Abstract
Many studies have reported the association of X-ray repair cross-complementing group 1 (XRCC1) Arg399Gln, Arg194Trp, Arg280His, −77T>C, and X-ray repair cross-complementing group 3 (XRCC3) T241M polymorphisms with lung cancer risk, but the results remained controversial. Hence, we performed a meta-analysis to investigate the association between lung cancer risk and XRCC1 Arg399Gln (14,156 cases and 16,667 controls from 41 studies), Arg194Trp (7,426 cases and 9,603 controls from 23 studies), Arg280His (6,211 cases and 6,763 controls from 16 studies), −77T>C (2,487 cases and 2,576 controls from 5 studies), and XRCC3 T241M (8,560 cases and 11,557 controls from 19 studies) in different inheritance models. We found that −77T>C polymorphism was associated with increased lung cancer risk (dominant model: odds ration [OR] = 1.45, 95% confidence interval [CI] = 1.27–1.66, recessive model: OR = 1.73, 95% CI = 1.14–2.62, additive model: OR = 1.91, 95% CI = 1.24–1.94) when all the eligible studies were pooled into the meta-analysis. In the stratified and sensitive analyses, significantly decreased lung cancer risk was observed in overall analysis (dominant model: OR = 0.83, 95% CI = 0.78–0.89; recessive model: OR = 0.90, 95% CI = 0.81–1.00; additive model: OR = 0.82, 95% CI = 0.74–0.92), Caucasians (dominant model: OR = 0.82, 95% CI = 0.76–0.87; recessive model: OR = 0.89, 95% CI = 0.80–0.99; additive model: OR = 0.81, 95% CI = 0.73–0.91), and hospital-based controls (dominant model: OR = 0.81, 95% CI = 0.76–0.88; recessive model: OR = 0.89, 95% CI = 0.79–1.00; additive model: OR = 0.80, 95% CI = 0.71–0.90) for XRCC3 T241M. In conclusion, this meta-analysis indicates that XRCC1 −77T>C shows an increased lung cancer risk and XRCC3 T241M polymorphism is associated with decreased lung cancer risk, especially in Caucasians.
Introduction
Lung cancer is a major cause of cancer-related death in the worldwide and the overall survival rate has still an extremely poor [1]. Although cigarette smoking is the major cause of lung cancer, only a small fraction of smokers develop this disease, suggesting that other causes, including genetic susceptibility, might contribute to the variation in individual lung cancer risk [2], [3]. Genetic susceptibility to environmental or occupational diseases is believed to play an important role in determining individual differences in the development of cancer. Research activities have focused on polymorphisms in DNA-repair genes as an important component of susceptibility because DNA-repair activities are critical for the protection of the genome and the prevention of cancer [4]. At the cellular level, checkpoints can be activated to arrest the cell cycle and transcription can be unregulated to compensate for the damage or the cell can apoptosis [5]. DNA repair is essential in protecting the cellular genome from environmental hazards, such as tobacco smoke [6]. Several studies have shown that a reduced DNA repair capacity is associated with increased lung cancer risk [7]–[9]. Many DNA repair genes carry genetic polymorphisms, with the potential to modulate gene function and alter DNA repair capacity [10].
The DNA repair pathways, including nucleotide excision repair (NER), base excision repair (BER) and double-strand break repair (DSBR) play an important role in repairing the DNA damage resulting from chemical alterations of a single base, such as methylated, oxidized, or reduced bases [11], [12]. The DNA repair enzymes XRCC1 play a central role in the BER pathway [13], [14]. XRCC1 is located on chromosome no. 19q13.2–13.3, and its gene product is implicated in single-strand break repair and base excision repair mechanisms [15]. XRCC1 encodes a protein that function in the repair of single-strand breaks. Shen et al [16] identified three coding polymorphisms in the XRCC1 gene at codons 194 (Arg to Trp), 280 (Arg to His), and 399 (Arg to Gln). 5′UTR–77T>C is a novel polymorphism identified in the XRCC1 gene located in the 5′untranslated region. Hao et al. [50] have reported that functional SNP −77T>C decreased transcriptional activity of C-allelecontaining promoter with higher affinity to Sp1 binding.
In the DSBR pathway, XRCC3 participate in DNA double-strand break/recombination repair and likely participates [17]–[19]. DSBs are the most common form of radiation-induced DNA damage [20] and are repaired by two pathways-homologous recombination repair (HRR) and no homologous end-joining [21]–[23]. The HRR pathway consists of at least 16 protein components, including XRCC3. A common polymorphism in exon 7 of the XRCC3 gene results in an amino acid substitution at codon 241 (Thr241Met) that may affect the enzyme function and/or its interaction with other proteins involved in DNA damage and repair [24].
Molecular epidemiological studies have reported the association of XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and XRCC3 T241M with lung cancer risk [25]–[73], but the results remain conflicting rather than conclusive. Although several studies [81]–[86] previously performed pooling analyses regarding the association of XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and XRCC3 T241M with lung cancer risk. However, several published studies were not included in these meta-analyses and additional original studies with larger sample sizes have been published since then. Importantly, the previous meta-analyses on XRCC1 Arg194Trp, Arg280His, and Arg399Gln with lung cancer risk have shown conflicting conclusions. Hence, the association of these polymorphic genes remains unknown. In order to explore the association between XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and XRCC3 T241M polymorphisms with lung cancer risk, a meta-analysis was conducted to summarize the data. Meta-analysis is a powerful tool for summarizing the different studies. It can not only overcome the problem of small size and inadequate statistical power of genetic studies of complex traits, but also provide more reliable results than a single case–control study.
Materials and Methods
Identification and eligibility of relevant studies
A comprehensive literature search was performed using the PubMed, ISI, and Embase databases for relevant articles published (last search was updated on Jan 12, 2013) with the following key words “XRCC1” or “XRCC3”, “polymorphism”, and “cancer” or “carcinoma” combined with “lung”. All eligible studies were retrieved, and their bibliographies were checked for other relevant publications. We excluded data that were unpublished or published in abstract only. We also reviewed the Cochrane Library for relevant articles. Additional articles were identified by hand searching references in the eligible articles and review articles that possibly have been missed in the initial search. Authors were contacted directly regarding crucial data not reported in original articles. When the same sample was used in several publications, only the study with the largest sample size was included following careful examination.
Inclusion criteria
The included studies needed to have met the following criteria: (1) only the case–control studies were considered, (2) evaluated the XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and XRCC3 T241M polymorphisms and lung cancer risk, and (3) sufficient published data for estimating an odds ratio (OR) with 95% confidence interval (CI). Major reasons for exclusion of studies were as follows: (1) not cancer research, (2) only case population, (3) duplicate of previous publication, and (4) the distribution of genotypes among controls are not in Hardy–Weinberg equilibrium (P<0.01).
Data extraction
Information was carefully extracted from all eligible studies independently by two investigators according to the inclusion criteria listed above. The following data were collected from each study: first author's name, year of publication, country of origin, ethnicity, source of controls, genotyping method, match, sample size, and numbers of cases and controls in the XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and XRCC3 T241M genotypes whenever possible. Ethnicity was categorized as “Caucasian”, “African”, and “Asian”. When a study did not state which ethnic groups were included or if it was impossible to separate participants according to phenotype, the sample was termed as “mixed population”. We did not define any minimum number of patients to include in this meta-analysis. Articles that reported different ethnic groups and different countries or locations, we considered them different study samples for each category cited above.
Statistical analysis
Crude odds ratios (ORs) together with their corresponding 95% confidence intervals (95% CIs) were used to assess the strength of association between the XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and XRCC3 T241M polymorphisms and lung cancer risk. The pooled ORs were performed for dominant model (Arg399Gln: Arg/Gln+Gln/Gln vs. Arg/Arg, Arg194Trp: Arg/Trp+Trp/Trp vs. Arg/Arg, Arg280His: Arg/His+His/His vs. Arg/Arg, −77T>C: TC+CC vs. TT, and T241M: TM+MM vs. TT); recessive model (Arg399Gln: Arg/Gln+Arg/Arg vs. Gln/Gln, Arg194Trp: Arg/Trp+Arg/Arg vs. Trp/Trp, Arg280His: Arg/His+Arg/Arg vs. His/His, −77T>C: TC+TT vs. CC, and T241M: TM+TT vs. MM); additive model (Arg399Gln: Arg/Arg vs. Gln/Gln, Arg194Trp: Arg/Arg vs. Trp/Trp, Arg280His: Arg/Arg vs. His/His, −77T>C: TT vs. CC, and T241M: TT vs. MM), respectively. Between-study heterogeneity was assessed by calculating Q-statistic (Heterogeneity was considered statistically significant if P<0.10) [74] and quantified using the I2 value, Venice criteria [75] for the I2 test included: “I2<25% represents no heterogeneity, I2 = 25–50% represents moderate heterogeneity, I2 = 50–75% represents large heterogeneity, and I2>75% represents extreme heterogeneity”. If results were not heterogeneous, the pooled ORs were calculated by the fixed-effect model (we used the Q-statistic, which represents the magnitude of heterogeneity between-studies) [76]. Otherwise, a random-effect model was used (when the heterogeneity between-studies were significant) [77]. We also performed subgroup analyses by ethnicity (Caucasian and Asian), source of controls, histological type, gender, and smoking habits. Moreover, the extent to which the combined risk estimate might be affected by individual studies was assessed by consecutively omitting every study from the meta-analysis (leave-one-out sensitivity analysis). This approach would also capture the effect of the oldest or first positive study (first study effect). Secondly, we also ranked studies according to sample size, and then repeated this meta-analysis. Sample size was classified according to a minimum of 200 participants and those with fewer than 200 participants. The cite criteria were previously described [78]. We assessed Hardy–Weinberg equilibrium (HWE) for each study using the goodness-of-fit test (χ 2 or Fisher exact test) only in control groups, and deviation was considered when P<0.01. Begg's funnel plots [79] and Egger's linear regression test [80] were used to assess publication bias. If publication bias existed, the Duval and Tweedie non-parametric “trim and fill” method was used to adjust for it. A meta-regression analysis was carried out to identify the major sources of between-studies variation in the results, using the log of the ORs from each study as dependent variables, and ethnicity, source of controls, and sample size as the possible sources of heterogeneity. All of the calculations were performed using STATA version 10.0 (STATA Corporation, College Station, TX).
Results
Literature Search and Meta-analysis Databases
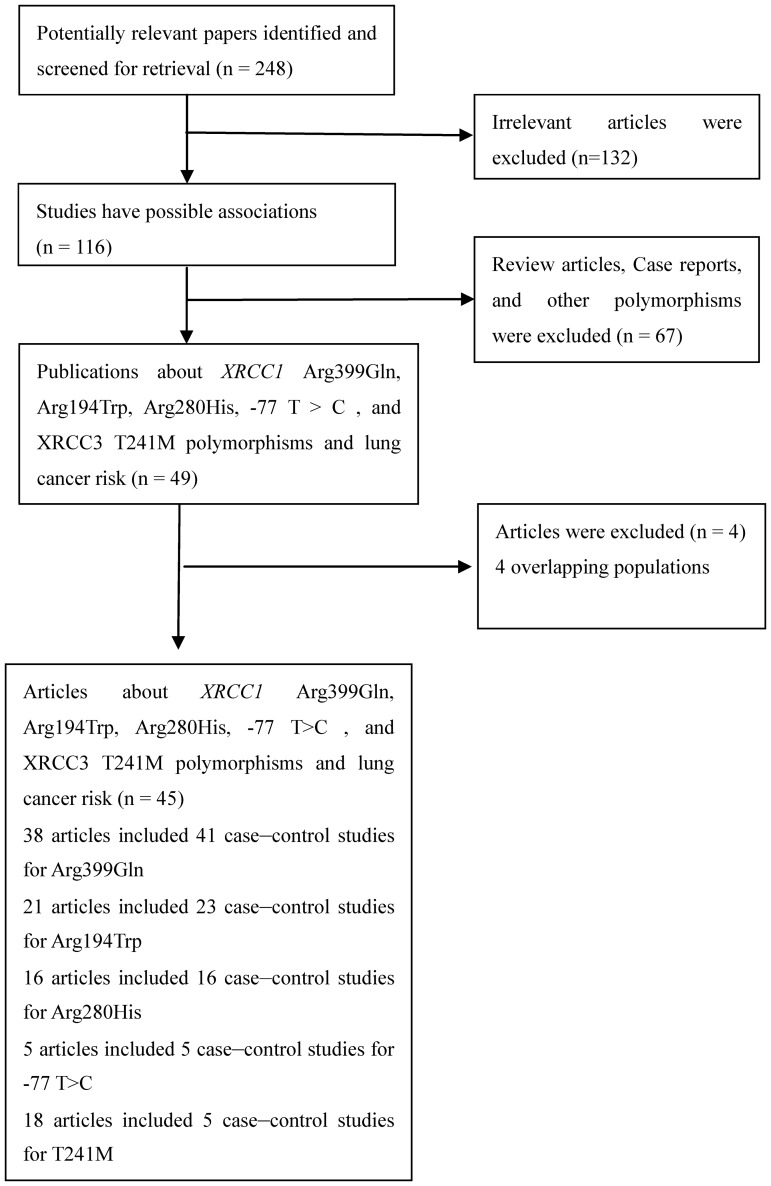
Relevant publications were retrieved and preliminarily screened. As shown in Fig. 1, 248 publications were identified, among which 132 irrelevant papers were excluded. Thus, 116 publications were eligible. Among these publications, 67 articles were excluded because they were review articles, case reports, and other polymorphisms of XRCC1 and XRCC3. In addition, Genotype distributions in the controls of all the eligible studies were in agreement with HWE. 4 articles [32], [37], [46], [60] were excluded because of their populations overlapped with another 2 included study [25], [33], [55], [59]. As summarized in Table 1, 45 articles with 104 case–control studies publications were selected in the final meta-analysis, including 14156 cases and 16,667 controls for XRCC1 Arg399Gln (from 41 studies), 7,426 cases and 9,603 controls for Arg194Trp (from 23 studies), 6,211 cases and 6,763 controls for Arg280His (from 16 studies), 2,487 cases and 2,576 controls for −77T>C (from 5 studies), and 8,560 cases and 11,557 controls for XRCC3 T241M (from 19 studies). Among these studies, five studies were included in the dominant model only because they provided the genotypes of TM+MM versus TT or Arg/Gln+Gln/Gln versus Arg/Arg as a whole and one study was included in the recessive model only because it provided the genotypes of TM+TT versus MM. 45 were population-based studies and 59 were hospital-based studies. 51 were conducted in Caucasians, 46 were conducted in Asians, and 6 studies were conducted in Africans. The remained were conducted in mixed ethnicity. Tables S1–S5 in File S1 listed ethnicity, HWE, and the numbers of cases and controls for XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and XRCC3 T241M. All of the cases were pathologically confirmed.
Figure 1. Study flow chart explaining the selection of the 45 eligible articles included in the meta-analysis.
Table 1. Main characteristics of all studies included in the meta-analysis.
| First author/year | Country | Ethnicity | SNPS | GM | SC | Matching |
| Ratnasinghe [25] 2001 | China | Asian | Arg399Gln | TaqMan | PB | Age/sex |
| Ratnasinghe [25] 2001 | China | Asian | Arg194Trp | TaqMan | PB | Age/sex |
| Ratnasinghe [25] 2001 | China | Asian | Arg280His | TaqMan | PB | Age/sex |
| David-Beabes [26] 2001 | USA | Caucasian | Arg399Gln | PCR-RFLP | PB | Age/sex/ethnicity |
| David-Beabes [26] 2001 | USA | Caucasian | Arg194Trp | PCR-RFLP | PB | Age/sex/ethnicity |
| David-Beabes [26] 2001 | USA | African | Arg399Gln | PCR-RFLP | PB | Age/sex/ethnicity |
| David-Beabes [26] 2001 | USA | African | Arg194Trp | PCR-RFLP | PB | Age/sex/ethnicity |
| David-Beabes [27] 2001 | USA | Caucasian | T241M | PCR-RFLP | PB | Age/sex/ethnicity |
| David-Beabes [27] 2001 | USA | African | T241M | PCR-RFLP | PB | Age/sex/ethnicity |
| Divine [28] 2001 | USA | Caucasian | Arg399Gln | PCR-RFLP | HB | No clear |
| Chen [29] 2002 | China | Asian | Arg399Gln | PCR | PB | Age/sex |
| Chen [29] 2002 | China | Asian | Arg194Trp | PCR | PB | Age/sex |
| Park [30] 2002 | Korea | Asian | Arg399Gln | PCR-RFLP | HB | Age |
| Misra [31] 2003 | USA | Caucasian | Arg399Gln | PCR | PB | Age |
| Misra [31] 2003 | USA | Caucasian | Arg280His | PCR | PB | Age |
| Misra [31] 2003 | USA | Caucasian | T241M | PCR | PB | Age |
| Zhou [33] 2003 | USA | Caucasian | Arg399Gln | PCR-RFLP | PB | No clear |
| Wang [34] 2003 | USA | Mixed | T241M | PCR-RFLP | PB | Age/ethnicity/gender |
| Ito [35] 2004 | Japan | Asian | Arg399Gln | PCR-CTTP | HB | Age/sex |
| Popanda [36] 2004 | German | Caucasian | Arg399Gln | PCR | HB | No clear |
| Popanda [36] 2004 | German | Caucasian | T241M | PCR | HB | No clear |
| Harms [38] 2004 | German | Caucasian | Arg399Gln | PCR | HB | Age/ethnicity/gender |
| Harms [38] 2004 | German | Caucasian | T241M | PCR | HB | Age/ethnicity/gender |
| Jacobsen [39] 2004 | Danish | Caucasian | T241M | PCR | PB | No clear |
| Zhang [40] 2005 | China | Asian | Arg399Gln | PCR-RFLP | PB | Age/sex |
| Hung [41] 2005 | Europe | Caucasian | Arg399Gln | PCR | HB | Age/sex/area |
| Hung [41] 2005 | Europe | Caucasian | Arg194Trp | PCR | HB | Age/sex/area |
| Hung [41] 2005 | Europe | Caucasian | Arg280His | PCR | HB | No clear |
| Hung [41] 2005 | Europe | Caucasian | T241M | PCR | HB | No clear |
| Vogel [42] 2004 | Danish | Caucasian | Arg399Gln | PCR | PB | No clear |
| Vogel [42] 2004 | Danish | Caucasian | Arg280His | PCR | PB | No clear |
| Schneider [43] 2005 | German | Caucasian | Arg399Gln | PCR | HB | No clear |
| Schneider [43] 2005 | German | Caucasian | Arg194Trp | PCR | HB | No clear |
| Schneider [43] 2005 | German | Caucasian | Arg280His | PCR | HB | No clear |
| Shen [44] 2005 | China | Asian | Arg399Gln | PCR | PB | Age/sex/village |
| Shen [44] 2005 | China | Asian | Arg194Trp | PCR | PB | Age/sex/village |
| Shen [44] 2005 | China | Asian | Arg280His | PCR | PB | Age/sex/village |
| Chan [45] 2005 | China | Asian | Arg399Gln | PCR-RFLP | HB | Age/sex |
| Chan [45] 2005 | China | Asian | Arg194Trp | PCR-RFLP | HB | Age/sex |
| Hu [47] 2005 | China | Asian | Arg399Gln | PCR | HB | Age/sex/area |
| Hu [47] 2005 | China | Asian | Arg194Trp | PCR | HB | Age/sex/area |
| Hu [47] 2005 | China | Asian | −77T>C | PCR-RFLP | HB | Age/sex/area |
| Zienolddiny [48] 2006 | Norway | Caucasian | Arg399Gln | TaqMan | PB | Age/sex/smoking |
| Zienolddiny [48] 2006 | Norway | Caucasian | Arg194Trp | TaqMan | PB | Age/sex/smoking |
| Zienolddiny [48] 2006 | Norway | Caucasian | Arg280His | TaqMan | PB | Age/sex/smoking |
| Zienolddiny [48] 2006 | Norway | Caucasian | T241M | TaqMan | PB | Age/sex/smoking |
| Matullo [49]2006 | Europe | Caucasian | Arg399Gln | TaqMan | PB | Age/sex/smoking |
| Matullo [49]2006 | Europe | Caucasian | T241M | TaqMan | PB | Age/sex/smoking |
| Hao [50] 2006 | China | Asian | Arg399Gln | PCR-RFLP | PB | Age/sex/ethnicity |
| Hao [50] 2006 | China | Asian | Arg194Trp | PCR-RFLP | PB | Age/sex/ethnicity |
| Hao [50] 2006 | China | Asian | Arg280His | PCR-RFLP | PB | Age/sex/ethnicity |
| Hao [50] 2006 | China | Asian | −77T>C | PCR-RFLP | PB | Age/sex/ethnicity |
| Landi [51] 2006 | Europe | Caucasian | Arg399Gln | PCR | HB | Age/sex/center/area |
| Landi [51] 2006 | Europe | Caucasian | Arg194Trp | PCR | HB | Age/sex/center/area |
| Landi [51] 2006 | Europe | Caucasian | Arg280His | PCR | HB | Age/sex/center/area |
| Landi [51] 2006 | Europe | Caucasian | T241M | PCR | HB | Age/sex/center/area |
| Ryk [52] 2006 | Swede | Caucasian | Arg399Gln | PCR | PB | Age/sex/smoking |
| Ryk [52] 2006 | Swede | Caucasian | T241M | TaqMan | PB | Age/sex/smoking |
| De Ruyck [53] 2007 | Belgium | Caucasian | Arg399Gln | PCR-RFLP | HB | Age/sex |
| De Ruyck [53] 2007 | Belgium | Caucasian | Arg194Trp | PCR-RFLP | HB | Age/sex |
| De Ruyck [53] 2007 | Belgium | Caucasian | Arg280His | PCR-RFLP | HB | Age/sex |
| De Ruyck [53] 2007 | Belgium | Caucasian | −77T>C | PCR-RFLP | HB | Age/sex |
| Pachouri [54] 2007 | India | Asian | Arg399Gln | PCR-RFLP | PB | No clear |
| Pachouri [54] 2007 | India | Asian | Arg194Trp | PCR-RFLP | PB | No clear |
| Yin [55] 2007 | China | Asian | Arg399Gln | PCR-RFLP | HB | Age/gender/ethnicity |
| Yin [55] 2007 | China | Asian | Arg194Trp | PCR-RFLP | HB | Age/gender/ethnicity |
| Yin [55] 2007 | China | Asian | Arg280His | PCR-RFLP | HB | Age/gender/ethnicity |
| Lopez-Cima [56] 2007 | Spain | Caucasian | Arg399Gln | PCR-RFLP | HB | Age/gender/ethnicity |
| Lopez-Cima [56] 2007 | Spain | Caucasian | T241M | PCR-RFLP | HB | Age/gender/ethnicity |
| Zhang [57] 2007 | China | Asian | T241M | PCR | HB | No clear |
| Improta [58] 2008 | Italy | Caucasian | Arg399Gln | PCR-RFLP | HB | Age/sex |
| Improta [58] 2008 | Italy | Caucasian | Arg194Trp | PCR-RFLP | HB | Age/sex |
| Improta [58] 2008 | Italy | Caucasian | T241M | PCR-RFLP | HB | Age/sex |
| Li [59] 2008 | China | Asian | Arg399Gln | PCR-RFLP | HB | Age |
| Li [59] 2008 | China | Asian | Arg194Trp | PCR-RFLP | HB | Age |
| Li [59] 2008 | China | Asian | Arg280His | PCR-RFLP | HB | Age |
| Li [59] 2008 | China | Asian | −77T>C | PCR-RFLP | HB | Age |
| Hsieh [61] 2009 | China | Asian | −77T>C | PCR | HB | No clear |
| Cote [62] 2009 | USA | Caucasian | Arg399Gln | PCR | PB | Age/race |
| Cote [62] 2009 | USA | African | Arg399Gln | PCR | PB | Age/race |
| Qian [63] 2010 | China | Asian | T241M | PCR | HB | Age/gender |
| Qian [63] 2010 | China | Asian | Arg399Gln | PCR | HB | Age/gender |
| Tanaka [64] 2010 | Japan | Asian | Arg194Trp | PCR | HB | Age/sex/ethnicity |
| Kim [65] 2010 | Korea | Asian | Arg399Gln | PCR | HB | No clear |
| Kim [65] 2010 | Korea | Asian | Arg280His | PCR | HB | No clear |
| Osawa [66] 2010 | Japan | Asian | T241M | PCR-RFLP | HB | No clear |
| Osawa [66] 2010 | Japan | Asian | Arg399Gln | PCR-RFLP | HB | No clear |
| Huang [67] 2011 | China | Asian | T241M | PCR-RFLP | HB | Age/sex |
| Janik [68] 2011 | Poland | Caucasian | Arg399Gln | PCR-SSCP | HB | Age/sex/smoking/diet |
| Janik [68] 2011 | Poland | Caucasian | Arg194Trp | PCR-SSCP | HB | Age/sex/smoking/diet |
| Janik [68]2011 | Poland | Caucasian | Arg280His | PCR-SSCP | HB | Age/sex/smoking/diet |
| Li [69] 2011 | China | Asian | Arg399Gln | PCR-CTTP | HB | Age/sex/area |
| Wang [70]2012 | China | Asian | Arg194Trp | PCR-RFLP | HB | Age/sex/area |
| Wang [70]2012 | China | Asian | Arg280His | PCR-RFLP | HB | Age/sex/area |
| Wang [70]2012 | China | Asian | Arg399Gln | PCR-RFLP | HB | Age/sex/area |
| Chikako [71] 2012 | Japan | Asian | Arg399Gln | PCR-RFLP | HB | Age/sex |
| Chikako [71] 2012 | Japan | Asian | T241M | PCR-RFLP | HB | Age/sex |
| Sreeja [72] 2008 | India | Asian | Arg399Gln | PCR-RFLP | HB | Age/sex |
| Chang [73] 2009 | USA | Caucasian | Arg399Gln | PCR-RFLP | PB | Age/sex/area |
| Chang [73] 2009 | USA | Caucasian | Arg194Trp | PCR-RFLP | PB | Age/sex/area |
| Chang [73] 2009 | USA | Caucasian | Arg280His | PCR-RFLP | PB | Age/sex/area |
| Chang [73] 2009 | USA | African | Arg399Gln | PCR-RFLP | PB | Age/sex/area |
| Chang [73] 2009 | USA | African | Arg194Trp | PCR-RFLP | PB | Age/sex/area |
SNPS Single-nucleotide polymorphism studied, GM Genotyping method, SC Source of controls, SSCP Single-strand conformation polymorphism, CTPP Contronting two-pair primers, SNPS Single-nucleotide polymorphism studied, PB Population-based study, HB Hospital-based study.
Quantitative synthesis
Table 2 listed the main results of the meta-analysis of XRCC1 Arg399Gln polymorphism and lung cancer risk. When all the eligible studies were pooled into the meta-analysis of XRCC1 Arg399Gln polymorphism, no significant association was found in any genetic model. However, significant between-study heterogeneity was detected in any genetic model. Hence, we performed subgroup analysis by ethnicity, histological type, smoker habits, gender, and source of controls. Among the stratified analysis, significantly increased lung cancer risk was observed in non-smokers (recessive model: OR = 1.57, 95% CI = 1.02–2.42, P value of heterogeneity test [P h] = 0.026, I 2 = 49.4%).
Table 2. Results of meta-analysis for XRCC1 and XRCC3 polymorphisms and lung cancer risk.
| Variables | No. comparisons (SZ case/control) | Dominant model | Recessive model | Additive model | |||
| OR (95% CI) | P h/I 2 | OR (95% CI) | P h/I 2 | OR (95% CI) | P h/I 2 | ||
| XRCC1 Arg399Gln | |||||||
| Overall | 41 (14,156/16,667) | 1.00 (0.94–1.07)* | 0.009/37.9% | 1.05 (0.94–1.18)* | 0.017/36.4% | 1.05 (0.93–1.19)* | 0.003/43.3% |
| Caucasian | 19 (7,308/9,140) | 0.98 (0.92–1.04) | 0.560/0.0% | 1.00 (0.87–1.16)* | 0.054/38.4% | 0.99 (0.89–1.10) | 0.120/29.7% |
| Asian | 19 (6,324/6,883) | 1.06 (0.94–1.20)* | <0.001/60.5% | 1.17 (0.96–1.41)* | 0.038/40.7% | 1.16 (0.93–1.46)* | 0.002/56.3% |
| African | 3 (524/644) | 1.04 (0.81–1.35) | 0.682/0.0% | 0.79 (0.39–1.62) | 0.603/0.0% | 0.80 (0.39–1.64) | 0.645/0.0% |
| PB | 18 (5,943/7,925) | 0.94 (0.87–1.01) | 0.116/29.5% | 1.01 (0.90–1.14) | 0.145/27.1% | 0.97 (0.86–1.10) | 0.119/29.8% |
| HB | 23 (8,213/8,742) | 1.07 (0.98–1.16)* | 0.062/33.4% | 1.15 (0.98–1.34)* | 0.015/44.7% | 1.17 (0.98–1.40)* | 0.004/50.9% |
| AC | 11 (1,821/5,536) | 1.13 (0.92–1.39)* | 0.002/64.4% | 1.31 (0.92–1.87)* | 0.001/66.7% | 1.34 (0.89–2.03)* | <0.001/73.3% |
| SC | 6 (1,688/4,014) | 0.97 (0.75–1.26)* | 0.006/69.4% | 1.06 (0.89–1.27) | 0.225/29.5% | 1.10 (0.77–1.57)* | 0.058/56.1% |
| SCLC | 3 (112/879) | 0.75 (0.37–1.55)* | 0.088/58.8% | 0.67 (0.32–1.43) | 0.642/0.0% | 0.62 (0.28–1.37) | 0.997/0.0% |
| Non-smokers | 15 (1,300/2,874) | 1.09 (0.83–1.43)* | 0.001/62.4% | 1.57 (1.02–2.42) * | 0.026/49.4% | 1.63 (0.99–2.68)* | 0.007/57.6% |
| Smokers | 16 (5,081/4,525) | 1.02 (0.94–1.11) | 0.536/0.0% | 1.02 (0.89–1.18) | 0.886/0.0% | 1.04 (0.89–1.21) | 0.743/0.0% |
| Male | 3 (441/414) | 1.08 (0.83–1.42) | 0.559/0.0% | 1.02 (0.39–4.31)* | 0.087/65.8% | 1.02 (0.60–1.72) | 0.159/49.7% |
| Female | 5 (773/826) | 0.96 (0.58–1.60)* | 0.001/78.1% | 1.94 (0.73–5.14)* | 0.014/71.8% | 1.86 (0.55–6.27)* | 0.001/80.6% |
| XRCC1 Arg194Trp | |||||||
| Overall | 23 (7,426/9,603) | 0.96 (0.86–1.07)* | 0.042/36.5% | 1.23 (1.05–1.44) | 0.216/18.8% | 1.22 (1.04–1.44) | 0.107/28.9% |
| Caucasian | 10 (3,926/5,639) | 0.88 (0.78–1.01) | 0.472/0.0% | 1.32 (0.78–2.23) | 0.104/41.2% | 1.29 (0.76–2.18) | 0.102/41.5% |
| Asian | 11 (3,091/3,441) | 1.02 (0.88–1.19)* | 0.065/42.6% | 1.22 (1.03–1.45) | 0.277/17.5% | 1.22 (1.02–1.45) | 0.111/36.0% |
| PB | 11 (2,610/4,446) | 0.98 (0.87–1.11) | 0.356/9.2% | 1.17 (0.93–1.49) | 0.359/9.1% | 1.16 (0.91–1.48) | 0.264/19.5% |
| HB | 12 (4,816/5,157) | 0.94 (0.80–1.11)* | 0.015/53.1% | 1.28 (1.03–1.59) | 0.141/32.2% | 1.29 (0.90–1.86)* | 0.077/40.8% |
| AC | 5 (880/3,276) | 0.97 (0.80–1.18) | 0.634/0.0% | 1.43 (0.86–2.40) | 0.587/0.0% | 1.41 (0.82–2.41) | 0.682/0.0% |
| SC | 3 (1,147/2,876) | 0.86 (0.70–1.05) | 0.850/0.0% | 1.38 (0.68–2.80) | 0.558/0.0% | 1.35 (0.63–2.88) | 0.554/0.0% |
| Non-smokers | 7 (618/1,666) | 1.07 (0.86–1.34) | 0.242/24.6% | 1.40 (0.38–5.17)* | 0.030/62.8% | 1.12 (0.26–4.79)* | 0.031/66.1% |
| Smokers | 6 (2,886/2,476) | 0.83 (0.71–0.98) | 0.141/39.7% | 0.93 (0.44–1.99) | 0.804/0.0% | 0.74 (0.30–1.85) | 0.681/0.0% |
| XRCC1 Arg280His | |||||||
| Overall | 16 (6,211/6,763) | 1.04 (0.83–1.29)* | <0.001/74.7% | 1.30 (0.71–2.37)* | 0.065/39.3% | 1.46 (0.99–2.15) | 0.146/29.0% |
| Caucasian | 9 (4,030/4,464) | 1.06 (0.92–1.22) | 0.133/35.6% | 0.96 (0.50–1.87) | 0.161/34.9% | 1.37 (0.68–2.78) | 0.721/0.0% |
| Asian | 7 (2,181/2,299) | 0.97 (0.64–1.48)* | <0.001/86.3% | 1.48 (0.68–3.21)* | 0.072/48.2% | 1.45 (0.60–3.48)* | 0.023/58.9% |
| PB | 7 (2,247/2,683) | 1.06 (0.90–1.23) | 0.334/12.5% | 1.32 (0.41–4.20)* | 0.048/52.9% | 1.43 (0.77–2.63) | 0.274/20.4% |
| HB | 9 (3,964/4,080) | 0.93 (0.64–1.35)* | <0.001/84.1% | 1.54 (0.94–2.51) | 0.244/24.2% | 1.32 (0.60–2.93)* | 0.097/44.1% |
| AC | 3 (795/2,864) | 0.70 (0.34–1.42)* | 0.001/85.5% | 0.36 (0.07–2.01) | – | 0.25 (0.04–1.39) | – |
| Non-smokers | 6 (715/1,340) | 0.63 (0.35–1.13)* | 0.001/74.7% | 0.78 (0.29–2.12) | 0.606/0.0% | 0.64 (0.23–1.75) | 0.380/0.0% |
| Smokers | 6 (2,977/2,457) | 1.04 (0.78–1.38) | 0.942/0.0% | 3.93 (0.44–35.3) | 0.820/0.0% | 4.16 (0.46–37.6) | 0.851/0.0% |
| XRCC1 −77T>C (rs3213245) | |||||||
| Overall | 5 (2,487/2,576) | 1.45 (1.27–1.66) | 0.638/0.0% | 1.73 (1.14–2.62) | 0.469/0.0% | 1.91 (1.24–2.94) | 0.494/0.0% |
| XRCC3 T241M (rs861539) | |||||||
| Overall | 19 (8,560/11,557) | 0.93 (0.83–1.04)* | 0.011/48.8% | 1.09 (0.88–1.35)* | 0.003/56.8% | 1.06 (0.83–1.37)* | <0.001//65.5% |
| Caucasian | 12 (6,089/8,992) | 0.92 (0.80–1.06)* | 0.003/60.6% | 1.07 (0.84–1.36)* | 0.001/67.6% | 1.04 (0.79–1.37)* | <0.001/72.5% |
| Asian | 5 (2,201/2,141) | 0.96 (0.78–1.18) | 0.447/0.0% | 1.20 (0.60–2.39) | 0.504/0.0% | 1.18 (0.54–2.55) | 0.302/16.5% |
| PB | 8 (1,528/2,950) | 0.91 (0.79–1.04) | 0.623/0.0% | 0.95 (0.75–1.20) | 0.820/0.0% | 0.93 (0.73–1.19) | 0.775/0.0% |
| HB | 11 (7,032/8,607) | 0.96 (0.80–1.14)* | 0.002/66.1% | 1.25 (0.88–1.77)* | <0.001/72.3% | 1.22 (0.81–1.85)* | <0.001/78.6% |
| Smokers | 5 (698/756) | 0.83 (0.67–1.03) | 0.137/42.8% | 1.32 (0.81–2.14) | 0.749/0.0% | 1.22 (0.74–2.01) | 0.822/0.0% |
AC Adenocarcinoma, SC Squamous cell carcinoma, SCLC Small cell lung cancer,
Random-effect model was used when P value of heterogeneity test (P h)<0.10; otherwise, fixed-effect model was used.
Table 2 also listed the main results of the meta-analysis of XRCC1 Arg194Trp polymorphism and lung cancer risk. When all the eligible studies were pooled into the meta-analysis of XRCC1 Arg194Trp polymorphism, significantly increased risk of lung cancer was observed in the recessive model (OR = 1.23, 95% CI = 1.05–1.44, P h = 0.216, I2 = 18.8%) and additive model (OR = 1.22, 95% CI = 1.04–1.44, P h = 0.107, I2 = 28.9%). Among the stratified analyses, significantly increased lung cancer risk was observed in Asians (recessive model: OR = 1.22, 95% CI = 1.03–1.45, P h = 0.277, I2 = 17.5%; additive model: OR = 1.22, 95% CI = 1.02–1.45, P h = 0.111, I2 = 36.0%) and the hospital-based controls (recessive model: OR = 1.28, 95% CI = 1.03–1.59, P h = 0.141, I2 = 32.2%).
Table 2 also listed the main results of the meta-analysis of XRCC1 Arg280His polymorphism and lung cancer risk. When all the eligible studies were pooled into the meta-analysis of XRCC1 Arg280His polymorphism, no significant association was observed in any genetic model. In the stratified analyses, there was not still significant association between XRCC1 Arg280His polymorphism and lung cancer risk.
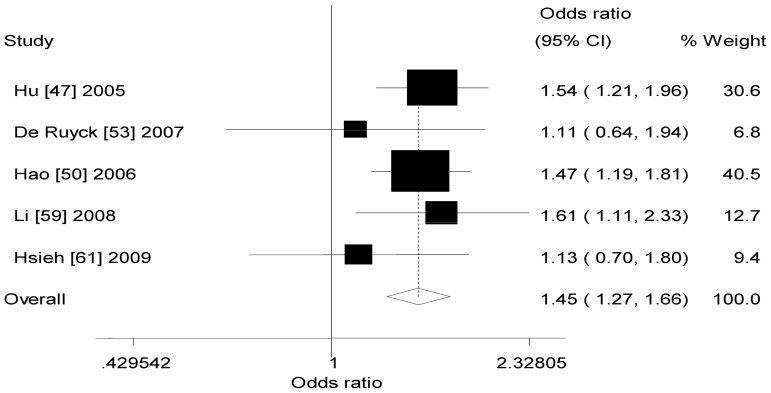
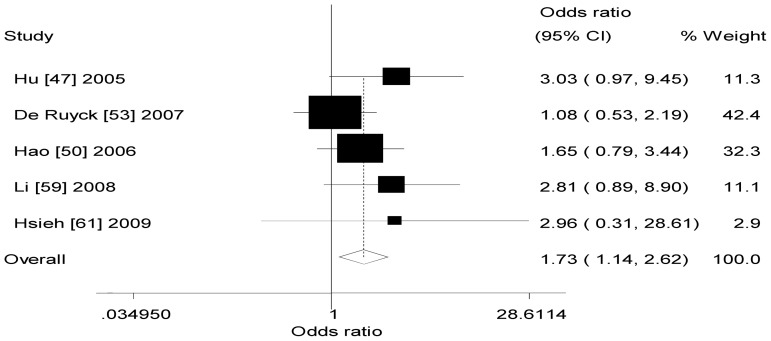
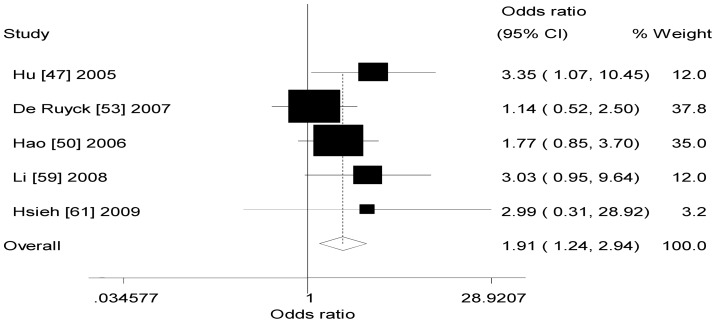
Table 2 also listed the main results of the meta-analysis of XRCC1 −77T>C polymorphism and lung cancer risk. When all the eligible studies were pooled into the meta-analysis of XRCC1 −77 T>C polymorphism, significant increased risk of lung cancer was observed in any genetic model (dominant model: OR = 1.45, 95% CI = 1.27–1.66, P h = 0.638, I2 = 0.0%, Fig. 2; recessive model: OR = 1.73, 95% CI = 1.14–2.62, P h = 0.469, I2 = 0.0%, Fig. 3; additive model: OR = 1.91, 95% CI = 1.24–2.94, P h = 0.494, I2 = 0.0%, Fig. 4).
Figure 2. Forest plot of XRCC1 −77T>C polymorphism and lung cancer risk (dominant model).
Figure 3. Forest plot of XRCC1 −77T>C polymorphism and lung cancer risk (recessive model).
Figure 4. Forest plot of XRCC1 −77T>C polymorphism and lung cancer risk (additive model).
Table 2 also listed the main results of the meta-analysis of XRCC3 T241M polymorphism and lung cancer risk. When all the eligible studies were pooled into the meta-analysis of XRCC3 T241M polymorphism, there was no evidence of significant association between lung cancer risk and XRCC3 T241M polymorphism in any genetic model. In the stratified analysis, there was not still significant association.
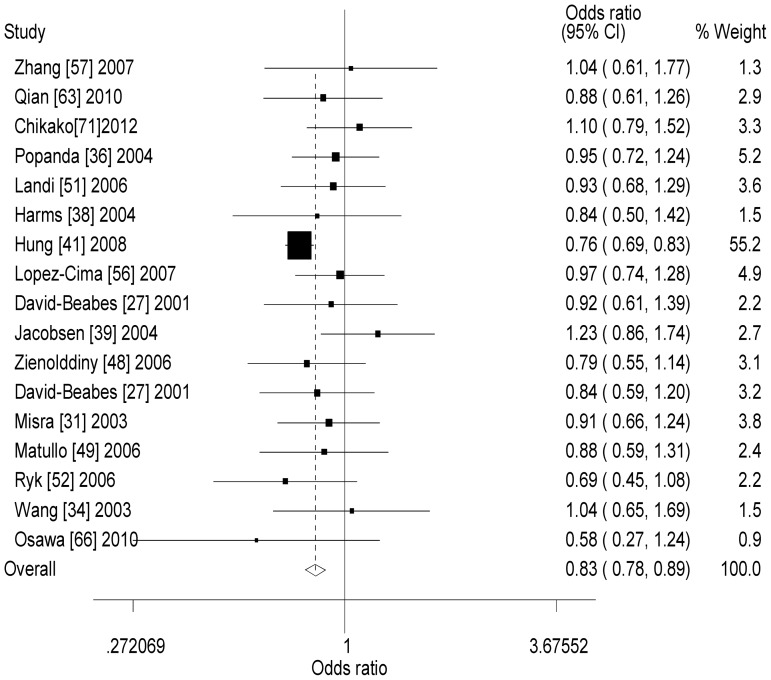
Heterogeneity and sensitive analysis
There was significant heterogeneity among these studies for dominant model comparison (XRCC1 Arg399Gln: P h = 0.009, XRCC1 Arg194Trp: P h = 0.042, XRCC1 Arg280His: P h<0.001, and XRCC3 T241M: P h = 0.011); recessive model comparison (XRCC1 Arg399Gln: P h = 0.017 and XRCC3 T241M = 0.003); additive model comparison (XRCC1 Arg399Gln: P h = 0.003 and XRCC3 T241M<0.001). Then, we assessed the source of heterogeneity by meta-regression analysis. We found that source of controls, ethnicity, and sample size did not contribute to substantial heterogeneity among the meta-analysis (data not shown). Sensitivity analyses were conducted to determine whether modification of the inclusion criteria of this meta-analysis affected the results. Although the sample size for cases and controls in all eligible studies ranged from 100 to 8,488, the corresponding pooled ORs were not qualitatively altered with or without the study of small sample. However, for XRCC1 Arg399Gln polymorphism, when one study was excluded, the results were changed in non-smokers (recessive model: OR = 1.12, 95% CI = 0.96–1.21, P h = 0.114, I2 = 32.6%). For XRCC1 Arg194Trp polymorphism, when one study was excluded, the results were also changed in overall analysis (recessive model: OR = 1.17, 95% CI = 0.99–1.39, P h = 0.313, I2 = 11.4%; additive model: OR = 1.15, 95% CI = 0.97–1.37, P h = 0.227, I2 = 18.3%), Asians (recessive model: OR = 1.16, 95% CI = 0.97–1.38, P h = 0.447, I2 = 0.0%; additive model: OR = 1.14, 95% CI = 0.95–1.37, P h = 0.295, I2 = 16.1%), hospital-based studies (recessive model: OR = 1.17, 95% CI = 0.92–1.49, P h = 0.241, I2 = 21.9%), and smokers (dominant model: OR = 0.87, 95% CI = 0.74–1.03, Ph = 0.409, I2 = 0.0%). For XRCC3 T241M polymorphism, when one study was excluded, significantly decreased lung cancer risk was observed in overall analysis (dominant model: OR = 0.83, 95% CI = 0.78–0.89, P h = 0.302, I 2 = 13.0%, Fig. 5; recessive model: OR = 0.90, 95% CI = 0.81–1.00, P h = 0.507, I 2 = 0.0%; additive model: OR = 0.82, 95% CI = 0.74–0.92, P h = 0.278, I 2 = 16.1%), Caucasians (dominant model: OR = 0.82, 95% CI = 0.76–0.87, P h = 0.248, I 2 = 20.5%; recessive model: OR = 0.89, 95% CI = 0.80–0.99, P h = 0.427, I 2 = 6.3%; additive model: OR = 0.81, 95% CI = 0.73–0.91, P h = 0.277, I 2 = 18.1%), and hospital-based controls (dominant model: OR = 0.81, 95% CI = 0.76–0.88, P h = 0.193, I 2 = 28.2%; recessive model: OR = 0.89, 95% CI = 0.79–1.00, P h = 0.213, I 2 = 25.9%; additive model: OR = 0.80, 95% CI = 0.71–0.90, P h = 0.108, I 2 = 40.6%).
Figure 5. Forest plot of XRCC3 T241M polymorphism and lung cancer risk when one study was excluded (dominant model).
Publication bias
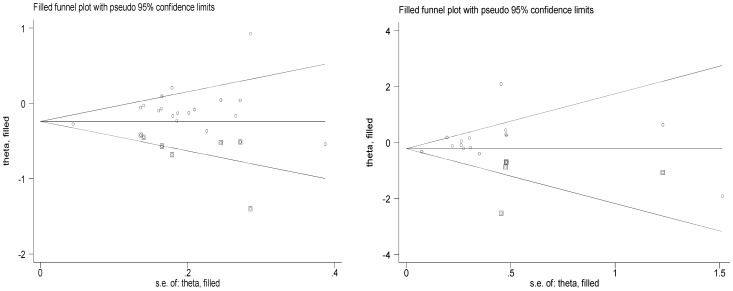
Begg's funnel plot and Egger's test did not reveal any publication bias for XRCC1 Arg399Gln (P = 0.546 for dominant model, P = 0.767 for recessive model, and P = 0.984 for additive model), Arg194Trp (P = 0.588 for dominant model, P = 0.416 for recessive model, P = 0.555 for additive model), Arg280His (P = 0.439 for dominant model, P = 0.520 for recessive model, P = 0.292 for additive mode), −77T>C (P = 0.186 for dominant model, P = 0.162 for recessive model, P = 0.246 for additive mode), although possible publication bias was suggested between XRCC3 T241M polymorphism and lung cancer risk in dominant model (P = 0.012) and additive model (P = 0.041). This might be a limitation for this meta-analysis because studies with null findings, especially those with small sample size, are less likely to be published. The Duval and Tweedie non-parametric “trim and fill” method was used to adjust for publication bias. Meta-analysis with and without “trim and fill” did not draw different conclusion (Fig. 6), indicating that our results were statistically robust.
Figure 6. The Duval and Tweedie nonparametric “trim and fill” method's funnel plot funnel plot of the meta-analysis of lung cancer risk and XRCC3 T241M polymorphism (dominant model and additive model).
Discussion
BER and DSBR play an important role in repairing the DNA damage resulting from chemical alterations of a single base, such as methylated, oxidized, or reduced bases. BER includes two major processes (excision of damaged base residues and core BER reaction, including strand incision at the abasic site, one nucleotide gap-filling reaction, and sealing of the remaining nick). It is well known that a number of proteins are involved in these steps, of which XRCC1 play key roles. XRCC1 acts as a facilitator or coordinator in BER, through its interaction with poly (ADP-ribose) polymerase, DNA polymerase b, and DNA ligase III [15], [95]. Four coding polymorphisms were identified in the XRCC1 gene at the codons 194 (Arg to Trp), 280 (Arg to His), 399 (Arg to Gln), and −77 T>C. Whereas the functional effects of these polymorphisms in XRCC1 have not been well known, amino acid changes at evolutionary conserved regions may alter its function. In particular, the 399Gln polymorphism resulting from a guanine to adenine nucleotide occurs in the poly (ADP-ribose) polymerase binding domain and may affect complex assembly or repair efficiency. The XRCC3 gene codes for a protein involved in homologous recombinational repair (HRR) for double strand breaks of DNA (DBSs) and cross-link repair in mammalian cells [20]. During HRR, the XRCC3 protein interacts with Rad51 protein and likely contributes to maintain chromosome stability. A common polymorphism in exon 7 of the XRCC3 gene results in an amino acid substitution at codon 241 (Thr241Met) that may affect the enzyme function and/or its interaction with other proteins involved in DNA damage and repair [20]. Many molecular epidemiological studies have reported the role of XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and XRCC3 T241M in lung cancer risk [25]–[73], but the results remain conflicting rather than conclusive. In order to resolve this conflict, meta-analysis was performed to examine the association between XRCC1 and XRCC3 polymorphisms and lung cancer risk, by critically reviewing 41 studies on XRCC1 Arg399Gln, 23 studies on Arg194Trp, 16 studies on Arg280His, 5 studies on −77T>C, and 19 studies on XRCC3 T241M.
Overall, our meta-analysis indicates that XRCC1 −77T>C polymorphism is associated with increased lung cancer risk when all eligible studies were pooled into the meta-analysis. In further stratified and sensitivity analyses, significantly decreased lung cancer risk was observed in Caucasians for XRCC3 T241M, but not in Asians. It should be considered that the apparent inconsistency of these results may underlie differences in ethnicity, lifestyle and disease prevalence as well as possible limitations due to the relatively small sample size. The current knowledge of carcinogenesis indicates a multi-factorial and multistep process that involves various genetic alterations and several biological pathways. Thus, it is unlikely that risk factors of cancer work in isolation from each other. And the same polymorphisms may play different roles in cancer susceptibility, because cancer is a complicated multi-genetic disease, and different genetic backgrounds may contribute to the discrepancy. And even more importantly, the low penetrance genetic effects of single polymorphism may largely depend on interaction with other polymorphisms and/or a particular environmental exposure.
Present meta-analysis results were not consistent with a previous meta-analysis [81]–[86] on XRCC1 and XRCC3 polymorphisms with lung cancer risk. Kiyohara et al. [81] included 18 case–control studies on XRCC1 Arg399Gln, 9 studies on Arg194Trp, and 7 studies on Arg280His. Their results suggested that XRCC1 Arg399Gln polymorphism was associated with increased lung cancer risk among Asians (OR = 1.34, 95% CI = 1.16–1.54) and Arg194Trp and Arg280His polymorphisms were not associated with lung cancer risk. However, at any case, their results about Arg399Gln and lung cancer risk essentially remains an open field in Asians, as the number of studies (n = 6) is considerably smaller than that needed for the achievement of robust conclusions [96]. Wang et al. [82] included 30 case–control studies on XRCC1 Arg399Gln and 16 studies on Arg194Trp. Their results indicated that certain XRCC1 codon 399 and 194 variant may affect the susceptibility of lung cancer. Dai et al. [83] included 39 studies on XRCC1 Arg399Gln, 22 studies on Arg194Trp, and 12 studies on Arg280His. Their meta-analysis had demonstrated that codon 194, codon 399 and −77 T>C polymorphisms of XRCC1 gene might have contributed to individual susceptibility to lung cancer. However, in further subgroup and sensitivity analyses, we found XRCC1 Arg399Gln and Arg194Trp polymorphisms were not associated with lung cancer risk when one study was excluded, hence, we thought XRCC1 Arg399Gln and Arg194Trp polymorphisms may be not associated with lung cancer risk. Sun et al. [84] in 2010 included 14 case–control studies on XRCC3 T241M, their meta-analysis found that there was no evidence showing a significant association between XRCC3 Thr241Met polymorphism and lung cancer risk. Zhan et al. [85] in 2013 included 17 case–control studies on XRCC3 T241M, their meta-analysis indicated that there was no evidence showing a significant correlation between XRCC3 Thr241Met polymorphism and lung cancer risk stratified analysis by ethnicity, histology and smoking status. Xu et al. [86] in 2013 included 17 case–control studies on XRCC3 T241M, their meta-analysis all available data did not support any appreciable association between the XRCC3 Thr241Met polymorphism and lung cancer risk in any populations. However, in further subgroup and sensitivity analyses, we found XRCC3 T241M polymorphism was associated with lung cancer risk in Caucasians. Vineis et al. [97] in 2009 only included 3 case–control studies on XRCC1 polymorphism, their found XRCC1 −77T>C polymorphism was associated with lung cancer risk. Having analyzed an almost twofold larger number of studies than the previous meta-analysis [81]–[86], our results seem to confirm and establish the trend in the meta-analysis of XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and T241M polymorphisms that the data by the previous meta-analysis [81]–[86] had indicated. Importantly, we carefully performed sensitivity analysis according to sample size and leave-one-out analysis, conducted different conclusions with the previous meta-analysis. For XRCC1 −77 T>C polymorphism, the T to C mutation greatly enhances the affinity of nuclear protein Sp1 to the XRCC1 promoter region, which may inhibit its transcription [50]. Up to now, only five case–control studies were conducted the association between −77 T>C polymorphism and lung cancer risk [47], [50], [53], [59], [61]. The pooled OR of these five studies, comparing the combined variant genotype CT+CC to wild genotype TT, was 1.45 (95% CI 1.27–1.66). Among these five studies, four studies carried out in Asians with large sample size all showed that −77 T>C polymorphism was significantly associated with increased risk of developing lung cancer and the summary OR was 1.48 (95% CI 1.28–1.70), which suggested that the −77 T>C polymorphism may be contributed to the developing of lung cancer in Asians. Due to the relative small sample size from the selected studies, a case–control study with larger sample size or multiple center study will be needed to get conclusive results. In addition, the sample size was also too small for the XRCC3 Thr241Met polymorphism and lung cancer risk in Asians and Africans. Hence, a case–control study with larger sample size or multiple center study will be needed to get conclusive results in Asians and Africans.
DNA repair is well known as a “double-edged sword” in cancer studies. Epidemiological evidence supports that DNA repair capacity is one of the determinants of genetic susceptibility to cancer [87]–[89]. Liu et al. [98] found that XRCC1 −77T>C polymorphism may be a genetic determinant for developing breast cancer. However, other cancer such as gastric cancer, colorectal cancer and so on with XRCC1 −77T>C polymorphism remained unclear. Hence, some new studies are needed to get conclusive results among other cancer. On the other hand, tumors with enhanced DNA repair capacity would exhibit an intrinsic resistance to the anti-tumour activity during chemotherapy and radiotherapy [90]. Fluorouracil (5-FU)/oxaliplatin-based chemotherapy induced DNA damages and causes cell death [91]. These damages are mainly repaired by the BER pathway. A 5-fold greater incidence of failure by 5-FU/oxaliplatin therapy had been reported for metastatic colorectal cancer patients with XRCC1 R399Q (QQ or QR) substitution compared with that of the RR genotype, suggesting that the polymorphism was associated with resistance to oxaliplatin/5-FU therapy [92]. In addition, it had been found that XRCC1 codon 194 variant was having a significant protective effect on development of late radiotherapy reactions in normal tissue [93]. It had also found that interactions among XRCC1 codon 194 variant was associated with sensitivity to platinum-based chemotherapy [100]. Furthermore, Sak et al. [94] indicated that high levels of XRCC1 protein expression were associated with improved cancer-specific survival in patients following radical radiotherapy. However, Liu et al. [99] indicated that XRCC1 T-77C could not be genetic determinant for prognosis of advanced non-small-cell lung cancer (NSCLC) patients treated with platinum-based chemotherapy. Therefore, XRCC1 Arg399Gln and Arg194Trp might play important roles in the drug sensitivity during chemotherapy and radio sensitivity during radiotherapy and XRCC1 −77 T>C may be not play important roles in the drug sensitivity during chemotherapy.
Heterogeneity is a potential problem when interpreting the results of all meta-analyses. As looked through our study carefully, we found that the study of Improta et al. [58] was noted to be a major source of heterogeneity for XRCC3 T241M and Li et al. [59] was also noted to be a major source of heterogeneity for XRCC1 Arg280His. The reason may be that the study of Improta et al. [58] and Li et al. [59] were hospital-based studies. Importantly, when Improta et al. [58] was excluded, significantly decreased lung cancer risk was observed in overall analysis, Caucasians, and hospital-based controls.
Some limitations of this meta-analysis should be addressed. First, misclassifications on disease status and genotypes may influence the results, because cases in some studies were not confirmed by pathology or other gold standard method, and the quality control of genotyping was also not well-documented in some studies. Second, in the subgroup analysis may have had insufficient statistical power to check an association, Third, our results were based on unadjusted estimates, while a more precise analysis should be conducted if individual data were available, which would allow for the adjustment by other co-variants, including environmental factors and other lifestyle. In spite of these, our meta-analysis also had some advantages. First, it provides pooled data on a substantial number of cases and controls and increased statistical power of the analysis. Second, although possible publication bias was suggested between XRCC3 T241M polymorphism and lung cancer risk, adjusting for possible publication bias using the Duval and Tweedie nonparametric “trim and fill” method showed that the results did not change, indicating that the whole pooled results should be unbiased. Third, our meta-analysis explores and analyzes the sources of heterogeneity between studies about XRCC3 T241M and Arg280His in lung cancer risk.
In conclusion, this meta-analysis indicates that XRCC1 −77T>C shows an increased lung cancer risk and XRCC3 T241M polymorphism is associated with decreased lung cancer risk in Caucasians. However, a study with a larger sample size is needed to further evaluate gene-environment interaction on XRCC1 Arg399Gln, Arg194Trp, Arg280His, −77T>C, and XRCC3 T241M polymorphisms and lung cancer risk.
Supporting Information
PRISMA 2009 checklist.
(DOC)
Table S1, Genotypes, p values and subset of cases of XRCC1 Arg399Gln polymorphism included in the meta-analysis. Table S2, Genotypes, p values and subset of cases of XRCC1 Arg194Trp (rs1799782) polymorphism included in the meta-analysis. Table S3, Genotypes, P values and subset of cases of XRCC1 Arg280His (rs25489) polymorphism included in the meta-analysis. Table S4, Genotypes, P values and subset of cases of XRCC1 −77T>C (rs3213245) polymorphism included in the meta-analysis. Table S5, Genotypes, P values and subset of cases of XRCC3 T241M (rs861539) polymorphism included in the meta-analysis.
(DOC)
Funding Statement
The authors have no support or funding to report.
References
- 1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, et al. (2011) Global cancer statistics. CA Cancer J Clin 61: 69–90. [DOI] [PubMed] [Google Scholar]
- 2. Tardon A, Lee WJ, Delgado-Rodriguez M, Dosemeci M, Albanes D, et al. (2005) Leisure-time physical activity and lung cancer: a meta-analysis. Cancer Causes Control 16: 389–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rodriguez V, Tardon A, Kogevinas M, Prieto CS, Cueto A, et al. (2000) Lung cancer risk in iron and steel foundry workers: a nested case–control study in Asturias, Spain. Am J Ind Me 38: 644–50. [DOI] [PubMed] [Google Scholar]
- 4. Spitz MR, Wei Q, Dong Q, Amos CI, Wu X (2003) Genetic susceptibility to lung cancer: the role of DNA damage and repair. Cancer Epidemiol Biomarkers Prev 12: 689–98. [PubMed] [Google Scholar]
- 5. Vispe S, Yung TM, Ritchot J, Serizawa H, Satoh MS (2000) A cellular defense pathway regulating transcription through poly (ADPribosyl) ation in response to DNA damage. Proc Natl Acad Sci U S A 97: 9886–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hoeijmakers JH (2001) Genome maintenance mechanisms for preventing cancer. Nature 411: 366–74. [DOI] [PubMed] [Google Scholar]
- 7. Wei Q, Cheng L, Hong WK, Spitz MR (1996) Reduced DNA repair capacity in lung cancer patients,. Cancer Res 56: 4103–7. [PubMed] [Google Scholar]
- 8. Wei Q, Cheng L, Amos CI, Wang LE, Guo Z, et al. (2000) Repair of tobacco carcinogen-induced DNA adducts and lung cancer risk: a molecular epidemiologic study. J Natl Cancer Inst 92: 1764–72. [DOI] [PubMed] [Google Scholar]
- 9. Shen H, Spitz MR, Qiao Y, Guo Z, Wang LE, et al. (2003) Smoking, DNA repair capacity and risk of non-small cell lung cancer. Int J Cancer 107: 84–88. [DOI] [PubMed] [Google Scholar]
- 10. Xi T, Jones IM, Mohrenweiser HW (2004) Many amino acid substitution variants identified in DNA repair genes during human population screenings are predicted to impact protein function. Genomics 83: 970–9. [DOI] [PubMed] [Google Scholar]
- 11. Yu Z, Chen J, Ford BN, Brackley ME, Glickman BW (1999) Human DNA repair systems: an overview. Environ Mol Mutagen 33: 3–20. [DOI] [PubMed] [Google Scholar]
- 12. Wood RD, Mitchell M, Sgouros J, Lindahl T (2001) Human DNA repair genes. Science 291: 1284–9. [DOI] [PubMed] [Google Scholar]
- 13. Vidal AE, Boiteux S, Hickson AD, Radicella JP (2001) XRCC1 coordinates the initial and late stages of DNA abasic site repair through protein–protein interactions,. EMBO J 20: 6530–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lu AL, Li XH, Gu YS, Wright PM, Chang DY (2001) Repair of oxidative DNA damage–mechanisms and functions,Cell Biochem. Biophys 35: 141–70. [DOI] [PubMed] [Google Scholar]
- 15. Kubota Y, Nash RA, Klungland A, Schär P, Barnes DE, et al. (1996) Resconstitution of DNA base excision repair with purified human proteins: Interaction between DNA polymerase beta and the XRCC1 protein. EMBO J 15: 6662–70. [PMC free article] [PubMed] [Google Scholar]
- 16. Shen MR, Jones IM, Mohrenweiser H (1998) No conservative amino acid substitution variants exist at polymorphic frequency in DNA repair genes in healthy humans. Cancer Res 58: 604–8. [PubMed] [Google Scholar]
- 17. Shin A, Lee KM, Ahn B, Park CG, Noh SK, et al. (2008) Genotype-phenotype relationship between DNA repair gene genetic polymorphisms and DNA repair capacity. Asian Pac J Cancer Prev 9: 501–5. [PubMed] [Google Scholar]
- 18. Tebbs RS, Zhao Y, Tucker JD, Scheerer JB, Siciliano MJ, et al. (1995) Correction of chromosomal instability and sensitivity to diverse mutagens by a cloned cDNA of the XRCC3 DNA repair gene. Proc Natl Acad Sci USA 92: 6354–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thacker J, Zdzienicka MZ (2004) The XRCC genes: expanding roles in DNA double-strand break repair. DNARepair (Amst.) 3: 1081–90. [DOI] [PubMed] [Google Scholar]
- 20. Matullo G, Palli D, Peluso M, Guarrera S, Carturan S, et al. (2001) XRCC1, XRCC3, XPD gene polymorphisms, smoking and 32P-DNA adducts in a sample of healthy subjects. Carcinogenesis 22: 1437–45. [DOI] [PubMed] [Google Scholar]
- 21. Ward J (1988) DNA damage produced by ionizing radiation in mammalian cells: identities, mechanisms of formation and reparability. Prog Nucleic Acids Res Mol Biol 35: 95–125. [DOI] [PubMed] [Google Scholar]
- 22. Mohrenweiser H, Wilson D, Jones I (2003) Challenges and complexities in estimating both the functional impact and the disease risk associated with the extensive genetic variation in human DNA repair genes. Mutat Res 526: 93–125. [DOI] [PubMed] [Google Scholar]
- 23. Goode E, Ulrich C, Potter J (2002) Polymorphisms in DNA repairs genes and associations with cancer risk. Cancer Epidemiol Biomarkers Prev 11: 1513–30. [PubMed] [Google Scholar]
- 24. Kuschel B, Auranen A, McBride S, Novik KL, Antoniou A, et al. (2002) Variants in double-strand break repair genes and breast cancer susceptibility. Hum Mol Genet 11: 1399–440. [DOI] [PubMed] [Google Scholar]
- 25. Ratnasinghe D, Yao SX, Tangrea JA, Qiao YL, Andersen MR, et al. (2001) Polymorphisms of the DNA repair gene XRCC1 and lung cancer risk. Cancer Epidemiol Biomarkers Prev 10: 119–23. [PubMed] [Google Scholar]
- 26. David-Beabes GL, London SJ (2001) Genetic polymorphism of XRCC1 and lung cancer risk among African-Americans and Caucasians. Lung Cancer 34: 333–9. [DOI] [PubMed] [Google Scholar]
- 27. David-Beabes GL, Lunn RM, London SJ (2001) No association between the XPD (Lys751G1n) polymorphism and the XRCC3 (Thr241Met) polymorphism and lung cancer risk. Cancer Epidemiol Biomarkers Prev 10: 911–2. [PubMed] [Google Scholar]
- 28. Divine KK, Gilliland FD, Crowell RE, Stidley CA, Bocklage TJ, et al. (2001) The XRCC1 399 glutamine allele is a risk factor for adenocarcinoma of the lung. Mutat Res 461: 273–8. [DOI] [PubMed] [Google Scholar]
- 29. Chen S, Tang D, Xue K, Xu L, Ma G, et al. (2002) DNA repair gene XRCC1 and XPD polymorphisms and risk of lung cancer in a Chinese population. Carcinogenesis 23: 1321–5. [DOI] [PubMed] [Google Scholar]
- 30. Park JY, Lee SY, Jeon HS, Bae NC, Chae SC, et al. (2002) Polymorphism of the DNA repair gene XRCC1 and risk of primary lung cancer. Cancer Epidemiol Biomarkers Prev 11: 23–7. [PubMed] [Google Scholar]
- 31. Misra RR, Ratnasinghe D, Tangrea JA, Virtamo J, Andersen MR, et al. (2003) Polymorphisms in the DNA repair genes XPD, XRCC1, XRCC3, and APE/ref-1, and the risk of lung cancer among male smokers in Finland. Cancer Lett 191: 171–8. [DOI] [PubMed] [Google Scholar]
- 32. Ratnasinghe DL, Yao SX, Forman M, Qiao YL, Andersen MR, et al. (2003) Gene-environment interactions between the codon 194 polymorphism of XRCC1 and antioxidants influence lung cancer risk. Anticancer Res 23: 627–32. [PubMed] [Google Scholar]
- 33. Zhou W, Liu G, Miller DP, Thurston SW, Xu LL, et al. (2004) Polymorphisms in the DNA repair genes XRCC1 and ERCC2, smoking, and lung cancer risk. Cancer Epidemiol Biomarkers Prev 12: 359–65. [PubMed] [Google Scholar]
- 34. Wang Y, Liang D, Spitz MR, Zhang K, Dong Q, et al. (2003) XRCC3 genetic polymorphism, smoking, and lung carcinoma risk in minority populations. Cancer 98: 1701–6. [DOI] [PubMed] [Google Scholar]
- 35. Ito H, Matsuo K, Hamajima N, Mitsudomi T, Sugiura T, et al. (2004) Gene-environment interactions between the smoking habit and polymorphisms in the DNA repair genes, APE1 Asp148Glu and XRCC1 Arg399Gln, in Japanese lung cancer risk. Carcinogenesis 25: 1395–401. [DOI] [PubMed] [Google Scholar]
- 36. Popanda O, Schattenberg T, Phong CT, Butkiewicz D, Risch A, et al. (2004) Specific combinations of DNA repair gene variants and increased risk for non-small cell lung cancer. Carcinogenesis 25: 2433–41. [DOI] [PubMed] [Google Scholar]
- 37. Liu G, Zhou W, Park S, Wang LI, Miller DP, et al. (2004) The SOD2 Val/Val genotype enhances the risk of non-small cell lung carcinoma by p53 and XRCC1 polymorphisms,. Cancer 101: 2802–8. [DOI] [PubMed] [Google Scholar]
- 38. Harms C, Salama SA, Sierra-Torres CH, Cajas-Salazar N, Au WW (2004) Polymorphisms in DNA repair genes, chromosome aberrations, and lung cancer. Environ Mol Mutagen 44: 74–82. [DOI] [PubMed] [Google Scholar]
- 39. Jacobsen NR, Raaschou-Nielsen O, Nexø B, Wallin H, Overvad K, et al. (2004) XRCC3 polymorphisms and risk of lung cancer. Cancer Lett 213: 67–72. [DOI] [PubMed] [Google Scholar]
- 40. Zhang X, Miao X, Liang G, Hao B, Wang Y, et al. (2005) Polymorphisms in DNA base excision repair genes ADPRT and XRCC1 and risk of lung cancer. Cancer Res 65: 722–6. [PubMed] [Google Scholar]
- 41. Hung RJ, Brennan P, Canzian F, Szeszenia-Dabrowska N, Zaridze D, et al. (2005) Large-scale investigation of base excision repair genetic polymorphisms and lung cancer risk in a multicenter study. J Natl Cancer Inst 97: 567–76. [DOI] [PubMed] [Google Scholar]
- 42. Vogel U, Nexo BA, Wallin H, Overvad K, Tjonneland A, et al. (2004) No association between base excision repair gene polymorphisms and risk of lung cancer. Biochem Genet 42: 453–60. [DOI] [PubMed] [Google Scholar]
- 43. Schneider J, Classen V, Bernges U, Philipp M (2005) XRCC1 polymorphism and lung cancer risk in relation to tobacco smoking. Int J Mol Med 16: 709–16. [PubMed] [Google Scholar]
- 44. Shen M, Berndt SI, Rothman N, Mumford JL, He X, et al. (2005) Polymorphisms in the DNA base excision repair genes APEX1 and XRCC1 and lung cancer risk in Xuan Wei, China. Anticancer Res 25: 537–42. [PubMed] [Google Scholar]
- 45. Chan EC, Lam SY, Fu KH, Kwong YL (2005) Polymorphisms of the GSTM1, GSTP1, MPO, XRCC1, and NQO1 genes in Chinese patients with non-small cell lung cancers: relationship with aberrant promoter methylation of the CDKN2A and RARB genes. Cancer Genet Cytogenet 162: 10–20. [DOI] [PubMed] [Google Scholar]
- 46. Li M, Yin Z, Cui Z, He Q, Zhou B (2005) Association of genetic polymorphism in DNA repair gene XRCC1 with risk of lung adenocarcinoma in nonsmoking women, Chinese J. Lung Cancer 8: 431–4. [DOI] [PubMed] [Google Scholar]
- 47. Hu Z, Ma H, Lu D, Zhou J, Chen Y, et al. (2005) A promoter polymorphism (−77T>C) of DNA repair gene XRCC1 is associated with risk of lung cancer in relation to tobacco smoking. Pharmacogenet Genomics 15: 457–63. [DOI] [PubMed] [Google Scholar]
- 48. Zienolddiny S, Campa D, Lind H, Ryberg D, Skaug V, et al. (2006) Polymorphisms of DNA repair genes and risk of nonsmall cell lung cancer. Carcinogenesis 27: 560–7. [DOI] [PubMed] [Google Scholar]
- 49. Matullo G, Dunning AM, Guarrera S, Baynes C, Polidoro S, et al. (2006) DNA repair polymorphisms and cancer risk in non-smokers in a cohort study. Carcinogenesis 27: 997–1007. [DOI] [PubMed] [Google Scholar]
- 50. Hao B, Miao X, Li Y, Zhang X, Sun T, et al. (2006) A novel T–77C polymorphism in DNA repair gene XRCC1 contributes to diminished promoter activity and increased risk of non-small cell lung cancer. Oncogene 25: 3613–20. [DOI] [PubMed] [Google Scholar]
- 51. Landi S, Gemignani F, Canzian F, Gaborieau V, Barale R, et al. (2006) DNA repair and cell cycle control genes and the risk of young-onset lung cancer. Cancer Res 66: 11062–9. [DOI] [PubMed] [Google Scholar]
- 52. Ryk C, Kumar R, Thirumaran RK, Hou SM (2006) Polymorphisms in the DNA repair genes XRCC1, APEX1, XRCC3 and NBS1, and the risk for lung cancer in never- and ever-smokers. Lung cancer 54: 285–92. [DOI] [PubMed] [Google Scholar]
- 53. De Ruyck K, Szaumkessel M, De Rudder I, Dehoorne A, Vral A, et al. (2007) Polymorphisms in base-excision repair and nucleotide-excision repair genes in relation to lung cancer risk. Mutat Res 631: 101–10. [DOI] [PubMed] [Google Scholar]
- 54. Pachouri SS, Sobti RC, Kaur P, Singh J (2007) Contrasting impact of DNA repair gene XRCC1 polymorphisms Arg399Gln and Arg194Trp on the risk of lung cancer in the north-Indian population. DNA Cell Biol 26: 186–91. [DOI] [PubMed] [Google Scholar]
- 55. Yin J, Vogel U, Ma Y, Qi R, Sun Z, et al. (2007) The DNA repair gene XRCC1 and genetic susceptibility of lung cancer in a northeastern Chinese population. Lung Cancer 56: 153–60. [DOI] [PubMed] [Google Scholar]
- 56. López-Cima MF, González-Arriaga P, García-Castro L, Pascual T, Marrón MG, et al. (2007) Polymorphisms in XPC, XPD, XRCC1, and XRCC3 DNA repair genes and lung cancer risk in a population of northern Spain,. BMC Cancer 7: 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Zhang ZL, Zhou CC, Zhang J, Tang L, Su B (2007) Relationship between polymorphisms of DNA repair gene XRCC3 and susceptibility to lung cancer. Zhonghua Jie He He Hu Xi Za Zhi 30: 936–40. [PubMed] [Google Scholar]
- 58. Improta G, Sgambato A, Bianchino G, Zupa A, Grieco V, et al. (2008) Polymorphisms of the DNA repair genes XRCC1 and XRCC3 and risk of lung and colorectal cancer: a case–control study in a Southern Italian population. Anticancer Res 28: 2941–6. [PubMed] [Google Scholar]
- 59. Li M, Yin Z, Guan P, Li X, Cui Z, et al. (2008) XRCC1 polymorphisms, cooking oil fume and lung cancer in Chinese women nonsmokers. Lung Cancer 62: 145–51. [DOI] [PubMed] [Google Scholar]
- 60. Yin J, Vogel U, Ma Y, Qi R, Wang H (2013) Association of DNA repair gene XRCC1 and lung cancer susceptibility among nonsmoking Chinese women. Cancer Genet Cytogenet 188: 26–31. [DOI] [PubMed] [Google Scholar]
- 61. Hsieh WC, Cheng YW, Lin CJ, Chou MC, Chen CY, et al. (2009) Prognostic significance of X-ray cross-complementing group 1 T–77C polymorphism in resected non-small cell lung cancer. Jpn J Clin Oncol 39: 81–5. [DOI] [PubMed] [Google Scholar]
- 62. Cote ML, Yoo W, Wenzlaff AS, Prysak GM, Santer SK, et al. (2009) Tobacco and estrogen metabolic polymorphisms and risk of non-small cell lung cancer in women. Carcinogenesis 30: 626–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Qian B, Zhang H, Zhang L, Zhou X, Yu H, et al. (2011) Association of genetic polymorphisms in DNA repair pathway genes with non-small cell lung cancer risk. Lung Cancer 73: 138–46. [DOI] [PubMed] [Google Scholar]
- 64. Tanaka Y, Maniwa Y, Bermudez VP, Doi T, Nishio W, et al. (2010) Nonsynonymous single nucleotide polymorphisms in DNA damage repair pathways and lung cancer risk. Cancer 116: 896–902. [DOI] [PubMed] [Google Scholar]
- 65. Kim IS, Lee GW, Kim DC, Kim HG, Kim S, et al. (2010) Polymorphisms and haplotypes in the XRCC1 gene and the risk of advanced non-small cell lung cancer. J Thorac Oncol 5: 1912–21. [DOI] [PubMed] [Google Scholar]
- 66. Osawa K, Miyaishi A, Uchino K, Osawa Y, Inoue N, et al. (2010) APEX1 Asp148Glu gene polymorphism is a risk factor for lung cancer in relation to smoking in Japanese. Asian Pac J Cancer Prev 11: 1181–6. [PubMed] [Google Scholar]
- 67. Huang M, Chen X, Qiu Y, Fan L, Chen J, et al. (2011) Relationship between XRCC3 gene polymorphisms and lung cancer. Wei Sheng Yan Jiu 40: 187–90. [PubMed] [Google Scholar]
- 68. Janik J, Swoboda M, Janowska B, Cies´la JM, Gackowski D, et al. (2011) 8-Oxoguanine incision activity is impaired in lung tissues of NSCLC patients with the polymorphism of OGG1 and XRCC1 genes. Mutat Res 709–710: 21–31. [DOI] [PubMed] [Google Scholar]
- 69. Li Z, Guan W, Li MX, Zhong ZY, Qian CY, et al. (2011) Genetic polymorphism of DNA base-excision repair genes (APE1, OGG1 and XRCC1) and their correlation with risk of lung cancer in a Chinese population. Arch Med Res 42: 226–34. [DOI] [PubMed] [Google Scholar]
- 70. Wang N, Wu Y, Zhou X, Wu Y (2013) Association between genetic polymorphism of metabolizing enzymes and DNA repairing enzymes and the susceptibility of lung cancer in Henan population. Wei Sheng Yan Jiu 41: 251–6. [PubMed] [Google Scholar]
- 71. Kiyohara C, Horiuchi T, Takayama K, Nakanishi Y (2012) Genetic polymorphisms involved in carcinogen metabolism and DNA repair and lung cancer risk in a Japanese population. J Thorac Oncol 7: 954–62. [DOI] [PubMed] [Google Scholar]
- 72. Sreeja L, Syamala VS, Syamala V, Hariharan S, Raveendran PB, et al. (2008) Prognostic importance of DNA repair gene polymorphisms of XRCC1 Arg399Gln and XPD Lys751Gln in lung cancer patients from India. J Cancer Res Clin Oncol 134 (6) 645–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Chang JS, Wrensch MR, Hansen HM, Sison JD, Aldrich MC, et al. (2009) Base excision repair genes and risk of lung cancer among San Francisco Bay Area Latinos and African-Americans. Carcinogenesis 30 (1) 78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Davey SG, Egger M (1997) Meta-analyses of randomized controlled trials. Lancet 350: 1182. [DOI] [PubMed] [Google Scholar]
- 75. Ioannidis JP, Boffetta P, Little J, O'Brien TR, Uitterlinden AG, et al. (2008) Assessment of cumulative evidence on genetic associations: interim guidelines. Int J Epidemiol 37: 120–32. [DOI] [PubMed] [Google Scholar]
- 76. Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. Natl Cancer Inst 22: 719–78. [PubMed] [Google Scholar]
- 77. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–88. [DOI] [PubMed] [Google Scholar]
- 78. Wang D, Lippard SJ (2005) Cellular processing of platinum anticancer drugs. Nat Rev Drug Discov 4: 307–320. [DOI] [PubMed] [Google Scholar]
- 79. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–101. [PubMed] [Google Scholar]
- 80. Egger M, Smith DG, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Kiyohara K, Takayama K, Nakanishi Y (2006) Association of genetic polymorphisms in the base excision repair pathway with lung cancer risk: a meta-analysis,. Lung Cancer 54: 267–83. [DOI] [PubMed] [Google Scholar]
- 82. Wang Y, Yang H, Li H, Li L, Wang H, et al. (2009) Association between X-ray repair cross complementing group 1 codon 399 and 194 polymorphisms and lung cancer risk: a meta-analysis. Cancer Lett 285: 134–40. [DOI] [PubMed] [Google Scholar]
- 83. Dai L, Duan F, Wang P, Song C, Wang K, et al. (2012) XRCC1 gene polymorphisms and lung cancer susceptibility: a meta-analysis of 44 case-control studies. Mol Biol Rep 39: 9535–47. [DOI] [PubMed] [Google Scholar]
- 84. Sun H, Qiao Y, Zhang X, Xu L, Jia X, et al. (2010) XRCC3 Thr241Met polymorphism with lung cancer and bladder cancer: a meta-analysis. Cancer Sci 101: 1777–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Zhan P, Wang Q, Qian Q, Yu LK (2013) XRCC3 Thr241Met gene polymorphisms and lung cancer risk: a meta-analysis. J Exp Clin Cancer Res 32 (1) 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Xu YH, Gu LP, Sun YJ, Cheng BJ, Lu S (2013) No significant association between the XRCC3 Thr241Met polymorphism and lung cancer risk: a meta-analysis. Tumour Biol [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 87. Lengauer C, Kinzler KW, Vogelstein B (1998) Genetic instabilities in human cancers. Nature 396: 643–649. [DOI] [PubMed] [Google Scholar]
- 88. Sia EA, Kokoska RJ, Dominska M, Greenwell P, Petes TD (1997) Microsatellite instability in yeast: dependence on repeat unit size and DNA mismatch repair genes. Mol Cell Biol 17: 2851–2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Aquilina G, Bignami M (2001) Mismatch repair in correction of replication errors and processing of DNA damage. J Cell Physiol 187: 145–154. [DOI] [PubMed] [Google Scholar]
- 90. Tomescu D, Kavanagh G, Ha T, Campbell H, Melton DW (2001) Nucleotide excision repair gene XPD polymorphisms and genetic predisposition to melanoma. Carcinogenesis 22: 403–408. [DOI] [PubMed] [Google Scholar]
- 91. Wang D, Lippard SJ (2005) Cellular processing of platinum anticancer drugs. Nat Rev Drug Discov 4: 307–320. [DOI] [PubMed] [Google Scholar]
- 92. Stoehlmacher J, Ghaderi V, Iobal S, Groshen S, Tsao-Wei D, et al. (2001) A polymorphism of the XRCC1 gene predicts for response to platinum based treatment in advanced colorectal cancer. Anticancer Res 21: 3075–3079. [PubMed] [Google Scholar]
- 93. De Ruyck K, Van Eijkeren M, Claes K, Morthier R, De Paepe A, et al. (2005) Radiation-induced damage to normal tissues after radiotherapy in patients treated for gynecologic tumors: association with single nucleotide polymorphisms in XRCC1, XRCC3, and OGG1 genes and in vitro chromosomal radiosensitivity in lymphocytes. Int J Radiat Oncol Biol Phys 62: 1140–1149. [DOI] [PubMed] [Google Scholar]
- 94. Sak SC, Harnden P, Johnston CF, Paul AB, Kiltie AE (2005) APE1 and XRCC1 protein expression levels predict cancer-specific survival following radical radiotherapy in bladder cancer. Clin Cancer Res 11: 6205–6211. [DOI] [PubMed] [Google Scholar]
- 95. Caldecott KW, McKeown CK, Tucker JD, Ljungquist S, Thompson LH (1994) An interaction between the mammalian DNA repair protein XRCC1 and DNA ligase III. Mol Cell Biol 14 (1) 68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews of interventions version 5.0.1. The Cochrane Collaboration, Oxford
- 97. Vineis P, Manuguerra M, Kavvoura FK, Guarrera S, Allione A, et al. (2005) A field synopsis on low-penetrance variants in DNA repair genes and cancer susceptibility. J Natl Cancer Inst 101 (1) 24–36. [DOI] [PubMed] [Google Scholar]
- 98. Liu L, Yuan P, Liu L, Wu C, Zhang X, et al. (2011) A functional −77T>C polymorphism in XRCC1 is associated with risk of breast cancer. Breast Cancer Res Treat 125 (2) 479–87. [DOI] [PubMed] [Google Scholar]
- 99. Liu L, Yuan P, Wu C, Zhang X, Wang F, et al. (2011) Assessment of XPD Lys751Gln and XRCC1 T-77C polymorphisms in advanced non-small-cell lung cancer patients treated with platinum-based chemotherapy. Lung Cancer 73 (1) 110–5. [DOI] [PubMed] [Google Scholar]
- 100. Liu L, Wu J, Zhong R, Wu C, Zou L, et al. (2012) Multi-loci analysis reveals the importance of genetic variations in sensitivity of platinum-based chemotherapy in non-small-cell lung cancer. Mol Carcinog doi: 10.1002/mc.21942 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA 2009 checklist.
(DOC)
Table S1, Genotypes, p values and subset of cases of XRCC1 Arg399Gln polymorphism included in the meta-analysis. Table S2, Genotypes, p values and subset of cases of XRCC1 Arg194Trp (rs1799782) polymorphism included in the meta-analysis. Table S3, Genotypes, P values and subset of cases of XRCC1 Arg280His (rs25489) polymorphism included in the meta-analysis. Table S4, Genotypes, P values and subset of cases of XRCC1 −77T>C (rs3213245) polymorphism included in the meta-analysis. Table S5, Genotypes, P values and subset of cases of XRCC3 T241M (rs861539) polymorphism included in the meta-analysis.
(DOC)