Abstract
Background:
Pneumococcal meningitis in adults is widely associated with intracranial complications, which occur in up to 74.7% of the patients.
Method:
Case report.
Results:
We report the case of a 40-year-old white female with pneumococcal meningitis after a sinus surgery, who developed a concomitant cerebral venous thrombosis and multiple cervical artery dissections. Following treatment with antibiotics and intravenous heparin, she had complete neurological recovery.
Conclusions:
Vascular complications should always be remembered and adequately treated in patients with bacterial meningitis. Cervical arterial dissections should be investigated as potential embolic sources of intracranial ischemic lesions.
Keywords: pneumococcal meningitis, cervical artery dissection, cerebral venous thrombosis
Introduction
Pneumococcal meningitis is widely associated with intracranial complications, which occur in up to 74.7% of adult patients.1,2 For example, cerebral venous thrombosis (CVT) occurred in 9.2%, and arterial infarction—mostly attributed to vasculitis—occurred in 21.8% of 87 consecutive patients with pneumococcal meningitis.1 The occurrence of cervical arterial dissection has not been previously reported in such patients.
Case Report
A 40-year-old white woman with a history of migraine presented to our service with headache, fever, and ear pain. She had had surgery of the right maxillary sinus for chronic recurring sinusitis 30 days before. Physical examination showed a normal habitus female (height 162 cm, weight 58 kg) with mild nuchal rigidity and an acute right-sided otitis media. A head computerized tomography (CT) scan showed a right-sided otomastoiditis and pansinusitis. Her cerebrospinal fluid (CSF) was turbid, with 3400 leucocytes/mm3 (96% neutrophils, 2% monocytes, and 2% lymphocytes), lactic acid was 81.9 mg/100 mL, glucose was 44 mg/dL (concomitant serum glucose was 150 mg/dL), proteins were 610 mg/100 mL. Gram stain revealed gram-positive diplococci and the CSF culture grew Streptococcus pneumoniae. She was immediately treated with intravenous ceftriaxone and dexamethasone. Five hours after admission, she became progressively drowsy and was intubated for airway protection. A transthoracic echocardiogram did not show any signs of endocarditis.
A follow-up head CT performed 24 hours after admission showed an area of infarction in the right cerebellar hemisphere confirmed by a brain magnetic resonance imaging (MRI) (Figure 1A), and slight reduction of the lateral ventricles when compared to the first CT. The brain MRI/MR angiography (MRA) revealed thrombosis of the left transverse and sigmoid dural venous sinuses and of the proximal jugular vein (Figure 1B and C). The cervical and intracranial arterial MRA was normal. Anticoagulation with intravenous heparin was initiated targeting an activated partial thromboplastin time (aPTT) 1.5 to 2 times the control. Her physical examination improved, and she was successfully extubated 48 hours after admission. Two days after the start of anticoagulation she became confused. A new head CT scan revealed a left parietal intraparenchymatous bleeding suggestive of a hemorrhagic venous infarct (Figure 1D). Heparin was therefore continued, and her neurological examination progressively improved. A control brain MRI showed partial recanalization of the left transverse and sigmoid dural venous sinuses and dissections of the cervical portion of the left internal carotid artery and of both vertebral arteries (Figure 2A, C, D, E, and F). A pseudoaneurysm in the V2 portion of the left vertebral artery was observed (2B). The CT angiography confirmed the dissections (Figure 2B). Screening for autoimmune disorders was negative (antinuclear antibody, anti-dsDNA, extractable nuclear antigens panel, antiphospholipid antibodies, lupus anticoagulant, perinuclear anti-neutrophil cytoplasmic antibody, and cytoplasmic anti-neutrophil cytoplasmic antibody). After 5 days of receiving intravenous heparin, she developed pain in her left arm and right leg. A CT scan revealed an acute hematoma of the left brachial and right iliopsoas muscles. Anticoagulation was discontinued, and she was started on aspirin. She continued to improve clinically, and after 14 days of intravenous ceftriaxone she was discharged home with no neurological symptoms (modified Rankin score: 0). A follow-up cervical MRA (6 months after discharge) showed resolution of the dissections and of the left vertebral pseudoaneurysm (Figure 3 E, F).
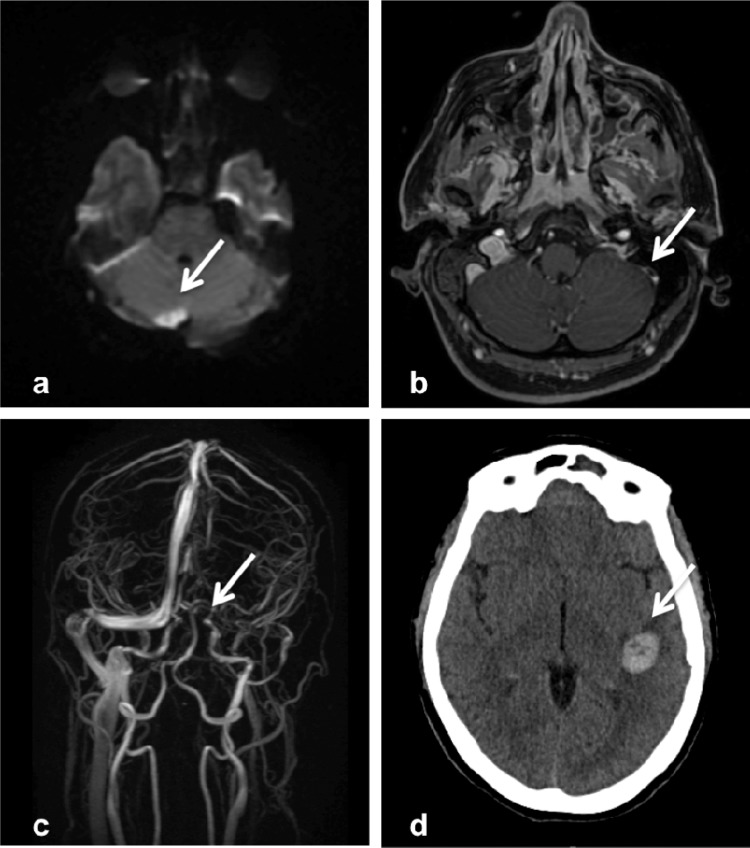
Figure 1.
A, Brain magnetic resonance imaging (MRI-DWI sequence) showing acute right cerebellar infarct. B and C, Brain MRI and MR venography showing thrombosis of the left transverse and sigmoid dural sinuses. D, Head computed tomography (CT) showing a left parietal intraparenchymatous bleeding.
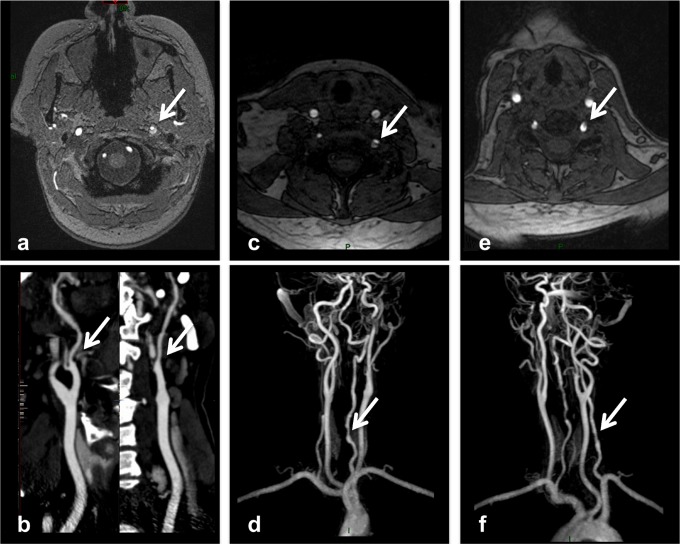
Figure 2.
A and B, Brain magnetic resonance imaging ([MRI] axial T1-weighted, fat-saturated image of the neck) and computed tomography (CT) angiography showing dissection of the left internal carotid artery. C, D, E, F, Brain magnetic resonance imaging (axial T1-weighted, fat-saturated image of the neck) and MR angiography showing dissection of both vertebral arteries. Observe pseudoaneurysm in the V2 portion of the left vertebral artery (B).
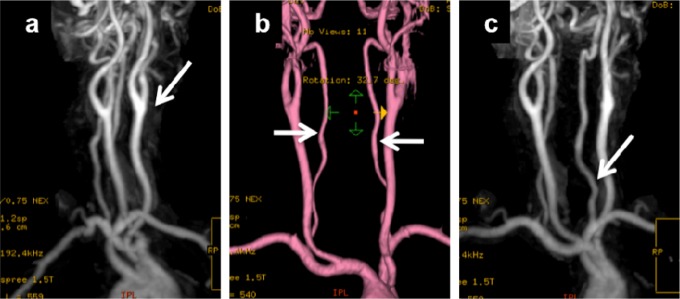
Figure 3.
A, B, C, Follow-up (6 months after discharge) magnetic resonance (MR) angiography showing resolution of cervical dissections, including resolution of the left V2 pseudoaneurysm (C, arrow).
Discussion
We presented the first report of the occurrence of cervical arterial dissections in a patient with bacterial meningitis and CVT. Pneumococcal meningitis in adults can be associated with several intracranial complications, such as diffuse brain swelling, hydrocephalus, hearing loss, ischemic and hemorrhagic stroke, and CVT.3–6 Our patient presented 2 major vascular complications (CVT and multiple cervical arteries dissections) of pneumococcal meningitis, probably caused by contiguous spread infection after a sinus surgery.
The cerebellar infarct in our patient was probably due to infectious vasculitis and not related to the vertebral dissections, because it appeared in the first MRI, in which there were no signs of cervical arterial dissection. The pathophysiology of the vascular damage in patients with pneumococcal meningitis is commonly attributed to infectious vasculitis.1,6,7 There is, however, no strong evidence that this is the only mechanism. Local bacteria invasion might also play a role in the vascular events in patients with bacterial meningitis, triggering the spread of procoagulant and antifibrinolytic agents, leading to intraparenchymal edema and intravascular coagulation.3,6 A significant association between recent infection and cervical artery dissection was previously described.8,9 In our patient, it is possible that the pneumococcal infection contributed to the development of the internal carotid and vertebral arteries dissections, although we cannot exclude the hypothesis that the endotracheal intubation, with hyperextension of the neck, might have played a role.9–11
The natural history of unruptured vertebral artery pseudoaneuryms as the one seen in our patient was described to be relatively benign, with a high probability of spontaneous angiographic cure.12,13 The 6-month follow-up MRI/MRA of our patient showed complete resolution of the dissections. In some patients with persistent aneurysmal dilatation, intravascular coil embolization or surgical procedures might be necessary.13
In conclusion, vascular complications should always be remembered and adequately treated in patients with bacterial meningitis. Cervical arterial dissections can happen in such patients and should be investigated as potential embolic sources of intracranial ischemic lesions.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: supported by CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico).
References
- 1.Kastenbauer S, Pfister HW. Pneumococcal meningitis in adults: spectrum of complications and prognostic factors in a series of 87 cases. Brain. 2003;126(pt 5):1015–1025 [DOI] [PubMed] [Google Scholar]
- 2.Kragsbjerg P, Kallman J, Olcen P. Pneumococcal meningitis in adults. Scand J Infect Dis. 1994;26(6):659–666 [DOI] [PubMed] [Google Scholar]
- 3.Weisfelt M, van de Beek D, Spanjaard L, Reitsma JB, de Gans J. Clinical features, complications, and outcome in adults with pneumococcal meningitis: a prospective case series. Lancet Neurol. 2006;5(2):123–129 [DOI] [PubMed] [Google Scholar]
- 4.Auburtin M, Porcher R, Bruneel F, et al. Pneumococcal meningitis in the intensive care unit: prognostic factors of clinical outcome in a series of 80 cases. Am J Respir Crit Care Med. 2002;165(5):713–717 [DOI] [PubMed] [Google Scholar]
- 5.Heckenberg SG, Brouwer MC, van der Ende A, Hensen EF, van de Beek D. Hearing loss in adults surviving pneumococcal meningitis is associated with otitis and pneumococcal serotype. Clin Microbiol Infect. 2012;18(9):849–855 [DOI] [PubMed] [Google Scholar]
- 6.Vergouwen MD, Schut ES, Troost D, van de Beek D. Diffuse cerebral intravascular coagulation and cerebral infarction in pneumococcal meningitis. Neurocrit Care. 2010;13(2):217–227 [DOI] [PubMed] [Google Scholar]
- 7.Kirkpatrick B, Reeves DS, MacGowan AP. A review of the clinical presentation, laboratory features, antimicrobial therapy and outcome of 77 episodes of pneumococcal meningitis occurring in children and adults. J Infect. 1994;29(2):171–182 [DOI] [PubMed] [Google Scholar]
- 8.Grau AJ, Brandt T, Buggle F, et al. Association of cervical artery dissection with recent infection. Arch Neurol. 1999;56(7):851–856 [DOI] [PubMed] [Google Scholar]
- 9.Rubinstein SM, Peerdeman SM, van Tulder MW, Riphagen I, Haldeman S. A systematic review of the risk factors for cervical artery dissection. Stroke. 2005;36(7):1575–1580 [DOI] [PubMed] [Google Scholar]
- 10.Testai FD, Gorelick PB. An unusual cause of vertebral artery dissection: Esophagogastroduodenoscopy. Stroke Res Treat. 2010;2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tettenborn B, Caplan LR, Sloan MA, et al. Postoperative brainstem and cerebellar infarcts. Neurology. 1993;43(3 pt 1):471–477 [DOI] [PubMed] [Google Scholar]
- 12.Nagahata M, Manabe H, Hasegawa S, Takemura A. Morphological change of unruptured vertebral artery dissection on serial mr examinations. Evaluation of the arterial outer contour by basi-parallel anatomical scanning (bpas)-mri. Interv Neuroradiol. 2006;12(suppl 1):133–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yamamoto J, Sakai N, Yokoyama T. Basi-parallel anatomical scanning magnetic resonance imaging in patients with bilateral vertebrobasilar artery dissections. Neurol Med Chir (Tokyo). 2011;51(8):575–578 [DOI] [PubMed] [Google Scholar]