Abstract
MicroRNAs (miRNAs) are a class of small noncoding RNA which exert post-transcriptional gene regulation activity by targeting messenger RNAs. miRNAs have been found to be involved in various fundamental biological processes and deregulation of miRNAs is known to result in pathological conditions. In this review, we provide an overview of recent discoveries on the role played by this class of molecules in lung development and in pulmonary diseases, such as asthma, cystic fibrosis, chronic obstructive pulmonary disease, and pulmonary artery hypertension. Considering the relevant role of these miRNAs under physiological and pathological conditions, they represent new clinical targets as well as diagnostic and prognostic tools. Therefore, this review pays special attention to recent advances and possible future directions for the use of miRNAs for clinical applications.
Keywords: asthma, COPD, cystic fibrosis, microRNA, pulmonary arterial hypertension, pulmonary development, pulmonary disease
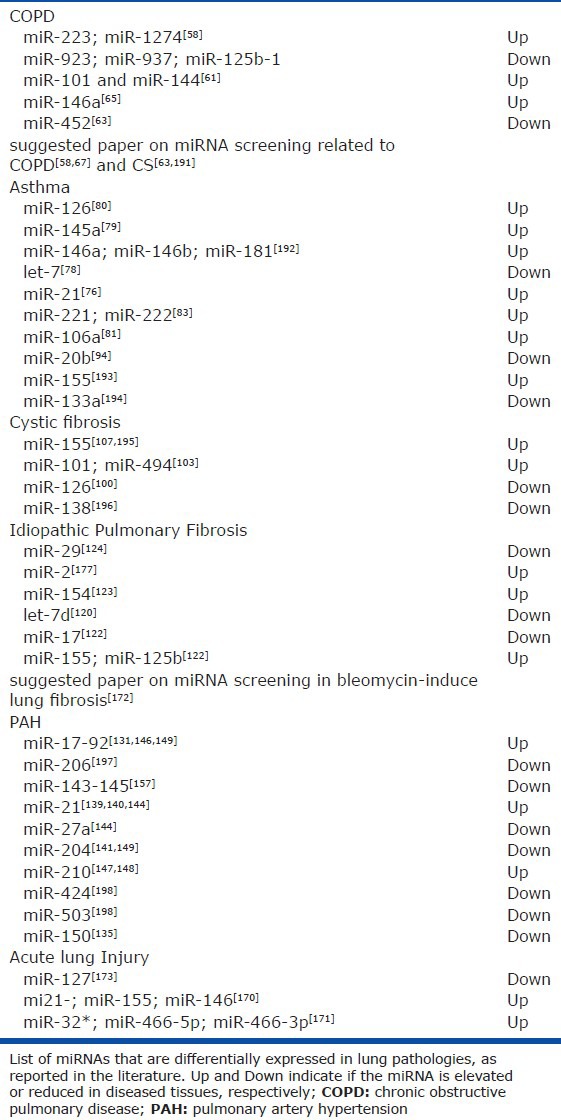
Significant development has been made towards understanding the contribution of microRNAs (miRNAs) in development of lung and pathogenesis of pulmonary diseases.[1,2] This review will provides an overview on the role of miRNAs in lung disease reassuming recent findings that extent our perspective on the importance of these molecules in guiding the cellular response upon different stress conditions. Interestingly, it appears that this class of non-coding regulatory RNA play a key role in several aspects of inflammation which is a determinant feature in many lung diseases[3] such as cystic fibrosis, emphysema, asthma and Chronic Obstructive Pulmonary Disease (CODP).[4] It is believed that miRNAs are involved in various aspects of innate and acquired immunity, and therefore, indirectly involved in these inflammatory lung diseases.[5,6] In this review, we will discuss the involvement of miRNAs in lung development as well as the pathogenesis of various pulmonary diseases (Table 1).
Table 1.
miRNAs in lung disease
MICRORNA BIOGENESIS AND FUNCTION
miRNAs are small noncoding RNAs that function by regulating target gene expression post-transcriptionally. The first miRNAs lin-4 and let-7[7,8] were discovered in 1993 and 2000 respectively in Caenorahabditis elegans (C. elegans) as genes involved in developmental timing by mediating sequence specific post-transcriptional regulation of gene expression. Initially this new class of RNA was thought to be present only in C. elegans, however, it was quickly revealed that it exists in many different animal species, including mammals.[9,10] Spatially and chronologically restricted expression patterns, and evolutionary conservation of miRNAs suggested that they have a broad regulatory function in plants and animals. It has been shown that the whole miRNA system regulates greater than 60% of protein-coding genes in a human cell.[11] Close to 2000 human miRNAs have been described to date (Sanger miRBase version 19, http://www.mirbase.org/blog/2012/08/mirbase-19-released/), which play critical roles in development and physiological and pathological processes.
MiRNAs are mainly encoded in either inter-genic regions or within protein coding genes, usually introns. The molecular origins of miRNAs and mRNA targets are not well established, however, it is suggested that miRNAs originate from transposome elements.[12,13] Indeed, several miRNA loci have been described at a repetitive element transposition and subsequent transcription across two tandems, inverted repeat elements.[14] Alternatively, miRNAs in plants seems to be originated from inverted duplication event of the target gene that can form a self-complementary hairpin with the potential to spawn in new miRNA genes if it can confer an advantage of positive selection.[15,16]
The biogenesis of miRNAs begins with the transcription of the primary transcript (pri-miRNA) of about few hundreds to few thousand nucleotides in length (Fig. 1). RNA polymerase II is involved in the production of this capped and polyadenylated stem-loop-structured pri-miRNA, even though it has been found that some pri-miRNAs, in particular those that lie within the Alu repeats, can be produced by RNA polymerase III.[14] Subsequently the pri-miRNA undergoes processing by RNA endonucleases (RNase) in two sequential cleavage steps. The first cleavage takes place in the nucleus by the type III RNase Drosha that liberates a shorter oligonucleotide of about ~70-90 nucleotide (nt) in length called precursor-miRNA (pre-miRNA).[17] Drosha cleaves pri-miRNAs together with a cofactor known as DiGeorge syndrome critical region gene 8 (DGCR8) which represents an important hub for many regulatory proteins involved in the regulation of the miRNA maturation process[18,19] (Fig. 1). The pre-miRNA is then exported to the cytoplasm by the Exportin 5 protein where it is further processed by the RNase III enzyme Dicer. Dicer generates a ~22 nt double-strand ribonucleotides with 5’ phosphate and two nucleotides 3’ overhangs (Fig. 1).[20] In the subsequent step, the two strands are separated and one of them is recruited by the Argonaute (Ago) proteins[21] to form a multi-protein complex known as the RNA-induced silencing complex (RISC)[22] (Fig. 1). This loaded RISC machinery is able to guide the miRNA to target partially complementary sequences, usually present in the 3’-untranslated region (UTR), on mRNA transcripts. Generally, just one strand of miRNA is accumulated inside the cell and loaded in the RISC complex by association with Ago1 and Ago2 which are the two most highly expressed Ago proteins present in mammalian cells.[23] The other strand, often referred as “miRNA*”, was originally considered as a byproduct of the miRNA biogenesis, however recent findings demonstrated that it retains biological activities.[24,25,26,27,28] The 6-8 nucleotide sequence at the 5’-end of miRNA which contributes to base paring with the target mRNAs is referred as the “seed sequence”. In recent years contrasting results have been published regarding the mechanism of miRNA binding to Ago proteins. Ago2 is the is the only isoform with RNase activity and mainly acts to promote mRNA degradation while Ago1 seems optimized for cleavage-independent repression.[29] Furthermore, Ago2 appears to have selectivity for siRNA-like duplexes with more extensive base pairing[29,30] It is noted that miR* strands represent an abundant fraction of RNA species bound to Ago2.[31] Therefore, miR:miR* duplex could be bifunctional with one strand associated with Ago1 which functions as a cleavage-independent repression of the mRNA, and the miR* associated with Ago2 which triggers a cleavage-dependent repression of the mRNA.[32]
Figure 1.

miRNA Biogenesis. miRNAs are transcribed in the nucleus by the RNA polymerase type II as long primary transcripts (pri-miRNA) of a few hundred up to few thousand nucleotides (nt). The pri-miRNA is cleaved by the microprocessor containing Drosha, which is the type III RNase designated for the cleavage of pri-miRNAs, in complex with several cofactors including DiGeorge syndrome Critical Region 8 (DGCR8). The processing of the pri-miRNA by the Drosha complex gives rise to RNA with a short hairpin structure of 70−90 nt called precursor miRNA (pre-miRNA). The pre-miRNA is then exported from the nucleus to the cytoplasm by Exportin 5 and then cleaved by the RNase type III enzyme Dicer. Dicer cleaves the pre-miRNA within a multi-protein complex that among several components contain two double-stranded RNA binding proteins, the human immunodeficiency virus transactivating response RNA-binding protein (TRBP) and PACT. As a result of cleavage by Dicer, pre-miRNA becomes the ~ 22 nt sequence, which is known as the mature form of the miRNA. One of two strands of the mature miRNA is loaded into the RNA-Induced Silencing Complex (RISC) which contains Argonaute (Ago), and is guided to the 3’-UTR of target messenger RNA (mRNA) where it then promotes translational inhibition or degradation of mRNA.
miRNAs IN LUNG DEVELOPMENT
miRNAs have rapidly emerged not only as critically contributing to various pulmonary diseases but also to normal development of the lung and maintenance of its homeostasis. Lung development can be arbitrarily divided into 6 stages that are found in all mammalian species: embryonic, glandular, canalicular, saccular, alveolar and vascular maturation. After the initial differentiation of lung epithelial cells from the endoderm, the epithelial tube is formed with little to no lumen in the glandular phase. In the canalicular phase, bronchioles are produced and undergo thinning of the interstitium and a flattening of the epithelium in order to form alveolar ducts and air sacs during the secular phase. At the final stage, alveoli are formed after birth.[33]
Fetal lung development is a complex process temporally and spatially orchestrated by a complex set of many genes.[34] The signalling molecules involved in lung development include fibroblast growth factors (FGFs),[35] transforming growth factor- β (TGF-β),[36] Wnts[37] and hedgehogs.[38] The evidence that miRNAs play a role in lung development derive from mice with conditional knockout of Dicer in lung epithelial cells that exhibit a failure of epithelial branching, underscoring the essential regulatory role of miRNAs in lung epithelial morphogenesis.[39] At embryonic stage 11.5 (E11.5) in the lung epithelial branching region, Ago1 and Ago2 are enriched in distal epithelium and mesenchyme respectively, further underscoring the important role of miRNAs in the dynamic changes occurring during lung remodeling and maturation.[40] Evaluation of miRNA expression patterns during the different phases of lung development revealed 27 miRNAs which are differentially expressed.[41] For instance miR-29a plays a role in limiting proliferation in the late stage of lung development.[41] It is also highly expressed in the adult lung and from over-expression in lung cancer cells appears to inhibit tumorigenicity.[42] The expression of the miR-17~92 cluster, which includes 6 miRNA genes (miR-17, -18a, -19a, -20a, -19b-1, and -92-1),[43] is decreased as development progresses.[41] An gene ontology (GO) analysis of the predicted targets of this cluster show that these miRNAs control genes which are critical for proper developmental progress, such as transcriptional factors and regulators of nucleic acid metabolism. The overexpression of this cluster is observed in lung cancer cells.[44] Studies on the role of miR-17-92 locus in lung development have found that miRNAs in this locus are highly expressed in undifferentiated lung progenitor epithelial cells and, by regulating the cell cycle regulator gene Retinoblastoma-like 2 (Rbl2), it promotes their proliferation.[45,46] In contrast, miR-127 and miR-351 are expressed transiently during the sacculo-alveolar phase initially in the mesenchymal compartment and later in the lung epithelial cells, suggesting their roles lie in the cellular reorganization and differentiation process during mesenchymal to epithelial transition (EMT).[41]
Additional studies on the miRNA expression pattern in lungs revealed two miRNAs, miR-200c and miR-195, which are specifically expressed in lung and nine miRNAs co-expressed in other organs, especially in the heart.[47] miR-29a and miR-29b are upregulated in adult lungs, while miR-154 is more abundant in neonatal lungs.[48] These data indicate a similarity in the overall expression profile between mouse and human lungs throughout the lung developmental process and highlight the evolutionarily conserved roles of miRNAs in this process. Finally, evaluation of the miRNA signature in aged lungs has been carried in order to figure out any characteristic changes in miRNAs regulation, however no substantial difference in miRNA expression have been observed in aged mouse lungs.[49]
miRNAs IN LUNG DISEASE
In this section, we will discuss the link between deregulation of miRNAs and the pathogenesis of different pulmonary diseases (Table 1) as well as the potential therapeutic approaches based on restoration of the physiological miRNA signature.
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) presents as the reduction of airflow due to abnormalities in the small airways compartment and associated infiltration of inflammatory cells, thickening of the alveolar wall and ultimately damage of the lung parenchymal and epithelium.[50] It encompasses both emphysema and chronic asthmatic bronchitis. Emphysema results from progressive alveolar septal destruction with concomitant reduction of the surface area available for gas exchange,[51] while bronchitis constricts the airways clogging them with the accumulation of inflammatory mucous exsudate.[52] Although cigarette smoke is a main risk factor for COPD, only 20% of smokers develop this pathology,[53] thus there are additional factors that are implicated in the pathogenesis of COPD, which is influenced by a combination of environmental,[54] genetic[55] and epigenetic components.[56] Study of miRNAs differentially expressed between non-smokers and smokers found that cigarette smoke results, generally, in the downregulation of miRNA expression (Table 1).[57] Seventy miRNAs were found differentially expressed in lung whole tissue between smoking patients affected by COPD and healthy smokers.[58] Among these differentially expressed miRNAs 57 were up regulated with miR-223, which has been demonstrated to be upregulated upon lipopolysaccharide (LPS) exposure,[59] and miR-1274a being the most highly induced.[58] In this study, the authors identified transforming growth factor (TGF)-β, Wnt and focal adhesion pathways as the most relevant pathways in which miRNAs may be involved in the pathogenesis of COPD.[58] In the same study, members of the miR10/107 family; miR-15b, 424, 107, were all upregulated with miR-15b more abundantly localized in areas of emphysema as well as fibrosis preventing the expression of SMAD7, an inhibitor of the TGF-β signaling.[60] A recent study addressed the role of two up regulated miRNAs, miR-101 and miR-144, upon cigarette smoke exposure of human airway epithelial cells and in vivo in lungs of mice exposed to smoke and in COPD patients.[61] It found that both these miRNAs target the cystic fibrosis transmembrane conductance regulator (CFTR) which is a chloride channel found to be suppressed by exposure to airway pollutants and cigarette smoke.[62]
MiRNA/mRNA microarray expression analyses carried out on human alveolar macrophages from smoker and non-smokers, found a general down modulation of miRNA expression in smokers. In particular, low expression of miR-452 has been linked to increased expression of matrix metalloproteinase 12 (MMP12),[63] which is known to be associated with the development of emphysema.[64] Interestingly, this study delineate an association between deregulation of miRNAs and macrophage polarization from an M2 immunosuppression-activated phenotype to an M1 microbicidal-activated phenotype.[63]
A regulatory role of miRNAs has also been observed in the fibrobrasts of tissue specimens derived from smokers affected by COPD who underwent surgery.[65] This experiments focused on the role of prostaglandin (PG) E2 since it is an important mediator of tissue inflammation that increases in expression in the lungs of patients with COPD.[66] Its production is induced by pro-inflammatory cytokines such as IL-1β and TNF-α and depends on the expression of COX-2 together with the expression of miR-146a which targets COX-2 mRNA.[65] The induction of miR-146a takes place both in COPD and control fibroblast, but to a lesser extend in COPD fibroblast. In this context miR-146a is thought to be a feedback control mechanism that limits the intensity and duration of inflammation by reducing the level of COX2 and hence the production of PGE2.[65]
Recently the search for biomarkers for early detection of COPD has drawn attention on the role of circulating miRNAs. A study found five deregulated circulating miRNAs in serum of COPD patients, four of them downregulated (miR-20, miR-28-3p, miR-34c-5p and miR-100) and one upregulated (miR-7) in comparison with healthy individuals.[67] Finally, similar attempts to apply miRNA expression signature as a diagnostic tool, suggest the possibility of distinguishing COPD patients from lung cancer patients by measuring their miRNA expression pattern.[68,69]
Asthma
Asthma is a lung condition that is increasingly prevalent in the western world, which is triggered by a sustained inflammatory response in the airway that is caused by a combination of air pollutants and genetic predisposition. Asthma is characterized by reversible airway obstruction, peribronchial inflammation and airway hyper responsiveness (AHR). A relevant feature of asthma is the occurrence of acute exacerbation events that involve enhanced contraction of the airway smooth muscle layer in response to inhaled stimuli and are the consequence of AHR. In the late stages of the disease, airway remodelling occurs which consists of epithelial desquamation, globet cells hyperplasia, smooth muscle cell hypertrophy and hyperplasia, an increase in matrix protein deposition, basement membrane thickening and growth, and proliferation of new blood vessels.[70] The inflammatory response plays a pivotal role in the progression and pathology of asthma featuring a production of IgE and involving a consistent recruitment of leukocytes, in particular eosinophils together with type 2 T-helper (Th2) cells and mast cells.[71] TGF-β signalling has been found to play a key role in the remodelling that occurs during the progression of asthma.[72] Indeed TGF-β, in addition to its pro-fibrotic action, characterized by increased synthesis of collagen[73] and fibronectin,[74] also promotes airway smooth muscle cell proliferation and epithelial apoptosis.[75]
Several aspects of asthma have been linked to the deregulation of miRNAs (Table 1). Of particular interest is the involvement of miRNAs in the regulation of the immune response and inflammation by targeting several immune receptors and cytokines. In this context, miR-21 has been described to target IL-12 which is a major cytokine involved in Th1 cell polarization.[76] MiR-21 ablation in mice challenged with ovalbumin has been described to mitigate the progression of the pathology by alleviating the allergic immune response and skewing the balance between Th1 and Th2 responses toward Th1.[77] In a opposite way, a cell polarization toward a Th2 response has been observed to be concomitant with the down modulation of let-7 family in inflamed airways.[78] Exogenous administration of let-7 in asthmatic mice was shown to reduce the level of IL-13, an important mediator of the Th2 response during allergic events.[78] An additional miRNA involved in the Th2 response and eosinophil recruitment is miR-145.[79] Mice challenged with House Dust Mite (HDM) allergen and then treated with miR-145 inhibitor displayed a reduction of pro-inflammation cytokines, IL-13 and IL-5, and alleviation of asthma symptoms. The anti-inflammatory effects of miR-145 inhibitor were comparable to those of steroid treatment.[79] T lymphocyte polarization is also regulated by miR-126, which is a potent and specific inducer of the Th2 allergic response and TLR4 signalling present in asthma.[80] Exposing the airways to a miR-126 inhibitor abolished HDM induced airway hyper responsiveness and attenuated mucus hyper-secretion and accumulation of eosinophils.[80] Beneficial effects have also been obtained by knocking down miR-106a in the ovoalbumin sensitized murine model of asthma; in this experiment knock-down of miR-106a increased the level of the anti-inflammatory cytokine IL-10 and reduced the Th2 response alleviating AHR.[81] The anti-inflammatory role of IL-10 is also dependent on its role in counteracting the LPS mediated induction of miR-155, which increases PIP3 levels and activates the downstream signalling of NF-KB and MAPK.[82] Studies have also been performed that address the role of mast cells in asthma. The miR-221, -222 family was demonstrated to be transcriptionally induced upon mast cell activation. In particular miR-221favors mast cell activation upon IgE-antigen complex stimulation by promoting cell adherence, cytokine production and degranulation.[83]
A comprehensive study of miRNAs differentially expressed in lung tissue of mice challenged with ovoalbumin - a model recapitulating the main phases of asthma progression - found 58, 66 and 75 miRNAs significantly modulated by short, intermediate and long-term challenge respectively.[84] Bioinformatics analysis of the data coming from this study found out miRNA-regulators of several pathways ranging from cell cycle, TGF-β, protein synthesis and inflammation. Interestingly, cell proliferation is more pronounced in the early stages of asthma than in the late ones. MiR-574-5p is involved in cell proliferation and inversely correlated with NuSAP, a microtubule-associate protein involved in mitotic spindle organization.[85] MiR-29b and miR-29c, which are correlated with matrix deposition and target MMPs, are downregulated in the late stages. Notably miR-146a, which is regulated by Toll Like Receptors (TLRs) was the only miRNA found to be regulated in all three phases.[84] Forced expression of miR-146a decreases the production of various pro-inflammatory cytokines and chemokines.[86,87] Moreover, T cell receptor driven NF-kB activation of miR-146a is important in down-regulating NF-kB activity in a negative feed back loop, at least partly through repressing the NF-kB signalling transducers TRAF6 and IRAK1, thus modulating the T-cell immune response.[88]
It is worth mentioning that increasing evidence suggests that angiogenesis plays an important role in the progression of asthma.[89,90] Vascular endothelial growth factor (VEGF) levels are increased in tissues obtained from asthmatic subjects and it has been demonstrated that alveolar epithelial cells,[91] fibroblast[92] and leukocytes[93] produce VEFG during the inflammatory process. Alveolar macrophages (AM) are an important source of VEGF during lung injury. Increased miR-20b expression in AM from asthmatic mice decreases VEGF protein levels.[94] Analysis of the contribution of the vasculature to the establishment of the aberrant inflammation response may lead to new insights in the treatment of asthma. For instance, overexpression of miR-181b in endothelial cell inhibits NF-kB nuclear localization and signalling which down-modulates leukocyte influx hence decreasing lung injury.[95] This discovery suggests that miR-181b may be a new target for anti-inflammatory therapy.
Cystic fibrosis
Cystic Fibrosis (CF) is a monogenic lung disease[96] characterized by mucus airway obstruction, neutrophil-dominated airway inflammation and bacterial infection that leads to progressive pulmonary damage and emphysema.[97] The gene involved in the insurgence of CF is the CFTR encoding for an ATP-dependent anion channel-protein present in the apical part of the epithelium. CTFR coordinates the secretion and absorption of NaCl, fluid and airway surface liquid homeostasis.[98] The most common CFTR mutation causes erroneous protein folding and degradation, which ultimately leads to an imbalance between Cl- secretion/Na+ absorption and airway surface liquid depletion. As a consequence of the epithelial layer dehydration, mucociliary clearance is impaired which affects innate immune defences favoring infection by opportunistic pathogens such as Pseudomonas aeruginosa and Staphylococcus aureus.[99] Neutrophil-dominated airway inflammation has been implicated as a driving force in the airway remodelling and bronchiectasis. These processes, characterized by bronchial wall thickening and tissues fibrosis, are mediated by the production of reactive oxygen species and metallo-proteases.
The first work describing miRNAs involvement in CF was published by Oglesby et. al.[6,100] (Table 1). In this work, miR-126 was shown to target TOM1 protein, a known regulator of endosomal trafficking of ubiquitinated proteins,[101] which is also a negative regulator of IL-1β, TNF-α and LPS signalling pathway.[102] miR-126, which is highly expressed in the lung, is down modulated in the epithelium of CF patients; this leads to increased expression of TOM1 and decreased NF-kB-induced cytokines, such as IL-8.[100] This mechanism may be an attempt of the lung epithelium to compensate for the high pro-inflammatory burden of CF.[6] miRNA Responsive elements (MRE) for miR-101 and miR-494 have been identified in the 3’UTR of the CFTR transcripts these miRNAs have be shown to inhibit CFTR translation.[103] Notably, these two miRNAs are elevated in CF patients and their alteration has been linked to other changes in pro-inflammatory cytokines, cells cycle progression and carcinogenesis.[104,105,106] CFTR is also indirectly regulated by miR-138, which targets the transcriptional regulatory protein SIN3A. MiR-138 relieves the transcriptional repression of SIN3A and allows the expression of wild type and mutant form of CFTR restoring Cl- transport in CF epithelia.[91]
In vitro comparison of differentially expressed miRNAs between CF epithelial cells and control epithelial cells found miR-155 to be highly elevated in diseased tissues[107] (Table 1). The same trend is mirrored in CF lung epithelial cells and circulating CF neutrophils.[107] MiR-155 specifically inhibits Phosphatidylinositol 3,4,5-trisphosphate 5-phosphatase 1 (SHIP1) expression, thereby promoting activation of the PI3K/Akt signalling pathway and promoting expression of the pro-inflammatory IL-8 cytokine[107] – the well-characterized chemotactic agent for neutrophils.
Advances in the care of patient with CF have lead to a dramatic increase in patient survival and a concomitant observation of additional complications, such as tumorigenesis in other organs ascribable to mutation and loss of expression of CFTR. Interestingly, the tumor suppression activity of CFTR is at least in part mediated by the up modulation of miR-193b[108] that in turn targets urokinase-type plasminogen activator (uPA) known to be involved in various malignant traits of cancer.[109]
Idiopathic pulmonary fibrosis
Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive fibrotic interstitial pneumonia of unknown causes characterized by a rapid progression over a few years.[110] However, several IPF risk factors are known; these include viral infection, occupational activities associated with a high probability of dust or vapour inhalation,[111] cigarette smoke[112] and pollutants.[111] IPF appears to be initially triggered by persistent and repetitive microinjuries to the alveolar epithelium.[113] Continuous damage of the epithelial cells leads to the destruction of the basal membrane and hence the activation of coagulation and metalloproteinases. Later steps of IPF include the massive deposition of extracellular matrix by activated myofibroblasts derived from different sources, such as fibroblast, pericytes, alveolar epithelial cells and mesothelial cells. IPF is characterized by aberrant activation of developmental signalling pathways, such WNT/β-catenin,[114] TGF-β[115] and Sonic hedgehog.[116] TGF-β is considered the driving force of epithelial-to-mesenchymal transition (EMT).[117] Cells expressing both epithelial and mesenchymal markers have been found in mice treated with TGF-β inhalation.[118] In vitro stimulation of alveolar epithelial cells with TGF-β can induce EMT.[119] The first miRNA demonstrated to be involved in the pathogenesis of IPF was let-7d.[120] Let-7d is downregulated in samples from IPF patients, which was sufficient to cause EMT in lung epithelial cells[120] (Table 1). Decreased let-7d is mediated by TGF-β via a SMAD-dependent mechanism.[120] Inhibition of let-7d triggers a global decrease in lung epithelial markers and a concomitant increase in alveolar septal thickening.[120]
Levels of miRNAs have been evaluated in different RNA samples from biopsies of IPF patients with varying speeds of disease progression (Table 1).[121] Generally, both slowly and rapidly progressive IPF biopsies revealed a down modulation of several miRNAs compared to normal tissue and specific miRNAs signature can provide predictive clues about the progression rate of the disease.[122] Interestingly, many upregulated mRNA found in IPF are implicated in EMT and correlate with the downmodulation of the respective targeting miRNA.[122] Furthermore, a decrease in key RISC components such as AGO1 and AGO2 has been observed. Another study found that 43 miRNAs are significantly upregulated in lung tissues from IPF patients and that the majority of them belong to the miR-155 family present as a cluster on chromosome 14.[123] Up regulation of miR-155 was triggered in vitro upon stimulation with TGF-β. Finally, biochemical studies confirmed a mitogenic effect of TGF-β on fibroblast mediated by miR-155 and WNT/β-catenin.[123] Two additionally studies connecting TGF-β signalling to miRNA regulation in IPF have been performed on miR-21 and miR-29. Mice with bleomycin-induced fibrosis present increased level of miR-21 in the lungs that is primarily localized in myofibroblasts.[77] MiR-21 upregulation is induced by TGF-β and promotes the activation of pulmonary fibroblast by targeting SMAD7, thus functioning in an amplifying circuit to promote lung fibrosis.[77] Reciprocally, miR-29 is suppressed by TGF-β in human fetal lung fibroblast. Knockdown of miR-29 derepressed extracellular matrix-associated genes and several fibrosis-related genes, including collagens, laminins and integrins.[124] Restoration of miRNA expression by targeting miRNAs up regulated during IPF may represent a valuable novel therapeutics treatment for this pathology.
Pulmonary artery hypertension
Pulmonary Artery Hypertension (PAH) is a disease characterized by hyperproliferation and neointima formation leading to vasoconstriction of the pulmonary artery and ultimately right ventricular heart failure and death. Both pulmonary artery smooth muscle cells (PASMCs) and pulmonary artery endothelial cells (PAECs) are involved in this disease and extensive studies have been performed on these cells looking for the aberrant molecular mechanisms responsible for the establishment of PAH. Regarding heritable PAH, which is the most frequent form of the disease, in almost 70% of cases the genetic alteration is represented by an autosomal dominant mutation in the bone morphogenic protein receptor 2 (BMPR2) in PASMC.[125] More rarely, mutations of Endoglin and activin receptor-like kinase 1 (ALK1) have been identified.[126] However, since mutation of BMPR2 occur in just slightly more than half of the case of heritable PAH it has been suggested that this mutation may cause susceptibility to other factors. Indeed, genetic and environmental stimuli such as dysregulated inflammation,[127] hypoxia[128] and aberrant Notch3[129] and TGF-β[130] signalling can promote the insurgence of PAH.
A first clue that suggested that miRNAs play a role in the pathogenesis of PAH derived from the observation that BMPR2 protein, but not its messenger, is reduced in PAH animal models. From this initial observation it has been found that IL-6 induces the expression of the miR-17-92 cluster through STAT3 activation and that several miRNAs from this cluster target BMPR2[131] (Table 1). Caruso et al. reported a screening of differentially expressed miRNAs in the monocrotaline and hypoxia induced rat models of PAH.[132] In this study the authors found miRNAs similarly deregulated between the two PAH models, in addition they also discovered specific miRNA signature in each group. The discovery of differentially regulated miRNAs between hypoxia and monocrotaline treated rats is in agreement with the differential pathobiology found in the two models. Indeed, monocrotaline challenge mainly targets the pulmonary vascular endothelium triggering strong inflammation while hypoxia stimulates changes also in medial and adventitial with less inflammation.[133,134] Moreover, researchers have identified specific changes in miRNAs signature during PAH progression.[132] An additional screening on deregulated miRNAs in circulating microvesicles of PAH patients and rat models found that the downregulation of miR-150 correlates with the severity and prognosis of PAH (Table 1).[135]
MiR-21 is consistently downregulated in monocrotaline-injected rats but not during hypoxia exposure.[132] MiR-21 expression is induced by pro-inflammatory cytokines such as IL-6[136] and TGF-β/BMP and it is known to drive SMC differentiation.[137] A recent work from Parikh et al. demonstrated on pulmonary artery endothelial cells that BMP-dependent signalling activation of miR-21 represses Rho-kinase activation, thus counteracting the Rho signalling in promoting pulmonary vascular pathology.[138] Moreover, miR-21-null mice presented overexpression of RhoB and hyperactivation of Rho-kinase activity accompanied by exaggerated manifestation of PAH.[139] in vitro administration of a miR-21inhibitor in hypoxia-exposed mice reduces pulmonary vascular remodelling and PAH-associated right ventricular hypertrophy.[140]
One of the first studies providing evidences for the involvement of a specific miRNA in the etiology of human PAH focused on the downregulation of miR-204 (Table 1),[141] which had been previously shown to be associated with cell proliferation in cancer cells[142] and epithelial retinal depolarization.[143] In PASMC STAT3 mediates downregulation of miR-204 which enhances the activity of Src thereby increasing proliferation and resistance to apoptosis.[141]
A connection between PAH insurgence, the TGF-β signalling pathway and miRNAs has been described in a form of heritable PAH that presents a mutated SMAD9 gene (protein Smad8).[144,145] This work demonstrated the role of Samd8 in promoting miRNA expression by the non-canonical BMP pathway. Specifically, two miRNAs have been described to be regulated by the non-canonical BMP pathway, miR-21 and miR-27a, whose expression are reduced in PAEC and PASMC in PAH patients.[144] Moreover, miR-21 expression levels are correlated with cell proliferation in PAEC derived from PAH patients.[144]
In a monocrotaline-induced rat model, miR-17 suppression with anti-miR-17 treatment has been shown to significantly counteract the pathological severity of the disease.[146] In both in vitro and in vitro treatment with anti-miR-17 a significant increasing of the miRNA's target p21 has been shown to be a central mechanism in the repression of the SMC proliferative feature of PAH.[146] A hypoxia induced miRNA found to be relevant in the pathology of PAH is miR-210, indeed it has been demonstrated that miR-210 expression increased in microarray analysis on human in hypoxic PASMC and in whole lungs of hypoxic mic.[147] The induction of miR-210 is HIF-1α-dependent and triggers anti-apoptotic effects via directly targeting the transcription factor E2F3.[147] Previously work carried out on PAECs showed an additional mechanism of adaptation to hypoxic conditions in which miR-210, by targeting Iron-Sulfur Cluster Assembly Proteins 1/2 (ISCU) represses mitochondrial metabolism, thus facilitating glycolysis.[148]
Additional clues about the involvement of miRNAs in the hypoxia-induced PAH focused on the cytoprotective action of secreted membrane microvesicles, called exosomes, delivered from mesenchymal stem cells (MSC).[149] Several reports showed that treatment with these microvesicles ameliorates symptoms and prevents progression in PAH and vascular injury.[150,151,152] In one recent report, it was shown that intravenous delivery of mesenchymal stromal cell-derived exosomes (MEX) interferes with early hypoxic signals in the lung by counteracting inflammation.[149] In particular MEX inhibits MCP-1 release and monocyte recruitment together with decreasing STAT3 phosphorylation, which is an important mediator in the inflammatory and pro-proliferative response triggered by hypoxia.[153] Inhibition of STAT3 activation also affects induction of the miR-17/92 cluster which targets BMPR2.[131] Moreover, treatment with exosomes from MSC also interferes with the STAT3 downregulation by miR-204, which inhibits pro-proliferative action of STAT3 in SMC.[141]
Due to the key role of the PASMC hyperproliferative phenotype in PAH, several studies tried to decipher the role played by miRNAs in this context. MiR-206, previously described as tumor suppressor,[154] is downregulated in hypertensive mouse with excessive right ventricular systolic pressure. Its anti proliferative action is mediated by directly targeting Notch3, whose signalling is known to be elevated in PAH.[129] Two miRNAs highly expressed in SMC; miR-145 and miR-143, have been shown to play a pivotal role in the modulation of SMC phenotype. In particular, their expression is transcriptionally activated by both TGF-β and BMP4 and promotes a contractile phenotype in SMC by targeting the Kruppel-like factor-4 (KLF4).[155] Knock-out of both miRNAs in mice leads to a development of thinner medial layer and hypotension.[156] One recent work investigated the effect of miR-145 modulation in the pathogenesis of PAH and demonstrated that its expression is induced by hypoxia and that its expression is elevated in PAH patients.[157] Genetic ablation or inhibition of miR-145 by antisense oligonucleotides in hypoxia-challenged animal exhibits a protective effect against PAH development.[157] Additional studies reported a downregulation of miR-145 during neointimal formation upon rat carotid balloon vascular injury and adenoviral overexpression of miR-145 confers a protective role against vessel wall.[158] On the contrary, a different study reported that mice deleted in miR-143 and/or miR-145, develop reduced neointima formation upon carotid artery ligation, thus pointing to a protective role of miR-145 ablation.[159] This phenotype is probably due to a depletion of SMC in the media due to the absence of these important miRNAs during the development.[160] The effects of miR-145 null mice in hypoxia-induced PAH and neointimal formation is likely dependant on regulatory networks influenced by a plethora of miR-145 direct and indirect targets affecting cytoskeleton dynamics and thus cell migration.[159] It is interesting to speculate that the effect of miR-145 on cytoskeleton organization and cell migration is context-dependent and that the effect of its deregulation can be different depending on the state of smooth muscle cell differentiation and on the microenvironment. Detailed analysis of miRNA expression has been performed in PAH patients by isolating plexiform (PLs) and concentric lesions (CLs).[161] This analysis focused on expression of the endothelial-specific miR-126[162] and the SMC-specific miR-145 and miR-143. Expression of miR-143 and miR-145 was significantly lower in PLs compared with CLs and healthy tissue. Decreased expression of miR-143/145 may reflect the more proliferative and undifferentiated phenotype of SMCs present in PLs. On the other hand, the expression level of miR-126 was higher in PLs when compared to CLs, in accordance with the higher abundance of EC in PLs than in PLs.[163] Thus this study provided a specific miRNA signature for different hypertensive pulmonary lesions potentially providing new diagnostic tools.
Acute lung injury and acute respiratory distress syndrome
Acute lung injury (ALI) is a phenotypically variable acute respiratory failure clinically characterized by progressive hypoxemia, reduced lung compliance and intense inflammation that results from either direct injury to the lung (pneumonia, thoracic trauma, smoke-related lung injury) or an indirect insult (pancreatitis). ALI together with its most severe manifestation namely the acute respiratory distress syndrome (ARDS) has a high incidence and high mortality.[164] Cellular characteristics of ALI and ARDS are the loss of alveolar-capillary membrane integrity consisting of a leakage of the endothelium and degradation of the alveolar basement membrane with the consequent extravasation of fluids from the circulation to the inside the small airways.[165]
It is well recognized that only a small proportion of exposed individuals will ultimately develop these syndromes and has been proposed that there is a genetic predisposition to the development of ALI pathology.[166,167,168] Recently, efforts in determining the genetic component of ALI/ARDS pathogenesis have been extended to the involvement of miRNAs in this process (Table 1). Several genes involved in the immune response and inflammation, already described to be targeted by miRNAs, have been suggested as candidates in the establishment of ALI.[169] A detailed study investigating changes in miRNA expression upon lung injury has been performed using the model of injury trigged by high volume tidal ventilation (HVTV).[170] In this study HVTV applied to mice induced an upregulation of several miRNAs, with a few exceptions.[170] Inflammatory and TGF-β-signalling miRNA-gene networks have been identified by in-silico pathway analysis as significant modulated in the onset of ALI.[170] MiR-21 was one of the most upregulated and treatment of mice with antisense oligonucleotides against miR-21 before HVTV ameliorated induction of pulmonary edema associated with the ventilation injury.[170] Other miRNAs associated with inflammation, such as miR-155, let-7 and miR-146, are similarly deregulated upon HVTV treatment[170] (Table 1). Another expression analysis on the effects of stress ventilation was performed by stretching rat alveolar epithelial cells to mimic mechanical ventilation.[171] In this study, the majority of miRNAs were again found to be upregulated.[171] Interestingly the highest fold-change occurred in the detection of miR-32*, suggesting a functional role for this miRNA passenger strand.[171] The authors of this work have also demonstrated a functional link between the levels of miR-466d-5p and miR-466f-3p, and the inhibition of stretch-induced permeability.[171]
An analysis of the miRNAs expression profile of mice with bleomycin-induced lung injury[172] showed that miR-127 is down modulated in macrophages. MiR-127 targets the Fc receptor for IgG (IgG FcγRI - CD64)[173] that activate the cells in the clearance of the immunocomplexes and in promoting inflammation by secreting cytokines. The same study demonstrated that overexpression of this miRNA can prevent exaggerated inflammation during injurious stimuli and the set of ALI in mice treated with bleomycin.[173]
A study on the role of miRNAs in the pathogenesis of ALI also identified the involvement of miR-16 in the resolution of pulmonary edema.[174] In this work, mice exposed to hyperoxia exhibited a decrease in miR-16 together with decreased expression of the epithelial sodium channel which is critical for driving fluids out of alveolar space.[175] MiR-16 has been found to target the serotonin transporter (SERT).[176] In vitro experiments using human alveolar epithelial cells demonstrates that overexpression of miR-16 reduces SERT and increases the epithelial sodium transporter proposing miR-16 as a candidate for the treatment of pulmonary edema and prevention of ALI.[174]
miRNAs AS THERAPEUTIC TARGETS
The recent achievements in manipulating miRNA expression in animal models of related human diseases, together with the increasing rate of discoveries about the role played by miRNAs in several human disorders have raised the possibility of using these molecules as a new class of therapeutic tools. Along with this concept, from the gain- and loss-of function studies it appears that dysregulation of miRNAs is well-tolerated in normal tissues but that it can influence the behaviour of the tissues experiencing pathological conditions.[177] The first clinical trial of a miR-122 mimicry as a therapy for suppression of hepatitis C virus (HCV) is currently under going.
Several molecular strategies have been employed in order to down modulate or overexpress miRNAs in vitro. Anti-microRNA oligonucleotides (anti-miR) have been generated and extensively chemically modified in order to increase the effectiveness and stability. Modification of the phosphodiester backbone with a phosphorothioate linkage between nucleotides or including a 2’O-methyl group (antagomir oligos[178]) are two common modifications for increasing stability and decreasing the in vitro clearance. Additionally, antagomirs containing a cholesterol moiety are thought to favour cellular uptake.[179] Special interest has been focused on the use of the Locked Nucleic Acid (LNA) that present a modification in the ribose ring improving nuclease resistant and conferring an high affinity for complementary sequence. LNA antagomirs against miR-33 showed beneficial effects in non-human primates for the treatment of atherosclerosis by increasing the level of high-density lipoprotein and lowering the level of low-density lipoprotein.[180] Systemic delivery of antagomir has been proven effective in the treatment of cardiac hypertrophy and fibrosis by down modulating miR-133[181] and miR-21[182] respectively. The anti-miR-21 therapeutic effect against fibrosis has also proven effective in the lungs[77] and for the treatment of diabetic nephropathy using a mouse model of type 2 diabetes.[183] Currently, the most effective means of delivering anti- or mimic miRNA is through adeno-associated virus (AAV).[184] This system benefits from the advantage of potential tissue enrichment as a result of the natural tropism of the different AAV serotypes. Moreover, the exogenous sequence can be continually expressed, resulting in a robust replacement or inhibition of miRNA expression.
It has been demonstrated that the introduction of miR-29 in the lung protects animals from the insurgence of the pathology in bleomycin-treated rats.[185] The therapeutic potential of miR-29 in pulmonary fibrosis was examined in both the induction phase and during established lung disease induced by bleomycin using the Sleeping Beauty (SB) transposon-mediated gene transfer system. Progresses in delivery of SB transposons have been achieved in the treatment of PAH, in inhibiting lung allograft fibrosis,[186] in lymphoma[187] and in various systemic disease, such as haemophilia.[188]
There are a few potential challenges for the clinical application of miRNA modulation methods, which include off-target effects of antagomirs, and the potential toxicity of phosphorothionate oligonucleotides.[189,190] For the treatment of pulmonary diseases, there is the great advantage that miRNA-related therapeutics can be delivered via inhalation. Inhalation will decrease systemic exposure of miRNA-related therapeutics and, therefore, limit potential off-target effects and toxicity to other organs.
CONCLUDING REMARKS
miRNA biology is a key mechanism for mediating cellular responses under various stress conditions. Lung tissues are constantly under threat of various stresses, such as chemical irritants and air pollutants. Indeed, growing evidence supports the idea that deregulation of protein coding gene expression as a result of aberrant expression of miRNAs is contributing to various stages of the pathogenesis of pulmonary diseases. Therefore, better understanding of the relationship between miRNAs and their target genes will lead to a development of more effective therapies. It is plausible to apply miRNA mimicry or antagonist as novel therapeutic tools. Finally, it is clear that a characteristic miRNA expression profile (or signature) is linked to a specific pathological condition (Table 1). Thus, miRNA signature can be used as a diagnostic tool or for the development of more personalized therapeutic strategy.
ACKNOWLEDGMENT
We apologize to those colleagues whose references we have omitted from this discussion; due to space restrictions and our focus we were unable to include all articles on this interesting and diverse subject matter. We wish to express our thanks to the members of the Hata lab for critical reading of the manuscript and discussion, in particular we are especially grateful to Matthew Blahna for his critical contribution in critical reading of the manuscript. This work was supported by grants from the National Institute of Health (HL093154 and HL108317), the American Heart Association (0940095N) and the LeDucq foundation Transatlantic network grant to A.H.[198]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Garofalo M, Romano G, Di Leva G, et al. EGFR and MET receptor tyrosine kinase-altered microRNA expression induces tumorigenesis and gefitinib resistance in lung cancers. Nat Med. 2012;18:74–82. doi: 10.1038/nm.2577. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.Calin GA, Croce CM. MicroRNA signatures in human cancers. Nat Rev Cancer. 2006;6:857–66. doi: 10.1038/nrc1997. [DOI] [PubMed] [Google Scholar]
- 3.Hassan T, McKiernan PJ, McElvaney NG, Cryan SA, Greene CM. Therapeutic modulation of miRNA for the treatment of proinflammatory lung diseases. Expert Rev Anti Infect Ther. 2012;10:359–68. doi: 10.1586/eri.11.175. [DOI] [PubMed] [Google Scholar]
- 4.Pagdin T, Lavender P. MicroRNAs in lung diseases. Thorax. 2012;67:183–4. doi: 10.1136/thoraxjnl-2011-200532. [DOI] [PubMed] [Google Scholar]
- 5.O’Neill LA, Sheedy FJ, McCoy CE. MicroRNAs: the fine-tuners of Toll-like receptor signalling. Nat Rev Immunol. 2011;11:163–75. doi: 10.1038/nri2957. [DOI] [PubMed] [Google Scholar]
- 6.Oglesby IK, McElvaney NG, Greene CM. MicroRNAs in inflammatory lung disease--master regulators or target practice? Respir Res. 2010;11:148. doi: 10.1186/1465-9921-11-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reinhart BJ, Slack FJ, Basson M, et al. The 21-nucleotide let-7 RNA regulates developmental timing in Caenorhabditis elegans. Nature. 2000;403:901–6. doi: 10.1038/35002607. [DOI] [PubMed] [Google Scholar]
- 8.Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75:843–54. doi: 10.1016/0092-8674(93)90529-y. [DOI] [PubMed] [Google Scholar]
- 9.Lagos-Quintana M, Rauhut R, Lendeckel W, Tuschl T. Identification of novel genes coding for small expressed RNAs. Science. 2001;294:853–8. doi: 10.1126/science.1064921. [DOI] [PubMed] [Google Scholar]
- 10.Pasquinelli AE, Reinhart BJ, Slack F, et al. Conservation of the sequence and temporal expression of let-7 heterochronic regulatory RNA. Nature. 2000;408:86–9. doi: 10.1038/35040556. [DOI] [PubMed] [Google Scholar]
- 11.Friedman RC, Farh KK, Burge CB, Bartel DP. Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 2009;19:92–105. doi: 10.1101/gr.082701.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smalheiser NR, Torvik VI. Alu elements within human mRNAs are probable microRNA targets. Trends Genet. 2006;22:532–6. doi: 10.1016/j.tig.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Borchert GM, Holton NW, Williams JD, et al. Comprehensive analysis of microRNA genomic loci identifies pervasive repetitive-element origins. Mob Genet Elements. 2011;1:8–17. doi: 10.4161/mge.1.1.15766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borchert GM, Lanier W, Davidson BL. RNA polymerase III transcribes human microRNAs. Nat Struct Mol Biol. 2006;13:1097–101. doi: 10.1038/nsmb1167. [DOI] [PubMed] [Google Scholar]
- 15.Cuperus JT, Fahlgren N, Carrington JC. Evolution and functional diversification of MIRNA genes. Plant Cell. 2011;23:431–42. doi: 10.1105/tpc.110.082784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang Y, Hindemitt T, Mayer KF. Significant sequence similarities in promoters and precursors of Arabidopsis thaliana non-conserved microRNAs. Bioinformatics. 2006;22:2585–9. doi: 10.1093/bioinformatics/btl437. [DOI] [PubMed] [Google Scholar]
- 17.Pillai RS. MicroRNA function: multiple mechanisms for a tiny RNA? RNA. 2005;11:1753–61. doi: 10.1261/rna.2248605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wada T, Kikuchi J, Furukawa Y. Histone deacetylase 1 enhances microRNA processing via deacetylation of DGCR8. EMBO Rep. 2012;13:142–9. doi: 10.1038/embor.2011.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Macias S, Plass M, Stajuda A, Michlewski G, Eyras E, Cáceres JF. DGCR8 HITS-CLIP reveals novel functions for the Microprocessor. Nat Struct Mol Biol. 2012;19:760–6. doi: 10.1038/nsmb.2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kok KH, Ng MH, Ching YP, Jin DY. Human TRBP and PACT directly interact with each other and associate with dicer to facilitate the production of small interfering RNA. J Biol Chem. 2007;282:17649–57. doi: 10.1074/jbc.M611768200. [DOI] [PubMed] [Google Scholar]
- 21.Peters L, Meister G. Argonaute proteins: mediators of RNA silencing. Mol Cell. 2007;26:611–23. doi: 10.1016/j.molcel.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 22.Hammond SM, Boettcher S, Caudy AA, Kobayashi R, Hannon GJ. Argonaute2, a link between genetic and biochemical analyses of RNAi. Science. 2001;293:1146–50. doi: 10.1126/science.1064023. [DOI] [PubMed] [Google Scholar]
- 23.Wang D, Zhang Z, O’Loughlin E, et al. Quantitative functions of Argonaute proteins in mammalian development. Genes Dev. 2012;26:693–704. doi: 10.1101/gad.182758.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou H, Huang X, Cui H, et al. miR-155 and its star-form partner miR-155* cooperatively regulate type I interferon production by human plasmacytoid dendritic cells. Blood. 2010;116:5885–94. doi: 10.1182/blood-2010-04-280156. [DOI] [PubMed] [Google Scholar]
- 25.Goff LA, Davila J, Swerdel MR, et al. Ago2 immunoprecipitation identifies predicted microRNAs in human embryonic stem cells and neural precursors. PLoS One. 2009;4:e7192. doi: 10.1371/journal.pone.0007192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang JS, Phillips MD, Betel D, et al. Widespread regulatory activity of vertebrate microRNA* species. RNA. 2011;17:312–26. doi: 10.1261/rna.2537911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Packer AN, Xing Y, Harper SQ, Jones L, Davidson BL. The bifunctional microRNA miR-9/miR-9* regulates REST and CoREST and is downregulated in Huntington's disease. J Neurosci. 2008;28:14341–6. doi: 10.1523/JNEUROSCI.2390-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsang WP, Kwok TT. The miR-18a* microRNA functions as a potential tumor suppressor by targeting on K-Ras. Carcinogenesis. 2009;30:953–9. doi: 10.1093/carcin/bgp094. [DOI] [PubMed] [Google Scholar]
- 29.Förstemann K, Horwich MD, Wee L, Tomari Y, Zamore PD. Drosophila microRNAs are sorted into functionally distinct argonaute complexes after production by dicer-1. Cell. 2007;130:287–97. doi: 10.1016/j.cell.2007.05.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tomari Y, Du T, Zamore PD. Sorting of Drosophila small silencing RNAs. Cell. 2007;130:299–308. doi: 10.1016/j.cell.2007.05.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Czech B, Zhou R, Erlich Y, et al. Hierarchical rules for Argonaute loading in Drosophila. Mol Cell. 2009;36:445–56. doi: 10.1016/j.molcel.2009.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Okamura K, Liu N, Lai EC. Distinct mechanisms for microRNA strand selection by Drosophila Argonautes. Mol Cell. 2009;36:431–44. doi: 10.1016/j.molcel.2009.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zoetis T, Hurtt ME. Species comparison of lung development. Birth Defects Res B Dev Reprod Toxicol. 2003;68:121–4. doi: 10.1002/bdrb.10014. [DOI] [PubMed] [Google Scholar]
- 34.Weng T, Chen Z, Jin N, Gao L, Liu L. Gene expression profiling identifies regulatory pathways involved in the late stage of rat fetal lung development. Am J Physiol Lung Cell Mol Physiol. 2006;291:L1027–37. doi: 10.1152/ajplung.00435.2005. [DOI] [PubMed] [Google Scholar]
- 35.Ramasamy SK, Mailleux AA, Gupte VV, et al. Fgf10 dosage is critical for the amplification of epithelial cell progenitors and for the formation of multiple mesenchymal lineages during lung development. Dev Biol. 2007;307:237–47. doi: 10.1016/j.ydbio.2007.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang X, Inoue S, Gu J, et al. Dysregulation of TGF-beta1 receptor activation leads to abnormal lung development and emphysema-like phenotype in core fucose-deficient mice. Proc Natl Acad Sci U S A. 2005;102:15791–6. doi: 10.1073/pnas.0507375102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang M, Shi J, Huang Y, Lai L. Expression of canonical WNT/β-CATENIN signaling components in the developing human lung. BMC Dev Biol. 2012;12:21. doi: 10.1186/1471-213X-12-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.White AC, Xu J, Yin Y, Smith C, Schmid G, Ornitz DM. FGF9 and SHH signaling coordinate lung growth and development through regulation of distinct mesenchymal domains. Development. 2006;133:1507–17. doi: 10.1242/dev.02313. [DOI] [PubMed] [Google Scholar]
- 39.Harris KS, Zhang Z, McManus MT, Harfe BD, Sun X. Dicer function is essential for lung epithelium morphogenesis. Proc Natl Acad Sci U S A. 2006;103:2208–13. doi: 10.1073/pnas.0510839103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lü J, Qian J, Chen F, Tang X, Li C, Cardoso WV. Differential expression of components of the microRNA machinery during mouse organogenesis. Biochem Biophys Res Commun. 2005;334:319–23. doi: 10.1016/j.bbrc.2005.05.206. [DOI] [PubMed] [Google Scholar]
- 41.Bhaskaran M, Wang Y, Zhang H, et al. MicroRNA-127 modulates fetal lung development. Physiol Genomics. 2009;37:268–78. doi: 10.1152/physiolgenomics.90268.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fabbri M, Garzon R, Cimmino A, et al. MicroRNA-29 family reverts aberrant methylation in lung cancer by targeting DNA methyltransferases 3A and 3B. Proc Natl Acad Sci U S A. 2007;104:15805–10. doi: 10.1073/pnas.0707628104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Olive V, Jiang I, He L. mir-17-92, a cluster of miRNAs in the midst of the cancer network. Int J Biochem Cell Biol. 2010;42:1348–54. doi: 10.1016/j.biocel.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hayashita Y, Osada H, Tatematsu Y, et al. A polycistronic microRNA cluster, miR-17-92, is overexpressed in human lung cancers and enhances cell proliferation. Cancer Res. 2005;65:9628–32. doi: 10.1158/0008-5472.CAN-05-2352. [DOI] [PubMed] [Google Scholar]
- 45.Lu Y, Okubo T, Rawlins E, Hogan BL. Epithelial progenitor cells of the embryonic lung and the role of microRNAs in their proliferation. Proc Am Thorac Soc. 2008;5:300–4. doi: 10.1513/pats.200710-162DR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu Y, Thomson JM, Wong HY, Hammond SM, Hogan BL. Transgenic over-expression of the microRNA miR-17-92 cluster promotes proliferation and inhibits differentiation of lung epithelial progenitor cells. Dev Biol. 2007;310:442–53. doi: 10.1016/j.ydbio.2007.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang Y, Weng T, Gou D, Chen Z, Chintagari NR, Liu L. Identification of rat lung-specific microRNAs by micoRNA microarray: valuable discoveries for the facilitation of lung research. BMC Genomics. 2007;8:29. doi: 10.1186/1471-2164-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams AE, Moschos SA, Perry MM, Barnes PJ, Lindsay MA. Maternally imprinted microRNAs are differentially expressed during mouse and human lung development. Dev Dyn. 2007;236:572–80. doi: 10.1002/dvdy.21047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Williams AE, Perry MM, Moschos SA, Lindsay MA. microRNA expression in the aging mouse lung. BMC Genomics. 2007;8:172. doi: 10.1186/1471-2164-8-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cosio M, Ghezzo H, Hogg JC, et al. The relations between structural changes in small airways and pulmonary-function tests. N Engl J Med. 1978;298:1277–81. doi: 10.1056/NEJM197806082982303. [DOI] [PubMed] [Google Scholar]
- 51.Saetta M, Ghezzo H, Kim WD, et al. Loss of alveolar attachments in smokers. A morphometric correlate of lung function impairment. Am Rev Respir Dis. 1985;132:894–900. doi: 10.1164/arrd.1985.132.4.894. [DOI] [PubMed] [Google Scholar]
- 52.Hogg JC, Chu F, Utokaparch S, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:2645–53. doi: 10.1056/NEJMoa032158. [DOI] [PubMed] [Google Scholar]
- 53.Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD) Lancet. 2004;364:613–20. doi: 10.1016/S0140-6736(04)16855-4. [DOI] [PubMed] [Google Scholar]
- 54.Hu G, Zhou Y, Tian J, et al. Risk of COPD from exposure to biomass smoke: a metaanalysis. Chest. 2010;138:20–31. doi: 10.1378/chest.08-2114. [DOI] [PubMed] [Google Scholar]
- 55.Shi W, Chen F, Cardoso WV. Mechanisms of lung development: contribution to adult lung disease and relevance to chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2009;6:558–63. doi: 10.1513/pats.200905-031RM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Adcock IM, Tsaprouni L, Bhavsar P, Ito K. Epigenetic regulation of airway inflammation. Curr Opin Immunol. 2007;19:694–700. doi: 10.1016/j.coi.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 57.De Flora S, Balansky R, D’Agostini F, et al. Smoke-induced microRNA and related proteome alterations. Modulation by chemopreventive agents. Int J Cancer. 2012;131:2763–73. doi: 10.1002/ijc.27814. [DOI] [PubMed] [Google Scholar]
- 58.Ezzie ME, Crawford M, Cho JH, et al. Gene expression networks in COPD: microRNA and mRNA regulation. Thorax. 2012;67:122–31. doi: 10.1136/thoraxjnl-2011-200089. [DOI] [PubMed] [Google Scholar]
- 59.Moschos SA, Williams AE, Perry MM, Birrell MA, Belvisi MG, Lindsay MA. Expression profiling in vivo demonstrates rapid changes in lung microRNA levels following lipopolysaccharide-induced inflammation but not in the anti-inflammatory action of glucocorticoids. BMC Genomics. 2007;8:240. doi: 10.1186/1471-2164-8-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hayashi H, Abdollah S, Qiu Y, et al. The MAD-related protein Smad7 associates with the TGFbeta receptor and functions as an antagonist of TGFbeta signaling. Cell. 1997;89:1165–73. doi: 10.1016/s0092-8674(00)80303-7. [DOI] [PubMed] [Google Scholar]
- 61.Hassan F, Nuovo GJ, Crawford M, et al. MiR-101 and miR-144 regulate the expression of the CFTR chloride channel in the lung. PLoS One. 2012;7:e50837. doi: 10.1371/journal.pone.0050837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Clunes LA, Davies CM, Coakley RD, et al. Cigarette smoke exposure induces CFTR internalization and insolubility, leading to airway surface liquid dehydration. FASEB J. 2012;26:533–45. doi: 10.1096/fj.11-192377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Graff JW, Powers LS, Dickson AM, et al. Cigarette Smoking Decreases Global MicroRNA Expression in Human Alveolar Macrophages. PLoS One. 2012;7:e44066. doi: 10.1371/journal.pone.0044066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hunninghake GM, Cho MH, Tesfaigzi Y, et al. MMP12, lung function, and COPD in high-risk populations. N Engl J Med. 2009;361:2599–608. doi: 10.1056/NEJMoa0904006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sato T, Liu X, Nelson A, et al. Reduced miR-146a increases prostaglandin E₂in chronic obstructive pulmonary disease fibroblasts. Am J Respir Crit Care Med. 2010;182:1020–9. doi: 10.1164/rccm.201001-0055OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huang SK, Wettlaufer SH, Chung J, Peters-Golden M. Prostaglandin E2 inhibits specific lung fibroblast functions via selective actions of PKA and Epac-1. Am J Respir Cell Mol Biol. 2008;39:482–9. doi: 10.1165/rcmb.2008-0080OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Akbas F, Coskunpinar E, Aynaci E, Oltulu YM, Yildiz P. Analysis of serum micro-RNAs as potential biomarker in chronic obstructive pulmonary disease. Exp Lung Res. 2012;38:286–94. doi: 10.3109/01902148.2012.689088. [DOI] [PubMed] [Google Scholar]
- 68.Leidinger P, Keller A, Borries A, et al. Specific peripheral miRNA profiles for distinguishing lung cancer from COPD. Lung Cancer. 2011;74:41–7. doi: 10.1016/j.lungcan.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 69.Sanfiorenzo C, Ilie MI, Belaid A, et al. Two Panels of Plasma MicroRNAs as Non-Invasive Biomarkers for Prediction of Recurrence in Resectable NSCLC. PLoS One. 2013;8:e54596. doi: 10.1371/journal.pone.0054596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Davies DE, Wicks J, Powell RM, Puddicombe SM, Holgate ST. Airway remodeling in asthma: new insights. J Allergy Clin Immunol. 2003;111:215–25. doi: 10.1067/mai.2003.128. quiz 26. [DOI] [PubMed] [Google Scholar]
- 71.Frieri M. Advances in the understanding of allergic asthma. Allergy Asthma Proc. 2007;28:614–9. doi: 10.2500/aap.2007.28.2952. [DOI] [PubMed] [Google Scholar]
- 72.Boxall C, Holgate ST, Davies DE. The contribution of transforming growth factor-beta and epidermal growth factor signalling to airway remodelling in chronic asthma. Eur Respir J. 2006;27:208–29. doi: 10.1183/09031936.06.00130004. [DOI] [PubMed] [Google Scholar]
- 73.Coutts A, Chen G, Stephens N, et al. Release of biologically active TGF-beta from airway smooth muscle cells induces autocrine synthesis of collagen. Am J Physiol Lung Cell Mol Physiol. 2001;280:L999–1008. doi: 10.1152/ajplung.2001.280.5.L999. [DOI] [PubMed] [Google Scholar]
- 74.Moir LM, Burgess JK, Black JL. Transforming growth factor beta 1 increases fibronectin deposition through integrin receptor alpha 5 beta 1 on human airway smooth muscle. J Allergy Clin Immunol. 2008;121:1034–9.e4. doi: 10.1016/j.jaci.2007.12.1159. [DOI] [PubMed] [Google Scholar]
- 75.Gregory LG, Mathie SA, Walker SA, Pegorier S, Jones CP, Lloyd CM. Overexpression of Smad2 drives house dust mite-mediated airway remodeling and airway hyperresponsiveness via activin and IL-25. Am J Respir Crit Care Med. 2010;182:143–54. doi: 10.1164/rccm.200905-0725OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lu TX, Hartner J, Lim EJ, et al. MicroRNA-21 limits in vivo immune response-mediated activation of the IL-12/IFN-gamma pathway, Th1 polarization, and the severity of delayed-type hypersensitivity. J Immunol. 2011;187:3362–73. doi: 10.4049/jimmunol.1101235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu G, Friggeri A, Yang Y, et al. miR-21 mediates fibrogenic activation of pulmonary fibroblasts and lung fibrosis. J Exp Med. 2010;207:1589–97. doi: 10.1084/jem.20100035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kumar M, Ahmad T, Sharma A, et al. Let-7 microRNA-mediated regulation of IL-13 and allergic airway inflammation. (e1-10).J Allergy Clin Immunol. 2011;128:1077–85. doi: 10.1016/j.jaci.2011.04.034. [DOI] [PubMed] [Google Scholar]
- 79.Collison A, Mattes J, Plank M, Foster PS. Inhibition of house dust mite-induced allergic airways disease by antagonism of microRNA-145 is comparable to glucocorticoid treatment. J Allergy Clin Immunol. 2011;128:160–7.e4. doi: 10.1016/j.jaci.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 80.Mattes J, Collison A, Plank M, Phipps S, Foster PS. Antagonism of microRNA-126 suppresses the effector function of TH2 cells and the development of allergic airways disease. Proc Natl Acad Sci U S A. 2009;106:18704–9. doi: 10.1073/pnas.0905063106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sharma A, Kumar M, Ahmad T, et al. Antagonism of mmu-mir-106a attenuates asthma features in allergic murine model. J Appl Physiol. 2012;113:459–64. doi: 10.1152/japplphysiol.00001.2012. [DOI] [PubMed] [Google Scholar]
- 82.McCoy CE, Sheedy FJ, Qualls JE, et al. IL-10 inhibits miR-155 induction by toll-like receptors. J Biol Chem. 2010;285:20492–8. doi: 10.1074/jbc.M110.102111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mayoral RJ, Deho L, Rusca N, et al. MiR-221 influences effector functions and actin cytoskeleton in mast cells. PLoS One. 2011;6:e26133. doi: 10.1371/journal.pone.0026133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Garbacki N, Di Valentin E, Huynh-Thu VA, et al. MicroRNAs profiling in murine models of acute and chronic asthma: a relationship with mRNAs targets. PLoS One. 2011;6:e16509. doi: 10.1371/journal.pone.0016509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Raemaekers T, Ribbeck K, Beaudouin J, et al. NuSAP, a novel microtubule-associated protein involved in mitotic spindle organization. J Cell Biol. 2003;162:1017–29. doi: 10.1083/jcb.200302129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Perry MM, Moschos SA, Williams AE, Shepherd NJ, Larner-Svensson HM, Lindsay MA. Rapid changes in microRNA-146a expression negatively regulate the IL-1beta-induced inflammatory response in human lung alveolar epithelial cells. J Immunol. 2008;180:5689–98. doi: 10.4049/jimmunol.180.8.5689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nahid MA, Pauley KM, Satoh M, Chan EK. miR-146a is critical for endotoxin-induced tolerance: IMPLICATION IN INNATE IMMUNITY. J Biol Chem. 2009;284:34590–9. doi: 10.1074/jbc.M109.056317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yang L, Boldin MP, Yu Y, et al. miR-146a controls the resolution of T cell responses in mice. J Exp Med. 2012;209:1655–70. doi: 10.1084/jem.20112218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lee CG, Link H, Baluk P, et al. Vascular endothelial growth factor (VEGF) induces remodeling and enhances TH2-mediated sensitization and inflammation in the lung. Nat Med. 2004;10:1095–103. doi: 10.1038/nm1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lee CG, Ma B, Takyar S, et al. Studies of vascular endothelial growth factor in asthma and chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2011;8:512–5. doi: 10.1513/pats.201102-018MW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Capetandes A, Zhuang M, Haque FN, Xie L, Frieri M. Vascular endothelial growth factor is increased by human pulmonary cells stimulated with Dermatophagoides sp. extract. Allergy Asthma Proc. 2007;28:324–30. doi: 10.2500/aap.2007.28.2999. [DOI] [PubMed] [Google Scholar]
- 92.Capetandes A, Horne NS, Frieri M. Dermatophagoides extract-treated confluent type II epithelial cells (cA549) and human lung mesenchymal cell growth. Ann Allergy Asthma Immunol. 2005;95:381–8. doi: 10.1016/S1081-1206(10)61157-X. [DOI] [PubMed] [Google Scholar]
- 93.Puxeddu I, Ribatti D, Crivellato E, Levi-Schaffer F. Mast cells and eosinophils: a novel link between inflammation and angiogenesis in allergic diseases. J Allergy Clin Immunol. 2005;116:531–6. doi: 10.1016/j.jaci.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 94.Song C, Ma H, Yao C, Tao X, Gan H. Alveolar macrophage-derived vascular endothelial growth factor contributes to allergic airway inflammation in a mouse asthma model. Scand J Immunol. 2012;75:599–605. doi: 10.1111/j.1365-3083.2012.02693.x. [DOI] [PubMed] [Google Scholar]
- 95.Sun X, Icli B, Wara AK, et al. MicroRNA-181b regulates NF-κB-mediated vascular inflammation. J Clin Invest. 2012;122:1973–90. doi: 10.1172/JCI61495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Riordan JR, Rommens JM, Kerem B, et al. Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA. Science. 1989;245:1066–73. doi: 10.1126/science.2475911. [DOI] [PubMed] [Google Scholar]
- 97.Ratjen F. What's new in CF airway inflammation: an update. Paediatr Respir Rev. 2006;7(Suppl 1):S70–2. doi: 10.1016/j.prrv.2006.04.170. [DOI] [PubMed] [Google Scholar]
- 98.Mall MA. Role of cilia, mucus, and airway surface liquid in mucociliary dysfunction: lessons from mouse models. J Aerosol Med Pulm Drug Deliv. 2008;21:13–24. doi: 10.1089/jamp.2007.0659. [DOI] [PubMed] [Google Scholar]
- 99.Worlitzsch D, Tarran R, Ulrich M, et al. Effects of reduced mucus oxygen concentration in airway Pseudomonas infections of cystic fibrosis patients. J Clin Invest. 2002;109:317–25. doi: 10.1172/JCI13870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Oglesby IK, Bray IM, Chotirmall SH, et al. miR-126 is downregulated in cystic fibrosis airway epithelial cells and regulates TOM1 expression. J Immunol. 2010;184:1702–9. doi: 10.4049/jimmunol.0902669. [DOI] [PubMed] [Google Scholar]
- 101.Katoh Y, Shiba Y, Mitsuhashi H, Yanagida Y, Takatsu H, Nakayama K. Tollip and Tom1 form a complex and recruit ubiquitin-conjugated proteins onto early endosomes. J Biol Chem. 2004;279:24435–43. doi: 10.1074/jbc.M400059200. [DOI] [PubMed] [Google Scholar]
- 102.Yamakami M, Yokosawa H. Tom1 (target of Myb 1) is a novel negative regulator of interleukin-1- and tumor necrosis factor-induced signaling pathways. Biol Pharm Bull. 2004;27:564–6. doi: 10.1248/bpb.27.564. [DOI] [PubMed] [Google Scholar]
- 103.Megiorni F, Cialfi S, Dominici C, Quattrucci S, Pizzuti A. Synergistic post-transcriptional regulation of the Cystic Fibrosis Transmembrane conductance Regulator (CFTR) by miR-101 and miR-494 specific binding. PLoS One. 2011;6:e26601. doi: 10.1371/journal.pone.0026601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jardim MJ, Fry RC, Jaspers I, Dailey L, Diaz-Sanchez D. Disruption of microRNA expression in human airway cells by diesel exhaust particles is linked to tumorigenesis-associated pathways. Environ Health Perspect. 2009;117:1745–51. doi: 10.1289/ehp.0900756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Duan H, Jiang Y, Zhang H, Wu Y. MiR-320 and miR-494 affect cell cycles of primary murine bronchial epithelial cells exposed to benzo[a ] pyrene. Toxicol In Vitro. 2010;24:928–35. doi: 10.1016/j.tiv.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 106.Zhu QY, Liu Q, Chen JX, Lan K, Ge BX. MicroRNA-101 targets MAPK phosphatase-1 to regulate the activation of MAPKs in macrophages. J Immunol. 2010;185:7435–42. doi: 10.4049/jimmunol.1000798. [DOI] [PubMed] [Google Scholar]
- 107.Bhattacharyya S, Balakathiresan NS, Dalgard C, et al. Elevated miR-155 promotes inflammation in cystic fibrosis by driving hyperexpression of interleukin-8. J Biol Chem. 2011;286:11604–15. doi: 10.1074/jbc.M110.198390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Xie C, Jiang XH, Zhang JT, et al. CFTR suppresses tumor progression through miR-193b targeting urokinase plasminogen activator (uPA) in prostate cancer. Oncogene. 2012 doi: 10.1038/onc.2012.251. [DOI] [PubMed] [Google Scholar]
- 109.McMahon B, Kwaan HC. The plasminogen activator system and cancer. Pathophysiol Haemost Thromb. 2008;36:184–94. doi: 10.1159/000175156. [DOI] [PubMed] [Google Scholar]
- 110.Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Baumgartner KB, Samet JM, Coultas DB, et al. Occupational and environmental risk factors for idiopathic pulmonary fibrosis: a multicenter case-control study. Collaborating Centers. Am J Epidemiol. 2000;152:307–15. doi: 10.1093/aje/152.4.307. [DOI] [PubMed] [Google Scholar]
- 112.Samara KD, Margaritopoulos G, Wells AU, Siafakas NM, Antoniou KM. Smoking and pulmonary fibrosis: novel insights. Pulm Med 2011. 2011 doi: 10.1155/2011/461439. 461439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fernandez IE, Eickelberg O. New cellular and molecular mechanisms of lung injury and fibrosis in idiopathic pulmonary fibrosis. Lancet. 2012;380:680–8. doi: 10.1016/S0140-6736(12)61144-1. [DOI] [PubMed] [Google Scholar]
- 114.Selman M, Pardo A, Kaminski N. Idiopathic pulmonary fibrosis: aberrant recapitulation of developmental programs? PLoS Med. 2008;5:e62. doi: 10.1371/journal.pmed.0050062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Xu YD, Hua J, Mui A, O’Connor R, Grotendorst G, Khalil N. Release of biologically active TGF-beta1 by alveolar epithelial cells results in pulmonary fibrosis. Am J Physiol Lung Cell Mol Physiol. 2003;285:L527–39. doi: 10.1152/ajplung.00298.2002. [DOI] [PubMed] [Google Scholar]
- 116.Fabian SL, Penchev RR, St-Jacques B, et al. Hedgehog-Gli pathway activation during kidney fibrosis. Am J Pathol. 2012;180:1441–53. doi: 10.1016/j.ajpath.2011.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Willis BC, Borok Z. TGF-beta-induced EMT: mechanisms and implications for fibrotic lung disease. Am J Physiol Lung Cell Mol Physiol. 2007;293:L525–34. doi: 10.1152/ajplung.00163.2007. [DOI] [PubMed] [Google Scholar]
- 118.Kim KK, Kugler MC, Wolters PJ, et al. Alveolar epithelial cell mesenchymal transition develops in vivo during pulmonary fibrosis and is regulated by the extracellular matrix. Proc Natl Acad Sci U S A. 2006;103:13180–5. doi: 10.1073/pnas.0605669103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kondo Y, Higa-Nakamine S, Noguchi N, et al. Induction of epithelial-mesenchymal transition by flagellin in cultured lung epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2012 doi: 10.1152/ajplung.00096.2012. [DOI] [PubMed] [Google Scholar]
- 120.Pandit KV, Corcoran D, Yousef H, et al. Inhibition and role of let-7d in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2010;182:220–9. doi: 10.1164/rccm.200911-1698OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Boon K, Bailey NW, Yang J, et al. Molecular phenotypes distinguish patients with relatively stable from progressive idiopathic pulmonary fibrosis (IPF) PLoS One. 2009;4:e5134. doi: 10.1371/journal.pone.0005134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Oak SR, Murray L, Herath A, et al. A micro RNA processing defect in rapidly progressing idiopathic pulmonary fibrosis. PLoS One. 2011;6:e21253. doi: 10.1371/journal.pone.0021253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Milosevic J, Pandit K, Magister M, et al. Profibrotic Role of miR-154 in Pulmonary Fibrosis. Am J Respir Cell Mol Biol. 2012 doi: 10.1165/rcmb.2011-0377OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Cushing L, Kuang PP, Qian J, et al. miR-29 is a major regulator of genes associated with pulmonary fibrosis. Am J Respir Cell Mol Biol. 2011;45:287–94. doi: 10.1165/rcmb.2010-0323OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Deng Z, Morse JH, Slager SL, et al. Familial primary pulmonary hypertension (gene PPH1) is caused by mutations in the bone morphogenetic protein receptor-II gene. Am J Hum Genet. 2000;67:737–44. doi: 10.1086/303059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Trembath RC, Thomson JR, Machado RD, et al. Clinical and molecular genetic features of pulmonary hypertension in patients with hereditary hemorrhagic telangiectasia. N Engl J Med. 2001;345:325–34. doi: 10.1056/NEJM200108023450503. [DOI] [PubMed] [Google Scholar]
- 127.Hagen M, Fagan K, Steudel W, et al. Interaction of interleukin-6 and the BMP pathway in pulmonary smooth muscle. Am J Physiol Lung Cell Mol Physiol. 2007;292:L1473–9. doi: 10.1152/ajplung.00197.2006. [DOI] [PubMed] [Google Scholar]
- 128.Wu X, Chang MS, Mitsialis SA, Kourembanas S. Hypoxia regulates bone morphogenetic protein signaling through C-terminal-binding protein 1. Circ Res. 2006;99:240–7. doi: 10.1161/01.RES.0000237021.65103.24. [DOI] [PubMed] [Google Scholar]
- 129.Li X, Zhang X, Leathers R, et al. Notch3 signaling promotes the development of pulmonary arterial hypertension. Nat Med. 2009;15:1289–97. doi: 10.1038/nm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Long L, Crosby A, Yang X, et al. Altered bone morphogenetic protein and transforming growth factor-beta signaling in rat models of pulmonary hypertension: potential for activin receptor-like kinase-5 inhibition in prevention and progression of disease. Circulation. 2009;119:566–76. doi: 10.1161/CIRCULATIONAHA.108.821504. [DOI] [PubMed] [Google Scholar]
- 131.Brock M, Trenkmann M, Gay RE, et al. Interleukin-6 modulates the expression of the bone morphogenic protein receptor type II through a novel STAT3-microRNA cluster 17/92 pathway. Circ Res. 2009;104:1184–91. doi: 10.1161/CIRCRESAHA.109.197491. [DOI] [PubMed] [Google Scholar]
- 132.Caruso P, MacLean MR, Khanin R, et al. Dynamic changes in lung microRNA profiles during the development of pulmonary hypertension due to chronic hypoxia and monocrotaline. Arterioscler Thromb Vasc Biol. 2010;30:716–23. doi: 10.1161/ATVBAHA.109.202028. [DOI] [PubMed] [Google Scholar]
- 133.Nicolls MR, Voelkel NF. Hypoxia and the lung: beyond hypoxic vasoconstriction. Antioxid Redox Signal. 2007;9:741–3. doi: 10.1089/ars.2007.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bauer NR, Moore TM, McMurtry IF. Rodent models of PAH: are we there yet? Am J Physiol Lung Cell Mol Physiol. 2007;293:L580–2. doi: 10.1152/ajplung.00281.2007. [DOI] [PubMed] [Google Scholar]
- 135.Rhodes CJ, Wharton J, Boon RA, et al. Reduced miR-150 is Associated with Poor Survival in Pulmonary Arterial Hypertension. Am J Respir Crit Care Med. 2012 doi: 10.1164/rccm.201205-0839OC. [DOI] [PubMed] [Google Scholar]
- 136.Loffler D, Brocke-Heidrich K, Pfeifer G, et al. Interleukin-6 dependent survival of multiple myeloma cells involves the Stat3-mediated induction of microRNA-21 through a highly conserved enhancer. Blood. 2007;110:1330–3. doi: 10.1182/blood-2007-03-081133. [DOI] [PubMed] [Google Scholar]
- 137.Davis BN, Hilyard AC, Lagna G, Hata A. SMAD proteins control DROSHA-mediated microRNA maturation. Nature. 2008;454:56–61. doi: 10.1038/nature07086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Connolly MJ, Aaronson PI. Key role of the RhoA/Rho kinase system in pulmonary hypertension. Pulm Pharmacol Ther. 2011;24:1–14. doi: 10.1016/j.pupt.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 139.Parikh VN, Jin RC, Rabello S, et al. MicroRNA-21 integrates pathogenic signaling to control pulmonary hypertension: results of a network bioinformatics approach. Circulation. 2012;125:1520–32. doi: 10.1161/CIRCULATIONAHA.111.060269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yang S, Banerjee S, Freitas A, et al. miR-21 regulates chronic hypoxia-induced pulmonary vascular remodeling. Am J Physiol Lung Cell Mol Physiol. 2012;302:L521–9. doi: 10.1152/ajplung.00316.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Courboulin A, Paulin R, Giguère NJ, et al. Role for miR-204 in human pulmonary arterial hypertension. J Exp Med. 2011;208:535–48. doi: 10.1084/jem.20101812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Turner DP, Findlay VJ, Moussa O, et al. Mechanisms and functional consequences of PDEF protein expression loss during prostate cancer progression. Prostate. 2011;71:1723–35. doi: 10.1002/pros.21389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Wang FE, Zhang C, Maminishkis A, et al. MicroRNA-204/211 alters epithelial physiology. FASEB J. 2010;24:1552–71. doi: 10.1096/fj.08-125856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Drake KM, Zygmunt D, Mavrakis L, et al. Altered MicroRNA processing in heritable pulmonary arterial hypertension: an important role for Smad-8. Am J Respir Crit Care Med. 2011;184:1400–8. doi: 10.1164/rccm.201106-1130OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shintani M, Yagi H, Nakayama T, Saji T, Matsuoka R. A new nonsense mutation of SMAD8 associated with pulmonary arterial hypertension. J Med Genet. 2009;46:331–7. doi: 10.1136/jmg.2008.062703. [DOI] [PubMed] [Google Scholar]
- 146.Pullamsetti SS, Doebele C, Fischer A, et al. Inhibition of microRNA-17 improves lung and heart function in experimental pulmonary hypertension. Am J Respir Crit Care Med. 2012;185:409–19. doi: 10.1164/rccm.201106-1093OC. [DOI] [PubMed] [Google Scholar]
- 147.Gou D, Ramchandran R, Peng X, et al. miR-210 has an antiapoptotic effect in pulmonary artery smooth muscle cells during hypoxia. Am J Physiol Lung Cell Mol Physiol. 2012;303:L682–91. doi: 10.1152/ajplung.00344.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Chan SY, Zhang YY, Hemann C, Mahoney CE, Zweier JL, Loscalzo J. MicroRNA-210 controls mitochondrial metabolism during hypoxia by repressing the iron-sulfur cluster assembly proteins ISCU1/2. Cell Metab. 2009;10:273–84. doi: 10.1016/j.cmet.2009.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lee C, Mitsialis SA, Aslam M, et al. Exosomes mediate the cytoprotective action of mesenchymal stromal cells on hypoxia-induced pulmonary hypertension. Circulation. 2012;126:2601–11. doi: 10.1161/CIRCULATIONAHA.112.114173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Baber SR, Deng W, Master RG, et al. Intratracheal mesenchymal stem cell administration attenuates monocrotaline-induced pulmonary hypertension and endothelial dysfunction. Am J Physiol Heart Circ Physiol. 2007;292:H1120–8. doi: 10.1152/ajpheart.00173.2006. [DOI] [PubMed] [Google Scholar]
- 151.Hansmann G, Fernandez-Gonzalez A, Aslam M, et al. Mesenchymal stem cell-mediated reversal of bronchopulmonary dysplasia and associated pulmonary hypertension. Pulm Circ. 2012;2:170–81. doi: 10.4103/2045-8932.97603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Lee JW, Fang X, Krasnodembskaya A, Howard JP, Matthay MA. Concise review: Mesenchymal stem cells for acute lung injury: role of paracrine soluble factors. Stem Cells. 2011;29:913–9. doi: 10.1002/stem.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Paulin R, Courboulin A, Meloche J, et al. Signal transducers and activators of transcription-3/pim1 axis plays a critical role in the pathogenesis of human pulmonary arterial hypertension. Circulation. 2011;123:1205–15. doi: 10.1161/CIRCULATIONAHA.110.963314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Chen X, Yan Q, Li S, et al. Expression of the tumor suppressor miR-206 is associated with cellular proliferative inhibition and impairs invasion in ERα-positive endometrioid adenocarcinoma. Cancer Lett. 2012;314:41–53. doi: 10.1016/j.canlet.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 155.Davis-Dusenbery BN, Chan MC, Reno KE, et al. down-regulation of Kruppel-like factor-4 (KLF4) by microRNA-143/145 is critical for modulation of vascular smooth muscle cell phenotype by transforming growth factor-beta and bone morphogenetic protein 4. J Biol Chem. 2011;286:28097–110. doi: 10.1074/jbc.M111.236950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Elia L, Quintavalle M, Zhang J, et al. The knockout of miR-143 and -145 alters smooth muscle cell maintenance and vascular homeostasis in mice: correlates with human disease. Cell Death Differ. 2009;16:1590–8. doi: 10.1038/cdd.2009.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Caruso P, Dempsie Y, Stevens HC, et al. A role for miR-145 in pulmonary arterial hypertension: evidence from mouse models and patient samples. Circ Res. 2012;111:290–300. doi: 10.1161/CIRCRESAHA.112.267591. [DOI] [PubMed] [Google Scholar]
- 158.Cheng Y, Liu X, Yang J, et al. MicroRNA-145, a novel smooth muscle cell phenotypic marker and modulator, controls vascular neointimal lesion formation. Circ Res. 2009;105:158–66. doi: 10.1161/CIRCRESAHA.109.197517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Xin M, Small EM, Sutherland LB, et al. MicroRNAs miR-143 and miR-145 modulate cytoskeletal dynamics and responsiveness of smooth muscle cells to injury. Genes Dev. 2009;23:2166–78. doi: 10.1101/gad.1842409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Cordes KR, Sheehy NT, White MP, et al. miR-145 and miR-143 regulate smooth muscle cell fate and plasticity. Nature. 2009;460:705–10. doi: 10.1038/nature08195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bockmeyer CL, Maegel L, Janciauskiene S, et al. Plexiform vasculopathy of severe pulmonary arterial hypertension and microRNA expression. J Heart Lung Transplant. 2012;31:764–72. doi: 10.1016/j.healun.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 162.Wang S, Aurora AB, Johnson BA, et al. The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev Cell. 2008;15:261–71. doi: 10.1016/j.devcel.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Jonigk D, Golpon H, Bockmeyer CL, et al. Plexiform lesions in pulmonary arterial hypertension composition, architecture, and microenvironment. Am J Pathol. 2011;179:167–79. doi: 10.1016/j.ajpath.2011.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Erickson SE, Martin GS, Davis JL, Matthay MA, Eisner MD, Network NNA. Recent trends in acute lung injury mortality: 1996-2005. Crit Care Med. 2009;37:1574–9. doi: 10.1097/CCM.0b013e31819fefdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Johnson ER, Matthay MA. Acute lung injury: epidemiology, pathogenesis, and treatment. J Aerosol Med Pulm Drug Deliv. 2010;23:243–52. doi: 10.1089/jamp.2009.0775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Peters JH, Grote MN, Lane NE, Maunder RJ. Changes in plasma fibronectin isoform levels predict distinct clinical outcomes in critically ill patients. Biomark Insights. 2011;6:59–68. doi: 10.4137/BMI.S7204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Meyer NJ, Huang Y, Singleton PA, et al. GADD45a is a novel candidate gene in inflammatory lung injury via influences on Akt signaling. FASEB J. 2009;23:1325–37. doi: 10.1096/fj.08-119073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Meyer NJ, Li M, Feng R, et al. ANGPT2 genetic variant is associated with trauma-associated acute lung injury and altered plasma angiopoietin-2 isoform ratio. Am J Respir Crit Care Med. 2011;183:1344–53. doi: 10.1164/rccm.201005-0701OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Zhou T, Garcia JG, Zhang W. Integrating microRNAs into a system biology approach to acute lung injury. Transl Res. 2011;157:180–90. doi: 10.1016/j.trsl.2011.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Vaporidi K, Vergadi E, Kaniaris E, et al. Pulmonary microRNA profiling in a mouse model of ventilator-induced lung injury. Am J Physiol Lung Cell Mol Physiol. 2012;303:L199–207. doi: 10.1152/ajplung.00370.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Yehya N, Yerrapureddy A, Tobias J, Margulies SS. MicroRNA modulate alveolar epithelial response to cyclic stretch. BMC Genomics. 2012;13:154. doi: 10.1186/1471-2164-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Xie T, Liang J, Guo R, Liu N, Noble PW, Jiang D. Comprehensive microRNA analysis in bleomycin-induced pulmonary fibrosis identifies multiple sites of molecular regulation. Physiol Genomics. 2011;43:479–87. doi: 10.1152/physiolgenomics.00222.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Xie T, Liang J, Liu N, et al. MicroRNA-127 inhibits lung inflammation by targeting IgG Fcγ receptor I. J Immunol. 2012;188:2437–44. doi: 10.4049/jimmunol.1101070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Tamarapu Parthasarathy P, Galam L, Huynh B, et al. MicroRNA 16 modulates epithelial sodium channel in human alveolar epithelial cells. Biochem Biophys Res Commun. 2012;426:203–8. doi: 10.1016/j.bbrc.2012.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Goolaerts A, Roux J, Ganter MT, et al. Serotonin decreases alveolar epithelial fluid transport via a direct inhibition of the epithelial sodium channel. Am J Respir Cell Mol Biol. 2010;43:99–108. doi: 10.1165/rcmb.2008-0472OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Baudry A, Mouillet-Richard S, Schneider B, Launay JM, Kellermann O. miR-16 targets the serotonin transporter: a new facet for adaptive responses to antidepressants. Science. 2010;329:1537–41. doi: 10.1126/science.1193692. [DOI] [PubMed] [Google Scholar]
- 177.Mendell JT, Olson EN. MicroRNAs in stress signaling and human disease. Cell. 2012;148:1172–87. doi: 10.1016/j.cell.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Krützfeldt J, Rajewsky N, Braich R, et al. Silencing of microRNAs in vivo with ‘antagomirs’. Nature. 2005;438:685–9. doi: 10.1038/nature04303. [DOI] [PubMed] [Google Scholar]
- 179.Krützfeldt J, Kuwajima S, Braich R, et al. Specificity, duplex degradation and subcellular localization of antagomirs. Nucleic Acids Res. 2007;35:2885–92. doi: 10.1093/nar/gkm024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Rayner KJ, Esau CC, Hussain FN, et al. Inhibition of miR-33a/b in non-human primates raises plasma HDL and lowers VLDL triglycerides. Nature. 2011;478:404–7. doi: 10.1038/nature10486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Carè A, Catalucci D, Felicetti F, et al. MicroRNA-133 controls cardiac hypertrophy. Nat Med. 2007;13:613–8. doi: 10.1038/nm1582. [DOI] [PubMed] [Google Scholar]
- 182.Thum T, Gross C, Fiedler J, et al. MicroRNA-21 contributes to myocardial disease by stimulating MAP kinase signalling in fibroblasts. Nature. 2008;456:980–4. doi: 10.1038/nature07511. [DOI] [PubMed] [Google Scholar]
- 183.Zhong X, Chung AC, Chen HY, et al. miR-21 is a key therapeutic target for renal injury in a mouse model of type 2 diabetes. Diabetologia. 2013;56:663–74. doi: 10.1007/s00125-012-2804-x. [DOI] [PubMed] [Google Scholar]
- 184.Kota J, Chivukula RR, O’Donnell KA, et al. Therapeutic microRNA delivery suppresses tumorigenesis in a murine liver cancer model. Cell. 2009;137:1005–17. doi: 10.1016/j.cell.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Xiao J, Meng XM, Huang XR, et al. miR-29 inhibits bleomycin-induced pulmonary fibrosis in mice. Mol Ther. 2012;20:1251–60. doi: 10.1038/mt.2012.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Liu H, Liu L, Fletcher BS, Visner GA. Sleeping Beauty-based gene therapy with indoleamine 2,3-dioxygenase inhibits lung allograft fibrosis. FASEB J. 2006;20:2384–6. doi: 10.1096/fj.06-6228fje. [DOI] [PubMed] [Google Scholar]
- 187.Huang X, Guo H, Kang J, et al. Sleeping Beauty transposon-mediated engineering of human primary T cells for therapy of CD19+ lymphoid malignancies. Mol Ther. 2008;16:580–9. doi: 10.1038/sj.mt.6300404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Aronovich EL, McIvor RS, Hackett PB. The Sleeping Beauty transposon system: a non-viral vector for gene therapy. Hum Mol Genet. 2011;20:R14–20. doi: 10.1093/hmg/ddr140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Li B, Yang L, Shen J, Wang C, Jiang Z. The antiproliferative effect of sildenafil on pulmonary artery smooth muscle cells is mediated via upregulation of mitogen-activated protein kinase phosphatase-1 and degradation of extracellular signal-regulated kinase 1/2 phosphorylation. Anesth Analg. 2007;105:1034–41. doi: 10.1213/01.ane.0000278736.81133.26. table of contents. [DOI] [PubMed] [Google Scholar]
- 190.Henry SP, Beattie G, Yeh G, et al. Complement activation is responsible for acute toxicities in rhesus monkeys treated with a phosphorothioate oligodeoxynucleotide. Int Immunopharmacol. 2002;2:1657–66. doi: 10.1016/s1567-5769(02)00142-x. [DOI] [PubMed] [Google Scholar]
- 191.Schembri F, Sridhar S, Perdomo C, et al. MicroRNAs as modulators of smoking-induced gene expression changes in human airway epithelium. Proc Natl Acad Sci U S A. 2009;106:2319–24. doi: 10.1073/pnas.0806383106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Feng MJ, Shi F, Qiu C, Peng WK. MicroRNA-181a, -146a and -146b in spleen CD4+ T lymphocytes play proinflammatory roles in a murine model of asthma. Int Immunopharmacol. 2012;13:347–53. doi: 10.1016/j.intimp.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 193.Zheng Y, Xiong S, Jiang P, et al. Glucocorticoids inhibit lipopolysaccharide-mediated inflammatory response by downregulating microRNA-155: a novel anti-inflammation mechanism. Free Radic Biol Med. 2012;52:1307–17. doi: 10.1016/j.freeradbiomed.2012.01.031. [DOI] [PubMed] [Google Scholar]
- 194.Chiba Y, Tanabe M, Goto K, Sakai H, Misawa M. Down-regulation of miR-133a contributes to up-regulation of Rhoa in bronchial smooth muscle cells. Am J Respir Crit Care Med. 2009;180:713–9. doi: 10.1164/rccm.200903-0325OC. [DOI] [PubMed] [Google Scholar]
- 195.Pottier N, Maurin T, Chevalier B, et al. Identification of keratinocyte growth factor as a target of microRNA-155 in lung fibroblasts: implication in epithelial-mesenchymal interactions. PLoS One. 2009;4:e6718. doi: 10.1371/journal.pone.0006718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Ramachandran S, Karp PH, Jiang P, et al. A microRNA network regulates expression and biosynthesis of wild-type and DeltaF508 mutant cystic fibrosis transmembrane conductance regulator. Proc Natl Acad Sci U S A. 2012;109:13362–7. doi: 10.1073/pnas.1210906109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Jalali S, Ramanathan GK, Parthasarathy PT, et al. Mir-206 regulates pulmonary artery smooth muscle cell proliferation and differentiation. PLoS One. 2012;7:e46808. doi: 10.1371/journal.pone.0046808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Kim J, Kang Y, Kojima Y, et al. An endothelial apelin-FGF link mediated by miR-424 and miR-503 is disrupted in pulmonary arterial hypertension. Nat Med. 2012 doi: 10.1038/nm.3040. [DOI] [PMC free article] [PubMed] [Google Scholar]


