Abstract
Objective
Sleep-restriction in humans increases risk for obesity, but previous rodent studies show weight loss following sleep deprivation, possibly due to stressful-methods used to prevent sleep. Obesity-resistant (OR) rats exhibit consolidated-sleep and resistance to weight-gain. We hypothesized that sleep disruption by a less-stressful method would increase body weight, and examined effect of partial sleep deprivation (PSD) on body weight in OR and Sprague-Dawley (SD) rats.
Design and Methods
OR and SD rats (n=12/group) were implanted with transmitters to record sleep/wake. After baseline recording, six SD and six OR rats underwent 8 h PSD during light-phase for 9 d. Sleep was reduced using recordings of random noise. Sleep/wake states were scored as wakefulness (W), slow-wave-sleep (SWS) and rapid-eye-movement-sleep (REMS). Total number of transitions between stages, SWS-delta-power, food intake and body weight were documented.
Results
Exposure to noise decreased SWS and REMS time, while increasing W time. Sleep-deprivation increased number of transitions between stages and SWS-delta-power. Further, PSD during the rest phase increased recovery-sleep during active phase. The PSD SD and OR rats had greater food intake and body weight compared to controls
Conclusions
PSD by less-stressful means increases body weight in rats. Also, PSD during rest phase increases active period sleep.
Introduction
Nearly one third of the population in the developed world has poor sleep quality or reduced sleep duration, and the parallel increase in obesity highlights the association between poor sleep quality and obesity (1–4). Though evidence suggests a bimodal relationship between sleep time and body weight gain in adults, chronic sleep deprivation (reduced total sleep time) or sleep fragmentation (an indicator of sleep quality) increases risk for obesity and metabolic disorders in humans (1, 3, 5). For instance, reductions in total sleep time are associated with weight gain in children (2, 3). Similarly, sleep fragmentation is associated with human obesity perhaps due to excessive daytime sleepiness (EDS), physical inactivity and food intake (1, 6). Improvements in sleep quality and reduced sleep fragmentation are noted after bariatric surgery (7) and fat mass gain is attenuated in short sleepers after increases in sleep duration (8). A recent study showed that sleep deprivation increases energy expenditure (EE), and that during recovery sleep EE is lower than during normal sleep (9). Collectively, these studies show that adequate total sleep time and quality influence the development of obesity.
Unlike human sleep deprivation studies, previous rodent sleep deprivation studies reported weight loss, activation of hypothalamus-pituitary-adrenal (HPA) axis, along with increased food intake and energy expenditure (10–13). Since many of these studies use the disk over water method, where rats fall into water when they sleep, these effects were likely due to immune responses and exposure to cold temperatures in addition to the disrupted sleep (12). A study showed that 72h of REM sleep deprivation increases preference for carbohydrate-rich food, food intake and body weight gain (10). In another study on rats, during ten d of sleep deprivation for 18h daily, a daily opportunity for 6h sleep attenuated the negative energy balance observed after total sleep deprivation, which contrasts with previous reports of total sleep-deprivation in rodents (14). Together, these studies suggest that total sleep deprivation by severe methods results in weight loss while PSD promotes weight gain, reconciling the opposing effects on body weight in early rodent sleep studies with more recent studies in rodents and humans. Likewise, several animal obesity models suggest that disordered sleep contributes to obesity (13, 15, 16).
Levin and colleagues showed that, when fed a high-energy diet, more than half of out-bred SD rats developed diet-induced obesity (DIO). The remaining rats showed diet-induced obesity resistance (DR). These rats are also called obesity prone (OP) and obesity resistant (OR) when high-energy dietary challenge is not the strategy used for classification into the obesity prone or resistant categories. DIO rats share many characteristics of human obesity and follow a polygenic mode of inheritance (17). The DIO and DR rats have been selectively bred for generations, and exhibit divergent body weight profiles despite similar caloric intake (13). To establish a polygenic rodent model of obesity with sleep pathology similar to humans we compared sleep profiles in outbred Sprague-Dawley rats and selectively-bred OR rats, which exhibit different adiposity and physical activity profiles (13, 18). In contrast to SD rats, OR rats have greater spontaneous physical activity (SPA), orexin-A induced SPA and orexin receptor mRNA in sleep and energy balance-related brain nuclei as well as better sleep quality indicated by less fragmented sleep, prolonged and consolidated sleep/wake states and lower sleep drive (18, 19). These data support the association between obesity resistance and better sleep quality and underscore the role of orexin in body weight and sleep regulation.
Here we report the effect of a novel and less severe partial sleep deprivation (PSD) method on body weight gain in this rodent model of obesity resistance. Given the relationship between obesity resistance and a more consolidated sleep/wake cycle, we hypothesized that partial sleep deprivation by environmental noise (8h/day for 9 d) would enhance food intake and body weight gain in rats, and OR rats would be resistant to body weight enhancing effects of PSD. These data provide the first evidence that partial sleep deprivation by noise increases body weight independent of obesity propensity.
Methods and Procedures
Animals
Three-month old male Sprague-Dawley (SD) and selectively bred male obesity resistant (SD and OR, n=12/group) rats (Charles River, Kingston, NY, USA) were housed individually in conventional hanging wire-cages with a 12 h light–12 h dark photoperiod (lights on at 0600) in a temperature controlled room (21–22 °C). Rodent chow (Teklad rodent diet 8604, Harlan, Madison, WI, USA) and water was available ad libitum throughout the experiment. Protein, fat and carbohydrate provided 33%, 14% and 53% of calories respectively, with a metabolizable energy of 3.1 kcals per gram. All experiments were approved by the Local Institutional Animal Care and Use Committee at the Minneapolis VA Healthcare System and University of Minnesota.
EEG and EMG lead implantation
Surface electroencephalogram (EEG) and electromyogram (EMG) leads connected to a radiotelemetry transmitter (F40-EET, Data Sciences International (DSI), St Paul, MN, USA), were implanted in each rat under Nembutal (60 mg/kg, intraperitoneal) anesthesia as described previously (18). Landmarks for bilateral EEG leads (3.1mm posterior and 1.5mm lateral to bregma; incisor bar set at 3.3mm below ear bars) were determined from the rat brain atlas as described in our earlier study (18). The transmitter was placed in a blunt dissected channel along the animals’ back. Animals were fed ad libitum and given a post-surgical recovery period of at least 7 d before the start of experiments.
EEG–EMG Recording
Rats were placed in a plastic solid-bottom cage with rodent bedding, ad libitum food and water, and habituated for 48 h in a sound-attenuating chamber (Med Associates, St Albans, VT, USA) to adapt to the free-moving sleep recording conditions followed by a 24 h baseline recording period. Recording sessions began between 0900 – 1000 and sleep was recorded with the EEG–EMG recording system as described previously (18). Briefly, EEG/EMG signals from the implanted transmitter were detected by a receiver (PhysioTel RPC-1, DSI, St. Paul, MN, USA). Electroencephalogram signals (1.0–30.0 Hz band pass) and EMG signals (30–100.0 Hz band pass) were amplified, filtered, digitized and stored electronically on a computer using the Data Exchange Matrix and Dataquest A.R.T 4.1 software (DSI, Saint Paul, MN, USA). The EEG and EMG signals were downloaded to a PC during the recordings. Throughout the sleep deprivation period rats remained in the solid bottom cage with a food hopper attached. The hopper was weighed every 2 d to measure food intake.
Sleep deprivation
Sprague-Dawley and OR rats (n=12/group) were subjected to PSD during the light phase (8 h/day beginning at 1000; 4 h after lights on and ending at 1800 (at the end of light cycle)) for 9 consecutive d after the 24 h baseline sleep recording. Sleep deprivation was achieved by exposing the animals to environmental noise (20, 21) (random street noises, vehicle horn, ambulance siren, hammering, sudden braking vehicle, bell, alarm, air plane sound etc.) by mounting a speaker inside the sound-attenuating box where the animals were placed during recording. The speaker was connected to an amplifier with digital audio player (Model: Insignia TMNS-R5101AHD-A). The sound sequence was 15 minutes long and was repeated for the 8 h duration of sleep deprivation. To prevent acclimation to the environmental noise, the noise events, duration of these events, frequency of sound (800 to 20000 Hz), amplitude (85 to 100 dB, average global intensity was 85 db) and inter-noise interval were randomly distributed. The events also consisted of periods of silence followed by sharp attack rate noises randomly distributed in the sound sequence. This amplitude and frequency has been shown previously to produce no damage to the rodent cochlea (20, 21). Since the rodent audiogram is different from the human audiogram and rodents have a better capacity to detect higher frequencies, we used high frequency sounds to match the rat audiogram. This adaptation was done using audio software Audacity (open source software) to translate frequencies between the human and rodent audiogram. Sound samples were selected from the Best Service Studio Box DVD3-Technical sample library (Best Service GmbH, Munchen, Germany), and were randomly arranged using Audacity (audio editor for recording, slicing and mixing audio clips) into a single 15 min track.
To identify behavioral states, EEG and EMG signals were visualized with the sleep scoring software NeuroScore (DSI, St. Paul, MN, USA) and sleep–wake behaviors were then scored manually on a personal computer as described previously (18). Briefly, consecutive 10-s epochs of EEG and EMG signals were graphically displayed on the computer monitor and epochs were classified into one of the following four behavioral states based on the EEG and EMG signal characteristics: (1) SWS (high-voltage EEG with low frequency slow waves, low-voltage EMG); (2) REM sleep (low-voltage and high frequency EEG combined with muscle atonia in EMG activity, with occasional shortduration, large amplitude deflections due to muscle twitches); (3) quiet wake (QW: lowvoltage fast EEG with EMG activity of a mean amplitude twice that observed in SWS); (4) active wake (AW: low-voltage fast EEG, sustained high-voltage EMG, with frequent movement deflections) as described previously (18). The appropriate EEG and EMG activity patterns needed to persist for a minimum of 15 s to assign an epoch to a valid behavioral state. Percent time spent in each state, number and mean duration of sleep–wake episodes for each behavioral state and total number of transitions between different stages were determined. The following were quantified for each recording session (either 8 h or 24 h) and then averaged over all the sessions: (a) total sleep time (SWS+REM); (b) percent time spent in wake (W+QW), SWS and REM sleep (c) total number of sleep–wake episodes; (d) mean duration of these episodes; (e) number of state transitions between different sleep–wake states and (f) SWS delta power.
For all animals in this study, body weight and food intake was determined on the baseline day (a day prior to beginning of PSD) and every other day throughout the PSD period. Cumulative food intake was determined as the sum of the total amount of food consumed by the rat over the duration of the PSD. We did not collect food spillage as it was not possible to do so in the solid bottom cage with bedding, without disruption of the animals’ behavior, and the primary endpoint was body weight. On visual inspection there was little food spilled. Body weight is expressed as change in body weight over the 9 d of PSD.
Statistics
Data were analyzed using Prism 5.0b (GraphPad Software, Inc., San Diego, CA) and XLSTAT (Addinsoft, New York, NY). These data are expressed as mean ± s.e.m. A significance level of 0.05 was used for all statistical tests. T-tests were used to determine the effect of PSD on sleep/wake parameters and the analysis was repeated separately (control vs. PSD) for SD and OR rats to compare the difference between control and PSD conditions.
One-way ANOVA followed by Tukey’s multiple comparison test was used to determine the effect of ‘recording day’ across the 9-d PSD period on the sleep/wake parameters. There was no main effect of recording day in both SD and OR rats during the PSD d, and therefore the sleep/wake parameters were averaged across the 9-d for both SD and OR groups.
To verify that the 8 h environmental noise partially reduced sleep time and to determine whether the effect of PSD differed across phenotypes, the sleep/wake data were analyzed by two-way ANOVA to identify the main effects of treatment (PSD and control conditions), phenotype (OR and SD) and treatment×phenotype interaction, followed by post-hoc testing with the Bonferroni T Test.
Cumulative food intake and body weight change data during sleep deprivation were subjected to two-way ANOVA (phenotype and treatment) followed by Bonferroni T Tests. To determine whether body weight change during PSD differed across phenotypes, change in body weight was analyzed by one-way ANCOVA with baseline body weight as a covariate to control for baseline differences in body weight between OR and SD rats.
Results
Verification that environmental noise produces PSD
To first confirm that environmental noise results in PSD, sleep–wake variables were compared between the control EEG/EMG recording and during PSD in SD and OR rats (Fig. 1A and B). Since PSD occurred during the light phase (1000–1800), the sleep/wake parameters were compared between the corresponding 8 h control (non-sleep deprivation conditions) recording time period and 8 h PSD period. There was no effect of recording day on the sleep/wake data indicating that sleep/wake was similar across 9 d of PSD and thus the data were averaged across the 9 d.
Figure 1.
Percent time spent in wake (W), REM sleep (RS) and slow-wave-sleep (SWS) in the 8 h recording period in OR (A, OR) and Sprague-Dawley (B, SD) rats. Percent change in W, RS and SWS from baseline in OR and SD rats (C). During partial sleep deprivation (PSD), both groups of rats spent more time in W and less time in SWS and RS. Results are expressed as percent of total recording time, and represented as mean ± S.E.M. N=6/group. **P < 0.01, ***P < 0.001 as compared to respective controls. πP < 0.05 as compared to W in SD rats during control recording conditions.
During the 8 h control recording conditions, time spent in SWS, and REM sleep were similar in OR and SD rats. However, the OR rats spent more time in wake than SD rats during control conditions (P < 0.05, 42.83 ± 2.96 vs. 49.58 ± 3.04, SD vs. OR). When compared to respective controls, PSD significantly increased the time spent in W and reduced the time spent in SWS and REM sleep in both OR and SD rats (P < 0.001, Fig. 1A, B). Total time spent in sleep was also significantly (P < 0.001) less during PSD compared to control conditions in OR and SD rats, indicating that exposure to random street noise reduces total time spent in sleep (OR: P < 0.0001, 52.08 ± 1.6% vs. 31.33 ± 3.1% and SD: P < 0.0001, 58 ± 1.9% vs. 36 ± 1.5%). Our results demonstrate that the PSD method used for this study, effectively reduced the total amount of sleep in both OR (by 40%) and SD (by 48%) animals (Fig. 1C).
The ANOVA results indicated that phenotype alone or the phenotype X treatment interaction did not affect changes in sleep/wake times during PSD, indicating that environmental noise increased wake in OR and SD rats to similar levels (OR: 69.33 ± 2.74% vs. SD: 63.75 ± 1.9%). However, as mentioned before, during control conditions, the OR rats spent slightly more time in wake than the SD rats (F (1,20) = 9.618, P < 0.05, 49.58 ± 3.04% vs. 42.83 ± 2.98; OR vs. SD).
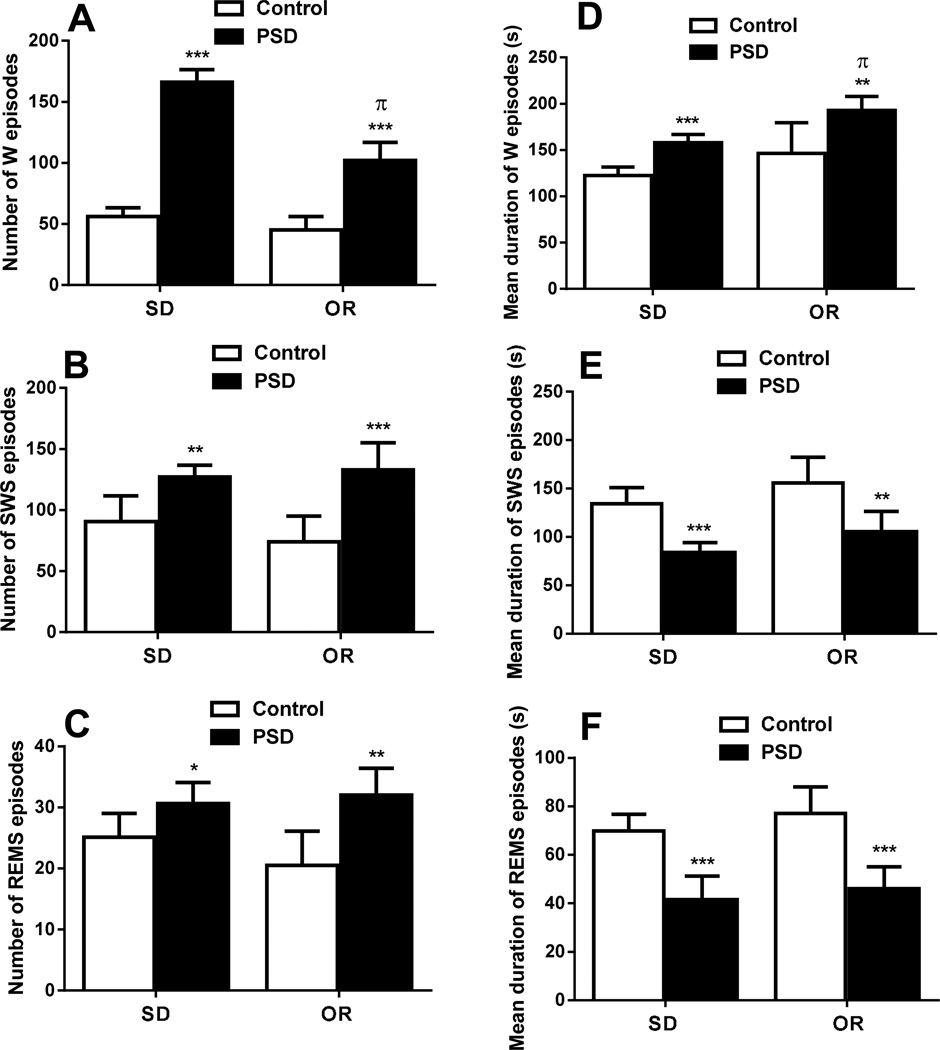
Sleep structure during PSD
To understand sleep structure, mean number and duration of the individual episodes of each sleep–wake state were compared during sleep deprivation and control conditions. Our PSD method resulted in significantly higher number of wake (P < 0.001), SWS (P < 0.01) and REM sleep (P < 0.05) episodes in SD rats during the 8 h of PSD (Fig. 2 A, B, C). Similarly, in OR rats PSD resulted in more wake (P < 0.001), SWS (P < 0.001) and REM sleep (P < 0.01) episodes (Fig. 2 A, B, C). The increased number of episodes was associated with an increased mean duration of W episodes (P < 0.001) and decreased duration of SWS (P < 0.001) and REM sleep episodes (P < 0.001) in SD rats (Fig. 2 D, E, F). Like SD rats, OR rats also showed increased duration of W episodes (P < 0.01) and decreased duration of SWS (P < 0.01) and REM sleep (P < 0.001) episodes during PSD protocol (Fig. 2 D, E, F). The increased number and decreased duration of REM sleep and SWS indicate severe sleep fragmentation by the environmental noise method of sleep deprivation.
Figure 2.
Average number of wake (W), slow-wave-sleep (SWS) and REM sleep (REMS) episodes (A,B,C), and average duration (in sec) of W, SWS and REMS episodes (D,E.F) in obesity resistant (OR) and Sprague-Dawley (SD) rats. A, B and C represent the number of episodes during the 8 h recording period, of W, SWS and REMs respectively. D, E and F represent the average duration of episodes during the 8 h recording period, of W, SWS and REMs respectively. Results are expressed as means ± S.E.M. n = 6/group. *P < 0.05, **P < 0.01 and ***P < 0.001 as compared to controls. πP < 0.001 as compared to number of W episodes and duration of W episodes in SD rats during sleep deprivation (PSD).
PSD resulted in increased number of SWS and REM sleep episodes, (which was likely caused by the increased sleep pressure during and after PSD), but decreased duration of SWS and REM sleep episodes. Increased W time in the PSD animals was due to both increased number and prolonged duration of W episodes. The sleep-deprived SD rats had higher (P < 0.001, 102.66 ± 6.02 vs. 166.33 ± 6.14; OR vs. SD) number of wake episodes than the sleep-deprived OR rats, showing an interaction effect between phenotype and treatment. However, wake episode duration was significantly higher in sleep-deprived OR rats than in sleep-deprived SD rats (P < 0.001, 193.00 ± 6.14 vs. 158.00 ± 6.14; OR vs. SD).
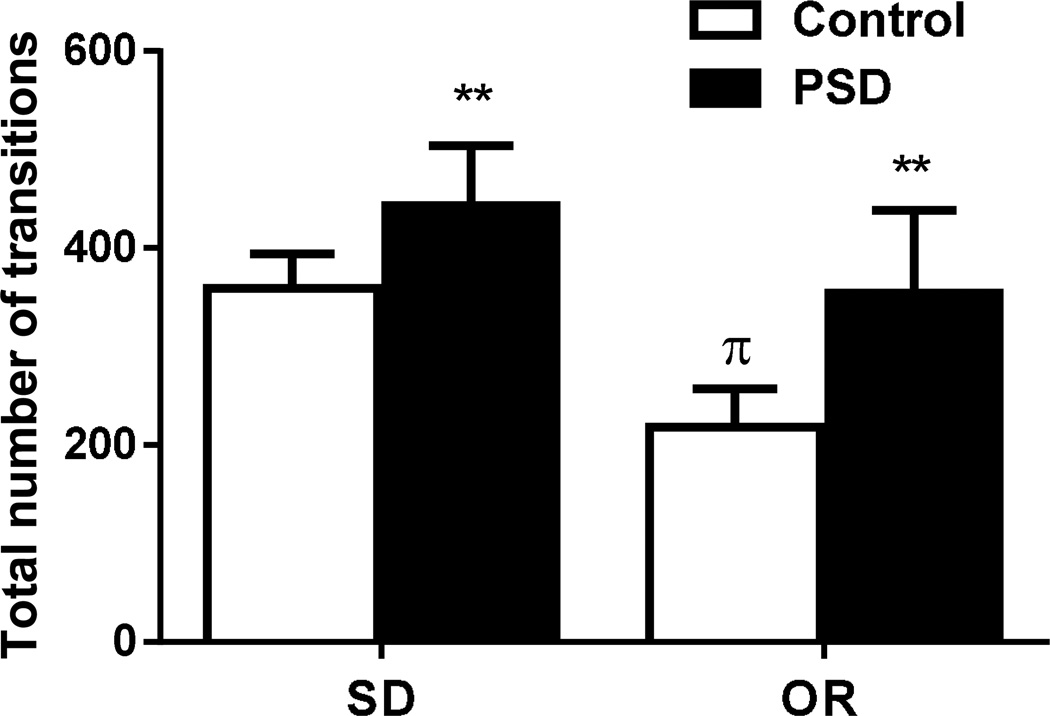
Transitions between sleep–wake stages
Stage shifts or transitions between different stages during the 8 h recording period were analyzed as a measure of sleep quality. The results showed increased number of stage transitions in sleep-deprived OR (P < 0.01) and SD (P < 0.01. Fig. 3) rats compared to their respective controls. During baseline there were fewer transitions in the OR rats as compared to the SD rats (OR vs. SD: P < 0.001, 218.66 ± 16.32 vs. 359.16 ± 14.28) indicating that OR rats had a less fragmented, more consolidated sleep–wake pattern under control conditions. Our results demonstrate that the noise technique of PSD decreases sleep quality in addition to reducing total sleep time.
Figure 3.
The total number of transitions between stages during the 8 h recording period in Sprague-Dawley (SD) and OR rats. Both groups of rats had significantly higher transitions between stages during sleep deprivation (PSD). Results are expressed as means ± S.E.M. N=6/group. **P < 0.01 compared to respective controls. πP < 0.001 as compared to SD rats during the control recording condition.
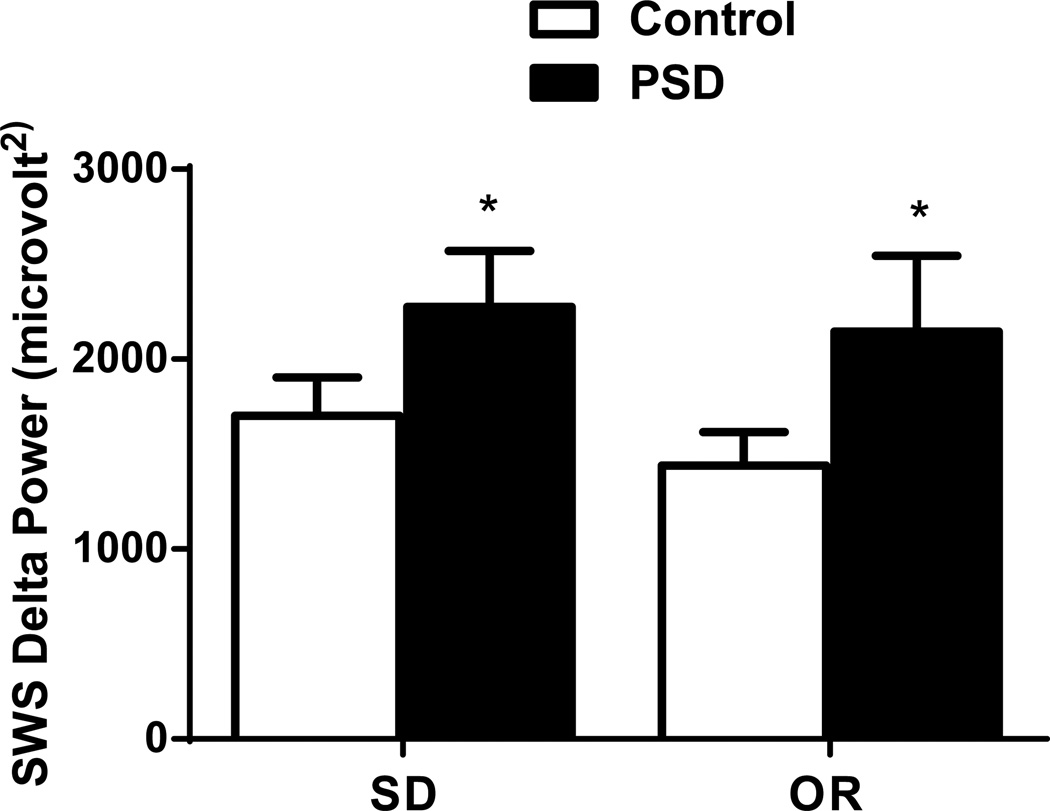
SWS delta power
To obtain a measure of sleep drive during the PSD protocol, we compared mean power density in the EEG delta band (0.5–4 Hz) during the residual SWS between sleep-deprived and control rats. EEG slow-wave activity during SWS was significantly (P < 0.05) higher in sleep-deprived OR rats compared with control OR rats. Similarly, sleep-deprived SD rats had significantly (P < 0.05, Fig. 4) higher SWS delta power during the 8 h of sleep deprivation. Though under control conditions OR rats had lower SWS delta power than SD rats, this was not statistically significant. Similarly, both SD and OR rats were identical in terms of SWS delta power during sleep deprivation. Thus, the PSD method used for this study also increases sleep drive independent of phenotype.
Figure 4.
Total power in the delta band during SWS in sleep deprived Sprague-Dawley (SD) and OR rats during 8 h of PSD or not (control conditions). Both groups of rats had significantly higher SWS delta power during sleep deprivation (PSD). Results are expressed as mean ± S.E.M. N = 6/group. *P < 0.01 compared to control SD and OR rats, respectively.
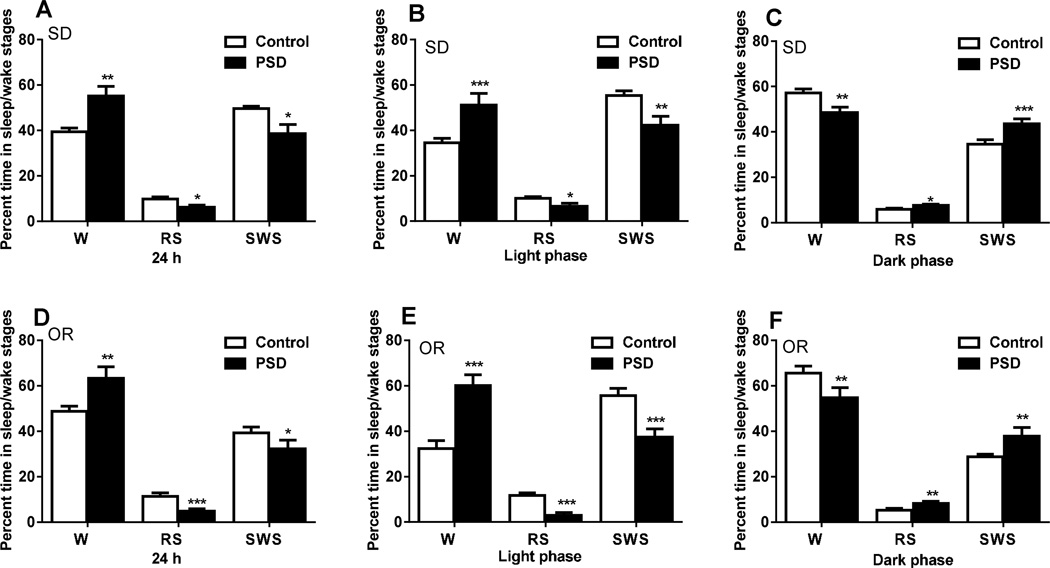
Twenty four h sleep/wake duration in PSD rats
Our results indicated that PSD by noise reduced rest phase sleep. To confirm that environmental noise induced PSD during the rest phase results in active period sleep, we compared 24 h sleep–wake variables between control conditions and PSD conditions in SD and OR rats (n = 6/group; Fig. 5 A–F). Time spent in SWS (P < 0.05), and REM sleep (P < 0.05) was significantly less, and time spent in W was significantly higher (P < 0.01) in PSD SD rats for the 24 h recording (Fig. 5A). Similarly, time spent in SWS (P < 0.05), and REM sleep (P < 0.001) were significantly less, and time spent in W was significantly higher (P < 0.01) in PSD OR rats for the 24 h period (Fig. 5D). When compared to the control conditions (non sleep deprived), PSD significantly increased the time spent in W (P < 0.001), and reduced the time spent in SWS (P < 0.01) and REM sleep (P < 0.05) in SD rats during the light (rest) phase (Fig. 5B). Like SD rats, PSD significantly increased the time spent in W (P < 0.001), and reduced the time spent in SWS (P < 0.001) and REM sleep (P < 0.001) in OR rats during the light phase (Fig. 5E). Our results demonstrate that the PSD method used for this study, effectively reduced 24 h and light phase sleep in both OR and SD animals, a finding similar to the result of 8 h recording.
Figure 5.
Percent time spent in wake (W), REM sleep (RS) and slow-wave-sleep (SWS) over the 24 h recording period (A), light phase (B) and dark phase (C) in control and PSD SD rats. Percent time spent in W, RS and SWS over the 24 h recording period (D), light phase (E) and dark phase (F) in PSD and Control OR rats. PSD rats from both groups of rats spent more time in W and less time in SWS and RS during the entire 24 h period and in the light phase. In contrast, PSD rats from both groups of rats spent less time in W and more time in SWS and RS during the 12 h active (dark) phase. Results are expressed as the percent of total recording time, and are represented as mean ± S.E.M. N=6/group. *P < 0.05, **P < 0.01 and ***P < 0.001 as compared to respective controls.
We next analyzed these sleep/wake variables for the 12 h dark (active) phase, predicting that sleep restriction during the rest phase might increase sleep rebound during the active phase. Our results indeed showed that compared to the respective controls, PSD significantly decreased the time spent in W (P < 0.001), and increased time spent in SWS (P < 0.001) and REM sleep (P < 0.05) in SD rats during the active phase (Fig. 5C). Similarly, PSD significantly decreased the time spent in W (P < 0.01), and increased the time spent in SWS (P < 0.01) and REM sleep (P < 0.01) in OR rats during the dark phase (Fig. 5F). Our results demonstrate that the PSD method used for this study, effectively reduced rest phase sleep and increased active phase sleep in both OR and SD animals, resembling human EDS.
Baseline body weight and food intake
Before sleep deprivation, OR rats weighed significantly less than the SD rats (OR vs. SD: 327.41 ± 5.8 vs. 442.0 ± 20.25 g, P < 0.001) independent of treatment (PSD vs. control) group, despite similar daily food intake (23.91 ± 3.8 vs. 22.8 ± 1.8, P = 0.17). Body weights were not different between the rats selected for PSD and control conditions, within the OR and SD groups.
Body weight and food intake during sleep deprivation
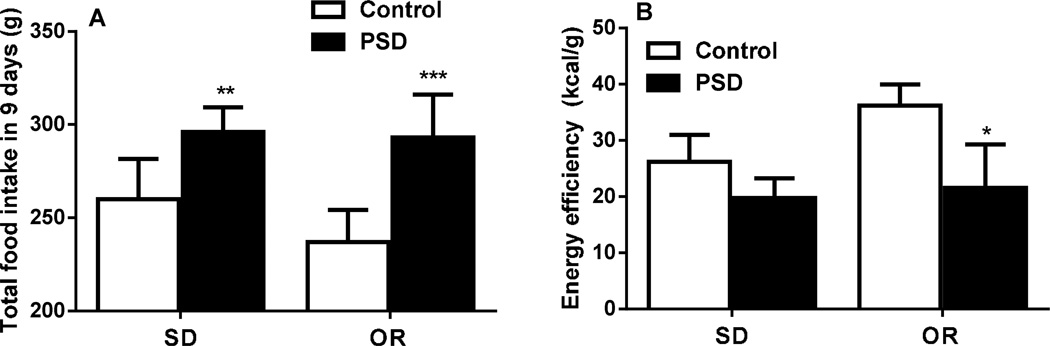
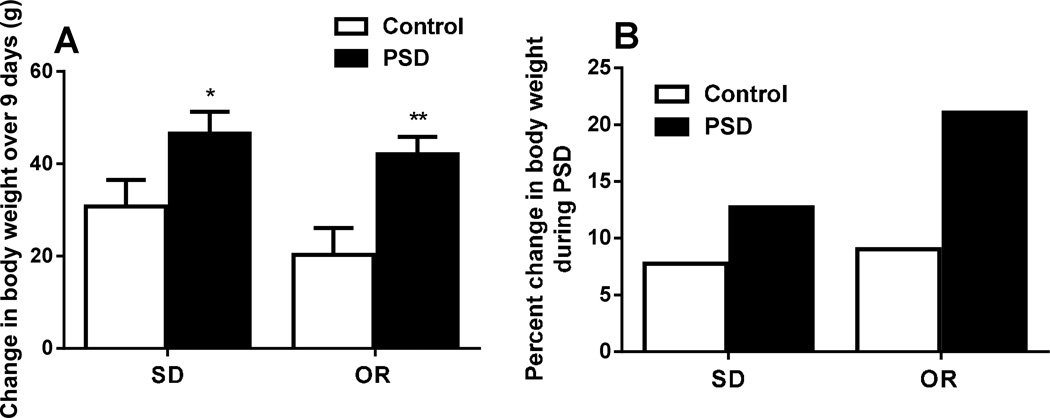
Sleep deprivation by environmental noise significantly increased cumulative food intake over 9 d of sleep deprivation in both OR (P < 0.001) and SD (P < 0.01) rats compared to respective controls (SD: PSD vs. control: 296.00 ± 13.30 vs. 260.00 ± 21.50, F (1,20) = 40.56, P < 0.01 and OR: PSD vs. control: 293.00 ± 23.01 vs. 237.00 ± 26.8 g, F (1,20) = 40.56, P < 0.001, Fig. 6A). The food intake was not different between OR-PSD and SD-PSD groups (P = 0.41). Moreover, body weight gain from day 1 to day 9 of sleep deprivation was significantly greater in sleep-deprived OR (F (1,20) = 20.92, P < 0.01, Fig. 7) and SD (F (1,20) = 20.92, P < 0.05, Fig. 7) rats compared with control OR and SD rats. Analysis of energy efficiency (kcal/g) over the period of PSD revealed that PSD in both SD and OR rats resulted in lower energy efficiency compared to respective controls, however, this reached significance only in OR PSD rats (P < 0.05, Fig. 6B). Similarly, both OR and PSD rats showed weight gain over 9 d of PSD. However, percent change in body weight from baseline was higher in OR PSD rats than in SD PSD rats (Fig. 7B).
Figure 6.
Cumulative food intake (A) and energy efficiency (B) over 9 days in sleep deprived (PSD) and Control, Sprague-Dawley (SD) and OR rats. Both groups of rat had significantly higher food intake during sleep deprivation. OR PSD rats exhibited significantly lower energy efficiency than Control OR rats. Results are expressed as means ± S.E.M. N=6/group. *P < 0.05, **P < 0.01 and ***P < 0.001 compared to respective controls. Note that food spillage was not collected; thus energy efficiency measures are based on uncorrected food intake values.
Figure 7.
Body weight change over 9 days in sleep deprived (PSD) and control Sprague-Dawley (SD) and OR rats (A). Percent change in body weight from baseline in PSD and control conditions in OR and SD rats (B). Both groups of rats gained significantly higher body weight due to sleep deprivation. Percent change from baseline was higher in OR rats than in SD rats. Results are expressed as means ± S.E.M. N=6/group. *P < 0.05 and **P < 0.01 compared to control SD and OR rats respectively.
Daily food intake and body weight changes in OR rats during sleep deprivation
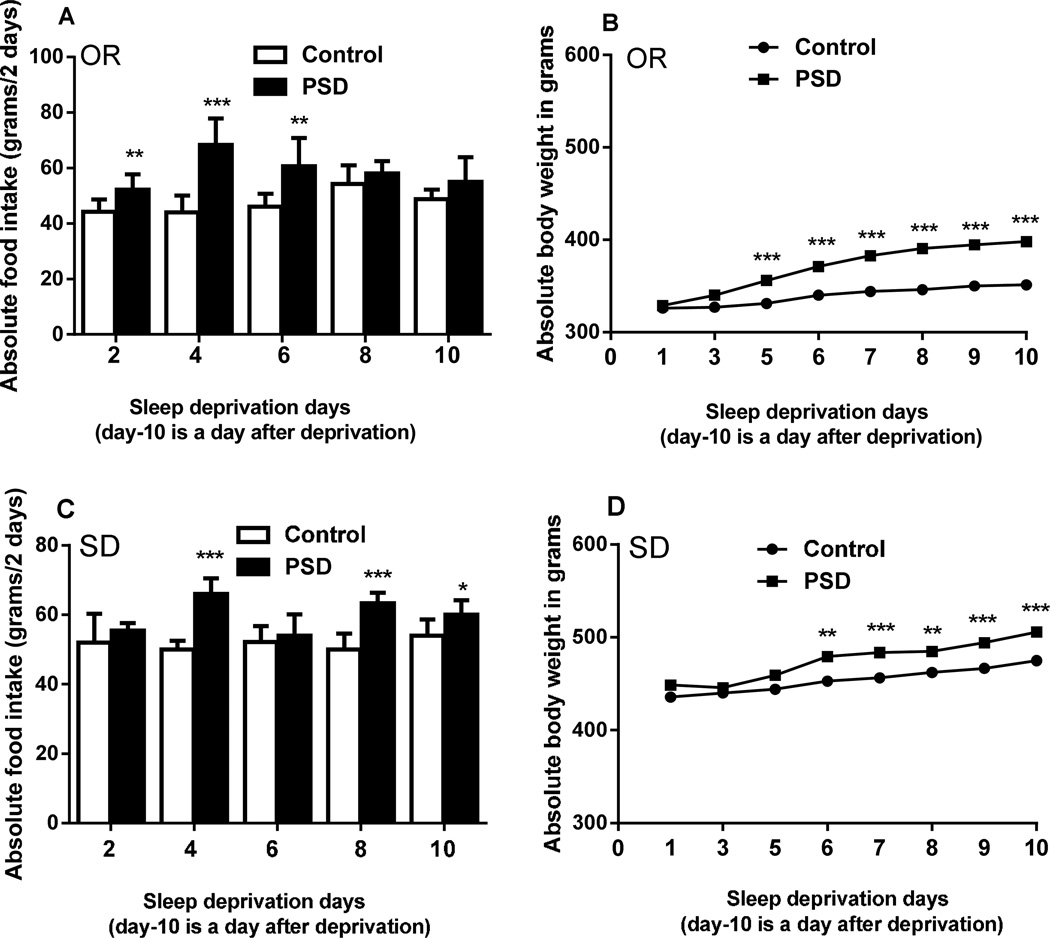
As illustrated in Figure 8 sleep-deprived OR rats’ food intake was higher on all d of PSD, and reached statistical significance on the 2nd (P < 0.01), 4th (P < 0.001) and 6th (P < 0.01, Fig. 8A) d of PSD. Similarly, the analysis indicated that sleep-deprived OR rats’ body weight was significantly higher on the 5th (P < 0.001) day and remained significantly greater through the end of the study (Fig. 8B).
Figure 8.
Daily food intake (A) and body weight (B) in sleep deprived (PSD) and Control OR rats. Both food intake and body weights were higher in sleep deprived OR rats compared to control OR rats. Daily food intake (C) and body weight (D) in sleep deprived (PSD) and Control Sprague-Dawley (SD) rats. Both food intake and body weights were higher in sleep deprived SD rats compared to control SD rats. Results are expressed as means ± S.E.M. N=6/group. *P < 0.05, **P < 0.01 and ***P < 0.001 compared to respective controls.
Like sleep-deprived OR rats, sleep-deprived SD rats’ food intake was higher throughout the deprivation period, and reached statistical significance on the 4th (P < 0.001), 8th (P < 0.001) and 10th (P < 0.05, Fig. 8C) d of PSD. Similarly, the analysis indicated that sleep-deprived SD rats’ body weight was significantly higher on the 6th day (P < 0.01), and remained significantly greater through the end of the study (day 7 (P < 0.001), 8 (P < 0.01), 9 (P < 0.001) and 10 (one day after conclusion of sleep deprivation, P < 0.001, Fig. 8D). Thus in both groups of OR and SD rats, increased food intake was followed by higher weight gain, but unexpectedly the differences in cumulative food intake between control and PSD conditions (P < 0.05, 57.16 ± 6.61 vs. 37.03 ± 8.40 g; OR vs. SD) was more pronounced and of earlier onset (day 2 vs. day 4) in OR rats.
To determine whether body weight change following PSD differed across phenotypes, change in body weight was analyzed by one-way ANCOVA with baseline (prior to PSD) body weight as a covariate to control for baseline differences in body weight between OR and SD rats. The analysis showed that change in body weight was not different between OR and SD rats F (1,11) = 4.06, P = 0.075. Thus, weight change during PSD was not statistically different between OR and SD rats (OR vs. SD; 46.5 ± 6.86 vs. 42.1 ± 3.45; P = 0.29).
Discussion
We exposed rats to random street noise for 8 h per day for 9 consecutive d, resulting in partial sleep deprivation, elevated sleep drive, hyperphagia, and weight gain. To our knowledge, this is the first demonstration of noise induced partial sleep deprivation that results in weight gain in rats, similar to the phenotype exhibited by modern day humans with PSD. The noise provision procedure is less severe than standard rodent sleep deprivation methods that employ more rigorous stressors, for example exposure to cold water or forced physical activity. These data show that daily exposure to environmental noise results in sleep deprivation and sleep fragmentation, indicative of poor quality sleep. These results are consistent with earlier animal and human studies, which indicate that unpredictable environmental noise exposure induces sleep disturbance (20, 21). Our results are also in accord with a recent human study showing that exposure to noise is associated with elevated risk of obesity and metabolic disorders (1).
The finding of hyperphagia and body weight gain in rats normally resistant to obesity highlights the critical role that sleep – both amount and quality - plays in maintaining a healthy body weight. It is possible that increased response to PSD might underlie the observed differences in food intake and body weight between OR and SD rats. For example, high fat diet (HFD) is considered to be a stressor resulting in hypothalamic pituitary adrenal (HPA) axis activation and increased serum cortisol (CORT) levels, and a study showed differential stress response in OR rats compared to OP rats (22). Data from Shin and colleagues (22) showed an enhancement in corticotrophin releasing hormone (CRH) and serum CORT levels following HFD in OR rats compared to DIO rats indicating a heightened stress response (HPA axis function). Although acute stress enhances CORT levels and suppresses food intake, a chronic increase in CORT could contribute to hyperphagia and obesity by decreasing CRH levels in a negative feedback manner (23). Moreover, OR rats express higher monoaminergic tone, a likely mediator of PSD stress. PSD may have stimulated paraventricular nucleus (PVN) CRH and hence CORT, indicating a heightened response to stress (22). Similarly, basal CRH and CORT levels are higher in OR rats compared with OP rats and these levels go even higher when exposed to unpredictable stress (17), again indicating greater response to stress in OR rats. All these might have contributed to elevated food intake and body weight in PSD OR rats.
In the present study, the sleep-deprived rats exhibited a greater number of, and more prolonged, waking episodes, which contributed to an overall increase in time spent awake. In contrast, the time spent in SWS and REM sleep was lower in PSD rats due to a shorter duration of these episodes, and in spite of increased total number of SWS and REM sleep episodes. Increased numbers of episodes indicate that sleep deprivation by environmental noise decreases sleep quality (more fragmentation) and elevates sleep drive, which was empirically demonstrated by the finding of enhanced SWS delta power (24). High sleep drive during the active phase may have resulted in less physical activity and energy expenditure, enhancing the observed weight gain. Supporting this idea, the 24 h recordings show that PSD rats slept more during the active phase. This would be similar to human EDS, in which more sleep during the day lowers physical activity and energy expenditure, and increases weight gain (4, 5, 25). The ability of this method of PSD to induce weight gain is in contrast to effects on weight in other animal sleep deprivation models, and is likely due to the less severe method used to disrupt sleep (11–13, 26–28). Although impossible to completely separate sleep deprivation effects from “stress”, as sleep deprivation is stressful in and of itself, models in which the impact of physiological stress is minimized have been recently developed, which includes the moving disc method and the gentle handling methods (29). However, these methods also introduce unrelated variables like physical activity and physical proximity of the experimenter to the animal. Thus, we developed an environmental noise exposure method that minimizes extraneous stress, physical activity and experimenter physical proximity.
Consistent with many earlier sleep deprivation studies that showed hyperphagia following sleep deprivation in rodents (11, 26, 27, 30), in the present study food intake was increased throughout the period of sleep deprivation independent of phenotype. In contrast, some studies have shown lack of hyperphagia during sleep deprivation, which was suggested to be due to a shorter duration of sleep deprivation (4 to 6 d) in those studies (31–33). In OR rats the increased food intake reached significance on day 2 compared to non-sleep deprived animals, suggesting they may be more sensitive to sleep deprivation. It is important to note however that food spillage was not measured due to feasibility, and thus the magnitude of intake could be artificially high. We do not suspect a large amount of spillage as visual inspection did not reveal such, and based on past experience we also do not suspect a large difference between food spillage of OR and SD rats.
One study consistent with the current results showed that 72h of REM sleep deprivation increased intake of carbohydrate rich food and body weight gain in rats (10). Similarly, a recent study showed that chronically sleep-restricted (18 h per day for ten d) rats exhibit less weight loss compared to rats with total sleep deprivation (14), suggesting that unlike total sleep deprivation, sleep restriction (with some daily sleep opportunities) might increase body weight. Our results are in line with human studies demonstrating increased hunger and appetite, increased food intake, decreased energy expenditure and increased body weight after sleep restriction (5–25). The decreased energy expenditure here appears due to excessive active period sleep and lower physical activity (34), as suggested by the 24 h recording, which show enhanced sleep during the active phase in PSD rats.
Another mechanism underlying PSD-induced weight gain in the current studies may be reduced amounts of REM sleep during the rest phase and increased REM sleep during the active phase. The 24 h recording showed that PSD during the rest phase corresponded to increased REM sleep during the active (dark) phase. Adequate amounts of REM sleep during the resting phase appears to be important for proper body weight maintenance (18). Narcolepsy/cataplexy, due to the loss of orexin-containing neurons or orexin receptors, increases REM sleep propensity and sleep onset REM periods during the active period and has been also associated with increased BMI (35). This indicates that daytime REM sleep might impair energy metabolism. Studies demonstrate an association between elevated body weight and decreased nocturnal total sleep and REM sleep in humans (36). Also it was suggested that endocrine changes like reduced leptin and increased ghrelin were more sensitive to reduced REM sleep during the rest phase (36). On the other hand, weight loss in humans significantly increases the percent of nighttime REM sleep and SWS (7). Similarly, obese ob/ob mice spent less time in REM sleep during the light (resting) phase compared with wild-type animals (13). This indicates that normal amounts of REM sleep during the rest phase might be crucial for normal body weight maintenance, and reductions in rest phase REM sleep may have enhanced active phase REM sleep and increased weight gain in the present study.
Our results indicate that enhanced food intake preceded increased body weight gain. Elevated food intake during sleep deprivation may be due to reductions in REM sleep as an earlier study showed that REM sleep deprivation during light phase enhances food intake (31). Further, our earlier study showed that OR rats have decreased sleep time during the dark, active phase (18). Our newly developed PSD method increased active phase sleep and body weight in SD and OR rats. Also, in diet induced obese mice, magnitude of weight gain was associated with increased active phase sleep time (15). Similarly, obese leptin-deficient ob/ob mice, leptin-resistant db/db mice and obese Zucker rats exhibit more sleep during the dark (active) phase, indicating poor quality sleep analogous to human EDS (7, 13, 37). The current results are consistent with these experimental findings and for the first time show that poor sleep quality during rest period leads to enhanced food intake and weight gain even in obesity resistant rats, which is likely due to recovery sleep during active phase. However, future studies with recordings of temporal patterns of feeding during sleep deprivation are necessary to further support this idea.
The results also show that increased food intake and body weight were accompanied by increased sleep fragmentation, which is similar to human studies showing a positive association between highly fragmented sleep and body mass index (1, 2, 6). Likewise, many rodent models show an association between sleep fragmentation and obesity, which includes obese leptin-deficient mice, leptin-resistant mice, obese Zucker rats and obesity resistant (OR) rats (13, 18, 37). Similarly, surgical weight loss results in a significant reduction in sleep fragmentation in humans (7). Thus, it is possible that enhanced body weight gain in OR and SD rats in the present study might also be partly due to sleep fragmentation, a measure of sleep quality.
There are several potential neurochemical mechanisms for the current findings. Sleep deprivation decreases circulating leptin, (3, 11), up-regulates neuropeptide Y (NPY) and down-regulates α-melanocyte stimulating hormone (α-MSH) in the hypothalamic arcuate nucleus (26). Sleep rebound following sleep deprivation also alters availability of orexin or orexin receptors (38). Thus, reduced availability of orexin might have reduced thermogenesis (both sympathetic nervous system stimulation induced and non-exercise activity thermogenesis), as orexin is a key player in energy expenditure. Decreased energy expenditure resulting from decreased orexin functioning during PSD rebound periods (active phase), combined with an increased behavioral drive to eat during PSD (resulting from, for instance, altered NPY and α-MSH signaling (26, 32, 39)) - may have together contributed to increased body weight. These suggestions are consistent with human sleep restriction studies, which show that feelings of hunger and the desire to eat calorie-dense foods are accompanied with changes in serum leptin and ghrelin following experimental sleep deprivation (3, 25), and a recent study in mice showing enhanced sleep during active phase following sleep disturbance during the rest phase (40).
In summary, the current data show that chronic PSD by environmental noise results in hyperphagia and weight gain, even in rats resistant to obesity, highlighting the idea that proper amounts of good quality sleep are necessary for normal body weight maintenance. These data demonstrate a new model for PSD-induced weight gain in rats, which is more similar to findings in humans. Further studies are necessary to assess the relative contributions of energy intake and energy expenditure in sleep deprivation induced weight gain and to further investigate the brain mechanisms involved in this model of PSD.
Acknowledgements
Funding for this publication was provided by the Department of Veterans Affairs CDA-2 F7212W (to JAT); NIH R01DK078985 (to CMK), NIH P30 DK050456 (to CJB) and NIH T32DK083250 (to CJB, CMK and VM) from the National Institute of Diabetes and Digestive and Kidney Diseases; and a grant from the Obesity Society (to JAT).
Footnotes
Disclosure: This was not an industry-supported study. The authors have no financial conflicts of interest.
References
- 1.Stamatakis KA, Punjabi NM. Effects of sleep fragmentation on glucose metabolism in normal subjects. Chest. 2010;137(1):95–101. doi: 10.1378/chest.09-0791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.von Kries R, Toschke AM, Wurmser H, Sauerwald T, Koletzko B. Reduced risk for overweight and obesity in 5- and 6-y-old children by duration of sleep--a crosssectional study. Int J Obes Relat Metab Disord. 2002;26(5):710–716. doi: 10.1038/sj.ijo.0801980. [DOI] [PubMed] [Google Scholar]
- 3.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 4.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. Plos Med. 2004;1(3):e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vgontzas AN, Bixler EO, Chrousos GP, Pejovic S. Obesity and sleep disturbances: meaningful sub-typing of obesity. Arch Physiol Biochem. 2008;114(4):224–236. doi: 10.1080/13813450802521507. [DOI] [PubMed] [Google Scholar]
- 6.van den Berg JF, Knvistingh Neven A, Tulen JH, Hofman A, Witteman JC, Miedema HM, et al. Actigraphic sleep duration and fragmentation are related to obesity in the elderly: the Rotterdam Study. Int J Obes. 2008;32(7):1083–1090. doi: 10.1038/ijo.2008.57. [DOI] [PubMed] [Google Scholar]
- 7.Kalra M, Mannaa M, Fitz K, Kumar S, Chakraborty R, Sheng X, et al. Effect of surgical weight loss on sleep architecture in adolescents with severe obesity. Obes Surg. 2008;18(6):675–679. doi: 10.1007/s11695-008-9472-4. [DOI] [PubMed] [Google Scholar]
- 8.Chaput JP, Despres JP, Bouchard C, Tremblay A. Longer sleep duration associates with lower adiposity gain in adult short sleepers. Int J Obes. 2012;36(5):752–756. doi: 10.1038/ijo.2011.110. [DOI] [PubMed] [Google Scholar]
- 9.Jung CM, Melanson EL, Frydendall EJ, Perreault L, Eckel RH, Wright KP. Energy expenditure during sleep, sleep deprivation and sleep following sleep deprivation in adult humans. J Physiol. 2011;589(Pt 1):235–244. doi: 10.1113/jphysiol.2010.197517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhanot JL, Chhina GS, Singh B, Sachdeva U, Kumar VM. REM sleep deprivation and food intake. Indian journal of physiology and pharmacology. 1989;33(3):139–145. [PubMed] [Google Scholar]
- 11.Everson CA. Clinical assessment of blood leukocytes, serum cytokines, and serum immunoglobulins as responses to sleep deprivation in laboratory rats. Am J Physiol Regul Integr Comp Physiol. 2005;289(4):R1054–R1063. doi: 10.1152/ajpregu.00021.2005. [DOI] [PubMed] [Google Scholar]
- 12.Rechtschaffen A, Bergmann BM, Everson CA, Kushida CA, Gilliland MA. Sleep deprivation in the rat: X3. Integration and discussion of the findings. 1989. Sleep. 2002;25(1):68–87. [PubMed] [Google Scholar]
- 13.Mavanji V, Billington CJ, Kotz CM, Teske JA. Sleep and obesity: a focus on animal models. Neurosci Biobehav Rev. 2012;36(3):1015–1029. doi: 10.1016/j.neubiorev.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caron AM, Stephenson R. Energy expenditure is affected by rate of accumulation of sleep deficit in rats. Sleep. 2010;33(9):1226–1235. doi: 10.1093/sleep/33.9.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guan Z, Vgontzas AN, Bixler EO, Fang J. Sleep is increased by weight gain and decreased by weight loss in mice. Sleep. 2008;31(5):627–633. doi: 10.1093/sleep/31.5.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laposky AD, Bradley MA, Williams DL, Bass J, Turek FW. Sleep-wake regulation is altered in leptin-resistant (db/db) genetically obese and diabetic mice. Am J Physiol Regul Integr Comp Physiol. 2008;295(6):R2059–R2066. doi: 10.1152/ajpregu.00026.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levin BE, Richard D, Michel C, Servatius R. Differential stress responsivity in diet-induced obese and resistant rats. Am J Physiol Regul Integr Comp Physiol. 2000;279(4):R1357–R1364. doi: 10.1152/ajpregu.2000.279.4.R1357. [DOI] [PubMed] [Google Scholar]
- 18.Mavanji V, Teske JA, Billington CJ, Kotz CM. Elevated sleep quality and orexin receptor mRNA in obesity-resistant rats. Int J Obes (Lond) 2010;34(11):1576–1588. doi: 10.1038/ijo.2010.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teske JA, Levine AS, Kuskowski M, Levine JA, Kotz CM. Elevated hypothalamic orexin signaling, sensitivity to orexin A, spontaneous physical activity in obesity-resistant rats. Am J Physiol Regul Integr Comp Physiol. 2006;291(4):R889–R899. doi: 10.1152/ajpregu.00536.2005. [DOI] [PubMed] [Google Scholar]
- 20.Rabat A, Bouyer JJ, Aran JM, Le Moal M, Mayo W. Chronic exposure to an environmental noise permanently disturbs sleep in rats: inter-individual vulnerability. Brain Res. 2005;1059(1):72–82. doi: 10.1016/j.brainres.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 21.Ouis D. Exposure to Nocturnal Road Traffic Noise: Sleep Disturbance and its After Effects. Noise Health. 1999;1(4):11–36. [PubMed] [Google Scholar]
- 22.Shin AC, MohanKumar SM, Sirivelu MP, Claycombe KJ, Haywood JR, Fink GD, et al. Chronic exposure to a high-fat diet affects stress axis function differentially in diet-induced obese and diet-resistant rats. Int J Obes (Lond) 2010;34(7):1218–1226. doi: 10.1038/ijo.2010.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dallman MF, la Fleur SE, Pecoraro NC, Gomez F, Houshyar H, Akana SF. Minireview: glucocorticoids--food intake, abdominal obesity, and wealthy nations in 2004. Endocrinology. 2004;145(6):2633–2638. doi: 10.1210/en.2004-0037. [DOI] [PubMed] [Google Scholar]
- 24.Brunner DP, Dijk DJ, Borbely AA. Repeated partial sleep deprivation progressively changes in EEG during sleep and wakefulness. Sleep. 1993;16(2):100–113. doi: 10.1093/sleep/16.2.100. [DOI] [PubMed] [Google Scholar]
- 25.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koban M, Le WW, Hoffman GE. Changes in hypothalamic corticotropinreleasing hormone, neuropeptide Y, proopiomelanocortin gene expression during chronic rapid eye movement sleep deprivation of rats. Endocrinology. 2006;147(1):421–431. doi: 10.1210/en.2005-0695. [DOI] [PubMed] [Google Scholar]
- 27.Koban M, Sita LV, Le WW, Hoffman GE. Sleep deprivation of rats: the hyperphagic response is real. Sleep. 2008;31(7):927–933. [PMC free article] [PubMed] [Google Scholar]
- 28.Suchecki D, Antunes J, Tufik S. Palatable solutions during paradoxical sleep deprivation: reduction of hypothalamic-pituitary-adrenal axis activity and lack of effect on energy imbalance. J Neuroendocrinol. 2003;15(9):815–821. doi: 10.1046/j.1365-2826.2003.01067.x. [DOI] [PubMed] [Google Scholar]
- 29.Datta S, Mavanji V, Ulloor J, Patterson EH. Activation of phasic pontine-wave generator prevents rapid eye movement sleep deprivation-induced learning impairment in the rat: a mechanism for sleep-dependent plasticity. J Neurosci. 2004;24(6):1416–1427. doi: 10.1523/JNEUROSCI.4111-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barf RP, Desprez T, Meerlo P, Scheurink AJ. Increased food intake and changes in metabolic hormones in response to chronic sleep restriction alternated with short periods of sleep allowance. Am J Physiol Regul Integr Comp Physiol. 2012;302(1):R112–R117. doi: 10.1152/ajpregu.00326.2011. [DOI] [PubMed] [Google Scholar]
- 31.Elomaa E. The light/dark difference in meal size in the laboratory rat on a standard diet is abolished during REM sleep deprivation. Physiol Behav. 1981;26(3):487–493. doi: 10.1016/0031-9384(81)90178-5. [DOI] [PubMed] [Google Scholar]
- 32.Martins PJ, Marques MS, Tufik S, D'Almeida V. Orexin activation precedes increased NPY expression, hyperphagia, and metabolic changes in response to sleep deprivation. Am J Physiol Endocrinol Metab. 2010;298(3):E726–E734. doi: 10.1152/ajpendo.00660.2009. [DOI] [PubMed] [Google Scholar]
- 33.Mendelson W, Guthrie RD, Guynn R, Harris RL, Wyatt RJ. Rapid eye movement (REM) sleep deprivation, stress and intermediary metabolism. J Neurochem. 1974;22(6):1157–1159. doi: 10.1111/j.1471-4159.1974.tb04353.x. [DOI] [PubMed] [Google Scholar]
- 34.Zhang S, Zeitzer JM, Sakurai T, Nishino S, Mignot E. Sleep/wake fragmentation disrupts metabolism in a mouse model of narcolepsy. J Physiol. 2007;581(Pt 2):649–663. doi: 10.1113/jphysiol.2007.129510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nishino S, Ripley B, Overeem S, Nevsimalova S, Lammers GJ, Vankova J, et al. Low cerebrospinal fluid hypocretin (Orexin) and altered energy homeostasis in human narcolepsy. Ann Neurol. 2001;50(3):381–388. doi: 10.1002/ana.1130. [DOI] [PubMed] [Google Scholar]
- 36.Liu X, Forbes EE, Ryan ND, Rofey D, Hannon TS, Dahl RE. Rapid eye movement sleep in relation to overweight in children and adolescents. Arch Gen Psychiatry. 2008;65(8):924–932. doi: 10.1001/archpsyc.65.8.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laposky AD, Shelton J, Bass J, Dugovic C, Perrino N, Turek FW. Altered sleep regulation in leptin-deficient mice. Am J Physiol Regul Integr Comp Physiol. 2006;290(4):R894–R903. doi: 10.1152/ajpregu.00304.2005. [DOI] [PubMed] [Google Scholar]
- 38.D'Almeida V, Hipolide DC, Raymond R, Barlow KB, Parkes JH, Pedrazzoli M, et al. Opposite effects of sleep rebound on orexin OX1 and OX2 receptor expression in rat brain. Brain Res Mol Brain Res. 2005;136(1–2):148–157. doi: 10.1016/j.molbrainres.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Kitka T, Adori C, Katai Z, Vas S, Molnar E, Papp RS, et al. Association between the activation of MCH and orexin immunorective neurons and REM sleep architecture during REM rebound after a three day long REM deprivation. Neurochem Int. 2011;59(5):686–694. doi: 10.1016/j.neuint.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 40.Nair D, Zhang SX, Ramesh V, Hakim F, Kaushal N, Wang Y, et al. Sleep fragmentation induces cognitive deficits via nicotinamide adenine dinucleotide phosphate oxidase-dependent pathways in mouse. Am J Respir Crit Care Med. 2011;184(11):1305–1312. doi: 10.1164/rccm.201107-1173OC. [DOI] [PMC free article] [PubMed] [Google Scholar]