Abstract
Natural killer T (NKT) cells are innate-like T cells that rapidly produce a variety of cytokines following T cell receptor (TCR) activation and can shape the immune response in many different settings. There are two main NKT cell subsets: type I NKT cells are typically characterized by the expression of a semi-invariant TCR, whereas the TCRs expressed by type II NKT cells are more diverse. This Review focuses on the defining features and emerging generalities regarding how NKT cells specifically recognize self, microbial and synthetic lipid-based antigens that are presented by CD1d. Such information is vitally important to better understand, and fully harness, the therapeutic potential of NKT cells.
T cells are usually viewed as being specific for peptide antigens that are presented on classical MHC molecules. However, many T cells actually respond to lipid-based antigens that are presented by the CD1 family of MHC-like molecules, which are typically expressed by professional antigen-presenting cells (APCs). The CD1 family is subdivided into at least three groups: group 1 comprises CD1a, CD1b and CD1c; group 2 comprises CD1d; and group 3 comprises CD1e1,2. The most extensively studied type of lipid-reactive T cell is the CD1d-restricted natural killer T (NKT) cell3 (FIG. 1a).
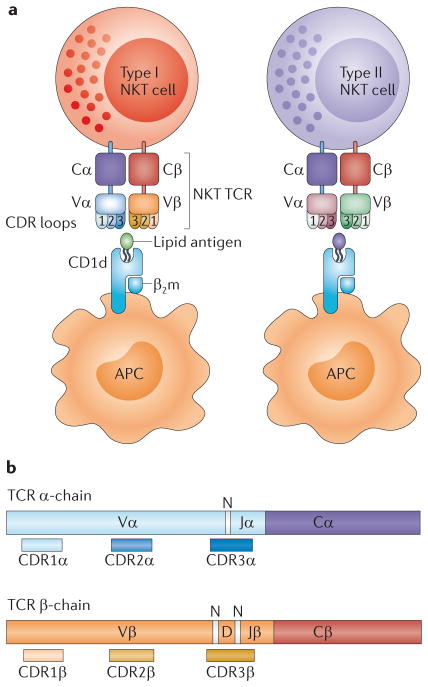
Figure 1. NKT cells.
a | The figure shows a schematic representation of type I and type II natural killer T (NKT) cells. These two subsets use different variable (V) region gene segments in the α- and β-chains of their T cell receptors (TCRs), and they recognize different CD1d-restricted antigens. b | The αβ TCR is composed of two chains, with the V domains containing the complementarity-determining region (CDR) loops. The CDR3 loops are encoded by multiple gene segments and also contain non-templated (N) regions, which add further diversity to the TCR repertoire. The colour coding is the same as that used for the type I NKT TCR in part a. β2m, β2-microglobulin; APC, antigen-presenting cell; C, constant; D, diversity; J, joining.
NKT cells are a specialized T cell subset that is functionally distinct from MHC-restricted T cells4. For example, NKT cells can rapidly produce very large amounts of cytokines — including interferon- γ(IFNγ), interleukin-4 (IL-4), IL-10, IL-13, IL-17, IL-21 and tumour necrosis factor (TNF) — following stimulation, and they are able to either promote or suppress cell-mediated immunity without the need for clonal expansion5,6. Thus, NKT cells can enhance the immune response to a range of infectious organisms, and some types of cancer, but can also suppress autoimmune disease, allograft rejection and graft-versus-host disease3. Consequently, NKT cells represent a potentially important immunotherapeutic target with widespread clinical potential7–9.
The interaction between the NKT cell antigen receptor — that is, the T cell receptor (TCR) expressed by NKT cells (referred to as the NKT TCR in this article) — and the antigen–CD1d complex represents a central event leading to NKT cell activation10. Since 2006, many studies on antigen recognition by NKT TCRs have helped us to begin to understand the factors that govern the antigenicity of a given ligand. Although CD1d is essentially monomorphic, it can bind to an array of lipid-based antigens, including synthetic, self and non-self antigens11–13. Uncovering the NKT cell stimulatory properties of these antigens, and the rules of engagement in the various NKT TCR–antigen–CD1d complexes, represents a key step in understanding NKT cell biology. This Review primarily focuses on how the various forms of type I NKT TCR function like ‘pattern-recognition receptors’ in engaging a variety of lipid-based antigens that exhibit diverse chemistries. We also highlight the contrasting ‘snapshot’ of type II NKT TCR-mediated antigen recognition, as well as the factors that govern the general principles of NKT cell-mediated antigen recognition and therapeutic implications.
NKT cell subsets
The αβ TCR is composed of an α-chain and a β-chain, with each chain being subdivided into a variable (V) domain and a constant (C) domain. In TCR α-chains, the V domains are encoded by V (TRAV) and joining (J; TRAJ) gene segments, whereas TCR β-chain V domains are encoded by V (TRBV), diversity (D; TRBD) and J (TRBJ) gene segments. Within the V domains, three complementarity-determining regions (CDRs) in each chain collectively form the antigen-binding site of the TCR. The CDR1 and CDR2 loops are encoded within the V gene segments, whereas the CDR3 loop is encoded at the junction of the rearranged V and J gene segments (for TCRα) or V, D and J gene segments (for TCRβ). The various permutations and combinations of V, D and J gene segments endow the CDR3 loops with the greatest diversity, which is further enhanced by random non-templated alterations at the V(D)J gene junctional boundaries (FIG. 1b).
Type I NKT cells
There are two main subsets of NKT cells, termed type I and type II NKT cells (FIG. 1). Type I NKT cells typically express an ‘invariant’ TCR α-chain (Vα24Jα18 (TRAV10–TRAJ18) in humans and the orthologous chain Vα14Jα18 (Trav11–Traj18) in mice), which is paired with a limited set of TCR β-chains (comprising Vβ11 (TRBV25-1) in humans and Vβ8.2 (Trbv13-2), Vβ7 (Trbv1) or Vβ2 (Trbv29) in mice)4,14–16. There is a high level of sequence identity in the CDR3α and CDR2β loops from human and mouse type I NKT TCRs16, which underpins the evolutionarily conserved reciprocal cross-species reactivity of these cells between mice and humans17–19. The importance of the CDR3α loop for NKT cell function is highlighted by the loss of most type I NKT cells in TCR Jα18 gene-targeted mice20, although studies on these mice may need to be revisited owing to a recent report that suggests that the diversity of the overall TCR repertoire is reduced in these mice21. As type I NKT cells typically express an invariant TCR α-chain, they are frequently referred to as ‘invariant’ NKT cells4. However, this is clearly a misnomer because NKT cells exhibit a high degree of natural variability in the CDR3β loop16,22,23. Thus, ‘semi-invariant’ is a more accurate, although still imperfect, description for type I NKT cells4.
Another parameter that is typically used to define type I NKT cells is their ability to recognize α-galactosylceramide (αGalCer)4. αGalCer — a glyco-lipid originally derived from the marine sponge Agelas mauritianus — was identified because of its potent antitumour effects in mice24. αGalCer is an important experimental tool, as it is the main ligand used for functional studies of type I NKT cells because physiological antigens are not as potent or as well characterized. The most commonly used form of αGalCer (also known as KRN7000) comprises an α-linked galactose head group and a ceramide base (consisting of an 18-carbon phytosphingosine chain and a 26-carbon acyl chain) (FIG. 2). Subsequently, αGalCer was shown to bind to human and mouse CD1d and potently activate type I NKT cells24–26.
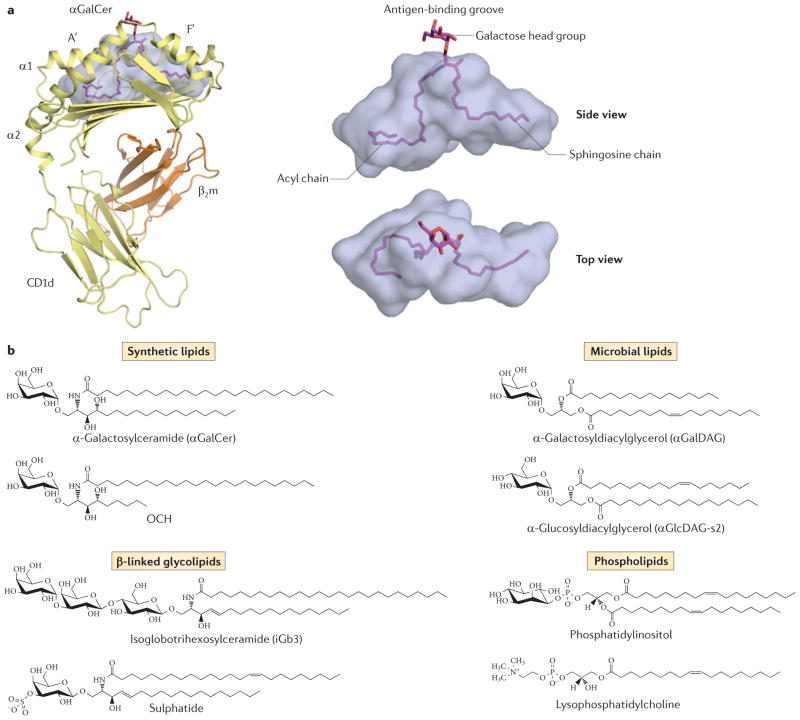
Figure 2. CD1d-mediated antigen presentation.
a | The figure shows the structure of human CD1d bound to α-galactosylceramide (αGalCer) (PDB code 1ZT4). αGalCer is positioned within the CD1d antigen-binding groove, which is characterized by two main pockets: the A′-pocket and the F′-pocket. The galactose head group is surface exposed, whereas the lipid tails are buried within the cavity. b | The figure shows the chemical structures of various lipid antigens that bind to CD1d. These include examples of synthetic lipids (αGalCer and OCH), microbial lipids (α-galactosyldiacylglycerol from Borrelia burgdorferi and α-glucosyldiacylcerol from Streptococcus pneumoniae), β-linked glycolipids (isoglobotrihexosylceramide and sulphatide) and phospholipids (phosphatidylinositol and lysophosphatidylcholine). β2m, β2-microglobulin.
Type II NKT cells
Type II NKT cells are CD1d-restricted T cells that lack the ‘semi-invariant’ TCR α-chain characteristic of type I NKT cells and do not recognize αGalCer4,27. Instead, type II NKT cells express a different and more diverse TCR repertoire than type I NKT cells. Although the antigen specificity of type II NKT cells is poorly understood, it includes antigens that are not generally considered to be agonists for type I NKT cells28–30. Currently, the most widely studied antigen for type II NKT cells is sulphatide, a sulphated glycolipid that is found abundantly in neuronal tissue and has been associated with the inhibition of experimental autoimmune encephalomyelitis by type II NKT cells28. Some biases in TCR chain usage have been described in type II NKT cells. For example, in mice, type II NKT cells appear to be enriched for particular TCR α-chain V segments (namely Vα3 and Vα8) and for Vβ8 (REF. 31). Furthermore, the TCRs of sulphatide-reactive type II NKT cells can have a more conserved CDR3β region than type I NKT TCRs30. Interestingly, a recent study of human sulphatide-reactive type II NKT cells suggested that this population includes some Vδ1+ γδ T cells32. The diversity of type II NKT cells highlights the fact that a great deal needs to be learnt about CD1d-restricted antigen specificity and recognition by type II NKT TCRs.
Atypical NKT cells
Not all NKT cells fit neatly into the current type I–type II NKT cell classification system. Although such atypical NKT cells represent a minor population of the entire NKT cell pool, they can exhibit distinct specificities33,34. For example, one atypical NKT cell subset in humans consists of Vα24−Jα18+Vβ11+ cells33–35. Another study examined αGalCer-reactive Vα24− NKT cell clones from healthy people and showed that, although many clones were enriched for Jα18 and Vβ11, others exhibited more diverse αβ TCR usage36. The recent characterization of Vα10+Jα50+Vβ8+ NKT cells provides a clear example of NKT cells that fall within this grey zone37. These NKT cells can respond to αGalCer–CD1d, but they show a greater reactivity to α-glucosylceramide (αGlcCer) and preferentially recognize a mycobacterial lipid known as α-glucuronosyldiacylglycerol37.
There may also be overlap between type I and type II NKT cell antigens. For example, the self antigen β-glucosylceramide (βGlcCer) is recognized by both subsets of NKT cells27,38,39. Thus, there seems to be a blurring of the boundaries regarding the classification, the antigen specificity and possibly the function of the various NKT cell subsets, and this overlap is likely to be determined, in part, by NKT TCR-mediated recognition. In order to properly understand the function and applications of NKT cells, we need to understand the TCR repertoire and associated antigen specificity of the different subsets of NKT cells.
Antigen presentation by CD1d
The first crystal structure of a CD1 family member, mouse CD1d, demonstrated that the CD1 family adopts an MHC class I-like fold with a hydrophobic antigen-binding cleft that has deep pockets ideally suited for binding lipid antigens40. Subsequently, the crystal structures of CD1a, CD1b, CD1c and CD1d have been determined with various lipid-based antigens bound41–45. In general, the CD1 binding cleft is characterized by two main pockets, the A′-pocket and the F′-pocket (FIG. 2a), which vary in shape and size between CD1 family members46–48. This variation, together with their distinct intracellular trafficking behaviour, enables each CD1 isoform to bind to a specific, albeit partly overlapping, repertoire of lipids46,49.
The determination of the structure of human CD1d and mouse CD1d in complex with αGalCer (or a closely related analogue)17,42,45 showed that the acyl chain of αGalCer is buried in the A′-pocket of CD1d and the phytosphingosine chain is buried in the F′-pocket. By contrast, the α-galactosyl head group protrudes from the cleft, such that it is directly available to make contact with the NKT TCR (FIG. 2a). The surface-exposed head group explains why NKT cell agonists include a chemically distinct range of synthetic, foreign and self antigens49,50 (FIG. 2b). These antigens can also vary in the nature of the linkage between the head group and the hydrophobic base region, and in the composition of their lipid tails13 (FIG. 2b). Such antigenic diversity poses many important questions, which have not been addressed fully. For instance: what determines an optimal NKT cell agonist? How do NKT cells discriminate between self and non-self antigens? Do antigen-specific subsets of NKT cells exist? Understanding the molecular basis of NKT TCR–antigen–CD1d interactions is central to addressing these fundamental questions.
Antigen recognition by type I NKT cells
The parallel universe of type I NKT TCR binding
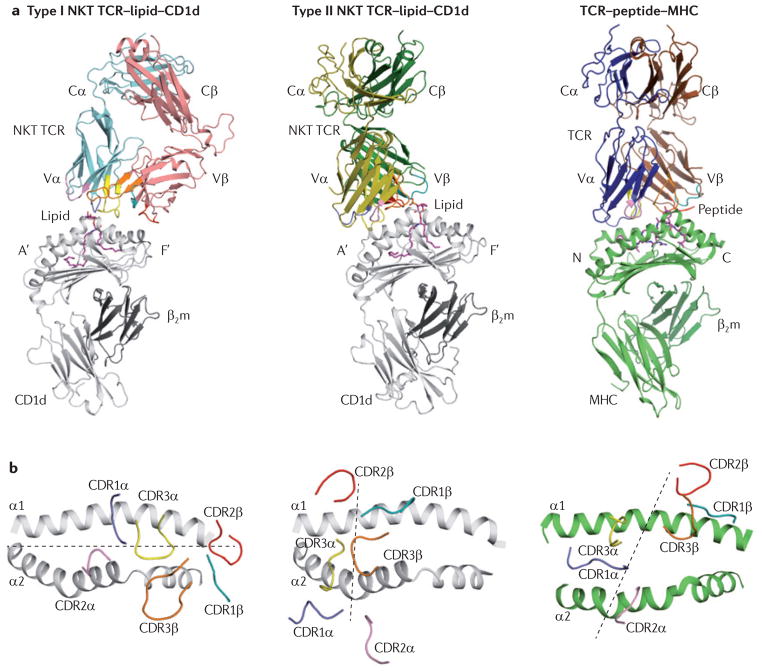
The fundamental principles underlying the NKT TCR– antigen–CD1d interaction were initially identified from the structure of the human type I Vα24–Vβ11 NKT TCR–αGalCer–CD1d complex51,52 (FIG. 3a). The NKT TCR is relatively rigid when binding to αGalCer–CD1d18,34,52, which exemplifies the innate-like characteristics of this interaction. Of interest, this type I NKT TCR ternary complex is remarkably different to all of the TCR–peptide–MHC class I structures that have been determined so far53,54 (FIG. 3a, b). Specifically, the human type I NKT TCR adopts a tilted and parallel docking mode over the F′-pocket of CD1d. Highlighting the highly conserved reactivity of type I NKT cells, an almost identical interaction was observed between the mouse type I Vα14–Vβ8.2 NKT TCR and αGalCer–CD1d55.
Figure 3. Structural comparison between NKT TCR–lipid–CD1d complexes and the conventional TCR–peptide–MHC complex.
a | The figure shows the docking mode of the T cell receptor (TCR) in a type I natural killer T (NKT) cell TCR–lipid–CD1d complex (left; PDB code 2PO6), a type II NKT TCR–lipid–CD1d complex (middle; PDB code 4EI5) and a TCR–peptide–MHC complex (right; PDB code 3SJV). The CD1d antigen-binding pockets are labelled A′ and F′, and the amino and carboxyl termini of the peptide are labelled N and C, respectively. b | The figure shows the view looking down into the antigen-binding groove of the three complexes showing the parallel docking mode in the type I NKT–lipid–CD1d complex (left), the orthogonal docking mode in the type II NKT–lipid–CD1d complex (middle) and the diagonal docking mode in the TCR–peptide–MHC complex (right). Dashed lines represent the docking mode. β2m, β2-microglobulin.
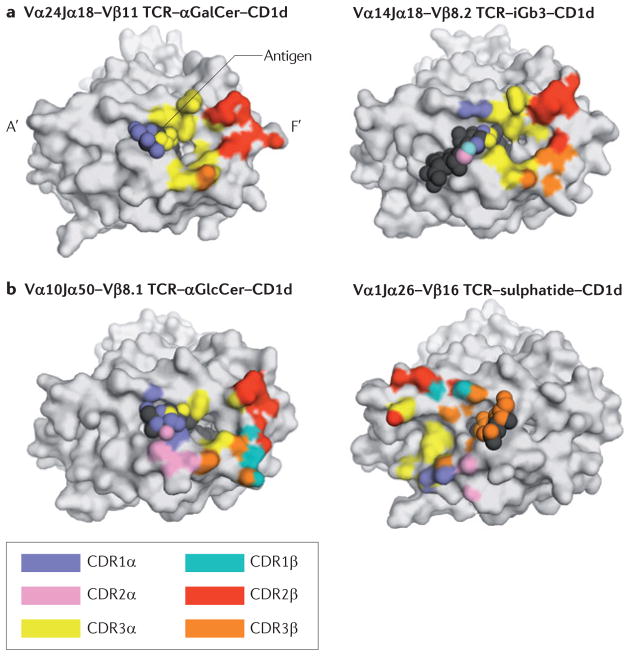
At the interface between the human type I Vα24–Vβ11 NKT TCR and αGalCer–CD1d, the CDR1α loop interacts with αGalCer, whereas the Jα18-encoded CDR3α loop contacts both CD1d and αGalCer52,55 (FIG. 4a). The intimate interactions between the invariant TCR α-chain and the galactose head group of αGalCer provide a basis for understanding the potency of this antigen in stimulating type I NKT cells (FIG. 4a). By contrast, the TCR β-chain interactions are dominated by two residues (Tyr48 and Tyr50) within the CDR2β loop, which contacts residues above the F′-pocket of CD1d52 (FIG. 4a). Although several residues within the CDR3α loop are important for binding, Leu99 seems to have a key role in modifying the CD1d interface. Specifically, this residue is inserted into the F′-pocket of CD1d, thereby forming a hydrophobic ‘roof’ that seems to be crucial for NKT TCR binding55–58. The energetic basis of the NKT TCR–antigen–CD1d interaction — as defined by residues that, when mutated, have a marked impact on the affinity of the interaction55,59–62 — underscores the importance of the CDR2β and CDR3α loops in driving the antigen–CD1d interaction.
Figure 4. The footprint of contact made by NKT TCRs on the surface of CD1d. a.
| The image on the left shows the footprint of the human type I natural killer T (NKT) cell Vα24Jα18–Vβ11 T cell receptor (TCR) on the surface of human CD1d, which is presenting an α-linked glycolipid, α-galactosylceramide (αGalCer) (PDB code 2PO6). The image on the right shows the footprint of the mouse type I NKT cell Vα14Jα18–Vβ8.2 TCR on the surface of mouse CD1d, which is presenting a β-linked glycolipid, isoglobotrihexosyl-ceramide (iGb3) (PDB code 3SCM). b | On the left is the footprint of the type I NKT cell Vα10Jα50–Vβ8.1 TCR on the surface of mouse CD1d, which is presenting α-glucosylceramide (αGlcCer) (PDB code 3RUG). On the right is the footprint of the mouse type II NKT cell Vα1Jα26–Vβ16 TCR on the surface of mouse CD1d, which is presenting a β-linked self glycolipid, sulphatide (PDB code 4EI5).
Modulation of TCR–CD1d interactions by the TCR α- and β-chains
All of the type I NKT TCR–antigen–CD1d structures elucidated so far have shown that the F′-pocket docking orientation is maintained, regardless of TCR α- and β-chain usage and the nature of the bound antigen10,63–65 (FIG. 4; TABLE 1). This reveals that the type I NKT TCR functions like a pattern- recognition receptor — that is, an innate-like, germline-encoded receptor that interacts in a conserved manner with its ligands. For example, in mouse type I NKT cells, TCRs containing Vβ8.2, Vβ7 or Vβ2 adopt the same docking mode55,62, despite sequence variation in the CDR2β loop52,55,62. Compensatory interactions are mediated by residues encoded within the respective Vβ gene segments of these NKT TCRs55,62,66. Furthermore, additional interactions are mediated by particular CDR3β loops that converge on a focal point within the a2 helix of CD1d62,67–70 (FIG. 4). This suggests a general mechanism pertaining to CD1d-dependent autoreactivity, as the CDR3β-mediated interaction does not involve direct contacts with the antigen itself.
Table 1.
Structures of NKT–TCR–lipid CD1d complexes
| Origin | Species | Lipid antigen | TCR α-chain | TCR β-chain | CDR3β sequence | PDB code | Refs |
|---|---|---|---|---|---|---|---|
| Type I NKT cell complexes | |||||||
| Synthetic lipids | Human | αGalCer | Vα24Jα18 | Vβ11 | CASSGLRDRGLYEQYF | 2PO6 | 52 |
| Human | αGalCer | Vα24Jα18 | Vβ11 | CASSGLRDRGLYEQYF | 3HUJ | 55 | |
| Human | αGalCer | Vα3.1Jα18 | Vβ11 | CASSENSGTGRIYEQYF | 4EN3 | 130 | |
| Mouse | αGalCer | Vα14Jα18 | Vβ8.2 | CASGDAGGNYAEQF | 3HE6 | 55 | |
| Mouse | αGalCer | Vα14Jα18 | Vβ7 | CASSSTGLDTQYF | 3HE7 | 55 | |
| Mouse | αGalCer | Vα14Jα18 | Vβ2 | CTSSADHWTNTGQLYF | 3TO4 | 62 | |
| Mouse | OCH | Vα14Jα18 | Vβ8.2 | CASGDAGGNYAEQF | 3ARB | 58 | |
| Mouse | C20:2 αGalCer | Vα14Jα18 | Vβ8.2 | CASGDAGGNYAEQF | 3ARF | 58 | |
| Mouse | 3′,4″-deoxy-αGalCer | Vα14Jα18 | Vβ8.2 | CASGDAGGNYAEQF | 3ARD | 58 | |
| Mouse | 4′,4″-deoxy-αGalCer | Vα14Jα18 | Vβ8.2 | CASGDAGGNYAEQF | 3ARE | 58 | |
| Mouse | αGlcCer | Vα14Jα18 | Vβ8.2 | CASGDAGGNYAEQF | 3ARG | 58 | |
| Mouse | α-C-GalCer | Vα14Jα18 | Vβ8.2 | CASGDAGGNYAEQF | 3TN0 | 75 | |
| Mouse | NU-αGalCer | Vα14Jα18 | Vβ8.2 | CASGDEGYTQYF | 3QUZ | 73 | |
| Mouse | α-C-GalCer | Vα14Jα18 | Vβ8.2 | CASGDEGYTQYF | 3QUX | 73 | |
| Mouse | BnNH-GSL-1′ | Vα14Jα18 | Vβ8.2 | CASGDEGYTQYF | 3QUY | 73 | |
| Mouse | SMC124 (a plakoside A analogue) | Vα14Jα18 | Vβ8.2 | CASGDEGYTQYF | 3TVM | 77 | |
| Mouse | HS44 (aminocyclitol) | Vα14Jα18 | Vβ8.2 | CASGDEGYTQYF | 3RTQ | 76 | |
| Mouse | αGlcCer | Vα10 Jα50 | Vβ8.1 | CASRLGGYEQYF | 3RUG | 37 | |
| Microbial lipids | Mouse | GalA-GSL | Vα14Jα18 | Vβ8.2 | CASGDEGYTQYF | 3O8X | 56 |
| Mouse | αGalDAG | Vα14Jα18 | Vβ8.2 | CASGDEGYTQYF | 3O9W | 56 | |
| Mouse | αGlcDAG-s2 | Vα14Jα18 | Vβ8.2 | CASGDEGYTQYF | 3TA3 | 57 | |
| Self lipids | Mouse | Phosphatidylinositol | Vα14Jα18 | Vβ6–Vβ8.2 hybrid | CASGSLLDVREVF | 3QI9 | 68 |
| Mouse | iGb3 | Vα14Jα18 | Vβ6–Vβ8.2 hybrid | CASGSLLDVREVF | 3SCM | 67 | |
| Mouse | βGalCer | Vα14Jα18 | Vβ6–Vβ8.2 hybrid | CASGSLLDVREVF | 3SDA | 67 | |
| Mouse | Gb3 | Vα14Jα18 | Vβ6–Vβ8.2 hybrid | CASGSLLDVREVF | 3SDC | 67 | |
| Mouse | βLacCer | Vα14Jα18 | Vβ6–Vβ8.2 hybrid | CASGSLLDVREVF | 3SDD | 67 | |
| Mouse | iGb3 | Vα14Jα18 | Vβ8.2 | CASGDEGYTQYF | 3RZC | 69 | |
| Human | Lysophosphatidylcholine | Vα24Jα18 | Vβ11 | CASSEEGALKESVGTQYF | 3TZV | 70 | |
| Human | βGalCer | Vα24Jα18 | Vβ11 | CASSEFGGTERTQETQYF | 3SDX | 67 | |
| Type II NKT cell complexes | |||||||
| Self lipids | Mouse | Sulphatide | Vα1 | Vβ16 | CASSFWGAYAEQFF | 4EI5 | 118 |
| Mouse | Lysosulphatide | Vα1 | Vβ16 | CASSFWGAYAEQFF | 4ELM | 119 | |
3′,4″-deoxy-αGalCer, an analogue of αGalCer with the 3′-OH of the sugar head group and the 4′-OH of the sphingosine chain removed; 4′,4″-deoxy-αGalCer, an analogue of αGalCer with the 4′-OH of the sugar head group and the 4′-OH of the sphingosine chain removed; α-C-GalCer, α-C-galactosylceramide (a C-glycoside analogue of αGalCer); αGalCer, α-galactosylceramide; αGalDAG, α-galactosyldiacylglycerol; αGlcCer, α-glucosylceramide; αGlcDAG-s2, α-glucosyldiacylglycerol; βGalCer, β-galactosylceramide; βLacCer, β-lactosylceramide; BnNH-GSL-1′, an analogue of αGalCer with an aromatic moiety connected to the sugar head group via an amide linkage; GalA-GSL, α-galacturonosylceramide; Gb3, globotrihexosylceramide; HS44, an analogue of αGalCer with the sugar moiety replaced by a carba cyclitol ring with an amino linkage to the lipid tail; iGb3, isoglobotrihexosylceramide; NKT, natural killer T; NU-αGalCer, naphthylurea-αGalCer; OCH, an analogue of αGalCer with a shorter acyl chain and sphingosine chain; SMC124, an analogue of αGalCer with the acyl chain of αGalCer and the sphingoid base of plakoside A; TCR, T cell receptor.
Studies have also indicated how the interplay between the germline- and non-germline-encoded regions of the TCR β-chain could influence the binding of mouse NKT TCRs66. Although the TCR β-chain does not directly contact the glycolipid antigen, variations in TCR β-chain usage cause subtle structural modifications in the conformation of the TCR α-chain, which indirectly contribute to the preferential recognition of some antigens55,62. This feature may be important in the context of infection and autoreactivity. In addition, although the Jα50-encoded loop of the atypical Vα10 NKT TCR is markedly different to the Jα18-encoded loop of the Vα14 NKT TCR, the Jα50 and Jα18 loops interact with the same region of CD1d. This suggests that other atypical type I NKT TCRs may adopt similar F′-pocket docking modes37, as has recently been demonstrated with the structure determination of a human Vα3.1Jα18 NKT TCR–αGalCer–CD1d complex130. Nevertheless, differences have been observed within the respective Vα10 and Vα14 NKT TCR–antigen–CD1d interfaces (FIG. 4), which provide insights into the molecular basis for the differing ligand specificities of the atypical Vα10+ NKT cell subset. These findings highlight the importance of understanding the functional and structural role of atypical type I NKT cells in mice and humans.
Antigens recognized by the type I NKT TCR
It is clear that, within the confinement of the consensus type I NKT TCR–CD1d footprint10 (FIG. 4), the type I NKT TCR binds to a diverse array of chemically distinct antigens. Here, we discuss how the NKT TCR achieves this feat of molecular recognition.
αGalCer and synthetic analogues
αGalCer can drive both T helper 1 (TH1)-type and TH2-type immune responses, thereby unpredictably causing either enhanced or suppressed immunity5. Thus, attention has centred on developing analogues of αGalCer that can bias the immune response in either direction9,13. These analogues have modifications in the head group, the acyl chain and/or the sphingosine chain71–74. The basis of how such modifications influence NKT TCR-mediated recognition has been established for a panel of αGalCer analogues58,73,75–77. The consensus type I NKT TCR–CD1d docking topology suggests that NKT cell function can be influenced, in part, by subtle alterations within the NKT TCR–antigen–CD1d interface58. As the effects of altered peptide ligands (APLs) on MHC-restricted immunity are associated with minor conformational shifts at the TCR–peptide–MHC interface78, we suggest the term ‘altered glycolipid ligands’ (AGLs) to describe closely related analogues that promote distinct functional NKT cell outcomes58.
Many head-group-modified AGLs are differentially recognized by NKT cells and thus have distinct effects on downstream immunity. Although no studies have examined the role of the 2′-OH of αGalCer, the distinct orientation of this moiety in α-mannosylceramide (a compound that has very little agonist activity24) suggests that the 2′-OH moiety is crucial for antigen recognition by type I NKT TCRs. AGLs with modifications at the 3′-OH and 4′-OH positions have fewer contacts with the NKT TCR than αGalCer does and thus are bound by the NKT TCR with lower affinity, resulting in decreased NKT cell activation60,79. Interestingly, αGlcCer is a more potent agonist than αGalCer for Vα10+Jα50+ NKT cells37, highlighting how variations in NKT TCR α-chain usage influence antigen specificity. Further studies of the functional potential of these AGLs are warranted, especially regarding human NKT cells80.
Several AGLs with substitutions or additions at the 6′-OH group promote TH1-biased immune responses and provide superior protection against tumour growth in mice73. This is reminiscent of the prototypical TH1-promoting AGL, α-C-GalCer, and its closely related derivatives72,76. Paradoxically, despite their superior anti-tumour and TH1-inducing potential, such compounds are bound by the NKT TCR with a lower affinity than αGalCer owing to reduced interactions with the TCR73,75. The superior TH1-type response induced by these (and other) ligands77 is attributable to the enhanced in vivo 73,75. Why do stability of the TH1-promoting compounds these compounds lead to TH1-biased responses? When NKT cells are activated, they immediately produce both IFNγ and IL-4. However, IL-4 production ceases within a few hours, whereas the production of IFNγ continues for 2–3 days and is mostly mediated by bystander natural killer (NK) cells following NKT cell activation72,81. This suggests that the lower affinity of the TH1-promoting compounds results in lower IL-4 and IFNγ levels in the short term, but that the increased stability of these compounds ensures sustained stimulation of NKT cells and NK cells as well as prolonged IFNγ production, primarily by the NK cells.
Modifications of the acyl or sphingosine chains of αGalCer can also have an impact on type I NKT cell function82,83. For example, two such compounds — known as C20:2 αGalCer (which has an unsaturated acyl chain) and OCH (which has a truncated sphingosine chain) — promote TH2-biased responses in vivo13. The C20:2 modification affects neither the affinity nor the mode of interaction with the NKT TCR58. This indicates that the TH2-biased in vivo cytokine response is primarily due to the very efficient and rapid uptake of C20:2 αGalCer by CD1d-expressing APCs, and also due to the increased turnover of this ligand and less sustained NKT cell activation83. Thus, C20:2 αGalCer potently induces short-term NKT cell stimulation and IL-4 and IFNγ production, but the long-term activation of NKT cells and bystander NK cells is reduced, leading to decreased IFNγ production and an effective bias towards a TH2-type response. A similar mechanism explains the TH2-biased response mediated by OCH58,81,83,84. In this case, however, the truncated sphingosine chain also has an impact on the affinity and association kinetics of the NKT TCR for OCH, as it modulates the architecture of the F′-pocket of CD1d58 (FIG. 5a).
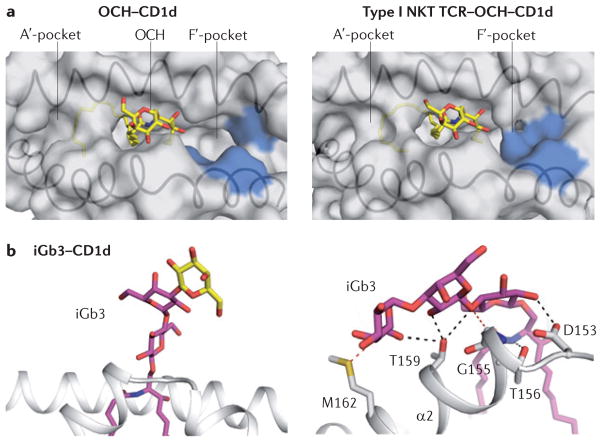
Figure 5. Changes in the conformation of the lipid or CD1d following binding to NKT TCRs.
a | The image on the left shows a surface representation of the α-galactosylceramide analogue OCH presented by CD1d, showing the A′ and F′ pockets (PDB code 3G08). The image on the right shows the closing of the F′-pocket roof in the CD1d–OCH complex following binding to the T cell receptor (TCR) (PDB code 3ARB), which is caused by movement of the side chains of Leu84, Vαl149 and Leu150 in CD1d (these residues are shown in blue). b | On the left is the structure of the β-linked glycolipid isoglobotrihexosylceramide (iGb3) presented by CD1d (PDB code 2Q7Y). The terminal sugar for iGb3 is modelled and shown in yellow. The image on the right shows the extensive interactions between the three sugars of the iGb3 head group and the residues of the CD1d α2-helix within type I natural killer T (NKT) cell TCR–iGb3–CD1d complex (PDB code 3SCM).
Overall, the bias towards the production of TH1- or TH2-type cytokines seems to be mainly related to CD1d loading, downstream events, APC types, ligand stability and the pharmacological properties of the AGLs themselves, rather than to altered NKT TCR–antigen–CD1d affinity58,83,85. However, the affinity of the type I NKT TCR–antigen–CD1d interaction seems to be a good measure of the efficacy of an AGL, in terms of absolute levels of cytokines produced by the NKT cells58. Thus, the studies using αGalCer-based AGLs showcase the potential of rationally designing NKT cell agonists that may result in more targeted type I NKT cell-based therapeutic regimens9. Moreover, the work carried out using synthetic αGalCer antigens has provided valuable insights into the factors that shape the antigenicity of physiologically relevant ligands.
Microbial ligands
Microbial lipid antigens that activate type I NKT cells have been identified in a broad range of microorganisms (FIG. 2b). Examples include α-glucuronosylceramides and α-galacturonosyl-ceramides from Sphingomonas spp., α-galactosyldiacylglycerols (αGalDAGs) from Borrelia burgdorferi, α-glucosyldiacylglycerols (αGlcDAGs) from Streptococcus pneumoniae and group B Streptococcus, and phosphatidylinositol mannosides (PIMs) from Mycobacterium tuberculosis37,86–92.
With the exception of the PIMs, which are phospho-lipids, these bacterial antigens possess a glycosyl head group that is conjugated, via an α-glycosidic linkage, to either a ceramide or a diacylglycerol (DAG) base. The α-glycosidic linkage defines a ‘microbial signature’, as most mammalian glycolipids have β-glycosidic linkages and, as such, αGalCer is considered to be a mimetic of the microbial α-glycolipids67,89. Nonetheless, the structures of these microbial lipid antigens are quite diverse, which highlights the range of foreign antigens that can be recognized by the type I NKT TCR. This recognition is partly achieved by the ability of the NKT TCR to mould the various head groups into a position that facilitates binding67,69, as well as by the diversity of the type I NKT TCR provided by the TCR β-chain55,75. As such, some microbial glycolipids seem to be recognized by only a subset of type I NKT cells90–92.
Much like in the case of αGalCer analogues, natural variations within the lipid tails of these microbial ligands can dramatically affect their antigenicity, although it is unclear whether this is due to a differential ability to dock into CD1d or due to alterations in CD1d-mediated presentation of the polar head group57,88,89,93. In support of the latter scenario, modifications of the DAG chain can determine the orientation of the lipid tails within the A′-pocket and F′-pocket of CD1d, thereby affecting the positioning of the glycosyl head group94. Furthermore, some microbial ligands leave an ‘open’ F′-pocket in CD1d, which is reshaped (closed) following recognition by the NKT TCR, in a similar manner to NKT TCR-mediated recognition of the αGalCer analogue OCH56 (FIG. 5a). Thus, there seems to be a subtle interplay between the head group and the lipid tails, which — together with type I NKT TCR specificity — ultimately determines the efficacy of the microbial lipid antigens57. Clearly, it will be important to establish a broader spectrum of microbial lipid antigens that can stimulate NKT cells and to address whether specific subsets within the NKT repertoire are more ideally tuned to interacting with defined microbial ligands.
Self antigens and NKT cell autoreactivity
Some NKT cells can respond to CD1d-expressing APCs in the absence of foreign agonist antigens3. Indeed, NKT cell-mediated recognition of CD1d-restricted self lipid antigens seems to be important for many immunopathological processes that involve NKT cells, including tumour rejection, autoimmunity, graft rejection and graft-versus-host disease5. Furthermore, when combined with pro-inflammatory cytokines, the reactivity of NKT cells to CD1d-restricted self lipids has an important role in NKT cell responses to infection11,38,95,96. Self antigens for NKT cells include phospholipid antigens and β-linked glycolipid antigens, and the relative importance of these molecules appears to be dependent on the cells involved and the presence of inflammatory signals.
Thymic selection by self antigens
Self-antigen recognition by NKT cells is likely to be imprinted in the thymus, where the recognition of CD1d-restricted self antigens is crucial for the intrathymic selection and survival of these cells97, similarly to the positive selection of T cells by self-peptide–MHC complexes98. Thus, the identification of the self lipid antigens that are involved in intrathymic NKT cell selection is a central goal. One candidate self lipid — isoglobotrihexosylceramide (iGb3) — is a moderate agonist for type I NKT cells99, although it remains controversial whether iGb3 is involved in NKT cell selection in mice or humans100–103. More recently, Facciotti et al. provided evidence that two peroxisome-generated, ether-bonded phospholipid antigens — plasmalogen lysophosphatidylethanolamine (pLPE) and ether lysophosphatidic acid (eLPA) — have a role in NKT cell development104. pLPE was capable of strongly activating type I NKT cells, and mice deficient in these peroxisomal lipids had impaired NKT cell development. It is quite possible that NKT cells are selected by a range of lipid-based antigens, including glycolipids and phospholipids, and that a level of redundancy exists in this process. Understanding the precise metabolic pathways involved in the generation of such self antigens will be central for determining whether different self antigens have unique roles in NKT cell biology, as well as for addressing how NKT TCRs recognize these structurally distinct self antigens.
Self-glycolipid recognition
Most mammalian glycolipids possess a β-linked glycolipid head group that protrudes from CD1d, in contrast to the ‘flattened’ conformation of the α-linked ligands105,106 (FIGS 3a, 5b). The study of NKT TCRs in complex with β-galactosylceramide (βGalCer) and iGb3 has provided insights into how type I NKT TCRs can recognize such distinct structural landscapes. Specifically, the NKT TCRs flatten the β-linked glycolipid head groups into a conformation that mirrors that of the α-linked antigens67,69 (FIG. 5b). This flattening of self antigens is reminiscent of the ‘bulldozer-like’ effect observed in some MHC-restricted T cell responses107–109 and reveals that, for the recognition of β-linked ligands, type I NKT TCRs operate through induced-fit molecular mimicry (FIG. 4a). In comparison to the NKT TCR-mediated recognition of α-linked antigens, the interactions between type I NKT TCRs and β-linked antigen–CD1d complexes are of considerably lower affinity67,69. This weak reactivity may be important for selecting an appropriate NKT TCR repertoire during development, so as to avoid overt NKT cell-mediated autoimmunity while ensuring the generation of an NKT cell repertoire that is poised for activation by foreign antigens.
Self-phospholipid recognition
Phospholipids represent a major component of biological membranes and thus are highly abundant but also extremely heterogeneous. Phospholipid self antigens for type I NKT cells include phosphatidylethanolamine, phosphatidylinositol95,104,110 and pLPE104. The structure of an engineered autoreactive type I NKT TCR–phosphatidylinositol–CD1d complex was shown to be very similar to that of type I NKT TCR–glycolipid–CD1d complexes68. The main difference was in the positioning of the phosphatidylinositol head group, which was orientated away from the NKT TCR–CD1d interface. Recently, the structure of a human type I NKT TCR–lysophosphatidylcholine–CD1d complex was elucidated, showing that the phosphatidylcholine head group shifts conformation markedly following the ligation of the type I NKT TCR70. This shift enables the formation of the consensus type I NKT TCR–CD1d docking topology, although there seems to be a slight ‘wobble’ in the overall docking topology in relation to other type I NKT TCR–CD1d complexes.
Mechanisms of self-antigen recognition
The reactivity of type I NKT cells to self antigens is strongly influenced by the TCR β-chain, which can affect the fine specificity of the NKT TCR55,61,62,66,68,111. Diversity within the CDR3β loop can engender CD1d-mediated autoreactivity by facilitating the direct interaction of this loop with CD1d68,111 (FIG. 4a), thereby reducing the specific energetic contribution required from the self antigens for interaction with the NKT TCR. Moreover, residues within the TCR β-chain can have an impact on the conformation of the invariant TCR α-chain, thereby indirectly modulating NKT TCR–antigen contacts55,70. These effects may explain the variability in the extent to which NKT TCRs can engage self antigens. Accordingly, multiple self antigens are recognized in a similar manner by these autoreactive type I NKT TCRs. Nevertheless, some CD1d-bound self glycolipids, such as the disialoganglioside GD3, can apparently ‘thwart’ the binding of the type I NKT TCR68, presumably through steric hindrance or charge repulsion. As CD1d molecules at the surface of APCs are likely to be loaded with a variety of self antigens with differing chemistries112, type I NKT cell autoreactivity caused by CDR3β loop diversity may be attributable to a shift in the balance between permissive and non-permissive self antigens.
Is autoreactivity limited to a subset of type I NKT TCRs with appropriate ‘autoreactive’ CDR3β loops? Given that all NKT cells are positively selected in the thymus, it is likely that they are all capable of interacting with self-antigen–CD1d complexes to some extent and that some self antigens may directly contribute to autoreactivity, regardless of CDR3β–CD1d interactions. These self antigens need not be strong agonists, and there may be heterogeneous lipid antigen species that support these processes in different settings, potentially with a differential role for type I and type II NKT cells. For example, the low-affinity self antigens βGlcCer and LPE are upregulated during bacterial and hepatitis B virus infections, respectively, resulting in NKT cell activation owing to the increased avidity of NKT TCR–antigen–CD1d binding combined with the presence of pro-inflammatory cytokines that co-stimulate these cells38,95. This illustrates two important concepts: first, that NKT cells are indirectly sensitized to microbial danger signals via the modulation of self lipid antigens presented by CD1d; and, second, that different self antigens may be important in different settings.
The factors that govern the antigenicity of specific ligands for type I and type II NKT cells are currently unclear, although the closely related nature of these antigens suggests that antigen density and CD1d-loading efficiency may be important factors in NKT cell auto-reactivity70,95,104,113–116. Overall, NKT cell autoreactivity remains a poorly understood area of NKT cell biology, and — considering that it is likely to be central for NKT cell responses in health and disease — it represents a key area for further investigation.
Type II NKT TCR-mediated recognition
Our understanding of the specificity and function of type II NKT cells is limited, and this is largely due to a lack of reagents to directly study this NKT cell subset. Do type I and type II NKT cells represent functionally similar cells with distinct antigen specificities or do they also mediate different immunological functions following activation? In support of the latter possibility, type I NKT cells are usually associated with the promotion of tumour rejection in mice, whereas type II NKT cells seem to suppress tumour rejection in mice and can antagonize the functions of type I NKT cells117. In a more recent study, type I and type II NKT cells seemed to work together in protecting against hepatitis B virus infection in mice95. Central to our understanding of the role of type II NKT cells in immunity is the establishment of their antigen specificity and the way in which their TCRs recognize these CD1d-presented antigens.
A key question is whether type II NKT TCRs adopt a different docking strategy from type I NKT TCRs. Two recent studies have provided the first snapshot of type II NKT TCR-mediated recognition, by determining the ternary structure of a type II NKT TCR (Vα1Jα26–Vβ16Jβ2.1) in complex with sulphatide–CD1d118 or lysosulphatide–CD1d119. Despite the difference in these forms of sulphatide, the docking modes of the type II NKT TCR were remarkably similar to each other. The type II NKT TCR docked orthogonally above the A′-pocket of CD1d, and the complex was thus distinct from all type I NKT TCR complexes10 (FIGS 3,4). Unlike the recognition of β-linked glycolipids by the type I NKT TCR67, the type II NKT TCR does not ‘flatten’ the sulphatide head group during ligation, although the positioning of the sulphatide head groups in the two type II ternary complexes was slightly different, suggesting a degree of flexibility in type II NKT TCR-mediated recognition. Moreover, the CDR3 loops of this TCR dominate the interaction, with the CDR3α and CDR3β loops interacting primarily with CD1d and sulphatide, respectively118 (FIG. 4b). These findings will fuel speculation as to whether all type II NKT TCRs dock over the A′-pocket, or whether the diverse type II NKT cell repertoire results in a myriad of distinct docking modes. Consistent with the latter possibility, mutagenesis studies of TCRs from other type II NKT cell clones have suggested that these TCRs have distinct docking footprints25,29,118–120. These initial studies suggest that type II NKT TCR-mediated antigen recognition is fundamentally distinct from type I NKT TCR-mediated recognition.
NKT cell recognition: implications for therapy
Great progress has been made since the discovery that αGalCer is an antigen for type I NKT cells24. Despite the very high affinity of the interaction with this antigen and its obvious therapeutic potential as an NKT cell agonist9, the physiological antigens for NKT cells are self lipid molecules that are recognized with much lower affinity38. For type I NKT cells, the antigen must be presented by CD1d in such a way that the polar head group can either contribute to the interaction or be flattened in a manner that does not destabilize the conserved interaction that defines all type I NKT TCR–antigen–CD1d complexes. Moreover, in the context of β-linked ligand recognition, we have shown that the antigenicity of a ligand is attributable to compensatory interactions between CD1d and the ligand itself that occur after NKT TCR ligation67 (FIG. 5b). Collectively, ligand antigenicity is determined by multiple factors, including the composition of the polar head group and lipid tails, ligand flexibility, and the ability of the ligand to be stabilized by either the NKT TCR or CD1d. The same variables may influence antigen recognition by type II NKT cells, with the important distinction that the greater TCR diversity within this population may facilitate a greater diversity in antigen recognition and TCR docking modes. The observation that type II NKT cells do not recognize αGalCer, despite its potency for activating type I NKT cells, highlights the fact that these two lineages are not redundant, although some antigens may be capable of activating both type I and type II NKT cells27,38.
Given that NKT cells can be activated by self antigens, the question that arises is how NKT cells normally avoid overt autoreactivity. It seems that, in steady-state conditions, the amount of signalling induced by self lipid antigens is insufficient to trigger NKT cell activation. However, modulation of the biosynthesis or degradation of self lipids, combined with increased co-stimulatory signalling, enables NKT cells to act as an early warning system for infections38,95 (FIG. 6). Similar mechanisms may explain NKT cell responses to tumours and in auto-immune diseases. Nonetheless, only some self antigens are capable of promoting NKT cell activation under these circumstances38,95,110, suggesting that low-affinity interactions with the NKT TCR are important factors in this process. Lastly, if NKT cell activation can be driven by the modulation of self-antigen expression, what is the significance of high-affinity, α-linked foreign antigens such as αGalCer in NKT cell biology? The difference in TCR signal strength is likely to result in distinct NKT cell functional programmes and, as such, have a differential impact on downstream effector responses. It is also possible that, for NKT cell activation, a small number of high-affinity antigens might be complemented by more abundant low-affinity self antigens, much like what is seen with peptide–MHC reactivity in conventional T cells121.
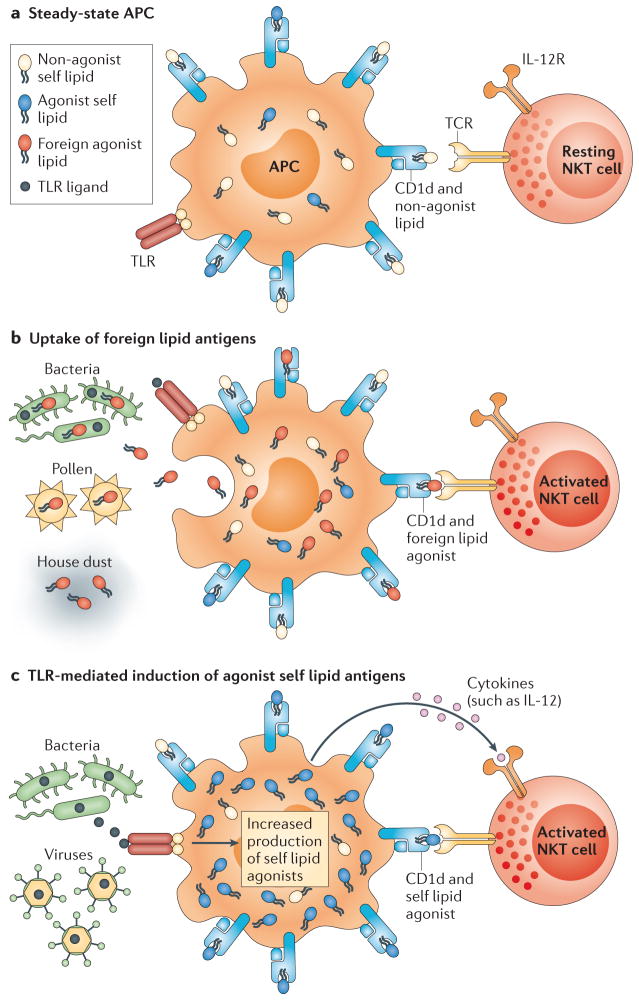
Figure 6. Modes of NKT cell activation.
a | In the steady state, antigen-presenting cells (APCs) present non-agonist self lipids on CD1d molecules that do not promote the activation of the natural killer T (NKT) cell T cell receptor (TCR).b | APCs can present non-self lipids derived from bacteria or environmental allergens on CD1d molecules. The direct recognition of foreign lipid antigens from these sources can promote NKT cell activation. c | Activation of Toll-like receptors (TLRs) on APCs can induce the production of self lipid antigens (such as β-galactosylceramide) that can serve as agonists for the NKT TCR. Recognition of these CD1d-presented self lipid agonists, in conjunction with exposure to TLR-induced inflammatory cytokines, leads to NKT cell activation. IL-12, interleukin-12; IL-12R, IL-12 receptor.
NKT cells can have both beneficial and deleterious roles in the immune system. NKT cells can enhance immunity to infection and some forms of cancer, and they are capable of protecting against graft-versus-host disease, allograft rejection and some types of autoimmunity5. In other settings, however, NKT cells can be activated in response to lipid allergens found in house dust extract12 or pollen122 and trigger allergic responses and airway hyperreactivity123. Similarly, the activation of NKT cells by circulating lipid antigens that are associated with atherosclerosis contributes to cardiovascular disease124, and NKT cell activation can also exacerbate some forms of autoimmune disease and prevent the efficient clearance of tumour cells in some models of cancer5,117. Thus, although the therapeutic potential of NKT cells is broad, the influence of these cells in different disease settings is complicated and unpredictable. Nevertheless, despite these challenges, recent clinical trials involving combination therapy using both αGalCer-pulsed autologous DCs and in vitro-expanded autologous NKT cells resulted in an increase in NKT cell frequency and improved anti-tumour immunity in a cohort of patients suffering from head and neck squamous cell carcinoma125,126. Such studies highlight the fact that it is vital that we gain a better understanding of the functions of the different types of NKT cells, as well as of the influence of different classes of antigens and other microenvironmental factors on these cells, in order to safely harness their therapeutic potential.
Future directions
There are fundamental differences between the recognition of lipid-based antigens by the αβ TCRs of type I NKT cells and the interaction of peptide-based antigens with the TCRs of conventional T cells. Our understanding of lipid antigen recognition by type I NKT TCRs has progressed markedly in recent years and has provided valuable insights into the factors that govern antigenicity and the functional impact of different types of antigen. This in turn helps us to understand the natural antigenic targets of NKT cells and informs the development of superior and more tailored therapeutic reagents to harness NKT cell activity. There are many outstanding questions, including whether minor subsets of antigen-specific NKT cells can undergo clonal expansion and develop into memory-like populations. Moreover, what determines the threshold of NKT cell self-tolerance versus self-reactivity? Do NKT cells with distinct antigen specificities, such as type I and type II NKT cells, accordingly exhibit distinct functions? Addressing these questions is not only crucial for our understanding of NKT cell biology, but also central to the development of effective therapeutics.
Notably, CD1d-restricted NKT cells represent only a small subset of lipid-reactive T cells in humans1. There are also T cells that recognize lipids presented by group 1 CD1 molecules, as well as other subsets of innate-like T cells, such as MR1-restricted mucosa-associated invariant T cells (MAIT cells) — which have recently been shown to recognize microbial vitamin B metabolites131 — and γδ T cells. These T cell subsets collectively represent 10% or more of the peripheral blood mono-nuclear cells in humans and an even higher proportion of the total leukocyte population found in tissues such as the gut and liver. Considering this, it is clear that there remains an enormous amount to learn about this important T cell arm of the immune system127–129.
Acknowledgments
This work was supported by the US National Institutes of Health (grants AI090450 and AI092108), Australian National Health and Medical Research Council (NHMRC) program and project grants, Cancer Council Victoria and the Australian Research Council (ARC). D.I.G. was supported by an NHMRC Senior Principal Research Fellowship; J.R. was supported by an NHMRC Australia Fellowship. O.P. was supported by an ARC Future Fellowship.
Glossary
- γδ T cells
T cells express either a T cell receptor (TCR) composed of α- and β-subunits (αβ TCR) or a TCR composed of γ- and δ-subunits (γδ TCR). The majority (more than 90%) of human T cells express αβ TCRs, which mainly recognize antigenic peptides bound to conventional MHC class I or II molecules. T cells that express γδ TCRs are less abundant, and the ligands for these receptors are less well characterized
- Altered peptide ligands (APLs)
Peptides that are analogues of an original antigenic peptide. They commonly have amino acid substitutions at residues that make contact with the T cell receptor (TCR). TCR engagement by these APLs usually leads to partial or incomplete T cell activation. Some APLs (antagonists) can specifically antagonize and inhibit T cell activation by the wild-type antigenic peptide
- Peroxisome
An indispensable cytoplasmic organelle that has essential roles in antioxidant defence, cholesterol and bile-acid synthesis, eicosanoid metabolism and the β- and ω-oxidation of long-chain and very-long-chain fatty acids
- Mucosa-associated invariant T cells (MAIT cells)
A population of innate-like lymphocytes. MAIT cells express an evolutionarily conserved invariant T cell receptor and are selected by the MHC class I-related molecule MR1. They are abundant in human blood, in the intestinal mucosa and in mesenteric lymph nodes, and they can produce interferon-γ in response to various bacterial infections
Footnotes
Competing interests statement
The authors declare no competing financial interests.
References
- 1.Brigl M, Brenner MB. CD1: antigen presentation and T cell function. Annu Rev Immunol. 2004;22:817–890. doi: 10.1146/annurev.immunol.22.012703.104608. [DOI] [PubMed] [Google Scholar]
- 2.Mori L, De Libero G. T cells specific for lipid antigens. Immunol Res. 2012;53:191–199. doi: 10.1007/s12026-012-8294-6. [DOI] [PubMed] [Google Scholar]
- 3.Bendelac A, Savage PB, Teyton L. The biology of NKT cells. Annu Rev Immunol. 2007;25:297–336. doi: 10.1146/annurev.immunol.25.022106.141711. [DOI] [PubMed] [Google Scholar]
- 4.Godfrey DI, MacDonald HR, Kronenberg M, Smyth MJ, Van Kaer L. NKT cells: what’s in a name? Nature Rev Immunol. 2004;4:231–237. doi: 10.1038/nri1309. [DOI] [PubMed] [Google Scholar]
- 5.Godfrey DI, Kronenberg M. Going both ways: immune regulation via CD1d-dependent NKT cells. J Clin Invest. 2004;114:1379–1388. doi: 10.1172/JCI23594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsuda JL, Mallevaey T, Scott-Browne J, Gapin L. CD1d-restricted iNKT cells, the ‘Swiss-Army knife’ of the immune system. Curr Opin Immunol. 2008;20:358–368. doi: 10.1016/j.coi.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berzins SP, Smyth MJ, Baxter AG. Presumed guilty: natural killer T cell defects and human disease. Nature Rev Immunol. 2011;11:131–142. doi: 10.1038/nri2904. [DOI] [PubMed] [Google Scholar]
- 8.Cerundolo V, Barral P, Batista FD. Synthetic iNKT cell-agonists as vaccine adjuvants — finding the balance. Curr Opin Immunol. 2010;22:417–424. doi: 10.1016/j.coi.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 9.Cerundolo V, Silk JD, Masri SH, Salio M. Harnessing invariant NKT cells in vaccination strategies. Nature Rev Immunol. 2009;9:28–38. doi: 10.1038/nri2451. [DOI] [PubMed] [Google Scholar]
- 10.Godfrey DI, et al. Antigen recognition by CD1d-restricted NKT T cell receptors. Semin Immunol. 2010;22:61–67. doi: 10.1016/j.smim.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Godfrey DI, Rossjohn J. New ways to turn on NKT cells. J Exp Med. 2011;208:1121–1125. doi: 10.1084/jem.20110983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wingender G, et al. Invariant NKT cells are required for airway inflammation induced by environmental antigens. J Exp Med. 2011;208:1151–1162. doi: 10.1084/jem.20102229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Venkataswamy MM, Porcelli SA. Lipid and glycolipid antigens of CD1d-restricted natural killer T cells. Semin Immunol. 2010;22:68–78. doi: 10.1016/j.smim.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dellabona P, Padovan E, Casorati G, Brockhaus M, Lanzavecchia A. An invariant Vα24–JαQ/Vβ11 T cell receptor is expressed in all individuals by clonally expanded CD4–8– T cells. J Exp Med. 1994;180:1171–1176. doi: 10.1084/jem.180.3.1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Porcelli S, Yockey CE, Brenner MB, Balk SP. Analysis of T cell antigen receptor (TCR) expression by human peripheral blood CD4–8– α/β T cells demonstrates preferential use of several Vβ genes and an invariant TCR α chain. J Exp Med. 1993;178:1–16. doi: 10.1084/jem.178.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lantz O, Bendelac A. An invariant T cell receptor α chain is used by a unique subset of major histocompatibility complex class I-specific CD4+ and CD4–8– T cells in mice and humans. J Exp Med. 1994;180:1097–1106. doi: 10.1084/jem.180.3.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Godfrey DI, McCluskey J, Rossjohn J. CD1d antigen presentation: treats for NKT cells. Nature Immunol. 2005;6:754–756. doi: 10.1038/ni0805-754. [DOI] [PubMed] [Google Scholar]
- 18.Kjer-Nielsen L, et al. A structural basis for selection and cross-species reactivity of the semi-invariant NKT cell receptor in CD1d/glycolipid recognition. J Exp Med. 2006;203:661–673. doi: 10.1084/jem.20051777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brossay L, et al. Cd1d-mediated recognition of an α-galactosylceramide by natural killer T cells is highly conserved through mammalian evolution. J Exp Med. 1998;188:1521–1528. doi: 10.1084/jem.188.8.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cui JQ, et al. Requirement for Vα14 NKT cells in IL-12-mediated rejection of tumors. Science. 1997;278:1623–1626. doi: 10.1126/science.278.5343.1623. [DOI] [PubMed] [Google Scholar]
- 21.Bedel R, et al. Lower TCR repertoire diversity in Traj18-deficient mice. Nature Immunol. 2012;13:705–706. doi: 10.1038/ni.2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matsuda JL, et al. Natural killer T cells reactive to a single glycolipid exhibit a highly diverse T cell receptor β repertoire and small clone size. Proc Natl Acad Sci USA. 2001;98:12636–12641. doi: 10.1073/pnas.221445298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gapin L. iNKT cell autoreactivity: what is ‘self’ and how is it recognized? Nature Rev Immunol. 2010;10:272–277. doi: 10.1038/nri2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kawano T, et al. CD1d-restricted and TCR-mediated activation of Vα14 NKT cells by glycosylceramides. Science. 1997;278:1626–1629. doi: 10.1126/science.278.5343.1626. This study characterizes α-galactosylceramide as a ligand for type I NKT cells. [DOI] [PubMed] [Google Scholar]
- 25.Burdin N, et al. Structural requirements for antigen presentation by mouse CD1. Proc Natl Acad Sci USA. 2000;97:10156–10161. doi: 10.1073/pnas.97.18.10156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burdin N, et al. Selective ability of mouse CD1 to present glycolipids: α-galactosylceramide specifically stimulates Vα14+ NK T lymphocytes. J Immunol. 1998;161:3271–3281. [PubMed] [Google Scholar]
- 27.Rhost S, Sedimbi S, Kadri N, Cardell SL. Immunomodulatory type II natural killer T (NKT) lymphocytes in health and disease. Scand J Immunol. 2012;76:246–255. doi: 10.1111/j.1365-3083.2012.02750.x. [DOI] [PubMed] [Google Scholar]
- 28.Jahng A, et al. Prevention of autoimmunity by targeting a distinct, noninvariant CD1d-reactive T cell population reactive to sulfatide. J Exp Med. 2004;199:947–957. doi: 10.1084/jem.20031389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cardell S, et al. CD1-restricted CD4+ T cells in major histocompatibility complex class II-deficient mice. J Exp Med. 1995;182:993–1004. doi: 10.1084/jem.182.4.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arrenberg P, Halder R, Dai Y, Maricic I, Kumar V. Oligoclonality and innate-like features in the TCR repertoire of type II NKT cells reactive to a β-linked self-glycolipid. Proc Natl Acad Sci USA. 2010;107:10984–10989. doi: 10.1073/pnas.1000576107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park SH, et al. The mouse CD1d-restricted repertoire is dominated by a few autoreactive T cell receptor families. J Exp Med. 2001;193:893–904. doi: 10.1084/jem.193.8.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bai L, et al. The majority of CD1d–sulfatide-specific T cells in human blood use a semiinvariant Vδ1 TCR. Eur J Immunol. 2012;42:2505–2510. doi: 10.1002/eji.201242531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gadola SD, Dulphy N, Salio M, Cerundolo V. Vα24-JαQ-independent, CD1d-restricted recognition of α-galactosylceramide by human CD4+ and CD8αβ+ T lymphocytes. J Immunol. 2002;168:5514–5520. doi: 10.4049/jimmunol.168.11.5514. [DOI] [PubMed] [Google Scholar]
- 34.Gadola SD, et al. Structure and binding kinetics of three different human CD1d–α-galactosylceramide-specific T cell receptors. J Exp Med. 2006;203:699–710. doi: 10.1084/jem.20052369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brigl M, et al. Conserved and heterogeneous lipid antigen specificities of CD1d-restricted NKT cell receptors. J Immunol. 2006;176:3625–3634. doi: 10.4049/jimmunol.176.6.3625. [DOI] [PubMed] [Google Scholar]
- 36.Constantinides MG, Picard D, Savage AK, Bendelac AA. Naive-like population of human CD1d-restricted T cells expressing intermediate levels of promyelocytic leukemia zinc finger. J Immunol. 2011;187:309–315. doi: 10.4049/jimmunol.1100761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Uldrich AP, et al. A semi-invariant Vα10+ T cell antigen receptor defines a population of natural killer T cells with distinct glycolipid antigen-recognition properties. Nature Immunol. 2011;12:616–623. doi: 10.1038/ni.2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brennan PJ, et al. Invariant natural killer T cells recognize lipid self antigen induced by microbial danger signals. Nature Immunol. 2011;12:1202–1211. doi: 10.1038/ni.2143. This study shows that a particular form of βGlcCer represents a self ligand for the NKT TCR that is upregulated during infection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rhost S, et al. Identification of novel glycolipid ligands activating a sulfatide reactive, CD1d-restricted, type II natural killer T lymphocyte. Eur J Immunol. 2012 Jul 10; doi: 10.1002/eji.201142350. [DOI] [PubMed] [Google Scholar]
- 40.Zeng Z, et al. Crystal structure of mouse CD1: an MHC-like fold with a large hydrophobic binding groove. Science. 1997;277:339–345. doi: 10.1126/science.277.5324.339. [DOI] [PubMed] [Google Scholar]
- 41.Gadola SD, et al. Structure of human CD1b with bound ligands at 2.3 Å, a maze for alkyl chains. Nature Immunol. 2002;3:721–726. doi: 10.1038/ni821. [DOI] [PubMed] [Google Scholar]
- 42.Zajonc DM, et al. Structure and function of a potent agonist for the semi-invariant natural killer T cell receptor. Nature Immunol. 2005;6:810–818. doi: 10.1038/ni1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zajonc DM, Elsliger MA, Teyton L, Wilson IA. Crystal structure of CD1a in complex with a sulfatide self antigen at a resolution of 2.15 Å. Nature Immunol. 2003;4:808–815. doi: 10.1038/ni948. [DOI] [PubMed] [Google Scholar]
- 44.Scharf L, et al. The 2.5Å structure of CD1c in complex with a mycobacterial lipid reveals an open groove ideally suited for diverse antigen presentation. Immunity. 2010;33:853–862. doi: 10.1016/j.immuni.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Koch M, et al. The crystal structure of human CD1d with and without α-galactosylceramide. Nature Immunol. 2005;6:819–826. doi: 10.1038/ni1225. [DOI] [PubMed] [Google Scholar]
- 46.Moody DB, Zajonc DM, Wilson IA. Anatomy of CD1–lipid antigen complexes. Nature Rev Immunol. 2005;5:387–399. doi: 10.1038/nri1605. [DOI] [PubMed] [Google Scholar]
- 47.Zajonc DM, Wilson IA. Architecture of CD1 proteins. Curr Top Microbiol Immunol. 2007;314:27–50. doi: 10.1007/978-3-540-69511-0_2. [DOI] [PubMed] [Google Scholar]
- 48.Salio M, Silk JD, Cerundolo V. Recent advances in processing and presentation of CD1 bound lipid antigens. Curr Opin Immunol. 2010;22:81–88. doi: 10.1016/j.coi.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 49.Cohen NR, Garg S, Brenner MB. Antigen presentation by CD1: lipids, T cells, and NKT cells in microbial immunity. Adv Immunol. 2009;102:1–94. doi: 10.1016/S0065-2776(09)01201-2. [DOI] [PubMed] [Google Scholar]
- 50.Brutkiewicz RR. CD1d ligands: the good, the bad, and the ugly. J Immunol. 2006;177:769–775. doi: 10.4049/jimmunol.177.2.769. [DOI] [PubMed] [Google Scholar]
- 51.Borg NA, Kjer-Nielsen L, McCluskey J, Rossjohn J. Structural insight into natural killer T cell receptor recognition of CD1d. Adv Exp Med Biol. 2007;598:20–34. doi: 10.1007/978-0-387-71767-8_3. [DOI] [PubMed] [Google Scholar]
- 52.Borg NA, et al. CD1d–lipid-antigen recognition by the semi-invariant NKT T-cell receptor. Nature. 2007;448:44–49. doi: 10.1038/nature05907. This study provides the first description of a type I NKT TCR–antigen–CD1d interaction. [DOI] [PubMed] [Google Scholar]
- 53.Godfrey DI, Rossjohn J, McCluskey J. The fidelity, occasional promiscuity, and versatility of T cell receptor recognition. Immunity. 2008;28:304–314. doi: 10.1016/j.immuni.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 54.Burrows SR, et al. Hard wiring of T cell receptor specificity for the major histocompatibility complex is underpinned by TCR adaptability. Proc Natl Acad Sci USA. 2010;107:10608–10613. doi: 10.1073/pnas.1004926107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pellicci DG, et al. Differential recognition of CD1d– α-galactosyl ceramide by the Vβ8.2 and Vβ7 semi-invariant NKT T cell receptors. Immunity. 2009;31:47–59. doi: 10.1016/j.immuni.2009.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li Y, et al. The Va14 invariant natural killer T cell TCR forces microbial glycolipids and CD1d into a conserved binding mode. J Exp Med. 2010;207:2383–2393. doi: 10.1084/jem.20101335. This report provided the first insights into how the type I NKT TCR can interact with microbial ligands. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Girardi E, et al. Unique interplay between sugar and lipid in determining the antigenic potency of bacterial antigens for NKT cells. PLoS Biol. 2011;9:e1001189. doi: 10.1371/journal.pbio.1001189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wun KS, et al. A molecular basis for the exquisite CD1d-restricted antigen specificity and functional responses of natural killer T cells. Immunity. 2011;34:327–339. doi: 10.1016/j.immuni.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Scott-Browne JP, et al. Germline-encoded recognition of diverse glycolipids by natural killer T cells. Nature Immunol. 2007;8:1105–1113. doi: 10.1038/ni1510. This study showed for the first time how the type I NKT TCR can function like a pattern-recognition receptor. [DOI] [PubMed] [Google Scholar]
- 60.Wun KS, et al. A minimal binding footprint on CD1d–glycolipid is a basis for selection of the unique human NKT TCR. J Exp Med. 2008;205:939–949. doi: 10.1084/jem.20072141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Florence WC, et al. Adaptability of the semi-invariant natural killer T-cell receptor towards structurally diverse CD1d-restricted ligands. EMBO J. 2009;28:3579–3590. doi: 10.1038/emboj.2009.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Patel O, et al. Vb2 natural killer T cell antigen receptor-mediated recognition of CD1d–glycolipid antigen. Proc Natl Acad Sci USA. 2011;108:19007–19012. doi: 10.1073/pnas.1109066108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Joyce S, Girardi E, Zajonc DM. NKT cell ligand recognition logic: molecular basis for a synaptic duet and transmission of inflammatory effectors. J Immunol. 2011;187:1081–1089. doi: 10.4049/jimmunol.1001910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mallevaey T, Selvanantham T. Strategy of lipid recognition by invariant natural killer T cells: ‘one for all and all for one’. Immunology. 2012;136:273–282. doi: 10.1111/j.1365-2567.2012.03580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Adams EJ, Lopez-Sagaseta J. The immutable recognition of CD1d. Immunity. 2011;34:281–283. doi: 10.1016/j.immuni.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 66.Mallevaey T, et al. T cell receptor CDR2β and CDR3β loops collaborate functionally to shape the iNKT cell repertoire. Immunity. 2009;31:60–71. doi: 10.1016/j.immuni.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pellicci DG, et al. Recognition of β-linked self glycolipids mediated by natural killer T cell antigen receptors. Nature Immunol. 2011;12:827–833. doi: 10.1038/ni.2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mallevaey T, et al. A molecular basis for NKT cell recognition of CD1d–self-antigen. Immunity. 2011;34:315–326. doi: 10.1016/j.immuni.2011.01.013. This report provided the first structural insights into the basis of CD1d-mediated autoreactivity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yu ED, Girardi E, Wang J, Zajonc DM. Cutting edge: structural basis for the recognition of β-linked glycolipid antigens by invariant NKT cells. J Immunol. 2011;187:2079–2083. doi: 10.4049/jimmunol.1101636. Together with reference 67, this study showed that the type I NKT TCR can ‘bulldoze’ β-linked ligands to enable CD1d engagement. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lopez-Sagaseta J, Sibener LV, Kung JE, Gumperz J, Adams EJ. Lysophospholipid presentation by CD1d and recognition by a human natural killer T-cell receptor. EMBO J. 2012;31:2047–2059. doi: 10.1038/emboj.2012.54. This is the first description of how an NKT TCR can recognize lysophospholipids. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Miyamoto K, Miyake S, Yamamura T. A synthetic glycolipid prevents autoimmune encephalomyelitis by inducing TH2 bias of natural killer T cells. Nature. 2001;413:531–534. doi: 10.1038/35097097. [DOI] [PubMed] [Google Scholar]
- 72.Schmieg J, Yang G, Franck RW, Tsuji M. Superior protection against malaria and melanoma metastases by a C-glycoside analogue of the natural killer T cell ligand α-galactosylceramide. J Exp Med. 2003;198:1631–1641. doi: 10.1084/jem.20031192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Aspeslagh S, et al. Galactose-modified iNKT cell agonists stabilized by an induced fit of CD1d prevent tumour metastasis. EMBO J. 2011;30:2294–2305. doi: 10.1038/emboj.2011.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yu KO, et al. Modulation of CD1d-restricted NKT cell responses by using N-acyl variants of α-galactosylceramides. Proc Natl Acad Sci USA. 2005;102:3383–3388. doi: 10.1073/pnas.0407488102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Patel O, et al. NKT TCR recognition of CD1d– α-C-galactosylceramide. J Immunol. 2011;187:4705–4713. doi: 10.4049/jimmunol.1100794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kerzerho J, et al. Structural and functional characterization of a novel nonglycosidic type I NKT agonist with immunomodulatory properties. J Immunol. 2012;188:2254–2265. doi: 10.4049/jimmunol.1103049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tyznik AJ, et al. Glycolipids that elicit IFN-γ-biased responses from natural killer T cells. Chem Biol. 2011;18:1620–1630. doi: 10.1016/j.chembiol.2011.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sloan-Lancaster J, Allen PM. Altered peptide ligand-induced partial T cell activation: molecular mechanisms and role in T cell biology. Annu Rev Immunol. 1996;14:1–27. doi: 10.1146/annurev.immunol.14.1.1. [DOI] [PubMed] [Google Scholar]
- 79.Raju R, et al. Synthesis and evaluation of 3″- and 4″-deoxy and -fluoro analogs of the immunostimulatory glycolipid, KRN7000. Bioorg Med Chem Lett. 2009;19:4122–4125. doi: 10.1016/j.bmcl.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wun KS, et al. Human and mouse type I natural killer T-cell antigen receptors exhibit different fine specificities for CD1d–antigen. J Biol Chem. 2012 Sep 20; doi: 10.1074/jbc.M112.412320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sullivan BA, et al. Mechanisms for glycolipid antigen-driven cytokine polarization by Vα14i NKT cells. J Immunol. 2010;184:141–153. doi: 10.4049/jimmunol.0902880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.McCarthy C, et al. The length of lipids bound to human CD1d molecules modulates the affinity of NKT cell TCR and the threshold of NKT cell activation. J Exp Med. 2007;204:1131–1144. doi: 10.1084/jem.20062342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Im JS, et al. Kinetics and cellular site of glycolipid loading control the outcome of natural killer T cell activation. Immunity. 2009;30:888–898. doi: 10.1016/j.immuni.2009.03.022. This study shows how mechanisms pertaining to antigen loading can relate to the efficacy of an antigen in activating NKT cells. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bai L, et al. Lysosomal recycling terminates CD1d- mediated presentation of short and polyunsaturated variants of the NKT cell lipid antigen αGalCer. Proc Natl Acad Sci USA. 2009;106:10254–10259. doi: 10.1073/pnas.0901228106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bai L, et al. Distinct APCs explain the cytokine bias of α-galactosylceramide variants in vivo. J Immunol. 2012;188:3053–3061. doi: 10.4049/jimmunol.1102414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mattner J, et al. Exogenous and endogenous glycolipid antigens activate NKT cells during microbial infections. Nature. 2005;434:525–529. doi: 10.1038/nature03408. [DOI] [PubMed] [Google Scholar]
- 87.Sriram V, Du W, Gervay-Hague J, Brutkiewicz RR. Cell wall glycosphingolipids of Sphingomonas paucimobilis are CD1d-specific ligands for NKT cells. Eur J Immunol. 2005;35:1692–1701. doi: 10.1002/eji.200526157. [DOI] [PubMed] [Google Scholar]
- 88.Kinjo Y, et al. Invariant natural killer T cells recognize glycolipids from pathogenic Gram-positive bacteria. Nature Immunol. 2011;12:966–974. doi: 10.1038/ni.2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kinjo Y, et al. Natural killer T cells recognize diacylglycerol antigens from pathogenic bacteria. Nature Immunol. 2006;7:978–986. doi: 10.1038/ni1380. [DOI] [PubMed] [Google Scholar]
- 90.Kinjo Y, et al. Recognition of bacterial glycosphingolipids by natural killer T cells. Nature. 2005;434:520–525. doi: 10.1038/nature03407. This report describes the importance of NKT cells in protective immunity to infection. [DOI] [PubMed] [Google Scholar]
- 91.Fischer K, et al. Mycobacterial phosphatidylinositol mannoside is a natural antigen for CD1d-restricted T cells. Proc Natl Acad Sci USA. 2004;101:10685–10690. doi: 10.1073/pnas.0403787101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chang YJ, et al. Influenza infection in suckling mice expands an NKT cell subset that protects against airway hyperreactivity. J Clin Invest. 2011;121:57–69. doi: 10.1172/JCI44845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wu D, et al. Design of natural killer T cell activators: structure and function of a microbial glycosphingolipid bound to mouse CD1d. Proc Natl Acad Sci USA. 2006;103:3972–3977. doi: 10.1073/pnas.0600285103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang J, et al. Lipid binding orientation within CD1d affects recognition of Borrelia burgorferi antigens by NKT cells. Proc Natl Acad Sci USA. 2010;107:1535–1540. doi: 10.1073/pnas.0909479107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zeissig S, et al. Hepatitis B virus-induced lipid alterations contribute to natural killer T cell-dependent protective immunity. Nature Med. 2012;18:1060–1068. doi: 10.1038/nm.2811. This report describes a role for phospholipid- reactive type II NKT cells in promoting immunity to hepatitis B virus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Brigl M, et al. Innate and cytokine-driven signals, rather than microbial antigens, dominate in natural killer T cell activation during microbial infection. J Exp Med. 2011;208:1163–1177. doi: 10.1084/jem.20102555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chiu YH, et al. Multiple defects in antigen presentation and T cell development by mice expressing cytoplasmic tail-truncated CD1d. Nature Immunol. 2002;3:55–60. doi: 10.1038/ni740. [DOI] [PubMed] [Google Scholar]
- 98.Hogquist KA, et al. T cell receptor antagonist peptides induce positive selection. Cell. 1994;76:17–27. doi: 10.1016/0092-8674(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 99.Zhou D, et al. Lysosomal glycosphingolipid recognition by NKT cells. Science. 2004;306:1786–1789. doi: 10.1126/science.1103440. [DOI] [PubMed] [Google Scholar]
- 100.Speak AO, et al. Implications for invariant natural killer T cell ligands due to the restricted presence of isoglobotrihexosylceramide in mammals. Proc Natl Acad Sci USA. 2007;104:5971–5976. doi: 10.1073/pnas.0607285104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Porubsky S, et al. Normal development and function of invariant natural killer T cells in mice with isoglobotrihexosylceramide (iGb3) deficiency. Proc Natl Acad Sci USA. 2007;104:5977–5982. doi: 10.1073/pnas.0611139104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Christiansen D, et al. Humans lack iGb3 due to the absence of functional iGb3-synthase: implications for NKT cell development and transplantation. PLoS Biol. 2008;6:e172. doi: 10.1371/journal.pbio.0060172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Porubsky S, et al. Globosides but not isoglobosides can impact the development of invariant NKT cells and their interaction with dendritic cells. J Immunol. 2012;189:3007–3017. doi: 10.4049/jimmunol.1201483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Facciotti F, et al. Peroxisome-derived lipids are self antigens that stimulate invariant natural killer T cells in the thymus. Nature Immunol. 2012;13:474–480. doi: 10.1038/ni.2245. [DOI] [PubMed] [Google Scholar]
- 105.Zajonc DM, Ainge GD, Painter GF, Severn WB, Wilson IA. Structural characterization of mycobacterial phosphatidylinositol mannoside binding to mouse CD1d. J Immunol. 2006;177:4577–4583. doi: 10.4049/jimmunol.177.7.4577. [DOI] [PubMed] [Google Scholar]
- 106.Zajonc DM, Savage PB, Bendelac A, Wilson IA, Teyton L. Crystal structures of mouse CD1d–iGb3 complex and its cognate Vα14 T cell receptor suggest a model for dual recognition of foreign and self glycolipids. J Mol Biol. 2008;377:1104–1116. doi: 10.1016/j.jmb.2008.01.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Macdonald WA, et al. T cell allorecognition via molecular mimicry. Immunity. 2009;31:897–908. doi: 10.1016/j.immuni.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 108.Archbold JK, et al. Natural micropolymorphism in human leukocyte antigens provides a basis for genetic control of antigen recognition. J Exp Med. 2009;206:209–219. doi: 10.1084/jem.20082136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tynan FE, et al. A T cell receptor flattens a bulged antigenic peptide presented by a major histocompatibility complex class I molecule. Nature Immunol. 2007;8:268–276. doi: 10.1038/ni1432. [DOI] [PubMed] [Google Scholar]
- 110.Gumperz JE, et al. Murine CD1d-restricted T cell recognition of cellular lipids. Immunity. 2000;12:211–221. doi: 10.1016/s1074-7613(00)80174-0. [DOI] [PubMed] [Google Scholar]
- 111.Matulis G, et al. Innate-like control of human iNKT cell autoreactivity via the hypervariable CDR3β loop. PLoS Biol. 2010;8:e1000402. doi: 10.1371/journal.pbio.1000402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Muindi K, et al. Activation state and intracellular trafficking contribute to the repertoire of endogenous glycosphingolipids presented by CD1d. Proc Natl Acad Sci USA. 2010;107:3052–3057. doi: 10.1073/pnas.0915056107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Blomqvist M, et al. Multiple tissue-specific isoforms of sulfatide activate CD1d-restricted type II NKT cells. Eur J Immunol. 2009;39:1726–1735. doi: 10.1002/eji.200839001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chang DH, et al. Inflammation associated lysophospholipids as ligands for CD1d restricted T cells in human cancer. Blood. 2008;112:1308–1316. doi: 10.1182/blood-2008-04-149831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fox LM, et al. Recognition of lysophospholipids by human natural killer T lymphocytes. PLoS Biol. 2009;7:e1000228. doi: 10.1371/journal.pbio.1000228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pei B, et al. Diverse endogenous antigens for mouse NKT cells: self-antigens that are not glycosphingolipids. J Immunol. 2011;186:1348–1360. doi: 10.4049/jimmunol.1001008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Berzofsky JA, Terabe M. NKT cells in tumor immunity: opposing subsets define a new immunoregulatory axis. J Immunol. 2008;180:3627–3635. doi: 10.4049/jimmunol.180.6.3627. [DOI] [PubMed] [Google Scholar]
- 118.Patel O, et al. Recognition of CD1d–sulfatide mediated by a type II natural killer T cell antigen receptor. Nature Immunol. 2012;13:857–863. doi: 10.1038/ni.2372. [DOI] [PubMed] [Google Scholar]
- 119.Girardi E, et al. Type II natural killer T cells use features of both innate-like and conventional T cells to recognize sulfatide self antigens. Nature Immunol. 2012;13:851–856. doi: 10.1038/ni.2371. Together with reference 118, this study provided the first description of a type II NKT TCR–antigen–CD1d interaction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Monzon-Casanova E, et al. CD1d expression in Paneth cells and rat exocrine pancreas revealed by novel monoclonal antibodies which differentially affect NKT cell activation. PLoS ONE. 2010;5:e13089. doi: 10.1371/journal.pone.0013089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Krogsgaard M, et al. Agonist/endogenous peptide–MHC heterodimers drive T cell activation and sensitivity. Nature. 2005;434:238–243. doi: 10.1038/nature03391. [DOI] [PubMed] [Google Scholar]
- 122.Agea E, et al. Human CD1-restricted T cell recognition of lipids from pollens. J Exp Med. 2005;202:295–308. doi: 10.1084/jem.20050773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Umetsu DT, DeKruyff RH. Natural killer T cells are important in the pathogenesis of asthma: the many pathways to asthma. J Allergy Clin Immunol. 2010;125:975–979. doi: 10.1016/j.jaci.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Braun NA, Covarrubias R, Major AS. Natural killer T cells and atherosclerosis: form and function meet pathogenesis. J Innate Immun. 2010;2:316–324. doi: 10.1159/000296915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kunii N, et al. Combination therapy of in vitro-expanded natural killer T cells and α-galactosylceramide-pulsed antigen-presenting cells in patients with recurrent head and neck carcinoma. Cancer Sci. 2009;100:1092–1098. doi: 10.1111/j.1349-7006.2009.01135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Yamasaki K, et al. Induction of NKT cell-specific immune responses in cancer tissues after NKT cell-targeted adoptive immunotherapy. Clin Immunol. 2011;138:255–265. doi: 10.1016/j.clim.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 127.Reantragoon R, et al. Structural insight into MR1-mediated recognition of the mucosal associated invariant T cell receptor. J Exp Med. 2012;209:761–774. doi: 10.1084/jem.20112095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Treiner E, et al. Selection of evolutionarily conserved mucosal-associated invariant T cells by MR1. Nature. 2003;422:164–169. doi: 10.1038/nature01433. [DOI] [PubMed] [Google Scholar]
- 129.Hooper LV, Littman DR, Macpherson AJ. Interactions between the microbiota and the immune system. Science. 2012;336:1268–1273. doi: 10.1126/science.1223490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.López-Sagaseta J, Kung JE, Savage PB, Gumperz J, Adams EJ. The molecular basis for recognition of CD1d/α-galactosylceramide by a human non-Vα24 T cell receptor. PLoS Biol. 2012;10:e1001412. doi: 10.1371/journal.pbio.1001412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kjer-Nielsen L, et al. MR1 presents microbial vitamin B metabolites to MAIT cells. Nature. 2012 Oct 10; doi: 10.1038/nature11605. [DOI] [PubMed] [Google Scholar]