Abstract
Objective
The limited success of current smoking cessation therapies encourages research into new treatment strategies. Mind-body practices such as yoga and meditation have the potential to aid smoking cessation and become an alternative drug-free treatment option. The aim of this article is to assess the efficacy of yoga and other meditation-based interventions for smoking cessation, to identify the challenges of clinical trials applying mind-body treatments, and to outline directions for future research on these types of mind-body therapies to assist in smoking cessation.
Method
A systematic review of the scientific literature.
Results
Fourteen clinical trials met the inclusion criteria defined for this review. Each article was reviewed thoroughly, and evaluated for quality, design, and methodology. Although primary outcomes differed between studies, the fourteen articles, most with some limitations, reported promising effects supporting further investigation of the use of these practices to improve smoking cessation.
Conclusions
The literature supports yoga and meditation-based therapies as candidates to assist smoking cessation. However, the small number of studies available and associated methodological problems require more clinical trials with larger sample sizes and carefully monitored interventions to determine rigorously if yoga and meditation are effective treatments.
Keywords: nicotine dependence, cigarette craving, yoga, meditation, mindfulness, systematic review
1. INTRODUCTION
1.1 Prevalence and health problems associated to tobacco smoking
Tobacco smoking is a major preventable cause of premature death and disease. Despite knowledge about its negative health consequences, the global adult cigarette smoking prevalence in 2010 was still 23.7%. Previous declines in smoking prevalence have plateaued since 1990 and, in status quo conditions, prevalence is predicted to be of 22% in 2030 (Mendez et al., 2013). The World Health Organization (WHO) estimates that approximately 5.4 million people die each year due to smoking-related illnesses and an increase to more than 8 million a year is expected by 2030 (Mathers and Loncar, 2006; World Health Organization, 2008a). Smoking causes cancer, heart disease, stroke, and lung diseases (including emphysema, bronchitis, and chronic airway obstruction). Data from the United States, indicate that, for 2000 through 2004, leading causes of smoking-attributable death were cancer (41%), cardiovascular diseases (32.7%), and respiratory diseases (26.3%; Centers for Disease Control and Prevention, 2008).
1.2 Present smoking cessation treatments
As described in the International Classification of Diseases (ICD-10; World Health Organization, 2008b), tobacco is addictive and conforms with the characteristics of a substance abuse disorder: repeated administration, impaired control over use, repeated relapse after quit attempts, high motivation to seek the drug, and physical dependence (tolerance, withdrawal). The majority of adult smokers state that they want to quit smoking (69%) and 52% report having at least one quit attempt within the past year, but only 6.2% are still abstinent one year after quitting (Centers for Disease Control and Prevention, 2011). A number of cessation treatments are available, including behavioral therapies (telephone quit-lines, one-on-one counseling sessions, or cessation clinics, classes, or support groups) and pharmacological approaches. Among non-pharmacological interventions, counseling is the most frequently used approach, but others have also been explored, including mindfulness-based approaches, cognitive behavioral therapy, behavioral activation therapy, motivational interviewing, contingency management, and exposure and/or aversion to smoking (Niaura, 2008; Schlam and Baker, 2013). Approved pharmacological interventions include a variety of nicotine replacement therapies (gum, lozenge, patch, nasal spray and oral inhaler) with effect sizes of 1.60 (1.53, 1.68) as compared to placebo at 6-months follow-up (Stead et al., 2012), the atypical antidepressant bupropion (effect size 1.69 [1.53, 1.85] when compared to placebo with follow-up at 6-months (Hughes et al., 2007)), and varenicline (effect size 2.27 [2.02, 2.55] compared to placebo at 6-months follow-up [Cahill et al., 2012]). However, to date, pharmacological treatments produce side effects (varenicline has been associated with depression and cardiovascular disease [Moore et al., 2011; Singh et al., 2011]), and have shown modest efficacy in the long term (12-month abstinence rates have been lower than 30%; Alberg et al., 2005; Borland et al., 2012; Eisenberg et al., 2008; Hughes et al., 2007; Pierce and Gilpin, 2002; Schlam and Baker, 2013; Tonnesen et al., 2003). Combinations of interventions appear more effective than single approaches, and the combination of pharmacotherapy plus non-pharmacologic interventions is more effective than either method alone (effect size of 1.82 [1.66, 2.00] when compared to a minimal intervention or usual care, and 12-month cessation rates over 30% being reported in the literature [Anthonisen et al., 1994; Stead and Lancaster, 2012]). Therefore, at present, evidence-based recommendations suggest a combination of pharmacological treatments and behavioral methods to improve long-term cessation (Fiore et al., 2008). Maintenance of abstinence is still a major challenge for ex-smokers (Centers for Disease Control and Prevention, 2011; Schlam and Baker, 2013) and underlies the need for identifying additional long-term efficacious smoking cessation treatments.
1.3 CAM treatments for smoking cessation
Complementary and alternative medicine (CAM), including a subset consisting of traditional medicine, is a group of medical, healthcare, and lifestyle practices that are not presently considered to be part of conventional medicine in the country’s dominant healthcare system (National Center for Complementary and Alternative Medicine, 2008a; World Health Organization, 2000). In the past decade there has been renewed attention and interest in the use of CAM globally (Harris et al., 2012). A survey-based study showed that a significant percentage of smokers (27%) use CAM in addition to, or as replacement of, conventional smoking cessation treatments (Sood et al., 2006). In addition, 67% of smokers seeking treatment indicate that they would be interested in using CAM practices such as yoga, meditation or massage to relieve stress and help them quit smoking (Sood et al., 2006).
CAM therapies are typically not reliant on expensive technology or equipment. This supports the idea that CAM may provide more cost-effective treatments than conventional medicine, with the exception of those that might involve longer practitioner time. However, there are limited cost-effectiveness studies on CAM approaches mainly due to methodological difficulties associated with outcomes that can be challenging to assess using standard medically-oriented measures (Hollinghurst et al., 2008; Mason et al., 2002). The interest, growing availability, and increased usage of CAM (Barnes et al., 2008; Furlan et al., 2012; Kooreman and Baars, 2012), together with the potential for lower implementation cost, underscore the need for clinical trials to evaluate the efficacy of mind-body interventions for smoking cessation.
1.4 Mind-body practices
Mind-body therapies focus on the interactions among brain, mind, body, and behavior to affect physical functioning and promote health (National Center for Complementary and Alternative Medicine, NCCAM). Among mind-body practices, deep breathing, meditation, and yoga showed an increase in use between 2002 and 2007 in the United States, 12.7% of adults had used deep-breathing exercises, 9.4% had practiced meditation, and 6.1% had practiced yoga (Barnes et al., 2008; Nahin et al. 2007). Although the majority of reported use is to treat pain conditions, over 40% of adults with neuropsychiatric symptoms use mind-body therapies, with more symptoms associated with increased use, as compared to 30% use by adults without neuropsychiatric symptoms (Purohit et al., 2013). Examples include depression, anxiety, attention deficit disorder, and insomnia (Balasubramaniam et al., 2012; D'Silva et al., 2012; Grant et al., 2013; Khalsa, 2004). Despite the increase in the number of scientific studies and clinical trials assessing the therapeutic effects and feasibility of mind-body treatments, there is further need for research to determine the efficacy and cost-effectiveness of implementation, as well as identify the mechanisms by which these practices have their efficacious effects.
Mind-body practices include meditation (mantra meditation, mindfulness meditation, and others), qi gong, tai chi, and yoga (Ospina et al., 2008). In general, meditation practices are based on promoting a non-judgmental and non-reactive state of awareness that in the long-term may improve one’s ability to modify automatic behaviors (Kabat-Zinn, 2005). Internal qi gong is a traditional Chinese medicine practice of self-regulation that combines different breathing patterns with physical postures, and meditation techniques (Jahnke et al., 2010). Tai chi also has its roots in traditional Chinese medicine emphasizing dynamic balance between opposing phenomena with practitioners moving slowly with awareness, while breathing deeply (Jahnke et al., 2010). Yoga is an ancient Indian system of philosophy and practice that trains body and mind to attain physical, emotional, and spiritual health. In the West, yoga is a practice that typically combines breathing exercises, physical exercise, and meditation (Desikachar, 1999; Iyengar, 1995; McCall, 2007).
To date, benefits from yoga and meditation treatments have been suggested for anxiety and mood disorders, chronic pain, depression, addiction, sleep disturbances, stress, immune imbalances and a number of musculo-skeletal conditions, amongst others (Chiesa and Serretti, 2011; Field, 2011; Garland et al., 2010; Hofmann et al., 2010; Kiecolt-Glaser et al., 2010; Kozasa et al., 2010; Oken et al., 2004; Piet and Hougaard, 2011; Pullen et al., 2008; Sherman et al., 2011; Uebelacker et al., 2010; Wahbeh et al., 2008; Wren et al., 2011; Zeidan et al., 2012). Randomized controlled trials (RCTs) have suggested that yoga and meditation practices act on the hypothalamic–pituitary–adrenal axis (HPA) axis to reduce cortisol levels in plasma (Brand et al., 2012; Vadiraja et al., 2009; Vedamurthachar et al., 2006; West et al., 2004), as well as reduce sympathetic nervous system tone, increase vagal activity (Bernardi et al., 2000; Riley, 2004), and elevate brain γ-aminobutyric acid (GABA) levels (Streeter et al., 2010). Research on the neurobiology of substance abuse disorders indicates that chronic drug use is associated with deregulated prefrontal-dependent cognitive control, which may impact affect and inhibitory pathways (Koob and Volkow, 2010). Neuroimaging data suggest mindfulness practice has the capacity to modify and enhance mechanisms of cognitive control of automatic behaviors (also known as top-down neural activity) which could help reduce reactivity towards nicotine and, consequently, aid smoking cessation (Allen et al., 2012; Cahn and Polich, 2006; Farb et al., 2007; Lazar et al., 2005).
1.5 Advantages of mind-body interventions for smoking cessation
A number of aspects make mind-body interventions promising for increasing cessation success. (1) Breath. As part of a yoga practice or a seated meditation, attention to the breath cycle can reduce anxiety, stress and reactivity, and become a beneficial, low-risk, and low-cost adjunct treatment for substance abuse (Brown and Gerbarg, 2005, 2009). Furthermore, the Public Health Service and smokers themselves cite paying attention to the breath cycle and breathing deeper and fuller as a strategy for coping with withdrawal symptoms during smoking cessation (O'Connell et al., 1998). The slowing down of the breath cycle has a direct effect on the parasympathetic nervous system inducing a state of relaxation as opposed to the ‘fight or flight’ response induced by the sympathetic branch of the autonomous nervous system (Bernardi et al., 2000; Conrad et al., 2007). (2) Physical body. Yoga improves cardiopulmonary fitness, flexibility, balance, muscle strength, and endurance (Oken et al., 2006; Raub, 2002; Tran et al., 2001). An essential component of yoga practice is physical movement, the pace and intensity of which varies between styles (e.g., hatha yoga, vinyasa yoga, yin yoga). Exercise and movement have been proposed as aids to smoking cessation because of the capacity to enhance mood, reduce negative affect and decrease the severity of withdrawal symptoms (Bock et al., 1999; Scully et al., 1998; Ussher et al., 2000). Most interestingly, in addition to providing coping skills, yoga and meditation can increase knowledge of the human body, and promote appreciation, acceptance, self-respect, and lead to a healthier lifestyle that might include smoking cessation. (3) Mindfulness. The practice of mindfulness and meditation is a central aspect of mind-body interventions. Mindfulness involves self-regulation of attention to immediate experience, adopting a particular orientation toward one’s experiences in the present moment characterized by curiosity, openness, and acceptance (Bishop et al., 2004). Trait mindfulness has been inversely associated to severity of nicotine dependence and withdrawal, and positively associated to smoking cessation self-efficacy (Vidrine et al., 2009). A consequence from a consistent mind-body practice is self-knowledge, an essential factor for decreasing automatic behavior. In this line, the well-established association between smoking behavior and impulsivity, (Mitchell, 1999), suggests that the reduced reactivity and increased awareness associated with mindful practices might counteract the impulsive behaviors that prevent smokers from successfully quitting. Other advantages of mind-body interventions for smoking cessation include: (4) mind-body interventions are not limited to ‘ill’ populations or the clinical setting and are free from the ‘illness treatment‘ label or stigma that might prevent some individuals from pursuing help and limit their capacity to successfully quit smoking (Ross and Thomas, 2010; Wolever et al., 2012); (5) yoga and meditation classes are broadly available and relatively affordable (Sobel, 2000; Wahbeh et al., 2008); (6) mind-body practices can complement conventional treatments (Astin et al., 2003; Elkins et al., 2010; Kozasa et al., 2010); (7) mind-body practices can be tailored to satisfy the needs of groups with special concerns (elderly populations, physical limitations, mental disorders, pregnancy, etc.) (Beddoe and Lee, 2008; Kaley-Isley et al., 2010; Krisanaprakornkit et al., 2010; Oken et al., 2004; Oken et al., 2006; Senders et al., 2012); and (8) when taught by an experienced teacher, these practices are relatively safe and individually adaptable (National Center for Complementary and Alternative Medicine, 2006, 2008b; Ventegodt and Merrick, 2009).
1.6 How do mind-body practices complement smoking cessation?
Drug dependence is associated with increased reactivity to drug-related stimuli through activation of mesolimbic reward circuits that override more elaborate cognitive processes (bottom-up neural activity) (Bradley et al., 2008; Nestor et al., 2011). In addition, drug-related cues elicit a strong attentional bias that may be implicit in maintaining addictive behaviors and contributing to relapse (Bradley et al., 2008; Waters et al., 2003). Recently, neuroimaging data has shown that current smokers have less neural activity in cortical regions associated with attentional and cognitive control, and more activity in subcortical areas of the limbic system than non-smokers and ex-smokers (Nestor et al., 2011). Furthermore, ex-smokers showed increased prefrontal activity compared to smokers or controls, suggesting that successful cessation might involve increases in cognitive control to restrain from cigarette smoking and avoid relapse (top-down neural activity; Nestor et al., 2011). It is known that mind-body interventions increase top-down cognitive control, awareness of automaticity, cognitive flexibility, emotional regulation, and the capacity to re-orient attention (Allen et al.,2012), in addition to reducing cue-reactivity and conditioned responses (Garland et al., 2010). Therefore, if proven effective, mind-body treatments can support smoking cessation by increasing cognitive control, by reducing reactivity to smoking cues and nicotine withdrawal, by providing a method to cope with stress and cigarette craving, and by enhancing mood and quality of life. The lifelong aspect of these practices can reinforce non-smoking once treatment ends.
1.7 Why a systematic review of mind-body interventions for smoking cessation?
As participation rates in mind-body programs such as yoga or mindfulness meditation continue to increase (Barnes et al., 2008; Nahin et al., 2009), it is imperative that we learn more about their therapeutic benefits and potential applications. Thus, with this purpose, reviews of the mind-body literature such as this one are timely and important in identifying all relevant studies, synthesizing results, evaluating and interpreting the findings, and providing suggestions for future research. Through a systematic review of the scientific literature, the present paper analyzes the feasibility of mind-body interventions in smoking cessation treatments. The main aims of this review are (1) to assess the effectiveness of yoga, meditation, and breathing exercises to aid cessation, (2) to describe some of the major challenges encountered by smoking cessation trials that use mind-body practices, and (3) to identify directions for future studies examining yoga and meditation as smoking cessation treatments or adjuvant treatments.
2. METHODS
2.1 Literature Search
We performed a review of existing literature published between 1946 and 2012 using the search terms: yoga, meditation, mindfulness, mind-body, pranayama, smoking, tobacco, and nicotine in various combinations as needed in order to maximize our capacity to identify all relevant studies. We performed searches to specifically address tai chi and qi gong interventions for smoking cessation, but these yielded no results. Only English-written peer-reviewed articles were considered. Databases searched were: Ovid MEDLINE(R), PsycINFO, EBM Reviews Cochrane Central Register of Controlled Trials 2011, PubMed, Scopus, and Google Scholar. The search included references from retrieved articles that had been selected for further review. The abstract content was used to determine their relevance. Literature searches ended January 2013.
2.2 Article selection
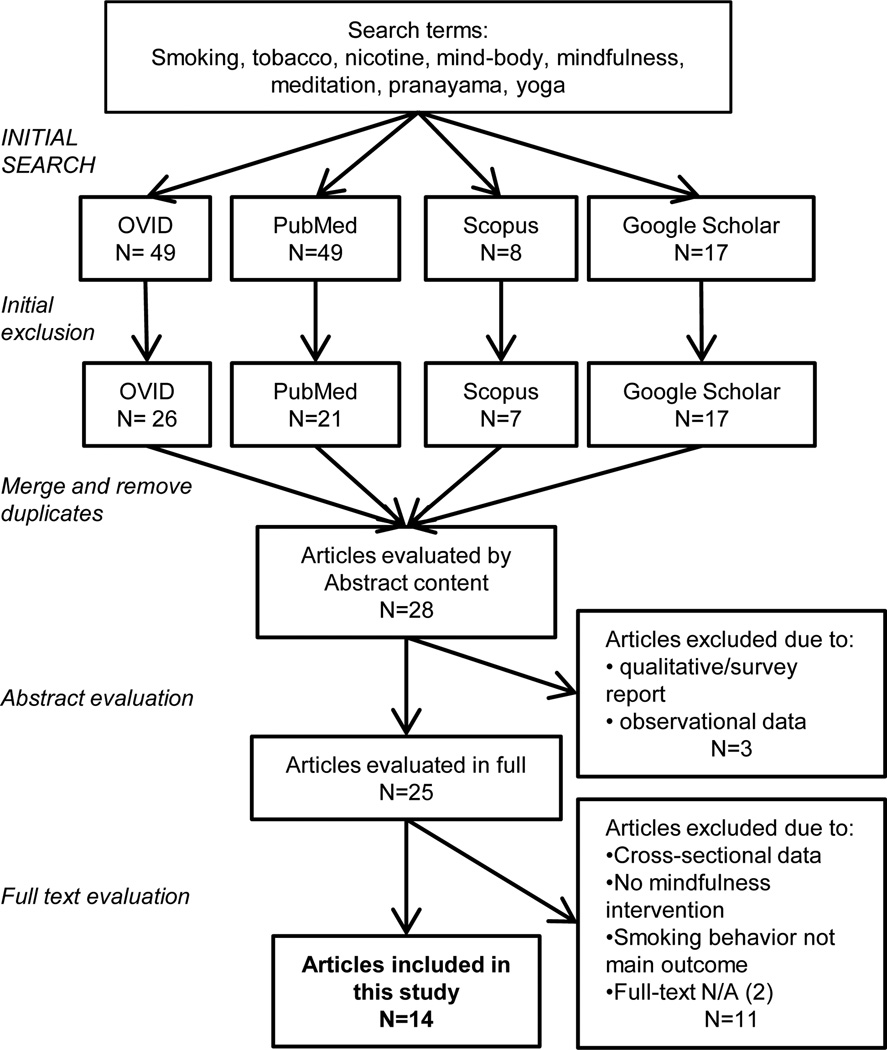
To be selected, studies had to assess a mind-body intervention such as yoga, meditation, breathing, tai chi, or qi gong using a study population of tobacco smokers. Studies had to focus on smoking behavior or related predictors of smoking as the primary outcome. Study designs included non-controlled trials as well as controlled studies with or without randomization. Exclusion criteria were: review articles, survey reports, multifaceted interventions in which the intervention of interest was part of a lifestyle modification that included exercise, diet, etc. A flow of the selection process can be found in Figure 1. The main features of the studies included in this review are shown in Table 1.
Figure 1.
Flowchart of article eligibility and final inclusion in this systematic review.
Table 1.
Summary of studies included in this systematic review. Studies are grouped according to study design: rows 1–8 are RCTs (randomized controlled trial), rows 9–11 are CTs (controlled trial), and rows 12–14 are Pre-post designs.
| Reference | Study design | Study population | Active intervention | Control condition/s | Outcome measure | Findings |
|---|---|---|---|---|---|---|
| Elibero et al. 2011 | 3-arm RCT | Not intending to quit smokers |
Hatha Yoga n=26; Exercise n=25 |
Watch video n=25 |
Cigarette craving |
Active interventions vs. control comparison Attenuation of cigarette cravings: Hatha yoga (p<0.05), Exercise (p<0.05) |
| Ussher et al. 2009 | 3-arm RCT | Adult smokers | Isometric exercise (IE) n=14 Body Scan(BS) n=18 |
Natural history audio n=16 |
Desire to smoke |
Active interventions vs. control comparison Decreased desire to smoke: IE (p=0.009) and BS (p=0.044) |
| Shahab et al. 2013 | 2-arm RCT | Adult smokers | Yogic breathing n=48 | Watch video about yogic breathing n=48 |
Cigarette craving |
Active intervention vs. control comparison Lower strength of craving (p<0.001) post intervention |
| Bock et al. 2011 | 2-arm RCT | Intending to quit female smokers |
Vinyasa Yoga + CBT n=55 |
Wellness + CBT n=23 |
Smoking abstinence |
Active intervention vs. control comparison 7-day ppa 40.6% vs. 13% at 8-week (p=0.03) 21.9% vs. 8.7% at 12-week (p=0.012) |
| Brewer et al. 2011 | 2-arm RCT | Treatment-seeking adult smokers |
Mindfulness training n=41 |
Smoking cessation n=47 |
Smoking abstinence |
Active intervention vs. control comparison: 7-day ppa 35% vs. 15% at 4-week (p=0.063) 30% vs. 5% at 17-week (p=0.012) |
| Rogojanski et al. 2011 | 2-arm RCT | Adult smokers | Cue-exposure + Mindfulness n=31 |
Cue-exposure + Thought suppression n=30 |
Smoking amount at 7-day post |
Pre vs. post intervention comparison: 20% decrease in cigarettes/day (p<0.001) Active intervention vs. control comparison No differences between conditions (p=0.17) |
| Bowen et al. 2009 | 2-arm RCT | Adult smokers | Cue-exposure + Mindfulness n=61 |
Cue-exposure + Usual coping n=62 |
Smoking amount at 7-day post |
Active intervention vs. control comparison: 26% decrease in cigarettes/day vs. 11% (p=0.002) at 7- day follow-up |
| Cropley et al. 2007 | 2-arm RCT | 12h abstinent smokers |
Body Scan n=15 |
Natural history passage n=15 |
Desire to smoke |
Active intervention vs. control comparison: Decreased desire to smoke (p<0.001) |
| Westbrook et al. 2011 | CT (within subject, 3 conditions) |
12h abstinent smokers |
Cue-exposure + Mindfulness n=47 |
Cue-exposure or Neutral- cue + Usual coping n=47 |
Cigarette craving |
Active intervention vs. control comparison Reduced craving (p<.001). |
| McClernon et al. 2004 | CT (within subject, 2 conditions) |
Adult smokers |
Controlled deep breathing n=21 |
Sitting quietly n=21 |
Cigarette craving |
Active intervention vs. control comparison Decreased craving (p=0.002) and negative affect (p=0.002) |
| Royer 1994 | 2-arm CT | Adult smokers |
TM n=110 |
No treatment n=214 |
Smoking abstinence |
Active intervention vs. control comparison: 51% abstinence vs. 21% (p=0.003) at 2-year follow-up |
| Davis et al. 2007 | Pre-post | Smokers motivated to quit |
MBSR n=18 |
n/a | Smoking abstinence |
Pre vs. post intervention comparison: 55.6% 7-day ppa at 6-week post |
| Kochupillai et al. 2005 | Pre-Post | Tobacco users |
Sudarshan Kriya breathing n=82 |
n/a | Smoking abstinence |
Pre vs. post intervention comparison: 21% (17/82 ) abstinence at 6-month |
| McIver et al. 2004 | Pre-Post | Inpatient not intending to quit smokers |
Hatha Yoga n=20 |
n/a | Stage of change |
Pre vs. post intervention comparison: Shift towards intention to stop smoking Page 47 of 49 |
The intervention is highlighted in bold. Other acronyms are: CBT, cognitive behavioral therapy; TM, transcendental meditation; MBSR, mindfulness-based stress reduction; ppa, point prevalence abstinence.
2.3 Outcome measures
Due to limitations in the number of studies assessing mind-body practices for smoking cessation, we included all studies for which one of the main outcomes was some measure of smoking behavior or predictor of smoking. Therefore, outcome measures varied between studies and included abstinence rates, changes in intention to quit smoking, withdrawal symptoms, and intensity of cravings to smoke.
2.4 Data extraction and quality assessment
A formal meta-analysis of the literature was not feasible because of the differences in study population, study design and outcome measures. Instead, we used a qualitative systematic review approach to assess the effect of mind-body practices on smoking and to explore future directions for mind-body and nicotine addiction research. Data were extracted from the original reports by the authors. The quality of each article was rated using the Scale for Assessing Scientific Quality of Investigations in CAM (SASQI-CAM) (Meeks et al., 2007). The SASQI-CAM tool has been devised to assess specifically the quality of studies that use CAM interventions taking into consideration the difficulties in CAM research for masking group assignment and setting up appropriate control conditions. The resulting score is a numerical value between 0 and 21. A SASQI score above 9 has been considered of sufficient scientific quality (D'Silva et al., 2012). One of the authors, LC-T, evaluated and scored all the eligible articles. Four articles were chosen randomly and reviewed by both LC-T and SHM. Scoring was compared and any discrepancies were discussed (the inter-rater correlation was 0.86). Disagreements in the evaluation of the articles were solved with a ―tie-breaker vote‖ provided by BSO.
3. RESULTS
3.1 Characteristics of included studies
The original literature search yielded a total of 124 articles, which included duplicated records. A first round of filtering and duplicate removal excluded 96 articles. Twenty-eight papers were evaluated with more detail beginning with the Abstract section. Twenty-five of them were subsequently evaluated in full. Qualitative papers and survey reports were excluded, as well as those applying cross-sectional designs, or presenting observational data (Rogojanski et al., 2011b; Vidrine et al., 2009). We excluded articles in which smoking behavior or a predictor was not a primary inclusion criteria or outcome (Haaga et al., 2011). We considered a broad definition for smoking behavior, did not add study design to our inclusion/exclusion criteria, and did not limit the type or duration of the intervention. However, we did exclude all studies in which there were multifaceted interventions or in which smoking cessation and mind-body practices were both part of the intervention. For example, a number of studies implemented smoking cessation programs that included diet, education material, exercise, yoga, help lines, and peer support (Sussman et al., 2004; Zheng et al., 2004), and others analyzed the effectiveness of lifestyle changes that included quitting smoking and, for example, practicing yoga, amongst others, to treat hypertension (Arya, 2000; Silverberg, 1990), to improve menopausal symptoms (Maclennan, 2009), to manage diabetes (Sahay and Sahay, 2002), or for cardiac rehabilitation (Jatuporn et al., 2003).
Fourteen studies were eligible to be included (Table 1). Out of fourteen, three studies applied yoga, three used breathing techniques, and eight focused on meditation. It is important to note that the interventions are not mutually exclusive and share numerous aspects and components (i.e., yoga includes physical movement, meditation and breathing exercises; meditation includes breath awareness; tai chi and qi gong both include movement of the body). In addition, each practice has many styles and variations (e.g., vinyasa yoga, restorative yoga, kundalini yoga). Most were randomized controlled clinical trials (8 out of 14). Of the rest, one was a nonrandomized controlled trial, two studies applied within subject controlled designs, and three used pre-post designs. Eight studies applied acute one-time interventions, whilst the remaining used a number of training sessions that ranged between 4 and 16. For example, acute effects of a one-time 30-minute yoga session on cigarette craving (Elibero et al., 2011), in contrast to smoking cessation in an 8-week twice a week yoga training (Bock et al., 2012). There were also substantial differences in follow-up periods between studies. Generally acute one-time interventions had no follow up (Cropley et al., 2007; Elibero et al., 2011; McClernon et al., 2004; McIver et al., 2004; Ussher et al., 2009; Westbrook et al., 2013). Studies assessing amount of smoking post intervention (7-day point prevalence abstinence, number of cigarettes smoked per day, or percentage of abstinent participants) applied follow up periods that ranged from 7-days to 2-years (Bock et al., 2012; Bowen and Marlatt, 2009; Brewer et al., 2011; Davis et al., 2007; Kochupillai et al., 2005; Rogojanski et al., 2011a; Royer, 1994).
We found differences within each intervention category regarding style, length, guidance, and session setting (group or one-on-one). For example, the yoga intervention was defined as hatha yoga, a slow paced practice, in 2 studies (Elibero et al., 2011; McIver et al., 2004), and as vinyasa yoga, a more dynamic style, in 1 study (Bock et al., 2012). Within the meditation intervention, five out of eight studies used mindfulness meditation techniques (Bowen and Marlatt, 2009; Brewer et al., 2011; Davis et al., 2007; Rogojanski et al., 2011a; Westbrook et al., 2013), two used body scan practices, a cognitive relaxation technique focused on guiding attention to different parts of the body, (Cropley et al., 2007; Ussher et al., 2009), and one applied Transcendental Meditation training (TM; Royer, 1994). The three papers that applied breathing techniques also differed in length (one-time vs. 6-day training), style (deep breathing, yogic breathing, or Sudarshan Kriya and Pranayam training), and group vs. individual setting (Kochupillai et al., 2005; McClernon et al., 2004; Shahab et al., 2013).
3.2 Characteristics of the study sample
Study populations differed dramatically between studies regarding age, gender, smoking amount and quitting status. One study limited recruitment to middle age female smokers that intended to quit tobacco smoking (Bock et al., 2012); and at least three more studies used smokers intending to quit (Brewer et al., 2011; Davis et al., 2007; Westbrook et al., 2013). The remaining studies used active smokers, but few specified whether or not they were intending to quit or would like to in the future. Sample sizes were modest ranging from 15 to 110 participants in the active arm of the intervention. The amount of daily smoking and the level of nicotine dependence differed between studies. The majority assessed heavy smokers, ranging between 10 and 29 cigarettes/day.
3.3 Primary outcome measure: smoking behavior and related predictors
Our systematic review included all studies that reported some kind of smoking behavior or predictor of smoking behavior outcome (e.g. days of abstinence, cigarette craving, smoking amount, withdrawal symptoms, or Prochaska’s stages of change (Prochaska et al., 1992)). Five out of 14 studies reported smoking abstinence rates post-treatment in the 21% to 56% range (Bock et al., 2012; Brewer et al., 2011; Davis et al., 2007; Kochupillai et al., 2005; Royer, 1994). Six studies analyzed the impact of mind-body practices on cigarette craving and desire to smoke (Bowen and Marlatt, 2009; Cropley et al., 2007; Elibero et al., 2011; McClernon et al., 2004; Shahab et al., 2013; Ussher et al., 2009; Westbrook et al., 2013) finding reductions in both outcomes. In addition, two studies reported 20% and 26% decreases in the number of cigarettes smoked per day (Bowen and Marlatt, 2009; Rogojanski et al., 2011a). Smokers with no initial intention to quit that practiced yoga advanced a stage in Prochaska’s stages of change scale (McIver et al., 2004).
Despite the differences in the outcome measures and quality of studies, all 14 studies showed some positive results related to smoking cessation (Table 1).
3.4 Characteristics of interventions
Within intervention category (yoga, meditation, breathing) there were differences regarding style, syllabus, number and duration of sessions, group setting, or presence of instructor. With the exception of the Mindfulness-Based Stress Reduction program (MBSR; Kabat-Zinn, 1982) and TM based interventions, for which there is a standardized curriculum and teacher certification, most papers provided insufficient detail about the intervention to allow for accurate replication or to be applied in clinical settings. Meditation interventions encompassed, for example, a one-time 10 minute body-scan (Cropley et al., 2007; Ussher et al., 2009); a 4-day TM training with a follow-up practice of 20 minutes/day (Royer, 1994); or the full 8-week MBSR course that includes daily homework and a day-long retreat (Davis et al., 2007). A similar situation was found with the studies using yoga interventions. Two out of three studies implemented weekly yoga classes lasting 5 or 8 weeks (Bock et al., 2012; McIver et al., 2004), and one study utilized a 30 minute video to guide participants through a one-time only hatha yoga practice (Elibero et al., 2011). Studies applying one-time interventions (meditation, yoga, or breathing techniques) tended to assess changes in desire to smoke, cigarette craving, and/or withdrawal symptoms, critical factors for smoking cessation.
Compared to short-term interventions, longer interventions are more feasible to support achieving full cessation. However, long term interventions require a significant commitment on the participant’s behalf. Therefore, in these types of interventions it is essential to monitor adherence and compliance to treatment. Out of six studies that applied multiple visit interventions, four addressed adherence and compliance in their analysis (Bock et al., 2012; Brewer et al., 2011; Davis et al., 2007; Royer, 1994). Using correlation analysis, there was an inverse relationship between time of meditation practice and number of cigarettes/day (Brewer et al., 2011). Two studies showed that adherence to treatment, meditation in this case, is strongly associated with smoking abstinence, decreased perceived stress, and reduced affective distress (Davis et al., 2007; Royer, 1994).
3.5 Other aspects to consider
3.5.1 Control conditions
Eleven out of 14 studies included control conditions. The type of control varied between studies and included passive controls such as wait-lists, no-treatment, or usual care (Bowen and Marlatt, 2009; McClernon et al., 2004; Royer, 1994; Westbrook et al., 2013), and more active interventions such as watching a video, listening to a passage, attending a wellness program, following an already established smoking cessation treatment, or learning different strategies (e.g., thought suppression) (Bock et al., 2012; Brewer et al., 2011; Cropley et al., 2007; Elibero et al., 2011; Rogojanski et al., 2011a; Shahab et al., 2013; Ussher et al., 2009). Credibility of the control condition was only assessed in four studies (Bock et al., 2012; Elibero et al., 2011; Rogojanski et al., 2011a; Royer, 1994). Two studies used a 3-arm design that included an active control condition (exercise program).
3.5.2 Adverse events
None of the studies reported any adverse event from the intervention.
3.5.3 Article quality
We used the Scale for Assessing Scientific Quality of Investigations in CAM (SASQI-CAM) to evaluate the studies (Table 2). The average SASQI score was highest for the meditation papers (14/21), followed by yoga (12/21), and breathing (9/21). Taken together, mind-body articles included in this review had an average quality score of 11/21. As expected the SASQI score was higher when only considering RCTs (16/21).
Table 2.
Study quality ratings using the Scale for Assessing Scientific Quality of Investigations in CAM (SASQI-CAM).
| Reference | Score | Type of intervention |
Study design | |||
|---|---|---|---|---|---|---|
| Elibero et al. 2011 | 14/21 | Hatha Yoga | RCT | |||
| Ussher et al. 2009 | 15/21 | Body Scan | ||||
| Shahab et al. 2013 | 14/21 | Yogic breathing | ||||
| Bock et al. 2011 | 14/21 | Vinyasa Yoga | ||||
| Brewer et al. 2011 | 17/21 | Mindfulness training |
||||
| Rogojanski et al. 2011 | 12/21 | Mindfulness | ||||
| Bowen et al. 2009 | 15/21 | Mindfulness | ||||
| Cropley et al. 2007 | 13/21 | Body Scan | ||||
| Westbrook et al. 2011 | 14/21 | Mindfulness | CT | |||
| McClernon et al. 2004 | 10/21 | Controlled deep breathing |
||||
| Royer 1994 | 14/21 | TM | ||||
| Davis et al. 2007 | 13/21 | MBSR | Pre-post | |||
| Kochupillai et al. 2005 | 4/21 | Sudarshan Kriya breathing |
||||
| McIver et al. 2004 | 9/21 | Hatha Yoga | ||||
RCT, randomized controlled trial; CT, controlled trial; TM, transcendental meditation; MBSR, mindfulness-based stress reduction.
4. DISCUSSION
4.1 Are mind-body practices effective to treat nicotine addiction?
Overall, this systematic review found that current mind-body research suggests that mind-body interventions have the potential to help reduce cigarette smoking and therefore, aid smoking cessation. All fourteen papers included in this review observed changes in smoking behavior or in predictors of smoking behavior that could be beneficial for smoking cessation (e.g., abstinence, decreased number of cigarettes smoked, lower intensity of cravings, changes in attitude regards smoking). However, the scarcity of papers, low quality of some publications as indexed by the SASQI, and the numerous limitations of the studies (e.g., reduced sample size, limitations of study design, lack of adherence monitoring, lack of objective measures, inadequate or absent control conditions, absence of blinding) hinder drawing any definite conclusions.
Three factors prevented us from performing a meta-analysis to evaluate the effectiveness of these practices for smoking cessation. First, there were important differences in research design between studies. Out of fourteen eligible studies, only eight were RCTs with different number of study arms. Second, study populations varied widely regarding nicotine dependence, smoking amount, and intention to quit. For example, one study recruited heavy smokers with no intention to quit, another targeted middle-aged women smokers that wanted to stop smoking, and others used temporarily abstinent not-intending-to-quit smokers. Lastly, there was little overlap in primary outcome measures between studies. Primary measures were: craving to smoke, smoking abstinence, desire to smoke, number of cigarettes/day, and change in attitude towards smoking.
4.2 Challenges of mind-body interventions
4.2.1 Control condition
The selection of an appropriate control condition in mind-body research is a critical task. No-treatment, treatment-as-usual, and wait-list controls account for the natural course of the primary outcome measure, but are not effective in controlling for placebo effects or effects due to attention, personal contact, physical movement, and engagement in an activity. Furthermore, ethically, no-treatment is not always an acceptable alternative (Hughes, 2009). Multiple arm studies that incorporate an active placebo in addition to the no-treatment or wait-list control, allow for head-to-head efficacy comparisons between different interventions or levels of intervention under similar circumstances (Elibero et al., 2011; Ussher et al., 2009). The main disadvantage for such study designs is that they require larger sample sizes to achieve the same power as a traditional two-arm trial. Typical control conditions for meditation practices include wellness classes, listening to an audio, or learning a different coping strategy (Jain et al., 2007; MacCoon et al., 2012; Roberts-Wolfe et al., 2012). Active control conditions for yoga interventions are usually some kind of physical exercise (de Godoy et al., 2006; Oken et al., 2004; Sherman et al., 2011; Sinha et al., 2007). There is evidence of the benefits of exercise for smoking cessation (Ussher et al., 2009), and although recent papers support that yoga provides more benefits than exercise (Smith et al., 2011), clinical trials are still needed to determine if the differences between yoga and exercise account for differences in smoking cessation outcomes. Alternatives to three-arm designs include testing the new treatment as an add-on to an existing proven treatment (Bock et al., 2012), using unequal randomization, or dismantling interventions to compare full treatments to components of that same treatment (for a more exhaustive discussion of control conditions in smoking cessation clinical studies see Hughes, 2009).
4.2.2 Bias
Recruitment bias is a concern in clinical studies of behavioral interventions. More specifically, personal beliefs about yoga or meditation, inclination or aversion for the practices, and personal preferences, can significantly bias the sample population and compromise the generalizability of the results (Andrade, 1995; Wragg et al., 2000). For example, advertisements containing explicit references to mind-body practices or to the study hypothesis have the potential to encourage a certain segment of the population to participate and, at the same time, discourage another. It is important to acknowledge this potential for bias during recruitment and describe the specific measures taken to minimize it. In general, the papers in this review described their recruitment strategies very superficially. Insufficient information was provided about how the authors avoided recruitment bias (e.g., how, who, and when, was the study presented to participants, or what was the wording of advertisements). There was limited discussion about the potential influence of recruitment bias on the study sample, participant’s expectancy of treatment, or the study’s results.
4.2.3 Blinding
Blinding of participants is not usually feasible in yoga or meditation interventions. Therefore, strategies need to be applied to compensate for such a limitation including maintenance of equipoise. First, both the experimental and control condition should be equally believable and acceptable to participants. Second, it is important to implement blinding of assessors and data analysts. Third, other strategies should be applied to minimize bias such as not releasing the research question, limiting participant interchange of experiences (especially between study groups), or adding an expectancy and credibility questionnaire before and after group assignment. In general, blinding was insufficiently discussed in the selected papers.
4.2.4 Participant drop-outs and adherence to treatment
Despite drop-outs being less of an issue for one-time interventions, ideally this aspect of the research should be mentioned in the article. In the case of multiple visit/session interventions it is essential to report drop-out and adherence rates. Because mind-body interventions require greater effort from participants to adhere to treatment, reporting adherence rates and investigating strategies to maximize it require special attention (Flegal et al., 2007). One strategy to maximize adherence is to use inpatient settings (McIver et al., 2004). However, in such cases it is important to take into account that this requires a compromise between adherence and generalizability because one of the main limitations of such an approach is the extrapolation of results to the general population and the potential for confounding by co-existing disorders (e.g. mental health issues and substance use disorders). Other strategies are to implement interventions in the workplace (e.g., hospital staff), as well as offering suitable compensations for completing participation.
4.2.5 Mind-body intervention
The interventions were heterogeneous and generally only briefly described in the methodology sections of the papers. To facilitate implementation and accurate replication of interventions by other studies it has been recommended that authors publish a manual of reference that methodologically describes the intervention (Uebelacker et al., 2010). An example of this is the MBSR intervention and its derivatives (e.g., Mindfulness-based Relapse Prevention, MBRP (Bowen et al., 2009)) that have standardized programs and teacher trainings. The manual should describe the sequence of events in any given session of the intervention. It should include descriptions of physical movements, timing, detailed instruction on breathing exercises and focusing of the mind, the presence/absence of ethical/spiritual themes for the sessions, a description of the environment (lighting, music, temperature), details about the meditation (type, length, guided or not, seated or lying down, eyes opened or closed), and other aspects that are important when implementing the intervention such as group size, target population, instructor’s background and experience, and use of props. A manual allows for a uniform delivery of the intervention and is important for determining validity and reliability. Manuals can be used to compare different mind-body interventions and assist in identifying the physiological and psychological mechanisms underlying any treatment effects. For example, some yoga interventions might emphasize physical movement and breath over meditation, others might be of slower pace with increased focus on yoga philosophy, and others might prioritize meditation. Some meditation practices approach it as an open range state with general awareness, while other practices prioritize arriving to more concentrative states. An exploration of how these different practices might benefit different populations and diseases in different ways is interesting from a clinical point of view and from a mechanistic perspective.
The influence of the instructor is important. Instructors should be monitored to ensure maintenance of methodological rigor, consistency, and fidelity to the content of the intervention. Using instructional media specifically developed for the study (DVDs, audio CDs, and/or websites) can be an effective strategy to reduce the potential for instructor generated bias. However, using recorded practice sessions might not be ideal for monitoring adherence to protocol and ensuring participant safety. Ways of reducing bias and optimizing fidelity and consistency of mind-body interventions include: using more than one instructor, placing a person in the room to specifically evaluate the instructor and class content, questioning participants for their opinion on the quality of each session, or using a mixture of recorded instructions and personal presence.
4.3 Limitations
A significant issue for this review, as for all systematic reviews, comes from publication bias, that is, the tendency to report and publish results that show significant findings differently from results that are negative or inconclusive (Dickersin, 1997; Dwan et al., 2008). Therefore, due to the deficit in published articles reporting negative results, caution is warranted when affirming, based on the published literature, that a specific intervention is an effective treatment, as those results may have been generated in studies for which effects sizes were at the large tail of the distribution, potentially leading to an over-estimation of the true effect sizes. Our review has other limitations too. Our literature search was limited to English written peer-reviewed articles and excluded conference communications or doctoral theses. As mentioned previously, the small number of studies available, the variety in research design, and the differences in smoking primary outcomes significantly limits our ability to find a definite answer to our main research question. Despite these issues, our review provides evidence that encourages investigating further the potential of mind-body treatments to improve smoking cessation outcomes.
4.4 Future directions in mind-body research for smoking cessation
All fourteen studies eligible for this review suggest that mind-body interventions could aid smoking cessation. However, mind-body research for smoking cessation is still in its very early stages and further investigation on the topic is needed. Research areas that we consider in need of more immediate effort are: the development of objective measures of yoga and meditation practice (e.g. mindfulness, acceptance, resilience, reactivity, stress, breathing, awareness, meditative state) and their inclusion in intervention trials; the application of standard outcome measures of smoking cessation such as those proposed by Hughes (2003) and by West and collaborators (2005); the publication of interventions in manual form to allow reliable replication and future implementation; the study of the long term effects of these practices on nicotine addiction; and, the development of tools to monitor objectively self-practice, compliance, and adherence with the interventions. Once enough evidence supports the efficacy of mind-body strategies to improve smoking cessation, other questions to be pursued might be: Are specific practices more effective for smoking cessation than others? What are the individual predictors of success for each type of mind-body practice? Are mind-body interventions for smoking cessation adaptable and effective to treat other substance use disorders?
4.5 Conclusion
This review provides a description of mind-body therapies for smoking cessation. We have reviewed, evaluated, and summarized the existing literature applying mind-body treatments, examined some of the challenges of mind-body research, and explored future directions.
The impact of smoking, together with the increase in use and demand for alternative non-drug based treatments (Barnes et al., 2008), underscores the need for investigating new smoking cessation strategies. Mind-body practices are a good candidate. We identified fourteen studies that matched our eligibility criteria. All fourteen suggested that mind-body practices could be beneficial for improving smoking cessation. However, due to the scarcity and limitations of the studies available, more clinical trials with larger sample sizes, adequate control conditions, measures of adherence and compliance, and objective standardized outcomes, are needed to establish if mind-body practices are efficacious as smoking cessation treatments.
Acknowledgments
AUTHOR DISCLOSURES
Role of Funding Source
This research has been supported by NIH grants T32AT002688 and K24AT002656. NIH had no further role in study design, collection, analysis and interpretation of data, manuscript writing, or in the decision to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
LC-T performed the literature search, applied selection criteria and wrote the first draft of the manuscript. SHM and BSO read and edited the manuscript, and assessed the quality of the articles. All authors have contributed to and approved the final manuscript.
Conflict of Interest
The authors have no conflicts of interest.
REFERENCES
- Alberg AJ, Patnaik JL, May JW, Hoffman SC, Gitchelle J, Comstock GW, Helzlsouer KJ. Nicotine replacement therapy use among a cohort of smokers. J Addict. Dis. 2005;24:101–113. doi: 10.1300/J069v24n01_09. [DOI] [PubMed] [Google Scholar]
- Allen M, Dietz M, Blair KS, van Beek M, Rees G, Vestergaard-Poulsen P, Lutz A, Roepstorff A. Cognitive-affective neural plasticity following active-controlled mindfulness intervention. J. Neurosci. 2012;32:15601–15610. doi: 10.1523/JNEUROSCI.2957-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade C. Yoga: some unanswered questions. Indian J. Psychiatry. 1995;37:189. [PMC free article] [PubMed] [Google Scholar]
- Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, Conway WA, Jr, Enright PL, Kanner RE, O'Hara P, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994;272:1497–1505. [PubMed] [Google Scholar]
- Arya SN. The problems of hypertension in the elderly. J. Indian Med. Assoc. 2000;98:176–179. [PubMed] [Google Scholar]
- Astin JA, Shapiro SL, Eisenberg DM, Forys KL. Mind-body medicine: state of the science, implications for practice. J. Am. Board Fam. Pract. 2003;16:131–147. doi: 10.3122/jabfm.16.2.131. [DOI] [PubMed] [Google Scholar]
- Balasubramaniam M, Telles S, Doraiswamy PM. Yoga on our minds: a systematic review of yoga for neuropsychiatric disorders. Front. Psychiatry. 2012;31:17. doi: 10.3389/fpsyt.2012.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl. Health Stat. Rep. 2008;12:1–23. [PubMed] [Google Scholar]
- Beddoe AE, Lee KA. Mind-body interventions during pregnancy. J. Obstet. Gynecol. Neonatal Nurs. 2008;37:165–175. doi: 10.1111/j.1552-6909.2008.00218.x. [DOI] [PubMed] [Google Scholar]
- Bernardi L, Wdowczyk-Szulc J, Valenti C, Castoldi S, Passino C, Spadacini G, Sleight P. Effects of controlled breathing, mental activity and mental stress with or without verbalization on heart rate variability. J. Am. Coll. Cardiol. 2000;35:1462–1469. doi: 10.1016/s0735-1097(00)00595-7. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Segal ZV, Abbey S, Speca M, Velting D, Devins G. Mindfulness: a proposed operational definition. Clin. Psychol. (New York) 2004;11:230–241. [Google Scholar]
- Bock BC, Fava JL, Gaskins R, Morrow KM, Williams DM, Jennings E, Becker BM, Tremont G, Marcus BH. Yoga as a complementary treatment for smoking cessation in women. J. Womens Health (Larchmt) 2012;21:240–248. doi: 10.1089/jwh.2011.2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bock BC, Marcus BH, King TK, Borrelli B, Roberts MR. Exercise effects on withdrawal and mood among women attempting smoking cessation. Addict. Behav. 1999;24:399–410. doi: 10.1016/s0306-4603(98)00088-4. [DOI] [PubMed] [Google Scholar]
- Borland R, Partos TR, Yong HH, Cummings KM, Hyland A. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control Four Country cohort survey. Addiction. 2012;107:673–682. doi: 10.1111/j.1360-0443.2011.03685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Clifasefi S, Garner M, Douglass A, Larimer ME, Marlatt A. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Subst. Abuse. 2009;30:295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Marlatt A. Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychol. Addict. Behav. 2009;23:666–671. doi: 10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Bradley BP, Field M, Healy H, Mogg K. Do the affective properties of smoking-related cues influence attentional and approach biases in cigarette smokers? J. Psychopharmacol. 2008;22:737–745. doi: 10.1177/0269881107083844. [DOI] [PubMed] [Google Scholar]
- Brand S, Holsboer-Trachsler E, Naranjo JR, Schmidt S. Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology. 2012;65:109–118. doi: 10.1159/000330362. [DOI] [PubMed] [Google Scholar]
- Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, Minnix-Cotton CA, Byrne SA, Kober H, Weinstein AJ, Carroll KM, Rounsaville BJ. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend. 2011;119:72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: part I-neurophysiologic model. J. Altern. Complement. Med. 2005;11:189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- Brown RP, Gerbarg PL. Yoga breathing, meditation, and longevity. Ann. N. Y. Acad. Sci. 2009;1172:54–62. doi: 10.1111/j.1749-6632.2009.04394.x. [DOI] [PubMed] [Google Scholar]
- Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst. Rev. 2012;4 doi: 10.1002/14651858.CD006103.pub2. CD006103. [DOI] [PubMed] [Google Scholar]
- Cahn BR, Polich J. Meditation states and traits: EEG, ERP, and neuroimaging studies. Psychol. Bull. 2006;132:180–211. doi: 10.1037/0033-2909.132.2.180. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Annual smoking-attributable mortality, years of potential life lost, and productivity losses--United States, 2000–2004. MMWR. 2008;57:1226–1228. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Quitting Smoking Among Adults— United States, 2001–2010. MMWR. 2011;60:1513–1519. [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness-based interventions for chronic pain: a systematic review of the evidence. J. Altern. Complement. Med. 2011;17:83–93. doi: 10.1089/acm.2009.0546. [DOI] [PubMed] [Google Scholar]
- Conrad A, Muller A, Doberenz S, Kim S, Meuret AE, Wollburg E, Roth WT. Psychophysiological effects of breathing instructions for stress management. Appl. Psychophysiol. Biofeedback. 2007;32:89–98. doi: 10.1007/s10484-007-9034-x. [DOI] [PubMed] [Google Scholar]
- Cropley M, Ussher M, Charitou E. Acute effects of a guided relaxation routine (body scan) on tobacco withdrawal symptoms and cravings in abstinent smokers. Addiction. 2007;102:989–993. doi: 10.1111/j.1360-0443.2007.01832.x. [DOI] [PubMed] [Google Scholar]
- D'Silva S, Poscablo C, Habousha R, Kogan M, Kligler B. Mind-body medicine therapies for a range of depression severity: a systematic review. Psychosomatics. 2012;53:407–423. doi: 10.1016/j.psym.2012.04.006. [DOI] [PubMed] [Google Scholar]
- Davis JM, Fleming MF, Bonus KA, Baker TB. A pilot study on mindfulness based stress reduction for smokers. BMC Complement. Altern. Med. 2007;7:2. doi: 10.1186/1472-6882-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Godoy DV, Bringhenti RL, Severa A, de Gasperi R, Poli LV. Yoga versus aerobic activity: effects on spirometry results and maximal inspiratory pressure. J. Bras. Pneumol. 2006;32:130–135. doi: 10.1590/s1806-37132006000200008. [DOI] [PubMed] [Google Scholar]
- Desikachar TKV. The Heart of Yoga: Developing a Personal Practice. Rochester, VT: Inner Traditions International; 1999. [Google Scholar]
- Dickersin K. How important is publication bias? A synthesis of available data. AIDS Educ. Prev. 1997;9(1 Suppl):15–21. [PubMed] [Google Scholar]
- Dwan K, Altman DG, Arnaiz JA, Bloom J, Chan AW, Cronin E, Decullier E, Easterbrook PJ, Von Elm E, Gamble C, Ghersi D, Ioannidis JP, Simes J, Williamson PR. Systematic review of the empirical evidence of study publication bias and outcome reporting bias. PLoS One. 2008;3:e3081. doi: 10.1371/journal.pone.0003081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg MJ, Filion KB, Yavin D, Belisle P, Mottillo S, Joseph L, Gervais A, O'Loughlin J, Paradis G, Rinfret S, Pilote L. Pharmacotherapies for smoking cessation: a meta-analysis of randomized controlled trials. CMAJ. 2008;179:135–144. doi: 10.1503/cmaj.070256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elibero A, Janse Van Rensburg K, Drobes DJ. Acute effects of aerobic exercise and Hatha yoga on craving to smoke. Nicotine Tob. Res. 2011;13:1140–1148. doi: 10.1093/ntr/ntr163. [DOI] [PubMed] [Google Scholar]
- Elkins G, Fisher W, Johnson A. Mind-body therapies in integrative oncology. Curr. Treat. Options Oncol. 2010;11:128–140. doi: 10.1007/s11864-010-0129-x. [DOI] [PubMed] [Google Scholar]
- Farb NAS, Segal ZV, Mayberg H, Bean J, McKeon D, Fatima Z, Anderson AK. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc. Cogn. Affect. Neurosci. 2007;2:313–322. doi: 10.1093/scan/nsm030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T. Yoga clinical research review. Complement. Ther. Clin. Pract. 2011;17:1–8. doi: 10.1016/j.ctcp.2010.09.007. [DOI] [PubMed] [Google Scholar]
- Fiore M, Jaén C, Baker T, Bailey W, Benowitz N, Curry S, Dorfman S, Froelicher E, Goldstein M, Froelicher E, Healton C, et al. A clinical practice guideline for treating tobacco use and dependence: 2008 Update. A U.S. Public Health Service report. Am. J. Prev. Med. 2008;35:158–176. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KE, Kishiyama S, Zajdel D, Haas M, Oken BS. Adherence to yoga and exercise interventions in a 6-month clinical. trial BMC Complement. Altern. Med. 2007;7:37. doi: 10.1186/1472-6882-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Van Tulder M, Santaguida L, Gagnier J, Ammendolia C, Dryden T, Doucette S, Skidmore B, Daniel R, Ostermann T, Tsouros S. A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain. Evid. Based Complement. Alternat. Med. 2012 doi: 10.1155/2012/953139. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: results of a randomized controlled pilot trial. J. Psychoactive Drugs. 2010;42:177–192. doi: 10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JA, Duerden EG, Courtemanche J, Cherkasova M, Duncan GH, Rainville P. Cortical thickness, mental absorption and meditative practice: possible implications for disorders of attention. Biol. Psychol. 2013;92:275–281. doi: 10.1016/j.biopsycho.2012.09.007. [DOI] [PubMed] [Google Scholar]
- Haaga DA, Grosswald S, Gaylord-King C, Rainforth M, Tanner M, Travis F, Nidich S, Schneider RH. Effects of the transcendental meditation program on substance use among university students. Cardiol. Res. Pract. 2011 doi: 10.4061/2011/537101. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PE, Cooper KL, Relton C, Thomas KJ. Prevalence of complementary and alternative medicine (CAM) use by the general population: a systematic review and update. Int. J. Clin. Pract. 2012;66:924–939. doi: 10.1111/j.1742-1241.2012.02945.x. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J. Consult. Clin. Psychol. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollinghurst S, Shaw A, Thompson EA. Capturing the value of complementary and alternative medicine: including patient preferences in economic evaluation. Complement. Ther. Med. 2008;16:47–51. doi: 10.1016/j.ctim.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Hughes JR. Ethical concerns about non-active conditions in smoking cessation trials and methods to decrease such concerns. Drug Alcohol Depend. 2009;100:187–193. doi: 10.1016/j.drugalcdep.2008.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine Tob. Res. 2003;5:13–25. [PubMed] [Google Scholar]
- Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst. Rev. 2007;1 doi: 10.1002/14651858.CD000031.pub3. CD000031. [DOI] [PubMed] [Google Scholar]
- Iyengar BKS. Light on Yoga: Yoga Dipika. New York, USA: Schocken Books; 1995. [Google Scholar]
- Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of qigong and tai chi. Am. J. Health Promot. 2010;24:e1–e25. doi: 10.4278/ajhp.081013-LIT-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain S, Shapiro SL, Swanick S, Roesch SC, Mills PJ, Bell I, Schwartz GE. A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Ann. Behav. Med. 2007;33:11–21. doi: 10.1207/s15324796abm3301_2. [DOI] [PubMed] [Google Scholar]
- Jatuporn S, Sangwatanaroj S, Saengsiri AO, Rattanapruks S, Srimahachota S, Uthayachalerm W, Kuanoon W, Panpakdee O, Tangkijvanich P, Tosukhowong P. Short-term effects of an intensive lifestyle modification program on lipid peroxidation and antioxidant systems in patients with coronary artery disease. Clin. Hemorheol. Microcirc. 2003;29:429–436. [PubMed] [Google Scholar]
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen. Hosp. Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of your Body and Mind to Face Stress, Pain, and illness. New York, USA: Delta Trade Paperbacks; 2005. [Google Scholar]
- Kaley-Isley LC, Peterson J, Fischer C, Peterson E. Yoga as a complementary therapy for children and adolescents: a guide for clinicians. Psychiatry (Edgmont) 2010;7:20–32. [PMC free article] [PubMed] [Google Scholar]
- Khalsa SB. Treatment of chronic insomnia with yoga: a preliminary study with sleep-wake diaries. Appl. Psychophysiol. Biofeedback. 2004;29:269–278. doi: 10.1007/s10484-004-0387-0. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Christian L, Preston H, Houts CR, Malarkey WB, Emery CF, Glaser R. Stress, inflammation, and yoga practice. Psychosom. Med. 2010;72:113–121. doi: 10.1097/PSY.0b013e3181cb9377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochupillai V, Kumar P, Singh D, Aggarwal D, Bhardwaj N, Bhutani M, Das SN. Effect of rhythmic breathing (Sudarshan Kriya and Pranayam) on immune functions and tobacco addiction. Ann. N. Y. Acad. Sci. 2005;1056:242–252. doi: 10.1196/annals.1352.039. [DOI] [PubMed] [Google Scholar]
- Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–238. doi: 10.1038/npp.2009.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kooreman P, Baars EW. Patients whose GP knows complementary medicine tend to have lower costs and live longer. Eur. J. Health Econ. 2012;13:769–776. doi: 10.1007/s10198-011-0330-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozasa EH, Hachul H, Monson C, Pinto L, Jr, Garcia MC, Mello LE, Tufik S. Mind-body interventions for the treatment of insomnia: a review. Rev. Bras. Psiquiatr. 2010;32:437–443. doi: 10.1590/s1516-44462010000400018. [DOI] [PubMed] [Google Scholar]
- Krisanaprakornkit T, Ngamjarus C, Witoonchart C, Piyavhatkul N. Meditation therapies for attention-deficit/hyperactivity disorder (ADHD) Cochrane Database Syst. Rev. 2010;6 doi: 10.1002/14651858.CD006507.pub2. CD006507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazar SW, Kerr CE, Wasserman RH, Gray JR, Greve DN, Treadway MT, McGarvey M, Quinn BT, Dusek JA, Benson H, Rauch SL, Moore CI, Fischl B. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005;16:1893–1897. doi: 10.1097/01.wnr.0000186598.66243.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, Bonus KA, Stoney CM, Salomons TV, Davidson RJ, Lutz A. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behav. Res. Ther. 2012;50:3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maclennan AH. Evidence-based review of therapies at the menopause. Int. J. Evid. Based Healthc. 2009;7:112–123. doi: 10.1111/j.1744-1609.2009.00133.x. [DOI] [PubMed] [Google Scholar]
- Mason S, Tovey P, Long AF. Evaluating complementary medicine: methodological challenges of randomised controlled trials. BMJ. 2002;325:832–834. doi: 10.1136/bmj.325.7368.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall T. Yoga as Medicine: The Yogic Prescription for Health and Healing. New York, USA: Bantam; 2007. [Google Scholar]
- McClernon FJ, Westman EC, Rose JE. The effects of controlled deep breathing on smoking withdrawal symptoms in dependent smokers. Addict. Behav. 2004;29:765–772. doi: 10.1016/j.addbeh.2004.02.005. [DOI] [PubMed] [Google Scholar]
- McIver S, O'Halloran P, McGartland M. The impact of Hatha yoga on smoking behavior. Altern. Ther. Health Med. 2004;10:22–23. [PubMed] [Google Scholar]
- Meeks TW, Wetherell JL, Irwin MR, Redwine LS, Jeste DV. Complementary and alternative treatments for late-life depression, anxiety, and sleep disturbance: a review of randomized controlled trials. J. Clin. Psychiatry. 2007;68:1461–1471. doi: 10.4088/jcp.v68n1001. [DOI] [PubMed] [Google Scholar]
- Mendez D, Alshanqeety O, Warner KE. The potential impact of smoking control policies on future global smoking trends. Tob. Control. 2013;22:46–51. doi: 10.1136/tobaccocontrol-2011-050147. [DOI] [PubMed] [Google Scholar]
- Mitchell SH. Measures of impulsivity in cigarette smokers and non-smokers. Psychopharmacology (Berl.) 1999;146:455–464. doi: 10.1007/pl00005491. [DOI] [PubMed] [Google Scholar]
- Moore TJ, Furberg CD, Glenmullen J, Maltsberger JT, Singh S. Suicidal behavior and depression in smoking cessation treatments. PLoS One. 2011;6 doi: 10.1371/journal.pone.0027016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahin RL, Barnes PM, Stussman BJ, Bloom B. Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. Natl. Health Stat. Rep. 2009;18:1–14. [PubMed] [Google Scholar]
- National Center for Complementary and Alternative Medicine. [accessed on February 27th 2013];Meditation: an introduction. 2006 http://nccam.nih.gov/health/meditation/overview.htm#sideeffects.
- National Center for Complementary and Alternative Medicine. [accessed on March 6th 2013];What Is Complementary and Alternative Medicine? 2008a http://nccam.nih.gov/health/whatiscam.
- National Center for Complementary and Alternative Medicine. [accessed on February 27th 2013];Yoga for Health. 2008b http://nccam.nih.gov/health/yoga/introduction.htm?nav=gsa#hed1.
- Nestor L, McCabe E, Jones J, Clancy L, Garavan H. Differences in “bottom-up” and “top-down” neural activity in current and former cigarette smokers: Evidence for neural substrates which may promote nicotine abstinence through increased cognitive control. Neuroimage. 2011;56:2258–2275. doi: 10.1016/j.neuroimage.2011.03.054. [DOI] [PubMed] [Google Scholar]
- Niaura R. Nonpharmacologic therapy for smoking cessation: characteristics and efficacy of current approaches. Am. J. Med. 2008;121(Suppl. 1):S11–S19. doi: 10.1016/j.amjmed.2008.01.021. [DOI] [PubMed] [Google Scholar]
- O'Connell KA, Gerkovich MM, Cook MR, Shiffman S, Hickcox M, Kakolewski KE. Coping in real time: using Ecological Momentary Assessment techniques to assess coping with the urge to smoke. Res. Nurs. Health. 1998;21:487–497. doi: 10.1002/(sici)1098-240x(199812)21:6<487::aid-nur3>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Oken BS, Kishiyama S, Zajdel D, Bourdette D, Carlsen J, Haas M, Hugos C, Kraemer DF, Lawrence J, Mass M. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004;62:2058–2064. doi: 10.1212/01.wnl.0000129534.88602.5c. [DOI] [PubMed] [Google Scholar]
- Oken BS, Zajdel D, Kishiyama S, Flegal K, Dehen C, Haas M, Kraemer DF, Lawrence J, Leyva J. Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern. Ther. Health Med. 2006;12:40–47. [PMC free article] [PubMed] [Google Scholar]
- Ospina MB, Bond K, Karkhaneh M, Buscemi N, Dryden DM, Barnes V, Carlson LE, Dusek JA, Shannahoff-Khalsa D. Clinical trials of meditation practices in health care: characteristics and quality. J. Altern. Complement. Med. 2008;14:1199–1213. doi: 10.1089/acm.2008.0307. [DOI] [PubMed] [Google Scholar]
- Pierce JP, Gilpin EA. Impact of over-the-counter sales on effectiveness of pharmaceutical aids for smoking cessation. JAMA. 2002;288:1260–1264. doi: 10.1001/jama.288.10.1260. [DOI] [PubMed] [Google Scholar]
- Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin. Psychol. Rev. 2011;31:1032–1040. doi: 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am. Psychol. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Pullen PR, Nagamia SH, Mehta PK, Thompson WR, Benardot D, Hammoud R, Parrott JM, Sola S, Khan BV. Effects of yoga on inflammation and exercise capacity in patients with chronic heart failure. J. Card. Fail. 2008;14:407–413. doi: 10.1016/j.cardfail.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Purohit MP, Wells RE, Zafonte RD, Davis RB, Phillips RS. Neuropsychiatric symptoms and the use of complementary and alternative medicine. PM R. 2013;5:24–31. doi: 10.1016/j.pmrj.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raub JA. Psychophysiologic effects of Hatha Yoga on musculoskeletal and cardiopulmonary function: a literature review. J. Altern. Complement. Med. 2002;8:797–812. doi: 10.1089/10755530260511810. [DOI] [PubMed] [Google Scholar]
- Riley D. Hatha yoga and the treatment of illness. Altern. Ther. Health Med. 2004;10:20–21. [PubMed] [Google Scholar]
- Roberts-Wolfe D, Sacchet M, Hastings E, Roth H, Britton W. Mindfulness training alters emotional memory recall compared to active controls: support for an emotional information processing model of mindfulness. Front. Hum. Neurosci. 2012;6:15. doi: 10.3389/fnhum.2012.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogojanski J, Vettese L, Antony M. Coping with cigarette cravings: comparison of suppression versus mindfulness-based strategies. Mindfulness. 2011a;2:14–26. doi: 10.1002/jclp.20774. [DOI] [PubMed] [Google Scholar]
- Rogojanski J, Vettese LC, Antony MM. Role of sensitivity to anxiety symptoms in responsiveness to mindfulness versus suppression strategies for coping with smoking cravings. J. Clin. Psychol. 2011b;67:439–445. doi: 10.1002/jclp.20774. [DOI] [PubMed] [Google Scholar]
- Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J. Altern. Complement. Med. 2010;16:3–12. doi: 10.1089/acm.2009.0044. [DOI] [PubMed] [Google Scholar]
- Royer A. The role of the transcendental meditation technique in promoting smoking cessation. Alcohol. Treat. Q. 1994;11:221–238. [Google Scholar]
- Sahay BK, Sahay RK. Lifestyle modification in management of diabetes mellitus. J. Indian Med. Assoc. 2002;100:178–180. [PubMed] [Google Scholar]
- Schlam TR, Baker TB. Interventions for tobacco smoking. Annu. Rev. Clin. Psychol. 2013;9:675–702. doi: 10.1146/annurev-clinpsy-050212-185602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scully D, Kremer J, Meade MM, Graham R, Dudgeon K. Physical exercise and psychological well being: a critical review. Br. J. Sports Med. 1998;32:111–120. doi: 10.1136/bjsm.32.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senders A, Wahbeh H, Spain R, Shinto L. Mind-body medicine for multiple sclerosis: a systematic review. Autoimmune Dis. 2012;2012:567324. doi: 10.1155/2012/567324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahab L, Sarkar BK, West R. The acute effects of yogic breathing exercises on craving and withdrawal symptoms in abstaining smokers. Psychopharmacology (Berl.) 2013;225:875–882. doi: 10.1007/s00213-012-2876-9. [DOI] [PubMed] [Google Scholar]
- Sherman KJ, Cherkin DC, Wellman RD, Cook AJ, Hawkes RJ, Delaney K, Deyo RA. A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Arch. Int. Med. 2011;171:2019–2026. doi: 10.1001/archinternmed.2011.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverberg DS. Non-pharmacological treatment of hypertension. J. Hypertens. 1990;(Suppl. 8):S21–S26. [PubMed] [Google Scholar]
- Singh S, Loke YK, Spangler JG, Furberg CD. Risk of serious adverse cardiovascular events associated with varenicline: a systematic review and meta-analysis. CMAJ. 2011;183:1359–1366. doi: 10.1503/cmaj.110218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha S, Singh SN, Monga YP, Ray US. Improvement of glutathione and total antioxidant status with yoga. J. Altern. Complement. Med. 2007;13:1085–1090. doi: 10.1089/acm.2007.0567. [DOI] [PubMed] [Google Scholar]
- Smith JA, Greer T, Sheets T, Watson S. Is there more to yoga than exercise? Altern. Ther. Health Med. 2011;17:22–29. [PubMed] [Google Scholar]
- Sobel DS. The cost-effectiveness of mind-body medicine interventions. Prog. Brain Res. 1999;122:393–412. [PubMed] [Google Scholar]
- Sood A, Ebbert JO, Sood R, Stevens SR. Complementary treatments for tobacco cessation: a survey. Nicotine Tob. Res. 2006;8:767–771. doi: 10.1080/14622200601004109. [DOI] [PubMed] [Google Scholar]
- Stead LF, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst. Rev. 2012;10 doi: 10.1002/14651858.CD008286.pub2. CD008286. [DOI] [PubMed] [Google Scholar]
- Stead LF, Perera R, Bullen C, Mant D, Hartmann-Boyce J, Cahill K, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 2012;11 doi: 10.1002/14651858.CD000146.pub4. CD000146. [DOI] [PubMed] [Google Scholar]
- Streeter CC, Whitfield TH, Owen L, Rein T, Karri SK, Yakhkind A, Perlmutter R, Prescot A, Renshaw PF, Ciraulo DA, Jensen JE. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: a randomized controlled MRS study. J. Altern. Complement. Med. 2010;16:1145–1152. doi: 10.1089/acm.2010.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, McCuller WJ, Zheng H, Pfingston YM, Miyano J, Dent CW. Project EX: a program of empirical research on adolescent tobacco use cessation. Tob. Induc. Dis. 2004;2:119–132. doi: 10.1186/1617-9625-2-3-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonnesen P, Tonstad S, Hjalmarson A, Lebargy F, Van Spiegel PI, Hider A, Sweet R, Townsend J. A multicentre, randomized, double-blind, placebo-controlled, 1-year study of bupropion SR for smoking cessation. J. Intern. Med. 2003;254:184–192. doi: 10.1046/j.1365-2796.2003.01185.x. [DOI] [PubMed] [Google Scholar]
- Tran MD, Holly RG, Lashbrook J, Amsterdam EA. Effects of hatha yoga practice on the health-related aspects of physical fitness. Prev. Cardiol. 2001;4:165–170. doi: 10.1111/j.1520-037x.2001.00542.x. [DOI] [PubMed] [Google Scholar]
- Uebelacker LA, Epstein-Lubow G, Gaudiano BA, Tremont G, Battle CL, Miller IW. Hatha yoga for depression: critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. J. Psychiatr. Pract. 2010;16:22–33. doi: 10.1097/01.pra.0000367775.88388.96. [DOI] [PubMed] [Google Scholar]
- Ussher M, Cropley M, Playle S, Mohidin R, West R. Effect of isometric exercise and body scanning on cigarette cravings and withdrawal symptoms. Addiction. 2009;104:1251–1257. doi: 10.1111/j.1360-0443.2009.02605.x. [DOI] [PubMed] [Google Scholar]
- Ussher MH, Taylor AH, West R, McEwen A. Does exercise aid smoking cessation? A systematic review. Addiction. 2000;95:199–208. doi: 10.1046/j.1360-0443.2000.9521996.x. [DOI] [PubMed] [Google Scholar]
- Vadiraja HS, Raghavendra RM, Nagarathna R, Nagendra HR, Rekha M, Vanitha N, Gopinath KS, Srinath BS, Vishweshwara MS, Madhavi YS, Ajaikumar BS, Ramesh BS, Nalini R, Kumar V. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Integr. Cancer Ther. 2009;8:37–46. doi: 10.1177/1534735409331456. [DOI] [PubMed] [Google Scholar]
- Vedamurthachar A, Janakiramaiah N, Hegde JM, Shetty TK, Subbakrishna DK, Sureshbabu SV, Gangadhar BN. Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. J. Affect. Disord. 2006;94:249–253. doi: 10.1016/j.jad.2006.04.025. [DOI] [PubMed] [Google Scholar]
- Ventegodt S, Merrick J. Meta-analysis of positive effects, side effects and adverse events of holistic mind-body medicine (clinical holistic medicine): experience from Denmark, Sweden, United Kingdom and Germany. Int. J. Adolesc. Med. Health. 2009;21:441–456. doi: 10.1515/ijamh.2009.21.4.441. [DOI] [PubMed] [Google Scholar]
- Vidrine JI, Businelle MS, Cinciripini P, Li Y, Marcus MT, Waters AJ, Reitzel LR, Wetter DW. Associations of mindfulness with nicotine dependence, withdrawal, and agency. Subst. Abuse. 2009;30:318–327. doi: 10.1080/08897070903252973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahbeh H, Elsas SM, Oken BS. Mind-body interventions: applications in neurology. Neurology. 2008;70:2321–2328. doi: 10.1212/01.wnl.0000314667.16386.5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters AJ, Shiffman S, Bradley BP, Mogg K. Attentional shifts to smoking cues in smokers. Addiction. 2003;98:1409–1417. doi: 10.1046/j.1360-0443.2003.00465.x. [DOI] [PubMed] [Google Scholar]
- West J, Otte C, Geher K, Johnson J, Mohr DC. Effects of hatha yoga and African dance on perceived stress, affect, and salivary cortisol. Ann. Behav. Med. 2004;28:114–118. doi: 10.1207/s15324796abm2802_6. [DOI] [PubMed] [Google Scholar]
- West R, Hajek P, Stead L, Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction. 2005;100:299–303. doi: 10.1111/j.1360-0443.2004.00995.x. [DOI] [PubMed] [Google Scholar]
- Westbrook C, Creswell JD, Tabibnia G, Julson E, Kober H, Tindle HA. Mindful attention reduces neural and self-reported cue-induced craving in smokers. Soc. Cogn. Affect. Neurosci. 2013;8:73–84. doi: 10.1093/scan/nsr076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolever RQ, Bobinet KJ, McCabe K, Mackenzie ER, Fekete E, Kusnick CA, Baime M. Effective and viable mind-body stress reduction in the workplace: a randomized controlled trial. J. Occup. Health Psychol. 2012;17:246–258. doi: 10.1037/a0027278. [DOI] [PubMed] [Google Scholar]
- World Health Organization. [accessed on March 6th 2013];General Guidelines for Methodologies on Research and Evaluation of Traditional Medicine. 2000 http://www.who.int/medicines/areas/traditional/definitions/en/index.html.
- World Health Organization. [accessed on March 6th 2013];Report on the Global Tobacco Epidemic, 2008: The MPOWER package. 2008a http://www.who.int/tobacco/mpower/2008/en/index.html.
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems. New York, NY: WHO; 2008b. (10th Rev. ed.) [Google Scholar]
- Wragg JA, Robinson EJ, Lilford RJ. Information presentation and decisions to enter clinical trials: a hypothetical trial of hormone replacement therapy. Soc. Sci. Med. 2000;51:453–462. doi: 10.1016/s0277-9536(99)00477-3. [DOI] [PubMed] [Google Scholar]
- Wren AA, Wright MA, Carson JW, Keefe FJ. Yoga for persistent pain: new findings and directions for an ancient practice. Pain. 2011;152:477–480. doi: 10.1016/j.pain.2010.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan F, Grant JA, Brown CA, McHaffie JG, Coghill RC. Mindfulness meditation-related pain relief: evidence for unique brain mechanisms in the regulation of pain. Neurosci. Lett. 2012;520:165–173. doi: 10.1016/j.neulet.2012.03.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H, Sussman S, Chen X, Wang Y, Xia J, Gong J, Liu C, Shan J, Unger J, Johnson CA. Project EX--a teen smoking cessation initial study in Wuhan, China. Addict. Behav. 2004;29:1725–1733. doi: 10.1016/j.addbeh.2004.03.035. [DOI] [PubMed] [Google Scholar]