Abstract
Accumulation of extracellular matrix (ECM) materials in the trabecular meshwork (TM) is believed to be a contributing factor to intraocular pressure (IOP) elevation, a risk factor/cause of primary open angle glaucoma, a major blinding disease. Matrix metalloproteinase-3 (MMP-3) is one of the proteinases that can effectively degrade ECM elements such as fibronectin, and MMP-3 delivery to the TM represents a promising approach for IOP reduction and treatment of glaucoma. In this study, we tested the feasibility of using polymeric microparticles to achieve a slow and sustained release of active MMP-3 to cultured human TM cells. β-Casein, with molecular weight (24 kDa) and hydrophobicity similar to those of the active MMP-3 fragment (19.2 kDa), was first employed as a model for initial testing. β-casein was encapsulated into poly(lactic-co-glycolic acid) (PLGA) microparticles using a double emulsion procedure at an encapsulation efficiency of approximately 45%. The PLGA microparticles were chosen given their biocompatibility and the proven capacity of sustained release of encapsulated molecules. The release test conducted in the culture medium showed a slow and sustained release of the protein over 20 days without a significant initial burst release. Active MMP-3 was subsequently encapsulated into PLGA microparticles with an encapsulation efficiency of approximately 50%. A bio-functional assay utilizing human TM cells was set up in which the reduction of fibronectin was used as an indicator of enzyme activity. It was observed that fibronectin staining was markedly reduced by the medium collected from MMP-3-microparticle-treated cultures compared to that from blank- and β-casein-microparticle controls, which was validated using a direct MMP-3 activity assay. The controlled release of MMP-3 from the microparticles resulted in sustained degradation of fibronectin up to 10 days. This proof-of-concept undertaking represents the first study on the controlled and sustained release of active MMP-3 to TM cells via encapsulation into PLGA microparticles as the potential treatment of glaucoma.
Keywords: Matrix metalloproteinase, Microparticles, Trabecular meshwork, Controlled release, Glaucoma
INTRODUCTION
Glaucoma, a leading cause of blindness worldwide,1,2 is characterized by progressive degeneration of retinal ganglion cells and axonal loss as well as visual impairment. It is estimated that by 2020, 79.6 million people worldwide will be diagnosed with the most common form of glaucoma, primary open angle glaucoma (POAG).3A major risk factor of POAG is an elevation of the pressure within the eye or the intraocular pressure (IOP), which is controlled by a delicate balance between the production and drainage of the aqueous humor. The IOP elevation is often caused by an increase in the resistance of the aqueous outflow exerted by the trabecular meshwork (TM),4 a specialized tissue located in the chamber angle of the eye neighboring the cornea. The TM tissue is composed of layers of trabecular beams that are made up of extracellular matrix (ECM) elements including fibronectin, collagen, laminin and proteoglycans. Both the TM cells that line the trabecular beams and the ECM in the TM are factors essential for maintenance of the normal aqueous humor outflow.5-7In the eyes of patients with POAG, excessive accumulation of ECM materials has been observed in the TM.6-9Such an abnormal accumulation is believed to decrease the extracellular spacing in the TM and increase the aqueous outflow resistance, resulting in IOP elevation and glaucomatous conditions.10
There is currently not a cure for glaucoma. Lowering the IOP via various medications and/or surgical procedures such as laser trabeculoplasty remains to be the mainstay solution of glaucoma treatment. Medications have to be applied once or several times a day and patient adherence to medication regimens varies.11There are also ocular and/or systemic side effects. Laser and other surgeries are often successful initially, but treatment failure can occur later.12
Matrix metalloproteinase-3 (MMP-3) is one of the major matrix metalloproteinases expressed in TM cells.13,14It can degrade a number of ECM materials such as fibronectin, collagens, and proteoglycans.9Increasing MMP-3 activity by adding the purified enzyme15or by inducing the expression of MMP-3 by interleukin-1α6,15or tert-butylhydroquinone16has been shown to enhance the outflow facility in perfused human anterior segment organ cultures. Conversely, blocking the endogenous activity of MMP-3 by MMP inhibitors reduces the outflow facility and elevates the pressure.6,7These findings suggest that promoting MMP-3 activity may help in reducing ECM accumulation and outflow resistance in glaucomatous eyes. While effective, the existing MMP-3 delivery strategies such as direct application of the active enzyme or induction of its expression have been shown to trigger surged enzyme action that dissipates in 2 to 3 days.15This highlights the need for a delivery platform that can prolong the duration of MMP-3 action by controlling its release profile over extended periods of time without loss of activity.
In this study, we revisited microparticle technology, which has a long track record of success in a variety of biomedical applications, to achieve a novel approach for the controlled delivery of MMP-3 to the TM. Due to their minimal toxicity and biocompatibility, biodegradable polyesters such as poly(ε-caprolactone) (PCL), poly(d,l-lactide) (PLA), and poly(lactide-co-glycolide) (PLGA) have generated immense interest as drug delivery carriers.17-21 PLGA in particular has been utilized extensively in biomedical and tissue engineering applications to formulate microparticles and nanoparticles for the sustained delivery of small drugs, proteins, and other macromolecules up to several days to weeks.20,22
We hypothesized that the controlled, sustained delivery of MMP-3 from a biodegradable microparticle system such as PLGA, can provide a steady supply of the active enzyme to the aqueous humor outflow system, thereby reducing ECM accumulation. In this proof-of-concept study, PLGA microparticles were first formulated to encapsulate β-casein, a protein with properties similar to MMP-3, to test the encapsulation and release conditions. An active MMP-3 fragment was subsequently encapsulated into PLGA microparticles. The enzyme release from the microparticles and its activity were assessed in cultured human TM cells, based on a bio-functional assay using the fibronectin level as an indicator of MMP-3 activity, which was also validated using a fluorometric MMP-3 activity assay. To our knowledge, this is the first report on the use of a biodegradable polymer-based delivery system for controlled release of active MMP-3 over an extended period of time to cultured TM cells, which has implications for the potential treatment of glaucoma.
EXPERIMENTAL SECTION
Materials
PLGA (75:25 lactide–to-glycolide, molecular weight or MW 66-107 kDa), dichloromethane (DCM), poly(vinyl alcohol) (PVA, 87-89% hydrolyzed, MW 13-23 kDa), β-casein from bovine milk (MW 24 kDa), bovine serum albumin (BSA), Dulbecco’s Eagle’s minimum essential medium (DMEM), and fetal calf serum were all obtained from Sigma-Aldrich (St. Louis, MO). The catalytic domain fragment of human MMP-3 (active MMP-3, MW 19.2 kDa) was obtained from Biovision (Milpitas, CA).
Encapsulation of proteins into PLGA microparticles
β-Casein- and MMP-3-encapsulated PLGA microparticles were prepared using a double emulsion method as described previously.23PLGA (44 mg) was dissolved in 1 mL of DCM. β-Casein (2.2 mg) and MMP-3 (5 Jg) were each dissolved in 100 μL deionized distilled water (ddH2O). The protein solutions were each added to the PLGA solution and the mixture was sonicated for 30 sec using a Misonix XL ultrasonic processor (25% duty cycle, 475 W, 1/8” tip, QSonica, LLC, Newtown, CT). One milliliter of 3% PVA was then added to the two mixtures, followed by sonication for 30 sec at 25% duty cycle. The two double emulsions were each poured into 20 mL of 0.3% PVA, and vigorously stirred at room temperature for 24 h to evaporate DCM. Unencapsulated proteins and PVA were removed by centrifuging the microparticles at 21,130 × g for 30 min using a Beckman Avanti J2-Centrifuge (Beckman Coulter, Brea, CA) and washing with ddH2O five times. The resulting pellets were resuspended in ddH2O, lyophilized over 2 days, and stored at −20° C for further characterization. The supernatants that contained PVA and unencapsulated proteins were either stored at −20°C or lyophilized. Blank PLGA microparticles without proteins were prepared in parallel by adding 100 μL ddH2O instead of the protein solution.
Scanning Electron Microscopy (SEM) observations
The surface morphology of PLGA microparticles was examined by scanning electron microscopy (SEM) using a JEOL-JSM 6320F field emission microscope (JEOL USA, Peabody, MA) as described earlier.24,25Freeze-dried microparticle samples were placed onto a carbon adhesive strip mounted on an aluminum stub. Samples were sputter-coated with Pt/Pd at a coating thickness of 6 nm (Polaron E-100 sputter coater system, Polaron, UK) and visualized at an accelerating voltage of 5.0 mV and 8.0 mm working distance.
Encapsulation efficiencies of protein-encapsulated microparticles
Protein encapsulation efficiency was calculated as the ratio of actual protein amount encapsulated into microparticles to the total amount loaded initially. For β-casein-encapsulated microparticles, the encapsulation efficiency was estimated via two different methods. In the first method, β-casein-encapsulated microparticles were incubated in 0.5 N NaOH on an orbital shaking incubator (operating at 37° C and 250 rpm, under air) for 4 h to accelerate PLGA degradation. The amount of β-casein released was measured using the Bradford protein assay (Bio-Rad, Hercules, CA) based on a standard curve obtained using 0.2 - 2 μg of β-casein. The encapsulation efficiency was then determined based on the ratio of the β-casein in the microparticles to the amount initially added. In the second method, the encapsulation efficiency was determined indirectly by measuring the amount of unencapsulated β-casein in the supernatant recovered following the encapsulation procedure. The result was subtracted from the initial amount of protein loaded to estimate the amount encapsulated, and the encapsulation efficiency was calculated. For MMP-3-encapsulated microparticles, the encapsulation efficiency was determined by measuring the amount of unencapsulated MMP-3 in the supernatant recovered following microparticle fabrication, using the Bradford protein assay as described above.
Release kinetics of β-casein-encapsulated PLGA microparticles
Two milligrams of β-casein-containing microparticles were dispersed in 1 mL of DMEM in triplicates in microcentrifuge tubes, and placed in a shaking incubator (37°C and 100 rpm, under air). At 8 h, and 1, 4, 7, 10, 15, and 20 day time points, the samples were centrifuged at 21,130 × g for 5 min and the supernatants were collected. The pellet was redispersed in 1 mL of fresh DMEM and placed back in the incubator. The amount of protein released over time was measured using the Bradford protein assay based on a standard curve of β-casein.
Cell culture
Normal human TM tissues were dissected from corneo-scleral rims obtained from human donors 33, 43, 48, 60, and 62 years of age (Illinois Eye Bank, Chicago, IL). The tissues were placed onto Falcon Primaria flasks (BD Biosciences, San Jose, CA) and cultured at 37°C under 5% CO2 in complete medium containing DMEM and 10% fetal calf serum.26Cells grown from the explants were gently spread in the flasks. Once confluency was reached, the cells were passaged. Second- or third-passaged cells were used in the experiments.
β-Casein release in the presence or absence of TM cells
Human TM cells seeded at 10,000 cells/well in Lab-Tek 8-well CC2 glass chamber slides (Nalge Nunc, Rochester, NY) were incubated with 250 μL of DMEM without or with the addition of 0.25 mg blank or β-casein-encapsulated microparticles for 8 h, and 1, 2, 3, 4, 5, 7, and 10 days. Cell morphology and density were monitored by phase contrast microscopy. Blank or β-casein-encapsulated microparticles were also added to another set of wells without TM cells. At each time point, the media were collected and centrifuged at 21,130 × g for 5 min. The amount of the β-casein remaining in the pellet (microparticles) was measured using the Bradford protein assay with β-casein as the standard.
Activity of unencapsulated MMP-3 in the supernatant
The MMP-3 activity in the supernatant recovered from microparticle fabrication was measured by a bio-functional assay, in which the degradation or reduction of fibronectin, an ECM protein and one of the substrates for MMP-3, was used as an indicator of enzyme activity in human TM cells. Briefly, TM cells (8,000 cells/well) on uncoated 8-well chamber slides were incubated for 48 h in serum-free DMEM with 0, 25, or 50 μL of the supernatant. Cells were then fixed with ice-cold methanol for 15 min, blocked with 3% BSA, and incubated with mouse anti-human fibronectin antibody (1:100, BD Transduction Laboratories, Lexington, KY). Following incubation with fluorescein isothiocyanate (FITC)-conjugated goat anti-mouse secondary antibody (1:100, Jackson ImmunoResearch, West Grove, PA), the slides were mounted in Vectashield (Vector Laboratories, Burlingame, CA) anti-photobleaching mounting media with DAPI (4′,6′-diamidino-2-phenylindole dihydrochloride). The staining was visualized using Axioscope (Carl Zeiss MicroImaging, Thornwood, NY). Images of 10 visual fields were acquired with the 10× objective. The staining intensity of the fibronectin network in the cultures was quantified using the Metamorph software and the number of cell nuclei per field was counted. The total intensity per cell was calculated and Student’s t-test was performed to compare results from different groups. MMP-3, if present and active, would result in diminished staining intensity or reduced fibronectin level.
Fibronectin has been shown to be digested quickly by MMP-3 in vitro. A previous report by Wilhelm and colleagues27 noted that 50% of fibronectin was digested within 5 h at pH 7.5 and 90% digested at pH 5.5. The fibronectin digestion by 0.1 μg recombinant active MMP-3 fragment (as judged by the bio-functional immunostaining assay) was already copiously evident by 24 h (data not shown). However, in consideration of the possible low amount of unencapsulated MMP-3 in the supernatant as well as that of MMP-3 released from microparticles, the incubation (digestion) time was expanded to 48 h to allow the enzyme to take full action, improving thereby the sensitivity of the bioassay.
MMP-3 release in TM cultures
Human TM cells (10,000 cells/well) in 8-well chamber slides were incubated in 250 μL serum-free DMEM with MMP-3-encapsulated, β-casein-encapsulated, or blank microparticles (3 mg each) for 4 days. The media harvested were centrifuged at 21,130 × g for 5 min. The supernatant fractions collected were added to another set of human TM cultures. Cells were incubated for 48 h, and were fixed as described above. The fibronectin assay was performed as above with each of the collected supernatant along with 0.1 and 0.5 μg of active MMP-3 enzyme as positive controls. The media collected from β-casein-containing and blank microparticles served as negative controls.
MMP-3 activity assay (fluorometric green)
MMP-3 activity assay (Abcam, Cambridge, MA) was performed per manufacturer’s protocol on aliquots of culture medium from cells incubated with DMEM only, and those incubated with MMP-3-microparticles for 4 days. The MMP-3 active fragment (0.1 μg) was included as a positive control. The assay uses a green fluorescence probe/fluorescence resonance energy transfer (FRET) peptide as the MMP-3 activity indicator. In the intact FRET peptide, the fluorescence of one half of the probe is quenched by the other part. Upon cleavage into two separate fragments by MMP-3, the green fluorescence is recovered. The fluorescence was detected at excitation wavelength 450 nm and emission wavelength 535 nm. The fluorescence unit (minus that for the reagent control) was determined for each sample group. Statistical analysis (n = 3) was performed with Student’s t- test.
Release profile of MMP-3 from PLGA microparticles in TM cultures
The release profile of MMP-3 from PLGA microparticles in TM cultures was subsequently examined. Human TM cells (10,000 cells/well) in 8-well chamber slides were incubated with 250 μL DMEM containing 3 mg of MMP-3-encapsulated microparticles. The culture medium was removed 24 h later, centrifuged, and the supernatant was harvested as the 24 h or day 1 MMP-3-microparticle medium. The microparticle-containing pellet was redispersed in 250 μL of fresh DMEM and placed back onto the cells. This procedure was repeated up to 21 days and the MMP-3-microparticle media were collected on a daily basis. To test the MMP-3 activity in these media, another set of TM cells were incubated for 48 h with each of the MMP-3-micropaticle media collected. As a control, TM cells were also incubated in serum-free DMEM without any MMP-3-microparticle media. Immunofluorescence staining for fibronectin was carried out and image analyses were performed to quantify the level of fibronectin in each specimen.
In a control experiment, recombinant active MMP-3 fragment (0.1 μg) was added onto human TM cells. After incubation for 2, 3, or 4 days, the media were collected from the cultures. The activity of MMP-3 in these media was tested by the fibronectin bio-functional assay as described above. Fresh active MMP-3 fragment (0.1 μg) and the media from the untreated cells served respectively, as positive and untreated control.
RESULTS
Characterization of microparticles
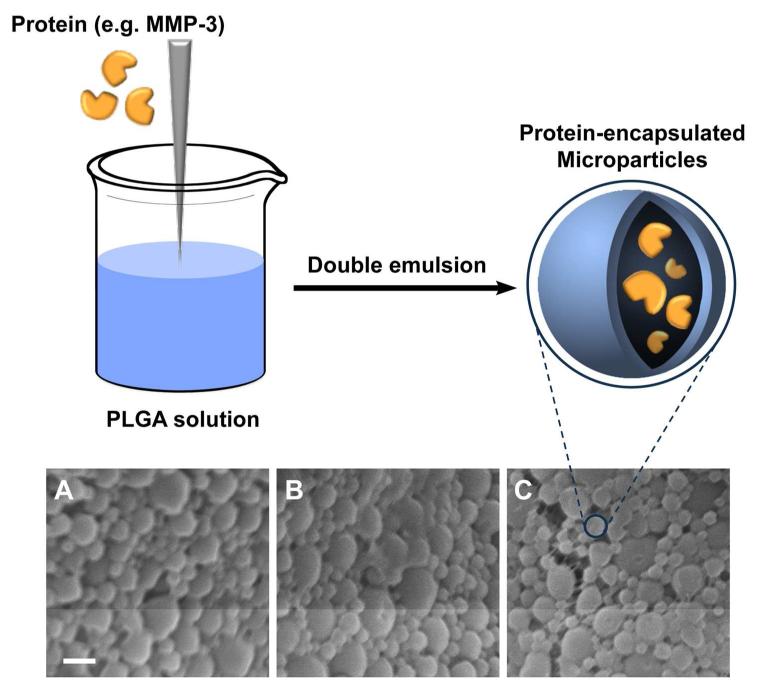
SEM observations revealed the blank (Figure 1A), β-casein (Figure 1B)- and MMP-3 (Figure 1C)-encapsulated microparticles to be spherical in shape, with smooth, primarily poreless, surface. The particle size was estimated to be 0.4 −1.6 μm (Figure 1).
Figure 1.
Overview of the microparticle fabrication process (top) and SEM images (bottom) of (A) blank particles, (B) β-casein-encapsulated microparticles, and (C) MMP-3-encapsulated microparticles. Scale bar, 1 μm.
The encapsulation efficiency was calculated as the ratio of actual amount of protein encapsulated into microparticles to the initial protein loading. An initial amount of 2.2 mg of β-casein was used for preparation of 44.0 mg microparticles. The encapsulation efficiency for β-casein-encapsulated microparticles was determined from both the microparticle pellet and the supernatant. The total amount of β-casein measured after dissolving the microparticle pellet in 0.5 N NaOH was 1.0 mg. The total amount of unencapsulated protein in the supernatant fraction was assayed to be 1.2 mg, indicating that the amount encapsulated was 1.0 mg. The encapsulation efficiency from both methods was measured to be 45%.
For active MMP-3 protein fragment, the initial protein loading was 5 μg. The total amount of unencapsulated MMP-3 in the supernatant was 2.5 μg. The encapsulation efficiency was thus estimated to be 50%.
Release kinetics of β-casein-encapsulated microparticles
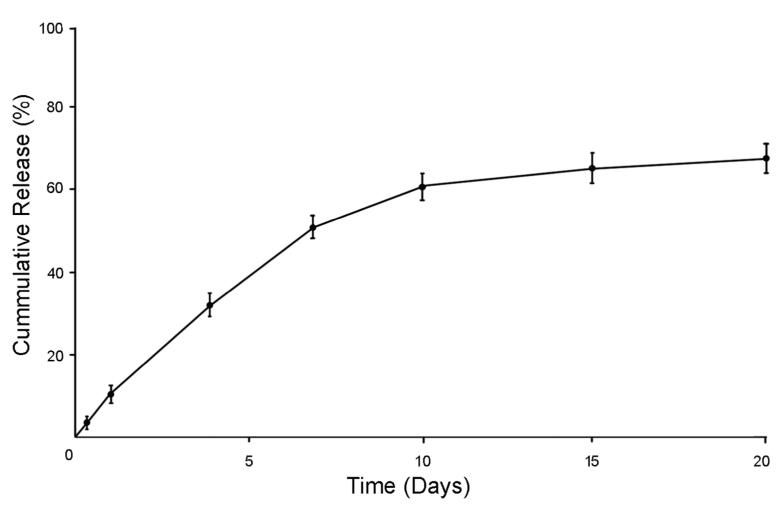
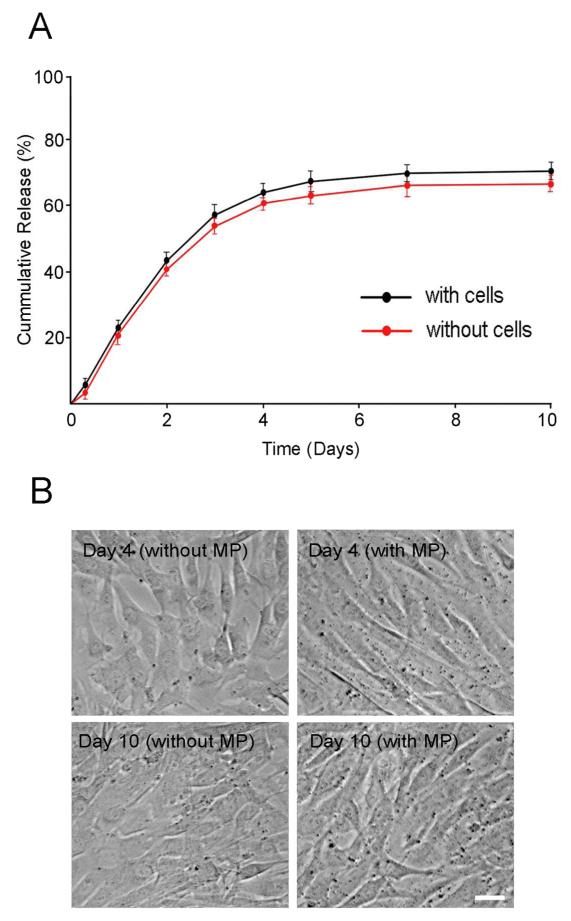
β-casein was used as a model protein to study the release kinetics of the microparticles. The release of β-casein from PLGA microparticles was examined under two sets of conditions, in an orbital shaking incubator (operating at 37° C and 100 rpm, under air) and in a cell culture incubator (37° C and 5% CO2). As shown in Figure 2, approximately 35% of β-casein was released within the first 4 days in the shaking incubator, reaching 50% in 7 days, and then steadily increasing to 67% in 20 days. As for the release in the cell culture incubator in the presence or absence of cells, β-casein-containing- or blank microparticles were added to wells pre-plated or not-plated with human TM cells. The microparticles were recovered after incubation for various time periods, and the amount of β-casein remaining was measured. The release, which was biphasic, increased linearly to around 60% in 4 days and then leveled off thereafter (Figure 3A). The β-casein release curve was similar regardless of the presence of TM cells. No protein was detected in any of the blank microparticle samples. The microparticle incubation did not affect either the TM cell morphology or the cell density during the course of the experiment (Figure 3B).
Figure 2.
Release profile of β-casein-encapsulated PLGA microparticles in DMEM in a shaking incubator under air. Results are shown as mean ± SD (n = 3). The release test conducted in DMEM shows an initial, linear release in 7 days and then a slowed and sustained release of the protein over 20 days. Note that ~67% of the encapsulated protein was released at the 20 day time point, indicating that the controlled release was extended to a significantly longer period of time.
Figure 3.
(A) Release of β-casein from PLGA microparticles in the presence (black line) or absence (red line) of human TM cells in serum-free DMEM under tissue culture conditions. Note that ~60% of the encapsulated protein was released in 4 days. The release leveled off thereafter. No β-casein was detected in any of the time points when blank PLGA microparticles were used (negative controls). (B) Phase contrast micrographs of human TM cells without or with microparticle (MP) incubation for 4 or 10 days. The TM cell morphology and density were not affected by incubation with β-casein-encapsulated microparticles. Scale bar, 20 μm.
MMP-3 activity in the supernatant collected during microparticle fabrication
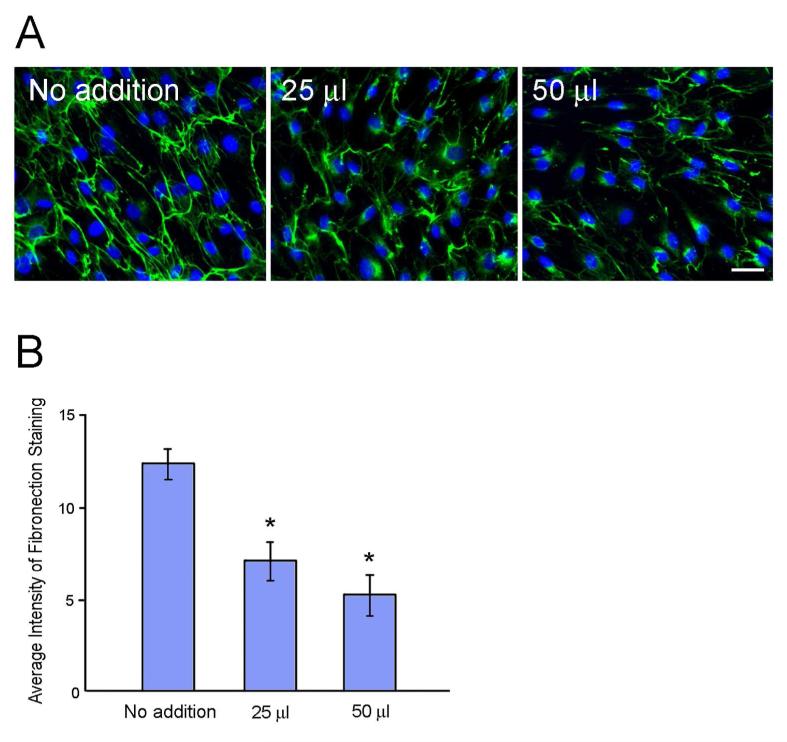
The supernatant fraction that contained unencapsulated MMP-3 was used to determine the amount of encapsulated protein and to measure the MMP-3 activity. For the latter, 0, 25, or 50 μL of the resuspended supernatant was applied to human TM cells and incubated for 48 h. The cells were immunostained for fibronectin in a bio-functional assay. As seen in Figure 4A, cells not incubated with any supernatant showed robust fibrillar fibronectin staining. Addition of both 25 and 50 μL of supernatant resulted in a reduction of fibronectin staining intensity compared to the no addition control. Quantification (Figure 4B) of the fluorescence intensity indicated that the difference was statistically significant (p < 0.0001).
Figure 4.
MMP-3 activity in the supernatant collected and lyophilized following fabrication of microparticles that contained unencapsulated MMP-3 fragment. (A) Human TM cells in DMEM were treated with 0 (No addition), 25, or 50 μL of re-suspended supernatant for 48 h, fixed, and immunostained for fibronectin, an MMP-3 substrate. A reduction in fibronectin staining (green) is indicative of the MMP-3 enzyme activity. The nuclei were stained with DAPI in blue. The cell density was similar in all specimens, suggesting that the decreased fibronectin staining was not related to the reduction in cell numbers. Scale bar, 20 μm. (B) Quantification of the green fluorescence intensity. Results are presented as mean ± SD (n = 10). *, p < 0.0001 compared to untreated (No addition) controls. Experiments were repeated 2 times with similar results.
As stated above, the supernatant was measured to contain approximately 2.5 μg of unencapsulated MMP-3. Since the initial amount of MMP-3 used for microparticle fabrication was 5 μg, the estimation was that 2.5 μg of MMP-3 was encapsulated into the microparticles. Results shown in Figure 4 indicated that 25 μL of the supernatant, containing about 0.14 μg of MMP-3, was amply effective in diminishing the fibronectin staining intensity with sufficient sensitivity in the bioassay. Subsequent release experiments were therefore set up using 3 mg of MMP-3-microparticles with approximately 0.17 μg of MMP-3 contained therein.
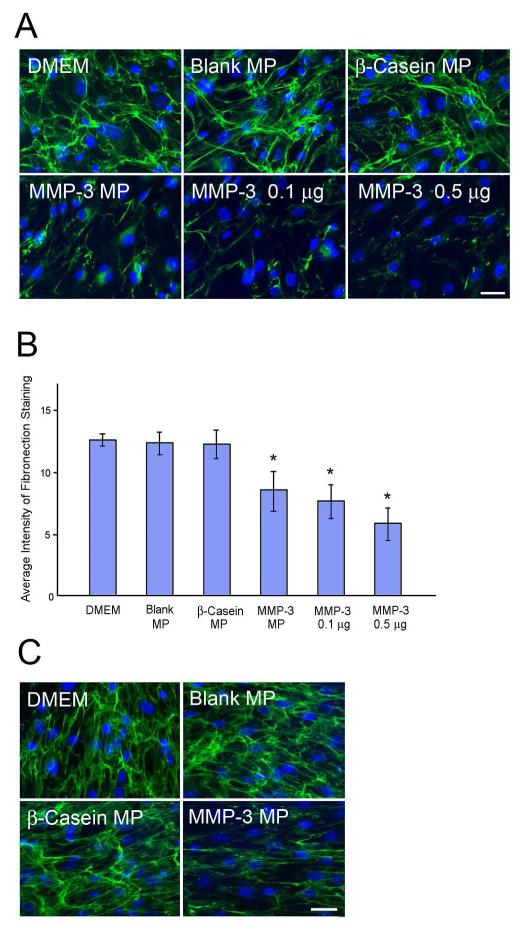
Release of MMP-3 from microparticles in the presence of TM cells
To determine whether MMP-3 was released and whether it was still active, TM cells were treated with blank, β-casein- or MMP-3-encapsulated microparticles for 4 days. The medium collected was centrifuged at 21,130 × g for 5 min and the supernatant was added to a different set of human TM cultures for 48 h. These cells were then immunostained for fibronectin. Figure 5A denotes that the fibronectin staining was markedly reduced not only by the active enzyme (added as positive control) but also by the medium collected from MMP-3-microparticle-treated cultures compared to that of untreated, blank-, and β-casein-microparticle-treated controls. Quantification of the fibronectin staining intensity (Figure 5B) confirmed that the fibronectin reduction (~31%) in MMP-3-microparticle-treated samples was significant (p < 0.001). This result indicated that MMP-3 was released to the medium, and that the activity was present in the medium collected up to 4 days. The fibronectin staining was likewise found diminished, compared to controls, in the cells incubated with MMP-3-containing microparticles for 4 days (Figure 5C), after the media had been removed. None of the microparticles altered the TM cell morphology or density (data not shown).
Figure 5.
Immunofluorescence for fibronectin. (A) TM cells were treated with DMEM only, or blank, β-casein-, or MMP-3-encapsulated microparticles (Blank MP, β-Casein MP or MMP-3 MP). The media collected from the cultures 4 days later as well as 0.1 and 0.5 μg active MMP-3 fragment were added to another set of TM cells. After 48 h, the cultures were stained for fibronectin. A reduction in fibronectin staining (green fluorescence) was noted in MMP-3 MP release medium. The nuclei were stained with DAPI in blue. Experiments were repeated at least 3 times with similar results. (B) Quantification of the green fluorescence intensity from images in A. Results are presented as mean ± SD (n = 10). *, p < 0.001 compared to untreated DMEM controls. (C) Fibronectin staining was performed directly on the cells following incubation with microparticles for 4 days and removal of the release media. A reduction in fibronectin staining was seen in MMP-3 MP-incubated cells compared to DMEM, blank and β-casein MP controls. Scale bar, 20 μm.
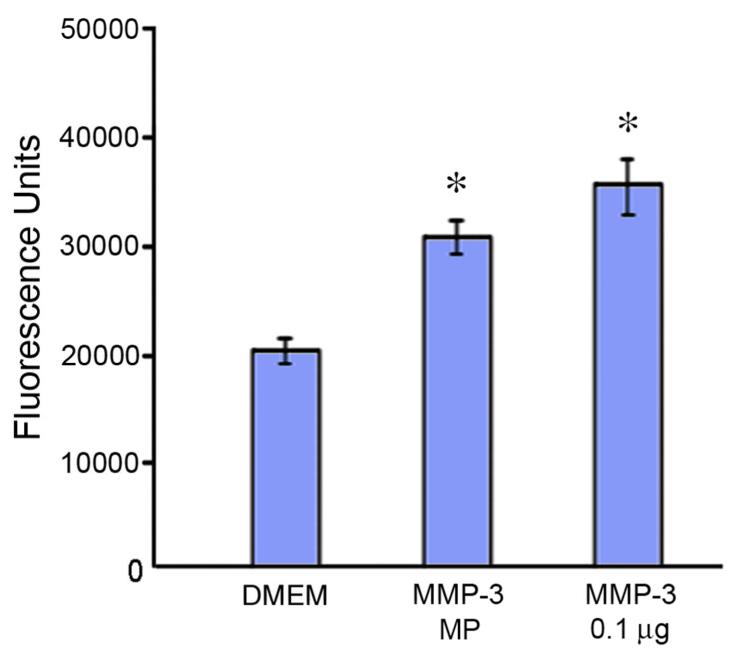
To verify the fibronectin fibril bio-functional assay for the MMP-3 activity, a direct MMP-3 activity fluorometric assay was performed. MMP-3, if present and active in the culture medium, should be able to cleave a FRET peptide composed of a green fluorescence probe and a quencher. Upon peptide cleavage into two separate fragments by MMP-3, the green fluorescence is recovered. As shown in Figure 6, TM cells incubated with DMEM only showed a low level of MMP-3 activity, indicating that the cells were functional, secreting a basal level of the enzyme. The MMP-3 positive control showed significantly higher fluoresecence units. The release medium from the cells incubated with MMP-3-encapsulated microparticles exibited a level of fluorescence (enzyme activity) similar to the positive control, which was significantly higher (p < 0.00031) than that of the untreated DMEM group. These results validate the fibronectin fibril assay data, indicating that MMP-3 was released from the microparticles and remained active upon release, capable of cleaving its specific substrate.
Figure 6.
MMP-3 activity fluorometric assay. The enzyme activity in the media from cells treated with DMEM (no MP control) or those treated with MMP-3-MP was assayed with the Abcam MMP-3 assay kit. Recombinant active MMP-3 fragment (0.1 μg) was used as a positive control. The fluoresecence units obtained were subtracted from those of the reagent blank. Results are presented as mean ± SD (n = 3). *, p < 0.00031 compared to DMEM controls.
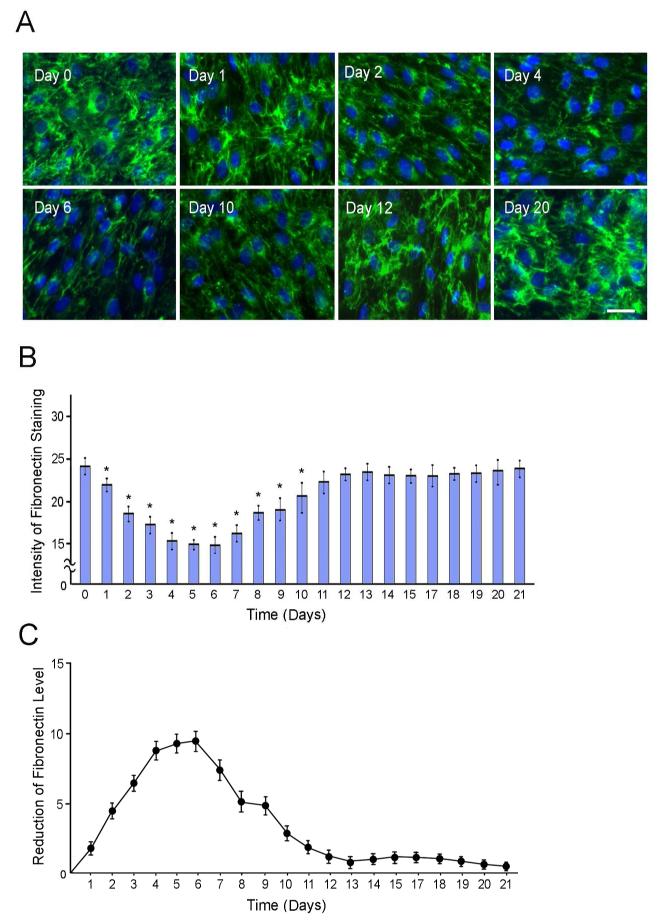
The release profile of MMP-3 from the microparticles in human TM cells was determined by the fibronectin bio-functional assay. TM cells were incubated with DMEM containing MMP-3-encapsulated microparticles (3 mg) and the medium was collected on a daily basis for 21 days. The MMP-3 activity in these MMP-3-microparticle media was subsequently tested using fibronectin immunofluorescence in another set of TM cells as described above. Cells incubated for 48 h in DMEM without any MMP-3-microparticle media served as controls. Representative images in Figure 7A demonstrated that compared to control cells incubated with DMEM only (day 0), cells incubated with MMP-3-microparticle media collected at days 2, 4, 6, and 10 showed a significant reduction in fibronectin staining. In contrast, cells incubated with the media collected at days 12 and 20 had robust fibronectin intensity as the controls. The quantified results are shown in Figure 7B and the profile of fibronectin reduction, representing MMP-3 activity, deduced from Figure 7B, is presented in Figure 7C. MMP-3 activity was detected in the MMP-3-microparticle media collected up to day 10. The most dramatic release was seen between day 4 and day 6 and the release leveled off or ceased beyond day 11.
Figure 7.
(A) Fibronectin staining in human TM cultures following a 48-h incubation with MMP-3-MP media collected on days 0 (control), 1, 2, 4, 6, 10, 12, and 20. A reduction in the fibronectin staining (green), indicative of MMP-3 activity, was observed in the day 1, 2, 4, 6, and 10 release media. Cell nuclei were stained with DAPI in blue. Experiments were repeated 3 times with similar results. Scale bar, 20 μm. (B) Quantification of the fluorescence intensity with MMP-3-MP media collected from day 1 to day 21. Results are presented as mean ± SD (n = 10). *, p < 0.05 compared to untreated day 0 controls. (C) Profile of the fibronectin reduction, indicative of MMP-3 activity or release deduced from data shown in B.
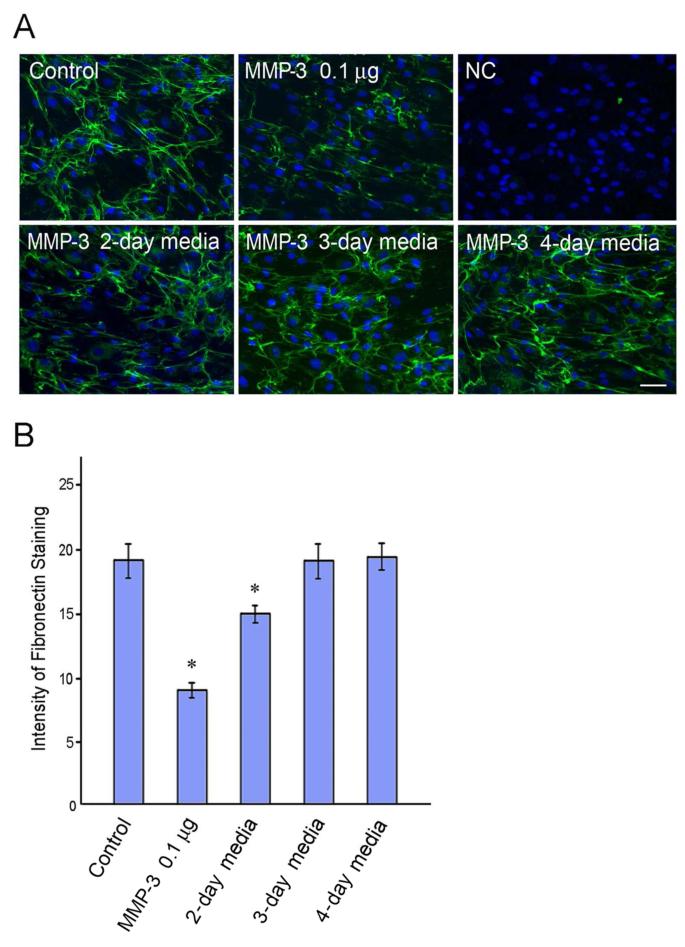
In a control experiment, active MMP-3 fragment (0.1 μg) was added directly to TM cells. After incubation for 2, 3, or 4 days, the media were removed and assayed by the fibronectin fibril bioassay for the enzyme activity remained therein. It was found that the MMP-3 added to the cultures was still active, albeit at a reduced capacity, 2 days later (Figure 8). The enzyme activity was completely dissipated by 3 days, consistent with previous findings.15 The results from Figure 7 thus suggested that MMP-3 was protected by the PLGA shell. The enzyme was released from the microparticles and the released enzyme was active even after 10 days of incubation in culture. It is unclear however whether the loss of MMP-3 beyond day 10 was due to a lack of release or a loss of the enzyme activity.
Figure 8.
Fibronectin staining in human TM cells. (A) Active MMP-3 fragment (0.1 μg) was added to the cells. Media collected 2, 3, and 4 days later were subjected to a fibronectin functional assay. The no addition control (Control) showed strong fibronectin staining, which was markedly reduced by freshly added active enzyme (0.1 μg, positive control). The fibronectin staining was partially reduced by the 2-day media but not by the 3- and 4-day media. NC, negative control, in which the primary antibody was replaced by normal mouse IgG during the immunostaining procedure. The nuclei were stained with DAPI in blue. Scale bar, 20 μm. (B) Quantification of the green fluorescence intensity from images in A. Results are presented as mean ± SD (n = 10). *, p < 0.0001 compared to no addition control.
DISCUSSION
MMPs are a family of enzymes that act to modify or degrade collagen and other ECM molecules.28At least 23 family members have been identified and are categorized into different groups. MMP-1 for example is one of the collagenases and MMP-3 is one of the stromelysins. MMPs have been implicated in outflow resistance in the TM system in relation to glaucoma,10 a major blinding disease. TM cells are known to express a number of MMPs,13,14 and their mRNA and protein levels have been shown to be upregulated in response to mechanical stretching29 and various cytokines and growth factors.14,30In perfusion organ cultures, adding purified MMPs or agents15,16 such as interleukin-1α15 to promote MMP expression enhances the outflow facility and reduces the pressure. Moreover, laser trabeculoplasty, a surgical treatment for glaucoma, induces MMP expression which is believed to be a mechanism mediating the IOP lowering effect of the surgery.31 Among the various MMPs, MMP-3 is of significance since one of its substrates, versican, a large chondroitin sulfate proteoglycan, is believed to be a critical component of the outflow resistance.32
In this study, we present a novel approach to achieve controlled, sustained delivery of MMP-3 to the TM system by revisiting a long established technology using biodegradable polymeric microparticles. PLGA has been commonly used to fabricate devices for controlled and sustained delivery of both small and large biomolecules for various biomedical applications such as cancer and cardiovascular disease.21,33The excellent biocompatibility and safety profile of this copolymer has also extended its application to ocular drug delivery.34-37We herein tested the feasibility of encapsulating active MMP-3 fragment into PLGA microparticles, as a means to control the release of the enzyme to the TM system using cultured human TM cells as the in vitro model. The initial tests were carried out using β-casein for cost-effectiveness, a protein with similar molecular weight and hydrophobicity to that of the active MMP-3 fragment. As revealed by the Kyte-Doolittlescale (http://www.vivo.colostate.edu/molkit/hydropathy/index.html) for delineating the hydrophobic character of proteins, the active MMP-3 fragment and β-casein had similar hydrophobicity, containing respectively, 39.8% and 42.7% hydrophobic amino acid residues.
Both β-casein- and MMP-3-encapsulated microparticles showed uniform particle sizes and homogeneity with a narrow size distribution as revealed by SEM (Figure 1). The encapsulation efficiency was around 45-50%, in the lower range of typical encapsulation efficiency (45-90%) reported for nanoparticles and microparticles.23,38The ratio between the protein and PLGA, the sonication time, and concentrations can be re-optimized to improve the efficiency in future investigations.
In agreement with our previous report,23the PLGA polymeric particles were not toxic to TM cells (Figure 3B). The release profile of β-casein from PLGA microparticles in a shaking incubator was biphasic (Figure 2). A linear release of approximately 50% of the protein was observed within the first 7 days, which was followed by a slower and sustained release profile up to 20 days. These results indicate that the controlled release of macromolecules such as β-casein can be achieved over a long period of time without a significant initial burst release. The biphasic pattern has been documented previously as a result of drug or biomaterial release by diffusion, dissolution, and PLGA biodegradation, or a combination of these processes.23-25 Notably, the release of β-casein was accelerated in tissue culture conditions, reaching approximately 60% in 4 days irrespective of whether TM cells were present (Figure 3A). The acceleration was probably related to several factors. The pH of the release buffer was found to be around 11 in the non-culture shaking incubator with very low CO2, and 8.5 in the culture conditions with 5% CO2. It has been reported that the release from biodegradable polymers such as PLGA is pH-dependent.39-43We found the release to be faster at the lower pH in the culture incubator. This was likely attributed to the presence of esterases and other enzymes released by the cells, which led to faster degradation of PLGA.25 Culture conditions in general have been associated with faster release kinetics of proteins from PLGA microparticles, even without the presence of cells.44 It is also possible that the high pH caused denaturation of β-casein,45 which may have resulted in underestimation of the amount released by the Bradford assay. Nevertheless, the release of β-casein in the more relevant culture conditions was clearly sustained over a prolonged period, and adequately serves as a surrogate for the sustained release of active MMP-3.
In light of the observations that tissue culture conditions give relatively rapid release, future studies may aim to optimize the release rate of PLGA microparticles by adjusting the MW of the copolymer, which is known to influence the degradation rate and release from similar biodegradable polyesters.24
Consistent with the results of β-casein release in tissue culture, MMP-3 was released from microparticles in the presence of human TM cells within one day of incubation. The release was most dramatically observed between days 4 and 6. It is expected that the activity of proteases in TM cultures would degrade the enzyme, causing it to lose its activity. However, the released MMP-3 retained its enzymatic activity, capable of degrading fibronectin as revealed by the bio-functional assay. These results indicate a potential protective role imparted by the PLGA polymeric shell, which has been shown to alter the cellular interaction and uptake kinetics of macromolecules.23,36Such protection presumably allows the MMP-3 molecules to escape from protease digestion and remain active even after 10 days of incubation. The current findings also validate the rationale of using a biodegradable microparticle delivery system to extend the duration of action of therapeutic agents for ocular delivery. This approach would significantly reduce dosage frequency and thus represents a distinct advantage for eventual clinical application. Unlike current glaucoma medications that need to be administered daily, an extended release form of MMP-3 may be tailored for the desired release rate and administration regiments to maximize patient compliance.
The current undertaking represents the first study on the use of a biodegradable microparticle platform to control the release of MMP-3 enzyme. The enzyme activity was maintained throughout the encapsulation process and the MMP-3-encapsulated PLGA microparticles were able to successfully reduce the build up of fibronectin in TM cultures for up to 10 days. Future studies will include testing of the microparticle system in a perfusion organ culture ex-vivo environment as well as in in vivo animal models. The cellular uptake of the microparticles also needs to be investigated. Factors such as the composition (ratio of lactic to glycolic acid) and MW of PLGA, and protein loading also need to be optimized to adjust the degradation and protein release rate for a sustained and yet low level of MMP-3 release to minimize side effects.39Nonetheless, the promising results in this investigation demonstrate the potential for development of a treatment modality for ECM and IOP reduction in glaucoma.
CONCLUSIONS
Active MMP-3 was successfully encapsulated into PLGA microparticles. The enzyme remained active through the encapsulation procedure. MMP-3 released from the microparticles in TM cell cultures also retained its activity, capable of degrading the MMP-3 substrate fibronectin in a bio-functional assay. The release and activity lasted for at least 10 days. The current project demonstrates the feasibility of encapsulating MMP-3 into PLGA microparticles and the potential of developing a novel modality for delivering active MMP-3 enzyme to the TM system to treat glaucoma.
ACKNOWLEDGMENTS
This work was partially supported by the Illinois Society for the Prevention of Blindness, Chicago, IL and the National Eye Institute (EY018828 and EY001792), Bethesda, Maryland. The authors thank Xiang Shen for expert technical assistance.
Footnotes
Notes
The authors declare no competing financial interest.
REFERENCES
- (1).Allingham RR, Liu Y, Rhee DJ. The Genetics of Primary Open-Angle Glaucoma: a Review. Exp. Eye Res. 2009;88:837–844. doi: 10.1016/j.exer.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Wiggs JL. The Cell and Molecular Biology of Complex Forms of Glaucoma: Updates on Genetic, Environmental, and Epigenetic Risk Factors. Invest. Ophthalmol. Vis. Sci. 2012;53:2467–2469. doi: 10.1167/iovs.12-9483e. [DOI] [PubMed] [Google Scholar]
- (3).Quigley HA, Broman AT. The Number of People with Glaucoma Worldwide in 2010 and 2020. Br. J. Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (4).Bill A. The Drainage of Aqueous Humor. Invest. Ophthalmol. 1975;14:153. [PubMed] [Google Scholar]
- (5).Yue BY. The Extracellular Matrix and Its Modulation in the Trabecular Meshwork. Surv. Ophthalmol. 1996;40:379–390. doi: 10.1016/s0039-6257(96)80066-x. [DOI] [PubMed] [Google Scholar]
- (6).Acott TS, Kelley MJ. Extracellular Matrix in the Trabecular Meshwork. Exp. Eye Res. 2008;86:543–561. doi: 10.1016/j.exer.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (7).Stamer WD, Acott TS. Current Understanding of Conventional Outflow Dysfunction in Glaucoma. Curr. Opin. Ophthalmol. 2012;23:135–143. doi: 10.1097/ICU.0b013e32834ff23e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Lütjen-Drecoll E, Shimizu T, Rohrbach M, Rohen JW. Quantitative Analysis of ‘Plaque Material’ in the Inner- and Outer Wall of Schlemm’s Canal in Normal- and Glaucomatous Eyes. Exp. Eye Res. 1986;42:443–455. doi: 10.1016/0014-4835(86)90004-7. [DOI] [PubMed] [Google Scholar]
- (9).Lütjen-Drecoll E, Rittig M, Rauterberg J, Jander R, Mollenhauer J. Immunomicroscopical Study of Type VI Collagen in the Trabecular Meshwork of Normal and Glaucomatous Eyes. Exp. Eye Res. 1989;48:139–147. doi: 10.1016/0014-4835(89)90027-4. [DOI] [PubMed] [Google Scholar]
- (10).Keller KE, Aga M, Bradley JM, Kelley MJ, Acott TS. Extracellular matrix Turnover and Outflow Resistance. Exp. Eye Res. 2009;88:676–682. doi: 10.1016/j.exer.2008.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Tsai JC. A Comprehensive Perspective on Patient Adherence to Topical Glaucoma Therapy. Ophthalmology. 2009;116:S30–36. doi: 10.1016/j.ophtha.2009.06.024. [DOI] [PubMed] [Google Scholar]
- (12).Shingleton BJ, Richter CU, Dharma SK, Tong L, Bellows AR, Hutchinson BT, Glynn RJ. Long-Term Efficacy of Argon Laser Trabeculoplasty. A 10-year Follow-Up Study. Ophthalmology. 1993;100:1324–1329. doi: 10.1016/s0161-6420(93)31480-6. [DOI] [PubMed] [Google Scholar]
- (13).Alexander JP, Samples JR, Van Buskirk EM, Acott TS. Expression of Matrix Metalloproteinases and Inhibitor by Human Trabecular Meshwork. Invest. Ophthalmol. Vis. Sci. 1991;32:172–180. [PubMed] [Google Scholar]
- (14).Pang IH, Hellberg PE, Fleenor DL, Jacobson N, Clark AF. Expression of Matrix Metalloproteinase and Their inhibitors in Human Trabecular Meshwork Cells. Invest. Ophthalmol. Vis. Sci. 2003;44:3485–3493. doi: 10.1167/iovs.02-0756. [DOI] [PubMed] [Google Scholar]
- (15).Bradley JM, Vranka J, Colvis CM, Conger DM, Alexander JP, Fisk AS, Samples JR, Acott TS. Effect of Matrix Metalloproteinases Activity on Outflow in Perfused Human Organ Culture. Invest. Ophthalmol. Vis. Sci. 1998;39:2649–2658. [PubMed] [Google Scholar]
- (16).Pang IH, Fleenor DL, Hellberg PE, Stropki K, McCartney MD, Clark AF. Aqueous Outflow-Enhancing Effect of Tert-Butylhydroquinone: Involvement of AP-1 Activation and MMP-3 Expression. Invest. Ophthalmol. Vis. Sci. 2003;44:3502–3510. doi: 10.1167/iovs.02-0758. [DOI] [PubMed] [Google Scholar]
- (17).Wischke C, Schwendeman SP. Principles of Encapsulating Hydrophobic Drugs in PLA/PLGA Microparticles. Int. J. Pharm. 2008;364:298–327. doi: 10.1016/j.ijpharm.2008.04.042. [DOI] [PubMed] [Google Scholar]
- (18).Jain RA. The Manufecturing Techniques of Various Drug Loaded Biodegradable Poly(Lactude-Co-Glycolide) (PLGA) Devices. Biomaterials. 2000;21:2475–2490. doi: 10.1016/s0142-9612(00)00115-0. [DOI] [PubMed] [Google Scholar]
- (19).Varde NK, Pack DW. Microspheres for Controlled Release Drug Delivery. Expert Opin. Biol. Ther. 2004;4:35–51. doi: 10.1517/14712598.4.1.35. [DOI] [PubMed] [Google Scholar]
- (20).Mundargi RC, Babu VR, Rangaswamy V, Patel P, Aminabhavi TM. Nano/Micro Technologies for Delivering Macromolecular Therapeutics Using poly(D,L-Lactide-Co-Glycolide) and Its Derivatives. J. Controlled Release. 2008;125:193–209. doi: 10.1016/j.jconrel.2007.09.013. [DOI] [PubMed] [Google Scholar]
- (21).Danhier F, Ansorena E, Silva JM, Coco R, Le Breton A, Preat V. PLGA-Based Nanoparticles: An Overview of Biomedical Applications. J. Controlled Release. 2012;161:505–522. doi: 10.1016/j.jconrel.2012.01.043. [DOI] [PubMed] [Google Scholar]
- (22).Sandor M, Enscore D, Weston P, Mathiowitz E. Effect of Protein Molecular Weight on Release from Micron-Sized PLGA Microspheres. J. Controlled Release. 2001;76:2975–311. doi: 10.1016/s0168-3659(01)00446-1. [DOI] [PubMed] [Google Scholar]
- (23).Sunoqrot S, Bae JW, Jin SE, Pearson RM, Liu Y, Hong SP. Kinetically Controlled Cellular Interactions of Polymer-Polymer and Polymer-Liposome Nanohybrid systems. Bioconjug. Chem. 2011;22:466–474. doi: 10.1021/bc100484t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Sunoqrot S, Bae JW, Pearson RM, Shyu K, Liu Y, Kim DH, Hong S. Temporal Control over Cellular Targeting Through Hybridization of Folate-Targeted Dendrimers and PEG-PLA nanoparticles. Biomacromolecules. 2012;13:1223–1230. doi: 10.1021/bm300316n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (25).Sunoqrot S, Liu Y, Kim DH, Hong S. In vitro Evaluation of Dendrimer-Polymer Hybrid Nanoparticles on Their Controlled Cellular Targeting Kinetics. Mol. Pharm. 2013 doi: 10.1021/mp300560n. DOI: 10.1021/mp300-60n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Wilhelm SM, Shao ZH, Housley TJ, Seperack PK, Baumann AP, Gunja-Smith Z, Woessner JF., Jr. Matrix metalloproteinase-3 (stromelysin-1). Identification as the Cartilage Acid Metalloprotease and Effect of pH on Catalytic Properties and Calcium Affinity. J. Biol. Chem. 1993;268:21906–21913. [PubMed] [Google Scholar]
- (27).Wentz-Hunter K, Shen X, Okazaki K, Tanihara H, Yue BY. Overexpression of Myocilin in Cultured Human Trabecular Meshwork Cells. Exp. Cell Res. 2004;297:39–48. doi: 10.1016/j.yexcr.2004.02.024. [DOI] [PubMed] [Google Scholar]
- (28).Lu P, Takai K, Weaver VM, Werb Z. Extracellular Matrix Degradation and Remodeling in Development and Disease. Cold Spring Harb. Perspec. Biol. 2011;3:a00–058. doi: 10.1101/cshperspect.a005058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Bradley JMB, Kelley MJ, Zhu X, Anderson AM, Alexander JP, Acott TS. Effects of Mechanical Stretching on Trabecular Matrix Metalloproteinaseas. Invest. Ophthealmol. Vis. Sci. 2001;42:1505–1513. [PubMed] [Google Scholar]
- (30).Alexander JP, Samples JR, Acott TS. Growth Factor and Cytokine Modulation of Trabecular Meshwork Matrix Metalloproteinase and TIMP Expression. Curr. Eye Res. 1998;17:276–285. doi: 10.1076/ceyr.17.3.276.5219. [DOI] [PubMed] [Google Scholar]
- (31).Parshley DE, Bradley JM, Fisk A, Hadaegh A, Samples JR, Van Buskirk EM, Acott TS. Laser trabeculoplasty Induces Stromelysin Expression by Trabecular Juxtacanalicular Cells. Invest. Ophthalmol. Vis. Sci. 1996;37:795–804. [PubMed] [Google Scholar]
- (32).Keller KE, Bradley JM, Vranka JA, Acott TS. Segmental Versican Expression in the Trabecular Meshwork and Involvement in Outflow Facility. Invest. Ophthalmol. Vis. Sci. 2011;52:50495–057. doi: 10.1167/iovs.10-6948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (33).Formiga FR, Pelacho B, Garbayo E, Abizanda G, Gavira JJ, Simon-Yarza T, Mazo M, Tayamo E, Jauquicoa C, Ortiz-de-Solorzano C, Prosper F, Blanco-Prieto MJ. Sustained Release of VEGF Through PLGA Microparticles Improves Vasculogenesis and Tissue Remodeling in an Acute Myocardial Ischemia-Reperfusion Model. J. Controlled Release. 2010;147:30–37. doi: 10.1016/j.jconrel.2010.07.097. [DOI] [PubMed] [Google Scholar]
- (34).Gavini E, Chetoni P, Cossu M, Alvarez MG, Saettone MF, Ciunchedi P. PLGA Microspheres for the Ocular Delivery of a Peptide Drug, Vancomycin Using Emulsification/Spray-Drying as the Peparation Method: in vitro/in vivo Studies. Eur. J. Pharm. Biopharm. 2004;57:207–212. doi: 10.1016/j.ejpb.2003.10.018. [DOI] [PubMed] [Google Scholar]
- (35).Giordano GG, Chevez-Barrios P, Refojo MF, Garcia CA. Biodegradation and Tissue Reaction to Intravitreous Biodegradable Poly(D,L-Lactic-Co-gGycolic) Acid Microspheres. Curr. Eye Res. 1995;14:761–768. doi: 10.3109/02713689508995797. [DOI] [PubMed] [Google Scholar]
- (36).Mordenti J, Thomsen K, Licko V, Berleau L, Kahn JW, Cuthbertson RA, Duenas ET, Ryan AM, Schofield C, Berger TW, Meng YG, Cleland J. Intraocular Pharmacokinetics and Safety of a Humanized Monoclonal Antibody in Rabbits after Intravitreal Administration of a Solution or a PLGA Microsphere Formulation. Toxicol. Sci. 1999;52:101–106. doi: 10.1093/toxsci/52.1.101. [DOI] [PubMed] [Google Scholar]
- (37).Sinha VR, Trehan A. Biodegradable Microspheres for Protein Delivery. J. Controlled Release. 2003;90:261–280. doi: 10.1016/s0168-3659(03)00194-9. [DOI] [PubMed] [Google Scholar]
- (38).Vauthier C, Bouchemal K. Methods for the Preparation and Manufacture of Polymeric Nanoparticles. Pharm. Res. 2009;26:1025–1058. doi: 10.1007/s11095-008-9800-3. [DOI] [PubMed] [Google Scholar]
- (39).Makadia HK, Siegel SJ. Poly Lactic-Co-Glycolic Acid (PLGA) as Biodegradable Controlled Drug Delivery Carrier. Polymers. 2011;3:1377–1397. doi: 10.3390/polym3031377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (40).Holy C. In vitro Degradation of a Novel Poly(Lactide-Co-Glycolide)75/25 Foam. Biomaterials. 1999;20:1177–1185. doi: 10.1016/s0142-9612(98)00256-7. [DOI] [PubMed] [Google Scholar]
- (41).Zolnik BS, Burgess DJ. Effect of Acidic pH on PLGA Microsphere Degradation and Release. J. Controlled Release. 2007;122:338–344. doi: 10.1016/j.jconrel.2007.05.034. [DOI] [PubMed] [Google Scholar]
- (42).Faisant N, Akiki J, Siepmann F, Benoit JP, Siepmann J. Effects of the Type of Release Medium on Drug Release from PLGA-Based Microparticles: Experiment and Theory. Int. J. Pharm. 2006;314:189–197. doi: 10.1016/j.ijpharm.2005.07.030. [DOI] [PubMed] [Google Scholar]
- (43).Li J, Jiang GQ, Ding FX. The Effect of pH on the Polymer Degradation and Drug Release from PLGA-mPEG Microparticles. J. Appl. Polym. Sci. 2008;109:475–482. [Google Scholar]
- (44).Gorth DJ, Mauck RL, Chiaro JA, Mohanraj B, Hebela NM, Dodge GR, Elliott DM, Smith LJ. IL-1ra Delivered from Poly(lactic-co-glycolic acid) Microspheres Attenuates IL-1beta-mediated Degradation of Nucleus Pulposus in vitro. Arthritis Res Ther. 2012;14(4):R179. doi: 10.1186/ar3932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (45).Qi PX, Wickham ED, Farrell HM., Jr. Thermal and Alkaline Denaturation of Bovine Beta-Casein. Protein J. 2004;23(6):389–402. doi: 10.1023/b:jopc.0000039553.66233.3f. [DOI] [PubMed] [Google Scholar]