Abstract
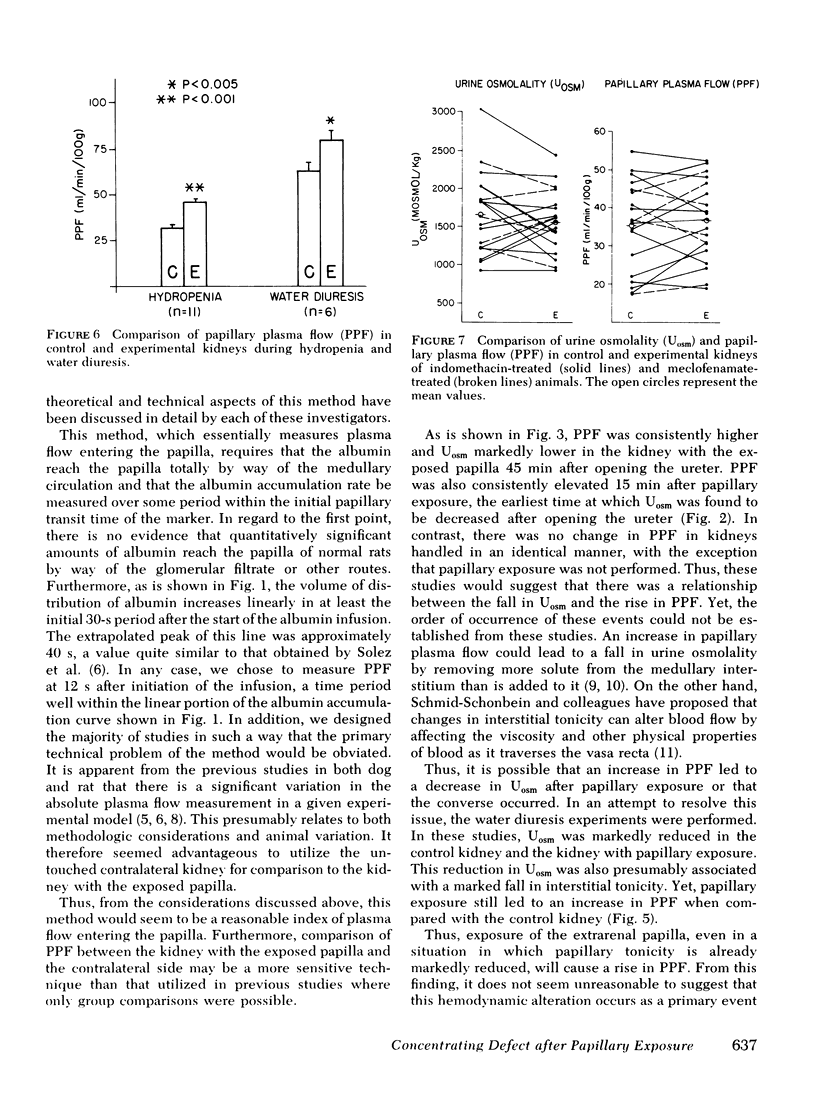
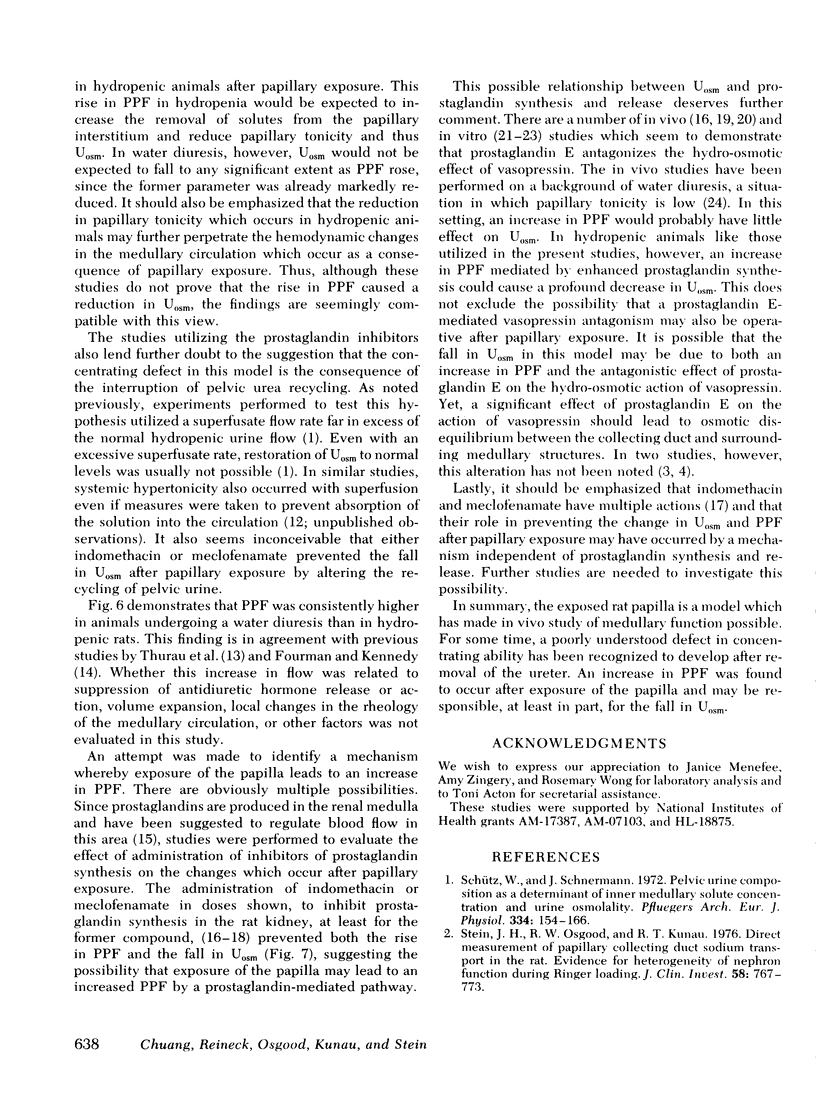
Studies were performed in Munich-Wistar rats to determine whether changes in papillary plasma flow might be responsible for the concentrating defect which occurs after exposure of the extrarenal papilla. Papillary plasma flow was measured by 125I-albumin accumulation. Initial studies in hydropenic animals revealed that papillary plasma flow was 40% higher in the kidney with the exposured papilla, 41 vs. 29 ml/min per 100 g of papilla (P < 0.001). This increase in papillary plasma flow was detectable 15 or 45 min after removing the ureter. Because it was unclear whether the rise in papillary plasma flow was a cause or the result of the fall in urine osmolality, similar studies were performed in animals undergoing a water diuresis. In this setting, papillary plasma flow still increased on the exposed side compared to the control side, 81 vs. 60 ml/min per 100 g, despite similarly low urine osmolalities of 155 and 174 mosmol/kg, respectively. This finding is compatible with the possibility that papillary exposure per se causes an increase in papillary plasma flow and that this hemodynamic alteration may lead to a reduction in urinary osmolality secondary to washout of the medullary interstitium. A final group of hydropenic rats was given either indomethacin or meclofenamate before removing the ureter. In these studies, there was no difference in either the papillary plasma flow or the urine osmolality between control and exposed kidneys. It is therefore suggested that opening the ureter induces an increase in papillary plasma flow by some mechanism which may involve an alteration in prostaglandin synthesis.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BERLINER R. W., LEVINSKY N. G., DAVIDSON D. G., EDEN M. Dilution and concentration of the urine and the action of antidiuretic hormone. Am J Med. 1958 May;24(5):730–744. doi: 10.1016/0002-9343(58)90377-2. [DOI] [PubMed] [Google Scholar]
- Berl T., Raz A., Wald H., Horowitz J., Czaczkes W. Prostaglandin synthesis inhibition and the action of vasopressin: studies in man and rat. Am J Physiol. 1977 Jun;232(6):F529–F537. doi: 10.1152/ajprenal.1977.232.6.F529. [DOI] [PubMed] [Google Scholar]
- Flower R. J. Drugs which inhibit prostaglandin biosynthesis. Pharmacol Rev. 1974 Mar;26(1):33–67. [PubMed] [Google Scholar]
- Fourman J., Kennedy G. C. An effect of antidiuretic hormone on the flow of blood through the vasa recta of the rat kidney. J Endocrinol. 1966 Jun;35(2):173–176. doi: 10.1677/joe.0.0350173. [DOI] [PubMed] [Google Scholar]
- GOTTSCHALK C. W. OSMOTIC CONCENTRATION AND DILUTION OF THE URINE. Am J Med. 1964 May;36:670–685. doi: 10.1016/0002-9343(64)90179-2. [DOI] [PubMed] [Google Scholar]
- Ganguli M., Tobian L. Does the kidney autoregulate papillary plasma flow in chronic postsalt hypertension? Am J Physiol. 1974 Feb;226(2):330–333. doi: 10.1152/ajplegacy.1974.226.2.330. [DOI] [PubMed] [Google Scholar]
- Grantham J. J., Orloff J. Effect of prostaglandin E1 on the permeability response of the isolated collecting tubule to vasopressin, adenosine 3',5'-monophosphate, and theophylline. J Clin Invest. 1968 May;47(5):1154–1161. doi: 10.1172/JCI105804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamison R. L., Buerkert J., Lacy F. A micropuncture study of collecting tubule function in rats with hereditary diabetes insipidus. J Clin Invest. 1971 Nov;50(11):2444–2452. doi: 10.1172/JCI106743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LILIENFIELD L. S., MAGANZINI H. C., BAUER M. H. Blood flow in the renal medulla. Circ Res. 1961 May;9:614–617. doi: 10.1161/01.res.9.3.614. [DOI] [PubMed] [Google Scholar]
- Lipson L. C., Sharp G. W. Effect of prostaglandin E1 on sodium transport and osmotic water flow in the toad bladder. Am J Physiol. 1971 Apr;220(4):1046–1052. doi: 10.1152/ajplegacy.1971.220.4.1046. [DOI] [PubMed] [Google Scholar]
- Lum G. M., Aisenbrey G. A., Dunn M. J., Berl T., Schrier R. W., McDonald K. M. In vivo effect of indomethacin to potentiate the renal medullary cyclic AMP response to vasopressin. J Clin Invest. 1977 Jan;59(1):8–13. doi: 10.1172/JCI108624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGiff J. C., Crowshaw K., Itskovitz H. D. Prostaglandins and renal function. Fed Proc. 1974 Jan;33(1):39–47. [PubMed] [Google Scholar]
- ORLOFF J., HANDLER J. S., BERGSTROM S. EFFECT OF PROSTAGLANDIN (PGE-1) ON THE PERMEABILITY RESPONSE OF TOAD BLADDER TO VASOPRESSIN, THEOPHYLLINE AND ADENOSINE 3',5'-MONOPHOSPHATE. Nature. 1965 Jan 23;205:397–398. doi: 10.1038/205397a0. [DOI] [PubMed] [Google Scholar]
- Schütz W., Schnermann J. Pelvic urine composition as a determinant of inner medullary solute concentration and urine osmolarity. Pflugers Arch. 1972;334(2):154–166. doi: 10.1007/BF00586788. [DOI] [PubMed] [Google Scholar]
- Solez K., Fox J. A., Miller M., Heptinstall R. H. Effects of indomethacin on renal inner medullary plasma flow. Prostaglandins. 1974 Jul 25;7(2):91–98. doi: 10.1016/0090-6980(74)90126-9. [DOI] [PubMed] [Google Scholar]
- Solez K., Kramer E. C., Fox J. A., Heptinstall R. H. Medullary plasma flow and intravascular leukocyte accumulation in acute renal failure. Kidney Int. 1974 Jul;6(1):24–37. doi: 10.1038/ki.1974.74. [DOI] [PubMed] [Google Scholar]
- Stein J. H., Osgood R. W., Kunau R. T., Jr Direct measurement of papillary collecting duct sodium transport in the rat. Evidence for heterogeneity of nephron function during Ringer loading. J Clin Invest. 1976 Oct;58(4):767–773. doi: 10.1172/JCI108527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- THURAU K. RENAL HEMODYNAMICS. Am J Med. 1964 May;36:698–719. doi: 10.1016/0002-9343(64)90181-0. [DOI] [PubMed] [Google Scholar]


