Abstract
Objectives
To report the incidence of lower urinary tract symptoms (LUTS) in a racially/ethnically and age-diverse U.S. population-based sample of men and women.
Methods
We conducted a prospective cohort study with 5-year follow-up. A stratified 2-stage cluster random sampling method was used to recruit 5,502 Boston residents aged 30–79 years of black, Hispanic, or white race/ethnicity; 4,144 individuals (1,610 men; 2,534 women) completed follow-up. The American Urological Association Symptom Index (AUASI) was used to define moderate-to-severe LUTS.
Results
Among the 3,301 men and women with no or mild LUTS at baseline, the 5-year incidence of moderate-to-severe LUTS (AUASI≥8) was 11.4% overall, and higher for women than men (13.9% vs. 8.5%, P=0.02). Although the incidence increased with age (P<0.001), it had a plateau among women between ages 50–70 years of age and then doubled to 35.0% among women ≥70 years. White men had a distinctly lower incidence (7%), compared to all other sex/race sub-groups (13%).
Conclusions
Approximately one in ten adults had newly developed LUTS at 5-year follow-up, with differences by sex and race/ethnicity, indicating greater occurrence of urological problems among black and Hispanic participants or women.
MeSH Keywords: Lower urinary tract symptoms, Voiding dysfunction, Benign prostatic hyperplasia, Urinary bladder, overactive, Epidemiology, Bladder Outlet Obstruction
Introduction
Approximately one in five adults report moderate-to-severe lower urinary tract symptoms (LUTS), which may include a constellation of urinary storage and voiding problems. LUTS has been shown to substantially decrease quality of life and is associated with various health conditions, including depression.1–5 The various symptoms included in the umbrella of LUTS, such as urgency, frequent urination, weak urinary stream, and urine leakage, have led to a scattering of epidemiological studies of prevalence and incidence, with various definitions for patient-reported outcomes and related risk factors. A limitation of the research to date is that the majority of studies focused primarily on urine leakage, included only women, and/or were conducted in European populations.6–10 One large recent study of LUTS incidence in the U.S included a largely uniform and Caucasian sample of male health professionals.11 None of the previously published longitudinal studies of LUTS have included both men and women of diverse ages and racial/ethnic backgrounds.
The objective of this report is to describe the new development (“incidence”) of general LUTS after a period of 5 years in a racially/ethnically diverse U.S. population-based sample of men and women.
Methods
Study Design and Population: The Boston Area Community Health (BACH) Survey
We conducted an observational prospective cohort study of men and women to assess the epidemiology of urologic symptoms in a racially/ethnically diverse population-based sample. The BACH Survey recruited a random sample of 5,502 residents (2,301 men, 3,201 women) aged 30–79 years from three racial/ethnic groups in Boston, MA. Participants completed an in-person interview at baseline (occurring between 2002 and 2005) and approximately 5 years later (2006–2010). A detailed report of the study’s methods has been published.12 All participants provided written informed consent. The study was approved by the New England Research Institutes’ Institutional Review Board.
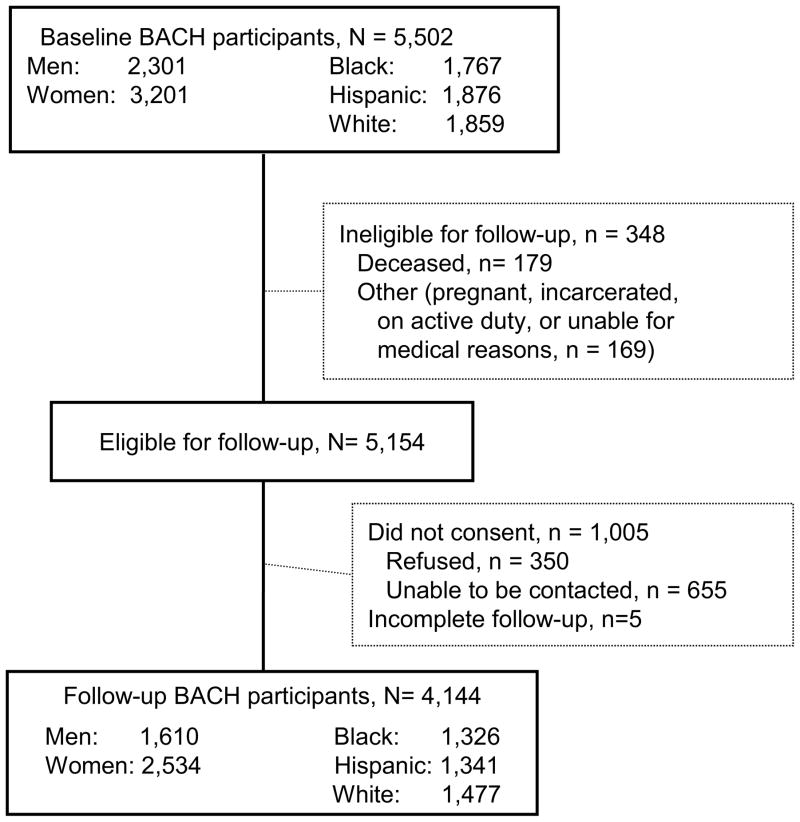
Completed follow-up interviews were obtained for 4,144 individuals (1,610 men; 2,534 women) from the 5,154 eligible, resulting in an overall response rate of 80.4% (Figure 1). Those lost to follow-up were mostly due to non-contact and were more likely to be Hispanic, >70 y old, and male gender, but there were no significant differences by presence/absence of LUTS at baseline.
Figure 1.
Boston Area Community Health (BACH) Survey Participation Flow
Measurement of Lower Urinary Tract Symptoms
During in-person interviews at both baseline and follow-up, LUTS was assessed by the validated English or Spanish versions of the American Urological Symptom Index (AUASI), also referred to as the International Prostate Symptom Score for men.13 The AUASI was originally developed and validated for benign prostatic hyperplasia in men,13 but has been validated14 and repeatedly shown to capture LUTS in women.1,15–18 Symptom severity is traditionally classified as: ≤7 points=none or mild; 8–20 points=moderate; and 20–35 points=severe. In addition to the primary outcome of total score, we also calculated the incidence of symptom type as voiding or storage. Voiding symptoms are measured by the AUASI with four questions regarding incomplete bladder emptying, intermittency, weak urinary stream, and hesitancy; a score ≥ 5 (of 20) indicates moderate-to-severe voiding symptoms. Storage symptoms are based on three AUASI questions assessing frequency, urgency, and nocturia; a score ≥ 4 (of 15) indicates moderate-to-severe storage symptoms. These subscales of voiding and storage symptoms have been shown to have internal consistency in both the BACH and other datasets.19
Statistical Analysis
Newly developed LUTS (herein referred to as “incidence”) was examined by restricting the analytic sample to men and women with no/mild LUTS at baseline (AUASI 0–7 points) and reporting the age-adjusted percentage who reported moderate-to-severe LUTS (8–35 points) at follow-up. The resulting sample size for the primary analyses was 3,301 participants (1,305 men, 1,996 women). For comparison with prior studies, we also examined the cut-point for higher severity LUTS of AUASI≥15 among those with AUASI≤7 at baseline.11,20 Sample sizes differed for the secondary analyses of voiding (N=3,657; 1,418 men, 2,240 women) or storage (N=2,752; 1,135 men, 1,616 women) symptoms, based on the exclusion of participants having had the symptom subtype present at baseline. Incidence estimates were calculated overall and by sex, 10-year age strata, and race/ethnicity. Odds ratios for incident LUTS were obtained using logistic regression models adjusted for sex, age, and race/ethnicity. Interactions between these variables were tested using cross-product terms in the model and by stratified analysis. Observations were weighted inversely to their probability of selection at baseline, adjusted for non-response bias at follow-up, and then post-stratified to the Boston census population in 2000. Multiple imputation based upon multivariate sequential regression was used to generate 15 complete datasets to account for missing values. No subjects were missing data on race/ethnicity, age, or gender and less than 1% of data on urologic symptoms was missing prior to imputation. The multiple imputation was performed in IVEware,21 and analyses were conducted in SAS v.9.3 (SAS Institute, Cary, NC) and SUDAAN v.11.0 (Research Triangle Park, NC).
Results
Demographic characteristics at baseline for the 3,301 men and women in the primary analytic sample are presented in Table 1. The mean (SD) time between the baseline and follow-up assessments was 4.8 (0.6) years. Table 2 presents data on incidence of moderate-to-severe LUTS, higher severity (AUASI ≥ 15) LUTS, voiding, and storage symptoms. Moderate-to-severe LUTS substantially increased with age for both men and women (P-trend<0.001), with an exception of a plateau among women aged 50–70 years. In contrast, incidence of higher severity LUTS remained less than 3% across all age groups (P=0.5), and actually decreased with increasing age among women (i.e., decreasing from 2.5% among age<40 y, to 0.3% among ages ≥70 y). The interactions between age and sex were not statistically significant (For AUASI>=8, Pintx=0.77; AUASI≥15, Pintx=0.26). The incidence of severe LUTS (AUASI ≥ 20) was less than 1% for both men and women. Voiding symptoms occurred most frequently among men aged 60–69 years, and were relatively uncommon among women until age 70 y. The incidence of storage symptoms increased with age among men, ranging from 15.7% for the youngest to 29.7% for the oldest age groups, but rose less drastically with age among women.
Table 1.
Unweighted Baseline (2002–2005) Age and Racial/Ethnic Distribution of Men and Women with No/Mild LUTS at Baseline
| Total (N=3,301) | Male (n=1,305) | Female (n=1,996) | |
|---|---|---|---|
| Age, mean (SE) years | 49.4 (0.3) | 48.4 (0.4) | 50.1 (0.4) |
| Age category, % | |||
| <40 y | 27.5 | 28.8 | 26.7 |
| 40–49 y | 27.6 | 30.7 | 25.5 |
| 50–59 y | 23.4 | 22.0 | 24.4 |
| 60–69 y | 15.2 | 13.0 | 16.6 |
| 70+ y | 6.3 | 5.5 | 6.8 |
| Race/ethnicity, % | |||
| Black | 31.5 | 29.9 | 32.6 |
| Hispanic | 33.3 | 31.8 | 34.2 |
| White | 35.2 | 38.4 | 33.2 |
Table 2.
Percentage of men and women with incident LUTS, overall and by baseline age group, among those with no/mild LUTS at Baseline
| Moderate to Severe, %* (AUASI ≥ 8) | Higher Severity, %* (AUASI ≥ 15) | Voiding, %† (AUASI subscore ≥ 5) | Storage, %‡ (AUASI subscore ≥ 4) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female | |
| Total | 11.4 | 8.5 | 13.9 | 1.8 | 1.6 | 1.9 | 7.1 | 7.4 | 6.8 | 21.3 | 18.8 | 23.7 |
| Age | ||||||||||||
| 30–39 y | 5.9 | 4.3 | 7.6 | 2.1 | 1.8 | 2.5 | 4.9 | 2.9 | 7.0 | 15.7 | 13.4 | 18.5 |
| 40–49 y | 10.7 | 8.6 | 12.5 | 1.5 | 1.1 | 1.9 | 7.3 | 9.7 | 5.2 | 21.8 | 18.4 | 25.0 |
| 50–59 y | 12.3 | 9.5 | 14.7 | 1.4 | 0.8 | 1.8 | 6.4 | 7.2 | 5.7 | 26.0 | 24.0 | 27.7 |
| 60–69 y | 15.7 | 17.5 | 14.6 | 2.0 | 2.2 | 1.8 | 10.1 | 18.0 | 5.0 | 27.8 | 29.6 | 26.4 |
| ≥ 70 y | 29.1 | 18.9 | 35.0 | 1.5 | 3.6 | 0.3 | 12.5 | 10.1 | 13.8 | 29.7 | 30.5 | 29.2 |
LUTS = Lower urinary tract symptoms; AUASI=American Urological Association Symptom Index
N=3,301 (1,305 men, 1,996 women)
N=3,657 (1,418 men, 2,240 women)
N=2,752 (1,135 men, 1,616 women)
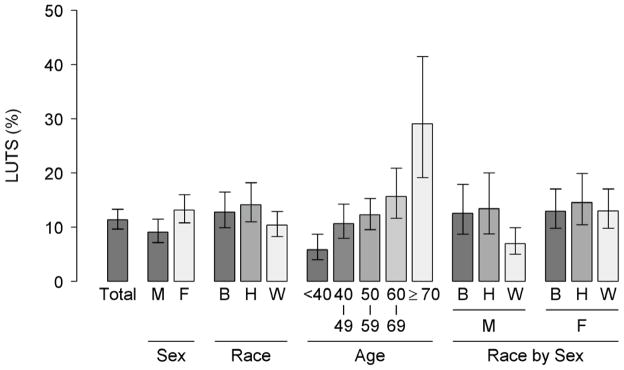
Figure 2 shows the LUTS incidence percentages by age, sex, and race/ethnicity groups. At follow-up, 11.4% of participants newly reported moderate-to-severe LUTS (AUASI ≥ 8). Women had 50% higher odds of LUTS compared to men (age-adjusted OR=1.54, 95% CI 1.09–2.17, P=0.02). Combining sex/race subgroups, the LUTS incidence percentage of 13% was consistent across black males, black females, Hispanic males, and white females. In contrast, a distinctly lower percentage (7%) was observed in white males, while among Hispanic females it was higher (15%) (Pintx=0.12 for interaction between race and sex). Overall, race differences were not statistically significant (e.g., for Hispanics age-adjusted OR=1.46, 95% CI 0.97–2.19; for blacks age-adjusted OR=1.29, 95% CI 0.87–1.91). However, among men, both black (OR=1.98, 95% CI 1.11– 3.54) and Hispanic (OR=2.20, 95% CI 1.16–4.15) men were at higher odds of LUTS compared to white men (P=0.018). This racial difference among men persisted for higher severity LUTS as well (P=0.035, data not shown). Among women, there was no association between race/ethnicity and LUTS incidence (P=0.9).
Figure 2.
Age-adjusted Incidence of Moderate-to-Severe LUTS among BACH-II Participants with No/Mild LUTS at Baseline, Overall and by Population Subgroups. M=male, F=female, B=black, H=Hispanic, W=white.
Discussion
BACH is the first U.S. population-based cohort study designed to examine lower urinary tract symptoms in a racially/ethnically balanced sample of men and women over time. This manuscript is the first from BACH to describe the 5-year point incidence among individuals with no or mild LUTS at baseline. Results showed that women had 50% higher odds of developing moderate-to-severe LUTS. Both men and women were at greater odds of incident moderate-to-severe LUTS with increasing age. For higher severity LUTS among women, the incidence peaked among younger women and declined with age, unlike the incidence among older men. These findings support the notion that LUTS in men often reflect the development of benign prostatic obstruction or hyperplasia, which is generally slow and protracted. In contrast, a more dynamic nature of women’s symptoms across the age span may indicate fluctuations in underlying contributors, such as recent reproductive experiences (e.g., childbirth) or the hormonal milieu (e.g., menopausal transition), and may be more related to overactive bladder, rather than voiding obstruction. Among men, Black and Hispanic participants were twice as likely to develop LUTS, compared to white men; racial/ethnic differences were not statistically significant among women.
Comparisons of these findings with those of previous studies must be made in light of differences in follow-up lengths and ages of study participants across studies. Generally, the percentage of BACH men who had newly developed moderate-to-severe LUTS at follow-up was lower than that reported in previous studies of men. For example, compared to our finding of approximately 9% of men, a study of Austrian men aged 40–84 found a 5-year incidence of approximately 18%.22 In a community-based study of 223 Japanese men (40–79 years old), 21% had newly developed LUTS at 3-year follow-up.23 A study of older men (the Osteoporotic Fractures in Men Study, mean baseline age 74 y) found 29% of men with none/mild LUTS at baseline newly reported moderate-to-severe LUTS at 2-year follow-up.24 Although one study of men from Spain found a comparable estimate of 10% of men newly reporting LUTS after 2-year follow-up, the study restricted its sample to men with no LUTS or very mild LUTS (AUA-SI ≤2) at baseline.25 For women, our results seem consistent with findings among Danish women, where the 1-year incidence of LUTS was 10%,26 and possibly aligned with findings among Swedish women, where the 16-year incidence of overactive bladder symptoms was 20%.7
White men had the lowest rates for LUTS incidence, which is consistent with results comparing race/ethnic groups among men in the Prostate Cancer Prevention Trial.20 However, compared to a small study of black men aged 40–79 years with 4 or 5 years follow-up from Flint Michigan, the incidence percentage among black BACH participants was considerably lower.27 The Flint study found that 26% of men with no/mild symptoms at baseline reported moderate-to-severe LUTS at follow-up, notably higher than the 13% newly reporting symptoms in BACH. Prior longitudinal studies on racial/ethnic differences in female LUTS are lacking.
A difficulty with research in this area is that LUTS, unlike most chronic diseases or diagnosed events, are rarely determined by a single event and may not be chronic in nature. Therefore, incidence rates, which are based on the timing of the first instance of a health outcome, are difficult to calculate for LUTS. Frequently repeated assessments of symptoms in BACH and in numerous other studies of LUTS incidence7,8,22,27 would have helped capture a more detailed natural disease history. Nonetheless, BACH has unique strengths in the field of urological research. As the first study to examine LUTS in both men and women of younger and older ages from the same community-based population, this may be the first reliable and generalizable comparison of sex and racial/ethnic differences in rates of LUTS development. Unlike other longitudinal studies of LUTS, we accounted for non-response at both baseline and follow-up interviews and used complex sampling methodology to ensure a representative sample. This approach minimizes concerns regarding selection bias by accounting for differences in participation (e.g., the higher rate of participation among women compared to men). Furthermore, it promotes our ability to translate findings for use in public health efforts for information dissemination, as well as clinical utility in anticipating future treatment needs among similar populations. For example, patient education, self-assessment, or symptom management tools may be designed to appeal to gender or age subgroups found to have a higher risk of LUTS. In addition to the sex and racial/ethnic differences reported here, future analyses from BACH and other longitudinal studies are needed to better understand the relative contributions of socioeconomic factors, genetic predispositions, reproductive factors, nutrition/diet, concurrent chronic or acute medical conditions and medications to the development of LUTS and specific symptom subtypes over time.
Acknowledgments
Source of Funding: This project was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, Grant No. U01DK56842. The content of this work is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Abbreviations used in this manuscript
- AUASI
American Urological Association Symptom Index
- BACH
Boston Area Community Health
- BPH
Benign prostatic hyperplasia
- LUTS
Lower urinary tract symptoms
Footnotes
Author Financial Disclosures:
The authors report no financial disclosures.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kupelian V, Wei JT, O’Leary MP, et al. Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) Survey. Arch Intern Med. 2006;21:2381–7. doi: 10.1001/archinte.166.21.2381. [DOI] [PubMed] [Google Scholar]
- 2.Kupelian V, Rosen RC, Link CL, et al. Association of urological symptoms and chronic illness in men and women: contributions of symptom severity and duration--results from the BACH Survey. J Urol. 2009;2:694–700. doi: 10.1016/j.juro.2008.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coyne KS, Kaplan SA, Chapple CR, et al. Risk factors and comorbid conditions associated with lower urinary tract symptoms: EpiLUTS. BJU Int. 2009:24–32. doi: 10.1111/j.1464-410X.2009.08438.x. [DOI] [PubMed] [Google Scholar]
- 4.Coyne KS, Wein AJ, Tubaro A, et al. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 2009:4–11. doi: 10.1111/j.1464-410X.2009.08371.x. [DOI] [PubMed] [Google Scholar]
- 5.Malmsten UG, Molander U, Peeker R, et al. Urinary incontinence, overactive bladder, and other lower urinary tract symptoms: a longitudinal population-based survey in men aged 45–103 years. Eur Urol. 2010;1:149–56. doi: 10.1016/j.eururo.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 6.Irwin DE, Milsom I, Chancellor MB, et al. Dynamic progression of overactive bladder and urinary incontinence symptoms: a systematic review. Eur Urol. 2010;4:532–43. doi: 10.1016/j.eururo.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Wennberg AL, Molander U, Fall M, et al. A longitudinal population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in women. Eur Urol. 2009;4:783–91. doi: 10.1016/j.eururo.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Wong SY, Woo J, Leung JC, et al. Depressive symptoms and lifestyle factors as risk factors of lower urinary tract symptoms in Southern Chinese men: a prospective study. Aging Male. 2010;2:113–9. doi: 10.3109/13685530903440432. [DOI] [PubMed] [Google Scholar]
- 9.Heidler S, Deveza C, Temml C, et al. The natural history of lower urinary tract symptoms in females: analysis of a health screening project. Eur Urol. 2007;6:1744–50. doi: 10.1016/j.eururo.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 10.Heidler S, Mert C, Temml C, et al. The natural history of the overactive bladder syndrome in females: a long-term analysis of a health screening project. Neurourol Urodyn. 2011;8:1437–41. doi: 10.1002/nau.21093. [DOI] [PubMed] [Google Scholar]
- 11.Platz EA, Joshu CE, Mondul AM, et al. Incidence and progression of lower urinary tract symptoms in a large prospective cohort of United States men. J Urol. 2012;2:496–501. doi: 10.1016/j.juro.2012.03.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McKinlay JB, Link CL. Measuring the Urologic Iceberg: Design and Implementation of the Boston Area Community Health (BACH) Survey. Eur Urol. 2007;2:389–96. doi: 10.1016/j.eururo.2007.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barry MJ, Fowler FJ, Jr, O’Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;5:1549–57. doi: 10.1016/s0022-5347(17)36966-5. discussion 1564. [DOI] [PubMed] [Google Scholar]
- 14.Okamura K, Nojiri Y, Osuga Y, et al. Psychometric analysis of international prostate symptom score for female lower urinary tract symptoms. Urology. 2009;6:1199–202. doi: 10.1016/j.urology.2009.01.054. [DOI] [PubMed] [Google Scholar]
- 15.Boyle P, Robertson C, Mazzetta C, et al. The prevalence of lower urinary tract symptoms in men and women in four centres. The UrEpik study BJU Int. 2003;4:409–14. doi: 10.1046/j.1464-410x.2003.04369.x. [DOI] [PubMed] [Google Scholar]
- 16.Boyle P, Robertson C, Mazzetta C, et al. The relationship between lower urinary tract symptoms and health status: the UREPIK study. BJU Int. 2003;6:575–80. doi: 10.1046/j.1464-410x.2003.04448.x. [DOI] [PubMed] [Google Scholar]
- 17.Scarpero HM, Fiske J, Xue X, et al. American Urological Association Symptom Index for lower urinary tract symptoms in women: correlation with degree of bother and impact on quality of life. Urology. 2003;6:1118–22. doi: 10.1016/s0090-4295(03)00037-2. [DOI] [PubMed] [Google Scholar]
- 18.Terai A, Matsui Y, Ichioka K, et al. Comparative analysis of lower urinary tract symptoms and bother in both sexes. Urology. 2004;3:487–91. doi: 10.1016/j.urology.2003.09.070. [DOI] [PubMed] [Google Scholar]
- 19.Welch G, Kawachi I, Barry MJ, et al. Distinction between symptoms of voiding and filling in benign prostatic hyperplasia: findings from the Health Professionals Follow-up Study. Urology. 1998;3:422–7. doi: 10.1016/s0090-4295(97)00626-2. [DOI] [PubMed] [Google Scholar]
- 20.Kristal AR, Arnold KB, Schenk JM, et al. Race/ethnicity, obesity, health related behaviors and the risk of symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. J Urol. 2007;4:1395–400. doi: 10.1016/j.juro.2006.11.065. quiz 1591. [DOI] [PubMed] [Google Scholar]
- 21.Raghunathan TE, Solenberger P, Van Hoewyk J. IVEware: Imputation and Variance Estimation Software User Guide. Survey Research Center, Institute for Social Research, University of Michigan; 2002. http://www.isr.umich.edu/src/smp/ive. [Google Scholar]
- 22.Temml C, Brossner C, Schatzl G, et al. The natural history of lower urinary tract symptoms over five years. Eur Urol. 2003;4:374–80. doi: 10.1016/s0302-2838(03)00084-8. [DOI] [PubMed] [Google Scholar]
- 23.Masumori N, Tsukamoto T, Rhodes T, et al. Natural history of lower urinary tract symptoms in men--result of a longitudinal community-based study in Japan. Urology. 2003;5:956–60. doi: 10.1016/s0090-4295(02)02594-3. [DOI] [PubMed] [Google Scholar]
- 24.Parsons JK, Wilt TJ, Wang PY, et al. Progression of lower urinary tract symptoms in older men: a community based study. J Urol. 2010;5:1915–20. doi: 10.1016/j.juro.2010.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moreno Sierra J, Fernandez Perez C, Cano Escudero S, et al. Progression of null or mild lower urinary tract symptoms indicative of benign prostatic hyperplasia after 2 years of follow-up in non-treated men aged 40 years or older. Urology. 2011;3:693–8. doi: 10.1016/j.urology.2010.07.459. [DOI] [PubMed] [Google Scholar]
- 26.Moller LA, Lose G, Jorgensen T. Incidence and remission rates of lower urinary tract symptoms at one year in women aged 40–60: longitudinal study. Bmj. 2000;7247:1429–32. doi: 10.1136/bmj.320.7247.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sarma AV, McLaughlin JC, Jacobsen SJ, et al. Longitudinal changes in lower urinary tract symptoms among a cohort of black American men: the Flint Men’s Health Study. Urology. 2004;5:959–65. doi: 10.1016/j.urology.2004.06.043. [DOI] [PubMed] [Google Scholar]