Abstract
Human health experiments systematically expose people to conditions beyond the boundaries of medical evidence. Such experiments have included legal-medical collaboration, exemplified in the US by the PHS Syphilis Study (Tuskegee). That medical experiment was legal, conforming to segregationist protocols and specific legislative authorization which excluded a selected group of African Americans from any medical protection from syphilis. Subsequent corrective action outlawed unethical medical experiments but did not address other forms of collaboration, including PHS submission to laws which may have placed African American women at increased risk from AIDS and breast cancer. Today, anti-lobbying law makes it a felony for PHS workers to openly question legally anointed suspension of medical evidence. African Americans and other vulnerable populations may thereby face excess risks -- not only from cancer, but also from motor vehicle crashes, firearm assault, end stage renal disease and other problems -- with PHS workers as silent partners.
Keywords: Bioethics; public health; disparity, healthcare; communicable disease contact tracing; breast cancer; Medicare;
Introduction
In human subject research, experimental protocols are used to systematically expose people to interventions beyond the boundaries prescribed by the best available medical evidence. Further, it is possible to distinguish between legal mandates for medical human health experiments and legal mandates for social human health experiments. Requirements for medical human health experiments include a rationale comprising medical evidence showing that the potential benefits of the proposed intervention outweigh the potential risks.1 In clinical trials, for example, this may involve estimation of expected improvements in clinical outcome based on successful tests of a new drug. Before the trial, knowledge about the consequences is beyond the boundaries of existing medical evidence. There are, nonetheless, medically based, scientific reasons to justify the human experiment.
Legal protocols deviate from medical experiments, however, in that there are no requirements to provide medical evidence that the likely benefits of an intervention outweigh the risks. On the contrary, US lawmakers are free to mandate human exposures to interventions which are harmful according to the best available medical evidence. For example, US lawmakers have sorted the nation into a social experiment based on primary and secondary automobile seat belt laws. According to the best available medical evidence, primary laws (which allow police citations solely on the basis of failure to wear a seat belt) save more lives than secondary laws (which allow police citations for seat belts only after a driver has been stopped for some other reason).2 Moreover, additional medical evidence shows that secondary seat belt laws may be especially harmful to racial and ethnic minorities.3,4 At present, however, 17 US states have secondary laws, 32 have primary laws, and one has no law.5 Clearly, evidence from political science, business analyses, and other disciplines has been given primacy over medical evidence. This is an important freedom, and is founded, in part, on the ethical principle of autonomy. It is analogous to an individual’s right to reject medical recommendations for a particular procedure. While individuals may make such decisions on their own, however, we argue that the ethical principles of beneficence, non-maleficence, justice, caring, and solidarity require continued medical surveillance, reporting, and advocacy regarding the outcomes of population-based, legally mandated, human experimentation.
Continued medical surveillance is possible, in part, because the distribution of human exposure under legally anointed social protocols mimics clinical research. Results from different arms (that is, conditions) of the resultant social experiments may therefore be compared in ways that are similar to analyses used for medical experiments. Thus, for example, it is possible to compare automobile crash deaths in states with primary and secondary seat belt laws. The best available evidence shows a median decrease of 8% for fatal crashes in primary law states versus secondary law states, and a median increase in observed seat belt use of 14% in primary law states versus secondary law states.2 Such analyses are ignored by legislators and, as will be shown, PHS workers are enjoined from advocacy on behalf of adversely affected people residing in places where the secondary law arm of this social experiment is enforced. In the present report, we describe similar instances of lawful social experimentation that may relegate African Americans to conditions outside the boundaries prescribed by the best available medical evidence for cancer-related disease.
The Legally Mandated Medical Experiment at Tuskegee
Prior to the well-known and now infamous US Public Health Service (PHS) Syphilis Study at Tuskegee (1932-1972), social experimenters in the Southern US had developed a complex intervention embodied in a codification of, “Laws and policies systematically disadvantaging African Americans during and long after their 246-year enslavement.”6 While slavery was abolished in 1865, there was no immediate organized effort to correct its abuses. Whites continued to regard former slaves as intellectually, morally, and physically inferior.6,7 It was not until passage of the Civil Rights Act in 1964 that rights originally promised with the 1868 passage of the 14th amendment were reaffirmed,6 meaning that throughout the 400 years blacks and whites have lived together in the US, the basic citizenship of African Americans has been specifically affirmed for less than 50 of those years.6,7
In Alabama, the state where the PHS Syphilis study occurred, the State Constitutional Convention of 1901 specifically codified white supremacy: Sections 178 and 180 through 182 included provisions specifically designed to disenfranchise black voters. Section 256 established an entirely segregated school system. Section 102 prevented the legislature from ever allowing interracial marriages. “Custom, backed up by the threat of violence from the police or lynch mobs, enforced forms of residential, economic, and social segregation encompassing banking (separate banks), medicine (separate medical practices and hospitals), law (informal exclusion of blacks on juries), religion (separate churches), and daily life (encompassing separate residential areas, schools, and even cemeteries). If these measures failed to enforce whites’ preferences to avoid associating with blacks, the state stood ready to step in.”8
Racially segregated medical care available to Alabama residents in the 1930’s adversely affected African American access to health care in general9,10 and to services for the treatment of syphilis in particular.11,12 In general, health care in the Jim Crow South degraded black patients and black physicians alike, dispensing services through a complex maze of separated and unequal care.9,10 More specific to syphilis, in 1926, Moore and Keidel11,12 reported that continuous treatment of early syphilis, including 21 injections of an arsphenamine, reduced clinical or serological relapse to 21% as against 89.2% in patients receiving one to eight injections. In Macon County, Alabama the initial peer reviewed paper from the PHS Syphilis study confirmed that, “‘Adequate treatment has not been freely available to most indigent citizens for a period longer than a decade.’”12,13 Indigence, in turn, was more common among African Americans,14 and poor blacks, knowing they could not pay for proper health care, often declined to seek it. Patent medicine, folk healing, and/or unlicensed practitioners were substituted.9 By 1954, care had not substantially improved, and PHS researchers commented that even though medical facilities were available in the county, “Costs are prohibitive or patients are unaware of them.”12 Alabama laws and policies operant at the start of the PHS Syphilis study therefore constituted the protocols for a legally mandated social experiment that subjected African Americans to health care that was inconsistent with recommendations prescribed by the best available medical evidence even if and when they approached the health care system.
Application of benchmarks such as respect for persons, justice, beneficence, nonmaleficence, caring and solidarity15 would have made it clear that the only ethical avenue for federal PHS physicians working in Alabama was advocacy for change consistent with the best available medical evidence. In particular, the principle of respect for persons establishes that provision of unequal healthcare on the basis of race is unjust. Moreover, while justice may encompass, “aridity, impersonality, disconnectedness, and emotional neutrality”,16 caring compensates by requiring, an empathic attunement to patient needs.15 Additionally, solidarity, includes concern for the oppressed, thereby reinforcing, “The egalitarian perspective that addressing the needs of the worst off should prima facae be the first priority of justice.”17 The PHS physicians who designed the Syphilis study might have fought to provide a model for excellence in health care. Instead, their study not only embraced Alabama’s unjust social protocols, but distilled them to the point that inadequate care became no care – simultaneously cloaked in a web of lies to make participants believe they had been freed from unjust treatment. Moreover, this unethical medical experiment was entirely legal according to federal statute – one reason that no one involved was either indicted or charged with a legal violation.18 The consequences of this multifaceted betrayal are still being felt.19
Corrective federal laws and policies following exposure of the PHS Syphilis study outlawed medical research, but lawmakers and bioethicists alike failed to address ethical issues relating to other mechanisms for legal suspension of medical evidence. We next describe two examples in which this may have occurred, both to the disadvantage of African American women and their families.
Methods
The overall form of the case presentations is intended to represent consideration of two case examples for reflective bioethical consideration as described by Beauchamp and Childress.20 The cases concern HIV, an important risk factor for cancer,21 and malignant neoplasm of the female breast.
Case Example One
Comparisons between the historical processes in the Syphilis Study and those related to a public policy requiring HIV contact tracing were drawn from secondary sources, including reports in the scientific and historical literature. Data for mortality classified as HIV disease (HIV/AIDS). including race-sex-specific, age-adjusted rates and 95% confidence intervals were obtained from publically available Compressed Mortality Files, a death certificate resource of the National Center for Health Statistics as presented on the publicly available WONDER internet site of the US Centers for Disease Control and Prevention.22,23 Specifically, we compared age-adjusted (15-85+ years) black female HIV/AIDS mortality in States which began to require HIV contact tracing by name in 1990-1993 (LA, MI, NV, NJ, NC, OH, and TN) and the States and the District of Columbia which delayed this requirement until 1999-2008 – that is, three or more years after HAART (Highly Active Anti-Retroviral Treatment effective against HIV/AIDS) became available (AK, CA, CT, DE, DC, FL, GA, HI, IL, IA, KS, KY, ME, MD, MA, NE, NH, NM, NY, OR, PA, RI, TX, WA). Information on when the laws were enacted came from the Kaiser Family Foundation.24 These two groups of States were of interest, in part, because mortality rates for black women were statistically indistinguishable (no overlap in 95% confidence intervals) prior to 1990. This permitted a description of year-by-year mortality as the two groups of States parted ways on the issue of HIV-contact tracing and when they eventually began to move back together ultimately rejoining in unanimous requirements for HIV contact tracing by name. States passing laws requiring HIV contact tracing by name before 1990 were not included since they never had HIV/AIDS mortality rates that were comparable to the two other groups. Specifically, HIV/AIDS mortality among black women in states requiring contact tracing by name before 1990 was significantly lower than both of the other groups, regardless of when reporting requirements changed.
Case Example Two
We obtained claims data for two cohorts each comprising 1,000,000 non-Hispanic black and non-Hispanic white women. A complex probability sample was taken from all Medicare beneficiaries, structured to enrich Black inclusion. Members of each cohort were alive from 1992-1995 or 2005-2008. We described regular screening mammography in 1992-1995 (T1) and 2005-2008 (T2) among the black and white beneficiaries, consistent with the US Preventive Services Task Force (USPSTF) B-rated recommendation of ≥1 mammography screening every two years for women ages 50-74 years.25 Women older than 74 years were not included in these analyses since the USPSTF found insufficient evidence for or against a mammography benefit in that age group. Outpatient and physician Medicare claims were reviewed. Women receiving regular mammography, defined as at least one screening mammogram every two years were identified using an algorithm adapted from Smith-Bindman et al.26 Socioeconomic and demographic data were obtained, in part, from GeoLytics, Inc. (East Brunswick, NJ). We collected 1990 and 2000 data at the county level. GeoLytics bases their estimates on US Census Bureau reports and limited population estimates, then expands on those to provide multiple population-based variables.27 GeoLytics variables included low educational attainment (percent of population age 25 or older who are not high school graduates), percent of population with annual income below poverty, percent single parent households, median income, income inequality, and percent unemployment. County level estimates of black residential isolation were obtained from the publicly available web site of the Arizona State University GeoDa Center.28 Race-specific absolute increase in percent county population receiving regular screening mammography was used as a measure of diffusion into the population. Race-specific ordinary least squared (OLS) regression analyses29 were done to estimate the magnitude of association between demographic factors and diffusion of Medicare’s innovative mammography screening policy.
Results
Case Example One
Historical Review
Penicillin was not the only form of health care withheld in the Syphilis Study. Aside from other types of individual therapy, Dr. Joshua Williams noted that participants were not reported to local public health departments for follow-up of their diagnosed syphilis. While participant recruitment for the study was restricted to persons in the late latency phase of infection, public health referral was clearly indicated for some.30 Failure to report subverted a 1927 Alabama law requiring reporting and treatment of syphilis,31 and blocked receipt of state benefits from federal grants-in-aid for prevention and treatment of syphilis which were available under provisions of the 1938 amendments to the Venereal Disease Control Act of 1918.32 While not all of Williams’ observations are given full credence,30 withholding such reports would have been consistent with the objective of assuring that the Tuskegee men received no treatment. It also expanded the circle of victims to include wives and babies. The best estimates are 22 wives, 17 children and two grandchildren were infected but untreated, although exact numbers are unknown.33,34
Contact tracing via health provider referral became the standard public health medical practice for controlling sexually transmitted diseases in the 1940’s.35-37 Although American data were sparse, a 1972 British review published at about the same time the Syphilis Study was being closed estimated, “That efficient contact tracing lowers the rate of venereal disease by about 20 per cent.”38 After that, contact tracing continued as the reference standard for sexually transmitted disease control, as exemplified by the US Guide to Community Preventive Services and the American Public Health Association’s Control of Communicable Diseases Manual.39,40
While medical care standards of contact tracing remained relatively stable, legislative and political opposition to these standards grew stronger, particularly as the HIV (Human Immunodeficiency Virus) Disease epidemic emerged. Source individuals could anticipate a harsh social response when confidentiality was breached, and there were public health concerns about voluntary cooperation.41-43 Requirements for health provider reports of communicable disease are a matter of state jurisdiction, however, and many states failed to make HIV-disease a reportable disease, especially during the early years of the epidemic,44 thereby treating HIV as if it were not a sexually transmitted disease. Evidence published in leading general and public health journals in 1991 and 199245,46 about failures of affected individuals to notify their partners was ignored. The common law duties of physicians and similar health professionals to warn known third parties of a predictable danger47 were undercut by grants of extraordinary immunity from liability for failure to notify known, at-risk partners of HIV-infected people.46 Common law for such notification had been established in several cases, notably Tarasoff v. Regents of University of California, as well as specific cases involving smallpox, tuberculosis, syphilis, typhus, meningitis, scarlet fever, and diphtheria.46,47 As the Commissioner of a major city learned, public health officers who supported reporting and other types of politically unpalatable, but medically supportable public health care, could lose their jobs.48,49
When legislators considered making HIV reportable, organizations such as The Gay Men’s Health Crisis50 and the American Civil Liberties Union (ACLU)51 were opposed. The former cited recommendations against contact tracing, “From an overwhelming majority of AIDS organizations” and argued that, “If implemented, these regulations will interfere with efforts to provide services to people living with HIV and hamper our ability to reduce HIV infection rates among at-risk populations…”50 The ACLU saw partner notification as a threat to minorities, noting that, “While gay and bisexual men made up the largest at-risk population in the first decade of the AIDS epidemic, in the second decade new cases of HIV are increasingly occurring among people of color and injection drug users51 The ACLU also presented a limited review of scientific evidence, noting CDC information that traditional partner notification had failed to stop some outbreaks of syphilis.51 These results were said to echo those of Oregon syphilis control workers, who reported difficulty with locating partners, an observation which was attributed to the long infectious period of the disease and the high incidence of drug use and prostitution among those infected. The Oregon study concluded that the failure of traditional methods to control the syphilis epidemic was of particular concern because many of the risk factors for that epidemic were the same as those for HIV infection.51
When successful, this opposition formulated one arm of a legally mandated experiment which placed at special risk exactly the same groups of ancillary victims as the PHS Syphilis Study, namely black women and their babies. Also, as was true for Syphilis study, government health workers were aware of this risk. Specifically, in 1978, Bell and Wineberg observed that the occurrence of persons with the behavior of having sex with both men and women seemed more frequent among blacks than other groups.52 In 1988, public health workers in the AIDS Program of the US Centers for Disease Control (now US Centers for Disease Control and Prevention, CDC) cited Bell and Wineberg’s52 work as a possible explanation of their own observations that women whose sexual partners were males who also had sex with men were 4.6 times more likely to be black as white and 3.6 times more likely to be Hispanic as white. These workers recommended that preventive programs take cognizance.53 Contemporaneous reports corroborated increased risks faced by black women,54,55 including evidence that many women may not be aware of their partner’s behavior and (in a small California study) that 20% of black female partners of men who also have sex with men were aware of their male partner’s sexual behavior, compared to 80% of white female partners.54,56 All of this information was available in the peer-reviewed scientific literature as of 1992.
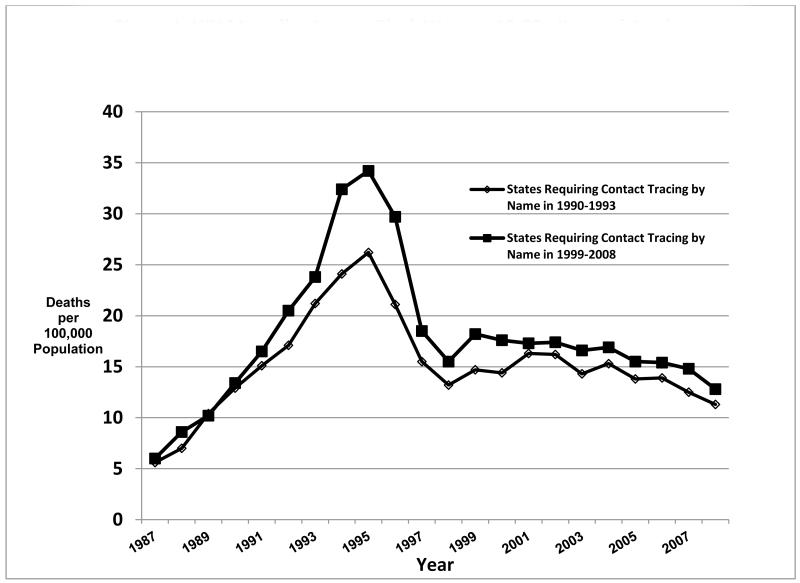
HIV Mortality
Results comparing different arms of the social experiment engineered by advocates against HIV contact tracing are shown in Figure 1 (black rates) and Table 1 (black rates and 95 % confidence intervals). With the exception of 1992, there was no overlap in the 95% confidence intervals for overall age-adjusted (15-85+ years) mortality among black women in the two groups of states from 1987 (the first year for which data are available) to 1993, when LA, MI, NV, NJ, NC, OH, and TN had passed legislation requiring contact tracing by name. From 1994 to 2000, however, the states requiring contact tracing by name had significantly lower mortality among black women than states without the requirement. Then, from 2001 to 2008 (the most recent year for which data are available), and after the second group of states had begun to require contact tracing, rates for both groups of states were again indistinguishable in that there was overlap in the 95% confidence intervals. No such pattern was found for white women, white men, or black men (data not shown).
Figure 1.
HIV Mortality Among Black Women 15-85+ Years of Age in States with Contact Tracing by Name Beginning in 1990-93 and States in Which Contact Tracing by Name was Delayed Until 1999-2008.
Table 1. Age-adjusted HIV Infection Mortality and 95% Confidence Intervals Among Black Women Ages 15 to 85+ Years in US States With HIV Contact Tracing by Name Beginning in 1990-93 and 1999-2007.
| HIV Contact Tracing by Name Beginning in 1990-1993 |
HIV Contact Tracing by Name Beginning in 1999-2007 |
|||||
|---|---|---|---|---|---|---|
| Year | Lower Bound, 95% Confidence Interval |
Age- adjusted Rate |
Upper Bound, 95% Confidence Interval |
Lower Bound, 95% Confidence Interval |
Age- adjusted Rate |
Upper Bound, 95% Confidence Interval |
| 1987 | 4.7 | 5.6 | 6.5 | 5.4 | 6 | 6.7 |
| 1988 | 6 | 7 | 8 | 7.8 | 8.6 | 9.4 |
| 1989 | 9.2 | 10.4 | 11.7 | 9.4 | 10.2 | 11 |
| 1990 | 11.6 | 12.9 | 14.3 | 12.4 | 13.4 | 14.3 |
| 1991 | 13.7 | 15.1 | 16.5 | 15.5 | 16.5 | 17.5 |
| 1992 | 15.6 | 17.1 | 18.6 | 19.4 | 20.5 | 21.6 |
| 1993 | 19.5 | 21.2 | 22.9 | 22.6 | 23.8 | 25 |
| 1994 | 22.3 | 24.1 | 25.8 | 31 | 32.4 | 33.8 |
| 1995 | 24.4 | 26.2 | 28 | 32.8 | 34.2 | 35.6 |
| 1996 | 19.5 | 21.1 | 22.7 | 28.4 | 29.7 | 31 |
| 1997 | 14.1 | 15.5 | 16.9 | 17.5 | 18.5 | 19.6 |
| 1998 | 12 | 13.2 | 14.4 | 14.5 | 15.5 | 16.4 |
| 1999 | 13.4 | 14.7 | 16.1 | 17.2 | 18.2 | 19.2 |
| 2000 | 13.1 | 14.4 | 15.7 | 16.6 | 17.6 | 18.6 |
| 2001 | 14.9 | 16.3 | 17.6 | 16.3 | 17.3 | 18.2 |
| 2002 | 14.8 | 16.2 | 17.5 | 16.4 | 17.4 | 18.3 |
| 2003 | 13.1 | 14.3 | 15.6 | 15.7 | 16.6 | 17.5 |
| 2004 | 14 | 15.3 | 16.6 | 16 | 16.9 | 17.8 |
| 2005 | 12.6 | 13.8 | 15.1 | 14.6 | 15.5 | 16.4 |
| 2006 | 12.6 | 13.9 | 15.1 | 14.5 | 15.4 | 16.2 |
| 2007 | 11.3 | 12.5 | 13.6 | 14 | 14.8 | 15.7 |
| 2008 | 10.2 | 11.3 | 12.4 | 12 | 12.8 | 13.6 |
Case Example Two
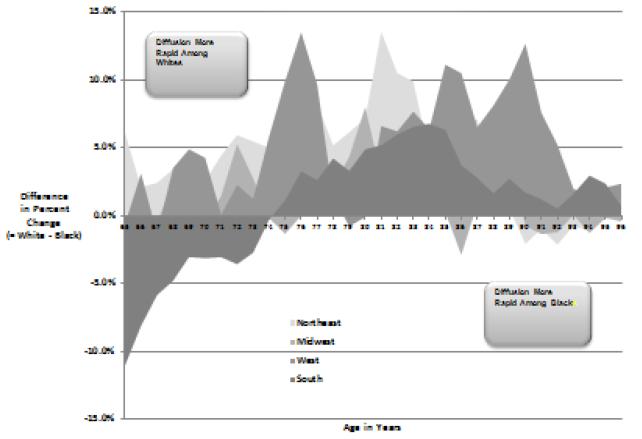
Diffusion of the Medicare Mammography Benefit
The sample included 153,857 (T1) and 128,919 (T2) black women and 465,669 (T1) and 403,085 (T2) white women. Overall, regular screening rates were 31% in in T1 and 47% in T2, with absolute increases among blacks exceeding those for whites by 2% (15% to 13%) %. Overall percentages, however, were driven by large increases from low baselines in the Southern US. As shown in Figure 2, diffusion was more rapid for whites at nearly every age level, except in the South. Additionally, we merged county level black and white rates of regular mammography from the 1992 cohort (T1) and 2005 cohort (T2) with socio-economic and geographic indicators in order to estimate several ordinary least squared (OLS) regression models. The first models estimated the absolute rates in T1 and T2. The final model controls for the rate of regular screening at T1, so the coefficients reflect the increase in screening associated with each independent variable. High colinearity among these variables (e.g., low educational attainment, poverty, black residential isolation and single parent households) prohibited their inclusion in a single model. Table 2 displays the results from a 1st change model including rates of low educational attainment and unemployment. As expected, the rate of screening at T1 affects the rate at T2. A 1% difference in rate at T1 is associated with 0.42% (black women) and 0.44% (white women) higher rates at T2. Low educational attainment affects regular screening at T2 after adjusting for screening rates at T1. Each percentage increase in women with low educational attainment is associated with a 0.17% decrease in regular screening mammography for black women and a 0.28% decrease among white women. Moreover, the race difference in the effects of education differs significantly (p<0.01). Controlling for Census Division results attenuated racial differences in the effects of the low education. In this model an increase in one percent of the population with less than high school is associated with a 0.23% decline in regular screening for black beneficiaries and a 0.29% decrease among white beneficiaries. The county rate of unemployment appears to affect screening only among black women. The association between unemployment and screening failed to achieve significance after accounting for Census Division.
Figure 2.
Difference in Absolute white and Absolute Balck Percent Change in Regular Mammography Among United States Medicare Beneficiaries from 1992-95 to 2005-08. US Census Regions.
Table 2.
Coefficients from 1st change models predicting regular screening mammography at T2
| BLACK WOMEN | WHITE WOMEN | |||
|---|---|---|---|---|
| VAR | b | p-value | b | 95% CL |
| CONSTANT | 0.352 | <0.0001 | 0.393 | <0.0001 |
| REGULAR SCREENING MAMMOGRAPHY AT TIME ONE (T1) |
0.419 | <0.0001 | 0.441 | <0.0001 |
| PERCENT POPULATION AGE 25+ YEARS WITH LESS THAN HIGH SCHOOL EDUCATION |
−0.173 | <0.0001 | −0.282 | <0.0001 |
| PERCENT UNEMPLOYMENT |
−0.583 | 0.0021 | −0.222 | 0.1486 |
Discussion and Reflective Consideration
Case Example One
As reviewed above, the PHS Syphilis Study at Tuskegee was an unethical medical experiment which exaggerated an unethical, legally mandated, social experiment. PHS providers magnified the existing social protocols for segregated health care, assuring that African American men would receive no care for syphilis as opposed to inadequate care. By the late 1980’s overt problems related to medical research were recognized as unacceptable. What transpired in Case Example 1, however, is that laws were once again manipulated so that African American women and their babies were forcibly separated from access to healthcare consistent with the best medical evidence (that is personal contact tracing as the best means for protecting the partners of people with HIV/AIDS). There was no acceptable medical evidence to support the decision whereby lawmakers and policymakers excluded HIV/AIDS from the list of sexually transmitted diseases requiring contact tracing in some states. Nor was there a body of medical evidence to support legal policies designed to discourage physicians from performing partner notification in cases of exposure to an infectious disease. On the contrary, these actions comprised a legally mandated rejection of medical evidence that placed African American women in non-contact tracing states at special risk. They were denied basic public health care without their knowledge or consent. When PHS scientists provided warnings about the possible dangers, they acquiesced, were fired for refusing to do so, or left public health on their own.
While a definitive answer is precluded by the traditional problems of death certificate data,57 the ecologic nature of the observations which makes it impossible to ascertain what happened in individual cases, and the absence comparable descriptions for Hispanic women58, the descriptive data for Case Example 1 are consistent with the hypothesis that a legislatively mandated experiment occurred, whereby one group of states enacted HIV contact tracing laws in 1990-1993 and a second group of states rejected recommended medical practice and delayed passage of contact tracing by name until several years later. . When the two groups of States both lacked requirements for contact tracing by name (1987-1989), there was no statistically significant difference in overall, age-adjusted HIV mortality among black women. This establishes the comparability of the two groups of states for baseline HIV risk among black women. Nor was there a significantly significant difference when both groups of states moved back toward consistency in requiring contact tracing by name. In between these periods, however, black women residing in states that were quicker to enact contact tracing laws had a significant HIV-survival advantage in comparison to black women residing in states that did not. These descriptive observations are consistent with the additional hypothesis that contact tracing consistent with the best available medical evidence protected black women in states requiring contact tracing for the period 1990-1993. If so, then public health workers who were not fired may have joined their Tuskegee forebears, not as active medical experimenters, but rather as silent partners in a legally mandated experiment that withheld medical care from African Americans: Tuskegee redux.
Medical and legal advocates against HIV contact tracing may have believed that exaggeration of existing laws and policies designed to protect HIV partners served the best interests of the population as a whole; certainly we know of no evidence that they intended to harm black women or their babies. We argue, however, that just as was true at the time of the PHS Syphilis study, respect for persons establishes that provision of unequal healthcare on the basis of race or gender is unjust. Recognition of this principle could have guarded against “Putting an unjustly low priority on care for any group or individual according to a consequentialist calculus.”17 Moreover, application of the benchmarks of caring and solidarity might have alerted everyone about the pitfalls of emphasizing the perceived interests of one group in such a way as to potentially promote avoidable harms to another, potentially more vulnerable group – all the more so since effective anti-retroviral treatment became available at the time that the legal protocols for the two groups of states diverged.
Case Example Two
Medicare has had many benefits, including those which systematically aid blacks. The law is credited, for example, with achieving the elimination of segregated hospital care in the Southern US.59 Additionally, Medicare dramatically reduced out-of-pocket expenditures for health care, thereby producing welfare gains for people of all races and ethnicities that may have been sufficient to cover between half and three-quarters of Medicare costs during the first decade of the program.60 Available evidence, however, suggests that Medicare may have had little or no impact on mortality60 and that blacks and other non-whites are less likely to know about Medicare services, particularly coverage and benefits, enrollment/disenrollment, and plan choice.61 If, as suggested by the cohort data presented here, one of the reasons for Medicare’s low health impact is to systematically (if unintentionally) favor acquisition of screening mammography by whites for reasons of socioeconomic position, it would therefore be doing so without the knowledge of the people most adversely affected.
While Medicare claims data are less limited than comparisons based on death certificates, additional research is still needed to confirm Medicare’s hypothesized causative role in producing disparate screening rates. For example, while claims represent individual data, the demographic characteristics attached to geographic regions are ecologic. Nonetheless the data from this example showing more rapid diffusion of the mammography benefit among whites in most parts of the nation support the hypothesis that Medicare law may represent a social experiment whereby the legislative definition of medical assistance for obtaining a potentially lifesaving service unintentionally favors acquisition by whites relative to blacks. The multivariable analyses provide additional support for this hypothesis by showing that county-level variations in educational attainment, which may, in part, reflect lack of societal investment in human capital,62 are significantly associated with regular acquisition of the screening mammography benefit.
Context of the Case Examples
These examples are not isolated occurrences. Overall disparities in black:white mortality persisted throughout the 20th century63 and in 2008, were approximately equal to the level achieved in 1922.23,64 Inequalities affect infants,65 children,6 youth,66,67 middle aged men,68 women69 and the elderly.15 As noted by Margaret Whitehead (W.H. Duncan Professor of Public Health and Head of the Department of Public Health Policy, Health and Society in the Institute of Psychology, University of Liverpool) these disparities are, “‘Systematic, socially produced and therefore modifiable) and unfair’ and result from the unjust distribution of social, economic, political, and environmental conditions that determine health.”70 While recent medical publications have sought to deflect this debate into the realm of genetics, the evidence being presented is primarily inferential.71 On the contrary, as noted by Gravlee and Mulligan, genetic inferences require genetic data.72 In contrast, Dorothy Roberts, (JD and Kirkland & Ellis Professor, Northwestern University Law School Department of African-American Studies and Sociology) points to more than one hundred scientific studies documenting the adverse effects of racial discrimination on health, with chronic exposure to stress, segregation in unhealthy neighborhoods, and transgenerational transmission of harm via fetal exposures serving to augment the consequences of low socioeconomic status.71,73-77 She concludes that both government and business have failed to develop adequate and high quality healthcare resources for Africans, concluding that the observed inequalities are not simply bad luck: “Blacks and other minorities are systematically denied access to equal treatment and exposed to conditions that are harmful to their health.”78
In other words, the US today is not far removed from Alabama of the 1930’s. It is still engaged in social experimentation based on laws and policies that systematically expose African Americans and other vulnerable populations to social conditions and healthcare which are beyond the borders prescribed by the best available medical evidence.
Where is the PHS? Certainly it is no longer magnifying unjust social protocols to formulate medical experiments as it did in the 1930’s, but neither is it bringing the full weight of medical public health inquiry to bear by challenging unjust laws and policies. Instead, it is acquiescing to what may be the most unjust law of all, namely the so-called “Anti-lobbying Act” and related legislation, including Section 503, Division F, Title V, FY 12 Consolidated Appropriations Act) interpreted in grant conditions by the US Centers for Disease Control and Prevention79) as follows:
“No part of any appropriation contained in this Act…shall be used to pay the salary or expenses of any grant or contract recipient, or agent acting for such recipient, related to any activity designed to influence the enactment of legislation, appropriations, regulation, administrative action, or Executive order proposed or pending before the Congress or any State government, State legislature or local legislature or legislative body, other than for normal and recognized executive-legislative relationships or participation by an agency or officer of a State, local or tribal government in policymaking and administrative processes within the executive branch of that government…The prohibitions…shall include any activity to advocate or promote any proposed, pending or future Federal, State or local tax increase, or any proposed, pending, or future requirement or restriction on any legal consumer product, including its sale or marketing, including but not limited to the advocacy or promotion of gun control.
Further, this law is supported by modern day bioethics as noted by the United States National Institutes of Health Ethics Program80 “normal and recognized executive-legislative relationships” refers to use of funds to support Administration and Department positions in that employees are permitted to:
“communicate through normal channels with Members of Congress and State and local officials and their staffs in support of Administration or Department positions…
communicate with the public through public speeches, appearances and published writings to support Administration positions….
communicate privately with members of the public to inform them of Administration positions and to promote those positions -- but only to the extent that such communications do not involve the prohibited activities listed above.
lobby Congress or the public to support Administration positions on nominations.”
In other words, PHS employees and grantees may parrot Administration positions, but may not address, “any proposed, pending or future Federal, State or local tax increase, or any proposed, pending, or future requirement or restriction on any legal consumer product.” Since the environmental conditions leading to social inequality are almost inevitably bound to “consumer products”, this is clearly intended to silence scientific challenges to potentially unjust social experiments engendered by unjust laws and policies, present or future.
The reference to “gun control” in the CDC document79 is particularly pointed Specifically, in a 1996 action the Congress of the United States instructed the PHS to consider only the descriptive data put forth by academic gun advocates against gun control. Such data are useful to formulate but not test hypotheses.81 Some of the same gun advocates, publishing in the Harvard Journal of Law and Policy (2005), theorized that homicide is more frequent among African Americans, in part, because socially aberrant behavior is more frequent.3 The PHS has acquiesced to the Congressional ban66 although an extensive review by the US Task Force for Community Preventive Services stated that, “Current evidence is inconsistent and, in general, methodologically inadequate, based on Task Force standards, to draw conclusions about causal effects. Moreover, even if findings were clear, the design of index studies conducted to date would not allow us to specify which firearms laws did or did not contribute to the reduction of violence. Additional research is needed to determine the relationship(s) between specific types and degree of firearms regulation and the rates of specified types of violence in given jurisdictions.”82 The PHS, however, is banned from such research. Within three years of the Congressional action, downward trends in homicide mortality from firearm among African American males and females between 15 and 34 years of age came to a halt and remained stagnant for at least a decade.83 Disparities affecting Hispanic white males relative to non-Hispanic white males also remained stable.83 None of this has mattered to legislators any more than the aforementioned evidence concerning primary seat belt law and fatal traffic crashes.
Table 3 summarizes the evolution of legally mandated human experiments from Tuskegee to Tuskegee Redux. We suggest that the fundamental structure of Tuskegee experiment – legally mandated decisions which systematically expose African Americans (and now other minority groups) to conditions outside the boundaries of the best medical evidence – has been preserved through continuing and legally anointed social experiments which are either clearly or possibly unethical and to which the PHS remains partnered. PHS acquiescence puts it outside the boundaries of medical evidence; outside the boundaries of the ethical values of autonomy, justice, beneficence, non-maleficence, caring and solidarity; and outside of medicine itself. As for public health law, the words of the Reverend Martin Luther King Jr. are just as relevant today than they were when he wrote them from jail in Birmingham, Alabama: ”… there are two types of laws: just and unjust. I would be the first to advocate obeying just laws. One has not only a legal but a moral responsibility to obey just laws. Conversely, one has a moral responsibility to disobey unjust laws. I would agree with St. Augustine that ‘an unjust law is no law at all.’”84
Table 3. PATTERNS AND EVOLUTION OF LEGALLY MANDATED HUMAN EXPERIMENTS: FROM TUSKEGEE TO TUSKEGEE REDUX.
| TUSKEGEE | |||||
|---|---|---|---|---|---|
| LEGAL REJECTION OF MEDICAL EVIDENCE |
LEGALLY MANDATED HUMAN SUBJECT RESEARCH |
LEGAL PLACEMENT OF BLACKS IN THE HIGH RISK EXPERIMENTAL CONDITION |
PUBLIC HEALTH COLLABORA- TION WITH LEGAL MANDATE |
ADVERSE OUTCOMES TO BLACKS |
CURRENT STATUS |
|
Venereal Disease Control Act: Permitted human experimenta- tion to withhold individual and public health treatment for syphilis among African American men even if medical evidence suggested the possibility that treatment could help.(Roy). |
PHS Syphilis Study at Tuskegee: Natural History of Syphilis in the untreated African American male; lack of treatment included interference with partner notification |
Blacks=High Risk Condition: No individual treatment or Public Health care (contact tracing) for Syphilis. Whites= Usual Risk Condition:Usual Individual and Public Health Care for Syphilis |
Active: design and execution of PHS Syphilis Study |
Study Men: Syphilis Untreated Female Partners/Babies Affected by Study Men: Contact notification blocked; women and babies infected |
Unethical medical experiments no longer legal. Freedom of lawmakers to establish social experiments by passing laws which ignore medical evidence preserved. |
| TUSKEGEE REDUX | |||||
|---|---|---|---|---|---|
| LEGAL REJECTION OF MEDICAL EVIDENCE (Cancer- related) |
LEGALLY MANDATED HUMAN EXPERIMENT |
LEGAL PLACEMENT OF BLACKS IN THE HIGH RISK EXPERIMENTAL CONDITION |
PUBLIC HEALTH COLLABORA- TION WITH LEGAL MANDATE |
POSSIBLE ADVERSE OUTCOMES TO BLACKS |
CURRENT STATUS |
| 23 states and the District of Columbia outlawed HIV contact tracing by name despite medical evidence that this is the best practice for control of sexually transmitted disease. These stats also ignored corroborating medical evidence that partner notification was inadequate for partner protection. |
Female partners of men who have sex with men were not notified by public health agencies in states which outlawed HIV contact tracing by name (= human experiment since people were systematically placed in a condition outside the boundaries of best medical practice) and were notified by public health agencies in states where contact tracing was allowed. |
Black Women=High Risk Experimental Condition ---known to have greater risk of exposure to men who have sex with men than white women White Women=Low Risk Experimental Condition --known to have lower risk of exposure to men who have sex with men |
Silent Partnership: Acquiescence to laws placing black women in high risk experimental condition. |
Increased mortality from HIV in states outlawing HIV contact tracing by name during the time period when HIV contact tracing by name was outlawed; no excess mortality after laws outlawing HIV contact tracing by name were overturned |
Named HIV contact identification is part of public health practice. |
|
Medicare definition of medical assistance limited to reimbursement of providers for screening mammography despite public health medical evidence that blacks that blacks are more likely to face non-cash barriers to service acquisition |
Acquisition of screening mammography by those with additional barriers to service acquisition versus Acquisition of screening mammography by persons for whom provider reimbursement is the primary barrier versus (= Human experiment since medical evidence does not recommend restriction of screening mammography to those with fewer barriers to service acquisition). |
Black women=High Risk Condition --known to have greater non-cash barriers to acquisition of screening mammography services White women=Low Risk Condition (known to have fewer non-cash barriers to acquisition of screening mammography) |
Silent partnership: Limited surveillance and no challenge to Medicare per terms of Anti- lobbying law |
Increased rate of diffusion of screening mammography services to White Medicare beneficiaries throughout most of the US |
No change. |
We believe that the proper role of public health medicine, in part, is to question, describe, and analyze outcomes and to formulate interventions based on a sufficient totality of medical evidence. Lawmakers are not bound to heed the advice that arises from such activities, but if public health is to remain part of medicine’s ethical sphere, it must have the charge and the capacity to continuously and independently evaluate the health consequences of laws and policies which lawmakers decide to enact. However unintentional, if the consequences of laws bring selective and remediable harm to members of the public, PHS workers must have the authority to bring this to the attention of those affected, to advocate for change – including change in laws -- and to develop and test other alternative approaches. The history of Tuskegee includes a tragic episode in which PHS Syphilis Study investigators became open and vocal partners in an unjust social experiment. By acquiescing to anti-lobbying law, PHS workers of today may become silent partners of a similar sort.
Acknowledgments
Sources of funding: “Funding for this activity was made possible (in part) by grants3P20MD000516-07S2 and 3S21MD000104 -11S1 from the National Center on Minority Health and Health Disparities (NIH). The views expressed do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention by trade names, commercial practices, or organizations imply endorsement by the U.S. Government.”
Footnotes
Disclaimers: The authors have no conflicts of interest or previous publications on this research project to declare.
References
- 1.Amdur R, Bankert EA. Institutional Review Board: Member Handbook. Third Edition Jones and Bartlett Publishers; Sudbury, MA: 2011. p. 47. [Google Scholar]
- 2.Guide to Community Preventive Services . Use of Safety Belts: Primary (vs. Secondary) Enforcement. Centers for Disease Control and Prevention; [Accessed: 07/23/2012]. www.thecommunityguide.org/cancer/screening/client-oriented/reminders.html. [Google Scholar]
- 3.Briggs NC, Schlundt DG, Levine RS, Goldzweig IA, Stinson N, Jr., Warren RC. Seat belt law enforcement and racial disparities in seat belt use. Am J Prev Med. 2006;31(2):135–141. doi: 10.1016/j.amepre.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 4.Briggs NC, Schlundt DG, Levine RS, Goldzweig IA, Stinson N, Jr, Warren RC. Seatbelt use among Hispanic ethnic subgroups of National origin. Inj Prev. 2006;12:421–6. doi: 10.1136/ip.2006.012435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anonymous [Accessed July 19, 2012];Safety belt and child restraint laws. 2012 Jul; Available at URL: http://www.iihs.org/laws/mapbeltenforcement.aspx.
- 6.Moseley KL, Kershaw DB. African American and white disparities in pediatric kidney transplantation in the United States - unfortunate or unjust? Camb Q Healthc Ethics. 2012 Jul;21(3):353–65. doi: 10.1017/S0963180112000072. [DOI] [PubMed] [Google Scholar]
- 7.Byrd WM, Clayton LA. Race, medicine and health care in the United States: A historical survey. JNMA. 2001;93(3 Suppl):11S–34S. [PMC free article] [PubMed] [Google Scholar]
- 8.Novkov J. [Accessed July 23, 2012];Segregation (Jim Crow) Encyclopedia of Alabama. Available at URL: http://www.encyclopediaofalabama.org/face/Article.jsp?id=h-1248 legal basis for) Published July 23, 2007. Last updated March 8, 2011.
- 9.Ward TJ., Jr. [Accessed July 29, 2012];Health care. The Jim Crow Encyclopedia. Available at URL: http://testaae.greenwood.com/doc_print.aspx?fileID=GR4181&chapterID=GR4181-3616&path=encyclopedias/greenwood.
- 10.Ward TJ., Jr. [Accessed July 29, 2012];Black hospital movement in Alabama. Encyclopedia of Alabama. Available at URL: http://encyclopediaofalabama.org/face/Article.jsp?id=h-2410. [Google Scholar]
- 11.Moore JE, Keidel A. The treatment of early syphilis. I. A plan of treatment for routine use. Bull Johns Hopkins Hosp. 1926;39:1–55. [Google Scholar]
- 12.Kampmeier RH. The Tuskegee study of untreated syphilis. In: Reverby SM, editor. Tuskegee’s Truths: Rethinking the Tuskegee syphilis study. University of North Carolina Press; Chapel Hill: 2000. pp. 193–201. [Google Scholar]
- 13.Vonderlehr RA, Clark T, Wenger OC, Heller JR., Jr. Untreated syphilis in the male Negro: A comparative study of treated and untreated cases. JAMA. 1936;107 [Google Scholar]
- 14.Flynt W. [Accessed July 23, 2012];Poverty in Alabama. Encyclopedia of Alabama. Available at URL: http://www.encyclopediaofalabama.org/face/Article.jsp?id=h-1387 Published November 6, 2007. Last updated September 8, 2011.
- 15.Stone JR. Elderly and older racial/ethnic minority healthcare inequalities: Care, solidarity and action. Cambr Quart Healthc Ethics. 2012;21:342–52. doi: 10.1017/S0963180112000060. [DOI] [PubMed] [Google Scholar]
- 16.Stone JR. Elderly and older racial/ethnic minority healthcare inequalities: Care, solidarity and action. Cambr Quart Healthc Ethics. 2012;21:344. doi: 10.1017/S0963180112000060. [DOI] [PubMed] [Google Scholar]
- 17.Stone JR. Elderly and older racial/ethnic minority healthcare inequalities: Care, solidarity and action. Cambr Quart Healthc Ethics. 2012;21:346. doi: 10.1017/S0963180112000060. [DOI] [PubMed] [Google Scholar]
- 18.Roy B. The Tuskegee syphilis experiment: Biotechnology and the administrative state. JNMA. 1995;87:56–67. Reprinted in Reverby SM, Editor. Tuskegee’s truths: Rethinking the Tuskegee syphilis study. Chapel Hill: University of North Carolina Press. 2000. Pp.299-317. [PMC free article] [PubMed] [Google Scholar]
- 19.Reverby SM. Introduction. More than a metaphor: An overview of the scholarship of the study. In: Reverby SM, editor. Tuskegee’s Truths: Rethinking the Tuskegee syphilis study. University of North Carolina Press; Chapel Hill: 2000. pp. 1–11. [Google Scholar]
- 20.Beauchamp TL, Childress JF. Principles of Bioethics. Oxford University Press; New York: 2001. [Google Scholar]
- 21.National Cancer Institute Fact Sheet [Accessed March 4, 2012];HIV infection and cancer risk. Available at URL: http://www.cancer.gov/cancertopics/factsheet/Risk/hiv-infection.
- 22.Centers for Disease Control and Prevention, National Center for Health Statistics Compressed Mortality File 1979-1998. CDC WONDER On-line Database, compiled from Compressed Mortality File CMF 1968-1988, Series 20, No. 2A, 2000 and CMF 1989-1998, Series 20, No. 2E, 2003. Accessed at http://wonder.cdc.gov/cmf-icd9.html on Mar 4, 2012 6:07:25 PM.
- 23.Centers for Disease Control and Prevention, National Center for Health Statistics Compressed Mortality File 1999-2008. CDC WONDER Online Database, compiled from Compressed Mortality File 1999-2008 Series 20 No. 2N 2011. Accessed at http://wonder.cdc.gov/cmf-icd10.html on Mar 4, 2012 6:15:06 PM.
- 24.Kaiser Family Facts [Accessed March 4, 2012];State Health Facts. Available at URL: http://www.statehealthfacts.org/comparemaptable.jsp?ind=559&cat=11&sub=128&yr=201&typ=5.
- 25.Anon [Accessed July 23, 2012];Breast Cancer Screening. United States Preventive Services Task Force Recommendations. Available at URL: http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrca.htm Current as of July 2010.
- 26.Smith-Bindman R, Miglioretti DL, Lurie N, Abraham L, Barbash RB, Strzelczyk J, Dignan M, Barlow WE, Beasley CM, Kerlikowske K. Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Ann Intern Med. 2006 Apr 18;144(8):541–53. doi: 10.7326/0003-4819-144-8-200604180-00004. [DOI] [PubMed] [Google Scholar]
- 27.Geraghty EM, Balsbaugh T, Nuovo J, Tandon S. Using Geographic Information Systems (GIS) to assess outcome disparities in patients with type 2 diabetes and hyperlipidemia. J Am Board Fam Med. 2010 Jan-Feb;23(1):88–96. doi: 10.3122/jabfm.2010.01.090149. [DOI] [PubMed] [Google Scholar]
- 28.Anselin Luc, Syabri Ibnu, Kho Youngihn. GeoDa: An Introduction to Spatial Data Analysis. Geographical Analysis. 2006;38(1):5–22. [Google Scholar]
- 29.Armitage P, Berry G, Matthews JNS., III . Statistical Methods in Medical Research. 4th Edition Blackwell Science, Inc; Malden, MA: 2002. [Google Scholar]
- 30.Reverby S. The Infamous Syphilis Study and Its Legacy: Examining Tuskegee. University of North Carolina Press; Chapel Hill, NC: 2009. [Google Scholar]
- 31.Heintzelman CA. [Accessed March 4, 2012];The Tuskegee syphilis study and its implications for the 21st century. The New Social Worker. 2003 10(4) Located at URL: http://www.socialworker.com/tuskegee.htm and accessable via Google search for “Heintzelman CA. The Tuskegee syphilis study and its implications for the 21st century.”. [Google Scholar]
- 32.WHO Syphilis Study Commission . Venereal-disease control in the USA. World Health Org.; 1950. Techn. Rep. Ser. 15. [Google Scholar]
- 33.Yoon CK. Families emerge as silent victims. In: Reverby SM, editor. Tuskegee’s Truths Rethinking the Tuskegee Syphilis Study. The University of North Carolina Press; Chapel Hill, NC: 2000. pp. 457–60. [Google Scholar]
- 34.Reverby SM. Escaping melodramas: Rethinking the U.S. Public Health Service “infamous” studies in Tuskegee and Guatemala. S.S. Kresge Learning Resource Center Lecture Hall 3. Meharry Medical College; Nashville, TN: Feb 29, 2012. Tuskegee Study. [Google Scholar]
- 35.Brandt AM. No magic bullet – a social history of venereal disease in the United State since 1880. Oxford University Press; New York: 1987. Expanded Edition. [Google Scholar]
- 36.Cowan FM, French R, Johnson AM. The role and effectiveness of partner notification in STD control: A review. Genitourin Med. 1996;721:247–52. doi: 10.1136/sti.72.4.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rutherford GW, Woo JM. Contact tracing and the control of human immunodeficiency virus infection. JAMA. 1988 Jun 24;259(24):3609–10. [PubMed] [Google Scholar]
- 38.Wigfield AS. 27 years of uninterrupted contact tracing: The ‘Tyneside Scheme’. Brit J Vener Dis. 1972;48:37–50. doi: 10.1136/sti.48.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guide to Community Preventive Services [Accessed February 2012];Interventions to identify HIV-positive people through partner counseling and referral services. Available at URL: www.thecommunityguide.org/hiv/partnercounseling.html. Last updated: 12/22/2011;
- 40.Heyman D, editor. Control of Communicable Diseases Manual. 18th Edition American Public Health Association; Washington, DC: 2004. [Google Scholar]
- 41.Becker MS, Joseph JG. AIDS and behavior change to reduce risk: A review. Am J Public Health. 1988;78:394–410. doi: 10.2105/ajph.78.4.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Becker MH, Joseph JG. AIDS and behavior change. Pub Health Rev. 1988;16:1–11. [PubMed] [Google Scholar]
- 43.Brandt AM. AIDS in historical perspective: Four lessons from the history of sexually transmitted diseases. Am J Public Health. 1988;78:367–71. doi: 10.2105/ajph.78.4.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marks G, Richardson JL, Maldonado N. Self-disclosure of HIV infection to sexual partners. Am J Public Health. 1991;81:1321–3. doi: 10.2105/ajph.81.10.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Landis, et al. NEJM. McCusker J, Stoddard AM, McCarthy E. The validity of self-reported HIV antibody test results. Am J Public Health. 82:567–9. doi: 10.2105/ajph.82.4.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smereck GAD. Contact tracing for HIV infection: Policy and program implications from a 50-state survey. In: Fisher DG, Needle R, editors. AIDS and Community-Based Drug Intervention Programs: Evaluation and Outreach. The Haworth Press, Inc; New York: pp. 41–52. [Google Scholar]
- 47.Tarasoff v Regents of University of California, 131 Cal. Rptr. 14, 551 P.2d 334 (Calif. 1976) + Sm.
- 48.Joseph SJ. Dragon within the gates: The once and future AIDS epidemic. Carroll and Graf.; New York: 1992. [Google Scholar]
- 49.Joseph SJ. Towards an urban HIV policy. Bull NY Acad Med. 1993 Summer;70(1):37–49. [PMC free article] [PubMed] [Google Scholar]
- 50.Gay Men’s Health Crisis . The Body. Mar 12, 1999. GMHC opposes New York state health department’s draft regulations on partner notification. [Google Scholar]
- 51.American Civil Liberties Union [Accessed February 14, 2012];HIV Partner Notification: Why coercion won’t work. Available at URL: http://www.aclu.org/lgbt-rights_hiv-aids/hiv-partner-notification-why-coercion-won’t-work.
- 52.Bell A, Wineberg M. Homosexualities: A study of diversity in men and women. Simon and Shuster; New York: 1978. [Google Scholar]
- 53.Selik RM, Castro KG, Pappaioanou M. Racial/ethnic differences in the risk of AIDS in the United States. Am J Public Health. 1988;78:1539–45. doi: 10.2105/ajph.78.12.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Millett G, Malebranche D, Mason B, Spikes P. Focusing “down low”: Bisexual black men, HIV risk, and heterosexual transmission. J Nat Med Assoc. 2005;97(7):52S–59S. [PMC free article] [PubMed] [Google Scholar]
- 55.Chu SY, Peterman TA, Doll LS, Buehler JW, Curran JW. AIDS in bisexual men in the United States: Epidemiology and transmission to women. Am J Public Health. 1992;82:220–4. doi: 10.2105/ajph.82.2.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Padian NS. Female partners of bisexual men; Paper presented at the CDC Workshop on Bisexuality and AIDS; Atlanta, GA. October, 1989. [Google Scholar]
- 57.Hennekens CH, Buring JE. In: Epidemiology in Medicine. Mayrent SL, editor. Little, Brown & Co.; Boston, MA: 1987. [Google Scholar]
- 58.Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. Vital Health Stat. 1999 Sep;2(128):1–13. [PubMed] [Google Scholar]
- 59.Smith DB. The politics of racial disparities: Desegregating the hospitals in Jackson, Mississippi. The Milbank Quarterly. 2005;83(2):247–69. doi: 10.1111/j.1468-0009.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Finkelstein A, McKnight R. What Did Medicare Do? The Initial Impact of Medicare on Mortality and Out of Pocket Medical Spending. Journal of Public Economics. 2008;92:1644–1669. [Google Scholar]
- 61.Uhrig JD, Bann CM, McCormack LA, Rudolph N. Beneficiary knowledge of original Medicare and Medicare managed care. Med Care. 2006 Nov;44(11):1020–9. doi: 10.1097/01.mlr.0000228019.47200.f2. [DOI] [PubMed] [Google Scholar]
- 62.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997 Sep;87(9):1491–8. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Levine RS, Foster JE, Fullilove RE, Fullilove MT, Briggs NT, Hull PC, Husaini BA, Hennekens CH. Black-white inequalities in mortality and life-expectancy, 1933-1999: Implications for Healthy People 2010. Pub Health Rep. 116:474–483. doi: 10.1093/phr/116.5.474. US Bureau of the Census. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Historical Statistics of the United States From Colonial Times to 1970. US Government Printing Office; Washington: 1975. [Google Scholar]
- 65.Mechanic D. Disadvantage, inequality and social policy. Health Affairs. 2002;21(2):48–59. doi: 10.1377/hlthaff.21.2.48. [DOI] [PubMed] [Google Scholar]
- 66.Levine RS, Goldzweig I, Kilbourne B, Juarez P. Firearms, youth homicide, and public health. J Health Care Poor Underserved. 2012;23(1):7–19. doi: 10.1353/hpu.2012.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Drowos JC, Levine RS, Hennekens CH. Mortality among young black men: A new American tragedy. Amer J Med. 2013 doi: 10.1016/j.amjmed.2012.07.007. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 68.Levine RS, Rust G, Aliyu M, Pisu M, Zoorob R, Goldzweig I, Juarez P, Husaini B, Hennekens CH. United States Counties with low black male mortality rates. Amer J Med. 2012 doi: 10.1016/j.amjmed.2012.06.019. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Brawley OW. Is race really a negative prognostic factor for cancer? JNCI J Natl Cancer Inst. 2009;101(14):970–971. doi: 10.1093/jnci/djp185. [DOI] [PubMed] [Google Scholar]
- 70.Roberts D. Debating the cause of health disparities: Implications for bioethics and racial equality. Camb Quart Healthc Ethics. 2012;21:332–341. 333. doi: 10.1017/S0963180112000059. [DOI] [PubMed] [Google Scholar]
- 71.Roberts D. Debating the cause of health disparities: Implications for bioethics and racial equality. Camb Quart Healthc Ethics. 2012;21:332–341. doi: 10.1017/S0963180112000059. [DOI] [PubMed] [Google Scholar]
- 72.Gravlee CC, Mulligan CJ. Re: Racial Disparities in Cancer Survival Among Randomized Clinical Trials of the Southwest Oncology Group. J Natl Cancer Inst. 2010;102(4):280. doi: 10.1093/jnci/djp506. [DOI] [PubMed] [Google Scholar]
- 73.Gravlee CC. How race becomes biology: Embodiment of social inequality. Am J Phys Anthropol. 2009;139:49–57. doi: 10.1002/ajpa.20983. [DOI] [PubMed] [Google Scholar]
- 74.Barr DA. Health Disparities in the United States: Social Class, Race, Ethnicity, and Health. Johns Hopkins University Press; Baltimore, MD: 2008. [Google Scholar]
- 75.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. New Engl J Med. 2004;351:575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 76.Krieger N. The science and epidemiology of racism and health: Racial/ethnic categories, biological expressions of racism, and the embodiment of inequality— and ecosocial perspective. In: Whitmarsh I, Jones DS, editors. What’s the Use of Race? Modern Governance and the Biology of Difference. MIT Press; Cambridge, MA: 2010. pp. 225–255. [Google Scholar]
- 77.Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Roberts D. Debating the cause of health disparities: Implications for bioethics and racial equality. Camb Quart Healthc Ethics. 2012;21:332–341. 334. doi: 10.1017/S0963180112000059. [DOI] [PubMed] [Google Scholar]
- 79.Anon [Accessed July 24, 2012];CDC Implementation of Anti-Lobbying Provisions. Available at URL: http://changelabsolutions.org/sites/changelabsolutions.org/files/CDC%20Implementation%20of%20Anti-Lobbying%20Restrictions%20-%20June%202012.pdf.
- 80.Anon [Accessed July 24, 2012];Lobbying Activities. National Institutes of Health Ethics Program. Available at URL: http://ethics.od.nih.gov/topics/lobbying.htm.
- 81.Hennekens CH, DeMets D. Statistical association and causation: contributions of different types of evidence. JAMA. 2011;305(11):1134–5. doi: 10.1001/jama.2011.322. [DOI] [PubMed] [Google Scholar]
- 82.Hahn RA, Bilukha O, Crosby A, Fullilove MT, Liberman A, Moscicki E, Snyder S, Tuma F, Briss PA. Firearms laws and the reduction of violence: A systematic review. Am J Prev Med. 2005;28(2S1):40–71. doi: 10.1016/j.amepre.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 83.Centers for Disease Control and Prevention, National Center for Health Statistics Compressed Mortality File. 1979-1998 CDC WONDER On-line Database, compiled from Compressed Mortality File DMF 1968-1988, Series 20, No. 2A, 2000 and CMF1979-1988, Series 20, No. 2E, 2003. Accessed at http://wonder.cdc.gov/cmf-icd9.html on May 30, 2012 10:29:59 AM. [Google Scholar]
- 84.King MLK., Jr. “Letter from Birmingham Jail” in King MLK Jr. Why We Can’t Wait. Harper & Row; New York: 1964. [Google Scholar]