We found that dual-energy CT significantly increased reader accuracy and diagnostic confidence compared with those with conventional CT in determination of the source of contrast material extravasation in an animal model of penetrating abdominopelvic trauma.
Abstract
Purpose:
To compare the diagnostic performance of dual-energy (DE) computed tomography (CT) with two simultaneously administered contrast agents (hereafter, dual contrast) with that of conventional CT in the evaluation of the presence and source of extravasation in penetrating abdominopelvic trauma.
Materials and Methods:
Institutional animal care and use committee approval was obtained, and the study was performed in accordance with National Institutes of Health guidelines for the care and use of laboratory animals. Five rabbits with bowel trauma, vascular penetrating trauma, or both were imaged with simultaneous iodinated intravenous and bismuth subsalicylate enteric contrast material at DE CT. Four attending radiologists and six radiology residents without prior DE CT experience each evaluated 10 extraluminal collections to identify the vascular and/or enteric origin of extravasation and assess their level of diagnostic confidence, first with virtual monochromatic images simulating conventional CT and then with DE CT material decomposition attenuation maps.
Results:
Overall accuracy of identification of source of extravasation increased from 78% with conventional CT to 92% with DE CT (157 of 200 diagnoses vs 184 of 200 diagnoses, respectively; P < .001). Nine radiologists were more accurate with DE CT; one had no change. Mean confidence increased from 67% to 81% with DE CT (P < .001).
Conclusion:
In a rabbit abdominopelvic trauma model, dual-contrast DE CT significantly increased accuracy and confidence in the diagnosis of vascular versus enteric extravasated contrast material.
© RSNA, 2013
Introduction
X-ray computed tomography (CT) has become the cornerstone in the evaluation of the hemodynamically stable patient with penetrating trauma to the abdomen or pelvis (1–3). Both enteric and intravenous contrast media often are used to aid in diagnosis of bowel injury; extravasation of enteric luminal contrast material has been reported in approximately 20% of bowel injuries (4). A challenge in interpreting these CT scans is that all contrast materials appear as increased attenuation on images: extraluminal high-attenuation contrast material may represent extravasated enteric luminal contrast material because of bowel perforation, vascular contrast material because of bleeding, or a combination of the two. In some cases, contextual clues enable one to distinguish between these possibilities, but others remain ambiguous.
Clinical dual-energy (DE) CT scanners capable of simultaneously acquiring images at two different energies recently have become available (5). DE CT provides a means to distinguish different materials that would have equivalent attenuation at conventional CT (6). The ability of DE CT to help distinguish materials is based on differences in their attenuation ratios—the ratios of linear attenuation coefficients at low- and high-energy x-ray spectra. Because iodine and barium have similar attenuation ratios, they are indistinguishable with clinical DE CT scanners (7). To distinguish an enteric contrast medium from iodinated vascular contrast medium optimally, the enteric contrast medium must contain heavy atoms that both attenuate x-rays well and have attenuation ratios substantially different from the attenuation ratio of iodine. Such atoms include bismuth, tungsten, tantalum, and gold (8,9).
In this study, we investigated the application of DE CT with two simultaneously administered contrast media (hereafter, dual contrast) to penetrating abdominopelvic trauma—in particular, the effect of dual-contrast DE CT on the accuracy and confidence with which diagnosis of vascular versus enteric luminal contrast medium extravasation was made. Because there are no enteric contrast media with attenuation ratios different from that of iodine that are approved for clinical use at the doses required for imaging, we used a rabbit trauma model in this study. Bismuth subsalicylate was selected as the enteric contrast medium because it is readily available and has been shown to be an effective enteric contrast medium in phantoms (10) and in vivo (9). We investigated the diagnostic performance of dual-contrast DE CT compared with that of conventional CT in the evaluation of the presence and source of extravasation in penetrating abdominopelvic trauma.
Materials and Methods
Trauma Model
Approval from the institutional animal care and use committee was obtained, and the study was performed in accordance with the guidelines of the National Institutes of Health for the care and use of laboratory animals. Five female New Zealand white rabbits (Western Oregon Rabbit, Philomath, Ore) weighing between 4.3 and 4.8 kg were anesthetized separately with 35 mg of ketamine (Ketaset; Fort Dodge Animal Health, Fort Dodge, Iowa) per kilogram of body weight and 3 mg/kg xylazine hydrochloride (Spectrum, New Brunswick, NJ); anesthesia was maintained with inhaled isoflurane (Summit Anesthesia Equipment, Foster City, Calif).
A 12-F pediatric feeding tube was passed into the rabbit’s stomach, its position was confirmed at CT, and approximately 180 mL of 17.5 mg/mL suspension bismuth subsalicylate (Pepto-Bismol; Procter & Gamble, Cincinnati, Ohio) was instilled as a bolus. With CT guidance, sharp penetrating traumas were inflicted percutaneously by using large-bore needles, a scalpel blade, or both. Each of the five animals received a different set of one to three injuries, with each injury potentially resulting in multiple fluid collections in the (a) superior abdominal aorta only, (b) stomach and left upper quadrant small bowel, (c) both common iliac arteries and left upper quadrant small bowel, (d) inferior abdominal aorta and sigmoid colon, and (e) stomach and abdominal aorta, for a total of 10 injuries in the five rabbits. Then 700 mg of iohexol (Omnipaque 350; GE Healthcare, Princeton, NJ) per kilogram of body weight was injected via an intravenous catheter in the auricular vein immediately before DE CT.
Imaging
CT scans were obtained with a Discovery CT750 HD unit (GE Healthcare, Milwaukee, Wis) in DE gemstone spectral imaging (or GSI) mode by using protocol GSI-11 (medium filter, 0.8-second rotation time, 40-mm collimation). Scan data were postprocessed by using software (GSI Viewer; GE Healthcare) to generate 70-keV virtual monochromatic images that simulate 120-kVp conventional CT images. Iodine and simulated bismuth material density map images also were created by using this software. The current version of this software is limited to working with basis material definitions that do not have a k-edge between 40 and 140 keV. Thus, we used empirically determined x-ray attenuation coefficients in the software to simulate a material with the same attenuation ratio as that of bismuth but without a k-edge as the basis for material decomposition of iodine and bismuth.
Image Evaluation
Ten extraluminal collections were selected across the five rabbit studies and marked with an oval on the CT images. By using knowledge of the CT-guided injury and the DE CT images, the radiologists (J.M., B.M.Y.; 3 and 15 years of experience interpreting abdominal CT images, respectively) involved with injuring the rabbit viscera determined in consensus whether each collection contained extravasated enteric contrast material, vascular contrast material, or both. Ten other readers not involved with the rabbit injury or imaging were recruited. Four readers were subspecialty trained abdominal imaging attending physicians, four were 3rd-year radiology residents, and two were 1st-year radiology residents. All readers were from an academic medical center with a level 1 trauma center, and none of them had prior experience with DE CT. Before reading the studies, each reader received an approximately 5-minute introduction to DE CT and CT material density maps.
Each reader then viewed transverse and coronal image series for each rabbit by using a Digital Imaging and Communications in Medicine viewer (OsiriX, version 4.0; Pixmeo, Geneva, Switzerland) (11). For each site, the readers recorded whether, in their opinion, the site within the oval contained extravasated vascular contrast material (yes or no) and whether it contained extravasated enteric contrast material (yes or no), as well as their confidence in their overall diagnoses on a visual analog scale (0%–100%). To make their diagnoses, readers were permitted to use all the features of a typical picture archiving and communication system, including the ability to scroll to other images and adjust window level, zoom, and attenuation. Readers first evaluated all 10 sites by using only conventional CT (70-keV virtual monochromatic images, which simulate 120-kVp conventional CT images) and then reevaluated the sites by using iodine and bismuth material density maps unique to DE CT in conjunction with the conventional CT images. At the second evaluation, radiologists recorded responses to the same questions as at the first evaluation.
Analysis
Recorded diagnoses were scored as correct or incorrect against the consensus standard. A χ2 test was used for comparison of proportions, and the Shapiro-Wilk test for normality of distribution followed by a t test was used to compare continuous measures, all of which were performed by using a statistical software package (R, version 2.14; R Development Core Team, Vienna, Austria). Data on the accuracy of diagnosis were analyzed with results for all readers pooled and were stratified according to reader experience level. Pooled analysis and stratification according to correct and incorrect responses were performed for confidence data. Because the readers were evaluating specific designated traumatic fluid collections rather than reading complete studies to identify abnormalities, it was not necessary to correct for within-animal correlation in the occurrence of fluid collections. A P value of .05 was used as the threshold for statistical significance.
Results
Example CT images are shown in Figures 1 and 2. The aggregate accuracy of diagnosis across all readers was 78% (157 of 200 images) with use of only conventional CT; this increased to 92% (184 of 200 images) when diagnoses were made with the benefit of DE CT (P < .001). Improved accuracy came in the form of increased sensitivity with unchanged specificity: sensitivity for extravasated contrast material type increased from 72% (86 of 120 images) with conventional CT to 94% (113 of 120 images) with DE CT, whereas specificity was 89% (71 of 80 images) for both forms of CT. Nine of ten readers improved their accuracy with the addition of DE CT images (P = .03); one resident’s performance was unchanged. When stratified according to training level (resident vs attending physician), both groups showed significant increases in accuracy of similar magnitude (Table). The accuracy of residents interpreting DE CT images was slightly higher than that of attending physicians interpreting conventional CT images without DE CT images, but the difference was not significant (P = .08).
Figure 1:

Coronal CT images. A, A lateral left upper quadrant collection (oval) had minimally heterogeneous attenuation at conventional CT and was misinterpreted as representing only vascular or only enteric luminal extravasation by six of the 10 readers using conventional imaging. B, Iodine density map shows that the majority of the collection is vascular contrast material (arrow). C, Bismuth density map shows several foci of enteric contrast material within the collection (arrow). All 10 readers correctly identified the collection as containing both types of extravasation when using all of these images.
Figure 2:

Axial CT images show a collection medial to the stomach (ovals). High attenuation seen at the periphery of the collection at, A, conventional CT was thought to represent luminal or both luminal and vascular contrast material by four of the 10 readers when using only conventional CT. DE CT images showed high attenuation on, B, the iodine map but not on, C, the bismuth map. All 10 readers correctly identified the collection as representing only vascular extravasation when using all of these images.
Diagnostic Accuracy Stratified according to Experience Level
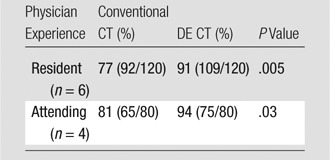
Note.—Data in parentheses are the raw data.
Mean confidence in diagnosis increased from 67% (95% confidence interval: 62%, 71%) with only conventional CT to 81% (95% confidence interval: 78%, 91%) with DE CT (P < .001). When the diagnosis made with DE CT was completely correct, the average increase in confidence was 16 percentage points (95% confidence interval: 12, 21), whereas the average increase for incorrect DE CT diagnosis was 4 percentage points (95% confidence interval: −11, 19). Use of a t test in these comparisons was supported by Shapiro-Wilk test failure to reject the null hypothesis of nonnormality for the distribution of changes in diagnostic confidence (W = 0.98, P = .17).
Discussion
We found that DE CT significantly increased reader accuracy and diagnostic confidence compared with those attained with conventional CT in the determination of the source of contrast material extravasation in an animal model of penetrating abdominopelvic trauma. These improvements were seen for radiologists with no prior DE CT experience; it seems reasonable to expect that greater improvements would be seen with additional experience and training. Although the overall performance of attending-level radiologists was superior to that of residents, the improvement in accuracy was not limited to less-experienced readers: both attending physicians and residents had similar improvements in accuracy. The current work builds on the findings of our recent in vivo study, which showed that appropriately selected pairs of vascular or vascular and enteric contrast material can be distinguished and digitally separated by means of DE CT (9). The dual-contrast DE CT technique has many potential benefits, including reduced radiation dose in multiphase studies and improved evaluation of bowel wall enhancement in positive enteric contrast material–enhanced imaging. Our current work evaluates a specific scenario—that of distinguishing the origin of abdominopelvic contrast material extravasation.
Although difficulties in identifying the source of extravasation are not widely discussed in the literature, they may be underrecognized. Our data suggest that some traumatic fluid collections can be difficult to evaluate correctly with traditional CT. The correct determination of the source of extravasation is critical to the correct triage of patients and mobilization of treatment teams for vascular surgery, interventional radiology, or general surgery. The representative collections, shown here, were misdiagnosed repeatedly with conventional CT images but were diagnosed correctly by all 10 readers with DE CT images.
Furthermore, readers had more confidence in diagnoses based on DE CT than in those based solely on conventional CT. Confidence is important because studies frequently are ordered to rule out injury; an uncertain diagnosis may not be considered to have excluded injury and may lead to unnecessary delay, treatments, or exploratory laparotomy. Readers’ subjectively reported confidence mirrored their objectively measured performance; increased confidence when using DE CT was paralleled by increased accuracy. In addition, when readers reached a correct diagnosis with DE CT images, they had significantly higher confidence than they did with conventional CT. When the diagnosis was incorrect, the data suggest that difference in confidence relative to conventional CT was small. In other words, in our trauma model, use of DE CT increased diagnostic confidence primarily when the diagnosis made on the basis of DE CT findings was correct.
The work presented here had several limitations. The artificially inflicted traumas in our study may not be representative of naturally occurring penetrating injuries, which may be more simple or more complex. Several factors may have limited the readers’ performance in using conventional CT images, including a lack of familiarity with rabbit anatomy and a lack of precontrast or delayed-phase images, which might have helped distinguish vascular from enteric contrast material. In addition, the readers in our study were from one academic medical center and may not have been representative of all radiologists who read trauma images. Nevertheless, our study covered a wide range of abdominal penetrating injuries and reader skill in interpretation of trauma CT images.
Another limitation that may have affected the immediate application of our findings was the fact that there are currently no Food and Drug Administration–approved enteric contrast materials that are distinguishable from iodinated vascular contrast materials at DE CT. Bismuth subsalicylate was chosen owing to its availability, attenuation characteristics, and relatively low toxicity; however, at the doses required for optimal imaging, it is likely to cause salicylate toxicity (12). This toxicity precluded inclusion of human subjects in this initial investigation of dual-contrast DE CT trauma imaging. The potential for improved diagnosis in clinical trauma imaging with dual-contrast DE CT techniques, demonstrated here in a rabbit model, provides motivation for the development of clinically approved enteric contrast materials with attenuation ratios complementary to that of iodine. Our group and others are working to develop such agents.
Practical applications: We found that in a rabbit model of abdominopelvic trauma, dual-contrast DE CT significantly increased accuracy and confidence in the diagnosis of vascular versus enteric extravasated contrast material. Further development of complementary contrast materials for human use can bring these benefits to clinical imaging.
Advances in Knowledge.
• Dual-contrast dual-energy (DE) computed tomography (CT) significantly increases sensitivity without loss of specificity when compared with conventional CT in the diagnosis of vascular versus enteric contrast material extravasation in an animal model of penetrating abdominopelvic trauma (sensitivity, 94% [113 of 120 readings] vs 72% [86 of 120 readings], P < .001; specificity, 89% [71 of 80 readings] for both modalities).
• Dual-contrast DE CT improves diagnostic accuracy for experienced radiologists (conventional CT, 81% [65 of 80 readings]; DE CT, 94% [75 of 80 readings]; P = .03) and less-experienced radiologists (conventional CT, 77% [92 of 120 readings]; DE CT, 91% [109 of 120 readings]; P = .005).
• Radiologists have greater confidence in assessments of type of extravasated contrast material made with DE CT (81%; 95% confidence interval: 78%, 91%) than in those made with conventional CT (67%; 95% confidence interval: 62%, 71%; significance of difference, P < .001).
Implication for Patient Care.
• Dual-contrast DE CT significantly increases diagnostic accuracy and confidence in the diagnosis of penetrating abdominopelvic trauma; further development of complementary contrast materials for human use may bring these benefits to clinical imaging.
Disclosures of Conflicts of Interest: J.M. No relevant conflicts of interest to disclose. S.R. No relevant conflicts of interest to disclose. Y.F. No relevant conflicts of interest to disclose. D.W.G. No relevant conflicts of interest to disclose. B.M.Y. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: is a consultant to GE Healthcare and Siemens Medical Systems; served as a speaker for GE Healthcare; institution received grants from Medrad and GE Healthcare. Other relationships: none to disclose.
Received June 8, 2012; revision requested July 25; revision received December 21; accepted February 4, 2013; final version accepted February 20.
Funding: This research was supported by the National Institutes of Health (grants 1 T32 EB001631, R01CA122257, and R21EB013816). J.M. is supported by NIBIB T32 training grant 1 T32 EB001631. S.R. is a Howard Hughes Medical Institute Medical Research Fellow.
Abbreviation:
- DE
- dual energy
References
- 1.Smith JE, Midwinter M, Lambert AW. Avoiding cavity surgery in penetrating torso trauma: the role of the computed tomography scan. Ann R Coll Surg Engl 2010;92(6):486–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beekley AC, Blackbourne LH, Sebesta JA, et al. Selective nonoperative management of penetrating torso injury from combat fragmentation wounds. J Trauma 2008;64(2 suppl):S108–S116; discussion S116–S117 [DOI] [PubMed] [Google Scholar]
- 3.Inaba K, Demetriades D. The nonoperative management of penetrating abdominal trauma. Adv Surg 2007;41:51–62 [DOI] [PubMed] [Google Scholar]
- 4.Shanmuganathan K, Mirvis SE, Chiu WC, Killeen KL, Hogan GJF, Scalea TM. Penetrating torso trauma: triple-contrast helical CT in peritoneal violation and organ injury—a prospective study in 200 patients. Radiology 2004;231(3):775–784 [DOI] [PubMed] [Google Scholar]
- 5.Fleischmann D, Boas FE. Computed tomography: old ideas and new technology. Eur Radiol 2011;21(3):510–517 [DOI] [PubMed] [Google Scholar]
- 6.Tran DN, Straka M, Roos JE, Napel S, Fleischmann D. Dual-energy CT discrimination of iodine and calcium: experimental results and implications for lower extremity CT angiography. Acad Radiol 2009;16(2):160–171 [DOI] [PubMed] [Google Scholar]
- 7.Anderson NG, Butler AP, Scott NJA, et al. Spectroscopic (multi-energy) CT distinguishes iodine and barium contrast material in MICE. Eur Radiol 2010;20(9):2126–2134 [DOI] [PubMed] [Google Scholar]
- 8.Nowak T, Hupfer M, Brauweiler R, Eisa F, Kalender WA. Potential of high-Z contrast agents in clinical contrast-enhanced computed tomography. Med Phys 2011;38(12):6469–6482 [DOI] [PubMed] [Google Scholar]
- 9.Mongan J, Rathnayake S, Fu Y, et al. In vivo differentiation of complementary contrast media at dual-energy CT. Radiology 2012;265(1):267–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qu M, Ehman E, Fletcher JG, et al. Toward biphasic computed tomography (CT) enteric contrast: material classification of luminal bismuth and mural iodine in a small-bowel phantom using dual-energy CT. J Comput Assist Tomogr 2012;36(5):554–559 [DOI] [PubMed] [Google Scholar]
- 11.Rosset A, Spadola L, Ratib O. OsiriX: an open-source software for navigating in multidimensional DICOM images. J Digit Imaging 2004;17:205–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sainsbury SJ. Fatal salicylate toxicity from bismuth subsalicylate. West J Med 1991;155(6):637–639 [PMC free article] [PubMed] [Google Scholar]


