Abstract
Injection site abscess is an iatrogenic infection. Intramuscular (IM) injection is a common route to administer medication. Microorganisms known to cause injection site abscess are Staphylococcus aureus, Pseudomonas, Klebsiella, Escherichia coli commonly, Atypical mycobacteria, Clostridium species rarely. Gas gangrene is a necrotic infection of soft tissue with high mortality, often necessitating amputation in order to control the infection. Here, presenting a case of gas gangrene in a 19-year-old healthy male, who developed a life-threatening infection after IM injection of sodium diclofenac. Prompt clinical diagnosis, laboratory support, and timely surgical intervention saved the patient's life.
Keywords: Clostridium welchii, gas gangrene, intramuscular injection
INTRODUCTION
Gas gangrene is seen after road accidents or battlefield. In hospitals, danger of gas gangrene occurring postoperatively is recognized, but following intramuscular (IM) injection is rare.[1] Clostridium species is a large intestine commensal and widely distributed in the perianal region and lower limb.[1] Before administering an injection, skin is cleaned with alcohol, which removes only the vegetative bacteria but not the spore form.[2] Two essential factors for gas gangrene are implantation of spores and lowered oxygen tension for germination and growth. Traumatic or postoperative gas gangrene accounts for 70% of the cases, followed by spontaneous or nontraumatic gangrene.[3]
CASE REPORT
A 19-year-old male, presented to our hospital in September 2008, with severe pain in the right gluteal region. He gave the history of receiving an IM injection- diclofenac sodium from a local practitioner for viral fever and body ache. Within 7-8 h of receiving the injection, pain increased in intensity and radiated toward thigh, by 10-12 h he developed fever and pain increased in severity. He also had difficulty in walking. With the above features, he visited our hospital emergency department. On examination, patient had diffuse swelling with signs of inflammation in the upper posterior aspect of gluteal region there was no hematoma or local tissue damage and patient was febrile (102°F). Systemic examination was normal without other toxic symptoms at the time of admission. Various investigations showed Hb %-11g%, total WBC count-11,400 cells/mm3, Differential count-neutrophil-75%, lyphocytes-20%, monocyte-3%, and eosinophil-2%, ESR-35 mm/h. The diagnosis was injection site abscess and treated with systemic antibiotics (cephalosporin group) and antipyretics.
Within 24 h, patient developed toxic symptoms and had difficulty in moving the limb. Signs of inflammation spread to the lateral part of the thigh. On palpation, crepitus was present. Immediately X-ray of the part was taken which showed gas-filled sac near right hip joint [Figure 1]. Patient was immediately shifted to operation theater and wound debridement was done. Tissue bits were sent for Gram's stain and anerobic culture. Gram's stain revealed plenty of thick, Gram positive bacilli, and very few pus cells. Culture on Robertson's cooked meat media showed abundant gas which was foul smelling. Growth on neomycin blood agar showed grey colonies with swarming. Growth on egg yolk media showed opalescence around the colony. Nagler's reaction was positive which confirmed the organism as C. welchii.
Figure 1.
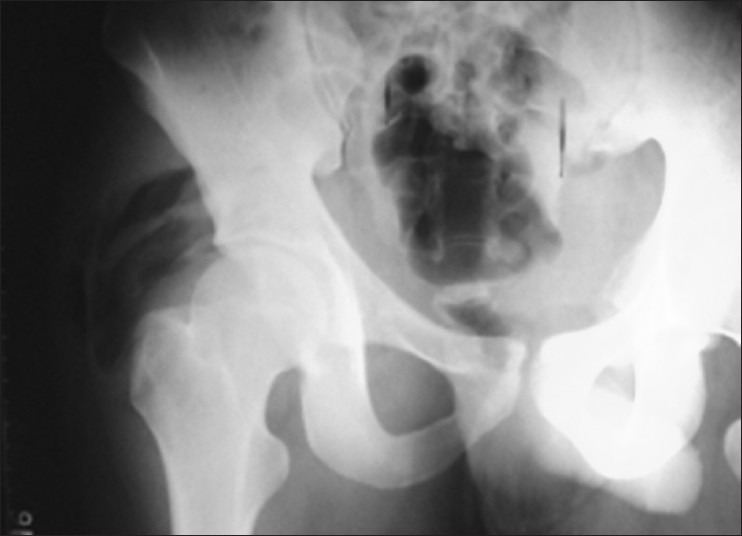
X-ray pelvis anterior posterior view shows evidence of IM gas lucencies, with soft tissue edema in the right gluteal region. No bone involvement
Postoperatively patient was started on systemic penicillin, ceftazidime, and metronidazole. Temperature and other vitals were regularly recorded which came to normal by the 8 postoperative day. Patient's general condition gradually improved and range of lower limb movements resumed thereafter. Patient went back home walking at the end of 30 days.
DISCUSSION
Gas gangrene following IM injection is rare and seldom reported in literature. Clostridium spores are ubiquitous. Gas gangrene is a rapidly developing and spreading infection mediated by toxins released by Clostridium spp.[4] These infections most likely present with pain out of proportion to the clinical examination. The presence of crepitus can be a late and non specific sign, so the absence of this sign should not sway one from pursuing this diagnosis.[5]
Identifying the type of Clostridium helps predict mortality. With Cl. Septicum, it is approximately 63%, and 11% with Cl. welchii.[5] But there is no difference in clinical findings between these two Clostridial species infections. Most patients present with nonspecific findings such as fever, leukocytosis, and pain as seen in our case.[6] Cl. welchii myonecrosis usually occurs following trauma. Cases of myonecrosis have been reported following IM administration of adrenaline[1,7] Vitamin B 12.[8] In our case the source of Cl. welchii could have been the needle, syringe, contamination of the injected fluid or the patient's own skin. The typical incubation period for gas gangrene is short (i.e., <24 h), but incubation periods of 1 h to 6 weeks has also been reported.[9] In our patient, the symptoms started early that is, 6-7 h.
It should be remembered that even routine procedures like administration of IM injections can lead to dreaded complication like gas gangrene; hence, precautions should be taken for prompt diagnosis and treatment.
The development of central supply department and introduction of disposable sterilized syringes have greatly reduced the infections but no means eliminated the risk of infection which can be introduced by injection.[1]
ACKNOWLEDGEMENTS
Department of General Surgery, Vydehi Institute of Medical Sciences and Research Center, Bangalore for referring the patient
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Harvey PW, Purnell GV. Fatal case of gas gangrene associated with intramuscular injection. Br Med J. 1968;1:744–6. doi: 10.1136/bmj.1.5594.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubbo SD, Gardner JF. Intramuscular injection and gas gangrene. Br Med J. 1968:241–2. doi: 10.1136/bmj.2.5599.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aggelidakis J, Lasithiotakis K, Topalidou A, Koutroumpas J, Kouvidis G, Katonis P. Limb salvage after gas gangrene: A case report and review of the literature. World J Emerg Surg. 2011;6:28. doi: 10.1186/1749-7922-6-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zelić M, Kunišek L, Mendrila D, Gudelj M, Abram M, Uravić M. Endogenous gas gangrene after laparoscopic cholecystectomy. West Indian Med J. 2011;60:96. [PubMed] [Google Scholar]
- 5.Feldman MJ, Prosciak M, Maleki Z, Milner SM. Gas gangrene. J Surg Radiol. 2010;1:100–1. [Google Scholar]
- 6.Myers G, Ngoi SS, Cennerazzo W, Harris L, DeCosse JJ. Clostridial septicemia in an urban hospital. Surg Gynecol Obstet. 1992;174:291–6. [PubMed] [Google Scholar]
- 7.van Hook R, Vandevelde AG. Gas gangrene after intramuscular injection of epinephrine: Report of a fatal case. Ann Intern Med. 1975;83:669–70. doi: 10.7326/0003-4819-83-5-669. [DOI] [PubMed] [Google Scholar]
- 8.Peerapur BV, Mantur BG, Uppin BC, Patil AV. Gas gangrene following intramuscular injection of vitamin B-Complex: Report of a fatal case. Indian J Med Microbiol. 2002;20:169. [PubMed] [Google Scholar]
- 9.Hoi Ho. Gas Gangrene. [Last accessed on 2012 Mar 15]. Available from http://emedicine.medscape.com/article/217943-overview#a0104 .


