Abstract
Background:
The clinical diagnosis of thumb ulnar collateral ligament disruption has been based on joint angulation during valgus stress testing. This report describes a definitive method of distinguishing between complete and partial ulnar collateral ligament injuries by quantifying translation of the proximal phalanx on the metacarpal head during valgus stress testing.
Methods:
Sixty-two cadaveric thumbs underwent standardized valgus stress testing under fluoroscopy with the ulnar collateral ligament intact, following an isolated release of the proper ulnar collateral ligament, and following a combined release of both the proper and the accessory ulnar collateral ligament (complete ulnar collateral ligament release). Following complete ulnar collateral ligament release, the final thirty-seven thumbs were also analyzed after the application of a valgus force sufficient to cause 45° of valgus angulation at the metacarpophalangeal joint to model more severe soft-tissue injury. Two independent reviewers measured coronal plane joint angulation (in degrees), ulnar joint line gap formation (in millimeters), and radial translation of the proximal phalanx on the metacarpal head (in millimeters) on digital fluoroscopic images that had been randomized.
Results:
Coronal angulation across the stressed metacarpophalangeal joint progressively increased through the stages of the testing protocol: ulnar collateral ligament intact (average [and standard deviation], 20° ± 8.1°), release of the proper ulnar collateral ligament (average, 23° ± 8.3°), and complete ulnar collateral ligament release (average, 30° ± 8.9°) (p < 0.01 for each comparison). Similarly, gap formation increased from the measurement in the intact state (5.1 ± 1.3 mm), to that following proper ulnar collateral ligament release (5.7 ± 1.5 mm), to that following complete ulnar collateral ligament release (7.2 ± 1.5 mm) (p < 0.01 for each comparison). Radial translation of the proximal phalanx on the metacarpal head did not increase after isolated release of the proper ulnar collateral ligament (1.6 ± 0.8 mm vs. 1.5 ± 0.9 mm in the intact state). There was a significant increase in translation following release of the complete ulnar collateral ligament complex (3.0 ± 0.9 mm; p < 0.01) and an additional increase after forcible angulation of the joint to 45° (4.1 ± 0.9 mm; p < 0.01). Translation 2 mm greater than that in the stressed control was 100% specific for complete disruption of the ulnar collateral ligament complex.
Conclusions:
While transection of the proper ulnar collateral ligament leads to an increase in metacarpophalangeal joint angulation and gapping on stress fluoroscopic evaluation, only release of both the accessory and the proper ulnar collateral ligament significantly increases translation of the proximal phalanx on the metacarpal head.
Clinical Relevance:
A finding of phalangeal translation on a stress fluoroscopic image distinguishes partial from complete tears of the thumb ulnar collateral ligament.
The ulnar collateral ligament is the primary static stabilizer against valgus stress at the metacarpophalangeal joint of the thumb. Disruption of the ligament, if untreated, can result in chronic joint instability, functional limitation in pinch, and persistent pain1. Previous clinical and cadaveric studies have suggested that, when a sufficient valgus force is applied to the thumb, the proper ulnar collateral ligament ruptures first, followed by rupture of the accessory ulnar collateral ligament2-4. While injuries of the proper ulnar collateral ligament alone are amenable to nonoperative treatment, disruption of both the proper and the accessory ulnar collateral ligament may lead to a Stener lesion, with marked displacement of the ulnar collateral ligament superficial to the adductor pollicis aponeurosis, requiring operative repair for satisfactory clinical outcomes5.
Ulnar collateral ligament disruption is a common injury, incurring substantial health-care costs as well as indirect societal costs. The annual incidence of ulnar collateral ligament injuries has been estimated to be fifty per 100,000 individuals6. In one ten-year experience, 66% of these injuries were in working adults, and the average time off from work was eighty-eight days, leading to substantial lost productivity. However, the diagnosis of a complete ulnar collateral ligament injury was definitively established clinically in only 38% of the cases; 62% required costly advanced imaging6.
Complete tears of the ulnar collateral ligament at the metacarpophalangeal joint involve both the proper ulnar collateral ligament and the accessory ulnar collateral ligament. The proper ulnar collateral ligament courses from the dorsal third of the metacarpal head to the proximal volar aspect of the proximal phalanx7. The accessory ulnar collateral ligament is positioned volar to the proper collateral ligament, spanning from the volar surface of the metacarpal head to the ulnar border of the volar plate (Fig. 1)8. A complete ulnar collateral ligament tear (i.e., disruption of both the proper ulnar collateral ligament and the accessory ulnar collateral ligament) is the minimum injury necessary to allow sufficient displacement of the ligament to produce the Stener lesion, which requires operative repair5. Previous studies have demonstrated that the volar plate and dorsal capsule of the metacarpophalangeal joint provide minimal contributions to varus and valgus stability9.
Fig. 1.
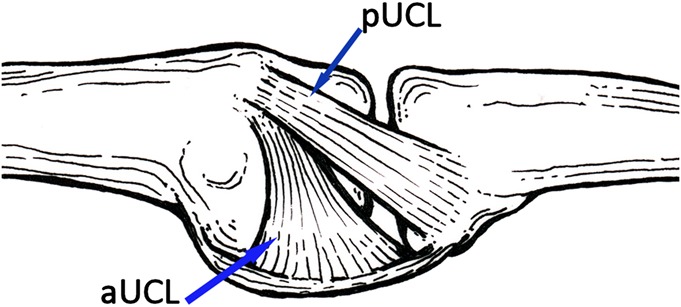
Diagram of a normal ulnar collateral ligament complex (view of the thumb metacarpophalangeal joint from the ulnar side). pUCL = proper ulnar collateral ligament and aUCL = accessory ulnar collateral ligament.
While magnetic resonance imaging (MRI) and ultrasound have been used to diagnose complete ulnar collateral ligament injuries, there are no universally accepted techniques for conclusively establishing the diagnosis of these injuries in the clinical setting. Given the recent concern over health-care expenditures, improving diagnostic accuracy without the use of advanced imaging is advantageous. The goal of this cadaveric study was to evaluate a novel, quantifiable measurement that differentiates partial from complete ulnar collateral ligament tears in the clinical setting. Our hypothesis was that the magnitude of radial translation of the proximal phalanx on the head of the thumb metacarpal could predict complete ulnar collateral ligament tears more accurately than could metacarpophalangeal joint angulation during valgus-stress fluoroscopic imaging.
Materials and Methods
Sixty-eight fresh-frozen cadaveric arms were obtained through a university-associated body-donation program. Arms were visually and fluoroscopically screened for any evidence of prior trauma or congenital malformation. Thirty-four right arms and thirty-four left unmatched arms were used. Thirty-five were obtained from male cadavers; thirty-one, from female cadavers; and two, from cadavers of unknown sex. The mean age of the donors at the time of death was seventy-nine years (range, forty-eight to ninety-nine years). Hand-dominance information was not available.
All arms were thawed to room temperature prior to experimentation. The thumbs were disarticulated through the carpometacarpal joint. The skin and subcutaneous tissues were dissected from the underlying fascia on the ulnar aspect of the metacarpophalangeal joint, exposing the adductor aponeurosis through a longitudinal dorsal incision centered at the metacarpophalangeal joint. On the basis of prior studies documenting that the adductor aponeurosis does not contribute to the ex vivo stability of the metacarpophalangeal joint2,3,10-12, the adductor aponeurosis was divided sharply and dissected away from the underlying ulnar collateral ligament. Each ulnar collateral ligament complex was visually confirmed to be intact.
Mechanical Testing
Each metacarpophalangeal joint was conditioned by maximal manual flexion and extension of the joint thirty times in a cyclical fashion. To ensure that stress testing did not produce rotation through the metacarpophalangeal joint, Kirschner wires were placed in a parallel fashion, from dorsal to volar, in the diaphysis of the thumb metacarpal and proximal phalanx. Prior to each image acquisition, the parallel position of the two wires was confirmed. If any pins were not parallel, the rotation was corrected before the image was obtained. Resting fluoroscopic images (anteroposterior, lateral, lateral in maximal flexion, and lateral in maximal extension) were made of each thumb. Stress imaging began with the ulnar collateral ligament intact. Then, the metacarpal was stabilized manually with a clamp and a 0.9-kg (2.0-lb) valgus force was applied perpendicular to the proximal phalanx, 1 cm proximal to the interphalangeal joint with use of an American Weigh SR-5 Yellow Digital Hanging Scale (Norcross, Georgia). We chose the 0.9-kg force following simulated ulnar collateral ligament stress testing by five hand-fellowship-trained surgeons. Each surgeon stressed a healthy volunteer’s thumb metacarpophalangeal joint against the scale positioned as described above. The mean force applied (by the five surgeons conducting three trials each) was 0.9 kg (range, 0.6 to 2.1 kg).
Once a force of 0.9 ± 0.05 kg had been applied and maintained for two seconds, an anteroposterior fluoroscopic stress image was obtained and stored digitally. Stress images were made with the metacarpophalangeal joint at 0° of flexion and were repeated at 30° of flexion with use of a custom radiolucent wedge. Positioned in the center of the image intensifier, the radiolucent wedge ensured that the metacarpophalangeal joint was imaged at a consistent distance from the x-ray source. After each stress image was obtained, the ligament and surrounding soft tissues were inspected, confirming that no inadvertent damage had been produced during the stress test.
The proper ulnar collateral ligament was then sectioned sharply at its distal insertion on the base of the proximal phalanx with use of a number-15 scalpel. The cut was made from volar to dorsal to avoid inadvertently injuring the accessory ulnar collateral ligament. The stress images were then repeated at 0° and 30° of metacarpophalangeal joint flexion. The accessory ulnar collateral ligament of each thumb was then sectioned sharply from its distal insertion on the volar plate.
Following release of the proper and accessory ulnar collateral ligaments, two conditions were tested to determine if our findings would remain consistent across a range of simulated soft-tissue injury. First, in all thumbs, sharp transection of the complete ulnar collateral ligament complex was followed by repeated stress imaging as described above. Second, the final thirty-seven thumbs were subjected to a single valgus force sufficient to produce coronal plane angulation of at least 45° and stress imaging (0.9-kg loading at 0° and 30° of metacarpophalangeal flexion) was again performed. This final condition was created to model a higher-force injury more closely simulating conditions often noted clinically.
Fluoroscopic Measurements
All fluoroscopic images were randomized. Two independent readers, blinded to the ulnar collateral ligament state (intact, proper ulnar collateral ligament released, proper and accessory ulnar collateral ligaments released), measured each image. Maximal joint flexion and extension were measured on the corresponding lateral images with use of a goniometer. Coronal metacarpophalangeal joint angulation, ulnar joint line gap, and radial translation of the proximal phalanx on the metacarpal head were measured on each anteroposterior image. Coronal joint angulation was measured with use of a goniometer and was defined by the angle (in degrees) between the longitudinal axes of the metacarpal and the proximal phalanx (see Appendix). The ulnar joint line gap (in millimeters) was defined as the distance between the ulnar-most aspects of the articular surfaces of the metacarpal head and the proximal phalanx (Fig. 2). Radial translation (in millimeters) of the proximal phalanx was measured by drawing a line parallel to the longitudinal axis of the metacarpal and passing it through the radial border of the metacarpal head articular surface. The shortest distance between this line and the radial border of the proximal phalanx articular surface was measured to determine radial translation (Fig. 3).
Fig. 2.

The ulnar joint line gap is determined by measuring the distance between the ulnar-most aspects of the articular surfaces (black dots).
Fig. 3.

Measurement of phalangeal radial translation.
All measurements were adjusted to scale with use of the diameter of a standardized circular marker imaged on the same Fluoroscan InSight-II machine (Hologic, Bedford, Massachusetts). This adjustment with use of a size marker can be replicated on any fluoroscopic image, radiograph, or digital radiograph. The final value for each fluoroscopic measurement represented the mean value from two readers. When the measurements of the two readers differed by more than 10° or 2 mm, the images were remeasured by each reader and a final value was determined by consensus.
Statistical Analysis
Six thumbs that were unable to flex at least 30° were excluded from further analysis, leaving sixty-two thumbs in the study and thirty-seven thumbs for the testing in the final high-energy state. Descriptive measures were produced to describe baseline fluoroscopic parameters. Following isolated release of the proper ulnar collateral ligament, a paired Student t test was used to examine the differences in each fluoroscopic measurement according to metacarpophalangeal joint flexion (0° versus 30°). As a result of the similarity between the data associated with the two metacarpophalangeal positions, all other analyses were conducted on data collected in metacarpophalangeal extension (0°) except where explicitly stated. Because sixty-two thumbs were analyzed in the initial ligament-release states (intact, release of the proper ulnar collateral ligament, and release of the proper and accessory ulnar collateral ligaments) and the final thirty-seven thumbs were subjected to the additional high-energy injury, a single mixed-model repeated-measures analysis of variance (ANOVA) was used to assess between-condition differences in the outcomes (radial translation of the proximal phalanx [in millimeters], metacarpophalangeal joint angle [in degrees], and metacarpophalangeal ulnar gap [in millimeters]). An unstructured covariance structure was used to model the repeated measurements. Normality and homogeneity of variance were satisfied. When the overall ANOVA was significant (p ≤ 0.05), Tukey-Kramer-adjusted least squares means were used to assess all pairwise comparisons between conditions to provide precise statistical insight into which conditions were significantly different.
Receiver operating characteristic curves were used to assess the ability of the increase in proximal phalanx radial translation and metacarpophalangeal joint angulation compared with the values in the stressed control state to distinguish disruption of the complete ulnar collateral ligament complex (proper and accessory ulnar collateral ligaments) from partial ulnar collateral ligament injury (of the proper ulnar collateral ligament only). Optimal clinical cutoff values were determined with the method of Youden to maximize the sum of sensitivity and specificity.
As a result of wide variation in the flexion arcs of thumb metacarpophalangeal joints, the association of the metacarpophalangeal flexion-extension arc with baseline coronal plane laxity (metacarpophalangeal joint at 0° of flexion) was analyzed with Pearson correlations. Rp values were interpreted as: no association (−0.3 < rp < 0.3), weak positive association (0.3 ≤ rp < 0.5), strong association (0.5 ≤ rp < 0.7), or very strong association (rp ≥ 0.7).
To determine if radial translation of the proximal phalanx was distinct from the measurements of metacarpophalangeal joint angulation and ulnar gapping, Pearson correlations were used to quantify the association between each fluoroscopic measure and each other fluoroscopic measure.
Source of Funding
This publication was made possible by grant UL1 RR024992 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Results
Baseline fluoroscopic parameters measured with the ulnar collateral ligament complex intact demonstrated a high degree of variability among the thumbs (see Appendix).
Following isolated release of the proper ulnar collateral ligament, valgus stress of the metacarpophalangeal joint in 30° of flexion failed to produce any significant differences from the measurements made at 0°. All fluoroscopic measures, including coronal joint angulation (23° versus 23°, p = 0.43), ulnar gap (5.7 mm versus 5.6 mm, p = 0.43), and radial translation (1.6 mm versus 1.5 mm, p = 0.26) remained similar.
Ulnar gap formation increased significantly at each step as the proper and accessory ulnar collateral ligaments were sequentially released (F [3,61] = 200, p < 0.001; Table I). Pairwise testing confirmed that release of the proper ulnar collateral ligament increased the ulnar gap significantly compared with that in the intact state (p < 0.01). Ulnar gap formation increased further with release of the complete ulnar collateral ligament complex (p < 0.01). Similarly, coronal joint angulation increased across the experimental conditions (F [3,61] = 106, p < 0.001) with significant increases between each state on pairwise testing (Table I). Radial translation of the proximal phalanx increased significantly across the ulnar collateral ligament conditions (F [3,61] = 110, p < 0.001). However, radial translation was unique among the fluoroscopic parameters in that it did not significantly increase, compared with the values in the intact state, after isolated release of the proper ulnar collateral ligament. On pairwise testing, radial translation was found to have increased significantly only after release of the complete ulnar collateral ligament complex when compared with the values in the intact-ligament state and after release of the proper ulnar collateral ligament (p < 0.01; Table I, Fig. 4, and Appendix).
TABLE I.
Radiographic Measures According to the State of the Ulnar Collateral Ligament (Metacarpophalangeal Joint at 0° of Flexion)*
| Measure | Intact Ulnar Collateral Ligament | Proper Ulnar Collateral Ligament Released | Proper and Accessory Ulnar Collateral Ligaments Released |
| Coronal joint angulation (°) | 20 ± 8.1 | 23 ± 8.3† | 30 ± 8.9‡ |
| Ulnar gap (mm) | 5.1 ± 1.3 | 5.7 ± 1.5† | 7.2 ± 1.5‡ |
| Radial translation (mm) | 1.5 ± 0.9 | 1.6 ± 0.8 | 3.0 ± 0.9‡ |
The values are given as the mean and standard deviation.
P < 0.01 compared with the intact ulnar collateral ligament.
P < 0.01 compared with the intact ulnar collateral ligament and with release of the proper ulnar collateral ligament.
Fig. 4.
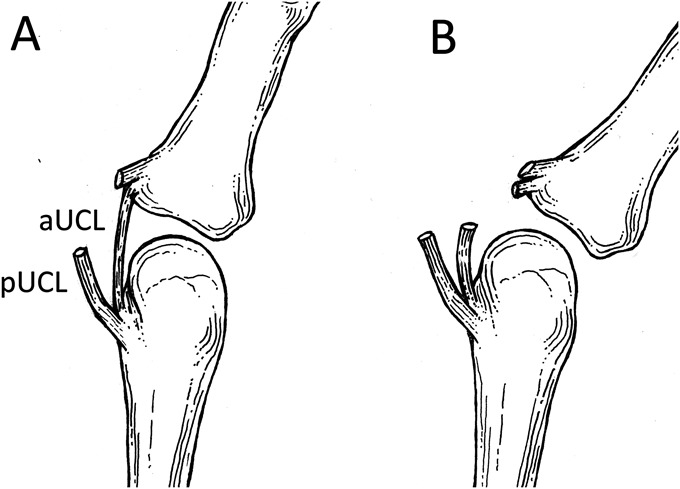
Diagrams, from the dorsal view, of joint angulation by ulnar gapping following release of the proper ulnar collateral ligament (pUCL) (Fig. 4-A) and angulation with radial translation following release of both the proper ulnar collateral ligament and the accessory ulnar collateral ligament (aUCL) (Fig. 4-B).
Receiver operating characteristic curves demonstrated that an increase in radial translation over that in the stressed baseline state was highly predictive of complete injury of the ulnar collateral ligament complex (area under curve = 0.882; Fig. 5). This slightly exceeded the performance, as a predictor, of increased joint angulation over the value in the intact state (area under curve = 0.772; Fig. 5). The increase in radial translation (over the value in the stressed control state) that had the optimal performance was 1 mm (sensitivity = 75%, specificity = 87%), while 5° of increased valgus joint angulation had optimal performance (sensitivity = 71%, specificity = 67%). Only thumbs with complete disruption of the ulnar collateral ligament complex demonstrated ≥2 mm of increased radial translation over the value in the intact state (specificity = 100%).
Fig. 5.
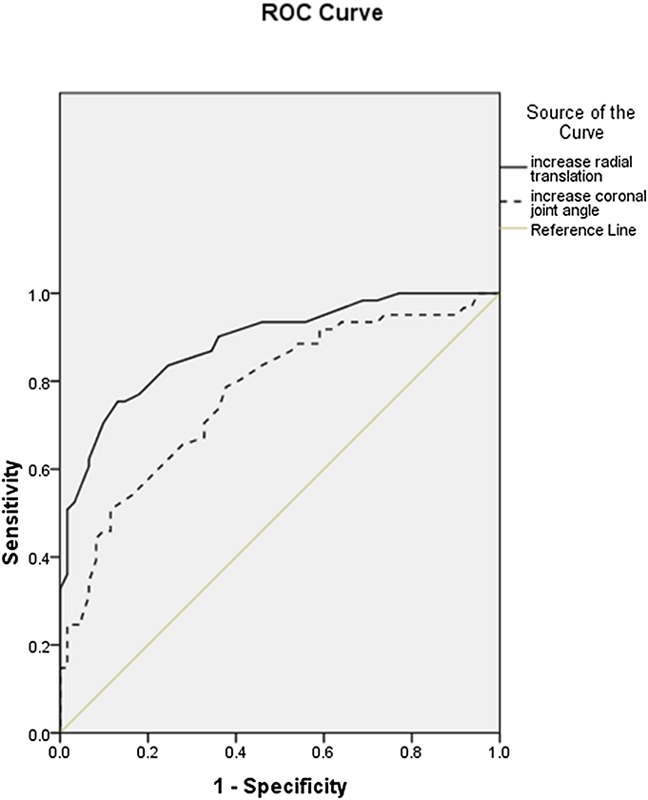
Receiver operating characteristic curves for increased phalangeal radial translation and increased metacarpophalangeal joint angulation predicting complete incompetence of the ulnar collateral ligament complex.
Sagittal plane motion at the metacarpophalangeal joint demonstrated little correlation with coronal plane laxity. The maximal metacarpophalangeal joint flexion-extension arc did not correlate with the stressed controls’ baseline measurements of coronal joint angulation (rp = 0.110), ulnar joint gapping (rp = −0.016), or radial translation (rp = −0.036). The flexion-extension arc showed no more than a weak correlation with an increase in coronal joint angulation (rp = 0.296 to 0.471), ulnar gapping (rp = 0.227 to 0.313), or radial translation (rp = 0.067 to 0.149) with sequential release of the proper ulnar collateral ligament and then the complete ulnar collateral ligament complex.
When we examined the associations between each of the fluoroscopic measures with each other fluoroscopic measure, we found increases in ulnar gapping and coronal joint angulation to be strongly correlated in each ulnar collateral ligament state (rp = 0.620 to 0.679). An increase in radial translation had no more than a weak correlation with either increased ulnar gapping or coronal joint angulation in each ulnar collateral ligament condition (rp = 0.033 to 0.238).
In the final, high-energy group, the mean force required to produce 45° of valgus angulation was 3.3 kg (range, 1.1 to 7.7 kg). In each specimen, increased angulation was associated with rupture of the dorsal-ulnar capsule off of the metacarpal head. All other surrounding soft tissues, including the volar plate, remained intact. Additional significant increases in coronal joint angulation, gapping, and translation were noted (Table II). Repeat receiver operating characteristic curves with inclusion of this high-energy group demonstrated that an increase in translation continued to outperform an increase in coronal angulation despite both measures being even more predictive of complete ulnar collateral ligament disruption (area under curve = 0.912 and 0.855, respectively) than they had been after release of the proper and accessory ulnar collateral ligaments but prior to high-force application.
TABLE II.
Radiographic Measures Following Complete Ulnar Collateral Ligament Release and Additional High-Energy Capsular Rupture*
| Measure | Proper and Accessory Ulnar Collateral Ligaments Released (N = 62) | Capsular Rupture After Proper and Accessory Ulnar Collateral Ligaments Released (N = 37) |
| Coronal joint angulation (°) | 30 ± 8.9 | 47 ± 9.9† |
| Ulnar gap (mm) | 7.2 ± 1.5 | 10.9 ± 1.8† |
| Radial translation (mm) | 3.0 ± 0.9 | 4.1 ± 0.9† |
The values are given as the mean and standard deviation.
P < 0.01.
Discussion
This study was designed to identify a quantifiable difference between thumbs with partial ulnar collateral ligament injury and those with complete ulnar injuries of the collateral ligament complex undergoing stress fluoroscopic examination. We chose this focus to identify changes that would aid the clinician in developing a treatment plan. Since a complete ulnar collateral ligament disruption is necessary for the development of a Stener lesion, which requires operative management, this distinction between partial and complete ulnar collateral ligament injuries represents the central branch point in the treatment algorithm for a traumatized ulnar collateral ligament. Therefore, it was our goal to identify a measure that does not change between baseline and isolated rupture of the proper ulnar collateral ligament but does change significantly following complete ulnar collateral ligament rupture.
We have demonstrated that radial translation of the proximal phalanx at the metacarpophalangeal joint serves as an indicator of complete ulnar collateral ligament injury at the metacarpophalangeal joint of the thumb. This measure is distinguished from traditional measures of gross joint angulation in that it does not increase with partial ulnar collateral ligament rupture (i.e., an isolated tear of the proper ulnar collateral ligament). Therefore, our data support the concept that valgus stress testing of the thumb ulnar collateral ligament produces coronal angulation across the metacarpophalangeal joint in two distinct manners. The metacarpophalangeal joint may gap open ulnarly (angulation) or the proximal phalanx may translate radially (translation). While angulation occurs following release of the proper ulnar collateral ligament, release of the entire ulnar collateral ligament complex is required to allow translation of the proximal phalanx on the metacarpal head.
Radial translation of the proximal phalanx is readily quantified in the office setting with use of manually applied valgus stress under fluoroscopy or radiography. Absolute distances can be measured on any image by placing a radiopaque ruler or radiopaque marker of known size in the field. Since we did not find a difference between measurements made with the metacarpophalangeal joint in 0° of flexion and those made in 30° of flexion, the thumb can be positioned with the metacarpophalangeal joint flat at 0° of flexion on the image intensifier to simplify positioning in a clinical setting. The fluoroscopic measurements can be performed regardless of clinician expertise. The valgus force applied in our study (0.9 kg [2 lb]) can be replicated in several ways. One method, similar to ours, is to use a hanging scale with a soft hook or loop to manually apply this valgus force across the distal aspect of the proximal phalanx of a patient’s thumbs. A second possibility is to stretch a new number-32 rubber band from 3.5 in (8.9 cm) at rest to 10 in (25.4 cm) in length; however, this method may be impacted by product variation or changes in the elastic properties of the rubber band with repeated use. Given the current health-care focus on increasing the efficiency of care, this measurement is of particular interest as it does not require advanced imaging modalities. While both MRI and ultrasound have demonstrated appropriate performance characteristics, MRI examinations are costly, dependent on magnet quality, and time-consuming. Ultrasound examinations are less expensive but are heavily operator-dependent and therefore are not universally available.
When analyzing the performance of each fluoroscopic measurement for predicting a complete ulnar collateral ligament tear, we used the increases in the measurements compared with the respective baseline measurements as opposed to absolute values. This choice was made because of the wide variation in thumb metacarpophalangeal joint properties among both the specimens in this study and in the population at large. The wide range in maximal thumb metacarpophalangeal flexion among individuals and the variation in coronal plane laxity at baseline limit the degree to which any absolute measurement can be applied to individual patients. Despite this marked individual variation, baseline measurements are presumed to be similar between the right and left thumbs of any given individual, with 88% of the volunteer subjects in one study having less than a 15° difference in joint angulation between their right and left thumbs when they underwent valgus stress testing in metacarpophalangeal joint extension13. With the metacarpophalangeal joint in 30° of flexion, 97% of subjects had less than a 15° difference between right and left thumb angulation under valgus stress. As the majority of thumb ulnar collateral ligament injuries are unilateral, the baseline stress examination in our study was used as a proxy for examination of the uninjured, contralateral thumb in the clinical setting. Thus, an increase in radial translation compared with the value on the contralateral side provides a measure that accounts for variation in baseline laxity among individuals. With use of a clinical cutoff such as an increase in 2 mm of radial translation over baseline with valgus stress, this measurement should be widely applicable.
There was less valgus joint laxity following staged release of the ulnar collateral ligament in our study than there was in the study by Heyman et al.2. Differences between their study and ours are likely attributable to the methods that were employed. Heyman et al. applied 4.5 kg (9.9 lb) of force across the metacarpophalangeal joint, which was markedly greater than the force used in the current investigation. Force levels of that magnitude would have been sufficient to injure the remaining dorsal capsular restraint, a finding that we noted in our final high-force angulation condition. Our data concur with those of Heyman et al., who documented a gradual increase in valgus joint angulation during a testing protocol consisting of stressing of the metacarpophalangeal joint with an intact ulnar collateral ligament (28°), release of the proper ulnar collateral ligament (43°), and release of the entire ulnar collateral ligament complex (63°). Our finding of dorsal capsular rupture with high-energy valgus stress contradicts previous observations that the dorsal capsule does not contribute to valgus stability9.
Several limitations are inherent to this ex vivo investigation. The specimens tested may not account for rare variations in anatomy, and they model only acute ligamentous injury. While the absolute strength and elasticity of ligaments injured in young adults may differ from those of cadaveric specimens, the relative effects of ligament release should remain similar. Additionally, traumatic ulnar collateral ligament disruption in vivo imparts a range of forces and soft-tissue damage to the thumb, which may differ from the injury created by sharp ligamentous release. Notably, we attempted to confirm the consistency in our findings across states designed to model various levels of injury, including associated disruption of the dorsal metacarpophalangeal joint capsule. Infrequently, the ulnar collateral ligament is disrupted in its midportion or proximal aspect as opposed to its distal aspect, which was modeled in this study. However, the location of the ligament disruption is unlikely to change the biomechanics of the resulting joint laxity. In this study, we focused on the appearance of the anteroposterior image with valgus stress examination, so we cannot comment on the changes that may occur in the sagittal plane. Finally, it is possible that our results would vary with alternative amounts of force applied during valgus stress testing of the metacarpophalangeal joint. However, we chose a magnitude of force similar to that applied in the clinical setting, by using a level of stress consistent with that employed by experienced hand surgeons.
Measuring the amount of radial translation of the proximal phalanx on the metacarpal head during a valgus stress fluoroscopic examination of the metacarpophalangeal joint may assist in distinguishing complete ulnar collateral ligament rupture from partial ulnar collateral ligament injury. When bilateral stress fluoroscopic examinations are compared, an increase in radial translation of at least 2 mm in comparison with that of the contralateral thumb is highly specific for a complete ulnar collateral ligament tear.
Appendix
A table showing radiographic parameters in stressed thumbs with an intact ulnar collateral ligament complex and figures demonstrating measurement of metacarpophalangeal joint angulation as well as images of joint angulation by ulnar gapping following release of the proper ulnar collateral ligament and angulation with radial translation following release of the proper and accessory ulnar collateral ligaments are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
A table showing radiographic parameters in stressed thumbs with an intact ulnar collateral ligament complex and figures demonstrating measurement of metacarpophalangeal joint angulation as well as images of joint angulation by ulnar gapping following release of the proper ulnar collateral ligament and angulation with radial translation following release of the proper and accessory ulnar collateral ligaments
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Tang P. Collateral ligament injuries of the thumb metacarpophalangeal joint. J Am Acad Orthop Surg. 2011 May;19(5):287-96 [DOI] [PubMed] [Google Scholar]
- 2.Heyman P, Gelberman RH, Duncan K, Hipp JA. Injuries of the ulnar collateral ligament of the thumb metacarpophalangeal joint. Biomechanical and prospective clinical studies on the usefulness of valgus stress testing. Clin Orthop Relat Res. 1993 Jul;(292):165-71 [PubMed] [Google Scholar]
- 3.Arranz López J, Alzaga F, Molina J. Acute ulnar collateral ligament injuries of the thumb metacarpophalangeal joint: an anatomical and clinical study. Acta Orthop Belg. 1998 Dec;64(4):378-84 [PubMed] [Google Scholar]
- 4.Melone CP, Jr, Beldner S, Basuk RS. Thumb collateral ligament injuries. An anatomic basis for treatment. Hand Clin. 2000 Aug;16(3):345-57 [PubMed] [Google Scholar]
- 5.Stener B. Displacement of the ruptured ulnar collateral ligament of the metacarpo-phalangeal joint of the thumb. J Bone Joint Surg Br. 1962;44:869-79 [Google Scholar]
- 6.Chuter GS, Muwanga CL, Irwin LR. Ulnar collateral ligament injuries of the thumb: 10 years of surgical experience. Injury. 2009 Jun;40(6):652-6 [DOI] [PubMed] [Google Scholar]
- 7.Bean CH, Tencer AF, Trumble TE. The effect of thumb metacarpophalangeal ulnar collateral ligament attachment site on joint range of motion: an in vitro study. J Hand Surg Am. 1999 Mar;24(2):283-7 [DOI] [PubMed] [Google Scholar]
- 8.Doyle J, Botte MJ. Surgical anatomy of the hand and upper extremity. Philadelphia: Lippincott, Williams & Wilkins, 2002 [Google Scholar]
- 9.Minami A, An KN, Cooney WP, 3rd, Linscheid RL, Chao EY. Ligament stability of the metacarpophalangeal joint: a biomechanical study. J Hand Surg Am. 1985 Mar;10(2):255-60 [DOI] [PubMed] [Google Scholar]
- 10.Draganich LF, Greenspahn S, Mass DP. Effects of the adductor pollicis and abductor pollicis brevis on thumb metacarpophalangeal joint laxity before and after ulnar collateral ligament reconstruction. J Hand Surg Am. 2004 May;29(3):481-8 [DOI] [PubMed] [Google Scholar]
- 11.Palmer AK, Louis DS. Assessing ulnar instability of the metacarpophalangeal joint of the thumb. J Hand Surg Am. 1978 Nov;3(6):542-6 [DOI] [PubMed] [Google Scholar]
- 12.Hsieh YF, Draganich LF, Mass DP. The effects of transection and reconstruction of the ulnar collateral ligament complex on the position of the proximal phalanx of the thumb during simulated tip pinch. J Hand Surg Am. 2000 Mar;25(2):313-21 [DOI] [PubMed] [Google Scholar]
- 13.Malik AK, Morris T, Chou D, Sorene E, Taylor E. Clinical testing of ulnar collateral ligament injuries of the thumb. J Hand Surg Eur Vol. 2009 Jun;34(3):363-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
A table showing radiographic parameters in stressed thumbs with an intact ulnar collateral ligament complex and figures demonstrating measurement of metacarpophalangeal joint angulation as well as images of joint angulation by ulnar gapping following release of the proper ulnar collateral ligament and angulation with radial translation following release of the proper and accessory ulnar collateral ligaments


