Abstract
Objective:
To ascertain the risk of a new vascular event (NVE) occurring after ischemic stroke and evaluate differences in risk based on stroke subtype.
Methods:
This was a prospective observational study of consecutive patients with nonfatal stroke recruited at a single tertiary stroke center with follow-up ranging from 2 to 5 years (average, 31 ± 15.9 months). An NVE (vascular death, nonfatal stroke or myocardial infarction, and hospitalization for other atherothrombotic events) was defined according to criteria used in a previously developed large multicenter register of atherothrombotic patients (Reduction of Atherothrombosis for Continued Health Registry [REACH]). We analyzed age, sex, and atherosclerotic burden (AB) based on a number of vascular risk factors, affected vascular areas, and stroke subtype according to Stop Stroke Study Trial of Org 10172 in Acute Stroke Treatment (SSS-TOAST) criteria in cardioaortic, large artery atherosclerosis (LAA), unclassified (more than one causal mechanism), small-artery disease (SAD), and undetermined (without cause) stroke categories.
Results:
The final cohort consisted of 748 patients. An NVE occurred in 162 patients (21.7%), equivalent to a rate of 0.084 events per patient/year. Multivariate analysis revealed that higher NVE risk was associated with AB and 3 stroke subtypes, namely cardioaortic (hazard ratio [HR] = 2.58; 95% confidence interval [CI] 1.27–5.22), LAA (HR = 4.17; 95% CI 2.03–8.56), and unclassified (HR = 5.70; 95% CI 2.49–13.08). Patients with SAD or stroke of undetermined cause had lower NVE risk.
Conclusions:
Patients who survive stroke are at increased risk for NVEs. The risk for NVE varies according to stroke subtype.
Little is known about a patient's vascular risk after ischemic stroke compared to risk after diagnosis with other vascular conditions, such as ischemic heart disease.1 Few validated vascular risk stratification scales are available to assess stroke patients, and published studies differ in their definition of new vascular events, variables analyzed, and length of follow-up.2–5 Further, ischemic stroke is characterized by highly differentiated subtypes.6–9 Although studies such as Reduction of Atherothrombosis for Continued Health Registry (REACH) (an international, prospective, observational study of individuals at risk for atherothrombotic events) demonstrated differences in prognosis according to vascular risk factors, those investigations did not consider stroke subtype.10,11 For this study, our objective was to analyze the risk of a new vascular event (NVE) occurring after the acute phase of an ischemic stroke and to evaluate differences in risk based on stroke subtype.
METHODS
Study design.
The prospective BasicMar register includes all patients who were diagnosed with ischemic stroke or cerebral hemorrhage at Barcelona's Hospital del Mar since 2005. This tertiary stroke center (with an on-call neurologist and a stroke unit, as well as capabilities for systemic thrombolysis and neurovascular interventions), which includes a catchment area comprising the 300,000 inhabitants of 3 of the 10 city districts of Barcelona, is the only public hospital capable of treating acute stroke. The hospital follows previously described patient care methods and secondary prevention measures according to the most recent European and American guidelines.12 We designed a complementary, prospective, observational registry of patients admitted from June 2007 to May 2010 (n = 1,002) who presented with NVE in the study follow-up period after having an ischemic stroke or TIA. Maximal follow-up was 60 months (through June 2012). We included all patients, regardless of history of cerebrovascular, coronary, or peripheral artery disease (PAD). For the defined follow-up period, detection of a 2% difference between stroke subtypes required a sample size of 93 cases for each stroke subtype. Exclusion criteria included the following: fatal stroke11 within 28 days of stroke onset (n = 163; 16.3%); residence outside the hospital service area, as it deterred long-term follow-up (n = 51; 6.1%); and stroke categorized according to Stop Stroke Study Trial of Org 10172 in Acute Stroke Treatment (SSS-TOAST) (an evidence-based causative classification system for ischemic stroke)7 as “other causes” (n = 32; 4.1%). We also excluded patients who did not undergo any extracranial or intracranial arterial studies to establish etiology (n = 4; 0.5%), those who did not present at the 3-month follow-up appointment (n = 3; 0.4%), and those who did not provide informed consent to participate in this study (n = 1; 0.1%) (figure e-1 on the Neurology® Web site at www.neurology.org).
Follow-up consisted of a clinic visit at 3 months and then, at the physician's discretion, a clinic appointment or telephone contact every 6 months thereafter. In the case of patients lost to follow-up after the 3-month visit (n = 62; 8.3%), we consulted electronic medical records, the primary care physician, or hospital admissions records. At study conclusion, we reviewed all patient events and death records. For all cases of NVE, we accessed the clinical record to determine all tests and procedures performed and events certified by a neurologist, cardiologist, or vascular surgeon. A member of the investigative team validated each event, and when necessary we contacted the attending doctors for confirmation.
Endpoint.
The study endpoint was presentation with an NVE, defined according to the REACH study criteria11: vascular death, nonfatal stroke, nonfatal myocardial infarction (MI), or hospitalization for an atherothrombotic event, including vascular interventions. We did not include patients in our analysis who presented with NVEs that occurred within 28 days of stroke onset. We did not consider vascular interventions performed at least 28 days after the stroke as a secondary prevention strategy or as a hospitalization event unless associated with a further vascular complication. We discovered 2 vascular deaths following utilization of secondary prevention strategies among the patients studied. One patient died from cerebral hemorrhage after intracranial stent placement and one from cardiac complications after carotid artery surgery.
Study variables.
We recorded age, sex, and anthropometric measurements, identified vascular risk factors according to REACH definitions, and included hypertension, dyslipidemia, diabetes, atrial fibrillation, heart failure, and obesity.11 In addition, we determined involvement of the following vascular disorders using REACH criteria: 1) documented coronary artery disease (CAD), consisting of one or more of the following: stable or unstable angina, history of percutaneous coronary intervention or surgery, or previous MI; 2) documented PAD, consisting of current intermittent claudication with an ankle brachial index of less than 0.9 or a history of intermittent claudication, together with a previous related intervention, such as amputation; or 3) documented cerebrovascular disease, consisting of a hospital or neurologist diagnosis of TIA or ischemic stroke.
Following the REACH methodology and based on previous data,13–15 we divided the cohort into 4 subgroups according to atherosclerotic burden (AB), using the following scores: 0 points, fewer than 3 vascular risk factors and not affecting other vascular territories (CAD or PAD); 1 point, 3 or more risk factors; 2 points, 1 vascular territory affected (in addition to cerebrovascular); and 3 points, 2 vascular territories affected. AB scores of 2 and 3 were independent of the number of vascular risk factors. For each patient, we determined stroke subtype according to SSS-TOAST classification7: large-artery atherosclerosis (LAA), small-artery disease (SAD), cardioaortic embolism (CE), undetermined causes, and unclassified strokes (more than one apparent mechanism). Physicians assessed patients with LAA for the presence of intracranial disease.
Standard protocol approvals, registrations, and patient consents.
The local ethics committee approved the study proposal. We obtained written informed consent from all participants (or a designated representative).
Statistical analysis.
For continuous variables, we present data as means ± SD and categorical variables as frequencies and percentages. We used t test and analysis of variance to evaluate the differences in means for continuous variables and the Fisher exact test for categorical variables. We calculated the relative average rate (events per patient-year) as the number of new events found during follow-up divided by the number of years at-risk patients were followed up. Further, we categorized vascular risk factors and history of vascular events into 4 subgroups based on defined AB scores. We used Cox regression survival analysis to estimate multivariate hazard ratio (HR) with 95% confidence interval (CI) for an NVE. Reference subgroups in multivariate analysis were those with an AB score of 0 and the stroke subtype with the lowest percentage of events (undetermined stroke). We adjusted all multivariate models by age and sex and considered 2-sided p values <0.05 as significant. A team biostatistician reviewed all statistical analyses.
RESULTS
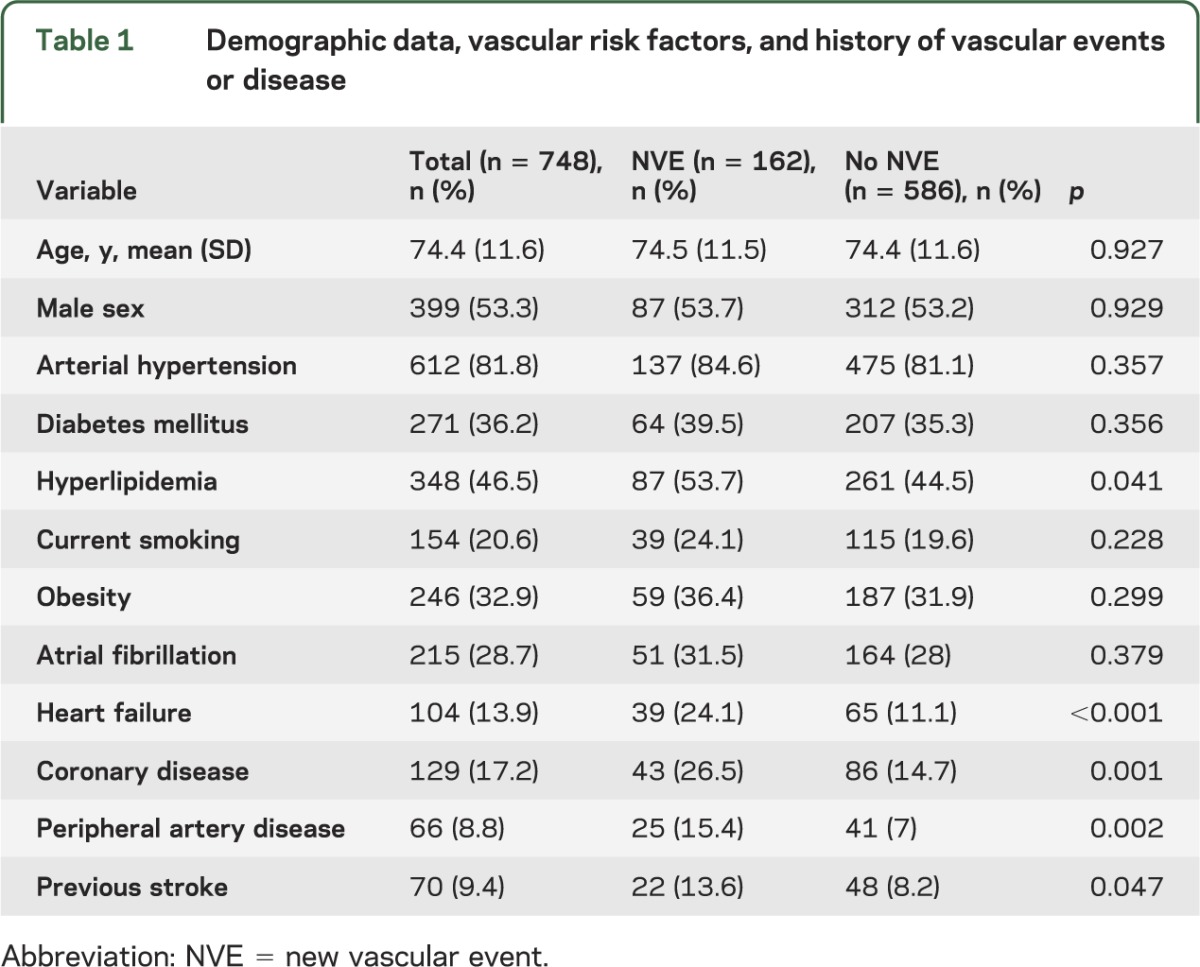
The final study sample consisted of 748 patients. Demographics and vascular risk factors are shown in table 1. All patients completed the follow-up through June 2012 except 124 cases that were lost to follow-up (n = 14, 11 discharged home outside the study area and 3 lost for unknown reasons) or death due to nonvascular causes (n = 107, notably with no NVE recorded during follow-up). An NVE was detected in 162 patients (21.7%), 0.084 events per patient/year. Average follow-up was 31 ± 15.9 months (35.2 ± 14 in patients with no event vs 15.9 ± 13 in those with an NVE).
Table 1.
Demographic data, vascular risk factors, and history of vascular events or disease
Types of event.
Recorded NVEs included 50 (6.7%) vascular deaths, which were then divided into the following subcategories: 24 due to fatal cerebrovascular disease (4 hemorrhagic), 4 to fatal MI, and 22 to other causes (6 other cardiac origin, 7 vascular or limb infarction origin, and 9 unexpected). Of 52 (7%) nonfatal strokes, 3 were hemorrhagic. Nonfatal MI occurred in 18 (2.4%) patients and 42 (5.6%) were hospitalized for atherothrombotic events (2 aortic pathology, 7 TIA, 15 cardiac origin, 18 vascular peripheral disease, 4 embolectomy, 7 vascular surgery or angioplasty, and 6 amputation of foot secondary to diabetic complications). Of these 162 events, 83 (11.1% of the patient cohort) were cerebrovascular (fatal stroke, nonfatal stroke, and hospitalized for TIA; rate of early recurrent stroke within 90 days was 2.9%) and 79 (10.6%) were noncerebrovascular, 53 of which (7.1%) had a cardiac NVE (cardiovascular death, MI, or hospitalization due to cardiac cause).
Factors associated with NVEs.
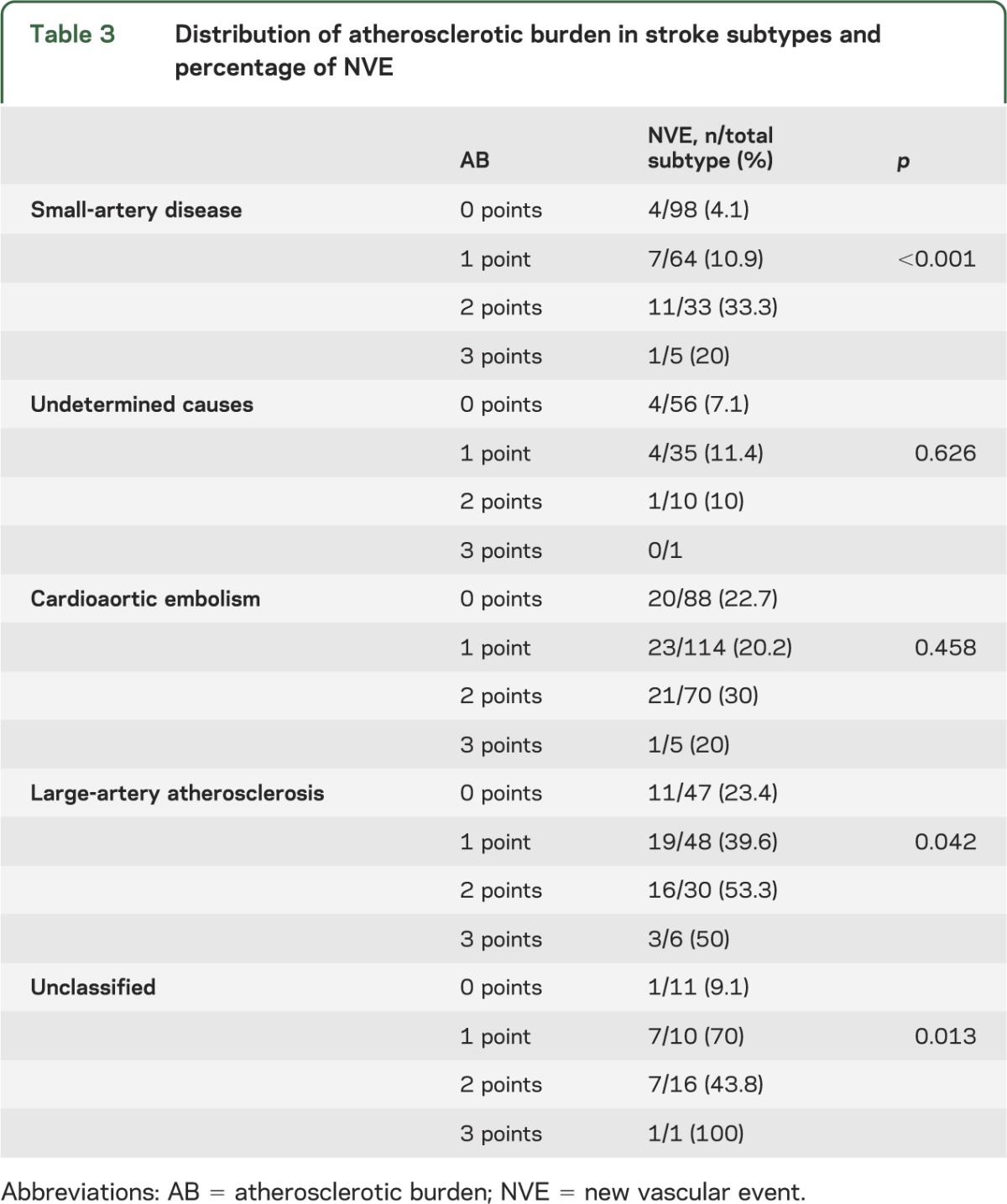
Univariate analysis of age, sex, and vascular risk factors or previous vascular events and relationship to NVE are described in table 1. We found associations of hyperlipidemia, heart failure, CAD, PAD, and previous stroke to NVE occurrence. Table 2 shows univariate analysis results of NVE related to AB subgroup and stroke subtype. There were a higher number of events by patient-year for patients with higher AB scores (p < 0.0001) and for 3 stroke subtypes, namely unclassified, LAA, and CE strokes (p < 0.001). In the LAA subtype, 78 (59.5%) patients had extracranial artery disease, 33 (25.2%) had intracranial disease, and 20 (15.3%) had both intracranial and extracranial disease. We found no association of risk for NVE (p = 0.435) with intracranial or extracranial disease. Table 3 shows the distribution of AB by stroke subtype and its relationship to NVE rate, which correlated to NVEs for the SAD, unclassified, and LAA subtypes.
Table 2.
Univariate analysis of new vascular events in relation to atherosclerotic burden and stroke subtype
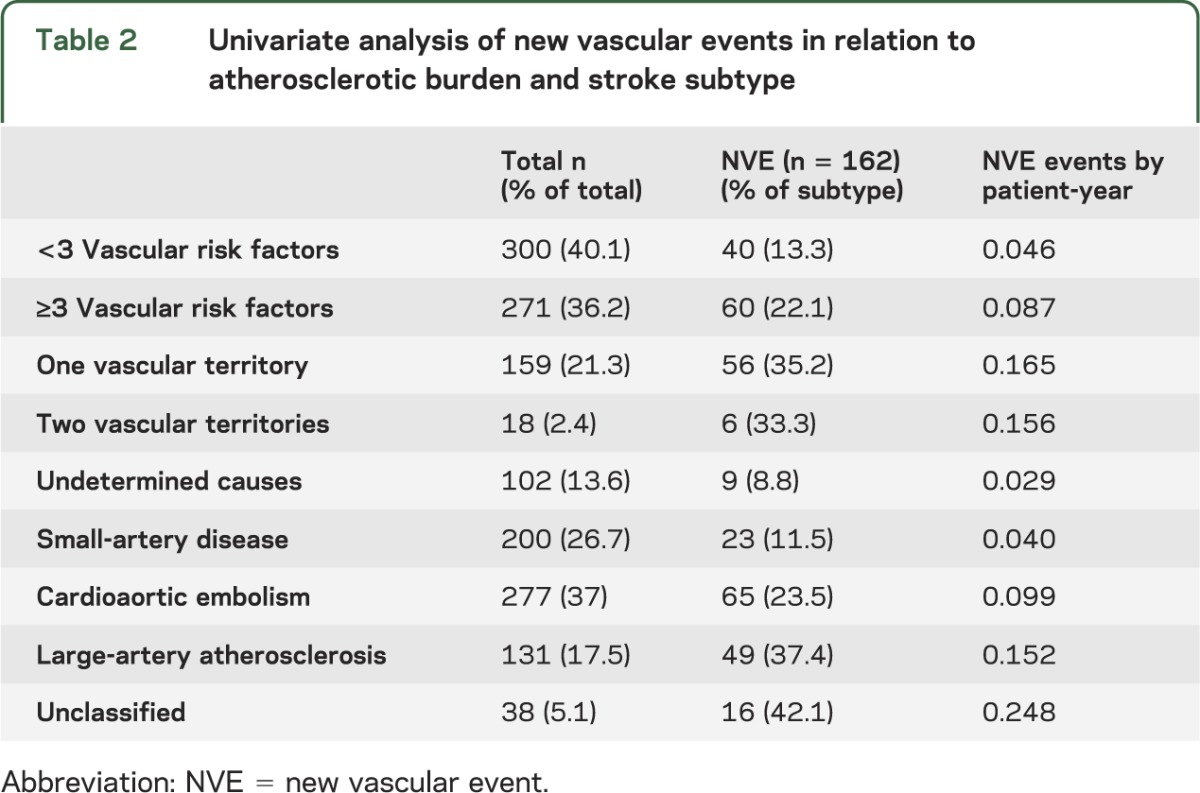
Table 3.
Distribution of atherosclerotic burden in stroke subtypes and percentage of NVE
When adjusted for age, sex, AB score, and stroke subtype, multivariate analysis showed associations between risk for NVE after stroke with AB and the same 3 stroke subtypes (table 4, figure 1, figure e-2). Using further multivariate model analysis that included the vascular risk factors identified by univariate analysis (hyperlipidemia, heart failure, PAD, CAD, and any other previous stroke), we found an independent association between NVEs after stroke and the same 3 stroke subtypes: CE (p = 0.006; adjusted HR = 2.7, 95% CI 1.3–5.5), LAA (p < 0.001; adjusted HR = 4, 95% CI 2–8.3), and unclassified (p < 0.001; adjusted HR = 6, 95% CI 2.6–13.8). Multivariate analysis for noncerebrovascular events only, including variables from the previous models, showed an independent association with the same stroke subtypes: CE (p = 0.025; adjusted HR = 3.9, 95% CI 1.2–12.7), LAA (p = 0.012; adjusted HR = 4.8, 95% CI 1.4–16.5), and unclassified (p = 0.005; adjusted HR = 7, 95% CI 1.8–27.7).
Table 4.
Multivariate analysis of new vascular events in relation to atherosclerotic burden and stroke subtype adjusted by age and sex
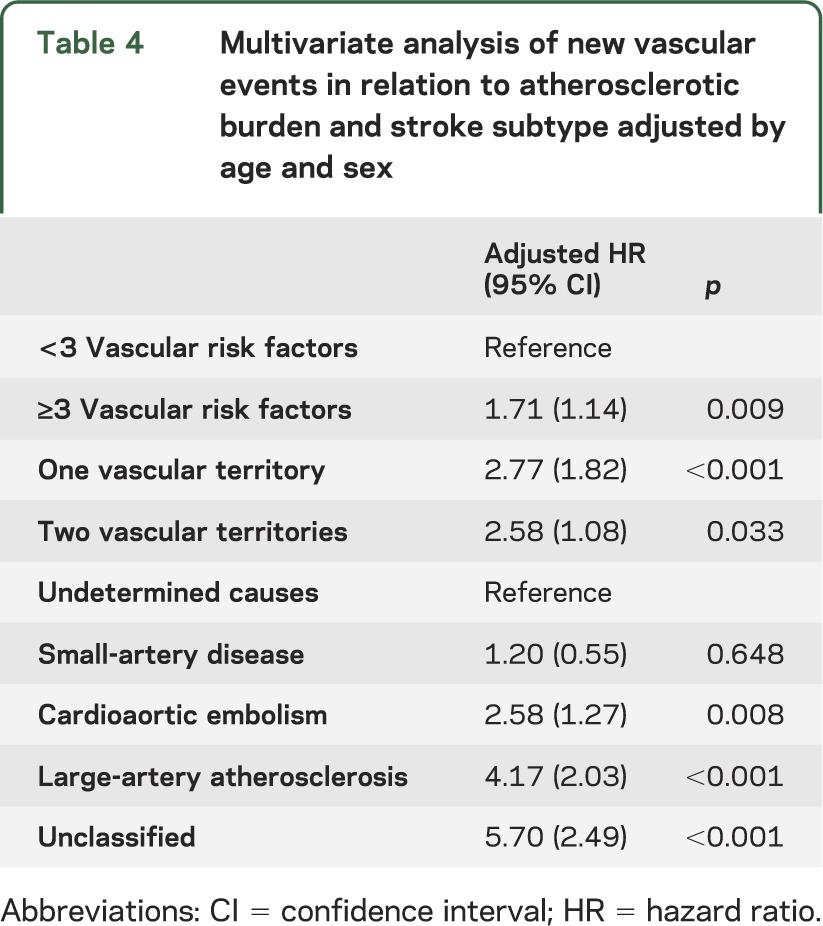
Figure 1. Risk for new vascular events (hazard function) by stroke subtypes adjusted for age, sex, and atherosclerotic burden.
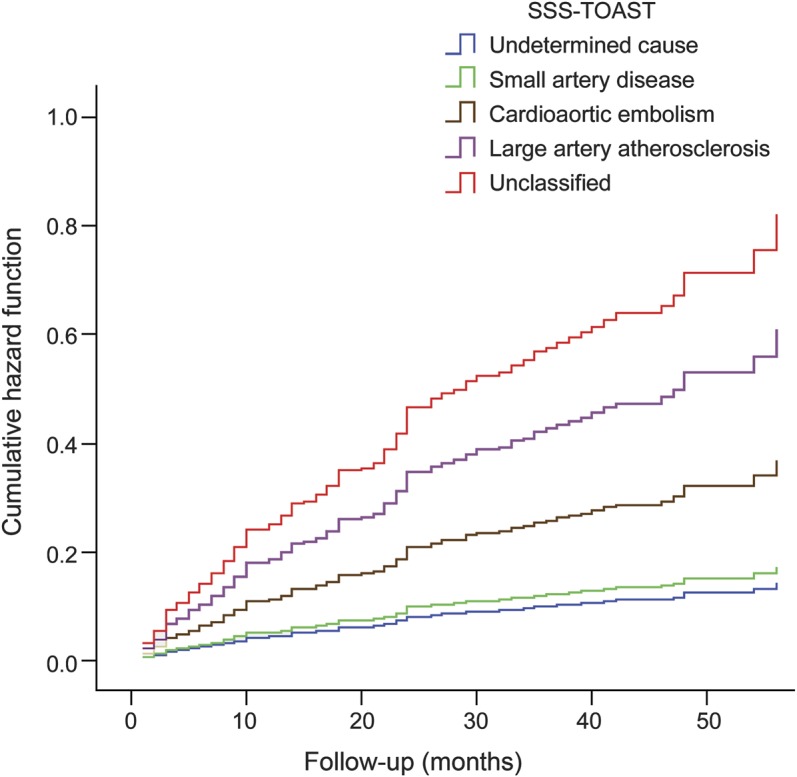
SSS-TOAST= Stop Stroke Study Trial of Org 10172 in Acute Stroke Treatment (evidence-based causative classification system for ischemic stroke).
DISCUSSION
We demonstrate groundbreaking evidence that ischemic stroke is a high-risk vascular disease (>20% overall risk of vascular complications at 10 years)16; further, we found independent differences in patients' vascular risk dependent upon stroke subtype classification by SSS-TOAST, a modern scale that focuses on the etiologic cause of the stroke.
Our observations regarding NVE risk after stroke are within the range described by previous studies that included long-term follow-up (17.4% to 41.3% at 4 or 5 years) and different vascular endpoints (MI, vascular death, or vascular events).3,5,17,18 Vascular risk after ischemic stroke is less well-described and available data are also heterogeneous because of differences in the length of follow-up and the definitions used. Most data come from the REACH register, a multicountry, multicenter study designed to mimic the best available epidemiologic data on atherothrombosis or at-risk outpatients in each participating country, which included 18,189 patients with history of cerebrovascular disease.10 REACH reported a 21.05% NVE rate at 2-year follow-up.15 Our patient profile differs from but complements the REACH dataset in that we report very similar data over a longer average follow-up, collected only for hospitalized patients in a single center.
Although some studies report no differences in risk based on stroke subtype,19–21 new American Heart Association recommendations include only patients with atherothrombotic stroke in the group at high coronary risk, which suggests a need for further analysis of other stroke subtypes.1 We specifically designed the present study to detect any NVE after stroke, and our results confirm the high-risk status of patients with LAA strokes,1,22 as well as those with unclassified and CE strokes. Traditionally, patients with unclassified stroke subtype (more than one causal mechanism of stroke) have been classified together with those whose cause of stroke is unknown (undetermined, according to the TOAST classification). As a result, the actual importance of the unclassified subtype in the overall context of stroke and the associated risk of vascular disease or of recurrence was not known. In our cohort, unclassified subtype made up 5% of all strokes and, as might be surmised from their multiple causes, patients in this category had the highest vascular risk, along with patients with LAA subtype. Given the important differences in risk between the unclassified and undetermined cause subtypes, this result warrants further study.
Our results also indicate greater vascular risk in patients with CE stroke subtype. In these patients, increased vascular risk can be explained by a high risk of embolism, primarily cerebrovascular but also in the peripheral arteries. Nonetheless, the RE-LY study23 reports that a control group of isolated atrial fibrillation patients taking warfarin had more ischemic cardiac events and cardiac deaths than cerebrovascular events. Therefore, we must take into account the major risk of noncerebrovascular complications in these patients.
SAD is an especially controversial stroke subtype. Contradictory prognostic data have been published; studies show greater vascular risk on the one hand, along with worse prognosis in the very long term,21,24,25 and on the other hand lower risk of recurrence and disability.19,22,26 Although stroke patients with SAD have the same vascular risk factors as other subtypes, the distinct absence of physiopathology associated with LAA or structural heart disease lowers their vascular risk according to our results. Occurrence and distribution of vascular complications are almost identical to those recently published in a lengthy international cohort study of rigorously selected patients with SAD (SPS3 study) and a follow-up period similar to ours.27
Patients in the undetermined stroke subtype in whom an exhaustive cardioembolism study is negative have traditionally been described as having low vascular risk and low stroke recurrence.28 A more recent study reports a higher recurrence risk in patients with undetermined cause of stroke than in those with SAD.29 In our study, however, the recurrence rate was low and similar in both subtypes.
In addition to our primary objective, we assessed other aspects that might be related to increased vascular risk. As might be expected, the percentage of individuals at risk of an NVE was higher in the presence of dyslipidemia, heart failure, and history of CAD, PAD, or stroke. Curiously, dyslipidemia is included in CAD and PAD scales but not in scales validated to assess risk after stroke.3 Only the SPI-II and REACH register evaluated heart failure, which may be an important vascular risk factor.3,11 Even though we did not aim to establish these factors as predictive of vascular risk after stroke, our results strongly support their inclusion in future risk estimation.
In our study, similar to other reports,13,14,30 we found that the number of vascular territories previously affected (AB) independently correlated with the NVE occurrence. Moreover, we found a clear increase in NVE risk based on the AB score in SAD and LAA subtype patients. Therefore, AB analysis may be a good tool for assessment of vascular risk in patients with a hypothetical low-risk profile.
Finally, it is well-known that in patients with ischemic stroke, NVEs are usually cerebrovascular.15,22,31 We found this as well in that more than half of NVEs were cerebrovascular. Fatal and nonfatal MIs and non-neurologic cause of death were less common. As a result, we only identified differences between stroke subtypes in terms of risk for NVE. To further explore this question, we reanalyzed our data, excluding any patient who presented with a new cerebrovascular event, and obtained results very similar to those discussed above with the same independent differences for stroke subtypes. Noncerebrovascular risk was highest in the unclassified subtype, followed by the LAA subtype. We did not have sufficient numbers to determine coronary risk in each stroke subtype.
Despite secondary prevention measures, we know that a high number of patients will present with an NVE over the course of prolonged follow-up after stroke. Observed differences in vascular risk based on stroke subtype are logical, taking into account the different causal mechanisms involved. Future studies aimed at evaluating the vascular risk of stroke patients must take stroke subtype into account. Vascular risk is lower in patients with SAD or undetermined stroke and higher when more than one causal mechanism or an atherothrombotic mechanism is determined. Therefore, it is essential to analyze cases of undetermined stroke as a subtype distinct from unclassified strokes. In stroke patients with SAD, the lower risk score for an NVE may be adjusted in accordance with the AB score.
Supplementary Material
ACKNOWLEDGMENT
Isaac Subirana, MSc, Epidemiology and Cardiovascular Genetics, Inflammatory and Cardiovascular Disorders Research Program (IMIM), reviewed statistical analysis. Elaine M. Lilly, PhD, Writers First Aid, provided assistance in the English translation and copyediting of the manuscript.
GLOSSARY
- AB
atherosclerotic burden
- CAD
coronary artery disease
- CE
cardioaortic embolism
- CI
confidence interval
- HR
hazard ratio
- LAA
large-artery atherosclerosis
- MI
myocardial infarction
- NVE
new vascular event
- PAD
peripheral artery disease
- REACH
Reduction of Atherothrombosis for Continued Health Registry
- SAD
small-artery disease
- SSS-TOAST
Stop Stroke Study Trial of Org 10172 in Acute Stroke Treatment
Footnotes
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
Angel Ois, Elisa Cuadrado-Godia, Ana Rodríguez-Campello, and Jaume Roquer contributed to study design, data interpretation, and revising the manuscript. Eva Giralt-Steinhauer, Jordi Jiménez-Conde, Miguel Lopez-Cuiña, Miguel Ley, and Carol Soriano contributed to data interpretation and revising the manuscript.
STUDY FUNDING
Supported in part by Spain's Ministry of Health (Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III FEDER, RD12/0042/0020).
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Lackland DT, Elkind MS, D'Agostino RS, et al. Inclusion of stroke in cardiovascular risk prediction instruments: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2012;43:1998–2027 [DOI] [PubMed] [Google Scholar]
- 2.Weimar C, Diener H, Alberts MJ, et al. The Essen stroke risk score predicts recurrent cardiovascular events. Stroke 2009;40:350–354 [DOI] [PubMed] [Google Scholar]
- 3.Weimar C, Benemann J, Michalski D, et al. Prediction of recurrent stroke and vascular death in patients with transient ischemic attack or nondisabling stroke. Stroke 2010;41:487–493 [DOI] [PubMed] [Google Scholar]
- 4.Wilson PW, D'Agostino RS, Bhatt DL, et al. An international model to predict recurrent cardiovascular disease. Am J Med 2012;125:695–703 [DOI] [PubMed] [Google Scholar]
- 5.Dhamoon MS, Tai W, Boden-Albala B, et al. Risk of myocardial infarction or vascular death after first ischemic stroke: the Northern Manhattan Study. Stroke 2007;38:1752–1758 [DOI] [PubMed] [Google Scholar]
- 6.Adams HP, Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial: TOAST: Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993;24:35–41 [DOI] [PubMed] [Google Scholar]
- 7.Ay H, Furie KL, Singhal A, Smith WS, Sorensen AG, Koroshetz WJ. An evidence-based causative classification system for acute ischemic stroke. Ann Neurol 2005;58:688–697 [DOI] [PubMed] [Google Scholar]
- 8.Lovett JK, Coull AJ, Rothwell PM. Early risk of recurrence by subtype of ischemic stroke in population-based incidence studies. Neurology 2004;62:569–573 [DOI] [PubMed] [Google Scholar]
- 9.Purroy F, Montaner J, Molina CA, Delgado P, Ribo M, Álvarez-Sabín J. Patterns and predictors of early risk of recurrence after transient ischemic attack with respect to etiologic subtypes. Stroke 2007;38:3225–3229 [DOI] [PubMed] [Google Scholar]
- 10.Bhatt DL, Eagle KA, Ohman EM, et al. Comparative determinants of 4-year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA 2010;304:1350–1357 [DOI] [PubMed] [Google Scholar]
- 11.Ohman EM, Bhatt DL, Steg PG, et al. The REduction of atherothrombosis for continued health (REACH) registry: an international, prospective, observational investigation in subjects at risk for atherothrombotic events-study design. Am Heart J 2006;151:786.e1–786.e10 [DOI] [PubMed] [Google Scholar]
- 12.Ois A, Cuadrado-Godia E, Rodriguez-Campello A, Jimenez-Conde J, Roquer J. High risk of early neurological recurrence in symptomatic carotid stenosis. Stroke 2009;40:2727–2731 [DOI] [PubMed] [Google Scholar]
- 13.Acharjee S, Qin J, Murphy SA, McCabe C, Cannon CP. Distribution of traditional and novel risk factors and their relation to subsequent cardiovascular events in patients with acute coronary syndromes (from the PROVE IT-TIMI 22 trial). Am J Cardiol 2010;105:619–623 [DOI] [PubMed] [Google Scholar]
- 14.Roquer J, Ois A, Rodriguez-Campello A, et al. Atherosclerotic burden and early mortality in acute ischemic stroke. Arch Neurol 2007;64:699–704 [DOI] [PubMed] [Google Scholar]
- 15.Venketasubramanian N, Rother J, Bhatt DL, et al. Two-year vascular event rates in patients with symptomatic cerebrovascular disease: the REACH registry. Cerebrovasc Dis 2011;32:254–260 [DOI] [PubMed] [Google Scholar]
- 16.Writing Committee Members, Greenland P, Alpert JS, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation 2010;122:e584–e636 [DOI] [PubMed] [Google Scholar]
- 17.Feng W, Hendry RM, Adams RJ. Risk of recurrent stroke, myocardial infarction, or death in hospitalized stroke patients. Neurology 2010;74:588–593 [DOI] [PubMed] [Google Scholar]
- 18.Kaplan RC, Tirschwell DL, Longstreth WT, et al. Vascular events, mortality, and preventive therapy following ischemic stroke in the elderly. Neurology 2005;65:835–842 [DOI] [PubMed] [Google Scholar]
- 19.Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke 2001;32:2735–2740 [DOI] [PubMed] [Google Scholar]
- 20.Mohan KM, Crichton SL, Grieve AP, Rudd AG, Wolfe CDA, Heuschmann PU. Frequency and predictors for the risk of stroke recurrence up to 10 years after stroke: the South London Stroke Register. J Neurol Neurosurg Psychiatry 2009;80:1012–1018 [DOI] [PubMed] [Google Scholar]
- 21.Jackson C, Sudlow C. Comparing risks of death and recurrent vascular events between lacunar and non-lacunar infarction. Brain 2005;128:2507–2517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shin D, Lee P, Bang O. Mechanisms of recurrence in subtypes of ischemic stroke: a hospital-based follow-up study. Arch Neurol 2005;62:1232–1237 [DOI] [PubMed] [Google Scholar]
- 23.Hohnloser SH, Oldgren J, Yang S, et al. Myocardial ischemic events in patients with atrial fibrillation treated with dabigatran or warfarin in the RE-LY (Randomized Evaluation of Long-term Anticoagulation Therapy) trial/clinical perspective. Circulation 2012;125:669–676 [DOI] [PubMed] [Google Scholar]
- 24.Melkas S, Putaala J, Oksala NKJ, et al. Small-vessel disease relates to poor poststroke survival in a 12-year follow-up. Neurology 2011;76:734–739 [DOI] [PubMed] [Google Scholar]
- 25.Arboix A, Font A, Garro C, García-Eroles L, Comes E, Massons J. Recurrent lacunar infarction following a previous lacunar stroke: a clinical study of 122 patients. J Neurol Neurosurg Psychiatry 2007;78:1392–1394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petty GW, Brown RD, Jr, Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of functional outcome, survival, and recurrence. Stroke 2000;31:1062–1068 [DOI] [PubMed] [Google Scholar]
- 27.SPS3 Investigators Benavente OR, Hart RG, et al. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med 2012;367:817–825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Serena J, Marti-Fàbregas J, Santamarina E, et al. Recurrent stroke and massive right-to-left shunt. Stroke 2008;39:3131–3136 [DOI] [PubMed] [Google Scholar]
- 29.Sumi S, Origasa H, Houkin K, et al. A modified Essen Stroke Risk score for predicting recurrent cardiovascular events: development and validation. Int J Stroke 2013;8:251–257 [DOI] [PubMed] [Google Scholar]
- 30.Bhatt DL, Steg PG, Ohman EM, et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 2006;295:180–189 [DOI] [PubMed] [Google Scholar]
- 31.Ay H, Gungor L, Arsava EM, et al. A score to predict early risk of recurrence after ischemic stroke. Neurology 2010;74:128–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


