matrix metalloproteinase (MMP)-28, which cleaves NCAM and latent TGF-β complexes (242). Thus, it remains unclear how upregulated NCAM expression and cleavage ultimately impact the ability of TGF-β to stimulate EMT in normal and malignant cells.
Protease Activation During EMT Induced by TGF-β
Matrix Metalloproteinases
One of the hallmarks of EMT is its propensity to bestow motile phenotypes in previously immotile cells (1–3). Matrix metalloproteinases (MMPs) are a superfamily of transmembrane and secreted endopeptidases that function in degrading a variety of ECM components, cytokines, and cell surface proteins and receptors. The net effect of these various MMP activities results in dramatic affects on cell differentiation, invasion, and EMT (243). Members of the MMP superfamily (e.g., MMPs 2, 9, 13, and 14; (179, 244–246)) also function in mediating the cleavage of latent TGF-β complexes, which releases mature TGF-β and initiates transmembrane signaling in neighboring MECs, as well as mediates E-cadherin cleavage and breast cancer progression (243, 247, 248). Along these lines, TGF-β is a potent regulator of the expression of MMPs 2, 9, and 13 (60, 203, 249–252), thereby establishing a positive autocrine TGF-β signaling loop that (i) drives breast cancer EMT, invasion, and metastasis, and (ii) is readily suppressed by constitutive c-Abl activation in normal and malignant MECs (60). Future studies need to address how aberrant MMP activation contributes to the initiation of type 2 EMT (see above), and how these events ultimately impact the initiation of type 3 EMT and metastasis by TGF-β in mammary tumors.
Urokinase Plasminogen Activator and Plasminogen Activator Inhibitor-1
Urokinase plasminogen activator (uPA) is serine protease that plays important roles in regulating the migration and invasion of breast cancer cells in part via its conversion of inactive plasminogen into active plasmin. Elevated expression of uPA correlates with increased tumor aggressiveness and poor clinical outcomes for a variety of cancers, including those of the breast (253–255). The role of uPA in promoting breast cancer progression and metastasis has been recapitulated in a mouse model of mammary tumorigenesis (255), and in a chick chorioallantoic membrane model of breast cancer metastasis, which also associated upregulated uPA expression with hypoxia-induced EMT (256). TGF-β induces uPA expression by activating JNK- and ILK-dependent signaling systems that functionally converge to induce EMT and increased cell motility (161, 170). As noted previously, these findings point to a prominent role of noncanonical TGF-β effectors in mediating the stimulation of EMT by TGF-β. Accordingly, the expression and activity of FAK is essential in stimulating the production of uPA and its initiation of metastasis in 4T1 cells (255), which we (46, 49, 51, 60, 180, 189, 203) and others (257–259) established as a late-stage model of TGF-β-responsive breast cancer. In addition, hypoxia-induced EMT stimulates the expression of the uPA receptor, uPAR, which interacts physically with α3β1 integrin and promotes the activation of Src, Akt, Rac1, and GSK-3β. The end product of these signaling inputs elicits Snail and Slug expression, which drive the acquisition of EMT phenotypes and loss of E-cadherin in transitioning cells (256, 260). Thus, future studies clearly need to define the connections linking the activation of these noncanonical TGF-β effectors to the formation of uPAR:integrin complexes.
Inappropriate activation of uPA is held in check by the expression of plasminogen activator inhibitor (PAI)-1 and PAI-2, which bind uPA:uPAR complexes and induce their internalization and degradation (253). Thus, elevated PAI-1/2 expression would be predicted to alleviate the EMT and metastasis promoting properties of uPA, an assumption that has been validated in a panel of breast, ovarian, endometrial, cervical, and osteosarcoma cell lines (261). Quite surprisingly, PAI-1 polymorphisms or its elevated expression has also been linked enhanced disease progression and metastasis development, and to decreased survival in breast cancer patients (253, 261, 262). TGF-β is a master regulator of PAI-1 expression, doing so through its stimulation of canonical and noncanonical effector systems (see (263)). In addition to binding and inactivating uPA:uPAR complexes, PAI-1 also interacts with vitronectin and prevents its activation of integrins (261), an event that may influence the coupling of integrin signaling to MEC migration. Thus, future studies need to clarify the tumor suppressing and promoting activities of PAI-1, particularly with respect to its role in mediating EMT and oncogenic TGF-β signaling in normal and malignant MECs.
Collagen
TGF-β has long be recognized for its ability to induce the expression of collagens (264), which function as important structural components of the ECM and serve as prominent ligands for integrins (243). In addition, activation of p38 MAPK by TGF-β upregulates the expression of MMPs 2 and 9, which cleave collagen to produce biologically active fragments that readily promote MEC migration and invasion (252). Along these lines, TGF-β stimulates breast cancer cells to upregulate their expression of the collagen receptor Endo180, which internalizes collagen and induces the growth of mammary tumors in mice (265). More recently, collagen binding to β1 integrins has been shown to activate TGF-β receptor signaling independent of TGF-β ligands, leading to the activation of FAK and Src that culminate in the stimulation of Smad2/3 activity in MECs (266). Collectively, these findings establish that TGF-β and collagen engage one another in a reciprocal relationship, yet how these events impact the ability of TGF-β to promote the acquisition of EMT and metastatic phenotypes mammary tumors remains an unresolved and interesting question.
Fibronectin
Fibronectin is an important component of the ECM and its expression is upregulated dramatically by TGF-β during EMT (264, 267). Functionally, fibronectin acts as a ligand for integrins during cell adhesion and migration, particularly in Ras-transformed MECs which concomitantly upregulate α5β1 integrin (268). Importantly, administration of neutralizing antibodies against α5 integrin blocked the ability of fibronectin and TGF-β to stimulate EMT and cell motility in MECs (268). In addition, fibronectin expression has been shown to modulate the response of cells to TGF-β. For instance, the ability of TGF-β to induce anchorage-independent growth in fibroblasts could be recapitulated by administration of fibronectin, whose activation of cell signaling was dependent upon integrin ligation (264). Besides its ability to enhance TGF-β stimulation of EMT in bronchial epithelial cells (269), fibronectin expression has also been linked to the development of the “premetastatic niche,” which serves as a depot to recruit circulating progenitor cells and metastatic carcinoma cells to sites of secondary tumor growth (270, 271). Future studies need to assess the relative contributions of TGF-β and fibronectin in mediating EMT and its potential involvement regulating the formation of metastatic niches during breast cancer progression.
Conclusions and Future Directions
TGF-β is universally recognized as a master regulator of EMT, including that occurring during embryonic develop and tissue morphogenesis (i.e., type 1 EMT), during wound healing and tissue fibrosis (i.e., type 2 EM), and during invasion and metastasis (i.e., type 3 EMT). Equally exciting are recent findings linking EMT stimulated by TGF-β to the acquisition of “stem-like” phenotypes in developing and progressing mammary tumors (16–19). Thus, pharmacological targeting of the TGF-β signaling system to alleviate EMT may elicit chemosensitivity in cancer stem cells previously resistant to standard treatment regimens, a supposition supported by recent findings obtained in a preclinical model of breast cancer progression (19). A corollary states that the phenomenon underlying selection and expansion of cancer stem cells via EMT may be “druggable” in clinical settings. Accordingly, high-throughput chemical screening technologies identified salinomycin as a novel agent capable of targeting breast cancer stem cells, thereby inhibiting mammary tumor growth in part by promoting epithelial differentiation (272). Future studies need to determine the efficacy of salinomycin and related compounds in antagonizing EMT stimulated by TGF-β in normal and malignant MECs, as well as investigate the relative contribution of cell microenvironments in mediating the various pathophysiological outcomes of EMT induced by TGF-β. Ultimately, these findings will form the foundation necessary to manipulate EMT and its initiation of the “TGF-β Paradox” in mammary tumors, and as such, to one day improve the clinical course of patients with metastatic breast cancer.
Figure 4.
Type 3 EMT in cancer metastasis. Normal epithelia that arose from type I EMT during development experience a carcinogenic event that ultimately results in their oncogenic transformation and tumor formation. The development and progression of mammary tumors is accompanied by their acquisition of dysplastic and abnormal morphologies, and by their evolution in chronically inflamed tumor microenvironments, which further enhances their acquisition of EMT and fibrotic phenotypes. Through its ability to stimulate oncogenic EMT, TGF-β enables transitioned mammary carcinoma cells to invade the underlying basement membrane (BM) and escape the confines of the primary tumor. Once liberated, metastatic MECs undergo intravasation and traverse the blood stream prior to taking up residence at distant locales, an event that ultimately leads to disease recurrence and poor clinical outcomes in breast cancer patients. See text for specific details on the molecular mechanisms whereby TGF-β promotes type 3 EMT and metastasis in breast cancer cells.
Acknowledgements
We thank members of the Schiemann Laboratory for critical comments and reading of the manuscript. W.P.S. was supported by grants from the National Institutes of Health (CA114039 and CA129359), the Komen Foundation (BCTR0706967), and the Department of Defense (BC084651), while M.A.T. was supported by the Department of Defense (BC093128).
Abbreviations
- α-SMA
α-smooth muscle actin
- BMP
bone morphogenic protein
- ECM
extracellular matrix
- EGF
epidermal growth factor
- EMT
epithelial-mesenchymal transition
- ERK
extracellular signal-regulated kinase
- FAK
focal adhesion kinase
- JNK
c-Jun N-terminal kinase
- MAP kinase
mitogen-activated protein kinase
- MEC
mammary epithelial cell
- mTOR
mammalian target of rapamycin
- MET
mesenchymal-epithelial transition
- MTA3
Metastasis associated protein 3
- NF-κB
nuclear factor-κB
- PAI
plasminogen activator inhibitor
- PDGF
platelet-derived growth factor
- PI3K
phosphoinositide-3-kinase
- TβR-I
TGF-β type I receptor
- TβR-II
TGF-β type II receptor
- TβR-III
TGF-β type III receptors
- TGF-β
transforming growth factor-β
- uPA
urokinase plasminogen activator
- uPAR
uPA receptor
- ZO-1
zonula occluden-1
References
- 1.Wendt MK, Allington TM, Schiemann WP. Mechanisms of the epithelial-mesenchymal transition by TGF-β. Future Oncol. 2009;5(8):1145–1168. doi: 10.2217/fon.09.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119(6):1420–1428. doi: 10.1172/JCI39104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139(5):871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Yang J, Weinberg RA. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev Cell. 2008;14(6):818–829. doi: 10.1016/j.devcel.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Hugo H, Ackland ML, Blick T, Lawrence MG, Clements JA, Williams ED, et al. Epithelial--mesenchymal and mesenchymal--epithelial transitions in carcinoma progression. J Cell Physiol. 2007;213(2):374–383. doi: 10.1002/jcp.21223. [DOI] [PubMed] [Google Scholar]
- 6.Wells A, Yates C, Shepard CR. E-cadherin as an indicator of mesenchymal to epithelial reverting transitions during the metastatic seeding of disseminated carcinomas. Clin Exp Metastasis. 2008;25(6):621–628. doi: 10.1007/s10585-008-9167-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barcellos-Hoff MH, Akhurst RJ. TGF-β in breast cancer: too much, too late. Breast Cancer Res. 2009;11(1):202. doi: 10.1186/bcr2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buck MB, Knabbe C. TGF-β signaling in breast cancer. Ann NY Acad Sci. 2006;1089:119–126. doi: 10.1196/annals.1386.024. [DOI] [PubMed] [Google Scholar]
- 9.Serra R, Crowley MR. Mouse models of TGF-β impact in breast development and cancer. Endocr Relat Cancer. 2005;12(4):749–760. doi: 10.1677/erc.1.00936. [DOI] [PubMed] [Google Scholar]
- 10.Schiemann WP. Targeted TGF-β chemotherapies: friend or foe in treating human malignancies? Expert Rev Anticancer Ther. 2007;7(5):609–611. doi: 10.1586/14737140.7.5.609. [DOI] [PubMed] [Google Scholar]
- 11.Shackleton M, Vaillant F, Simpson KJ, Stingl J, Smyth GK, Asselin-Labat ML, et al. Generation of a functional mammary gland from a single stem cell. Nature. 2006;439(7072):84–88. doi: 10.1038/nature04372. [DOI] [PubMed] [Google Scholar]
- 12.Stingl J, Raouf A, Eirew P, Eaves CJ. Deciphering the mammary epithelial cell hierarchy. Cell Cycle. 2006;5(14):1519–1522. doi: 10.4161/cc.5.14.2983. [DOI] [PubMed] [Google Scholar]
- 13.Villadsen R, Fridriksdottir AJ, Ronnov-Jessen L, Gudjonsson T, Rank F, LaBarge MA, et al. Evidence for a stem cell hierarchy in the adult human breast. J Cell Biol. 2007;177(1):87–101. doi: 10.1083/jcb.200611114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heldin CH, Landstrom M, Moustakas A. Mechanism of TGF-β signaling to growth arrest, apoptosis, and epithelial-mesenchymal transition. Curr Opin Cell Biol. 2009;21(2):166–176. doi: 10.1016/j.ceb.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Zavadil J, Bottinger EP. TGF-β and epithelial-to-mesenchymal transitions. Oncogene. 2005;24(37):5764–5774. doi: 10.1038/sj.onc.1208927. [DOI] [PubMed] [Google Scholar]
- 16.Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133(4):704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morel AP, Lievre M, Thomas C, Hinkal G, Ansieau S, Puisieux A. Generation of breast cancer stem cells through epithelial-mesenchymal transition. PLoS ONE. 2008;3(8):e2888. doi: 10.1371/journal.pone.0002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ben-Porath I, Thomson MW, Carey VJ, Ge R, Bell GW, Regev A, et al. An embryonic stem cell-like gene expression signature in poorly differentiated aggressive human tumors. Nat Genet. 2008;40(5):499–507. doi: 10.1038/ng.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shipitsin M, Campbell LL, Argani P, Weremowicz S, Bloushtain-Qimron N, Yao J, et al. Molecular definition of breast tumor heterogeneity. Cancer Cell. 2007;11(3):259–273. doi: 10.1016/j.ccr.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 20.Xu J, Lamouille S, Derynck R. TGF-β-induced epithelial to mesenchymal transition. Cell Res. 2009;19(2):156–172. doi: 10.1038/cr.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chang H, Brown CW, Matzuk MM. Genetic analysis of the mammalian TGF-β superfamily. Endocr Rev. 2002;23(6):787–823. doi: 10.1210/er.2002-0003. [DOI] [PubMed] [Google Scholar]
- 22.Massague J, Seoane J, Wotton D. Smad transcription factors. Genes Dev. 2005;19(23):2783–2810. doi: 10.1101/gad.1350705. [DOI] [PubMed] [Google Scholar]
- 23.Galliher AJ, Neil JR, Schiemann WP. Role of TGF-β in cancer progression. Future Oncol. 2006;2(6):743–763. doi: 10.2217/14796694.2.6.743. [DOI] [PubMed] [Google Scholar]
- 24.Tsukazaki T, Chiang TA, Davison AF, Attisano L, Wrana JL. SARA, a FYVE domain protein that recruits Smad2 to the TGF-β receptor. Cell. 1998;95(6):779–791. doi: 10.1016/s0092-8674(00)81701-8. [DOI] [PubMed] [Google Scholar]
- 25.Miura S, Takeshita T, Asao H, Kimura Y, Murata K, Sasaki Y, et al. Hgs (Hrs), a FYVE domain protein, is involved in Smad signaling through cooperation with SARA. Mol Cell Biol. 2000;20(24):9346–9355. doi: 10.1128/mcb.20.24.9346-9355.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hocevar BA, Smine A, Xu XX, Howe PH. The adaptor molecule Disabled-2 links the TGF-β receptors to the Smad pathway. EMBO J. 2001;20(11):2789–2801. doi: 10.1093/emboj/20.11.2789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mok SC, Wong KK, Chan RK, Lau CC, Tsao SW, Knapp RC, et al. Molecular cloning of differentially expressed genes in human epithelial ovarian cancer. Gynecol Oncol. 1994;52(2):247–252. doi: 10.1006/gyno.1994.1040. [DOI] [PubMed] [Google Scholar]
- 28.Xu XX, Yang W, Jackowski S, Rock CO. Cloning of a novel phosphoprotein regulated by colony-stimulating factor 1 shares a domain with the Drosophila disabled gene product. J Biol Chem. 1995;270(23):14184–14191. doi: 10.1074/jbc.270.23.14184. [DOI] [PubMed] [Google Scholar]
- 29.Hayashi H, Abdollah S, Qiu Y, Cai J, Xu YY, Grinnell BW, et al. The MAD-related protein Smad7 associates with the TGF-β receptor and functions as an antagonist of TGF-β signaling. Cell. 1997;89:1165–1173. doi: 10.1016/s0092-8674(00)80303-7. [DOI] [PubMed] [Google Scholar]
- 30.Nakao A, Afrakht M, Moren A, Nakayama T, Christian JL, Heuchel R, et al. Identification of Smad7, a TGF-β-inducible antagonist of TGF-β signalling. Nature. 1997;389:631–635. doi: 10.1038/39369. [DOI] [PubMed] [Google Scholar]
- 31.Souchelnytskyi S, Nakayama T, Nakao A, Moren A, Heldin CH, Christian JL, et al. Physical and functional interaction of murine and Xenopus Smad7 with bone morphogenetic protein receptors and TGF-β receptors. J. Biol. Chem. 1998;273:25364–25370. doi: 10.1074/jbc.273.39.25364. [DOI] [PubMed] [Google Scholar]
- 32.Ebisawa T, Fukuchi M, Murakami G, Chiba T, Tanaka K, Imamura T, et al. Smurf1 interacts with TGF-β type I receptor through Smad7 and induces receptor degradation. J Biol Chem. 2001;276(16):12477–12480. doi: 10.1074/jbc.C100008200. [DOI] [PubMed] [Google Scholar]
- 33.Kavsak P, Rasmussen RK, Causing CG, Bonni S, Zhu H, Thomsen GH, et al. Smad7 binds to Smurf2 to form an E3 ubiquitin ligase that targets the TGF-β receptor for degradation. Mol Cell. 2000;6(6):1365–1375. doi: 10.1016/s1097-2765(00)00134-9. [DOI] [PubMed] [Google Scholar]
- 34.Datta PK, Moses HL. STRAP and Smad7 synergize in the inhibition of TGF-β signaling. Mol Cell Biol. 2000;20(9):3157–3167. doi: 10.1128/mcb.20.9.3157-3167.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ibarrola N, Kratchmarova I, Nakajima D, Schiemann WP, Moustakas A, Pandey A, et al. Cloning of a novel signaling molecule, AMSH-2, that potentiates TGF-β signaling. BMC Cell Biol. 2004;5:2. doi: 10.1186/1471-2121-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koinuma D, Shinozaki M, Komuro A, Goto K, Saitoh M, Hanyu A, et al. Arkadia amplifies TGF-β superfamily signalling through degradation of Smad7. EMBO J. 2003;22(24):6458–6470. doi: 10.1093/emboj/cdg632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu FY, Li XZ, Peng YM, Liu H, Liu YH. Arkadia-Smad7-mediated positive regulation of TGF-β signaling in a rat model of tubulointerstitial fibrosis. Am J Nephrol. 2007;27(2):176–183. doi: 10.1159/000100518. [DOI] [PubMed] [Google Scholar]
- 38.Liu W, Rui H, Wang J, Lin S, He Y, Chen M, et al. Axin is a scaffold protein in TGF-β signaling that promotes degradation of Smad7 by Arkadia. EMBO J. 2006;25(8):1646–1658. doi: 10.1038/sj.emboj.7601057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bakin AV, Rinehart C, Tomlinson AK, Arteaga CL. p38 mitogen-activated protein kinase is required for TGF-β-mediated fibroblastic transdifferentiation and cell migration. J Cell Sci. 2002;115(Pt):3193–3206. doi: 10.1242/jcs.115.15.3193. 15. [DOI] [PubMed] [Google Scholar]
- 40.Bakin AV, Tomlinson AK, Bhowmick NA, Moses HL, Arteaga CL. Phosphatidylinositol 3-kinase function is required for TGF-β-mediated epithelial to mesenchymal transition and cell migration. J Biol Chem. 2000;275(47):36803–36810. doi: 10.1074/jbc.M005912200. [DOI] [PubMed] [Google Scholar]
- 41.Bhowmick NA, Ghiassi M, Bakin A, Aakre M, Lundquist CA, Engel ME, et al. TGF-β1 mediates epithelial to mesenchymal transdifferentiation through a RhoA-dependent mechanism. Mol Biol Cell. 2001;12(1):27–36. doi: 10.1091/mbc.12.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lamouille S, Derynck R. Cell size and invasion in TGF-β-induced epithelial to mesenchymal transition is regulated by activation of the mTOR pathway. J Cell Biol. 2007;178(3):437–451. doi: 10.1083/jcb.200611146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Perlman R, Schiemann WP, Brooks MW, Lodish HF, Weinberg RA. TGF-β-induced apoptosis is mediated by the adapter protein Daxx that facilitates JNK activation. Nat Cell Biol. 2001;3(8):708–714. doi: 10.1038/35087019. [DOI] [PubMed] [Google Scholar]
- 44.Zavadil J, Bitzer M, Liang D, Yang YC, Massimi A, Kneitz S, et al. Genetic programs of epithelial cell plasticity directed by TGF-β. Proc Natl Acad Sci USA. 2001;98(12):6686–6691. doi: 10.1073/pnas.111614398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Galliher AJ, Schiemann WP. β3 integrin and Src facilitate TGF-β mediated induction of epithelial-mesenchymal transition in mammary epithelial cells. Breast Cancer Res. 2006;8(4):R42. doi: 10.1186/bcr1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Galliher-Beckley AJ, Schiemann WP. Grb2 binding to Tyr284 in TβR-II is essential for mammary tumor growth and metastasis stimulated by TGF-β. Carcinogenesis. 2008;29(2):244–251. doi: 10.1093/carcin/bgm245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arsura M, Panta GR, Bilyeu JD, Cavin LG, Sovak MA, Oliver AA, et al. Transient activation of NF-κB through a TAK1/IKK kinase pathway by TGF-β1 inhibits AP-1/SMAD signaling and apoptosis: implications in liver tumor formation. Oncogene. 2003;22(3):412–425. doi: 10.1038/sj.onc.1206132. [DOI] [PubMed] [Google Scholar]
- 48.Park J-I, Lee M-G, Cho K, Park B-J, Chae K-S, Byun D-S, et al. TGF-β1 activates interleukin-6 expression in prostate cancer cells through the synergistic collaboration of the Smad2, p38-NF-κB, JNK, and Ras signaling pathways. Oncogene. 2003;22:4314–4332. doi: 10.1038/sj.onc.1206478. [DOI] [PubMed] [Google Scholar]
- 49.Neil JR, Schiemann WP. Altered TAB1:IκB kinase interaction promotes TGF-β-mediated NF-κB activation during breast cancer progression. Cancer Res. 2008;68(5):1462–1470. doi: 10.1158/0008-5472.CAN-07-3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Neil JR, Johnson KM, Nemenoff RA, Schiemann WP. Cox-2 inactivates Smad signaling and enhances EMT stimulated by TGF-β through a PGE2-dependent mechanisms. Carcinogenesis. 2008;29(11):2227–2235. doi: 10.1093/carcin/bgn202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tian M, Schiemann WP. PGE2 receptor EP2 mediates the antagonistic effect of COX-2 on TGF-β signaling during mammary tumorigenesis. FASEB J. 2010;24(4):1105–1116. doi: 10.1096/fj.09-141341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dong M, How T, Kirkbride KC, Gordon KJ, Lee JD, Hempel N, et al. The type III TGF-β receptor suppresses breast cancer progression. J Clin Invest. 2007;117(1):206–217. doi: 10.1172/JCI29293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sun L, Chen C. Expression of TGF-β type III receptor suppresses tumorigenicity of human breast cancer MDA-MB-231 cells. J Biol Chem. 1997;272(40):25367–25372. doi: 10.1074/jbc.272.40.25367. [DOI] [PubMed] [Google Scholar]
- 54.Gordon KJ, Blobe GC. Role of TGF-β superfamily signaling pathways in human disease. Biochim Biophys Acta. 2008;1782(4):197–228. doi: 10.1016/j.bbadis.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 55.Gordon KJ, Dong M, Chislock EM, Fields TA, Blobe GC. Loss of type III TGF-β receptor expression increases motility and invasiveness associated with epithelial to mesenchymal transition during pancreatic cancer progression. Carcinogenesis. 2008;29(2):252–262. doi: 10.1093/carcin/bgm249. [DOI] [PubMed] [Google Scholar]
- 56.Galliher AJ, Schiemann WP. Src phosphorylates Tyr284 in TGF-β type II receptor and regulates TGF-β stimulation of p38 MAPK during breast cancer cell proliferation and invasion. Cancer Res. 2007;67(8):3752–3758. doi: 10.1158/0008-5472.CAN-06-3851. [DOI] [PubMed] [Google Scholar]
- 57.Park SS, Eom YW, Kim EH, Lee JH, Min DS, Kim S, et al. Involvement of c-Src kinase in the regulation of TGF-β1-induced apoptosis. Oncogene. 2004;23(37):6272–6281. doi: 10.1038/sj.onc.1207856. [DOI] [PubMed] [Google Scholar]
- 58.Horowitz JC, Rogers DS, Sharma V, Vittal R, White ES, Cui Z, et al. Combinatorial activation of FAK and AKT by TGF-β1 confers an anoikis-resistant phenotype to myofibroblasts. Cell Signal. 2007;19(4):761–771. doi: 10.1016/j.cellsig.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thannickal VJ, Lee DY, White ES, Cui Z, Larios JM, Chacon R, et al. Myofibroblast differentiation by TGF-β1 is dependent on cell adhesion and integrin signaling via focal adhesion kinase. J Biol Chem. 2003;278(14):12384–12389. doi: 10.1074/jbc.M208544200. [DOI] [PubMed] [Google Scholar]
- 60.Allington TM, Galliher-Beckley AJ, Schiemann WP. Activated Abl kinase inhibits oncogenic TGF-β signaling and tumorigenesis in mammary tumors. FASEB J. 2009;23(12):4231–4243. doi: 10.1096/fj.09-138412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Micalizzi DS, Ford HL. Epithelial-mesenchymal transition in development and cancer. Future Oncol. 2009;5(8):1129–1143. doi: 10.2217/fon.09.94. [DOI] [PubMed] [Google Scholar]
- 62.Acloque H, Adams MS, Fishwick K, Bronner-Fraser M, Nieto MA. Epithelial-mesenchymal transitions: the importance of changing cell state in development and disease. J Clin Invest. 2009;119(6):1438–1449. doi: 10.1172/JCI38019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Skromne I, Stern CD. Interactions between Wnt and Vg1 signalling pathways initiate primitive streak formation in the chick embryo. Development. 2001;128(15):2915–2927. doi: 10.1242/dev.128.15.2915. [DOI] [PubMed] [Google Scholar]
- 64.Popperl H, Schmidt C, Wilson V, Hume CR, Dodd J, Krumlauf R, et al. Misexpression of Cwnt8C in the mouse induces an ectopic embryonic axis and causes a truncation of the anterior neuroectoderm. Development. 1997;124(15):2997–3005. doi: 10.1242/dev.124.15.2997. [DOI] [PubMed] [Google Scholar]
- 65.Liu P, Wakamiya M, Shea MJ, Albrecht U, Behringer RR, Bradley A. Requirement for Wnt3 in vertebrate axis formation. Nat Genet. 1999;22(4):361–365. doi: 10.1038/11932. [DOI] [PubMed] [Google Scholar]
- 66.Chea HK, Wright CV, Swalla BJ. Nodal signaling and the evolution of deuterostome gastrulation. Dev Dyn. 2005;234(2):269–278. doi: 10.1002/dvdy.20549. [DOI] [PubMed] [Google Scholar]
- 67.Zhou X, Sasaki H, Lowe L, Hogan BL, Kuehn MR. Nodal is a novel TGF-β-like gene expressed in the mouse node during gastrulation. Nature. 1993;361(6412):6543–7. doi: 10.1038/361543a0. [DOI] [PubMed] [Google Scholar]
- 68.Conlon FL, Lyons KM, Takaesu N, Barth KS, Kispert A, Herrmann B, et al. A primary requirement for nodal in the formation and maintenance of the primitive streak in the mouse. Development. 1994;120(7):1919–1928. doi: 10.1242/dev.120.7.1919. [DOI] [PubMed] [Google Scholar]
- 69.Birsoy B, Kofron M, Schaible K, Wylie C, Heasman J. Vg1 is an essential signaling molecule in Xenopus development. Development. 2006;133(1):15–20. doi: 10.1242/dev.02144. [DOI] [PubMed] [Google Scholar]
- 70.Shah SBSI, Hume CR, Kessler DS, Lee KJ, Stern CD, Dodd J. Misexpression of chick Vg1 in the marginal zone induces primitive streak formation. Development. 1997;125(24):5127–5138. doi: 10.1242/dev.124.24.5127. [DOI] [PubMed] [Google Scholar]
- 71.Sauka-Spengler T, Bronner-Fraser M. A gene regulatory network orchestrates neural crest formation. Nat Rev Mol Cell Biol. 2008;9(7):557–568. doi: 10.1038/nrm2428. [DOI] [PubMed] [Google Scholar]
- 72.Raible DW. Development of the neural crest: achieving specificity in regulatory pathways. Curr Opin Cell Biol. 2006;18(6):698–703. doi: 10.1016/j.ceb.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 73.Correia AC, Costa M, Moraes F, Bom J, Novoa A, Mallo M. BMP2 is required for migration but not for induction of neural crest cells in the mouse. Dev Dyn. 2007;236(9):2493–2501. doi: 10.1002/dvdy.21256. [DOI] [PubMed] [Google Scholar]
- 74.Wu MY, Hill CS. TGF-β superfamily signaling in embryonic development and homeostasis. Dev Cell. 2009;16(3):329–343. doi: 10.1016/j.devcel.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 75.Boyer AS, Ayerinskas II, Vincent EB, McKinney LA, Weeks DL, Runyan RB. TGF-β2 and TGF-β3 have separate and sequential activities during epithelial-mesenchymal cell transformation in the embryonic heart. Dev Biol. 1999;208(2):530–545. doi: 10.1006/dbio.1999.9211. [DOI] [PubMed] [Google Scholar]
- 76.Mercado-Pimentel ME, Hubbard AD, Runyan RB. Endoglin and Alk5 regulate epithelial-mesenchymal transformation during cardiac valve formation. Dev Biol. 2007;304(1):420–432. doi: 10.1016/j.ydbio.2006.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mercado-Pimentel ME, Runyan RB. Multiple TGF-β isoforms and receptors function during epithelial-mesenchymal cell transformation in the embryonic heart. Cells Tissues Organs. 2007;185(1–3):146–156. doi: 10.1159/000101315. [DOI] [PubMed] [Google Scholar]
- 78.Kaartinen V, Voncken JW, Shuler C, Warburton D, Bu D, Heisterkamp N, et al. Abnormal lung development and cleft palate in mice lacking TGF-β3 indicates defects of epithelial-mesenchymal interaction. Nat Genet. 1995;11(4):415–421. doi: 10.1038/ng1295-415. [DOI] [PubMed] [Google Scholar]
- 79.Ahmed S, Liu CC, Nawshad A. Mechanisms of palatal epithelial seam disintegration by TGF-β3. Dev Biol. 2007;309(2):193–207. doi: 10.1016/j.ydbio.2007.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Brown CB, Boyer AS, Runyan RB, Barnett JV. Requirement of type III TGF-β receptor for endocardial cell transformation in the heart. Science. 1999;283(5410):2080–2082. doi: 10.1126/science.283.5410.2080. [DOI] [PubMed] [Google Scholar]
- 81.Nakajima A, Ito Y, Asano M, Maeno M, Iwata K, Mitsui N, et al. Functional role of TGF-β type III receptor during palatal fusion. Dev Dyn. 2007;236(3):791–801. doi: 10.1002/dvdy.21090. [DOI] [PubMed] [Google Scholar]
- 82.Nelson CM, Vanduijn MM, Inman JL, Fletcher DA, Bissell MJ. Tissue geometry determines sites of mammary branching morphogenesis in organotypic cultures. Science. 2006;314(5797):298–300. doi: 10.1126/science.1131000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ewald AJ, Brenot A, Duong M, Chan BS, Werb Z. Collective epithelial migration and cell rearrangements drive mammary branching morphogenesis. Dev Cell. 2008;14(4):570–581. doi: 10.1016/j.devcel.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.McCoy EL, Iwanaga R, Jedlicka P, Abbey NS, Chodosh LA, Heichman KA, et al. Six1 expands the mouse mammary epithelial stem/progenitor cell pool and induces mammary tumors that undergo epithelial-mesenchymal transition. J Clin Invest. 2009;119(9):2663–2677. doi: 10.1172/JCI37691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Micalizzi DS, Christensen KL, Jedlicka P, Coletta RD, Baron AE, Harrell JC, et al. The Six1 homeoprotein induces human mammary carcinoma cells to undergo epithelial-mesenchymal transition and metastasis in mice through increasing TGF-β signaling. J Clin Invest. 2009;119(9):2678–2690. doi: 10.1172/JCI37815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wynn TA. Cellular and molecular mechanisms of fibrosis. J Pathol. 2008;214(2):199–210. doi: 10.1002/path.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wynn TA. Common and unique mechanisms regulate fibrosis in various fibroproliferative diseases. J Clin Invest. 2007;117(3):524–529. doi: 10.1172/JCI31487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Radisky DC, Przybylo JA. Matrix metalloproteinase-induced fibrosis and malignancy in breast and lung. Proc Am Thorac Soc. 2008;5(3):316–322. doi: 10.1513/pats.200711-166DR. [DOI] [PubMed] [Google Scholar]
- 89.Pohlers D, Brenmoehl J, Loffler I, Muller CK, Leipner C, Schultze-Mosgau S, et al. TGF-β and fibrosis in different organs - molecular pathway imprints. Biochim Biophys Acta. 2009;1792(8):746–756. doi: 10.1016/j.bbadis.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 90.Hay ED. The mesenchymal cell, its role in the embryo, and the remarkable signaling mechanisms that create it. Dev Dyn. 2005;233(3):706–720. doi: 10.1002/dvdy.20345. [DOI] [PubMed] [Google Scholar]
- 91.Vaughan MB, Howard EW, Tomasek JJ. TGF-β1 promotes the morphological and functional differentiation of the myofibroblast. Exp Cell Res. 2000;257(1):180–189. doi: 10.1006/excr.2000.4869. [DOI] [PubMed] [Google Scholar]
- 92.Wallace K, Burt AD, Wright MC. Liver fibrosis. Biochem J. 2008;411(1):1–18. doi: 10.1042/BJ20071570. [DOI] [PubMed] [Google Scholar]
- 93.Grande MT, Lopez-Novoa JM. Fibroblast activation and myofibroblast generation in obstructive nephropathy. Nat Rev Nephrol. 2009;5(6):319–328. doi: 10.1038/nrneph.2009.74. [DOI] [PubMed] [Google Scholar]
- 94.Guarino M, Tosoni A, Nebuloni M. Direct contribution of epithelium to organ fibrosis: epithelial-mesenchymal transition. Hum Pathol. 2009;40(10):1365–1376. doi: 10.1016/j.humpath.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 95.Yazhou C, Wenlv S, Weidong Z, Licun W. Clinicopathological significance of stromal myofibroblasts in invasive ductal carcinoma of the breast. Tumour Biol. 2004;25(5–6):290–295. doi: 10.1159/000081394. [DOI] [PubMed] [Google Scholar]
- 96.Masszi A, Di Ciano C, Sirokmany G, Arthur WT, Rotstein OD, Wang J, et al. Central role for Rho in TGF-β1-induced α-smooth muscle actin expression during epithelial-mesenchymal transition. Am J Physiol Renal Physiol. 2003;284(5):F911–F924. doi: 10.1152/ajprenal.00183.2002. [DOI] [PubMed] [Google Scholar]
- 97.Akhmetshina A, Dees C, Pileckyte M, Szucs G, Spriewald BM, Zwerina J, et al. Rho-associated kinases are crucial for myofibroblast differentiation and production of extracellular matrix in scleroderma fibroblasts. Arthritis Rheum. 2008;58(8):2553–2564. doi: 10.1002/art.23677. [DOI] [PubMed] [Google Scholar]
- 98.Vardouli L, Vasilaki E, Papadimitriou E, Kardassis D, Stournaras C. A novel mechanism of TGF-β-induced actin reorganization mediated by Smad proteins and Rho GTPases. FEBS J. 2008;275(16):4074–4087. doi: 10.1111/j.1742-4658.2008.06549.x. [DOI] [PubMed] [Google Scholar]
- 99.Vasilaki E, Papadimitriou E, Tajadura V, Ridley AJ, Stournaras C, Kardassis D. Transcriptional regulation of the small GTPase RhoB gene by TGF-β-induced signaling pathways. FASEN J. 2010;24(3):891–905. doi: 10.1096/fj.09-134742. [DOI] [PubMed] [Google Scholar]
- 100.Kim KK, Wei Y, Szekeres C, Kugler MC, Wolters PJ, Hill ML, et al. Epithelial cell α3β1 integrin links β-catenin and Smad signaling to promote myofibroblast formation and pulmonary fibrosis. J Clin Invest. 2009;119(1):213–224. doi: 10.1172/JCI36940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kim Y, Kugler MC, Wei Y, Kim KK, Li X, Brumwell AN, et al. Integrin α3β1-dependent β-catenin phosphorylation links epithelial Smad signaling to cell contacts. J Cell Biol. 2009;184(2):309–322. doi: 10.1083/jcb.200806067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.White LR, Blanchette JB, Ren L, Awn A, Trpkov K, Muruve DA. The characterization of α5-integrin expression on tubular epithelium during renal injury. Am J Physiol Renal Physiol. 2007;292(2):F567–F576. doi: 10.1152/ajprenal.00212.2006. [DOI] [PubMed] [Google Scholar]
- 103.Boyd NF, Dite GS, Stone J, Gunasekara A, English DR, McCredie MR, et al. Heritability of mammographic density, a risk factor for breast cancer. N Engl J Med. 2002;347(12):886–394. doi: 10.1056/NEJMoa013390. [DOI] [PubMed] [Google Scholar]
- 104.Boyd NF, Rommens JM, Vogt K, Lee V, Hopper JL, Yaffe MJ, et al. Mammographic breast density as an intermediate phenotype for breast cancer. Lancet Oncol. 2005;6(10):798–808. doi: 10.1016/S1470-2045(05)70390-9. [DOI] [PubMed] [Google Scholar]
- 105.Choi YW, Munden RF, Erasmus JJ, Park KJ, Chung WK, Jeon SC, et al. Effects of radiation therapy on the lung: radiologic appearances and differential diagnosis. Radiographics. 2004;24(4):985–997. doi: 10.1148/rg.244035160. [DOI] [PubMed] [Google Scholar]
- 106.Andarawewa KL, Erickson AC, Chou WS, Costes SV, Gascard P, Mott JD, et al. Ionizing radiation predisposes nonmalignant human mammary epithelial cells to undergo TGF-β induced epithelial to mesenchymal transition. Cancer Res. 2007;67(18):8662–8670. doi: 10.1158/0008-5472.CAN-07-1294. [DOI] [PubMed] [Google Scholar]
- 107.Butcher DT, Alliston T, Weaver VM. A tense situation: forcing tumour progression. Nat Rev Cancer. 2009;9(2):108–122. doi: 10.1038/nrc2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Paszek MJ, Zahir N, Johnson KR, Lakins JN, Rozenberg GI, Gefen A, et al. Tensional homeostasis and the malignant phenotype. Cancer Cell. 2005;8(3):241–254. doi: 10.1016/j.ccr.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 109.Turley EA, Veiseh M, Radisky DC, Bissell MJ. Mechanisms of disease: epithelial-mesenchymal transition--does cellular plasticity fuel neoplastic progression? Nat Clin Pract Oncol. 2008;5(5):280–290. doi: 10.1038/ncponc1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tian M, Schiemann WP. The TGF-β paradox in human cancer: an update. Future Oncol. 2009;5(2):259–271. doi: 10.2217/14796694.5.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;139(5):891–906. doi: 10.1016/j.cell.2009.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Frank NY, Schatton T, Frank MH. The therapeutic promise of the cancer stem cell concept. J Clin Invest. 2010;120(1):41–50. doi: 10.1172/JCI41004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Brown KA, Pietenpol JA, Moses HL. A tale of two proteins: differential roles and regulation of Smad2 and Smad3 in TGF-β signaling. J Cell Biochem. 2007;101(1):9–33. doi: 10.1002/jcb.21255. [DOI] [PubMed] [Google Scholar]
- 114.Hoot KE, Lighthall J, Han G, Lu SL, Li A, Ju W, et al. Keratinocyte-specific Smad2 ablation results in increased epithelial-mesenchymal transition during skin cancer formation and progression. J Clin Invest. 2008;118(8):2722–2732. doi: 10.1172/JCI33713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ju W, Ogawa A, Heyer J, Nierhof D, Yu L, Kucherlapati R, et al. Deletion of Smad2 in mouse liver reveals novel functions in hepatocyte growth and differentiation. Mol Cell Biol. 2006;26(2):654–667. doi: 10.1128/MCB.26.2.654-667.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Oft M, Akhurst RJ, Balmain A. Metastasis is driven by sequential elevation of H-Ras and Smad2 levels. Nat Cell Biol. 2002;4(7):487–494. doi: 10.1038/ncb807. [DOI] [PubMed] [Google Scholar]
- 117.Runyan CE, Hayashida T, Hubchak S, Curley JF, Schnaper HW. Role of SARA (SMAD anchor for receptor activation) in maintenance of epithelial cell phenotype. J Biol Chem. 2009;284(37):25181–25189. doi: 10.1074/jbc.M109.032847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Saika S, Kono-Saika S, Ohnishi Y, Sato M, Muragaki Y, Ooshima A, et al. Smad3 signaling is required for epithelial-mesenchymal transition of lens epithelium after injury. Am J Pathol. 2004;164(2):651–663. doi: 10.1016/S0002-9440(10)63153-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sato M, Muragaki Y, Saika S, Roberts AB, Ooshima A. Targeted disruption of TGF-β1/Smad3 signaling protects against renal tubulointerstitial fibrosis induced by unilateral ureteral obstruction. J Clin Invest. 2003;112(10):1486–1494. doi: 10.1172/JCI19270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ashcroft GS, Yang X, Glick AB, Weinstein M, Letterio JL, Mizel DE, et al. Mice lacking Smad3 show accelerated wound healing and an impaired local inflammatory response. Nat Cell Biol. 1999;1(5):260–266. doi: 10.1038/12971. [DOI] [PubMed] [Google Scholar]
- 121.Davies M, Robinson M, Smith E, Huntley S, Prime S, Paterson I. Induction of an epithelial to mesenchymal transition in human immortal and malignant keratinocytes by TGF-β1 involves MAPK, Smad and AP-1 signalling pathways. J Cell Biochem. 2005;95(5):918–931. doi: 10.1002/jcb.20458. [DOI] [PubMed] [Google Scholar]
- 122.Bardeesy N, Cheng KH, Berger JH, Chu GC, Pahler J, Olson P, et al. Smad4 is dispensable for normal pancreas development yet critical in progression and tumor biology of pancreas cancer. Genes Dev. 2006;20(22):3130–3146. doi: 10.1101/gad.1478706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Valcourt U, Kowanetz M, Niimi H, Heldin CH, Moustakas A. TGF-β and the Smad signaling pathway support transcriptomic reprogramming during epithelial-mesenchymal cell transition. Mol Biol Cell. 2005;16(4):1987–2002. doi: 10.1091/mbc.E04-08-0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Dooley S, Hamzavi J, Ciuclan L, Godoy P, Ilkavets I, Ehnert S, et al. Hepatocyte-specific Smad7 expression attenuates TGF-β-mediated fibrogenesis and protects against liver damage. Gastroenterology. 2008;135(2):642–659. doi: 10.1053/j.gastro.2008.04.038. [DOI] [PubMed] [Google Scholar]
- 125.Saika S, Ikeda K, Yamanaka O, Sato M, Muragaki Y, Ohnishi Y, et al. Transient adenoviral gene transfer of Smad7 prevents injury-induced epithelial-mesenchymal transition of lens epithelium in mice. Lab Invest. 2004;84(10):1259–1270. doi: 10.1038/labinvest.3700151. [DOI] [PubMed] [Google Scholar]
- 126.Gal A, Sjoblom T, Fedorova L, Imreh S, Beug H, Moustakas A. Sustained TGF-β exposure suppresses Smad and non-Smad signalling in mammary epithelial cells, leading to EMT and inhibition of growth arrest and apoptosis. Oncogene. 2008;27(9):1218–1230. doi: 10.1038/sj.onc.1210741. [DOI] [PubMed] [Google Scholar]
- 127.Deckers M, van Dinther M, Buijs J, Que I, Lowik C, van der Pluijm G, et al. The tumor suppressor Smad4 is required for TGF-β-induced epithelial to mesenchymal transition and bone metastasis of breast cancer cells. Cancer Res. 2006;66(4):2202–2209. doi: 10.1158/0008-5472.CAN-05-3560. [DOI] [PubMed] [Google Scholar]
- 128.Zhao BM, Hoffmann FM. Inhibition of TGF-β1-induced signaling and epithelial-to-mesenchymal transition by the Smad-binding peptide aptamer Trx-SARA. Mol Biol Cell. 2006;17(9):3819–3831. doi: 10.1091/mbc.E05-10-0990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Papageorgis P, Lambert AW, Ozturk S, Gao F, Pan H, Manne U, et al. Smad signaling is required to maintain epigenetic silencing during breast cancer progression. Cancer Res. 2010;70(3):968–978. doi: 10.1158/0008-5472.CAN-09-1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Liu IM, Schilling SH, Knouse KA, Choy L, Derynck R, Wang XF. TGF-β-stimulated Smad1/5 phosphorylation requires the ALK5 L45 loop and mediates the pro-migratory TGF-β switch. EMBO J. 2009;28(2):88–98. doi: 10.1038/emboj.2008.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hall A. Rho GTPases and the control of cell behaviour. Biochem Soc Trans. 2005;33(Pt 5):891–895. doi: 10.1042/BST20050891. [DOI] [PubMed] [Google Scholar]
- 132.Hall A, Nobes CD. Rho GTPases: molecular switches that control the organization and dynamics of the actin cytoskeleton. Philos Trans R Soc Lond B Biol Sci. 2000;355(1399):965–970. doi: 10.1098/rstb.2000.0632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Takaishi K, Sasaki T, Kotani H, Nishioka H, Takai Y. Regulation of cell-cell adhesion by Rac and Rho small G proteins in MDCK cells. J Cell Biol. 1997;139(4):1047–1059. doi: 10.1083/jcb.139.4.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sander EE, ten Klooster JP, van Delft S, van der Kammen RA, Collard JG. Rac downregulates Rho activity: reciprocal balance between both GTPases determines cellular morphology and migratory behavior. J Cell Biol. 1999;147(5):1009–1022. doi: 10.1083/jcb.147.5.1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mythreye K, Blobe GC. The type III TGF-β receptor regulates epithelial and cancer cell migration through β-arrestin2-mediated activation of Cdc42. Proc Natl Acad Sci USA. 2009;106(20):8221–8226. doi: 10.1073/pnas.0812879106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Simpson KJ, Dugan AS, Mercurio AM. Functional analysis of the contribution of RhoA and RhoC GTPases to invasive breast carcinoma. Cancer Res. 2004;64(23):8694–8701. doi: 10.1158/0008-5472.CAN-04-2247. [DOI] [PubMed] [Google Scholar]
- 137.Sequeira L, Dubyk CW, Riesenberger TA, Cooper CR, van Golen KL. Rho GTPases in PC-3 prostate cancer cell morphology, invasion and tumor cell diapedesis. Clin Exp Metastasis. 2008;25(5):569–579. doi: 10.1007/s10585-008-9173-3. [DOI] [PubMed] [Google Scholar]
- 138.Bellovin DI, Simpson KJ, Danilov T, Maynard E, Rimm DL, Oettgen P, et al. Reciprocal regulation of RhoA and RhoC characterizes the EMT and identifies RhoC as a prognostic marker of colon carcinoma. Oncogene. 2006;25(52):6959–6967. doi: 10.1038/sj.onc.1209682. [DOI] [PubMed] [Google Scholar]
- 139.Hutchison N, Hendry BM, Sharpe CC. Rho isoforms have distinct and specific functions in the process of epithelial to mesenchymal transition in renal proximal tubular cells. Cell Signal. 2009;21(10):1522–1531. doi: 10.1016/j.cellsig.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 140.Viloria-Petit AM, David L, Jia JY, Erdemir T, Bane AL, Pinnaduwage D, et al. A role for the TGF-β-Par6 polarity pathway in breast cancer progression. Proc Natl Acad Sci USA. 2009;106(33):14028–14033. doi: 10.1073/pnas.0906796106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ozdamar B, Bose R, Barrios-Rodiles M, Wang HR, Zhang Y, Wrana JL. Regulation of the polarity protein Par6 by TGF-β receptors controls epithelial cell plasticity. Science. 2005;307(5715):1603–1609. doi: 10.1126/science.1105718. [DOI] [PubMed] [Google Scholar]
- 142.Kong W, Yang H, He L, Zhao JJ, Coppola D, Dalton WS, et al. MicroRNA-155 is regulated by the TGF-β/Smad pathway and contributes to epithelial cell plasticity by targeting RhoA. Mol Cell Biol. 2008;28(22):6773–6784. doi: 10.1128/MCB.00941-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Valastyan S, Benaich N, Chang A, Reinhardt F, Weinberg RA. Concomitant suppression of three target genes can explain the impact of a microRNA on metastasis. Genes Dev. 2009;23(22):2592–2597. doi: 10.1101/gad.1832709. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 144.Valastyan S, Reinhardt F, Benaich N, Calogrias D, Szasz AM, Wang ZC, et al. A pleiotropically acting microRNA, miR-31, inhibits breast cancer metastasis. Cell. 2009;137(6):1032–1046. doi: 10.1016/j.cell.2009.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 145.Engelman JA. Targeting PI3K signalling in cancer: opportunities, challenges and limitations. Nat Rev Cancer. 2009;9(8):550–562. doi: 10.1038/nrc2664. [DOI] [PubMed] [Google Scholar]
- 146.Murillo MM, del Castillo G, Sanchez A, Fernandez M, Fabregat I. Involvement of EGF receptor and c-Src in the survival signals induced by TGF-β1 in hepatocytes. Oncogene. 2005;24(28):4580–4587. doi: 10.1038/sj.onc.1208664. [DOI] [PubMed] [Google Scholar]
- 147.Jechlinger M, Sommer A, Moriggl R, Seither P, Kraut N, Capodiecci P, et al. Autocrine PDGFR signaling promotes mammary cancer metastasis. J Clin Invest. 2006;116(6):1561–1570. doi: 10.1172/JCI24652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Uttamsingh S, Bao X, Nguyen KT, Bhanot M, Gong J, Chan JL, et al. Synergistic effect between EGF and TGF-β1 in inducing oncogenic properties of intestinal epithelial cells. Oncogene. 2008;27(18):2626–2634. doi: 10.1038/sj.onc.1210915. [DOI] [PubMed] [Google Scholar]
- 149.Karin M. NF-κB in cancer development and progression. Nature. 2006;441(7092):431–436. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 150.Sovak MA, Arsura M, Zanieski G, Kavanagh KT, Sonenshein GE. The inhibitory effects of TGF-β1 on breast cancer cell proliferation are mediated through regulation of aberrant NF-κB/Rel expression. Cell Growth Differ. 1999;10(8):537–544. [PubMed] [Google Scholar]
- 151.Arsura M, Wu M, Sonenshein GE. TGF-β1 inhibits NF-κB/Rel activity inducing apoptosis of B cells: transcriptional activation of IκBα. Immunity. 1996;5(1):31–40. doi: 10.1016/s1074-7613(00)80307-6. [DOI] [PubMed] [Google Scholar]
- 152.You HJ, How T, Blobe GC. The type III TGF-β receptor negatively regulates NF-κB signaling through its interaction with β-arrestin2. Carcinogenesis. 2009;30(8):1281–1287. doi: 10.1093/carcin/bgp071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Neil JR, Tian M, Schiemann WP. xIAP and its E3 ligase activity promote TGF-β-mediated NF-κB activation during breast cancer progression. J Biol Chem. 2009;284(32):21209–21217. doi: 10.1074/jbc.M109.018374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Chua HL, Bhat-Nakshatri P, Clare SE, Morimiya A, Badve S, Nakshatri H. NF-κB represses E-cadherin expression and enhances epithelial to mesenchymal transition of mammary epithelial cells: potential involvement of ZEB-1 and ZEB-2. Oncogene. 2007;26(5):711–724. doi: 10.1038/sj.onc.1209808. [DOI] [PubMed] [Google Scholar]
- 155.Huber MA, Azoitei N, Baumann B, Grunert S, Sommer A, Pehamberger H, et al. NF-κB is essential for epithelial-mesenchymal transition and metastasis in a model of breast cancer progression. J Clin Invest. 2004;114(4):569–581. doi: 10.1172/JCI21358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bertran E, Caja L, Navarro E, Sancho P, Mainez J, Murillo MM, et al. Role of CXCR4/SDF-1α in the migratory phenotype of hepatoma cells that have undergone epithelial-mesenchymal transition in response to the TGF-β. Cell Signal. 2009;21(11):1595–1606. doi: 10.1016/j.cellsig.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 157.Bhowmick NA, Zent R, Ghiassi M, McDonnell M, Moses HL. Integrin β1 signaling is necessary for TGF-β activation of p38MAPK and epithelial plasticity. J Biol Chem. 2001;276(50):46707–46713. doi: 10.1074/jbc.M106176200. [DOI] [PubMed] [Google Scholar]
- 158.Xie L, Law BK, Chytil AM, Brown KA, Aakre ME, Moses HL. Activation of the Erk pathway is required for TGF-β1-induced EMT in vitro. Neoplasia. 2004;6(5):603–610. doi: 10.1593/neo.04241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Atfi A, Djelloul S, Chastre E, Davis R, Gespach C. Evidence for a role of Rho-like GTPases and stress-activated protein kinase/c-Jun N-terminal kinase (SAPK/JNK) in TGF-β-mediated signaling. J. Biol. Chem. 1997;272(3):1429–1432. doi: 10.1074/jbc.272.3.1429. [DOI] [PubMed] [Google Scholar]
- 160.Hocevar BA, Prunier C, Howe PH. Disabled-2 (Dab2) mediates TGF-β-stimulated fibronectin synthesis through TGF-β-activated kinase 1 and activation of the JNK pathway. J Biol Chem. 2005;280(27):25920–25927. doi: 10.1074/jbc.M501150200. [DOI] [PubMed] [Google Scholar]
- 161.Santibanez JF. JNK mediates TGF-β1-induced epithelial mesenchymal transdifferentiation of mouse transformed keratinocytes. FEBS Lett. 2006;580(22):5385–5391. doi: 10.1016/j.febslet.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 162.Shintani Y, Wheelock MJ, Johnson KR. Phosphoinositide-3 kinase-Rac1-c-Jun NH2-terminal kinase signaling mediates collagen I-induced cell scattering and up-regulation of N-cadherin expression in mouse mammary epithelial cells. Mol Biol Cell. 2006;17(7):2963–2975. doi: 10.1091/mbc.E05-12-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Shintani Y, Hollingsworth MA, Wheelock MJ, Johnson KR. Collagen I promotes metastasis in pancreatic cancer by activating c-Jun NH(2)-terminal kinase 1 and up-regulating N-cadherin expression. Cancer Res. 2006;66(24):11745–11753. doi: 10.1158/0008-5472.CAN-06-2322. [DOI] [PubMed] [Google Scholar]
- 164.Zuo W, Chen YG. Specific activation of mitogen-activated protein kinase by TGF-β receptors in lipid rafts is required for epithelial cell plasticity. Mol Biol Cell. 2009;20(3):1020–1029. doi: 10.1091/mbc.E08-09-0898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Dedhar S, Williams B, Hannigan G. Integrin-linked kinase (ILK): a regulator of integrin and growth-factor signalling. Trends Cell Biol. 1999;9(8):319–323. doi: 10.1016/s0962-8924(99)01612-8. [DOI] [PubMed] [Google Scholar]
- 166.Hannigan G, Troussard AA, Dedhar S. Integrin-linked kinase: a cancer therapeutic target unique among its ILK. Nat Rev Cancer. 2005;5(1):51–63. doi: 10.1038/nrc1524. [DOI] [PubMed] [Google Scholar]
- 167.Hehlgans S, Haase M, Cordes N. Signalling via integrins: implications for cell survival and anticancer strategies. Biochim Biophys Acta. 2007;1775(1):163–180. doi: 10.1016/j.bbcan.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 168.Somasiri A, Howarth A, Goswami D, Dedhar S, Roskelley CD. Overexpression of the integrin-linked kinase mesenchymally transforms mammary epithelial cells. J Cell Sci. 2001;114(Pt 6):1125–1136. doi: 10.1242/jcs.114.6.1125. [DOI] [PubMed] [Google Scholar]
- 169.White DE, Cardiff RD, Dedhar S, Muller WJ. Mammary epithelial-specific expression of the integrin-linked kinase (ILK) results in the induction of mammary gland hyperplasias and tumors in transgenic mice. Oncogene. 2001;20(48):7064–7072. doi: 10.1038/sj.onc.1204910. [DOI] [PubMed] [Google Scholar]
- 170.Lin SW, Ke FC, Hsiao PW, Lee PP, Lee MT, Hwang JJ. Critical involvement of ILK in TGFbeta1-stimulated invasion/migration of human ovarian cancer cells is associated with urokinase plasminogen activator system. Exp Cell Res. 2007;313(3):602–613. doi: 10.1016/j.yexcr.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 171.Li Y, Dai C, Wu C, Liu Y. PINCH-1 promotes tubular epithelial-to-mesenchymal transition by interacting with integrin-linked kinase. J Am Soc Nephrol. 2007;18(9):2534–2543. doi: 10.1681/ASN.2007030315. [DOI] [PubMed] [Google Scholar]
- 172.Hood JD, Cheresh DA. Role of integrins in cell invasion and migration. Nat Rev Cancer. 2002;2(2):91–100. doi: 10.1038/nrc727. [DOI] [PubMed] [Google Scholar]
- 173.Mizejewski GJ. Role of integrins in cancer: survey of expression patterns. Proc Soc Exp Biol Med. 1999;222(2):124–138. doi: 10.1177/153537029922200203. [DOI] [PubMed] [Google Scholar]
- 174.Desgrosellier JS, Cheresh DA. Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer. 2010;10(1):9–22. doi: 10.1038/nrc2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Legate KR, Wickstrom SA, Fassler R. Genetic and cell biological analysis of integrin outside-in signaling. Genes Dev. 2009;23(4):397–418. doi: 10.1101/gad.1758709. [DOI] [PubMed] [Google Scholar]
- 176.Hauck CR, Sieg DJ, Hsia DA, Loftus JC, Gaarde WA, Monia BP, et al. Inhibition of focal adhesion kinase expression or activity disrupts epidermal growth factor-stimulated signaling promoting the migration of invasive human carcinoma cells. Cancer Res. 2001;61(19):7079–7090. [PubMed] [Google Scholar]
- 177.Sieg DJ, Hauck CR, Ilic D, Klingbeil CK, Schaefer E, Damsky CH, et al. FAK integrates growth-factor and integrin signals to promote cell migration. Nat Cell Biol. 2000;2(5):249–256. doi: 10.1038/35010517. [DOI] [PubMed] [Google Scholar]
- 178.Munger JS, Huang X, Kawakatsu H, Griffiths MJ, Dalton SL, Wu J, et al. The integrin αvβ6 binds and activates latent TGF-β1: a mechanism for regulating pulmonary inflammation and fibrosis. Cell. 1999;96(3):319–328. doi: 10.1016/s0092-8674(00)80545-0. [DOI] [PubMed] [Google Scholar]
- 179.Mu D, Cambier S, Fjellbirkeland L, Baron JL, Munger JS, Kawakatsu H, et al. The integrin αvβ8 mediates epithelial homeostasis through MT1-MMP-dependent activation of TGF-β1. J Cell Biol. 2002;157(3):493–507. doi: 10.1083/jcb.200109100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Wendt MK, Schiemann WP. Therapeutic targeting of the focal adhesion complex prevents oncogenic TGF-β signaling and metastasis. Breast Cancer Res. 2009;11(5):R68. doi: 10.1186/bcr2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Bandyopadhyay A, Agyin JK, Wang L, Tang Y, Lei X, Story BM, et al. Inhibition of pulmonary and skeletal metastasis by a TGF-β type I receptor kinase inhibitor. Cancer Res. 2006;66(13):6714–6721. doi: 10.1158/0008-5472.CAN-05-3565. [DOI] [PubMed] [Google Scholar]
- 182.Sloan EK, Pouliot N, Stanley KL, Chia J, Moseley JM, Hards DK, et al. Tumor-specific expression of αvβ3 integrin promotes spontaneous metastasis of breast cancer to bone. Breast Cancer Res. 2006;8(2):R20. doi: 10.1186/bcr1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Cicchini C, Laudadio I, Citarella F, Corazzari M, Steindler C, Conigliaro A, et al. TGF-β-induced EMT requires focal adhesion kinase (FAK) signaling. Exp Cell Res. 2008;314(1):143–152. doi: 10.1016/j.yexcr.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 184.Liu S, Xu SW, Kennedy L, Pala D, Chen Y, Eastwood M, et al. FAK is required for TGF-β-induced JNK phosphorylation in fibroblasts: implications for acquisition of a matrix-remodeling phenotype. Mol Biol Cell. 2007;18(6):2169–2178. doi: 10.1091/mbc.E06-12-1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kim W, Seok Kang Y, Soo Kim J, Shin NY, Hanks SK, Song WK. The integrin-coupled signaling adaptor p130Cas suppresses Smad3 function in TGF-β signaling. Mol Biol Cell. 2008;19(5):2135–2146. doi: 10.1091/mbc.E07-10-0991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.van der Flier S, Chan CM, Brinkman A, Smid M, Johnston SR, Dorssers LC, et al. BCAR1/p130Cas expression in untreated and acquired tamoxifen-resistant human breast carcinomas. Int J Cancer. 2000;89(5):465–468. doi: 10.1002/1097-0215(20000920)89:5<465::aid-ijc11>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 187.Ta HQ, Thomas KS, Schrecengost RS, Bouton AH. A novel association between p130Cas and resistance to the chemotherapeutic drug adriamycin in human breast cancer cells. Cancer Res. 2008;68(21):8796–8804. doi: 10.1158/0008-5472.CAN-08-2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Cabodi S, Tinnirello A, Di Stefano P, Bisaro B, Ambrosino E, Castellano I, et al. p130Cas as a new regulator of mammary epithelial cell proliferation, survival, and HER2-neu oncogene-dependent breast tumorigenesis. Cancer Res. 2006;66(9):4672–4680. doi: 10.1158/0008-5472.CAN-05-2909. [DOI] [PubMed] [Google Scholar]
- 189.Wendt MK, Smith JA, Schiemann WP. p130Cas is required for mammary tumor growth and TGF-β-mediated metastasis through regulation of Smad2/3 activity. J Biol Chem. 2009;284(49):34145–34156. doi: 10.1074/jbc.M109.023614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Tumbarello DA, Brown MC, Hetey SE, Turner CE. Regulation of paxillin family members during epithelial-mesenchymal transformation: a putative role for paxillin delta. J Cell Sci. 2005;118(Pt 20):4849–4863. doi: 10.1242/jcs.02615. [DOI] [PubMed] [Google Scholar]
- 191.Fujimoto N, Yeh S, Kang HY, Inui S, Chang HC, Mizokami A, et al. Cloning and characterization of androgen receptor coactivator, ARA55, in human prostate. J Biol Chem. 1999;274(12):8316–8321. doi: 10.1074/jbc.274.12.8316. [DOI] [PubMed] [Google Scholar]
- 192.Tumbarello DA, Turner CE. Hic-5 contributes to epithelial-mesenchymal transformation through a RhoA/ROCK-dependent pathway. J Cell Physiol. 2007;211(3):736–747. doi: 10.1002/jcp.20991. [DOI] [PubMed] [Google Scholar]
- 193.Wang H, Song K, Krebs TL, Yang J, Danielpour D. Smad7 is inactivated through a direct physical interaction with the LIM protein Hic-5/ARA55. Oncogene. 2008;27(54):6791–6805. doi: 10.1038/onc.2008.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Wang H, Song K, Sponseller TL, Danielpour D. Novel function of androgen receptor-associated protein 55/Hic-5 as a negative regulator of Smad3 signaling. J Biol Chem. 2005;280(7):5154–5162. doi: 10.1074/jbc.M411575200. [DOI] [PubMed] [Google Scholar]
- 195.Prunier C, Hocevar BA, Howe PH. Wnt signaling: physiology and pathology. Growth Factors. 2004;22(3):141–150. doi: 10.1080/08977190410001720860. [DOI] [PubMed] [Google Scholar]
- 196.Prunier C, Howe PH. Disabled-2 (Dab2) is required for TGF-β-induced epithelial to mesenchymal transition (EMT) J Biol Chem. 2005;280(17):17540–17548. doi: 10.1074/jbc.M500974200. [DOI] [PubMed] [Google Scholar]
- 197.Chaudhury A, Hussey GS, Ray PS, Jin G, Fox PL, Howe PH. TGF-β-mediated phosphorylation of hnRNP E1 induces EMT via transcript-selective translational induction of Dab2 and ILEI. Nat Cell Biol. 2010;12(3):286–293. doi: 10.1038/ncb2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Moreno-Bueno G, Portillo F, Cano A. Transcriptional regulation of cell polarity in EMT and cancer. Oncogene. 2008;27(55):6958–6969. doi: 10.1038/onc.2008.346. [DOI] [PubMed] [Google Scholar]
- 199.Peinado H, Olmeda D, Cano A. Snail, Zeb and bHLH factors in tumour progression: an alliance against the epithelial phenotype? Nat Rev Cancer. 2007;7(6):415–428. doi: 10.1038/nrc2131. [DOI] [PubMed] [Google Scholar]
- 200.Ikenouchi J, Matsuda M, Furuse M, Tsukita S. Regulation of tight junctions during the epithelium-mesenchyme transition: direct repression of the gene expression of claudins/occludin by Snail. J Cell Sci. 2003;116(Pt 10):1959–1967. doi: 10.1242/jcs.00389. [DOI] [PubMed] [Google Scholar]
- 201.Vincent T, Neve EP, Johnson JR, Kukalev A, Rojo F, Albanell J, et al. A SNAIL1-SMAD3/4 transcriptional repressor complex promotes TGF-β mediated epithelial-mesenchymal transition. Nat Cell Biol. 2009;11(8):943–950. doi: 10.1038/ncb1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Smith AP, Verrecchia A, Faga G, Doni M, Perna D, Martinato F, et al. A positive role for Myc in TGF-β-induced Snail transcription and epithelial-to-mesenchymal transition. Oncogene. 2009;28(3):422–430. doi: 10.1038/onc.2008.395. [DOI] [PubMed] [Google Scholar]
- 203.Lee YH, Albig AR, Regner M, Schiemann BJ, Schiemann WP. Fibulin-5 initiates epithelial-mesenchymal transition (EMT) and enhances EMT induced by TGF-β in mammary epithelial cells via a MMP-dependent mechanism. Carcinogenesis. 2008;29(12):2243–2251. doi: 10.1093/carcin/bgn199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Araki S, Eitel JA, Batuello CN, Bijangi-Vishehsaraei K, Xie XJ, Danielpour D, et al. TGF-β1-induced expression of human Mdm2 correlates with late-stage metastatic breast cancer. J Clin Invest. 2010;120(1):290–302. doi: 10.1172/JCI39194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Thuault S, Valcourt U, Petersen M, Manfioletti G, Heldin CH, Moustakas A. TGF-β employs HMGA2 to elicit epithelial-mesenchymal transition. J Cell Biol. 2006;174(2):175–183. doi: 10.1083/jcb.200512110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Yu M, Smolen GA, Zhang J, Wittner B, Schott BJ, Brachtel E, et al. A developmentally regulated inducer of EMT, LBX1, contributes to breast cancer progression. Genes Dev. 2009;23(15):1737–1742. doi: 10.1101/gad.1809309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Ali S, Coombes RC. Endocrine-responsive breast cancer and strategies for combating resistance. Nat Rev Cancer. 2002;2(2):101–112. doi: 10.1038/nrc721. [DOI] [PubMed] [Google Scholar]
- 208.Dhasarathy A, Kajita M, Wade PA. The transcription factor snail mediates epithelial to mesenchymal transitions by repression of estrogen receptor-alpha. Mol Endocrinol. 2007;21(12):2907–2918. doi: 10.1210/me.2007-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Fujita N, Jaye DL, Kajita M, Geigerman C, Moreno CS, Wade PA. MTA3, a Mi-2/NuRD complex subunit, regulates an invasive growth pathway in breast cancer. Cell. 2003;113(2):207–219. doi: 10.1016/s0092-8674(03)00234-4. [DOI] [PubMed] [Google Scholar]
- 210.Matsuda T, Yamamoto T, Muraguchi A, Saatcioglu F. Cross-talk between TGF-β and estrogen receptor signaling through Smad3. J Biol Chem. 2001;276(46):42908–42914. doi: 10.1074/jbc.M105316200. [DOI] [PubMed] [Google Scholar]
- 211.Radaelli E, Arnold A, Papanikolaou A, Garcia-Fernandez RA, Mattiello S, Scanziani E, et al. Mammary tumor phenotypes in wild-type aging female FVB/N mice with pituitary prolactinomas. Vet Pathol. 2009;46(4):736–745. doi: 10.1354/vp.08-VP-0280-R-FL. [DOI] [PubMed] [Google Scholar]
- 212.Iorio MV, Ferracin M, Liu CG, Veronese A, Spizzo R, Sabbioni S, et al. MicroRNA gene expression deregulation in human breast cancer. Cancer Res. 2005;65(16):7065–7070. doi: 10.1158/0008-5472.CAN-05-1783. [DOI] [PubMed] [Google Scholar]
- 213.Calin GA, Croce CM. MicroRNA signatures in human cancers. Nat Rev Cancer. 2006;6(11):857–866. doi: 10.1038/nrc1997. [DOI] [PubMed] [Google Scholar]
- 214.Silveri L, Tilly G, Vilotte JL, Le Provost F. MicroRNA involvement in mammary gland development and breast cancer. Reprod Nutr Dev. 2006;46(5):549–556. doi: 10.1051/rnd:2006026. [DOI] [PubMed] [Google Scholar]
- 215.Park SM, Gaur AB, Lengyel E, Peter ME. The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev. 2008;22(7):894–907. doi: 10.1101/gad.1640608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G, et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol. 2008;10(5):593–601. doi: 10.1038/ncb1722. [DOI] [PubMed] [Google Scholar]
- 217.Korpal M, Lee ES, Hu G, Kang Y. The miR-200 family inhibits epithelial-mesenchymal transition and cancer cell migration by direct targeting of E-cadherin transcriptional repressors ZEB1 and ZEB2. J Biol Chem. 2008;283(22):14910–14914. doi: 10.1074/jbc.C800074200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Burk U, Schubert J, Wellner U, Schmalhofer O, Vincan E, Spaderna S, et al. A reciprocal repression between ZEB1 and members of the miR-200 family promotes EMT and invasion in cancer cells. EMBO Rep. 2008;9(6):582–589. doi: 10.1038/embor.2008.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Zavadil J, Narasimhan M, Blumenberg M, Schneider RJ. TGF-β and microRNA:mRNA regulatory networks in epithelial plasticity. Cells Tissues Organs. 2007;185(1–3):157–161. doi: 10.1159/000101316. [DOI] [PubMed] [Google Scholar]
- 220.Zhu S, Si ML, Wu H, Mo YY. MicroRNA-21 targets the tumor suppressor gene tropomyosin 1 (TPM1) J Biol Chem. 2007;282(19):14328–14336. doi: 10.1074/jbc.M611393200. [DOI] [PubMed] [Google Scholar]
- 221.Zhu S, Wu H, Wu F, Nie D, Sheng S, Mo YY. MicroRNA-21 targets tumor suppressor genes in invasion and metastasis. Cell Res. 2008;18(3):350–359. doi: 10.1038/cr.2008.24. [DOI] [PubMed] [Google Scholar]
- 222.Lombaerts M, van Wezel T, Philippo K, Dierssen JW, Zimmerman RM, Oosting J, et al. E-cadherin transcriptional downregulation by promoter methylation but not mutation is related to epithelial-to-mesenchymal transition in breast cancer cell lines. Br J Cancer. 2006;94(5):661–671. doi: 10.1038/sj.bjc.6602996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Yoshiura K, Kanai Y, Ochiai A, Shimoyama Y, Sugimura T, Hirohashi S. Silencing of the E-cadherin invasion-suppressor gene by CpG methylation in human carcinomas. Proc Natl Acad Sci USA. 1995;92(16):7416–7419. doi: 10.1073/pnas.92.16.7416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Herman JG, Baylin SB. Gene silencing in cancer in association with promoter hypermethylation. N Engl J Med. 2003;349(21):2042–2054. doi: 10.1056/NEJMra023075. [DOI] [PubMed] [Google Scholar]
- 225.Vrba L, Jensen TJ, Garbe JC, Heimark RL, Cress AE, Dickinson S, et al. Role for DNA methylation in the regulation of miR-200c and miR-141 expression in normal and cancer cells. PLoS One. 2010;5(1):e8697. doi: 10.1371/journal.pone.0008697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Dumont N, Wilson MB, Crawford YG, Reynolds PA, Sigaroudinia M, Tlsty TD. Sustained induction of epithelial to mesenchymal transition activates DNA methylation of genes silenced in basal-like breast cancers. Proc Natl Acad Sci. 2008;105(39):14867–14872. doi: 10.1073/pnas.0807146105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Bierie B, Moses HL. Tumour microenvironment: TGF-β: the molecular Jekyll and Hyde of cancer. Nat Rev Cancer. 2006;6(7):506–520. doi: 10.1038/nrc1926. [DOI] [PubMed] [Google Scholar]
- 228.Bissell MJ, Labarge MA. Context, tissue plasticity, and cancer: are tumor stem cells also regulated by the microenvironment? Cancer Cell. 2005;7(1):17–23. doi: 10.1016/j.ccr.2004.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Radisky DC, Bissell MJ. Cancer. Respect thy neighbor! Science. 2004;303(5659):775–777. doi: 10.1126/science.1094412. [DOI] [PubMed] [Google Scholar]
- 230.Massague J. TGFbeta in Cancer. Cell. 2008;134(2):215–230. doi: 10.1016/j.cell.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Cavallaro U, Christofori G. Cell adhesion and signalling by cadherins and Ig-CAMs in cancer. Nat Rev Cancer. 2004;4(2):118–132. doi: 10.1038/nrc1276. [DOI] [PubMed] [Google Scholar]
- 232.Agiostratidou G, Hulit J, Phillips GR, Hazan RB. Differential cadherin expression: potential markers for epithelial to mesenchymal transformation during tumor progression. J Mammary Gland Biol Neoplasia. 2007;12(2–3):127–133. doi: 10.1007/s10911-007-9044-6. [DOI] [PubMed] [Google Scholar]
- 233.Christofori G. Changing neighbours, changing behaviour: cell adhesion molecule-mediated signalling during tumour progression. EMBO J. 2003;22(10):2318–2323. doi: 10.1093/emboj/cdg228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Graff JR, Greenberg VE, Herman JG, Westra WH, Boghaert ER, Ain KB, et al. Distinct patterns of E-cadherin CpG island methylation in papillary, follicular, Hurthle's cell, and poorly differentiated human thyroid carcinoma. Cancer Res. 1998;58(10):2063–2066. [PubMed] [Google Scholar]
- 235.Makrilia N, Kollias A, Manolopoulos L, Syrigos K. Cell adhesion molecules: role and clinical significance in cancer. Cancer Invest. 2009;27(10):1023–1037. doi: 10.3109/07357900902769749. [DOI] [PubMed] [Google Scholar]
- 236.Gravdal K, Halvorsen OJ, Haukaas SA, Akslen LA. A switch from E-cadherin to N-cadherin expression indicates epithelial to mesenchymal transition and is of strong and independent importance for the progress of prostate cancer. Clin Cancer Res. 2007;13(23):7003–7011. doi: 10.1158/1078-0432.CCR-07-1263. [DOI] [PubMed] [Google Scholar]
- 237.Tomita K, van Bokhoven A, van Leenders GJ, Ruijter ET, Jansen CF, Bussemakers MJ, et al. Cadherin switching in human prostate cancer progression. Cancer Res. 2000;60(13):3650–3654. [PubMed] [Google Scholar]
- 238.Pyo SW, Hashimoto M, Kim YS, Kim CH, Lee SH, Johnson KR, et al. Expression of E-cadherin, P-cadherin and N-cadherin in oral squamous cell carcinoma: correlation with the clinicopathologic features and patient outcome. J Craniomaxillofac Surg. 2007;35(1):1–9. doi: 10.1016/j.jcms.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 239.Hazan RB, Phillips GR, Qiao RF, Norton L, Aaronson SA. Exogenous expression of N-cadherin in breast cancer cells induces cell migration, invasion, and metastasis. J Cell Biol. 2000;148(4):779–790. doi: 10.1083/jcb.148.4.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Cavallaro U, Niedermeyer J, Fuxa M, Christofori G. N-CAM modulates tumour-cell adhesion to matrix by inducing FGF-receptor signalling. Nat Cell Biol. 2001;3(7):650–657. doi: 10.1038/35083041. [DOI] [PubMed] [Google Scholar]
- 241.Lehembre F, Yilmaz M, Wicki A, Schomber T, Strittmatter K, Ziegler D, et al. NCAM-induced focal adhesion assembly: a functional switch upon loss of E-cadherin. EMBO J. 2008;27(19):2603–2615. doi: 10.1038/emboj.2008.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Illman SA, Lehti K, Keski-Oja J, Lohi J. Epilysin (MMP-28) induces TGF-β mediated epithelial to mesenchymal transition in lung carcinoma cells. J Cell Sci. 2006;119(Pt 18):3856–3865. doi: 10.1242/jcs.03157. [DOI] [PubMed] [Google Scholar]
- 243.Egeblad M, Werb Z. New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer. 2002;2(3):161–174. doi: 10.1038/nrc745. [DOI] [PubMed] [Google Scholar]
- 244.Mott JD, Werb Z. Regulation of matrix biology by matrix metalloproteinases. Curr Opin Cell Biol. 2004;16(5):558–564. doi: 10.1016/j.ceb.2004.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Yu Q, Stamenkovic I. Cell surface-localized matrix metalloproteinase-9 proteolytically activates TGF-beta and promotes tumor invasion and angiogenesis. Genes Dev. 2000;14(2):163–176. [PMC free article] [PubMed] [Google Scholar]
- 246.Dangelo M, Sarment DP, Billings PC, Pacifici M. Activation of TGF-β in chondrocytes undergoing endochondral ossification. J Bone Miner Res. 2001;16(12):2339–2347. doi: 10.1359/jbmr.2001.16.12.2339. [DOI] [PubMed] [Google Scholar]
- 247.Noe V, Fingleton B, Jacobs K, Crawford HC, Vermeulen S, Steelant W, et al. Release of an invasion promoter E-cadherin fragment by matrilysin and stromelysin-1. J Cell Sci. 2001;114(Pt 1):111–118. doi: 10.1242/jcs.114.1.111. [DOI] [PubMed] [Google Scholar]
- 248.Radisky DC, Levy DD, Littlepage LE, Liu H, Nelson CM, Fata JE, et al. Rac1b and reactive oxygen species mediate MMP-3-induced EMT and genomic instability. Nature. 2005;436(7047):123–127. doi: 10.1038/nature03688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Stuelten CH, DaCosta Byfield S, Arany PR, Karpova TS, Stetler-Stevenson WG, Roberts AB. Breast cancer cells induce stromal fibroblasts to express MMP-9 via secretion of TNF-α and TGF-β. J Cell Sci. 2005;118(Pt 10):2143–2153. doi: 10.1242/jcs.02334. [DOI] [PubMed] [Google Scholar]
- 250.Duivenvoorden WC, Hirte HW, Singh G. TGF-β1 acts as an inducer of matrix metalloproteinase expression and activity in human bone-metastasizing cancer cells. Clin Exp Metastasis. 1999;17(1):27–34. doi: 10.1023/a:1026404227624. [DOI] [PubMed] [Google Scholar]
- 251.Kim ES, Sohn YW, Moon A. TGF-β-induced transcriptional activation of MMP-2 is mediated by activating transcription factor (ATF)2 in human breast epithelial cells. Cancer Lett. 2007;252(1):147–156. doi: 10.1016/j.canlet.2006.12.016. [DOI] [PubMed] [Google Scholar]
- 252.Kim ES, Kim MS, Moon A. TGF-β in conjunction with H-Ras activation promotes malignant progression of MCF10A breast epithelial cells. Cytokine. 2005;29(2):84–91. doi: 10.1016/j.cyto.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 253.Harbeck N, Kates RE, Gauger K, Willems A, Kiechle M, Magdolen V, et al. Urokinase-type plasminogen activator (uPA) and its inhibitor PAI-I: novel tumor-derived factors with a high prognostic and predictive impact in breast cancer. Thromb Haemost. 2004;91(3):450–456. doi: 10.1160/TH03-12-0798. [DOI] [PubMed] [Google Scholar]
- 254.Duffy MJ, Duggan C. The urokinase plasminogen activator system: a rich source of tumour markers for the individualised management of patients with cancer. Clin Biochem. 2004;37(7):541–548. doi: 10.1016/j.clinbiochem.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 255.Mitra SK, Lim ST, Chi A, Schlaepfer DD. Intrinsic focal adhesion kinase activity controls orthotopic breast carcinoma metastasis via the regulation of urokinase plasminogen activator expression in a syngeneic tumor model. Oncogene. 2006;25(32):4429–4440. doi: 10.1038/sj.onc.1209482. [DOI] [PubMed] [Google Scholar]
- 256.Lester RD, Jo M, Montel V, Takimoto S, Gonias SL. uPAR induces epithelial-mesenchymal transition in hypoxic breast cancer cells. J Cell Biol. 2007;178(3):425–436. doi: 10.1083/jcb.200701092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Ge R, Rajeev V, Ray P, Lattime E, Rittling S, Medicherla S, et al. Inhibition of growth and metastasis of mouse mammary carcinoma by selective inhibitor of TGF-β type I receptor kinase in vivo. Clin Cancer Res. 2006;12(14 Pt 1):4315–4330. doi: 10.1158/1078-0432.CCR-06-0162. [DOI] [PubMed] [Google Scholar]
- 258.Nam JS, Terabe M, Mamura M, Kang MJ, Chae H, Stuelten C, et al. An anti-TGF-β antibody suppresses metastasis via cooperative effects on multiple cell compartments. Cancer Res. 2008;68(10):3835–3843. doi: 10.1158/0008-5472.CAN-08-0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Yang L, Huang J, Ren X, Gorska AE, Chytil A, Aakre M, et al. Abrogation of TGF-β signaling in mammary carcinomas recruits Gr-1+CD11b+ myeloid cells that promote metastasis. Cancer Cell. 2008;13(1):23–35. doi: 10.1016/j.ccr.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Zhang F, Tom CC, Kugler MC, Ching TT, Kreidberg JA, Wei Y, et al. Distinct ligand binding sites in integrin α3β1 regulate matrix adhesion and cell-cell contact. J Cell Biol. 2003;163(1):177–188. doi: 10.1083/jcb.200304065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Whitley BR, Palmieri D, Twerdi CD, Church FC. Expression of active plasminogen activator inhibitor-1 reduces cell migration and invasion in breast and gynecological cancer cells. Exp Cell Res. 2004;296(2):151–162. doi: 10.1016/j.yexcr.2004.02.022. [DOI] [PubMed] [Google Scholar]
- 262.Descotes F, Riche B, Saez S, De Laroche G, Datchary J, Roy P, et al. Plasminogen activator inhibitor type 1 is the most significant of the usual tissue prognostic factors in node-negative breast ductal adenocarcinoma independent of urokinase-type plasminogen activator. Clin Breast Cancer. 2008;8(2):168–177. doi: 10.3816/CBC.2008.n.018. [DOI] [PubMed] [Google Scholar]
- 263.Samarakoon R, Higgins CE, Higgins SP, Higgins PJ. Differential requirement for MEK/ERK and SMAD signaling in PAI-1 and CTGF expression in response to microtubule disruption. Cell Signal. 2009;21(6):986–995. doi: 10.1016/j.cellsig.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Ignotz RA, Massague J. TGF-β stimulates the expression of fibronectin and collagen and their incorporation into the extracellular matrix. J Biol Chem. 1986;261(9):4337–4345. [PubMed] [Google Scholar]
- 265.Wienke D, Davies GC, Johnson DA, Sturge J, Lambros MB, Savage K, et al. The collagen receptor Endo180 (CD280) Is expressed on basal-like breast tumor cells and promotes tumor growth in vivo. Cancer Res. 2007;67(21):10230–10240. doi: 10.1158/0008-5472.CAN-06-3496. [DOI] [PubMed] [Google Scholar]
- 266.Garamszegi N, Garamszegi SP, Samavarchi-Tehrani P, Walford E, Schneiderbauer MM, Wrana JL, et al. Extracellular matrix-induced TGF-β receptor signaling dynamics. Oncogene. 2010 doi: 10.1038/onc.2009.514. PMID: 20101206. [DOI] [PubMed] [Google Scholar]
- 267.Xie L, Law BK, Aakre ME, Edgerton M, Shyr Y, Bhowmick NA, et al. TGF-β-regulated gene expression in a mouse mammary gland epithelial cell line. Breast Cancer Res. 2003;5(6):R187–R198. doi: 10.1186/bcr640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Maschler S, Wirl G, Spring H, Bredow DV, Sordat I, Beug H, et al. Tumor cell invasiveness correlates with changes in integrin expression and localization. Oncogene. 2005;24(12):2032–2041. doi: 10.1038/sj.onc.1208423. [DOI] [PubMed] [Google Scholar]
- 269.Camara J, Jarai G. Epithelial-mesenchymal transition in primary human bronchial epithelial cells is Smad-dependent and enhanced by fibronectin and TNF-α. Fibrogenesis Tissue Repair. 2010;3(1):2. doi: 10.1186/1755-1536-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Wels J, Kaplan RN, Rafii S, Lyden D. Migratory neighbors and distant invaders: tumor-associated niche cells. Genes Dev. 2008;22(5):559–574. doi: 10.1101/gad.1636908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Erler JT, Bennewith KL, Cox TR, Lang G, Bird D, Koong A, et al. Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the premetastatic niche. Cancer Cell. 2009;15(1):35–44. doi: 10.1016/j.ccr.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Gupta PB, Onder TT, Jiang G, Tao K, Kuperwasser C, Weinberg RA, et al. Identification of selective inhibitors of cancer stem cells by high-throughput screening. Cell. 2009;138(4):645–659. doi: 10.1016/j.cell.2009.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]