Abstract
Background:
Urinary incontinence is relatively common in women and is usually associated with pelvic organs prolapse. Our aim was to determine the relationship between type and intensity of urinary incontinence and different grades and types of pelvic organ prolapse among women.
Materials and Methods:
One-hundred female patients with the chief complaint of incontinence, who were diagnosed with pelvic organ prolapse participated in this study. Intensity of prolapse, stress and urge incontinence were evaluated using POP-Q (Pelvic Organ Prolapse Questionnaire), SEAPI (Stress related, Emptying ability, Anatomy, Protection, Inhibition) and Freeman criteria, respectively.
Results:
Patients’ mean age was 51.95 ± 12.82 years. The most common type of incontinence was stress incontinence (53%) and the most common prolapse type was cystocele (76%). Cystocele and rectocele had a significant relationship with stress (P value = 0.012) and urge incontinence (P value = 0.035), respectively; however, no relationship was observed between different grades of cystocele, rectocele and enterocele with different types of urinary incontinence (P value > 0.05). In patients with urge and mixed incontinence, prolapse grade significantly increased with age, but no such relationship was found in patients with stress incontinence. The number of vaginal deliveries had a significant relationship only with cystocele and rectocele grade; however, the relationship between other variables such as intensity of different types of urinary incontinence and enterocele grade with the number of deliveries was not significant.
Conclusion:
Pelvic organ prolapse had a significant relationship with urinary incontinence regardless of intensity and POP should be examined in all of these patients.
Keywords: Etiology, incontinence, pelvic organ prolapse
INTRODUCTION
One of the main problems of women with increasing age is urinary incontinence (UI). Among the anatomic reasons of urinary incontinence, pelvic organ prolapse (POP) and weakness of pelvic diaphragm muscles are considered as important etiologies. When the muscles and ligaments become weak, pelvic diaphragm becomes concave and pelvic contents, which are located on its surface, would be displaced. When the pelvic diaphragm muscles weaken, the hammock effect is eliminated and the pelvic viscera rely only on the ligament attachments.[1] Weakening of these ligaments fades the last possibility for preventing from their prolapsed and bladder and vagina are especially exposed to intra-abdominal pressure. The consequence of this pressure on these viscera is prolapse of the uterus and vagina and, following the prolapse of anterior and posterior walls of the vagina, the organs that are located in parallel with them (bladder and rectum) are also displaced and their natural dynamics of passing their content is disturbed. During stress and with increasing abdominal pressure, bladder neck is placed along with the bladder floor, which is in contrast to the normal physiology in which it must move in the opposite direction and stretch upwards and toward the back of the pubis bone. In this position, resisting the sudden increase in pressure is difficult for the internal and external sphincter muscles and, in case of internal sphincter deficiency, urine leakage.[2]
However, prolapse is not often limited to bladder neck; bladder floor prolapse in lateral cystocele can have an inverse effect on symptoms of incontinence and lead to outflow obstruction.[3]
In posterior prolapse, hypermobility of bladder neck seldom occurs and the main problem is downward displacement of the bladder floor. In both cases, with downward displacement of the bladder floor, a compartment of urine develops below the urethra; this, in turn, can reduce the effective capacity of the bladder, giving rise to urinary frequency. In addition, displacement of the bladder axis and angulation between the axes of the bladder and the urethra may mask the symptoms of stress urinary incontinence.[4,5]
If we can determine the causal relationship between urinary incontinence and intensity and type of prolapse, therapeutic solutions can be designed to treat incontinence among women according to their intensity and type of POP.
The purpose of this study was to determine the relationship between type and intensity of urinary incontinence and different grades and types of pelvic organs prolapse among women.
MATERIALS AND METHODS
In this cross-sectional study, women with chief complaint of urinary incontinence who were referred to urology clinic from September 2008 to September 2009 were investigated and those with some kind of POP entered this study. The exclusion criteria included virginity, injuries of spinal cords, multiple sclerosis or neuropathies, bladder or urinary tract disorder, bladder tumor and stone.
Overall, 187 women were investigated, 100 of whom entered the study. In order to determine the grade of POP, intensity of stress urinary incontinence and urge urinary incontinence, POP-Q (pelvic organ prolapse quantification) system,[6] SEAPI score[7] and Freeman criterion[8] were used, respectively. When, both stress and urge incontinences were observed, the patient was classified in the group of mixed urinary incontinence.
Demographic information was registered and entered into SPSS 16 software. Inferential statistical methods such as T-test, Spearman, Chi-square and ANOVA tests were used to analyze the mean difference of the samples.
RESULTS
In sum, 100 patients were studied. Mean age of the patients was 51.95 ± 12.82 years. Of them, 89% had the history of vaginal delivery, 11% had caesarean section and 20% had undergone hysterectomy.
Among these 100 patients, 53% suffered from stress urinary incontinence, nine had urge urinary incontinence and 38 patients had the mixed one. Among 53 patients who had stress urinary incontinence, 23 patients had mild stress urinary incontinence (SUI), 22 had moderate SUI and 8 had severe SUI. Among 9 UUI patients, 3, 5 and 1 patients had mild, moderate and severe urinary incontinence, respectively.
Seventy-six patients had cystocele including 25, 23, 19 and 9 patients with grade 1, grade 2, grade 3 and grade 4, respectively. Among 60 patients who had rectocele, 30, 24, 5 and 1 patients were in grade 1, grade 2, grade 3 and grade 4, respectively. Among 37 patients who had apical prolapse, 25 and 12 patients had grade 1 and grade 2 prolapse, respectively.
In patients with multiple types of POP, 27 cases had cystocele and rectocele, 3 cases cystocele and enterocele and 33 cases had cystocele, rectocele and enterocele, while 13 cases had only cystocele and one case had only enterocele.
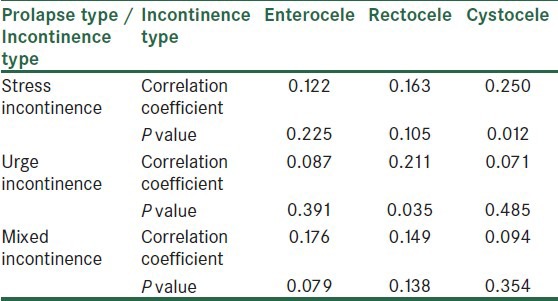
To investigate the relationship between incontinence type among women and different types of pelvic prolapse, Spearman statistical test was used. As is shown in Table 1, cystocele and rectocele had a significant relationship with stress and urge urinary incontinence, respectively.
Table 1.
The relationship between urinary incontinence and different types of pelvic prolapse among women
Chi-square statistical test was used to investigate the relationship between urinary incontinence among women and different grades of any pelvic prolapse types, which showed no relationship between different grades of cystocele, rectocele and enterocele and different types of urinary incontinence (P value > 0.05).
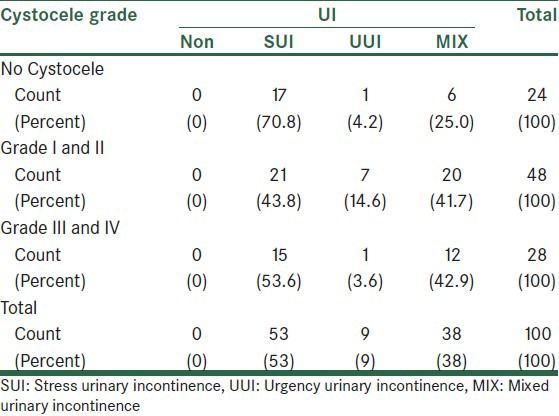
To further investigate the relationship between different grades of pelvic prolapse and type of urinary incontinence, grade 1 and 2 cystocele in one group and grade 3 and 4 cystocele in another group were compared with different types of incontinence, which indicated no significant relationship according to Table 2 (P value = 0.17).
Table 2.
Frequency of simultaneous occurrence of grade 1, 2 and 3, 4 cystocele in different types of urinary incontinence
Among all selected patients, 27 had simultaneous cystocele and rectocele, among whom 11 suffered from SUI, 3 cases from UUI and 13 cases from mixed incontinence, which did not demonstrate any significant relationship (P value = 0.60).
In order to investigate the relationship between patients’ age and intensity of incontinence, ANOVA statistical test was used, which showed that in patients with urge urinary incontinence (P value = 0.014) and mixed urinary incontinence (P value = 0.013), prolapse grade significantly increased with age. This relationship was not found for stress urinary incontinence (P value = 0.961).
To examine the relationship between number of vaginal deliveries and prolapse intensity and urinary incontinence among the patients, Spearman statistical test was used, which showed a significant relationship only between the number of vaginal delivery and cystocele (P value = 0.001) and rectocele intensity (P value = 0.005). However, no significant relationship was found between other variables like intensity of different types of incontinence and grade of enterocele and the number of deliveries (P value > 0.05).
DISCUSSION
The purpose of this study was to investigate the role of POP in urinary incontinence among women. For this purpose, all the patients taking part in this experiment were examined in terms of different types of prolapse, as well as urinary incontinence and its intensity by considering demographic data.
Prevalence of urinary incontinence among women, defined as any amount of urine leakage at least once during the last year, varies between 20 to 45%.[9] Studies have demonstrated that frequency of SUI among women is more common than that of the other incontinence types.[10] This finding confirms the results of the present study (SUI: 53% versus UUI: 9% and Mixed UI: 38%). UUI becomes more prevalent with increasing age.[11] In Ghanbari's study, which was performed on Iranian women, stress urinary incontinence was more prevalent than urge incontinence;[12] this result was also observed in the study of Bai et al.[13]
In the present study, among 53 cases with urinary incontinence, 24 patients had mild, 22 patients had moderate and only 8 patients had severe incontinence. Most of the patients suffering from pure urge urinary incontinence also had mild or moderate incontinence (3 patients mild, 5 patients moderate and 1 patient severe incontinence).
POP-Q system in this study showed that prevalence of cystocele was more than that of rectocele and epical prolapse (76%, 60% and 37%, respectively), among which the most simultaneous occurrences were between cystocele, rectocele and epical prolapse (33 cases) and cystocele and rectocele (27 cases).
Also, in the study by Bai,[13] the most reported type of prolapse was grade 1 and 2 cystocele. Among the patients suffering from rectocele and epical prolapse, 30, 24, 5 and 1 patients had grade 1, 2, 3 and 4 rectocele, respectively. Among the patients suffering from epical prolapse, 25 and 12 patients had grade 1 and 2 prolapse, respectively, and none of them had higher grades of prolapse. These results showed that among the patients suffering from incontinence, high grade POP is not prevalent, but with regard to the cause and effect relationship of this finding, no judgment can be made because the study was descriptive and cross-sectional and had no control group.
In this study, the investigation of relationship between different types of prolapse and urinary incontinence showed a significant relationship between cystocele and stress urinary incontinence (SUI) and also a significant relationship between rectocele and urge urinary incontinence (UUI). In another study by Bai et al., a significant relationship was demonstrated between stress urinary incontinence and prolapse of anterior vaginal wall (cystocele).[14] Buchsbaum also demonstrated a significant relationship between POP and urinary incontinence such that 60% of the patients suffering from POP were also suffering from incontinence; on the other hand, 40% of the patients suffering from incontinence had some grades of prolapse as well.[15] The sum of these results and the present work showed that POP must be examined in all the patients with urinary incontinence; in case the prolapse was the cause of incontinence, incontinence can be cured by the proper surgical procedure.
In this study, the relationship between simultaneous cystocele and rectocele and type of incontinence was investigated. Twenty-seven patients had cystocele and rectocele simultaneously; however, this concurrence did not have any significant relationship with type of incontinence. Based on these points, it can be concluded that rectocele may hide the symptoms of stress incontinence, which can lead to the increased prevalence of urge incontinence among the patients, who also have cystocele.
This study found no significant relationship between different grades of prolapse and intensity of incontinence. In terms of rectocele, the existence of which had a significant relationship with urge urinary incontinence, the present work showed no relationship between rectocele grade and intensity of incontinence; on the other hand, despite the relationship between stress urinary incontinence and cystocele, no relationship was found between cystocele grade and stress incontinence. Also, higher grades of POP did not increase the prevalence of incontinence. Bauchsbaum showed that higher grades of POP disrupt its relationship with incontinence, especially stress incontinence, in a way that lower grades of prolapse have a significant relationship with stress incontinence, but no significant relationship was found in higher grades.[15] In the study by Delancey, it was demonstrated that the higher the grades of cystocele, the lower the prevalence of stress incontinence and the more the prevalence of urge incontinence.[16] These findings are in contrast with our findings, in which no relationship was found between higher grades of cystocele and existence of urge incontinence; in other words, in higher grades of cystocele, the prevalence of stress urinary incontinence was not reduced. This difference can be caused by the difference in the studied groups; meaning that, in the present study, the number of patients with grade 4 cystocele was lower. Disappearance of SUI symptoms was maximized in grade 4 prolapse and lack of this relationship in the present work can be caused by the defect of the study in investigating this group with less prevalent disorder.
Evidence has shown that incontinence increases with age.[17] In this study, prevalence of urge and mixed urinary incontinence increased with age; however, no significant relationship was found between age and stress urinary incontinence. Age was also significantly related to the increasing grade of POP, which was valid for all types of prolapse and was caused by the progressive atrophy of pelvic muscles and ligaments with age.
The present study demonstrated a significant relationship between the number of vaginal delivery and the prevalence and intensity of cystocele and rectocele. This finding was in line with the available evidence that has shown a relationship between the number of deliveries and prevalence of prolapsed.[16] However, in this study, the number of deliveries did not have any relationship with the prevalence of different types of urinary incontinence and their intensity and also epical prolapse. In their study, Ghanbari et al., did not find any significant relationship between the number of vaginal deliveries and prevalence of different types of incontinence.[12] In our study, 13 patients had undergone caesarean section and the degree of incontinence among them was lower. But the number of caesarean section did not have any effect on the intensity of incontinence.
CONCLUSION
Pelvic organs prolapse has a relationship with urinary incontinence regardless of its intensity and the presence of POP needs to be examined in all the patients suffering from urinary incontinence.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.DeLancey JO. Structural aspects of the extrinsic continence mechanism. Obstet Gynecol. 1988;72:296–301. [PubMed] [Google Scholar]
- 2.Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185:1332–7. doi: 10.1067/mob.2001.119078. [DOI] [PubMed] [Google Scholar]
- 3.Gutman RE, Ford DE, Quiroz LH, Shippey SH, Handa VL. Is there a pelvic organ prolapse threshold that predicts pelvic floor symptoms? Am J Obstet Gynecol. 2008;199:683e1–7. doi: 10.1016/j.ajog.2008.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swift S, Woodman P, O’Boyle A, Kahn M, Valley M, Bland D, et al. Pelvic Organ Support Study (POSST): The distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192:795–806. doi: 10.1016/j.ajog.2004.10.602. [DOI] [PubMed] [Google Scholar]
- 5.Mouritsen L, Larsen JP. Symptoms, bother and POPQ in women referred with pelvic ogan prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:122. doi: 10.1007/s00192-002-1024-1. [DOI] [PubMed] [Google Scholar]
- 6.Brubaker L, Norton P. Current clinical nomenculature for description of pelvic organ prolapse. Journal ofPelvic Surgery. 1996;2:257–7. [Google Scholar]
- 7.Stothers L. Reliability, validity, and gender differences in the quality of life index of the SEAPI-QMM incontinence classification system. Neurourol Urodyn. 2004;23:223–8. doi: 10.1002/nau.20001. [DOI] [PubMed] [Google Scholar]
- 8.Cardozo L, Coyne KS, Versi E. Validation of the urgency perception scale. BJU Int. 2005;95:591–6. doi: 10.1111/j.1464-410X.2005.05345.x. [DOI] [PubMed] [Google Scholar]
- 9.Buckley BS, Lapitan MC. Epidemiology Committee of the Fourth International Consultation on Incontinence, Paris, 2008. Prevalence of urinary incontinence in men, women, and children–current evidence: Findings of the Fourth International Consultation on Incontinence. Urology. 2010;76:265–70. doi: 10.1016/j.urology.2009.11.078. [DOI] [PubMed] [Google Scholar]
- 10.Milson I, Altman D, Lapitan A. Epidemiology of urinary and faecal Incontinence and pelvic organ prolapse. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence. 4th ed. Plymouth, UK: Health Publication Ltd; 2009. pp. 35–112. [Google Scholar]
- 11.DuBeau CE, Kuchel GA, Johnson T. Abrams P, Cardozo L, Khoury S, Wein A. Incontinence. 4th ed. Plymouth, UK: Health Publication Ltd; 2009. Incontinence in the Frail Elderly; pp. 961–1024. [Google Scholar]
- 12.Ghanbari Z, Rostaminia Gh, Kajbafzadeh AB, Pirzadeh L, Haghollahi F, Naghizadeh MM, et al. Urodynamic evaluation of pelvic organ prolapse: Women with and without urinary incontinence. Tehran University Medical Journal. 2009;67:643. [Google Scholar]
- 13.Bai SW, Kang SH, Kim SK, Kim JY, Park KH. The effect of pelvic organ prolapse on lower urinary tract function. Yonesi Med J. 2003;44:94–8. doi: 10.3349/ymj.2003.44.1.94. [DOI] [PubMed] [Google Scholar]
- 14.Bai SW, Jeon MJ, Kim JY, Chung KA, Kim SK, Park KH. Relationship between stress urinary incontinence and pelvic organ prolapsed. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:256–60. doi: 10.1007/s001920200053. [DOI] [PubMed] [Google Scholar]
- 15.Buchsbaum GM. urinary incontinence and pelvic organ prolapsed. Minerva Urol Nefrol. 2006;58:311–9. [PubMed] [Google Scholar]
- 16.Delancy JO. Structural support of the urethra and its relation to stress urinary incontinence: The hammock hypothesis. Am J Obstet Gynecol. 1994;170:1713–20. doi: 10.1016/s0002-9378(94)70346-9. discussion 1720-3. [DOI] [PubMed] [Google Scholar]
- 17.Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300:1311–6. doi: 10.1001/jama.300.11.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]


