Abstract
Background:
Systemic administration of sclerostin neutralizing antibody has led to increased bone formation in animal models of osteoporosis. The purpose of this study was to determine if systemic administration of sclerostin neutralizing antibody could increase the healing response in a critical-sized femoral defect in rats.
Methods:
Critical-sized femoral defects were created in Lewis rats, and the rats were randomized into four groups. The sclerostin antibody (Scl-Ab) treatment groups included the continuous Scl-Ab group (twenty-one animals), the early Scl-Ab group (fifteen animals), and the delayed Scl-Ab group (fifteen animals), which received sclerostin antibody (25 mg/kg) twice weekly for weeks 0 through 12; weeks 0 through 2; and weeks 2 through 4; respectively. Twenty-one animals in the control group received vehicle from weeks 0 through 12. In a subsequent study, bone turnover markers were measured at zero, two, six, and twelve weeks after surgery in rats receiving vehicle or sclerostin neutralizing antibody for twelve weeks (fifteen rats per group). The quality of bone formed was evaluated with radiographs, microcomputed tomography, biomechanical testing, and histologic and histomorphometric analysis.
Results:
In the primary study, four of fifteen defects in the continuous (zero to twelve-week) Scl-Ab group, three of fifteen defects in the early (zero to two-week) Scl-Ab group, and four of fifteen defects in the delayed (two to four-week) Scl-Ab group healed at twelve weeks, while none of the defects healed in the control group. In both studies, treatment with sclerostin antibody for twelve weeks demonstrated a significant increase in new bone formation (p < 0.05) compared with the control group. The three treatment groups did not differ significantly with respect to the healing rates and the quality of new bone formed in the defect. The serum markers of bone formation were significantly elevated in the animals in the continuous Scl-Ab group (p < 0.05) compared with the controls.
Conclusions:
Administration of sclerostin neutralizing antibody led to increased bone formation, resulting in complete healing of femoral defects in a small subset of rats, with a majority of the animals not healing the defect by twelve weeks.
Clinical Relevance:
Sclerostin neutralizing antibody is a systemically delivered agent that exerts an anabolic effect during fracture repair and has the potential to be used as an adjuvant to enhance bone-healing in difficult bone-repair scenarios.
Approximately fifteen million fractures occur in the United States annually, and 5% to 10% of these fractures either fail to unite or demonstrate a delay in healing1. Nonunions require multiple surgical procedures to treat and lead to considerable morbidity, lost work days, and increased health care2. A need exists to develop new therapeutic strategies to enhance bone repair that would either prevent or treat fracture delayed unions or nonunions.
Widespread interest has focused on the use of growth factors to augment bone-healing3,4. Local delivery of recombinant human bone morphogenetic proteins (rhBMPs) has demonstrated efficacy similar to autologous bone grafts in promoting bone-healing in tibial fractures and spinal fusions in prospective randomized controlled trials5-7. RhBMP-2 is approved by the U.S. Food and Drug Administration for limited select indications. However, the high cost of rhBMPs, the variability of its efficacy in humans, and recent reports of serious side effects associated with its use are important factors limiting its clinical utility8-11.
The systemic delivery of a therapeutic agent that can enhance bone repair in fractures and nonunions is an attractive option because it does not involve any surgery, can be administered to the patient in the office setting, and may allow for prolonged and frequent dosing1. Sclerostin is a glycoprotein that is expressed by osteocytes and is a negative regulator of osteoblast development and bone formation12,13. Mutations in the human gene coding for sclerostin (SOST) causes Van Buchem disease and sclerosteosis, which are characterized by high bone mass and progressive bone thickening due to increased bone formation14-17. Although the specific molecular mechanism by which sclerostin inhibits bone formation is an area of continuing investigation, it has been postulated that sclerostin inhibits the BMP pathway and/or the canonical Wnt signaling pathway by modulating their receptors18-23. Preclinical studies in models of osteoporosis and a clinical trial have demonstrated that systemic administration of a neutralizing sclerostin antibody prevents bone loss and increases bone formation24-27. In another preclinical study performed using a closed femoral fracture model in rats and a fibular osteotomy model in cynomolgus monkeys, Ominsky et al. recently demonstrated that sclerostin antibody administration significantly increased the bone mass at the site of a fracture or osteotomy compared with the vehicle-treated controls28.
The purpose of the present study was to determine if systemic administration of sclerostin antibody can improve the healing response in a critical-sized segmental femoral defect in a rat model of bone repair.
Materials and Methods
Study Groups
Study 1
A total of seventy-two male Lewis rats underwent surgical procedures to create a femoral defect and were randomized into four study groups (Table I and Fig. 1). The sclerostin antibody (Scl-Ab) treatment groups included the continuous Scl-Ab group (twenty-one animals), the early Scl-Ab group (fifteen animals), and the delayed Scl-Ab group (fifteen animals), which received subcutaneous injections of sclerostin antibody (25 mg/kg) twice weekly for weeks 0 through 12, weeks 0 through 2, and weeks 2 through 4, respectively (Fig. 1). The control group (twenty-one animals) received subcutaneous injections of phosphate-buffered saline solution (PBS; vehicle) for a total of twelve weeks. At four weeks, six animals in the continuous Scl-Ab group and the control group were killed, and their femora were collected for histological analysis and microcomputed tomography (micro-CT) to detect differences in the early defect healing. The remaining sixty animals were killed at twelve weeks, and micro-CT was performed on all surgically treated femora followed by either torsional testing (eight per group) or histologic and histomorphometric analysis (seven per group). The biomechanical torsional testing was performed on completely healed specimens only.
TABLE I.
Study Design
| Groups | Total No. of Animals | Time Animals Killed | No. Imaged with Radiographs | No. Imaged with Micro-CT | No. Available for Torsional Testing | No. Available for Histologic Analysis |
| Study 1 | ||||||
| Control (vehicle control) | 21 | 6 at 4 wk and 15 at 12 wk | 21 | 6 at 4 wk and 15 at 12 wk | 8 | 6 at 4 wk and 7 at 12 wk |
| Continuous (0-12 wk) Scl-Ab treatment | 21 | 6 at 4 wk and 15 at 12 wk | 21 | 6 at 4 wk and 15 at 12 wk | 8 | 6 at 4 wk and 7 at 12 wk |
| Early (0-2 wk) Scl-Ab treatment | 21 | 12 wk | 15 | 15 | 8 | 7 |
| Delayed (2-4 wk) Scl-Ab treatment | 21 | 12 wk | 15 | 15 | 8 | 7 |
| Study 2 | ||||||
| Control (vehicle control) | 15 | 12 wk | 15 | 15 | 10 | 5 |
| Continuous (0-12 wk) Scl-Ab treatment | 15 | 12 wk | 15 | 15 | 10 | 5 |
Fig. 1.
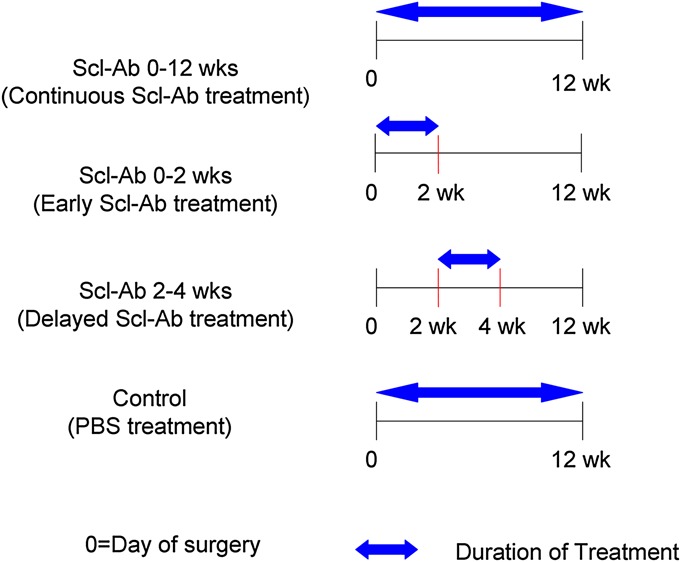
Study design and sclerostin antibody (Scl-Ab) treatment protocols.
Study 2
A second study was performed to confirm adequate drug (sclerostin antibody) exposure and analyze serum bone turnover markers. A total of thirty male Lewis rats underwent femoral defect surgeries and were randomized to receive vehicle (PBS; control) or 25 mg/kg of sclerostin antibody for twelve weeks (fifteen rats per group). Blood samples were collected to assess the biochemical markers of bone turnover. At the time that the rats were killed, micro-CT scans were performed on all surgically treated femora first and then the femora were randomized to undergo torsional testing (ten femora) or histologic and histomorphometric testing (five femora) in each group.
The sclerostin antibody used in this study (Scl-Ab III) was generated by ratizing a mouse antibody. Ratizing refers to the process of making a sequence of the antibody consistent with protein sequences found in the rats in order to make the antibody less immunogenic and less prone to clearance by the immune system29.
Serum Levels of Sclerostin Antibody and Biochemical Markers of Bone Turnover
To confirm continuous drug exposure, the sclerostin antibody levels were measured at twelve-weeks in the continuous Scl-Ab group using an ELISA (enzyme-linked immunosorbent assay) technique. Bone formation markers, intact N-terminal propeptide of type-1 procollagen (P1NP) and osteocalcin, were measured in serum samples prior to surgery and at two, six, and twelve weeks by ELISA (IDS, Fountain Hills, Arizona) and Luminex-based assays (RBN-31K-1OC; Millipore, St. Charles, Missouri), respectively. The bone resorption marker tartrate-resistant acid phosphatase 5b (TRACP 5b) was quantified using a rat ELISA kit.
Animal Model and Surgical Technique
A 6-mm critical-sized segmental femoral defect was created in fourteen-week-old, male Lewis rats (Charles River Laboratories International, Wilmington, Massachusetts) according to a previously published surgical protocol, which was approved by the Institutional Animal Care and Use Committee30-32. The animals were cared for in accordance with the Guide for the Care and Use of Laboratory Animals30,32. No carrier matrix was placed in the defect. Subcutaneous buprenorphine (0.5 mg/kg) was used for intraoperative and postoperative analgesia.
Radiographs
Radiographs were made using a digital radiography system (Faxitron X-Ray, Wheeling, Illinois), with the animals under anesthesia (1.5% to 2% isoflurane)32. Three blinded independent observers analyzed the radiographs to assess whether the femoral defect had healed and to score the amount of bone formed in each femoral defect using a previously established 6-point scale30,32,33 (Fig. 2).
Fig. 2.
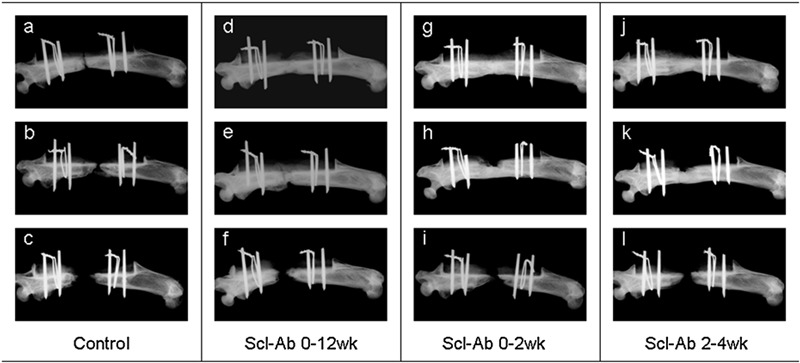
Representative radiographic images of femoral defects at twelve weeks, showing the best (top row), intermediate (middle row), and poorest (bottom row) outcome within each group in Study 1. The best images demonstrated that while none of the femoral defects were bridged by new bone in the control group, bridging of the femoral defect did occur in a subset of the Scl-Ab treatment groups (the continuous [zero to twelve-week] Scl-Ab group, early [zero to two-week] Scl-Ab group, and delayed [two to four-week] Scl-Ab group). The intermediate images also reflect the improved bone-healing with Scl-Ab treatment.
Microcomputed Tomography
Whole femora were scanned with a micro-focus x-ray computed tomography (CT) system (μCT40; Scanco Medical, Bruttisellen, Switzerland) after the animals were killed as described previously32,33. Serial three-dimensional tomographic 16-bit grayscale images were reconstructed (isometric16-μm voxels), and the new bone formed in the defect was identified on the basis of x-ray attenuation signatures and was segmented from marrow and soft tissue into discrete volumetric components. The bone volume (BV), total volume (TV), and bone volume fraction (BV/TV) were measured in the region of the femoral defect as described previously32,33.
Biomechanical Testing
Torsional testing was performed only on the healed femoral specimens using a universal testing machine (ELF-3200 series; Bose EnduraTEC, Minnetonka, Minnesota) as described previously31,32. Radiographs and micro-CT of the fifty-two animals randomized to torsional testing were reviewed, and manual palpation of the femoral specimens was performed (after removal of hardware) to assess for complete healing. Intact nonoperatively treated femora of six age and sex-matched Lewis rats (twenty-six-week-old males) were used as controls.
Histologic and Histomorphometric Analysis
Histologic and histomorphometric analysis was performed on fifty femora (Table I). The preparation of the femoral specimens and histologic sections were performed according to a previously established protocol30,32. The paraffin-embedded histologic section (5 μm thick) was stained with hematoxylin and eosin and Masson trichrome stain. Histomorphometric analysis was performed using the Bioquant analysis software (Bioquant Image Analysis, Nashville, Tennessee) according to a previously established protocol32.
Statistical Analysis
The primary outcome measure in Study 1 was to compare the healing rates in the control group and the continuous Scl-Ab group at twelve weeks. With alpha set at 0.05 and a beta error of 0.2, thirteen animals in each group would provide a power of 80% (G*Power version 3.1.2)34. However, the study was not powered for differences in healing among the different groups treated with sclerostin, and a potential for type-II error exists.
A chi-square test was used to compare radiographic healing rates, and a nonparametric Kruskal-Wallis test was used to compare the radiographic scores between the study groups. A kappa statistic was calculated as a measure of interobserver reliability among the three independent observers with respect to the radiographic grading. The results of serum markers of bone turnover, biomechanical testing, micro-CT imaging, and histomorphometric analysis were expressed as the mean and standard deviation. One-way analysis of variance (ANOVA) with a post hoc (Newman-Keuls multiple comparison) test or a Student t test was used to compare means among the four or two treatment groups, respectively. Significance was reported to be present when p < 0.05.
Source of Funding
Amgen Inc. (Thousand Oaks, California) provided the sclerostin antibody for this study. Amgen Inc. performed the assays to determine the sclerostin antibody levels and the markers for bone turnover. All assays were performed on blinded samples. Funding for this study was provided by Amgen Inc., which received funding from UCB Pharma (Slough, United Kingdom).
Results
Systemic Administration of Sclerostin Antibody Resulted in Higher Radiographic Scores and Healing in the Critical-Sized Femoral Defect After Twelve Weeks
Assessment of complete radiographic healing, defined as osseous continuity across the femoral defect, and radiographic scoring were performed for all animals. None of the femoral defects had healed in the control group of thirty animals at twelve weeks in either study (see Appendix and Fig. 2). Four defects healed in the continuous (zero to twelve-week) Scl-Ab group (four of fifteen defects in Study 1, and zero of fifteen in Study 2), three of fifteen defects healed in the early (zero to two-week) Scl-Ab group, and four of fifteen defects healed in the delayed (two to four-week) Scl-Ab group.
In Study 1, the radiographic scores were not significantly different between the control (1.05 ± 0.13) and the continuous Scl-Ab group (1.3 ± 0.63) at four weeks. However, at twelve weeks, the radiographic scores were significantly lower (p < 0.05) in the control group compared with the continuous Scl-Ab group. The radiographic scores were not significantly different among the three-sclerostin antibody treatment groups (see Appendix). In Study 2, the radiographic scores were also significantly lower (p = 0.0038) in the control group compared with the continuous (zero to twelve-week) Scl-Ab group, although the healing appeared to progress better in Study 1. The differences in bone-healing noted between the two studies were reflected in both the radiographic scoring and in the number of defects with complete radiographic healing in the continuous Scl-Ab group (four of fifteen in first study and zero of fifteen in the second study). A moderate agreement (kappa statistic, κ = 0.56) was found among the three independent observers for the radiographic scoring analysis (Study 1 and Study 2).
Systemic Administration of Sclerostin Antibody Resulted in Greater Bone Volume in the Critical-Sized Femoral Defects as Assessed with Micro-CT
In Study 1, the volumetric assessment of the new bone using micro-CT demonstrated no significant difference with respect to mean bone volume and bone volume fraction at four weeks between the control group (2.63 ± 1.6 mm3 and 5.9% ± 3%, respectively) and the continuous Scl-Ab group (3.04 ± 2.6 mm3 and 6.8% ± 5.4%, respectively). At twelve weeks, the bone volume fraction was significantly higher in the continuous Scl-Ab group (60% ± 17%; p < 0.05) compared with the control group (39.3% ± 15.3%). However, the early (zero to two-week) Scl-Ab and delayed (two to four-week) Scl-Ab groups were not significantly different from the control group with respect to the bone volume or bone volume fraction (see Appendix and Fig. 3). In Study 2, bone volume and bone volume fraction were significantly higher in the femoral defects in the continuous (zero to twelve-week) Scl-Ab group (p < 0.001) compared with the controls (see Appendix).
Fig. 3.
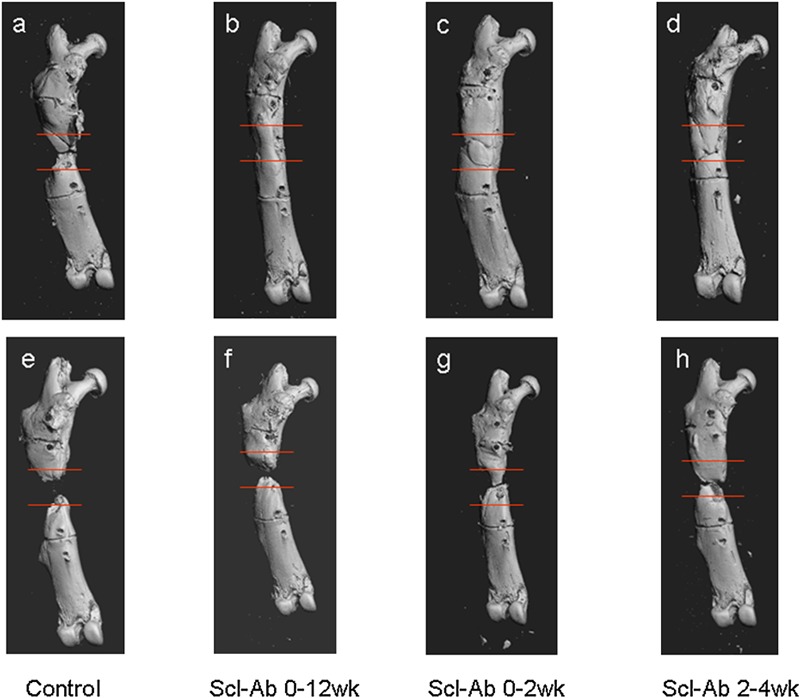
Representative micro-CT images of the healing of the femoral defects, showing the best (top panel) and poorest (bottom panel) bone-healing outcomes (bone volume) in each study group at twelve weeks. In each image, the boundaries of the femoral defect are delineated by two parallel red lines. The new bone formed in the defect was significantly higher in the continuous (zero to twelve-week) Scl-Ab group (Figs. 3-B and 3-F) compared with the controls (Figs. 3-A and 3-E).
Torsional Biomechanical Testing
A total of six of the fifty-two femoral specimens that were randomized to undergo torsional testing were completely healed (Table I) and therefore considered suitable for torsional testing (two specimens each from the three Scl-Ab treatment groups). With the available number of specimens for torsional testing in each experimental group (two per group), no meaningful interpretations and statistical comparisons could be made with respect to the biomechanical torsional testing parameters (data not shown).
Qualitative Histologic Analysis (Fig. 4)
Fig. 4.
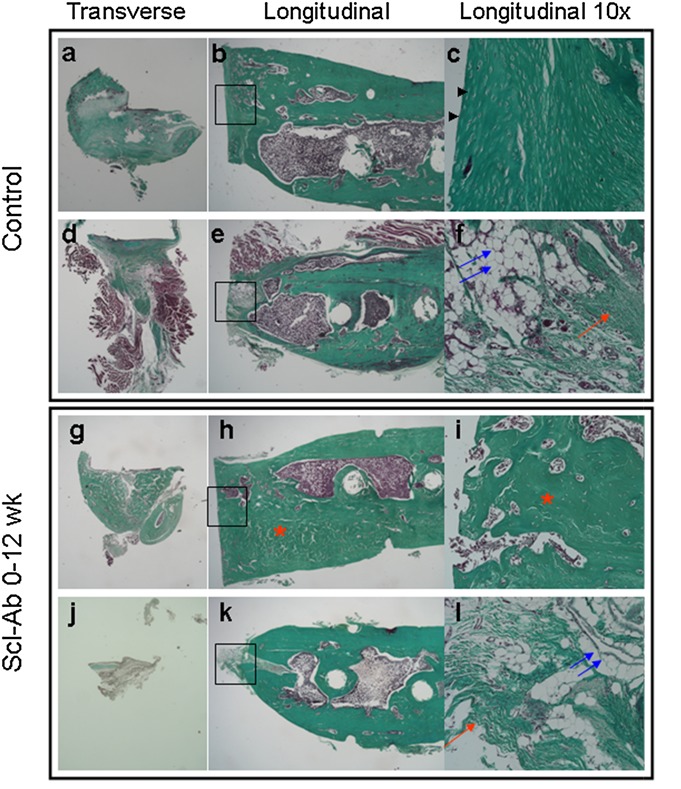
Histologic healing in a critical-sized bone defect in a rat model after twelve weeks. Masson trichrome-stained sections representing the best (top panel) and poorest (bottom panel) healing outcomes in the control group (Figs. 4-A through 4-F) and the continuous (zero to twelve-week) Scl-Ab group (Figs. 4-G through 4-L) are shown. Within each panel, the left image is a transverse section through the middle of the defect, the center image is a longitudinal section on one side of the defect, and the image on the right is a 10× magnification of the center of the defect from the longitudinal section (black rectangle). Femora that did not heal in the control group (Figs. 4-A through 4-F) had fibrous tissue (red arrow), cartilage (arrowheads), adipose tissue (blue arrows) mixed with moderate to no bone in the center of the defect. Femora that demonstrated complete healing in the Scl-Ab (zero to twelve-week) treatment group (Figs. 4-G, 4-H, and 4-I) had abundant bone formation (asterisks in Figs. 4-H and 4-I) in the center of the femoral defect and at the host-defect interface. The defects that did not heal in the Sci-Ab treatment groups (Figs. 4-J, 4-K, and 4-L) had a variable amount of bone formation at the defect interface mixed with fibrous tissue (red arrow) and adipose tissue (blue arrows.
Histologic examination of the femoral defects that healed completely in the Scl-Ab treatment groups demonstrated abundant intramedullary and periosteal new bone formation (Figs. 4-G, 4-H, and 4-I) without any reconstitution of the medullary canal.
All the femoral defects in the control group and femoral defects that did not heal completely in the Scl-Ab groups demonstrated histologic hallmarks of nonunion (Figs. 4-A through 4-F, 4-J, 4-K, and 4-L). Fibrous tissue and adipose tissue were present in the center of the defect, and there was some new bone formation at the proximal and distal ends of the femoral defect. Furthermore, a thin layer of intramedullary bone interrupted the medullary canal on either side of the femoral defect.
Histomorphometric Analysis of Femoral Defects
Histomorphometric analysis of femoral defects at four weeks demonstrated no significant difference with respect to bone area between the control group (7.34 ± 4.8 mm2) and the continuous Scl-Ab group (5.24 ± 4.0 mm2). At twelve weeks, no significant differences were found between the control group and any of the sclerostin treatment groups with respect to the bone area or bone area as a percentage of tissue area in Study 1 as well as Study 2 (see Appendix).
Treatment with Sclerostin Antibody Increases Systemic Bone Formation Markers in a Critical-Sized Femoral Defect in a Rat Model of Bone Repair
The serum levels of sclerostin antibody were measured in the serum samples from the continuous Scl-Ab group of animals to determine adequate exposure to sclerostin antibody (>20 μg/mL). The mean sclerostin antibody level was 461.3 ± 143.3 μg/mL (range, 22 to 629 μg/mL). There was no significant correlation or dose response relationship (data not shown) between the serum levels of sclerostin antibody and the amount of bone formed (micro-CT or radiographic grading) in the femoral defect.
The serum levels of markers of bone formation (osteocalcin and P1NP) and bone resorption (TRACP 5b) were not significantly different between the control and the continuous Scl-Ab group of animals before surgery (Fig. 5). The bone formation marker response to treatment with sclerostin antibody peaked at week 2 and remained significantly greater than that in the controls (p < 0.05) through week 12 for osteocalcin and through week 6 for P1NP. There were no significant differences between the two groups with respect to serum TRACP 5b levels at any time point.
Fig. 5.
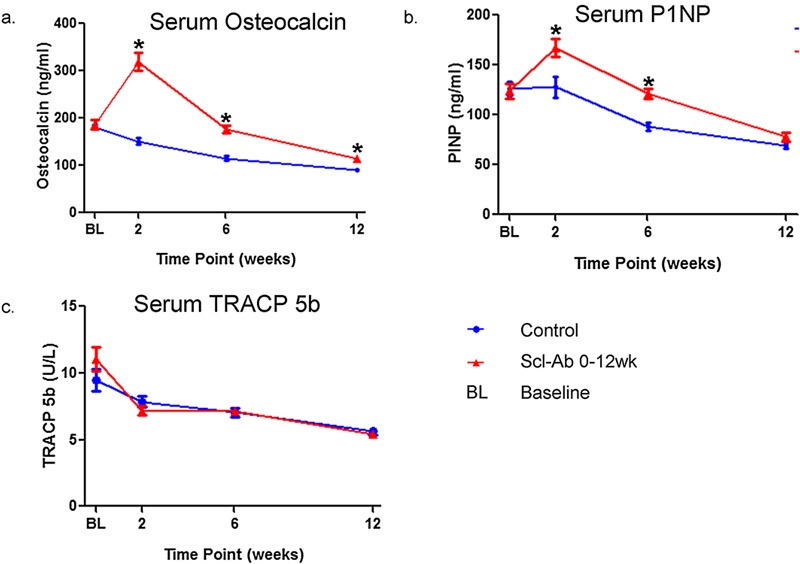
The response of serum markers of bone turnover to sclerostin antibody (Scl-Ab) treatment. The bone formation marker response to Scl-Ab treatment peaked at week 2 and remained significantly greater than that of the controls through week 12 for osteocalcin (Fig. 5-A) and through week 6 for P1NP (Fig. 5-B). There were no significant differences between the continuous (zero to twelve-week) Scl-Ab group and the control group with respect to the serum levels of tartrate-resistant acid phosphatase 5b (TRACP 5b) (Fig. 5-C), which is a biochemical marker for bone resorption. The values are given as the mean and the standard deviation. *Denotes significant difference from control (p < 0.05).
Discussion
The results of this preclinical animal study demonstrate that sclerostin antibody exerts an anabolic effect on bone repair in a 6-mm critical-sized femoral defect in a rat model. Continuous treatment with sclerostin antibody led to a significant increase in new bone formation in the femoral defect as demonstrated by the higher radiographic scores and increased bone volume compared with the control group. Treatment with sclerostin antibody induced complete healing in a subset of femora, but the defects in a majority of the animals did not heal by twelve weeks. We performed a second study to confirm that the animals received appropriate exposure to the systemic sclerostin antibody. The serum markers of bone formation were significantly higher in the animals treated with sclerostin antibody (continuous [zero to twelve-week] Scl-Ab; p < 0.05) compared with the controls.
Systemic treatment with sclerostin antibody is associated with increased bone formation, bone strength, and bone mineral density in preclinical models of osteoporosis24-26,35,36. Two previously published preclinical studies investigated the role of this therapy in bone repair28,29. Agholme et al. studied the influence of sclerostin antibody on metaphyseal bone-healing by measuring the pull-out strength of a screw inserted into the proximal part of the tibia of a Sprague-Dawley rat29. Animals treated with sclerostin antibody demonstrated increased bone volume fraction around the screw and a 50% higher pull-out strength of the screw compared with the saline solution-treated controls. Using a closed femoral fracture in a rat model and a fibular osteotomy in a primate model, Ominsky et al. demonstrated that in both models sclerostin antibody significantly increased the bone mass at the site of fracture or osteotomy28. Furthermore, a significant improvement in the biomechanical strength of the callus compared with the vehicle-treated controls was observed. However, the critical-sized bone defect model used in the present study represents a more challenging environment to test sclerostin antibody. In addition, the two prior studies did not investigate the effect of treatment duration on healing rates.
Modest differences in healing were observed between the two studies, with Study 2 resulting in lower radiographic scoring and a lack of complete healing of femoral defects. Although the source of this variation is unclear, it could be secondary to the biological variability in the rat litters. Nevertheless, the positive effect of sclerostin antibody treatment on new bone formation in the defect was consistent across both studies.
In the present study, there was no significant difference in the amount of bone repair among the three protocols of sclerostin antibody treatment, although a trend toward increased new bone formation was seen in the continuous and the delayed treatment groups compared with the early treatment group. Also, the delayed treatment group demonstrated similar healing on radiographs, micro-CT, and histologic and histomorphometric analysis compared with the continuous treatment group, which suggests that a longer duration of treatment may not be needed to promote bone repair in this model.
Systemic administration of sclerostin antibody led to occasional complete bridging of the bone defect, but was not potent enough to consistently produce complete healing. In prior experiments in our laboratory using the same animal model, rhBMP-2 on a collagen sponge consistently healed the critical-sized femoral defects30,33. The bone formation in the defect associated with the sclerostin antibody treatment occurred primarily from the ends of the defect. The ability of sclerostin antibody to increase bone formation on existing bone surfaces is consistent with the location of the osteocyte source of sclerostin at either end of the defect. The results of this study suggest that sclerostin antibody is not an osteoinductive agent like BMP. We theorize that sclerostin antibody may be associated with a more consistent and robust healing response if used to treat fractures with small bone defects. In this study, the femoral defect was left empty and was not bridged with a carrier matrix30,31,33. The healing rates may have been improved in our study if sclerostin antibody treatment was combined with a cell-based therapy, autogenous graft, allograft, or osteoconductive scaffold to provide surfaces on which osteoblasts could adhere and more bone could be formed.
Orthopaedic surgeons may encounter a spectrum of bone repair scenarios in clinical practice, and there is no single strategy that can be used to successfully manage every case, as the biologic requirements to induce bone formation are substantially different. The clinical indications for sclerostin antibody to promote bone repair have not been defined yet, but on the basis of the results from this animal study, we propose that sclerostin antibody may be useful as an adjunct to promote bone-healing in clinical situations characterized by nonunions and fractures with limited comminution and small gaps. Furthermore, sclerostin antibody is a systemically delivered therapy (via subcutaneous injection) and therefore can be administered in an outpatient setting and has the potential advantage of being administered for weeks after a surgical procedure.
There is also interest in using parathyroid hormone (PTH) to promote bone repair. However, mixed results have been reported with the use of recombinant human PTH (rhPTH) to promote fracture-healing. In a number of case reports and a randomized clinical trial, intermittent rhPTH enhanced fracture repair37-40. However, in a recent randomized clinical trial, rhPTH did not enhance the healing of distal radial fractures41. Another systemic agent with clinical potential is 5-lipoxygenase inhibitor (an oral agent), which needs to be assessed in prospective, randomized clinical studies in humans42.
In conclusion, systemic administration of sclerostin antibody leads to enhanced bone formation in a critical-sized femoral defect in a rat model. The ease of systemic administration and the presence of an anabolic effect on bone formation makes sclerostin antibody a potential adjuvant in human clinical scenarios, in which enhanced bone repair is necessary.
Appendix
Tables showing the radiographic scores and healing rates as well as data on the micro-CT and histomorphometric analyses are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Tables showing the radiographic scores and healing rates as well as data on the micro-CT and histomorphometric analyses
Acknowledgments
Note: The authors thank Marina Stolina and Denise Dwyer (Amgen Inc.) for their expertise in generating the serum biomarker data.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Axelrad TW, Kakar S, Einhorn TA. New technologies for the enhancement of skeletal repair. Injury. 2007 Mar;38(Suppl 1):S49-62 [DOI] [PubMed] [Google Scholar]
- 2.Heckman JD, Sarasohn-Kahn J. The economics of treating tibia fractures. The cost of delayed unions. Bull Hosp Jt Dis. 1997;56(1):63-72 [PubMed] [Google Scholar]
- 3.Lieberman JR, Daluiski A, Einhorn TA. The role of growth factors in the repair of bone. Biology and clinical applications. J Bone Joint Surg Am. 2002 Jun;84-A(6):1032-44 [DOI] [PubMed] [Google Scholar]
- 4.Riley EH, Lane JM, Urist MR, Lyons KM, Lieberman JR. Bone morphogenetic protein-2: biology and applications. Clin Orthop Relat Res. 1996 Mar;(324):39-46 [PubMed] [Google Scholar]
- 5.Govender S, Csimma C, Genant HK, Valentin-Opran A, Amit Y, Arbel R, Aro H, Atar D, Bishay M, Börner MG, Chiron P, Choong P, Cinats J, Courtenay B, Feibel R, Geulette B, Gravel C, Haas N, Raschke M, Hammacher E, van der Velde D, Hardy P, Holt M, Josten C, Ketterl RL, Lindeque B, Lob G, Mathevon H, McCoy G, Marsh D, Miller R, Munting E, Oevre S, Nordsletten L, Patel A, Pohl A, Rennie W, Reynders P, Rommens PM, Rondia J, Rossouw WC, Daneel PJ, Ruff S, Rüter A, Santavirta S, Schildhauer TA, Gekle C, Schnettler R, Segal D, Seiler H, Snowdowne RB, Stapert J, Taglang G, Verdonk R, Vogels L, Weckbach A, Wentzensen A, Wisniewski T; BMP-2 Evaluation in Surgery for Tibial Trauma (BESTT) Study Group Recombinant human bone morphogenetic protein-2 for treatment of open tibial fractures: a prospective, controlled, randomized study of four hundred and fifty patients. J Bone Joint Surg Am. 2002 Dec;84-A(12):2123-34 [DOI] [PubMed] [Google Scholar]
- 6.Glassman SD, Carreon LY, Djurasovic M, Campbell MJ, Puno RM, Johnson JR, Dimar JR. RhBMP-2 versus iliac crest bone graft for lumbar spine fusion: a randomized, controlled trial in patients over sixty years of age. Spine (Phila Pa 1976). 2008 Dec 15;33(26):2843-9 [DOI] [PubMed] [Google Scholar]
- 7.McKay WF, Peckham SM, Badura JM. A comprehensive clinical review of recombinant human bone morphogenetic protein-2 (INFUSE Bone Graft). Int Orthop. 2007 Dec;31(6):729-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crawford CH, 3rd, Carreon LY, McGinnis MD, Campbell MJ, Glassman SD. Perioperative complications of recombinant human bone morphogenetic protein-2 on an absorbable collagen sponge versus iliac crest bone graft for posterior cervical arthrodesis. Spine (Phila Pa 1976). 2009 Jun 1;34(13):1390-4 [DOI] [PubMed] [Google Scholar]
- 9.Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, Song F. Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review [iii-iv.]. Health Technol Assess. 2007 Aug;11(30):1-150: iii-iv [DOI] [PubMed] [Google Scholar]
- 10.Vaidya R, Carp J, Sethi A, Bartol S, Craig J, Les CM. Complications of anterior cervical discectomy and fusion using recombinant human bone morphogenetic protein-2. Eur Spine J. 2007 Aug;16(8):1257-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shields LB, Raque GH, Glassman SD, Campbell M, Vitaz T, Harpring J, Shields CB. Adverse effects associated with high-dose recombinant human bone morphogenetic protein-2 use in anterior cervical spine fusion. Spine (Phila Pa 1976). 2006 Mar 1;31(5):542-7 [DOI] [PubMed] [Google Scholar]
- 12.Poole KE, van Bezooijen RL, Loveridge N, Hamersma H, Papapoulos SE, Löwik CW, Reeve J. Sclerostin is a delayed secreted product of osteocytes that inhibits bone formation. FASEB J. 2005 Nov;19(13):1842-4 [DOI] [PubMed] [Google Scholar]
- 13.van Bezooijen RL, ten Dijke P, Papapoulos SE, Löwik CW. SOST/sclerostin, an osteocyte-derived negative regulator of bone formation. Cytokine Growth Factor Rev. 2005 Jun;16(3):319-27 [DOI] [PubMed] [Google Scholar]
- 14.Van Buchem FS, Hadders HN, Ubbens R. An uncommon familial systemic disease of the skeleton: hyperostosis corticalis generalisata familiaris. Acta radiol. 1955 Aug;44(2):109-20 [PubMed] [Google Scholar]
- 15.Balemans W, Patel N, Ebeling M, Van Hul E, Wuyts W, Lacza C, Dioszegi M, Dikkers FG, Hildering P, Willems PJ, Verheij JB, Lindpaintner K, Vickery B, Foernzler D, Van Hul W. Identification of a 52 kb deletion downstream of the SOST gene in patients with van Buchem disease. J Med Genet. 2002 Feb;39(2):91-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balemans W, Ebeling M, Patel N, Van Hul E, Olson P, Dioszegi M, Lacza C, Wuyts W, Van Den Ende J, Willems P, Paes-Alves AF, Hill S, Bueno M, Ramos FJ, Tacconi P, Dikkers FG, Stratakis C, Lindpaintner K, Vickery B, Foernzler D, Van Hul W. Increased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST). Hum Mol Genet. 2001 Mar 1;10(5):537-43 [DOI] [PubMed] [Google Scholar]
- 17.Beighton P, Barnard A, Hamersma H, van der Wouden A. The syndromic status of sclerosteosis and van Buchem disease. Clin Genet. 1984 Feb;25(2):175-81 [DOI] [PubMed] [Google Scholar]
- 18.Kamiya N, Ye L, Kobayashi T, Mochida Y, Yamauchi M, Kronenberg HM, Feng JQ, Mishina Y. BMP signaling negatively regulates bone mass through sclerostin by inhibiting the canonical Wnt pathway. Development. 2008 Nov;135(22):3801-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.ten Dijke P, Krause C, de Gorter DJ, Löwik CW, van Bezooijen RL. Osteocyte-derived sclerostin inhibits bone formation: its role in bone morphogenetic protein and Wnt signaling. J Bone Joint Surg Am. 2008 Feb;90(Suppl 1):31-5 [DOI] [PubMed] [Google Scholar]
- 20.Li X, Zhang Y, Kang H, Liu W, Liu P, Zhang J, Harris SE, Wu D. Sclerostin binds to LRP5/6 and antagonizes canonical Wnt signaling. J Biol Chem. 2005 May 20;280(20):19883-7 [DOI] [PubMed] [Google Scholar]
- 21.van Bezooijen RL, Svensson JP, Eefting D, Visser A, van der Horst G, Karperien M, Quax PH, Vrieling H, Papapoulos SE, ten Dijke P, Löwik CW. Wnt but not BMP signaling is involved in the inhibitory action of sclerostin on BMP-stimulated bone formation. J Bone Miner Res. 2007 Jan;22(1):19-28 [DOI] [PubMed] [Google Scholar]
- 22.Löwik CW, van Bezooijen RL. Wnt signaling is involved in the inhibitory action of sclerostin on BMP-stimulated bone formation. J Musculoskelet Neuronal Interact. 2006 Oct-Dec;6(4):357. [PubMed] [Google Scholar]
- 23.Krause C, Korchynskyi O, de Rooij K, Weidauer SE, de Gorter DJ, van Bezooijen RL, Hatsell S, Economides AN, Mueller TD, Löwik CW, ten Dijke P. Distinct modes of inhibition by sclerostin on bone morphogenetic protein and Wnt signaling pathways. J Biol Chem. 2010 Dec 31;285(53):41614-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tian X, Jee WS, Li X, Paszty C, Ke HZ. Sclerostin antibody increases bone mass by stimulating bone formation and inhibiting bone resorption in a hindlimb-immobilization rat model. Bone. 2011 Feb;48(2):197-201 [DOI] [PubMed] [Google Scholar]
- 25.Li X, Warmington KS, Niu QT, Asuncion FJ, Barrero M, Grisanti M, Dwyer D, Stouch B, Thway TM, Stolina M, Ominsky MS, Kostenuik PJ, Simonet WS, Paszty C, Ke HZ. Inhibition of sclerostin by monoclonal antibody increases bone formation, bone mass, and bone strength in aged male rats. J Bone Miner Res. 2010 Dec;25(12):2647-56 [DOI] [PubMed] [Google Scholar]
- 26.Li X, Ominsky MS, Warmington KS, Morony S, Gong J, Cao J, Gao Y, Shalhoub V, Tipton B, Haldankar R, Chen Q, Winters A, Boone T, Geng Z, Niu QT, Ke HZ, Kostenuik PJ, Simonet WS, Lacey DL, Paszty C. Sclerostin antibody treatment increases bone formation, bone mass, and bone strength in a rat model of postmenopausal osteoporosis. J Bone Miner Res. 2009 Apr;24(4):578-88 [DOI] [PubMed] [Google Scholar]
- 27.Padhi D, Jang G, Stouch B, Fang L, Posvar E. Single-dose, placebo-controlled, randomized study of AMG 785, a sclerostin monoclonal antibody. J Bone Miner Res. 2011 Jan;26(1):19-26 [DOI] [PubMed] [Google Scholar]
- 28.Ominsky MS, Li C, Li X, Tan HL, Lee E, Barrero M, Asuncion FJ, Dwyer D, Han CY, Vlasseros F, Samadfam R, Jolette J, Smith SY, Stolina M, Lacey DL, Simonet WS, Paszty C, Li G, Ke HZ. Inhibition of sclerostin by monoclonal antibody enhances bone healing and improves bone density and strength of nonfractured bones. J Bone Miner Res. 2011 May;26(5):1012-21 [DOI] [PubMed] [Google Scholar]
- 29.Agholme F, Li X, Isaksson H, Ke HZ, Aspenberg P. Sclerostin antibody treatment enhances metaphyseal bone healing in rats. J Bone Miner Res. 2010 Nov;25(11):2412-8 [DOI] [PubMed] [Google Scholar]
- 30.Lieberman JR, Daluiski A, Stevenson S, Wu L, McAllister P, Lee YP, Kabo JM, Finerman GA, Berk AJ, Witte ON. The effect of regional gene therapy with bone morphogenetic protein-2-producing bone-marrow cells on the repair of segmental femoral defects in rats. J Bone Joint Surg Am. 1999 Jul;81(7):905-17 [DOI] [PubMed] [Google Scholar]
- 31.Virk MS, Conduah A, Park SH, Liu N, Sugiyama O, Cuomo A, Kang C, Lieberman JR. Influence of short-term adenoviral vector and prolonged lentiviral vector mediated bone morphogenetic protein-2 expression on the quality of bone repair in a rat femoral defect model. Bone. 2008 May;42(5):921-31 [DOI] [PubMed] [Google Scholar]
- 32.Virk MS, Sugiyama O, Park SH, Gambhir SS, Adams DJ, Drissi H, Lieberman JR. “Same day” ex-vivo regional gene therapy: a novel strategy to enhance bone repair. Mol Ther. 2011 May;19(5):960-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cuomo AV, Virk M, Petrigliano F, Morgan EF, Lieberman JR. Mesenchymal stem cell concentration and bone repair: potential pitfalls from bench to bedside. J Bone Joint Surg Am. 2009 May;91(5):1073-83 [DOI] [PubMed] [Google Scholar]
- 34.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009 Nov;41(4):1149-60 [DOI] [PubMed] [Google Scholar]
- 35.Ominsky MS, Vlasseros F, Jolette J, Smith SY, Stouch B, Doellgast G, Gong J, Gao Y, Cao J, Graham K, Tipton B, Cai J, Deshpande R, Zhou L, Hale MD, Lightwood DJ, Henry AJ, Popplewell AG, Moore AR, Robinson MK, Lacey DL, Simonet WS, Paszty C. Two doses of sclerostin antibody in cynomolgus monkeys increases bone formation, bone mineral density, and bone strength. J Bone Miner Res. 2010 May;25(5):948-59 [DOI] [PubMed] [Google Scholar]
- 36.Eddleston A, Marenzana M, Moore AR, Stephens P, Muzylak M, Marshall D, Robinson MK. A short treatment with an antibody to sclerostin can inhibit bone loss in an ongoing model of colitis. J Bone Miner Res. 2009 Oct;24(10):1662-71 [DOI] [PubMed] [Google Scholar]
- 37.Gomberg SJ, Wustrack RL, Napoli N, Arnaud CD, Black DM. Teriparatide, vitamin D, and calcium healed bilateral subtrochanteric stress fractures in a postmenopausal woman with a 13-year history of continuous alendronate therapy. J Clin Endocrinol Metab. 2011 Jun;96(6):1627-32 [DOI] [PubMed] [Google Scholar]
- 38.Chintamaneni S, Finzel K, Gruber BL. Successful treatment of sternal fracture nonunion with teriparatide. Osteoporos Int. 2010 Jun;21(6):1059-63 [DOI] [PubMed] [Google Scholar]
- 39.Oteo-Alvaro A, Moreno E. Atrophic humeral shaft nonunion treated with teriparatide (rh PTH 1-34): a case report. J Shoulder Elbow Surg. 2010 Oct;19(7):e22-8 [DOI] [PubMed] [Google Scholar]
- 40.Resmini G, Iolascon G. 79-year-old post-menopausal woman with humerus fracture during teriparatide treatment. Aging Clin Exp Res. 2007 Aug;19(4)(Suppl):30-1 [PubMed] [Google Scholar]
- 41.Aspenberg P, Genant HK, Johansson T, Nino AJ, See K, Krohn K, García-Hernández PA, Recknor CP, Einhorn TA, Dalsky GP, Mitlak BH, Fierlinger A, Lakshmanan MC. Teriparatide for acceleration of fracture repair in humans: a prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J Bone Miner Res. 2010 Feb;25(2):404-14 [DOI] [PubMed] [Google Scholar]
- 42.Cottrell JA, O’Connor JP. Pharmacological inhibition of 5-lipoxygenase accelerates and enhances fracture-healing. J Bone Joint Surg Am. 2009 Nov;91(11):2653-65 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
Tables showing the radiographic scores and healing rates as well as data on the micro-CT and histomorphometric analyses


