Abstract
Objectives
To examine the effects of age and depressive symptom severity on changes in positive affect among older adults randomly assigned to a Mindfulness-Based Stress Reduction (MBSR) program or a waitlist control group. Drawing from the Motivational Theory of Life-Span Development, we hypothesized that lower levels of depressive symptom severity and older age would be associated with greater positive affect in response to the MBSR intervention.
Methods
Data were collected from a sample of community-dwelling English-speaking adults (n = 200) aged ≥ 65, randomly assigned to an 8-week MBSR program or a Waitlist Control group. Our main outcome variable was a 5-item measure of positive affect, which was measured at study entry as well as 8 weeks and 6-months later.
Results
At 6-month follow-up, we observed group by baseline depressive symptom severity (β = −.17, p = .02) and group by baseline depressive symptom severity by age (β = −.14, p = .05) interactions. Among MBSR participants, greater baseline depressive symptom severity was also associated with less improvement in positive affect at the 6-month follow-up (β = −.30, p = .003). Findings were qualified by a significant depressive symptom severity by age interaction (β = −.25, p = .01), such that MBSR participants who were 70 and over with lower baseline depressive symptom severity had the greatest improvement in positive affect at the 6-month follow-up.
Conclusion
MBSR improves positive affect for older adults with lower depressive symptom severity, perhaps because it capitalizes on naturalistic changes in control strategies.
Keywords: Mindfulness-based stress reduction, age, depressive symptom severity, positive affect
Introduction
A pivotal developmental task in older adulthood is the cultivation of emotion regulation strategies to influence the experience and expression of emotions (Gross & Barrett, 2011). Older adulthood is often accompanied by declining health, social losses, and other psychological stressors. However, contrary to conventional wisdom, these stressors are often met with emotional resilience (Albrecht & Devlieger, 1999; Gluth, Ebner, & Schmiedek, 2010). Although well-being normatively increases with age (Scheibe & Carstensen, 2009), improved emotion regulation in response to age-related stressors is not universal. Moreover, advanced older age may compromise the skills needed to regulate emotion (Teachman, 2006). Our goal is to apply the Motivational Theory of Life-Span Development (Heckhausen, Wrosch, & Schulz, 2010) to research on Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1990) with older adults. Within that theoretical framework, we will discuss the effects of MBSR on the optimization of emotion regulation skills in older adulthood and frame hypotheses about the key variables associated with MBSR-induced improvements in positive affect (Anderson, Lau, Segal, & Bishop, 2007; Davidson et al., 2003).
The Motivational Theory of Life-Span Development frames development as a repeated cycle of “selecting, pursuing, and adapting developmental and personal goals to reflect changes in life-course opportunities, activating behavioral and motivational strategies of goal engagement, disengaging from goals that have become futile and too costly, and replacing them with more appropriate goals” (Heckhausen et al., 2010, p. 32). Typically, the human motivational system seeks to maximize primary control, which is understood as the ability to master the environment to achieve desired goals (Heckhausen & Schulz, 1999). Examples of primary control include gaining an education, working, or maintaining relationships. Yet, when environmental mastery is impractical, people rely upon secondary control strategies, or changing oneself to accommodate to the environment. For example, people rely upon emotion regulation strategies to adjust to situations they cannot change. From the perspective of the Motivational Theory of Lifespan Development, older adults are motivated to maintain positive affect, which acts as a secondary control strategy. Another secondary control strategy is goal disengagement, which is the act of devaluing a chosen goal. Studies have demonstrated that disengagement from original goals and replacement with alternative goals are associated with increases in positive affect among older adults (Duke, Leventhal, Brownlee, & Leventhal, 2002; Wrosch, Scheier, Miller, Schulz, & Carver, 2003). Secondary control strategies are functional in that they provide emotional benefits in uncontrollable circumstances and also help empower people to engage in further attempts at primary control (McQuillen, Licht, & Licht, 2003; Poulin & Heckhausen, 2007). Given that one’s capacity for primary control decreases with age (Lachman & Firth, 2004; Wrosch & Hechhausen, 1999), interventions that increase secondary control strategies are particularly important for promoting successful emotional aging.
In this vein, MBSR is a therapeutic intervention that teaches participants to increase mindfulness, or nonjudgmental awareness, of their momentary affective, cognitive, and physical experiences, using stress-reduction techniques such as meditation or yoga. MBSR improves emotion regulation by increasing attention, awareness and acceptance of emotions as they arise at any given moment (Goldin & Gross, 2010; Hölzel et al., 2011; Jensen, Vangkilde, Frokjaer, & Hasselbalch, 2012; Kilpatrick et al., 2011; Rubia, 2009). Attentional control is the process of sustaining attention on a chosen object or experience (Hölzel et al., 2011). The act of maintaining focus increases attentional regulation. In line with the Motivational Theory of Life-Span Development, an older adult should be motivated to use attentional control to selectively pay attention to positive stimuli, which is a type of emotion-regulating secondary control strategy. MBSR thereby contributes directly to the development of secondary control strategies by reducing emotional reactivity, and in turn reducing emotional obstacles to primary control. MBSR has been used to improve emotional well-being in healthy participants, psychiatric patients, and patients with a variety of health conditions, including cancer and chronic diseases (Carmody & Baer, 2008; Dobkin & Zhao, 2011; Hofmann, Sawyer, Witt, & Oh, 2010).
Given age-related increases in motivational processes involved in maintaining positive affect via attentional control (Charles, 2010; Scheibe & Carstensen, 2010), older adults may be particularly well-prepared to practice MBSR. However, MBSR research involving older adults has been minimal (Chapman et al., 2011; Gallegos et al., in press; Morone & Greco, 2007; Moynihan et al., in press) and has not been framed within a broader theory of emotional aging, such as the Motivational Theory of Life-Span Development. This research gap is critical because the Motivational Theory of Life-Span Development can be used to guide hypotheses about MBSR interventions with older adults and ultimately improve interventions in emotional aging research.
In the present study, our primary aim was to examine the effect of MBSR on positive affect in a community sample of older adults participating in the MBSR intervention arm of a randomized controlled trial (RCT). In any intervention, it is likely that some individuals will experience greater benefits than others (Gabler et al., 2009; Kravitz, Duan, & Braslow, 2004). Therefore, we also sought to identify potential moderators of improved affectivity. Our moderation analyses are premised on the assumption that individuals differ in the rate and degree to which they are able to transition from primary to secondary control strategies. Primary control capacity declines with age (Heckhausen et al., 2010) and depressive symptoms have been described as a central factor undermining efforts to improve control strategies in older adulthood (Wrosch, Schulz, & Heckhausen, 2002, 2004). Potential mechanisms include depression-related changes in motivation, behavior, and biologic processes, such as a decrease in hippocampal neurogenesis and loss of cellular plasticity (Kempermann & Kronenberg, 2003; Schulz, Martire, Beach, & Scheier, 2000; Wrosch, Bauer, & Scheier, 2005). Hippocampal neurogenesis also decreases with increasing age (Kempermann & Kronenberg, 2003). We predicted that participation in MBSR would increase positive affect and, based on the Motivational Theory of Life-Span Development, we hypothesized that age and baseline depression severity would moderate heterogeneity effects in treatment outcomes. Based on the findings that depression undermines the efforts to improve control strategies in older adulthood (Wrosch et al., 2002, 2004), we hypothesized that greater depressive symptom severity would compromise MBSR’s capacity to boost positive affect. Because the use of secondary control strategies increases with age, we further hypothesized that increased age and lower depressive symptom severity would be associated with greater positive affect in response to an MBSR intervention.
Methods
Participants and Procedures
A detailed account of study procedures is available in Moynihan et al. (in press). Briefly, participants were English-speaking older adults recruited from a community sample through the use of newspaper advertisements and flyers posted at primary care offices. One of three masters-level research assistants administered all study measures. Participants were excluded if they had a potential cognitive impairment (Mini Mental Status Examination score ≤ 24; Folstein, Folstein, & McHugh, 1975) or uncorrected sensory impairment. Participants were also excluded if the Structured Clinical Interview for DSM-IV (SCID) revealed the presence of major depression with psychotic features, psychosis, lifetime history of schizophrenia, bipolar disorder, organic brain syndrome, mental retardation, or alcohol/substance abuse within the past year. A total of eight potential participants met exclusion criteria, one of whom was mistakenly randomized to the MBSR condition. That participant was excluded before beginning treatment. Participants meeting inclusion criteria were randomized to an 8-week MBSR intervention or waitlist control. Participant characteristics are reported in Table 1. Randomization was conducted using an Excel spreadsheet function for generating random numbers. This function was used to determine the treatment arm for each subject. Analyses were conducted to discern the adequacy of the randomization. The participants completed study measures at study entry, at 8 weeks (end of treatment), and at a follow-up assessment 6-months after the end of treatment.
Table 1.
Sample characteristics.
| MBSR n = 100 |
Waitlist Control n = 100 |
|
|---|---|---|
| Variable | M (SD) or % | M (SD) or % |
| Demographics | ||
| Age | 72.08 (6.74) | 73.45 (6.71) |
| Gender: % Female | 62% | 62% |
| Education: % attending College | 86% | 90% |
| Health Conditions | 2.16 (1.11) | 2.10 (1.54) |
| Baseline Depression Severity | ||
| Depressive Symptom Severity Composite | 0.21 (0.88) | −0.21 (1.07) |
| PANAS Positive Affect | ||
| Baseline | 34.36 (7.47) | 35.05 (7.07) |
| Treatment Completion | 35.31 (7.50) | 35.03 (7.02) |
| Follow-up, 6 months Post-treatment | 34.63 (8.07) | 34.36 (7.24) |
Note. N = 200. Depressive Symptom Severity Composite = the standardized summated composite of the CESD-R and HAM-D; PANAS = Positive and Negative Affect Schedule.
MSBR Intervention
The 8-week MBSR program consisted of nine group-based (15-20 member) sessions held at a University-affiliated health center in Rochester, N.Y., USA. Seven of these sessions were 2 hours in duration and one, at mid-treatment, was 7-hours. MBSR emphasizes the development of four mindfulness practices: yoga (mindful movement similar to Hatha yoga), sitting meditation (mindful awareness of one’s experience while sitting), informal meditation (meditation while walking or engaging in other activities), and body scan (serial attention to the sensations of different regions of the body). These practices can be conceptualized as secondary control strategies that are designed to foster a calm, non-judgmental awareness of one’s sensations and feelings. For the purposes of the present intervention, these activities were adapted on an individual basis to accommodate the unique mobility, sensory, and cognitive limitations of participants (e.g., sitting yoga for those in a wheelchair).
Measures
Depressive Symptom Severity
At baseline, participants were administered the Center for Epidemiologic Studies Depression Scale, Revised (CESD-R; Eaton, Smith, Ybarra, Muntaner, & Tien, 2004) and the Hamilton Rating Scale for Depression (HAM-D; Hamilton, 1960). The CESD-R (alpha = .89) is a 20-item self-report measure of depression symptoms. Participants rate the frequency with which they have experienced symptoms (e.g., I lost interest in my usual activities) during the past two weeks, using a scale from 0 (not at all or less than one day) to 4 (nearly every day for two weeks). The CESD-R is an updated version of the CES-D, which, among multiple aspects of the revision, eliminated the items reflecting positive affect to optimize its psychometric properties (Van Dam & Earleywine, 2011). The HAM-D (alpha = .73) is a 21-item clinician rating scale of depression severity. The interviewer rates the severity of symptoms (e.g., agitation), using rating scales customized by symptom, such as 0 (absent) to 4 (hand wringing, nail biting, hair-pulling, biting of lips). The reliability and validity of the CESD-R and HAM-D are well-established (Eaton et al., 2004; Shafer, 2006). These scales assess complementary but overlapping aspects of depression (r = .56, p < .001), with the HAM-D tapping symptoms that are broad and observable, and the CESD-R those that are more narrow and subjective. Accordingly, as in prior research (Eid & Diener, 2006), we standardized scores on each scale and added them to yield a composite indicator of depression symptom severity (alpha = .89).
Positive Affect
The Positive Affect (PA) scale of the Positive and Negative Affect Schedule (PANAS; Watson, Clark & Tellegen, 1988) yields a total score (alpha = .87) and three domain scores: joy, interest, and activation. In completing the survey, participants rated emotion words, such as “excited,” using a scale from 1 (very slightly or not at all) to 5 (extremely).
Covariates
In all analyses, we controlled for participants’ gender, education level (no college versus some college or greater), and the number of current health conditions on a checklist of 15 health conditions adapted from the MIDUS epidemiologic checklist (Goodwin & Friedman, 2006).
Statistical analyses
Using t-tests and ANOVA, we first compared MBSR and the waitlist control groups on baseline variables, and examined changes in outcomes over time. Next, we explored the moderating effects of age and baseline depression symptom severity. Specifically, we used regression to examine whether age, depressive symptom severity, and their interaction were associated with changes in positive affect over time. In regression analyses, we examined two outcomes: changes in positive affect from baseline to treatment completion and changes in positive affect from baseline to 6-month follow-up. Residualized change scores (e.g., positive affect at treatment completion, controlling for baseline positive affect) were used to compute the four outcome variables for regression analyses. Regression analyses were conducted while including all participants; however, group assignment (MBSR vs. control) significantly interacted with baseline depressive symptom severity and age to explain changes in affect, therefore subsequent analyses examined the effects of age, baseline depressive symptom severity, and their interaction separately by group. To explore and illustrate age moderation, we compared subjects 70 or older and those younger than 70. Acknowledging that any cut-off is arbitrary, this cut-point is theoretically meaningful (Rothermund & Brandtstädter, 2003). All analyses controlled for gender, education level, and number of health conditions.
Results
Participant demographic characteristics are shown in Table 1. At baseline, no significant group differences were found in gender, age, education level, or positive affect, although the MBSR group had greater baseline depressive symptom severity (Depressive Symptom Severity Composite: d = .43, t(198) = 3.10, p = .002) than the Waitlist Control group. CESD-R scores for the MBSR group ranged from 0-32 (M = 5.99, SD = 6.81) and the WLC group ranged from 0-41 (M = 4.06, SD = 6.26). The MBSR group HAM-D scores ranged from 0-28 (M = 7.79, SD = 5.10) and the WLC group scores ranged from 0-19 (M = 5.61, SD = 3.94). The mean scores for both groups on the two depression scales indicated no or mild depression, though some scores were in the severe depression range (Eaton et al., 2004; Hamilton, 1960). Using ANCOVA, the time-related changes in positive affect were non-significant, F(2,391) = 1.02, p = .36, and did not differ by group, F(2,391) = 0.89, p = .42. At the first follow-up, 54% of participants in the MBSR group experienced improved positive affect (average d = 0.12), compared to 46% in the waitlist control group (average d = 0.00).
Impact of Age and Baseline Depressive Symptom Severity
In analyses of positive affect outcomes at the 6-month follow-up, we found that group by baseline depressive symptom severity (β = −.17, p = .02) and group by baseline depressive symptom severity by age (β = −.14, p = .05) interactions were significant. Therefore, analyses examining the contributions of age and baseline depressive symptom severity to changes in positive affect were conducted separately for the MBSR and waitlist control groups.
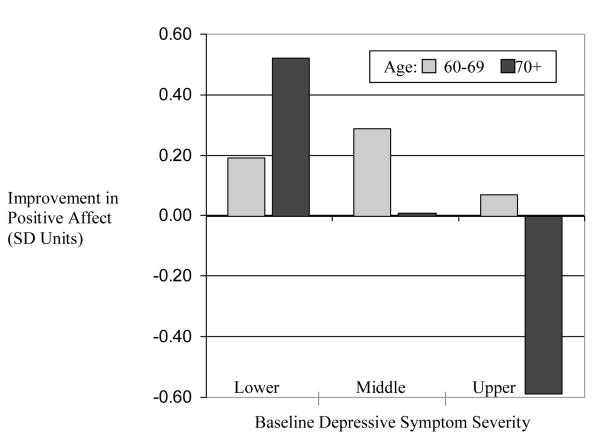
Baseline depressive symptom severity and age were associated with MBSR-related improvements in positive affect (see Table 2 and Figure 1). Specifically, within the MBSR group, participants who had greater baseline depressive symptom severity experienced less improvement in positive affect at treatment completion (β = −.21, p = .02); effects for age (β = .05, p = .66) and the depressive symptom severity by age interaction (β = −.03, p = .75) were non-significant. Among MBSR participants, greater baseline depressive symptom severity was also associated with less improvement in positive affect at the 6-month follow-up (β = −.30, p = .003); no main effect of age was found (β = −.05, p = .64), but findings were qualified by a significant depressive symptom severity by age interaction (β = −.25, p = .01). As shown in Figure 1, MBSR participants who were 70 and over with low baseline depressive symptom severity had the greatest improvement in positive affect at the 6-month follow-up, whereas those 70 and over with higher depressive symptom severity had the poorest outcomes. In particular, MBSR participants 70 and over with greater baseline depressive symptom severity showed less improvement (β = −.42, p = .002) than those under 70 (β = −.06, p = .69). Sensitivity analyses revealed that the influence of baseline depressive symptom severity on changes in positive affect (see Table 2) was similar across each of the three domains of positive affect (Z = .20, p = .84). The effects of age, baseline depressive symptom severity, or their interaction on changes in positive affect in the Waitlist Control group were non-significant.
Table 2.
Correlations between Baseline Depression Severity and Improvement in Positive Affect
| MBSR Group n = 100 |
Waitlist Control Group n = 100 |
|||
|---|---|---|---|---|
| Positive Affect | Completion | Follow-Up | Completion | Follow-up |
| Joy | −.21* | −.29** | −.01 | .01 |
| Interest | −.23* | −.29** | −.07 | −.07 |
| Activation | −.16 | −.30** | −.01 | .16 |
|
| ||||
| Total Positive | −.21* | −.29** | −.01 | .08 |
Note. Baseline depression symptom severity was measures as the standardized summated composite of scores on the CESD-R and the HAMD. Positive Affect was measured using the PANAS. Correlation values control for gender, education level, and number of health conditions.
p < .05
p < .01
Figure 1.
MBSR-related improvement in positive affect at the 6-month follow-up was greatest for participants 70 years and older with lower baseline depressive symptom severity. Depression severity is based on a composite score of the CESD-R* and HAM-D.** The composite score was divided into thirds to demonstrate lower, middle, and upper ranges of depression severity in this sample. Multivariate analyses yielded a significant main effect of baseline depression severity and a significant depression by age interaction. n = 100. * CESD-R scores for the MBSR group: lower (n = 32, M = 1.00, SD = 1.57), middle (n = 34, M = 4.41, SD = 3.29), and upper (n = 34, M = 12.26, SD = 7.67). ** HAM-D scores for the MBSR group: lower (n = 32, M = 2.66, SD = 1.68), middle (n = 34, M = 7.53, SD = 2.45), and upper (n = 34, M = 12.88, SD = 4.13).
Emotional Benefits of Mindfulness-Based Stress Reduction in Older Adults: The Moderating Roles of Age and Depressive Symptom Severity
Discussion
Our findings support the hypothesis that increased age and lower depressive symptom severity would be associated with greater positive affect in response to MBSR. Specifically, MBSR was most effective in improving positive affect for participants aged 70 and older with lower baseline depressive symptom severity on a composite score of the CESD-R and HAM-D; in contrast, those with higher depressive symptom severity reported less improvement in positive affect. In the waitlist control group, age and depressive symptom severity were not associated with affect changes.
To our knowledge, the Motivational Theory of Life-Span Development has not been previously applied to research on the effects of MBSR. We believe that it serves as a useful framework to explain the potential advantages of MBSR for older adults, as mindfulness practice may capitalize on and potentially enhance secondary control strategies normatively used by older adults. The finding that participation in MBSR increased positive affect among older adults with lower baseline depressive symptom severity suggests that MBSR may enhance secondary control strategies used to regulate emotion, but only when depressive symptom severity does not undermine improvement in control strategies. The exposure element of MBSR may have been particularly problematic for participants with depressive symptoms. MBSR instructs participants to allow thoughts, feelings, and sensations into conscious awareness, and to practice responding with acceptance. This type of exposure is intended to lead to reappraisal, which is the process of reinterpreting the meaning of a stimulus to change one’s emotional response to it (Hölzel et al., 2011). Perhaps individuals with depressive symptoms are unable to do so because of rumination and hopelessness.
The inferior improvement in positive affect for adults age 70 and older with greater depressive symptom severity should be understood in the context of what is known about the effect of aging and depression on positive affect. Although community studies suggest that positive affect is stable across the lifespan, there are definite declines in older age (Charles, Reynolds, & Gatz, 2001). Further, deficits in positive affect are frequently observed in depression, particularly among older adults (Fiske, Wetherell, & Gatz, 2009; Gallo, Anthony, & Muthen, 1994; Gatz & Hurwicz, 1990). In combination, older age and greater depressive symptom severity could explain why we did not observe MBSR-induced boosts in positive affect in older adults with more depressive symptoms. It has been argued that the small effect sizes in prior studies of the effects of mindfulness treatments on depression could be due to floor effects; participants were not particularly depressed at study entry, leaving little room to observe an effect (Bohlmeijer, Prenger, Taal, & Cuijpers, 2010; Nyklíček, van Son, & Pouwer, 2010). Recognizing that this study focused on positive affect, not depression, our data cast doubt on this hypothesis. Older, more depressed participants derived less benefit from treatment.
Our findings point to the need to consider the clinical implications of using MBSR with older adults who have depressive symptoms. As people age, the ability to disengage from unattainable goals and reengage in alternative, attainable goals contributes to the maintenance of well-being in the face of inevitable ageing related losses (Wahl, Becker, Burmedi, & Schilling 2004; Wrosch, Miller, Scheier, & De Pontet, 2007). Teaching mindfulness to older adults with depressive symptomatology warrants greater emphasis on non-striving and acceptance of limitations to encourage the goal-disengagement process and facilitate re-engagement with alternate goals. The concept of goal-disengagement aligns with the mindfulness practice of non-striving through acceptance. The MBSR instructor must emphasize that disengaging from an unattainable goal is not the same as passively giving up, nor is it a reflection of personal inadequacy (Engel, 1967). Rather, disengagement involves actively seeking an alternative opportunity to maximize control and consider other goal pursuits, which serves to protect the self and its motivational resources (Heckhausen et al. 2010). The clinician may also consider Mindfulness-Based Cognitive Therapy (MBCT) for depression, an intervention that is designed to prevent relapse of depression using meditative practices and cognitive control strategies to defuse depressogenic thinking. Geschwind at al. (2011) found that MBCT increased momentary experiences of positive emotions in adults aged ≥ 65 with depression. Future research should study the role of goal disengagement and cognitive therapy on positive emotions in older adults with depressive sympotomatology.
Several study limitation should be noted. First, the sample was limited in ethnic diversity, and therefore generalizing to non-Caucasian populations should be done with caution. Randomization failure was also a limitation of the study as the MBSR group had slightly greater baseline depressive symptom severity than the WLC. The strengths of this study include a multi-method assessment of depression (self-report and observer ratings), a reasonably large sample size for an RCT of a psychosocial treatment for older adults, and the examination of a novel, theoretically-important question.
Conclusion
This study demonstrates the beneficial effects of MBSR on positive affect among older adults with lower baseline depressive symptom severity. MBSR is a promising intervention for older adults, perhaps because it capitalizes on naturalistic changes in control strategies, particularly the transition from primary to secondary control. This hypothesis could be tested more directly in future research. The use of MBSR with older adults experiencing depressive symptoms also warrants more careful examination.
Acknowledgements
Dr. Gallegos was supported by the Program of Research and Innovation in Disparities Education (PRIDE), MHREG for Research in Ethnically Diverse Communities R25MH074898 (Duberstein, PI). Dr. Hoerger was supported by T32MH018911. Study funding came from R01AG025474 (Moynihan, PI) and R24AG031089 (Moynihan, PI).
References
- Albrecht GL, Devlieger PJ. The disability paradox: High quality of life against all odds. Social Science & Medicine. 1999;49:977–988. doi: 10.1016/s0277-9536(98)00411-0. doi:10.1016/S0277-9536(98)00411-0. [DOI] [PubMed] [Google Scholar]
- Anderson ND, Lau MA, Segal ZV, Bishop SR. Mindfulness-based stress reduction and attentional control. Clinical Psychology & Psychotherapy. 2007;14:449–463. doi:10.1002/cpp.544. [Google Scholar]
- Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: A meta-analysis. Journal of Psychosomatic Research. 2010;68:539–544. doi: 10.1016/j.jpsychores.2009.10.005. doi:10.1016/j.jpsychores.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. doi:10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Chapman BP, van Wijngaarden E, Seplaki CL, Talbot N, Duberstein P, Moynihan J. Openness and conscientiousness predict 34-week patterns of interleukin-6 in older persons. Brain, Behavior, and Immunity. 2011;25:667–673. doi: 10.1016/j.bbi.2011.01.003. doi:10.1016/j.bbi.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST. Strength and vulnerability integration: A model of emotional well-being across adulthood. Psychological Bulletin. 2010;136:1068–1091. doi: 10.1037/a0021232. doi:10.1037/a0021232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST, Reynolds CA, Gatz M. Age-related differences and change in positive and negative affect over 23 years. Journal of Personality and Social Psychology. 2001;80:136–151. doi:10.1037/0022-3514.80.1.136. [PubMed] [Google Scholar]
- Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, Sheridan JF. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003;65:564–570. doi: 10.1097/01.psy.0000077505.67574.e3. doi:10.1097/01.PSY.0000077505.67574.E3. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Zhao Q. Increased mindfulness – The active component of the mindfulness-based stress reduction program? Complementary Therapies in Clinical Practice. 2011;17:22–27. doi: 10.1016/j.ctcp.2010.03.002. doi:10.1016/j.ctcp.2010.03.002. [DOI] [PubMed] [Google Scholar]
- Duke J, Leventhal H, Brownlee S, Leventhal EA. Giving up and replacing activities in response to illness. Journal of Gerontology Series B: Psychological Sciences and Social Sciences. 2002;57:P367–P376. doi: 10.1093/geronb/57.4.p367. doi:10.1093/geronb/57.4.P367. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A. Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESD-R) In: Maruish ME, editor. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment (3rd Ed.), Volume 3: Instruments for Adults. Lawrence Erlbaum; Mahwah, NJ: 2004. pp. 363–377. [Google Scholar]
- Eid ME, Diener EE. Handbook of multimethod measurement in psychology. American Psychological Association; Washington, DC: 2006. [Google Scholar]
- Engel GL. A psychological setting of somatic disease: The ‘giving up-given up’ complex. Proceedings of the Royal Society of Medicine; 1967. pp. 553–555. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1901860/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annual Review of Clinical Psychology. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. doi:10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. doi:10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gabler NB, Duan N, Liao D, Elmore JG, Ganiats TG, Kravitz RL. Dealing with heterogeneity of treatment effects: Is the literature up to the challenge? Trials. 2009;10:43–55. doi: 10.1186/1745-6215-10-43. doi:10.1186/1745-6215-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallegos, Hoerger AM, Talbot M, L N, Krasner MS, Knight JM, Moynihan JA, Duberstein PR. Toward identifying the effects of the specific components of mindfulness-based stress reduction on biologic and emotional outcomes among older adults. The Journal of Alternative and Complementary Medicine. doi: 10.1089/acm.2012.0028. (in press) doi:10.1089/acm.2012.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo JJ, Anthony JC, Muthen BO. Age differences in the symptoms of depression: A latent trait analysis. Journal of Gerontology. 1994;49:P251–P264. doi: 10.1093/geronj/49.6.p251. doi:10.1093/geronj/49.6.P251. [DOI] [PubMed] [Google Scholar]
- Gatz M, Hurwicz ML. Are old people more depressed? Cross-sectional data on Center for Epidemiological Studies Depression Scale factors. Psychology and Aging. 1990;5:284–290. doi: 10.1037//0882-7974.5.2.284. doi:10.1037/0882-7974.5.2.284. [DOI] [PubMed] [Google Scholar]
- Geschwind N, Peeters F, Drukker M, van Os J, Wichers M. Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2011;79:618–628. doi: 10.1037/a0024595. doi:10.1037/a0024595. [DOI] [PubMed] [Google Scholar]
- Gluth S, Ebner NC, Schmiedek F. Attitudes toward younger and older adults: The German aging semantic differential. International Journal of Behavioral Development. 2010;34:147–158. doi:10.1177/0165025409350947. [Google Scholar]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2009;10:83–91. doi: 10.1037/a0018441. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ, Barrett LF. Emotion generation and emotion regulation: One or two depends on your point of view. Emotion Review. 2011;3:8–16. doi: 10.1177/1754073910380974. doi:10.1177/1754073910380974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. doi:10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckhausen J, Schulz R. The primacy of primary control is a human universal: A reply to Gould’s critique of the life-span theory of control. Psychological Review. 1999;106:605–609. doi: 10.1037/0033-295x.106.3.605. doi:10.1037/0033-295X.106.3.605. [DOI] [PubMed] [Google Scholar]
- Heckhausen J, Wrosch C, Schulz R. A motivational theory of life-span development. Psychological Review. 2010;117:32–60. doi: 10.1037/a0017668. doi:10.1037/a0017668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169–183. doi: 10.1037/a0018555. doi:10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6:537–559. doi: 10.1177/1745691611419671. doi:10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Jensen CG, Vangkilde S, Frokjaer V, Hasselbalch SG. Mindfulness training affects attention - or is it attentional effort? Journal of Experimental Psychology: General. 2012;141:106–123. doi: 10.1037/a0024931. doi: 10.1037/a0024931. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Dell; New York, NY: 1990. [Google Scholar]
- Kempermann G, Kronenberg G. Depressed new Neurons? – Adult hippocampal neurogenesis and a cellular plasticity hypothesis of major depression. Biological Psychiatry. 2003;54:499–503. doi: 10.1016/s0006-3223(03)00319-6. doi: 10.1016/S0006-3223(03)00319-6. [DOI] [PubMed] [Google Scholar]
- Kilpatrick LA, Suyenobu BY, Smith SR, Bueller JA, Goodman T, Creswell JD, Naliboff BD. Impact of mindfulness-based stress reduction training on intrinsic brain connectivity. NeuroImage. 2011;56:290–298. doi: 10.1016/j.neuroimage.2011.02.034. doi:10.1016/j.neuroimage.2011.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravitz RL, Duan N, Braslow J. Evidence - Based Medicine, Heterogeneity of Treatment Effects, and the Trouble with Averages. Milbank Quarterly. 2004;82:661–687. doi: 10.1111/j.0887-378X.2004.00327.x. doi:10.1111/j.0887-378X.2004.00327.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman ME, Firth KM. The adaptive value of feeling in control during midlife. In: Brim OG, Ryff CD, Kessler R, editors. How healthy are we? A national study of well-being at midlife. University of Chicago Press; Chicago, IL: 2004. pp. 320–349. [Google Scholar]
- McQuillen AD, Licht MH, Licht BG. Contributions of disease severity and perceptions of primary and secondary control to the prediction of psychosocial adjustment to Parkinson’s disease. Health Psychology. 2003;22:504–512. doi: 10.1037/0278-6133.22.5.504. doi:10.1037/0278-6133.22.5.504. [DOI] [PubMed] [Google Scholar]
- Morone NE, Greco CM. Mind-body interventions for chronic pain in older adults: A structured review. Pain Medicine. 2007;8:359–375. doi: 10.1111/j.1526-4637.2007.00312.x. doi:10.1111/j.1526-4637.2007.00312.x. [DOI] [PubMed] [Google Scholar]
- Moynihan JA, Chapman BP, Klorman R, Krasner MS, Duberstein PR, Brown KW, Talbot NL. Mindfulness-based stress reduction for older adults: Effects on executive function, frontal alpha asymmetry and immune function. Neuropsychobiology. doi: 10.1159/000350949. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyklíček I, van Son J, Pouwer F. Two recently published meta-analyses on the effectiveness of mindfulness-based interventions: What should the reader make of it? Journal of Psychosomatic Research. 2010;69:613–614. doi: 10.1016/j.jpsychores.2010.09.004. doi:10.1016/j.jpsychores.2010.09.004. [DOI] [PubMed] [Google Scholar]
- Poulin MJ, Heckhausen J. Stressful events compromise goal striving during a major life transition. Motivation and Emotion. 2007;31:300–311. doi:10.1007/s11031-007-9077-6. [Google Scholar]
- Rothermund K, Brandstädter J. Coping with deficits and losses in later life: From compensatory action to accommodation. Psychology and Aging. 2003;18:896–905. doi: 10.1037/0882-7974.18.4.896. doi:10.1037/0882-7974.18.4.896. [DOI] [PubMed] [Google Scholar]
- Rubia K. The neurobiology of meditation and its clinical effectiveness in psychiatric disorders. Biological Psychology. 2009;82(1):1–11. doi: 10.1016/j.biopsycho.2009.04.003. doi:10.1016/j.biopsycho.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Scheibe S, Carstensen LL. Emotional aging: Recent findings and future trends. Journals of Geronotology Series B: Psychological Sciences and Social Sciences. 2009;65B:135–144. doi: 10.1093/geronb/gbp132. doi:10.1093/geronb/gbp132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Martire LM, Beach SR, Scheier MF. Depression and mortality in the elderly. Current Directions in Psychological Science. 2000;9:204–208. doi:10.1111/1467-8721.00095. [Google Scholar]
- Shafer AB. Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton, and Zung. Journal of Clinical Psychology. 2006;62:123–146. doi: 10.1002/jclp.20213. doi:10.1002/jclp.20213. [DOI] [PubMed] [Google Scholar]
- Teachman BA. Aging and negative affect: The rise and fall and rise of anxiety and depression symptoms. Psychology and Aging. 2006;21:201–207. doi: 10.1037/0882-7974.21.1.201. doi:10.1037/0882-7974.21.1.201. [DOI] [PubMed] [Google Scholar]
- Van Dam NT, Earleywine M. Validation of the Center for Epidemiologic Studies Depression Scale – Revised (CESD-R): Pragmatic depression assessment in the general population. Psychiatry Research. 2011;186:128–132. doi: 10.1016/j.psychres.2010.08.018. doi:10.1016/j.psychres.2010.08.018. [DOI] [PubMed] [Google Scholar]
- Wahl HW, Becker S, Burmedi D, Schilling O. The role of primary and secondary control in adaptation to age-related vision loss: A study of older adults with macular degeneration. Psychology and Aging. 2004;19:235–239. doi: 10.1037/0882-7974.19.1.235. doi:10.1037/0882-7974.19.1.235. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measure of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. doi:10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Bauer I, Scheier MF. Regret and quality of life across the adult life span: The influence of disengagement and available future goals. Psychology and Aging. 2005;20:657–670. doi: 10.1037/0882-7974.20.4.657. doi:10.1037/0882-7974.20.4.657. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Heckhausen J. Control processes before and after passing a developmental deadline: Activation and deactivation of intimate relationship goals. Journal of Personality and Social Psychology. 1999;77:415–427. doi:10.1037/0022-3514.77.2.415. [Google Scholar]
- Wrosch C, Miller GE, Scheier MF, De Pontet SB. Giving up on unattainable goals: Benefits for health? Personality and Social Psychology Bulletin. 2007;33:251–265. doi: 10.1177/0146167206294905. doi:10.1177/0146167206294905. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Scheier MF, Miller GE, Schulz R, Carver CS. Adaptive self-regulation of unattainable goals: Goal disengagement, goal reengagement, and subjective well-being. Personality and Social Psychology Bulletin. 2003;29:1494–1508. doi: 10.1177/0146167203256921. doi:10.1177/0146167203256921. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Schulz R, Heckhausen J. Health stresses and depressive symptomatology in the elderly: The importance of health engagement control strategies. Health Psychology. 2002;21:340–348. doi: 10.1037//0278-6133.21.4.340. doi:10.1037/0278-6133.21.4.340. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Schulz R, Heckhausen J. Health stresses and depressive symptomatology in the elderly: A control-process approach. Current Directions in Psychological Science. 2004;13:17–20. doi:10.1111/j.0963-7214.2004.01301005.x. [Google Scholar]