Abstract
Study Objectives:
Examine the association between sleep duration and suicidal ideation in Korean adults.
Design:
Cross-sectional survey.
Setting:
Data obtained by the Korea National Health and Nutrition Examination Survey IV (2007-2009) using a rolling sampling design involving a complex, stratified, multistage, and probability-cluster survey of civilian non-institutionalized Korean residents.
Participants:
A total of 15,236 subjects (6,638 males and 8,598 females) ≥ 19 years old.
Measurements and Results:
The weighted prevalence of self-reported short sleep duration (≤ 5 h/day) was 11.7% in males and 15% in females, and of long sleep duration (≥ 9 h/day) was 6.7% in males and 8.9% in females. A U-shaped relationship existed, with both short and long sleep durations associated with a higher suicidal ideation risk. Multiple logistic regression analysis was used to analyze the relationship between sleep duration and suicidal ideation, adjusting for sociodemographic factors, health behavior, and health status. After controlling for covariates, people with short sleep were 38.1% more likely to have suicidal ideation (OR = 1.381, 95% CI 1.156-1.650) than people with sleep duration of 7 h/day. Suicidal ideation was 1.196 times higher (95% CI: 0.950-1.507) in long-sleeping people than people sleeping 7 h/day, although statistically not significant. Inclusion of depressive mood (a potential confounder) in multiple logistic regression models attenuated but did not eliminate the sleep duration/suicidal ideation association.
Limitations:
Sleep duration and suicidal ideation were assessed only by self-report.
Conclusions:
The sleep duration/suicidal ideation relationship is U-shaped in the Korean adult population. Self-reported habitual sleep duration may be a useful behavioral indicator for both individual and societal suicidal ideation risk.
Citation:
Kim JH; Park EC; Cho WH; Park JY; Choi WJ; Chang HS. Association between total sleep duration and suicidal ideation among the Korean general adult population. SLEEP 2013;36(10):1563-1572.
Keywords: Suicidal ideation, sleep, depressive symptom, gender
INTRODUCTION
The World Health Organization cites suicide as a major health issue in all countries.1 Many suicides are related to a combination of different factors: sociocultural, environmental, psychological, and biological elements.2–4 Sleep disturbances such as insomnia, hypersomnia, and nightmares are risk factors for suicidal ideation and behavior.5–7 Insomnia is one of the strongest predictors of completed suicide and can also be an indicator of suicide risk.8–10
In research examining the association between sleep duration and suicide, findings suggest a particular association between short sleep duration and suicide among teenagers.7,11 Research also suggests an association between the starting sleep time of teenagers and suicidal ideation.12 There is also research reporting a higher prevalence of suicidal ideation in Korean temporary workers with sleep duration ≤ 6 hours than those with 6 hours or more.13 Studies carried out in the West have sub-categorized insomnia into difficulty initiating sleep, difficulty maintaining sleep, and early morning awakenings to report their associations with suicidal ideation or suicide attempt.6 It is important to understand the associations between total sleep time and suicide against the backdrop of various sleep disorders. To date, most of the existing research on sleep and suicidality in adults has been described in clinical samples.9,14,15
Korea has the highest average suicide rate among the OECD (Organization for Economic Cooperation and Development) countries.16 The age-standardized suicide rate of South Korea increased from 10.2 (per 100,000) in 1985 to 21.5 in 2006 and more recently to 31.2/100,000 people in 2010.17,18 According to the Korean National Health and Nutrition Examination Survey data, the mean daily sleep duration (± SD) of Korean adults aged 19 years old and older in 1998 was 7.00 ± 1.37 h in 1998; the fraction of short sleepers was 11.44%, and the fraction of long sleepers was 7.96% of the general adult population. The mean daily sleep duration for 2001 was 6.89 ± 1.36 h, with the short sleep fraction analyzed as 12.48% and the long sleep fraction as 7.55%. In 2008, the mean daily sleep duration was 6.857 ± 1.49 h, with the short sleeper fraction as 13.79% and the long sleeper fraction as 9.6%. Recently, the mean sleep duration for Korean adults has decreased, showing an increase in the fraction of people with extreme sleep duration and paralleling the trend of increased suicide incidence. However, a definitive causal relationship between sleep duration and suicide risk remains to be established.
Too little or too much sleep is associated with increased risk of total mortality,19 coronary heart disease,20,21 stroke,20 type 2 diabetes mellitus,21,22 respiratory disorders,23 and the health-related quality of life.24 A recent study conducted on American adolescents reported that extremes in total sleep time were related to suicide risk.11 These findings have often shown a U-shaped association between sleep duration and suicidal ideation. A potential mechanism for this association suggested by Kohyama is that when mean sleep duration is longer, there is more serotonin secretion, which lowers the likelihood of suicide.25 Another study explained the relationship between attenuated sleep patterns and increased suicidal behavior by the negative impact that lack of sleep can have on judgment, concentration, impulse control, and mental illness.26 Suicide is associated with various mental disorders such as major depression, anxiety, and alcoholism.27 Sleep is very closely related to mental disorders, and sleep disturbances are included in the diagnostic criteria of disorders such as major depression, bipolar disorder, and generalized anxiety disorder.27 Existing studies are relatively consistent in reporting a relationship between short sleep duration and high suicide risk. However, it remains unclear whether the association between sleep duration and suicidal ideation exists independently of extant mental disorders. Indeed, the order of incidence between sleep duration and suicidal ideation, and the underlying mechanism(s), are not yet clarified.28 Socioeconomic environment, health risk behaviors (e.g., drinking and physical inactivity), and mental health problems (e.g., depression)5,29,30 affect suicide risk.31–33 It is possible that sociodemographic variables, lifestyle behaviors, and psychological and health conditions may confound or mediate the associations between short and long sleep duration and adverse health outcomes.29,34 However, very few studies have researched the general adult population in Asia in regard to the associations between sleep duration and suicidal ideation after adjusting for depression, health conditions, and sociodemographic factors.35,36
Previous research has demonstrated that suicide rates are higher in males in most countries, and many of the male attempters had alcohol drinking problems along with substance dependence. However, the rates of suicide attempts are also elevated in females with depression and eating disorders.37,38 A Spanish study investigated the relationship between sleep duration and suicidal ideation in adults; when a healthy group and attempted suicide group were compared, the rate of short sleep was significantly higher in the attempted suicide group versus the healthy group, for both males and females.39 However, few studies have evaluated the associations between sleep duration and suicide in the general population after sex stratification.
We examined the association between self-reported sleep duration and suicidality in a nationally representative sample of Korean adults. We hypothesized that suicidal ideation would be higher in respondents who slept ≤ 5 hours (short sleep) or ≥ 9 hours (long sleep) daily versus those who slept for 7 hours, thereby demonstrating a U-shaped association after adjustment for depressive mood and other potential confounders.
METHODS
Study Sample
The Fourth Korea National Health and Nutrition Examination Survey (KNHANES) data set was used to assess the relationship between sleep duration and suicidal ideation. KNHANES assesses the health and nutritional status of Korean civilians, beginning in 1998. The survey was conducted by the Korea Ministry of Health and Welfare and had 3 components: a health interview survey, a health examination survey, and a nutrition survey. The survey was approved by Institutional Review Board of the Korea Centers for Disease Control and Prevention. This study adhered to the tenets of the Declaration of Helsinki. The survey target population was all non-institutionalized South Korean civilian individuals aged 1 year or older. The KNHANES data has been released periodically between 1998 and 2005, and annually since 2007. The fourth KNHANES was conducted for 3 years (2007-2009) and employed stratified, multistage probability sampling units based on geographic area, sex, and age, which were determined by the household registries of the 2005 National Census Registry. The survey was carried out throughout the entire year, except for 2007 when it was implemented for only 6 months (July to December). Thus, the 2007 data were assigned half of the integrated weighted value reflection ratio when combined with the other data (2008-2009) to improve statistical power. The total target population consisted of 31,705 people aged ≥ 1 year (6,455 in 2007; 12,528 in 2008; and 12,722 in 2009), of whom 24,871 people (4,594 in 2007; 9,744 in 2008; and 10,533 in 2009) completed the survey. The average response rate for the survey was 78.4% (71.2% in 2007; 77.8% in 2008; and 82.8% in 2009).
We excluded information from 6,465 individuals aged 1-18 years old and included the data from 18,406 individuals (total response rate: 74.0%) aged ≥ 19 years. We further excluded 3,063 individuals without information on age, education, occupation, income, or marriage; 31 individuals without information on smoking, drinking, and walking; and 76 individuals without information on sleep duration, suicidal ideation, restriction of activity, depression, subjective health status, and chronic illnesses. Thus, a total of 15,236 individuals (1,396 in 2007; 6,505 in 2008; and 7,335 in 2009) were selected for this analysis, which accounts for 82.3% of the 18,406 adult responders.
Variables
Independent Variables
Sleep duration referred to self-reported data responding to the question “How many hours do you usually sleep?” Responses were assigned to one of 5 subcategories: ≤ 5 h, 6 h, 7 h, 8 h, and ≥ 9 h. We used the International Classification of Sleep Disorders 2nd edition definitions of sleep ≤ 5 h as “short sleep” and sleep ≥ 9 h as “long sleep.”40
Dependent Variables
In this study, self-reported data regarding suicidal ideation was extracted from responses to the question “Have you want to die during the last year?” Suicidal ideation was categorized as either “yes” or “no.”
Covariates
Sociodemographic Factors
Age, household income, education level, residency region, occupation, and marital status were included as sociodemographic factors in the analysis. The “age” variable was continuous, and other variables were categorical. Household income was calculated by dividing the household monthly income by the square root of the household size. Survey subjects were ranked from lowest to highest incomes and grouped into 4 household income quartiles. We used the predefined categories as in the raw KNHANES data for categorizing household income. Education level was categorized into 4 groups: elementary school or lower, middle school, high school, and college or higher. The residency regions were categorized into Urban (administrative divisions of a city: Seoul, Daejeon, Daegu, Busan, Incheon, Kwangju, or Ulsan), and Rural (not classified as administrative of a city). Occupational status was divided into 3 categories: white collar (administrative, engineering, scientific, teaching and related occupations, sales and related occupations, service occupation), blue collar (farming, forestry, fishing, and hunting occupations, craft and repair, operators, fabricators and laborers), and the unemployed (including housewife, student).
Health Behavior Factors
Questions about alcohol use, smoking status, walking days per week, and activity restriction were assessed by the health interview survey, and were included as covariates in our analyses. Alcohol use was further assessed by questioning the participants about their average frequency (days per week or month) of alcohol drinking during the last year.
Health Status Factors
The number of chronic diseases, perceived health status, and depressive mood continuing for ≥ 2 weeks during a 1-year time period were also included in the model. The “number of chronic disease(s)” variable included conditions such as high blood pressure, diabetes, stroke, myocardial infarction, and angina. The number of chronic diseases was operationalized into 4 different categories depending on how many were present: 0, 1, 2, and ≥ 3. In response to the question “How do you usually perceive your health?” perceived health status was subcategorized as: very good, good, average, bad, and very bad. In response to the question “Have you felt sadness or despair which hindered everyday life consistently for 2 weeks or more during the last year?” depressive mood was subcategorized as either “yes” or “no.”
Statistical Analysis
T-tests, χ2 tests, and multiple logistic regression analyses were used to analyze whether general characteristics, health status, and health risk behavior had a relationship with suicidal ideation. In this study, 3 different models were tested: Model 1 tested the relationship between sleep duration and suicidal ideation adjusted for age; Model 2 tested the relationship between sleep duration and suicidal ideation adjusted for sociodemographic factors (age, education level, occupation, household income, marital status, and region) and health behavior (alcohol use, smoking status, walking days a week); and Model 3 tested the relationship between sleep duration and suicidal ideation adjusted for health status (number of chronic diseases, activity restriction, perceived health status, and depressive mood) in addition to adjusting for the covariates from Model 2. Statistical analysis software SAS Version 9.2 (SAS Institute, Inc., Cary, NC) was used for data analysis.
RESULTS
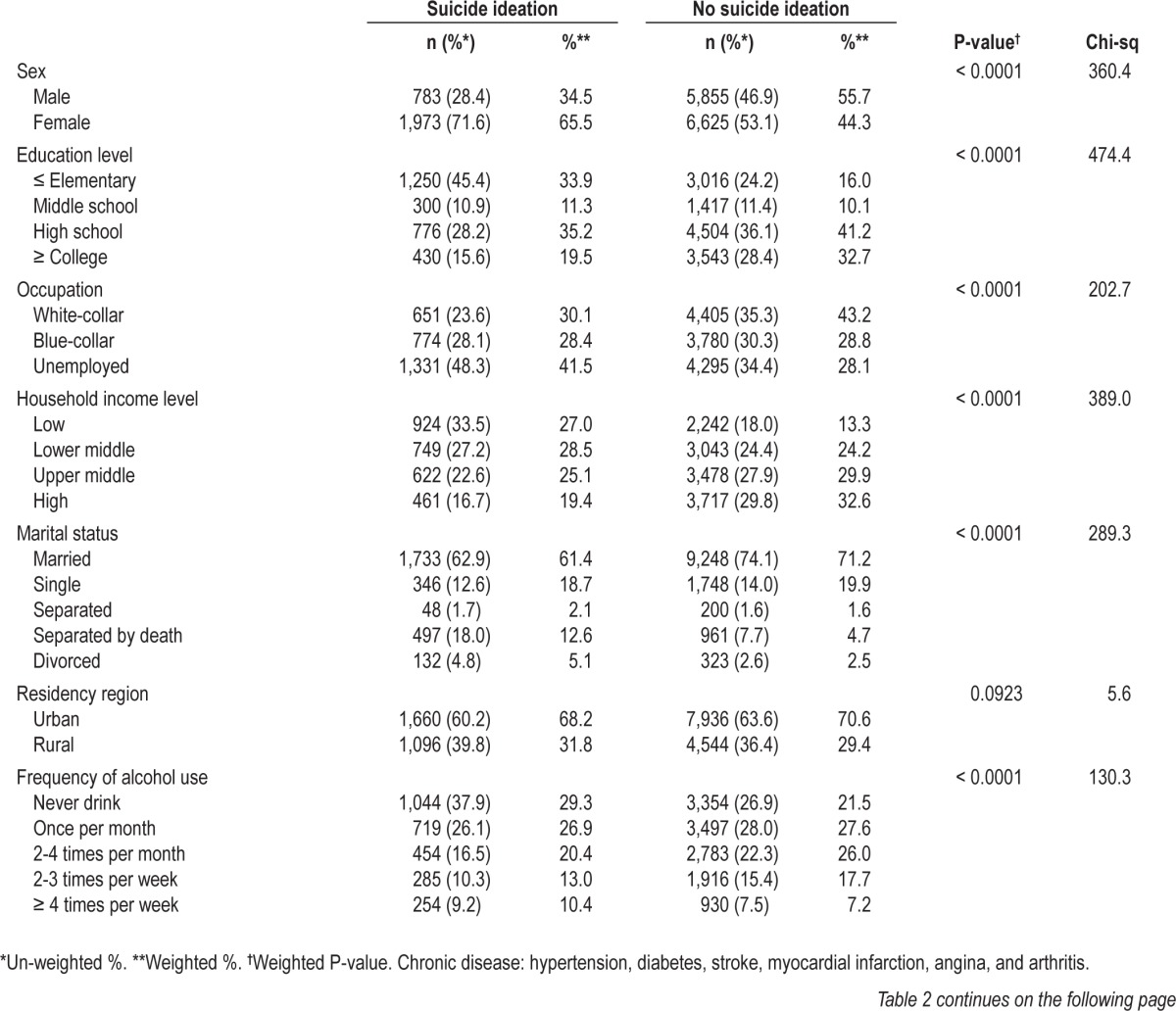
Prevalence of Short Sleep and Long Sleep
Of the 15,236 research subjects included in our study, there were 6,638 males and 8,598 females. The weighted mean age of total population was 43.0 ± 16.3 years. The weighted prevalence of short sleep (≤ 5 h) was 13.3%, and the weighted prevalence of long sleep (≥ 9 h) was 7.7% (Table 1). Of the total sample, 34.5% of males and 65.5% of females had thought of suicide within the prior year. The weighted prevalence of suicidal ideation in people with sleep duration of short sleep (≤ 5 h) was 21.1%, and the weighted prevalence of suicidal ideation in people with long sleep (≥ 9 h) was 9.8% (Table 2).
Table 1.
Demographic characteristics of the study population
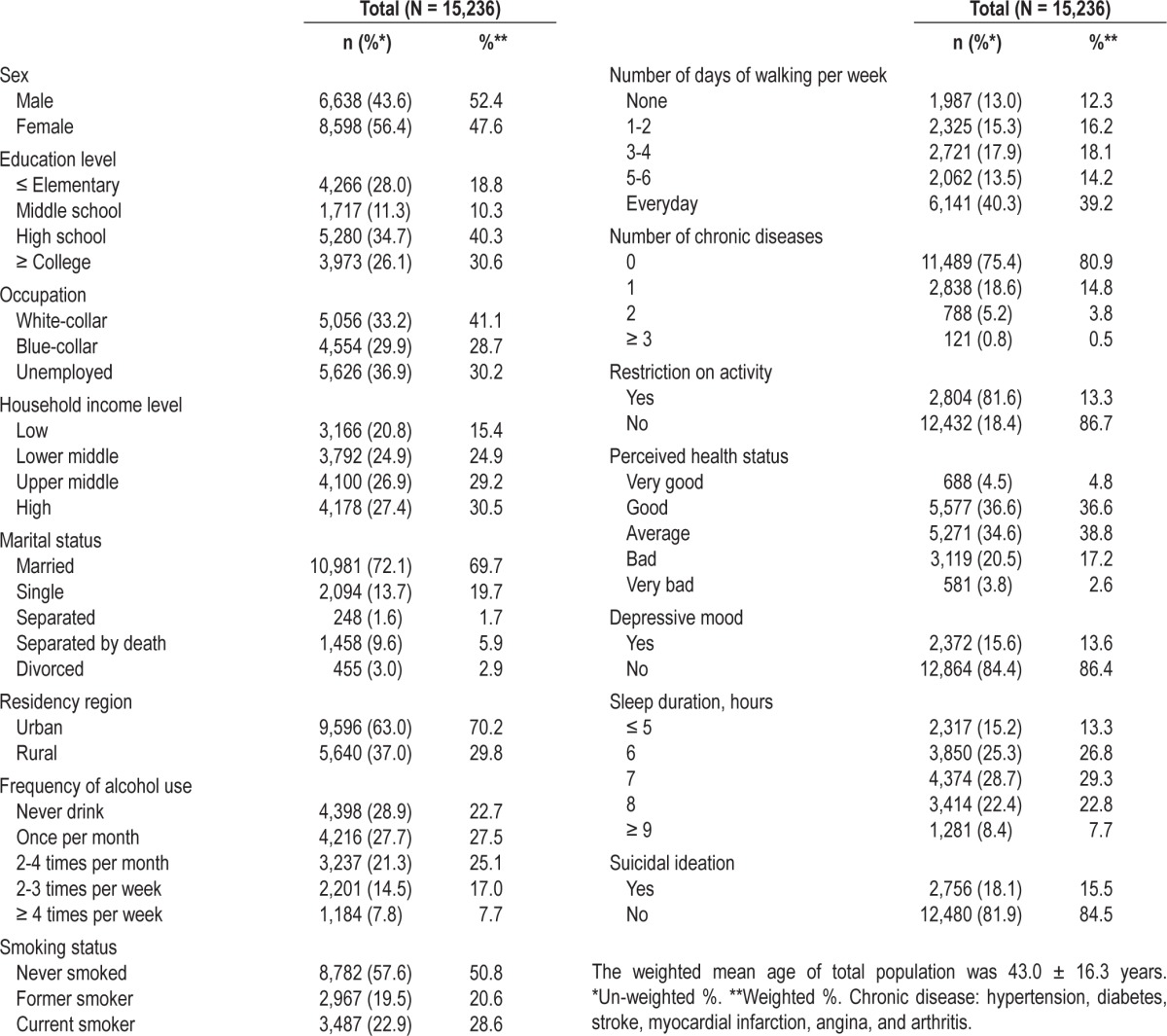
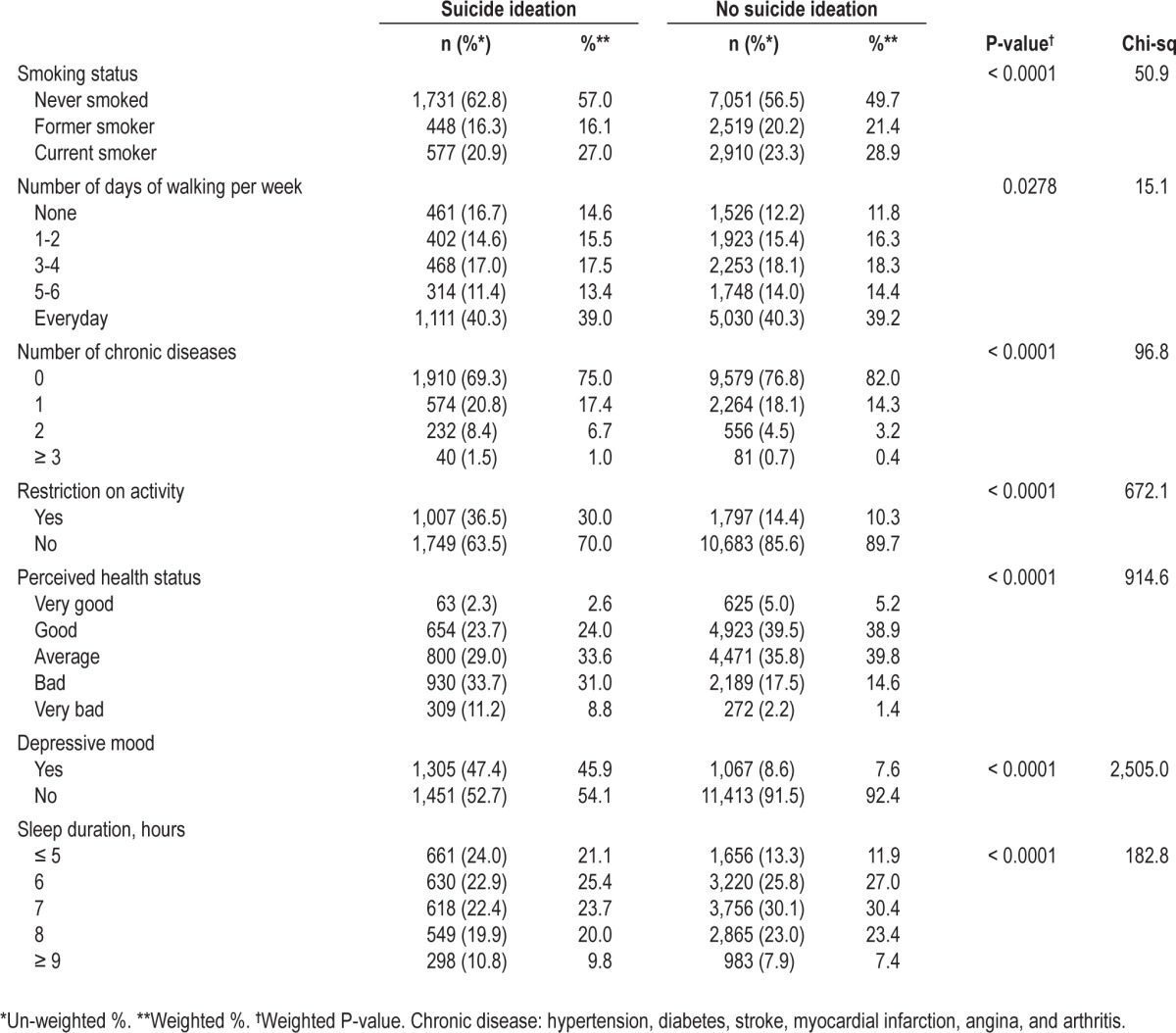
Table 2.
Association between variables and suicidal ideation
Association between Sleep and Suicidal Ideation
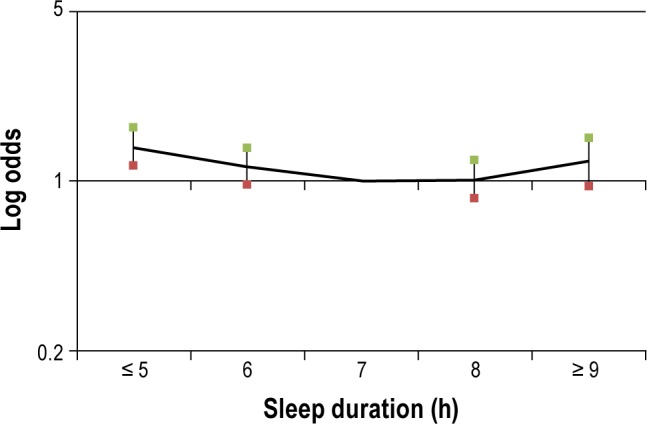
In Model 1 (Figures 1 and 2), adjusted for age and sex, the odds of suicidal ideation in people with short sleep duration was 1.908 times higher (95% CI 1.631-2.233) than in people with sleep duration of 7 h/day (Table 3). People with long sleep were 1.594 times higher (95% CI 1.307-1.945) than people with sleep duration for 7 hours (Table 3). Model 2 (Figures 1 and 2) adjusted for sociodemographic factors and health behavior covariates, in addition to age and sex. The odds of suicidal ideation in people with sleep duration ≤ 5 h/day was 1.569 times higher (95% CI 1.332-1.849) than in people with sleep duration of 7 h/day. The odds of suicidal ideation in people with sleep duration ≥ 9 h/day was 1.236 times higher (95% CI 1.001-1.525) than in people with sleep duration for 7 hours.
Figure 1.
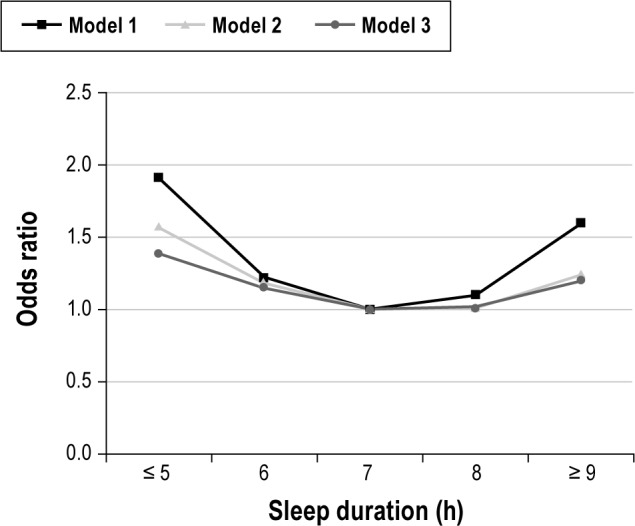
Adjusted association between sleep duration and suicidal ideation. Model 1: Adjusted for age, sex. Model 2: Adjusted for age, sex, education level, occupation, household income level, marital status, residency region, frequency of alcohol use, smoking status, and number of days of walking per week. Model 3: Adjusted for age, sex, education level, occupation, household income level, marital status, residency region, frequency of alcohol use, smoking status, number of days of walking per week, number of chronic disease, restriction on activity, perceived health status, and depressive mood.
Figure 2.
Log odds ratio for suicidal ideation according to sleep duration adjusted for age, sex, education level, occupation, household income level, marital status, residential region, frequency of alcohol use, smoking status, number of days of walking per week, number of chronic disease, restriction on activity, perceived health status, and depressive mood.
Table 3.
Association between sleep duration and suicidal ideation
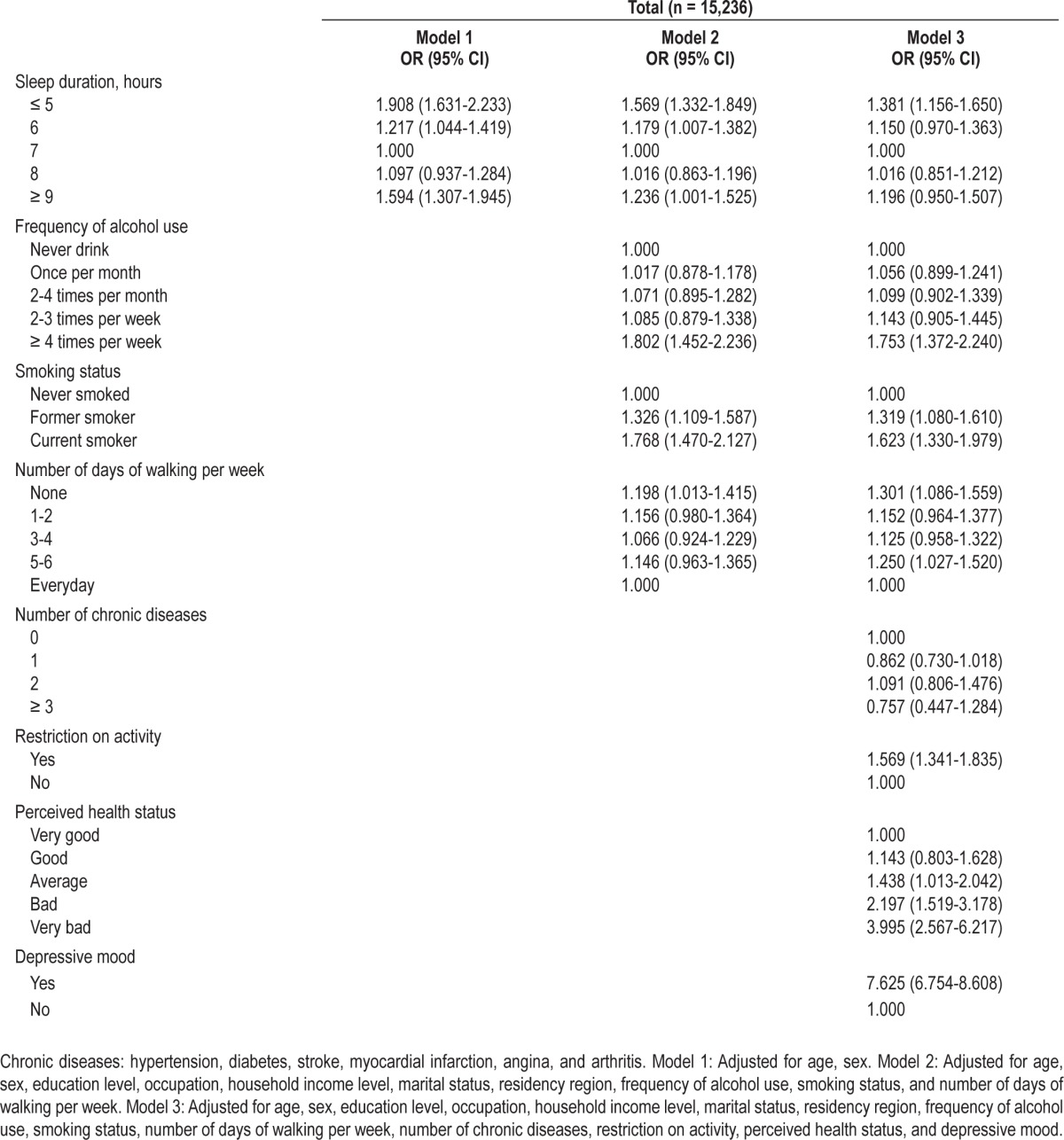
Model 3 (Figures 1 and 2) adjusted for age, sex, education level, occupation, household income, marital status, region, smoking status, alcohol use, exercise, activity restriction, number of chronic disease, perceived health status, and depressive mood. After adjusting for all of these confounders, the odds of suicidal ideation in short sleepers (≤ 5 h/day) (OR: 1.381 95% CI 1.156-1.650) was attenuated, but was still significantly elevated versus subjects who slept 7 hours/day. The odds of suicidal ideation in long sleepers (95% CI 0.950-1.507) was 1.196 times higher than those with sleep duration of 7 h/day, but this was not statistically significant (Table 3).
After adjusting for sociodemographic factors, health behavior and health status, males with short sleep were 52.1% more likely to have suicidal ideation (OR: 1.521 95% CI: 1.091-2.120) than males with 7-h sleep duration. Females with short sleep were 29.4% more likely to have suicidal ideation (OR: 1.294 95% CI 1.052-1.592) than females with 7-h sleep duration. The U-shape is found for both genders, although it appears stronger in males.
DISCUSSION
Sleep Duration among the South Korean Population
The mean sleep duration in 18 OECD countries was 502 minutes.41 Mean sleep duration for Koreans was 469 minutes, the shortest duration among the surveyed nations. The prevalence of insomnia is more than one-fifth (22.8%) of the 5,000 Korean subjects, and it is more common among women (25.3%) than men (20.2%).42 According to this international comparative study on the use of time, adult Korean men (age 20-74 years) worked an average of 381 minutes per day, American men worked 262 minutes per day, and German men worked an average of 225 minutes per day. The average working time of adult Korean women (age 20-74) was 217 minutes per day, whereas American women worked an average of 179 minutes per day and German women worked an average of 124 minutes per day.43 These findings indicate that adults in Korea work longer hours that adults in comparator nations and are therefore more likely to be sleep deprived.
Association between Sleep Duration and Suicidal Ideation
Consistent with previous investigations,5,6,11,14 our results showed that adults of both genders who reported sleeping five hours or less and nine hours or more had a significantly higher risk for suicidal ideation versus adults with sleep duration of seven hours in the age-adjusted model. The association between sleep duration and suicidal ideation is U-shaped and is attenuated by adjustments for other covariates such as sociodemographic factors, health behavior, and health status, the latter of which includes depressive mood.
Possible Mechanisms Associating Sleep and Suicidal Ideation
Short sleep in both genders was significantly associated with suicidal ideation after adjusting for all covariates. Sleep deprivation can cause diverse psychological and physiological impairments, along with endocrine and immunologic changes.44,45 Insufficient sleep can adversely affect judgment, concentration, and impulse control. Although the precise mechanisms of the association between sleep abnormalities and suicidal behaviors require elucidation, several researchers have proposed that inhibition of the serotonin (5-hydroxytriptamine; 5-HT) system plays a significant role in both suicide and sleep.25 In our study, the significant association between long sleep and suicidal ideation disappeared after adjusting for socioeconomic factors, health behavior, and health status, which included depressive mood. This suggests that the long sleep/suicidal ideation association may be mediated by these factors. The authors in the Nurses' Health Study II suggest that depressive symptoms and low socioeconomic status, such as unemployment are associated with long sleep.46 The investigators in the Whitehall II Study and the Western New York Health Study proposed that long sleep might be a consequence of, rather than a predictor for, unrecognized comorbidity.29 Although it has been hypothesized that psychiatric diseases, especially depression, may contribute to the relationship between long sleep and increased mortality, the underlying mechanisms are not well understood.47
Moderate sleep duration plays facilitates functional recovery of central nerves that are exhausted and damaged during the day, and is important in regulating the physical functions of the human body and maintaining overall health. Inadequate sleep deteriorates physical and mental functions and affects metabolism, thereby reducing work efficiency.27,48 Studies conducted in the West and Japan reported that groups with sleep duration less than five hours/day, or inadequate sleep quality or amount due to night terrors and insomnia, had a higher suicide risk.49,50 Clinical and preclinical studies showed a possible association between sleep disturbance and impulsive, aggressive behavior and emotional instability,51 and associated sleep deprivation with panic and anxiety.50 Major depression serves an important marker for suicidal ideation and suicide attempt.52 However, the possible relationship between short sleep duration and suicidal ideation regardless of mental disorder has not been clarified.28 When Spanish research compared patients admitted for mental disorders with the attempted suicide group, these groups had respective 32% and 63% rates of major depression episodes.39 Because sleep disturbance is included in the diagnostic criteria of major depression,27 there exists the possibility for mathematical overcorrection if major depression is adjusted for when analyzing the relationship between sleep duration and suicide risk. Our analysis only adjusted for continuing depressive mood for more than two weeks during the year preceding the survey. The likelihood of short sleep was significantly higher in the suicidal ideation group for both genders. Similarly, the cross-sectional analysis of the National Comorbidity Survey (N = 8,098) conducted in the United States determined that short sleep was related to increased risk of suicidal ideation and suicidal attack regardless of existent comorbid mental disorders.27 The HUNT I study conducted in Norway reported that suicide risk was significantly higher when there were worse sleep problems, although the correlation became weaker after adjusting for common mental disorders and alcohol use.53 To explain the mechanism of association between short sleep duration and increased suicidal ideation, suicide attempts, and suicides, further prospective cohort research that recognize mental disorders such as major depression, anxiety, alcoholism, drug addiction, and impulsive personality disorders are necessary.
Factors Associated with Sleep and Suicidal Ideation
In our study, females had significantly elevated likelihood of suicidal ideation when they walked fewer than two days per week, had smoking experience, or consumed alcohol four or more times per week. The likelihood of suicidal ideation in males was significantly higher when subjects were currently smoking and had activity restrictions. Thus, more attention should be given to the mental health of people who engage in unhealthy behavior. In the 2011 Korean mental health status epidemiologic survey, suicide-related behavior had a strong association with experiencing a mental disorder(s), alcohol use, and smoking.5 Several studies have investigated the associations between lifestyle factors (such as smoking, alcohol consumption, exercise, meals, and family relations) and mental health outcomes.29,54 Takada and colleagues reported that there is no association between suicidal ideation and either smoking or exercise, in either sex.54 They also reported that problem drinking was associated with suicidal ideation in both sexes. In the Whitehall II Study and the Western New York Health Study, researchers suggested that the association between long sleep duration and morbidity may be caused by the lack of physical activity having the effect of infirmity.29 In a prospective cohort study on Korean males and females, exercise was not associated with suicide.55 However, males and females who smoked cigarettes and were problem drinkers had a higher suicide risk.55 Further research into the relationships between lifestyle factors and mental health, including suicidal ideation and attempted suicides attempts, are required.
Study Strengths and Limitations
There are several limitations to this study. First, cross-sectional data was used, so the order of incidence and the causal mechanisms between sleep duration and suicidal ideation cannot be clearly delineated. Second, reported depressive mood was subjective because it was self-recorded, and recall bias can exist. Various mental illnesses including depression, anxiety, and drug addiction are reportedly correlated to suicidal ideation; however, we only controlled for depressive mood that was experienced by individuals for more than two weeks in the year prior to surveying. Future studies should investigate the associations between sleep duration and suicidal ideation after adjusting for other mental illnesses such as anxiety and drug addiction. Third, our measures of suicidal ideation and sleep duration were based on single questions in the survey, which were not specially designed to examine sleep duration/suicidal thoughts associations. The survey item that we designed in relation to the dependent variable, suicidal ideation, was “Have you wanted to die during the last year?” The subsequent survey item was “Have you attempted to kill yourself during the past 1 year?” Thus, although it is likely that the survey respondents accepted the phrase “wanted to die” as a question asking about suicide, the survey content on suicidal ideation remains partly subjective and open to recall bias. Therefore, these findings should be considered preliminary until they are replicated with validated and more precise measures. Despite these limitations, the primary strength of this study is that it assessed a large sample population, so that the results can be generalized to the adult South Korean population.
Implications for Future Study
Because this study has a cross-sectional design, the results possibly reflect reverse causality and bidirectional relations when assessing the association between sleep duration and suicidal ideation. Therefore, longitudinal studies with validated measures of suicidal ideation are required to replicate our findings and to clarify the causality and mechanisms that relatesleep duration, depression, and suicide. Future studies should also refine our understanding of how specific sleep problems contribute to suicidal ideation and behavior. More in-depth studies are needed to determine the associations between elevated suicide risk and sleep problems such as difficulty initiating sleep, difficulty maintaining sleep, time in bed, wake after sleep onset, sleep-onset latency, sleep quality, time at which one goes to bed in the evening, time at which lights are turned out with the intention to sleep, wake time in the morning, and time at which one gets out of bed in the morning, as well as insomnia. Although self-reporting is a valuable information source in large-scale epidemiologic studies, research using more objective measures of sleep duration and sleep problems, such as electroencephalography and actigraphy, are needed to understand the precise mechanisms of the sleep duration/suicidal ideation phenomenon. Serotonin levels are reportedly related not only to sleep duration but also to depression. Thus, conducting a stratified analysis on the association between sleep duration and suicide, according to the changes in serotonin level and depression, will be helpful in expanding our understanding of these related processes. As basic scientific research uncovers neurobiologic and immuno-logic pathway involvement in suicidal thoughts and behavior, it is crucial to clinically investigate how sleep duration interacts with these pathways. Lastly, because it is possible that the association between sleeping problems and suicide outcomes are based on different processes in adolescents and the elderly population when compared to other adults, it is important to conduct additional studies to verify the associations between sleep duration and suicidal ideation in diverse age groups.
CONCLUSIONS
We showed a relationship between extreme sleep duration and suicidal ideation, regardless of a history of depressive mood, in a general Korean adult population. This association existed for both males and females. In 60% of cases, suicide planning and suicide attempt occurs within one year of suicidal ideation.56–58 Revealing factors that are related to suicidal ideation will facilitate our ability to preventing suicide attempts. This research suggests that primary care clinicians should be more attentive in evaluating short sleep duration (reduced total sleep time) in the general population, and supports the need for more attention to depressive mood, suicidal ideation, and mental health in people with short sleep duration.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study was supported by a grant from the Korean Association for Suicide Prevention (7-2012-0110).
REFERENCES
- 1.World Health Organization. Geneva: WHO; 2000. Preventing suicide, mental and behavioural disorders. [Google Scholar]
- 2.Rowe JL, Bruce ML, Conwell Y. Correlates of suicide among home health care utilizers who died by suicide and community controls. Suicide Life Threat Behav. 2006;36:65–75. doi: 10.1521/suli.2006.36.1.65. [DOI] [PubMed] [Google Scholar]
- 3.Mann JJ, Brent DA, Arango V. The neurobiology and genetics of suicide and attempted suicide: A focus on the serotonergic system. Neuropsychopharmacology. 2001;24:467–77. doi: 10.1016/S0893-133X(00)00228-1. [DOI] [PubMed] [Google Scholar]
- 4.Atay IM, Eren I, Gundogar D. [The prevalence of death ideation and attempted suicide and the associated risk factors in isparta, Turkey] Turk Psikiyatri Derg. 2012;23:89–98. [PubMed] [Google Scholar]
- 5.Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31:1097–101. [PMC free article] [PubMed] [Google Scholar]
- 6.Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. J Psychiatr Res. 2009;43:526–31. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong MM, Brower KJ, Zucker RA. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J Psychiatr Res. 2011;45:505–11. doi: 10.1016/j.jpsychires.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agargun MY, Cartwright R. REM sleep, dream variables and suicidality in depressed patients. Psychiatry Res. 2003;119:33–9. doi: 10.1016/s0165-1781(03)00111-2. [DOI] [PubMed] [Google Scholar]
- 9.Bernert RA, Joiner TE, Jr., Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28:1135–41. doi: 10.1093/sleep/28.9.1135. [DOI] [PubMed] [Google Scholar]
- 10.Carli V, Roy A, Bevilacqua L, Maggi S, Cesaro C, Sarchiapone M. Insomnia and suicidal behaviour in prisoners. Psychiatry Res. 2011;185:141–4. doi: 10.1016/j.psychres.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 11.Fitzgerald CT, Messias E, Buysse DJ. Teen sleep and suicidality: results from the Youth Risk Behavior Surveys of 2007 and 2009. J Clin Sleep Med. 2011;7:351–6. doi: 10.5664/JCSM.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, Posner K. Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep. 2010;33:97–106. doi: 10.1093/sleep/33.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee W, Ha J. The association between nonstandard employment and suicidal ideation: data from the First~Fourth National Health and Nutrition Examination Surveys. Korean J Occup Environ Med. 2011;30:89–7. [Google Scholar]
- 14.Rocha FL, Hara C, Rodrigues CV, et al. Is insomnia a marker for psychiatric disorders in general hospitals? Sleep Med. 2005;6:549–53. doi: 10.1016/j.sleep.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Sjostrom N, Waern M, Hetta J. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 2007;30:91–5. doi: 10.1093/sleep/30.1.91. [DOI] [PubMed] [Google Scholar]
- 16.OECD. Paris: Organisation for Economic Cooperation and Development; 2009. OECD family database - OECD Health data 2009. [Google Scholar]
- 17.Kim SY, Kim MH, Kawachi I, Cho Y. Comparative epidemiology of suicide in South Korea and Japan: effects of age, gender and suicide methods. Crisis. 2011;32:5–14. doi: 10.1027/0227-5910/a000046. [DOI] [PubMed] [Google Scholar]
- 18.Hong JP. Seoul: Korean Association for Suicide Prevention; 2011. Korean annual suicide rates (2011) [Google Scholar]
- 19.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 21.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 22.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33:414–20. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bliwise DL. Sleep-related respiratory disturbances. J Gerontol. 1984;39:255. doi: 10.1093/geronj/39.2.255. [DOI] [PubMed] [Google Scholar]
- 24.Faubel R, Lopez-Garcia E, Guallar-Castillon P, et al. Sleep duration and health-related quality of life among older adults: a population-based cohort in Spain. Sleep. 2009;32:1059–68. [PMC free article] [PubMed] [Google Scholar]
- 25.Kohyama J. Sleep, serotonin, and suicide in Japan. J Physiol Anthropol. 2011;30:1–8. doi: 10.2114/jpa2.30.1. [DOI] [PubMed] [Google Scholar]
- 26.Sechter D, Bonin B, Bertschy G, Vandel S, Bizouard P. [Prediction of suicide risk] Encephale. 1991;17:361–4. Spec No 3. [PubMed] [Google Scholar]
- 27.Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004;27:1351–8. doi: 10.1093/sleep/27.7.1351. [DOI] [PubMed] [Google Scholar]
- 28.Agargun MY, Kara H, Solmaz M. Sleep disturbances and suicidal behavior in patients with major depression. J Clin Psychiatry. 1997;58:249–51. doi: 10.4088/jcp.v58n0602. [DOI] [PubMed] [Google Scholar]
- 29.Stranges S, Dorn JM, Shipley MJ, et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol. 2008;168:1353–64. doi: 10.1093/aje/kwn337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Monti JM, Monti D. Sleep disturbance in generalized anxiety disorder and its treatment. Sleep Med Rev. 2000;4:263–76. doi: 10.1053/smrv.1999.0096. [DOI] [PubMed] [Google Scholar]
- 31.Fortune SA, Hawton K. Deliberate self-harm in children and adolescents: a research update. Curr Opin Psychiatry. 2005;18:401–6. doi: 10.1097/01.yco.0000172059.55778.c9. [DOI] [PubMed] [Google Scholar]
- 32.Amitai M, Apter A. Social aspects of suicidal behavior and prevention in early life: a review. Int J Environ Res Public Health. 2012;9:985–94. doi: 10.3390/ijerph9030985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kokkevi A, Rotsika V, Arapaki A, Richardson C. Adolescents' self-reported suicide attempts, self-harm thoughts and their correlates across 17 European countries. J Child Psychol Psychiatry. 2012;53:381–9. doi: 10.1111/j.1469-7610.2011.02457.x. [DOI] [PubMed] [Google Scholar]
- 34.Knutson KL, Turek FW. The U-shaped association between sleep and health: the 2 peaks do not mean the same thing. Sleep. 2006;29:878–9. doi: 10.1093/sleep/29.7.878. [DOI] [PubMed] [Google Scholar]
- 35.Fujino Y, Mizoue T, Tokui N, Yoshimura T. Prospective cohort study of stress, life satisfaction, self-rated health, insomnia, and suicide death in Japan. Suicide Life Threat Behav. 2005;35:227–37. doi: 10.1521/suli.35.2.227.62876. [DOI] [PubMed] [Google Scholar]
- 36.Yen CF, King BH, Tang TC. The association between short and long nocturnal sleep durations and risky behaviours and the moderating factors in Taiwanese adolescents. Psychiatry Res. 2010;179:69–74. doi: 10.1016/j.psychres.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 37.Hawton K. Sex and suicide : Gender differences in suicidal behaviour. Br J Psychiatry. 2000;177:484–5. doi: 10.1192/bjp.177.6.484. [DOI] [PubMed] [Google Scholar]
- 38.Voros V, Osvath P, Fekete S. [Gender differences in suicidal behavior] Neuropsychopharmacol Hung. 2004;6:65–71. [PubMed] [Google Scholar]
- 39.Blasco-Fontecilla H, Alegria AA, Lopez-Castroman J, et al. Short self-reported sleep duration and suicidal behavior: a cross-sectional study. J Affect Disord. 2011;133:239–46. doi: 10.1016/j.jad.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 40.American Academy of Sleep Medicine. Westchester, Illinois: American Academy of Sleep Medicine; 2005. International classification of sleep disorders, 2nd ed.: diagnostic and coding manual. [Google Scholar]
- 41.OECD. Special Focus: Measuring Leisure in OECD Countries. Society at a Glance 2009: Organisation for Economic Cooperation and Development. 2009 [Google Scholar]
- 42.Cho YW, Shin WC, Yun CH, Hong SB, Kim J, Earley CJ. Epidemiology of insomnia in Korean adults: prevalence and associated factors. J Clin Neurol. 2009;5:20–3. doi: 10.3988/jcn.2009.5.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim OS, Lee KY, Lee YS, Cho HK, Lee SM. A comparative study of life time use for Korean, American, and German adults. Korea National Statistical Office. 2005 [Google Scholar]
- 44.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 45.Vgontzas AN, Mastorakos G, Bixler EO, Kales A, Gold PW, Chrousos GP. Sleep deprivation effects on the activity of the hypothalamic-pituitary-adrenal and growth axes: potential clinical implications. Clin Endocrinol (Oxf) 1999;51:205–15. doi: 10.1046/j.1365-2265.1999.00763.x. [DOI] [PubMed] [Google Scholar]
- 46.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Youngstedt SD, Kripke DF. Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev. 2004;8:159–74. doi: 10.1016/j.smrv.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 48.Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McCall WV, Blocker JN, D'Agostino R, Jr, et al. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med. 2010;11:822–7. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep. 2011;34:93–8. doi: 10.1093/sleep/34.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li SX, Lam SP, Yu MW, Zhang J, Wing YK. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. J Clin Psychiatry. 2010;71:1440–6. doi: 10.4088/JCP.09m05661gry. [DOI] [PubMed] [Google Scholar]
- 52.Nrugham L, Larsson B, Sund AM. Specific depressive symptoms and disorders as associates and predictors of suicidal acts across adolescence. J Affect Disord. 2008;111:83–93. doi: 10.1016/j.jad.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 53.Bjorngaard JH, Bjerkeset O, Romundstad P, Gunnell D. Sleeping problems and suicide in 75,000 Norwegian adults: a 20 year follow-up of the HUNT I study. Sleep. 2011;34:1155–9. doi: 10.5665/SLEEP.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Takada M, Suzuki A, Shima S, Inoue K, Kazukawa S, Hojoh M. Associations between lifestyle factors, working environment, depressive symptoms and suicidal ideation: a large-scale study in Japan. Ind Health. 2009;47:649–55. doi: 10.2486/indhealth.47.649. [DOI] [PubMed] [Google Scholar]
- 55.Jee SH, Kivimaki M, Kang HC, Park IS, Samet JM, Batty GD. Cardiovascular disease risk factors in relation to suicide mortality in Asia: prospective cohort study of over one million Korean men and women. Eur Heart J. 2011;32:2773–80. doi: 10.1093/eurheartj/ehr229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Crosby AE, Sacks JJ. Exposure to suicide: incidence and association with suicidal ideation and behavior: United States, 1994. Suicide Life Threat Behav. 2002;32:321–8. doi: 10.1521/suli.32.3.321.22170. [DOI] [PubMed] [Google Scholar]
- 57.De Leo D, Cerin E, Spathonis K, Burgis S. Lifetime risk of suicide ideation and attempts in an Australian community: prevalence, suicidal process, and help-seeking behaviour. J Affect Disord. 2005;86:215–24. doi: 10.1016/j.jad.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 58.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]


