Abstract
The number of available liver grafts is not sufficient to meet the current demand. A significant number of patients succumb before they receive a liver graft. However, approximately 10% of marginal livers are considered unsuitable for donation and are discarded. Calculating the primary non-function probability for any given liver graft can be performed using prognostic tools, such as the Donor Risk Index and the Eurotransplant Donor Risk Index. On the other hand, mortality on the waiting list, which is sometimes more than 15% per year of enlistment, directly correlates with its size, the graft supply and the gravity of the potential recipients' clinical condition. Up to 30% of the potential recipients will never receive a graft.
The purpose of this invited commentary is to examine whether the literature supports the utilization of the marginal liver grafts that would otherwise be discarded. It appears that there is sufficient evidence in favor of the development of a "B-list" for potential liver graft recipients. It should comprise all of the candidates who were definitely removed from the primary waiting list or were never included. The potential "B-list" recipients should only be eligible to receive grafts that would otherwise be discarded, i.e., "B-livers". Enrollment in a "B-list" might not only increase the overall patient survival (enlisted and transplanted combined) but might also improve candidate quality of life by maintaining their hope for a cure.
Keywords: Liver transplantation, organ allocation, marginal grafts, waiting list, equity, utility
Background
It is well known that the number of available liver grafts is not sufficient to meet the current demand. For this reason, grafts are allocated according to the gravity of the clinical condition of the potential recipients, i.e., patients are transplanted according the principle of equity. Using the MELD score to prioritize the liver transplantation waiting listing follows this principle of equity1. However, due to the organ shortage, a significant number of patients succumb before they receive a liver graft2. Nonetheless, many marginal livers are considered unsuitable for donation and are not utilized, particularly during the last decade, because the percentage of older donors has increased significantly3. One wonders whether discarded grafts could be used under certain circumstances. Is there sufficient bibliographic evidence to support the utilization of the marginal liver grafts that would be otherwise discarded in patients who were withdrawn from the recipient list or were never included because they did not meet certain criteria? To answer this question, the definition of a marginal unusable liver graft needs to be clarified. In addition, specific criteria for adding and removing patients from the recipient list should be agreed upon. All patients not included on the primary list could then be added to a secondary waiting list, the "B-list", to receive an otherwise unusable but potentially life-saving liver graft.
Defining the marginal unusable graft
The definition of the extended criteria donor (ECD) is certainly different from that of the extended criteria graft (ECG). An ECD yields a liver graft that has an increased probability of primary non-function (PNF) when compared to a graft procured by an "ideal" donor, i.e., donors less than 40 years old who are hemodynamically stable with non-steatotic livers4. The incidence of PNF when a liver from an «ideal» donor is transplanted to the average recipient is 8.1%. For this reason, donors are characterized as ECDs under the following conditions: older than 65 years; hemodynamic instability; macrovesicular steatosis greater than 30%; serum sodium greater than 155 mEq/lt; γGT greater than 200 IU/lt; and more than 5 days in the ICU5-8. In addition, every donor that carries a transmittable disease is considered an ECD. Currently, under specific circumstances, patients with tumors of the central nervous system or the urogenital system, microbial infections (even meningitis) or HBV, HCV or HIV are acceptable donors5,9.
Every ECD graft is characterized as an ECG. In addition, grafts that are procured from non-ECDs may iatrogenically become ECGs. For example, livers with a cold ischemia time greater than 12 hours are considered ECGs10. Moreover, ECGs include all grafts with a warm ischemia time greater than 60 minutes11. In addition, all segmental grafts (LDLTx, SLTx) are characterized as ECGs because the incidence of PNF is 13%12. Finally, livers procured from non-heart-beating donors are considered ECGs because the incidence of PNF is more than 15%13.
The characterization of donated livers as ECGs is secondary to the increased probability of PNF in 75% of the cases, whereas in the remaining 25%, the characterization is due to the presence of a transmittable disease2. Because grafts with a transmittable viral disease can be transplanted into patients that already carry the disease and because bacterial infections or the aforementioned neoplasias are almost never (< 1%) transmitted to recipients5, the debate about the allocation of ECGs concerns only livers with an increased probability of PNF. Therefore, the prediction of the probability of PNF for an ECG is of paramount importance.
Calculating the PNF probability for any given liver graft can be performed using prognostic tools, such as the Donor Risk Index (DRI)14. The DRI is a loge number that is calculated by a multivariate equation and lies between 0.0 ("best" graft) and 2.8 ("worst" graft). The "ideal" donor DRI is 1.0. The variables in the equation include donor age and height and cold ischemia time. Using the DRI, the predicted survival of the "average" recipient in the USA can be calculated in relation to the quality of the received graft (Table 1). For example, the one-year survival rates of the «average» recipient in USA are 88%, 80% and 71% for transplanted liver DRIs of 1.0, 1.6 and 2.0, respectively14. Similar calculations can be made with another prognostic tool, the Eurotransplant DRI. This index utilizes all the parameters of DRI with the exception of height and race and the addition of latest serum GGT and rescue allocation. It is a prognostic tool which predicts the quality of a specific liver graft that is transplanted within the Eurotransplant region15.
Table 1. Prediction of the mean recipient survival (3 months, 12 months and 36 months) based on graft quality, as measured by the DRI14.
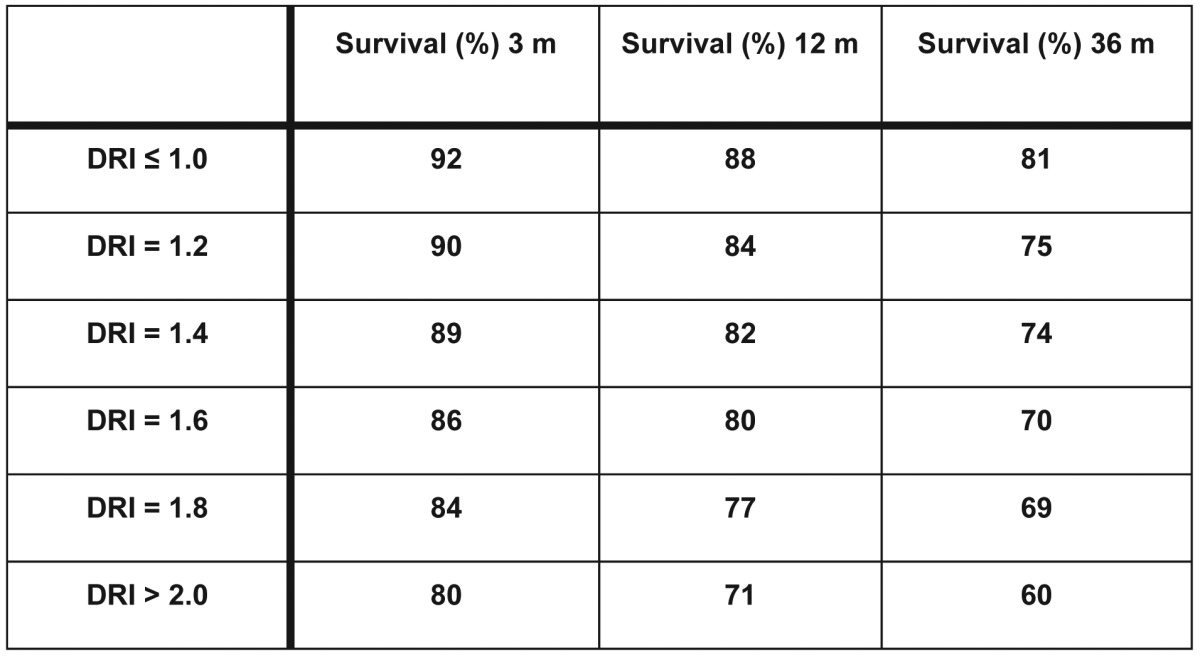
DRI: Donor Risk Index.
Approximately 20% of the donated livers are considered ECGs, and one out of three (7% of the total) is discarded2, primarily due to the fear of PNF. Indeed, the higher the DRI, the greater the chance that a donated liver will not be transplanted. For example, only 3.1% of grafts with a DRI = 1.0 are not transplanted, whereas one out of eight (12.5%) grafts with a DRI = 2.0 are not used2.
Reasons for withdrawal or non-enrollment on the liver transplant waiting list
The three most common reasons (other than receiving a transplant) for any potential liver recipient's withdrawal from the waiting list are: i) death while waiting; ii) significant deterioration of the clinical condition, which is typically reflected by a rise in the MELD score; and iii) for patients with hepatocellular cancer, an increase of the neoplastic load beyond the established criteria that the center follows (e.g., Milan, UCSF). In the last two cases, patients are withdrawn from the list (or primary non-enrollment) to maintain an average five-year liver recipient survival of at least 50%16.
Mortality on the list, while potential recipients are waiting for a graft, directly correlates with the size of the list, the graft supply and the gravity of the potential recipient's clinical condition. Approximately 15% of enlisted patients die every year while waiting for a liver transplant2.
A potential liver transplant recipient might be deemed too "sick" to transplant for one or more reasons. As far as the cardiovascular system is concerned, all transplant candidates with a coronary artery calcification index > 100 by coronary computed tomography should undergo a dobutamine stress echocardiogram. If the product of the equation 3.78 + 0.07*MELD - 0.05*MAHR (maximum achieved heart rate) exceeds zero, the candidate should be removed from the waiting list (or should not be enrolled, if it is the first evaluation). The incidence of serious intraoperative cardiovascular events for such a potential recipient is 47%17. Moreover, candidates with a mean pulmonary arterial pressure > 35 mmHg (under treatment) should be withdrawn from the list because their perioperative mortality exceeds 50%18. Regarding the respiratory system, when the potential recipient's pO2/FiO2 ratio is less than 100, 70% of the treating transplant physicians suggests removal from the list16. Finally, withdrawal from or non-enrollment on the liver transplant waiting list is justified when the candidate is of advanced age (> 70 years old), develops a serious infection, is greatly malnourished (> 20% of his body weight), continues to abuse substances or suffers from irreversible central nervous system damage19.
When a candidate's clinical condition deteriorates, his MELD score usually worsens. However, an increase in the MELD score alone, i.e., deterioration of the hepatic and/or renal function alone, without deterioration of any other system (e.g., cardiovascular, respiratory), should never lead to their removal from the list. A successful liver transplantation restores normal liver and, in most cases, renal function. Moreover, if renal function is unlikely to be restored after receiving a hepatic graft (i.e., estimated GFR constantly < 30 ml/min/1.73m2 for > 90 days), a combined liver/kidney transplant can be considered20. Although patients with higher MELD scores have a higher perioperative mortality rate, it needs to be stressed that these patients enjoy the highest survival benefit (up to 300 times) from liver transplantation (Table 2)21.
Table 2. Survival benefit (in days) for patients after liver transplantation when compared with candidates who are still waiting for a graft. Patients are stratified according to MELD score the day of operation (transplanted patients) or the day of enrollment (non-transplanted patients)21.
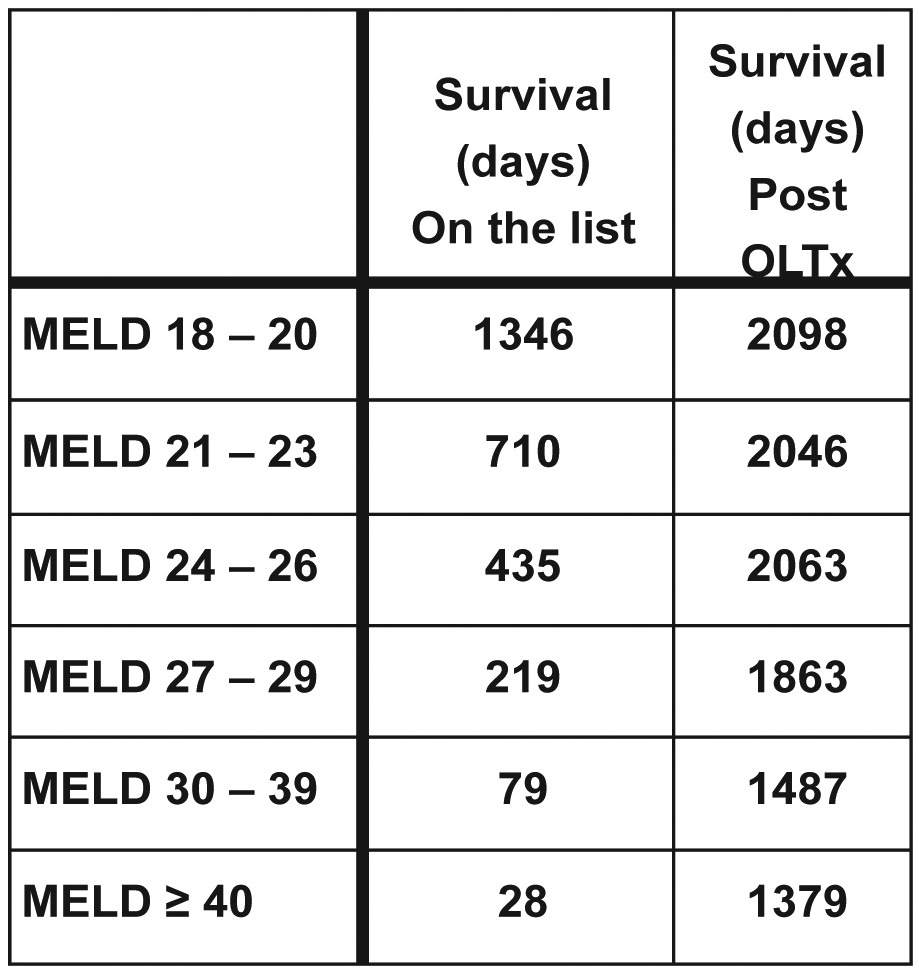
OLTx: Orthotopic Liver Transplantation.
The number of candidates with hepatocellular cancer that are removed from the waiting list (or not enrolled) due to increased tumor load, is dependent on the following: i) the transplantation criteria adopted by each specific center (e.g., Milan, UCSF), ii) the number of patients with hepatocellular cancer, iii) the size of the waiting list, iv) the gravity of the candidate's cirrhosis and v) the graft supply. Each year, approximately 25% of the potential recipients with hepatocellular cancer are removed from the waiting list due to increases in their neoplastic loads22.
Developing the "B-list" for liver transplant candidates
Based on the aforementioned facts and observations, it is clear that slightly less than 10% of donated livers are discarded. However, up to 30% of potential recipients will never receive a graft either because they succumb while waiting or because they are removed from the list. Of course, candidate removal from the waiting list invariably leads to their demise either due to the deterioration of liver function or secondary to the dissemination of hepatocellular cancer. Moreover, death is the only outcome for all of the patients not initially enrolled on the waiting list.
The "B-list" concept is simple. All potential candidates who were removed from the primary waiting list (the "A-list") or were not initially enlisted due to any medical reason should be placed on a secondary waiting list, the "B-list". The potential "B-list" recipients should be eligible to receive only livers that would otherwise be discarded, i.e., they would not be implanted into a patient on the primary waiting list ("B-livers"). Obtaining consent for a "B-liver" transplantation (a "B-liver" to a "B-list" recipient) should be a very detailed and lengthy process approved by the ethical committee of each transplantation center and should adhere to strict algorithms23. In this manner, no patient will stay off the list and almost no grafts will be discarded.
The development of the "B-list" will no doubt increase the average immediate postoperative mortality because patients and grafts of "poor quality" will lead to more complications. However, it will increase the cumulative survival of both the transplanted and the enlisted patients (intention to treat patients), i.e., it will increase the societal benefit. Indeed, the utilization of liver grafts of the lowest quality (DRI > 1.65) leads to an increased recipient survival, provided that they are transplanted to patients with a MELD score higher than 20 (Figure 1)24. In addition, the five-year survival rate after liver transplantation for hepatocellular cancer beyond any established criteria is 11%25.
Figure 1. The relative risk (RR) of death after liver transplantation with a low-quality graft (DRI > 1.65) compared to no transplantation, stratified according to patient MELD score. Liver transplantation with low-quality grafts is beneficial only when the recipient MELD score exceeds 20 (RR = 0.52)24. The RR for patients with MELD scores between 15 and 19 ranges from 0.65 to 0.83, but the 95% confidence intervals (CI) include 1.0 (CI not depicted for simplicity of the diagram). OLTx: Orthotopic Liver Transplantation.
Conclusion
The development of a "B-list" for liver transplant candidates will increase the overall patient survival (enlisted and transplanted combined) because patients without any chance of survival (those not included on the primary list) will have some probability of staying alive by receiving a "low-quality" liver graft, which until recently, was fully functional in the donor. In addition, if the initially discarded liver grafts are allocated according to some simple principles (e.g., recipients should have a MELD score higher than 20, HCV patients will be transplanted with organs from young donors26), survival will be even greater. Finally, enrollment of these gravely ill patients on some type of list (in this case a "B-list") maintains their hope for cure and improves their quality of life regardless of the liver transplant outcome.
Disclosures
This is an original article submitted as an invited commentary. This manuscript is not based on a previous communication. There were no sources of funding for this publication. There are no conflicts of interest for any of the authors.
References
- 1.Wiesner RH, McDiarmid SV, Kamath PS, Edwards EB, Malinchoc M, Kremers WK, et al. MELD and PELD: application of survival models to liver allocation. Liver Transpl. 2001;7:567–580. doi: 10.1053/jlts.2001.25879. [DOI] [PubMed] [Google Scholar]
- 2.Renz JF, Kin C, Kinkhabwala M, Jan D, Varadarajan R, Goldstein M, et al. Utilization of extended donor criteria liver allografts maximizes donor use and patient access to liver transplantation. Ann Surg. 2005;242:556–563. doi: 10.1097/01.sla.0000183973.49899.b1. discussion 563-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waki K. UNOS Liver Registry: ten year survivals. Clin Transpl. 2006:29–39. [PubMed] [Google Scholar]
- 4.Merion RM, Ashby VB, Wolfe RA, Distant DA, Hulbert-Shearon TE, Metzger RA, et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA. 2005;294:2726–2733. doi: 10.1001/jama.294.21.2726. [DOI] [PubMed] [Google Scholar]
- 5.Durand F, Renz JF, Alkofer B, Burra P, Clavien PA, Porte RJ, et al. Report of the Paris consensus meeting on expanded criteria donors in liver transplantation. Liver Transpl. 2008;14:1694–1701. doi: 10.1002/lt.21668. [DOI] [PubMed] [Google Scholar]
- 6.Figueras J, Busquets J, Grande L, Jaurrieta E, Perez-Ferreiroa J, Mir J, et al. The deleterious effect of donor high plasma sodium and extended preservation in liver transplantation. A multivariate analysis. Transplantation. 1996;61:410–413. doi: 10.1097/00007890-199602150-00016. [DOI] [PubMed] [Google Scholar]
- 7.Markmann JF, Markmann JW, Markmann DA, Bacquerizo A, Singer J, Holt CD, et al. Preoperative factors associated with outcome and their impact on resource use in 1148 consecutive primary liver transplants. Transplantation. 2001;72:1113–1122. doi: 10.1097/00007890-200109270-00023. [DOI] [PubMed] [Google Scholar]
- 8.Selzner M, Clavien PA. Fatty liver in liver transplantation and surgery. Semin Liver Dis. 2001;21:105–113. doi: 10.1055/s-2001-12933. [DOI] [PubMed] [Google Scholar]
- 9.Cerutti E, Stratta C, Romagnoli R, Serra R, Lepore M, Fop F, et al. Bacterial- and fungal-positive cultures in organ donors: clinical impact in liver transplantation. Liver Transpl. 2006;12:1253–1259. doi: 10.1002/lt.20811. [DOI] [PubMed] [Google Scholar]
- 10.Adam R, Cailliez V, Majno P, Karam V, McMaster P, Caine RY, et al. Normalised intrinsic mortality risk in liver transplantation: European Liver Transplant Registry study. Lancet. 2000;356:621–627. doi: 10.1016/s0140-6736(00)02603-9. [DOI] [PubMed] [Google Scholar]
- 11.Piratvisuth T, Tredger JM, Hayllar KA, Williams R. Contribution of true cold and rewarming ischemia times to factors determining outcome after orthotopic liver transplantation. Liver Transpl Surg. 1995;1:296–301. doi: 10.1002/lt.500010505. [DOI] [PubMed] [Google Scholar]
- 12.Olthoff KM, Merion RM, Ghobrial RM, Abecassis MM, Fair JH, Fisher RA, et al. Outcomes of 385 adult-to-adult living donor liver transplant recipients: a report from the A2ALL Consortium. Ann Surg. 2005;242:314–323. doi: 10.1097/01.sla.0000179646.37145.ef. www.oaml.com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abt PL, Desai NM, Crawford MD, Forman LM, Markmann JW, Olthoff KM, et al. Survival following liver transplantation from non-heart-beating donors. Ann Surg. 2004;239:87–92. doi: 10.1097/01.sla.0000103063.82181.2c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006;6:783–790. doi: 10.1111/j.1600-6143.2006.01242.x. [DOI] [PubMed] [Google Scholar]
- 15.Braat AE, Blok JJ, Putter H, Adam R, Burroughs AK, Rahmel AO, et al. The Eurotransplant Donor Risk Index in Liver Transplantation: ET-DRI. Am J Transplant. 2012;12:2789–2796. doi: 10.1111/j.1600-6143.2012.04195.x. [DOI] [PubMed] [Google Scholar]
- 16.Charpentier KP, Mavanur A. Removing patients from the liver transplant wait list: A survey of US liver transplant programs. Liver Transpl. 2008;14:303–307. doi: 10.1002/lt.21353. [DOI] [PubMed] [Google Scholar]
- 17.McAvoy NC, Kochar N, McKillop G, Newby DE, Hayes PC. Prevalence of coronary artery calcification in patients undergoing assessment for orthotopic liver transplantation. Liver Transpl. 2008;14:1725–1731. doi: 10.1002/lt.21540. [DOI] [PubMed] [Google Scholar]
- 18.Krowka MJ, Plevak DJ, Findlay JY, Rosen CB, Wiesner RH, Krom RA. Pulmonary hemodynamics and perioperative cardiopulmonary-related mortality in patients with portopulmonary hypertension undergoing liver transplantation. Liver Transpl. 2000;6:443–450. doi: 10.1053/jlts.2000.6356. [DOI] [PubMed] [Google Scholar]
- 19.Dawwas MF, Gimson AE. Candidate selection and organ allocation in liver transplantation. Semin Liver Dis. 2009;29:40–52. doi: 10.1055/s-0029-1192054. [DOI] [PubMed] [Google Scholar]
- 20.Ruebner R, Goldberg D, Abt PL, Bahirwani R, Levine M, Sawinski D, et al. Risk of end-stage renal disease among liver transplant recipients with pretransplant renal dysfunction. Am J Transplant. 2012;12:2958–2965. doi: 10.1111/j.1600-6143.2012.04177.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Merion RM. When is a patient too well and when is a patient too sick for a liver transplant? Liver Transpl. 2004;10:s69–s73. doi: 10.1002/lt.20265. [DOI] [PubMed] [Google Scholar]
- 22.Maddala YK, Stadheim L, Andrews JC, Burgart LJ, Rosen CB, Kremers WK, et al. Drop-out rates of patients with hepatocellular cancer listed for liver transplantation: outcome with chemoembolization. Liver Transpl. 2004;10:449–455. doi: 10.1002/lt.20099. [DOI] [PubMed] [Google Scholar]
- 23.Bruzzone P. A preliminary European study on extended-criteria liver donation and transplant recipient consent. Transplant Proc. 2012;44:1857–1858. doi: 10.1016/j.transproceed.2012.05.065. [DOI] [PubMed] [Google Scholar]
- 24.Schaubel DE, Sima CS, Goodrich NP, Feng S, Merion RM. The survival benefit of deceased donor liver transplantation as a function of candidate disease severity and donor quality. Am J Transplant. 2008;8:419–425. doi: 10.1111/j.1600-6143.2007.02086.x. [DOI] [PubMed] [Google Scholar]
- 25.Houben KW, McCall JL. Liver transplantation for hepatocellular carcinoma in patients without underlying liver disease: a systematic review. Liver Transpl Surg. 1999;5:91–95. doi: 10.1002/lt.500050201. [DOI] [PubMed] [Google Scholar]
- 26.Mutimer DJ, Gunson B, Chen J, Berenguer J, Neuhaus P, Castaing D, et al. Impact of donor age and year of transplantation on graft and patient survival following liver transplantation for hepatitis C virus. Transplantation. 2006;81:7–14. doi: 10.1097/01.tp.0000188619.30677.84. [DOI] [PubMed] [Google Scholar]



